Abstract
Background:
A consequence of the COVID-19 pandemic was that the provision of mental health services was reduced in several countries around the world, while the demand for mental health services increased.
Aims:
Our study aims to determine any variation in the number of users served, health appointments, and care activities conducted at 58 Peruvian community mental health centers (CMHCs) between March 2019 and October 2021.
Methods:
Our study used an observational design and analyzed information from the care provided in CMHCs. We evaluate the number of users served, health appointments, and care activities performed per month. The main statistical analysis used segmented regression with Newey-West standard errors, taking into account each month of the evaluation.
Results:
We had 988,456 unique users during the period evaluated. Regarding diagnoses, 7.4% (n = 72,818) had a severe mental problem, 39.4% (n = 389,330) a common mental problem, and 53.2% (n = 526,308) others health problems. The study found a reduction in the number of users served and health care appointments at the 58 CMHCs in March 2020, the month in which the closure measures were declared to reduce COVID-19 infections in Peru. This reduction was followed by an upward trend in the three variables during the pandemic in the 58 CMHCs studied. In, November 2020, 9 months after the pandemic started, the deficit in the average number of users served per month was recovered.
Conclusions:
Our study suggests that CMHCs in the Peruvian system were able to regain care capacity approximately 1 year after the pandemic. In addition, we discuss the efforts made to respond to mental health needs in the context of a global health crisis.
Keywords: Peru, mental health, COVID-19, interrupted time series analysis
Background
The COVID-19 pandemic has affected mental health around the world, increasing the prevalence of anxiety and depression (COVID-19 Mental Disorders Collaborators, 2021). This raise was associated with the increased rate of COVID-19 infection and a decrease in human mobility (COVID-19 Mental Disorders Collaborators, 2021), probably related to confinement measures such as quarantine or curfews (COVID-19 Mental Disorders Collaborators, 2021). Another consequence of the pandemic was that the provision of mental health services were reduced in 93% of countries worldwide, while the demand for mental health services increased (World Health Organization [WHO], 2020). In this situation, most low- and middle-income countries (LMICs) opted to introduce remote services, such as hotlines, video calls, and smartphone apps (Kola et al., 2021).
Peru is a middle-income country that in 2012 initiated a mental health reform that aims to guarantee the right of people with mental health problems to universal and equitable service access (Miranda et al., 2017; Toyama et al., 2017), through the implementation of a community mental health care model. It included, as one of its main strategies, the creation of 315 community mental health centers (CMHCs) throughout the country (Ministerio de Salud, 2018), one per 100,000 inhabitants (Ministerio de Salud, 2018). The CMHCs’ users can receive one or more health appointments per month, and each appointment may include one or more specific care activities, such as a physical evaluation, prescription of medicines, or psychiatric consultation. Since the number of CMHCs has been increasing annually, access to care for people with mental health problems increased from 11% in 2012 to 26% in 2018 (Castillo-Martell & Cutipé-Cárdenas, 2019). As of August 2022, Peru had 248 CMHCs nationwide.
On March 16, 2020, the Peruvian Government announced the first curfew to control the spread of COVID-19, which was one of the strictest and longest in the Americas (Mathieu et al., 2020). The government developed different strategies to reduce the impact of the pandemic, which included restricting mass gatherings of people and face-to-face health care. Despite these measurements, in June 2021, Peru was the country with the highest COVID-19 mortality rate in the world (Coronavirus Resource Center, 2023). Although the lockdown did not have the expected effect in reducing COVID-19 transmission, CMHCs had to provide care with limited capacity and following social distancing measures, which made users’ access more difficult. Therefore, the government implemented a series of policies and guidelines to reduce the mental health impact of the pandemic on the population. First, it established specific care guidelines for the general population (Ministerio de salud, 2020a), health workers (Ministerio de Salud, 2020c), and women victims of violence (Ministerio de Salud, 2020b). Second, it recommended and prioritized telemedicine care. However, many health facilities, including the CMHCs, had no previous experience offering remote care.
There is no available evidence of how the access to and the provision of mental health care in the CMHCs was affected in Peru during the COVID-19 pandemic and if the Government policies guaranteed the continuity of care. Therefore, this study aims to determine any variation in the number of users served, health appointments, and care activities conducted at CMHCs before and during the COVID-19 pandemic in Peru.
Methods
Study design
Our study is an interrupted time series analysis using data from 58 CMHCs from different cities in Peru, between 01 March 2019 and 31 October 2021. We considered 1 year before and one and a half years after the start of the pandemic in order to assess relatively equal periods before and after the blockade period of the Health Information System (HIS). The HIS’s information was requested from the Peruvian Health Ministry’s transparency portal (https://transparencia.gob.pe/enlaces/pte_transparencia_enlaces.aspx?id_entidad=143).
Setting
Our study used information from health care consultations provided by community mental health centers (CMHCs) in different areas of Peru. CMHCs are specialized mental health care centers that provide an array of health services, such as psychiatry, psychology, family medicine, nursing, social work, physical therapy, speech therapy, and rehabilitation. However, not all CMHCs provide this full range of services as it depends on the needs of the population and the capacity of the CMHC to implement them.
Peru implemented several health policies and strategies to strengthen mental health systems during the pandemic (Cavero et al., 2022). However, the Peruvian population experienced an increase in the prevalence of mental health problems; for example, one study found a trend of the increasing prevalence of moderate depressive symptoms since the beginning of the pandemic (David Villarreal-Zegarra et al., 2023).
Participants
Participants were users served in 58 CMHCs located in different geographical areas of Peru, between March 01, 2019 and October 31, 2021.
Information was requested from all CMHCs registered in the National Registry of Health Care Providers (RENIPRESS). We obtained information from 143 CMHCs but excluded those CMHCs that had complete data during the evaluation period. The reasons for not having information during the evaluation period were that the CMHC was established during the evaluation period or that the HIS had not recorded the CMHC’s information at the time of the information request. To be included in the analysis, CMHCs had to have the following sociodemographic data in the database: sex, age, anonymized ID, type of Service, type of health insurance, and diagnosis. A total of 58 CMHCs were obtained and included in the study.
Variables and measurement
Users served per month
Defined as the number of different users receiving care during a given month at all CMHCs.
Health appointments per month
Each time a person is seen is considered one health appointment; therefore, a user may receive one or more appointments per month. Health appointments per month is defined as the total number of health appointments provided by all CMHC in a given month.
Care activities per month
Within a health appointment users may receive one or more care activities, for example, a diagnosis (care activity 1), medication prescription (care activity 2), and a request for further examination (care activity 3). Care activities per month are defined as the total number of activities that all users served in all CMHC received in a given month.
Sociodemographic variables
Participants were classified according to sex (men or women), type of insurance (user pays, compressive health insurance [SIS] which is a national public insurance for all Peruvians who do not have any other insurance and those with low socioeconomic status, social health insurance [EsSalud], and others) and age groups such as children (0–12 years), adolescents (13–17 years), adults (18–64 years), and older adults (65 years and over). Also, we collected data on the health services where users received care (i.e. Psychology, Nursing, Psychiatry, Social Services, Family Medicine, Rehabilitation Medicine, General Medicine, Pharmacy, and others services).
In addition, participants were classified as users with a common mental problem (i.e. depressive episode [F32], recurrent depressive disorder [F33], anxiety disorder [F40], and other anxiety disorders [F41]), users with severe mental problem (i.e. schizophrenia [F20], bipolar disorder [F31]), and users with other health problem (WHO, 2018). A user was defined as having a common or severe mental disorder if at any time during the evaluation period (March 2019 and October 2021), received one of these diagnoses. If a user was diagnosed with a common mental health problem at one health appointment, and a severe mental health problem at another health appointment, the severe mental health problem diagnosis prevailed.
Statistical methods
Our study established a discrete number of measurements per month. We performed descriptive analyses of users served per month and sociodemographic variables of the total users of all 58 CMHCs.
For the interrupted time series analysis, the date on which the blockade was declared in Peru by COVID-19 (March 16, 2020) was considered the censoring period. Linear regression models were used to assess whether the number of users served, the number of health appointments and the number of care activities changed after the onset of the pandemic. A segmented regression analysis with Newey-West standard errors was used to model data for measures before the pandemic (March 1, 2019, to March 15, 2020) and during the pandemic (March 16, 2020, to October 31, 2021; Newey & West, 1987). Monthly time units were used. Only values with a 95% hypothesis test (p < .05) were considered significant. The estimated impact of the COVID-19 pandemic on the outcome (average monthly number of users, health appointments, and care activities) was assessed in terms of the change in level (intercept) and change in slope of the average monthly number over the time series before and after the COVID-19 pandemic disruption. The change in the intercept is only the immediate change in the level of the average monthly number of users, health appointments and care activities. Also, the change in the slope reflects the change in the trend of the average monthly number of users, health appointments, and care activities during each month. In addition, subgroup analyses were performed by sex, mental status, age groups, and type of service. Users with missing data were excluded from the analyses. Cumby-Huizinga (Breusch-Godfrey) tests were used with the ‘actest’ command to test for autocorrelation (Baum et al., 2007). Analyses were performed and tables were created with Stata, version 17.
Ethical aspects
The study protocol was approved by the institutional ethics committee of Universidad Peruana Cayetano Heredia in Lima, Peru (Approval record 573-33-20). Participants’ risk was minimal since all data was retrieved from a public institution that anonymized all participants’ identifiable information before sharing it. No prospective data collection of participants was performed; all data used was retrospective and collected by the Peruvian Ministry of Health. As this was a retrospective evaluation of an open-access database (anonymous), our study did not require informed consent from participants. Finally, we did not have access to any confidential data, hence, conducting these analyses did not represent an ethical hazard.
Results
Characteristics of the CHMCs’ users
Between March 2019 and October 2021, the number of users served per month by all the 58 CMHCs ranged from 19,529 (April 2020) to 41,447 (September 2021). We included 988,456 unique users during the period evaluated. Users served were mostly women (n = 542,033; 54.8%) and aged 18 to 64 years (n = 620,833; 62.8%). Regarding diagnoses, 7.4% (n = 72,818) had a severe mental problem, 39.4% (n = 389,330) a common mental problem and 53.2% (n = 526,308) other health problems. The most frequent services provided were psychology (n = 350,780; 35.4%) and nursing (n = 322,397; 32.7%); and the most common type of insurance among users was the compressive health insurance (n = 652,453; 66.0%). Table 1 shows the total number of users served per month and the sociodemographic characteristics of users from the 58 CMHCs studied.
Table 1.
Distribution of users served per month and sociodemographic characteristics (n = 988,456).
| N | % | |
|---|---|---|
| Months | ||
| Mar-2019 | 23,660 | 2.4 |
| Apr-2019 | 25,637 | 2.6 |
| May-2019 | 30,638 | 3.1 |
| Jun-2019 | 29,509 | 3.0 |
| Jul-2019 | 27,987 | 2.8 |
| Aug-2019 | 28,440 | 2.9 |
| Sep-2019 | 29,273 | 3.0 |
| Oct-2019 | 31,355 | 3.2 |
| Nov-2019 | 30,747 | 3.1 |
| Dec-2019 | 27,179 | 2.7 |
| Jan-2020 | 27,433 | 2.8 |
| Feb-2020 | 27,085 | 2.7 |
| Mar-2020 | 20,915 | 2.1 |
| Apr-2020 | 19,529 | 2.0 |
| May-2020 | 23,874 | 2.4 |
| Jun-2020 | 26,134 | 2.6 |
| Jul-2020 | 28,982 | 2.9 |
| Aug-2020 | 32,022 | 3.2 |
| Sep-2020 | 33,850 | 3.4 |
| Oct-2020 | 37,758 | 3.8 |
| Nov-2020 | 35,860 | 3.6 |
| Dec-2020 | 34,399 | 3.5 |
| Jan-2021 | 31,212 | 3.2 |
| Feb-2021 | 31,559 | 3.2 |
| Mar-2021 | 32,554 | 3.3 |
| Apr-2021 | 32,895 | 3.3 |
| May-2021 | 33,816 | 3.4 |
| Jun-2021 | 35,174 | 3.6 |
| Jul-2021 | 39,173 | 4.0 |
| Aug-2021 | 39,463 | 4.0 |
| Sep-2021 | 41,447 | 4.2 |
| Oct-2021 | 38,897 | 3.9 |
| Age (categories) | ||
| 0–12 | 182,665 | 18.5 |
| 13–17 | 121,037 | 12.2 |
| 18–64 | 620,833 | 62.8 |
| 65 to more | 63,921 | 6.5 |
| Sex | ||
| Women | 542,033 | 54.8 |
| Men | 446,423 | 45.2 |
| Mental status | ||
| Others health problems | 526,308 | 53.2 |
| Common mental health problem | 389,330 | 39.4 |
| Severe mental health problem | 72,818 | 7.4 |
| Type of service | ||
| Others | 63,139 | 6.4 |
| Psychology | 350,780 | 35.4 |
| Nursing | 322,397 | 32.7 |
| Psychiatry | 102,674 | 10.4 |
| Social services | 44,317 | 4.4 |
| Family medicine | 35,469 | 3.6 |
| Rehabilitation medicine | 25,854 | 2.6 |
| General medicine | 26,567 | 2.7 |
| Pharmacy | 17,259 | 1.7 |
| Type of insurance | ||
| User pays | 205,588 | 20.8 |
| SIS | 652,453 | 66.0 |
| EsSalud | 20,741 | 2.1 |
| Others | 109,674 | 11.1 |
Note. Common mental health problem (depressive episode [F32], recurrent depressive disorder [F33], anxiety disorder [F40], and other anxiety disorders [F41]). Severe mental health problem (schizophrenia [F20] and bipolar disorder [F31]). n = number; % = percentage of column.
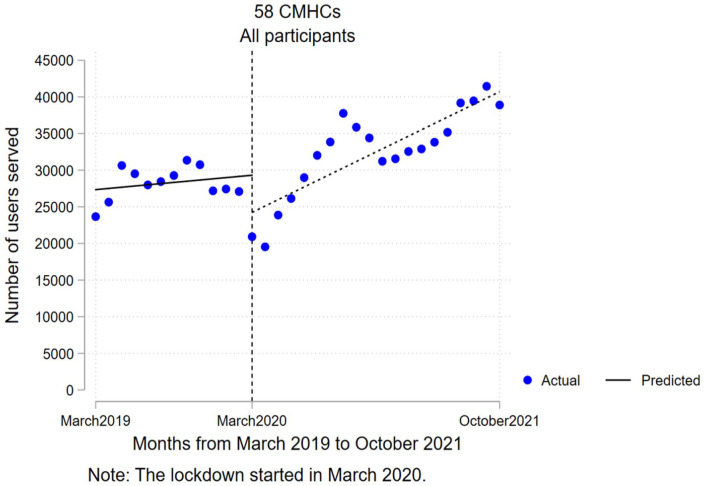
Users served per month
In March 2020, when the pandemic started, there was a reduction in the average monthly number of users served of −5,068.4 (95% CI [−10,416.8, 280.1]), compared with what was expected for that month (see Figure 1). However, this reduction was not significant (p = .062). It should be noted that in the month of the start of the pandemic (15 March 2020), CHMCs were operating normally for half of that month, so the immediate reduction seen at the start of the pandemic is only attributable to half of that month.
Figure 1.
Interrupted time series analysis for the number of users served per month between March 2019 and October 2021.
In addition, during the pandemic (March 2020–October 2021), there was a steady increase in the average number of users served per month, that is, an average monthly increase of 703.5 users served in all CMHCs (95% CI [96.2, 1,310.8]; p = .025) compared to the previous month. This trend of increase in the average number of users seen per month during the pandemic was significant. On the other hand, the analysis of predicted difference versus counterfactual identified that in November 2020, 9 months after the start of the pandemic, the deficit in the average number of users served per month was recovered (Coef. = 559.6; p = .879; 95% CI [−6,922.5, 8,041.7]).
Our study identified some specific subgroups that showed a significant reduction in the average number of users served per month in the first month of the pandemic (March 2020) compared to what was expected for that month based on pre-pandemic measurements (see Table 2). In particular, the biggest reduction were among users aged 0 to 12 years (Coef. = −2,798.1; p = .002; 95% CI [−4,479.8, −1,116.3]) and 13 to 17 years (Coef. = −2,013.8; p = .010; 95% CI [−3,508.9, −518.8]), and among users attending the nursing (Coef. = −2,005.3; p = .043; 95% CI [−3,942.1, −68.5]), and psychiatry services (Coef. = −1,237.3; p < .001; 95% CI [−1,846.0, -628.6]). In addition, we identified a significant trend in the increase of the average number of users served per month during the pandemic for men (Coef. = 424.5; p = .014; 95% CI [92.4, 756.6]), women (Coef. = 279.0; p = .048; 95% CI [2.7, 555.3]), users with other mental health problems (Coef. = 673.7; p = .009; 95% CI [186.1, 1,161.3]), adults (Coef. = 504.2; p = .001; 95% CI [228.0, 780.4]), and older adults (Coef. = 83.0; p = 0.002; 95% CI [33.9, 132.0]). Thus, each month, the number of users in these subgroups increased compared to the previous month, for example, after the start of the pandemic, the average number of older adult users increased by 83 per month in all CMHC.
Table 2.
Interrupted time series regression analysis for the number of users served.
| Coefficients | p-Value | 95% CI | |
|---|---|---|---|
| All user served (see Figure 1) | |||
| Pre intervention slope | 163.5 | .516 | [−345.1, 672.0] |
| Change in intercept | −5,068.4 | .062 | [−10,416.8, 280.1] |
| Change in slope (interaction) | 703.5 | .025 | [96.2, 1,310.8] |
| Intercept | 27,346.2 | .000 | [23,896.5, 30,795.9] |
| Post intervention linear trend | 867.0 | .000 | [563.5, 1,170.5] |
| Sex | |||
| Women | |||
| Pre intervention slope | 106.0 | .433 | [−166.9, 378.9] |
| Change in intercept | −2,724.1 | .075 | [−5,741.0, 292.8] |
| Change in slope (interaction) | 424.5 | .014 | [92.4, 756.6 |
| Intercept | 14,477.4 | .000 | [12,632.4, 16,322.4] |
| Post intervention linear trend | 530.5 | .000 | [357.1, 703.9] |
| Men | |||
| Pre intervention slope | 57.5 | .622 | [−178.9, 293.8] |
| Change in intercept | −2,344.2 | .050 | [−4,690.6, 2.2] |
| Change in slope (interaction) | 279.0 | .048 | [2.7, 555.3] |
| Intercept | 12,868.7 | .000 | [11,257.6, 14,479.9] |
| Post intervention linear trend | 336.5 | .000 | [205.8, 467.1] |
| Mental status | |||
| Others health problems | |||
| Pre intervention slope | −190.2 | .387 | [−633.5, 253.2] |
| Change in intercept | −4,581.2 | .014 | [−8,176.3, −986.2] |
| Change in slope (interaction) | 673.7 | .009 | [186.1, 1,161.3] |
| Intercept | 18,257.7 | .000 | [14,989.6, 21,525.9] |
| Post intervention linear trend | 483.5 | .000 | [287.4, 679.6] |
| Common mental health problem | |||
| Pre intervention slope | 299.2 | .000 | [201.1, 397.3] |
| Change in intercept | −487.0 | .614 | [−2,441.7, 1,467.6] |
| Change in slope (interaction) | 19.1 | .831 | [−162.7, 200.9] |
| Intercept | 7,720.6 | .000 | [7,297.4, 8,143.7] |
| Post intervention linear trend | 318.3 | .000 | [176.6, 459.9] |
| Severe mental health problem | |||
| Pre intervention slope | 54.5 | .000 | [47.4, 61.5] |
| Change in intercept | −0.1 | .999 | [−187.6, 187.3] |
| Change in slope (interaction) | 10.7 | .224 | [−6.9, 28.3] |
| Intercept | 1,367.9 | .000 | [1,319.9, 1,415.8] |
| Post intervention linear trend | 65.2 | .000 | [49.8, 80.5] |
| Age (categories) | |||
| 0–12 | |||
| Pre intervention slope | −28.2 | .808 | [−263.4, 207.1] |
| Change in intercept | −2,798.1 | .002 | [−4,479.8, −1,116.3] |
| Change in slope (interaction) | 79.7 | .493 | [−155.6, 315.1] |
| Intercept | 7,419.7 | .000 | [5,863.3, 8,976.2] |
| Post intervention linear trend | 51.6 | .001 | [24.2, 78.9] |
| 13–17 | |||
| Pre intervention slope | 37.6 | .688 | [−151.8, 226.9] |
| Change in intercept | −2,013.8 | .010 | [−3,508.9, −518.8] |
| Change in slope (interaction) | 36.6 | .698 | [−154.8, 228.0] |
| Intercept | 4,241.7 | .000 | [3,203.2, 5,280.3] |
| Post intervention linear trend | 74.2 | .000 | [49.1, 99.2] |
| 18–64 | |||
| Pre intervention slope | 157.0 | .017 | [30.3, 283.7] |
| Change in intercept | −240.0 | .889 | [−3,742.8, 3,262.8] |
| Change in slope (interaction) | 504.2 | .001 | [228.0, 780.4] |
| Intercept | 14,124.6 | .000 | [13,081.6, 15,167.7] |
| Post intervention linear trend | 661.2 | .000 | [417.9, 904.4] |
| 65 to more | |||
| Pre intervention slope | −2.9 | .817 | [−28.3, 22.5] |
| Change in intercept | −16.5 | .948 | [−530.7, 497.6] |
| Change in slope (interaction) | 83.0 | .002 | [33.9, 132.0] |
| Intercept | 1,560.1 | .000 | [1,361.0, 1,759.1] |
| Post intervention linear trend | 80.1 | .001 | [37.4, 122.7] |
| Type of service | |||
| Psychology | |||
| Pre intervention slope | −13.9 | .921 | [−297.5, 269.7] |
| Change in intercept | 163.5 | .909 | [−2,754.1, 3,081.1] |
| Change in slope (interaction) | 147.2 | .387 | [−196.0, 490.4] |
| Intercept | 10,200.7 | .000 | [8,369.4, 12,032.0] |
| Post intervention linear trend | 133.3 | .112 | [−32.9, 299.5] |
| Nursing | |||
| Pre intervention slope | 18.9 | .797 | [−130.0, 167.8] |
| Change in intercept | −2,005.3 | .043 | [−3,942.1, −68.5] |
| Change in slope (interaction) | 161.4 | .111 | [−39.4, 362.2] |
| Intercept | 10,072.0 | .000 | [8,814.0, 11,329.9] |
| Post intervention linear trend | 180.3 | .010 | [47.4, 313.1] |
| Psychiatry | |||
| Pre intervention slope | 62.8 | .022 | [9.7, 115.9] |
| Change in intercept | −1,237.3 | .000 | [−1,846.0, −628.6] |
| Change in slope (interaction) | 48.8 | .097 | [−9.3, 106.9] |
| Intercept | 2,722.4 | .000 | [2,370.9, 3,074.0] |
| Post intervention linear trend | 111.6 | .000 | [83.9, 139.2] |
Note. Intercept: The number of users served at the beginning of the study period. Pre intervention slope: The previous trend of number of users served. Change in intercept: Change in the number of users served at the beginning of the COVID-19 lockdown. Change in slope (interaction): Change in the trend of number of users served over the time after March 2020. Autocorrelation in lag(1) was considered.
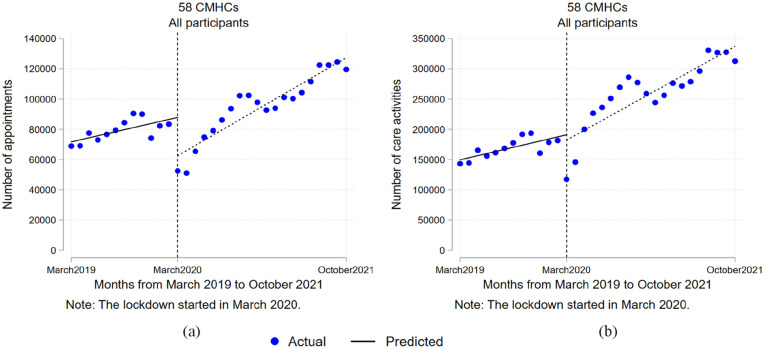
Health appointments and care activities per month
The number of health appointments per month decreased significantly in March 2020 by −25,356.8 health appointments, compared with what was expected for that month (p = .001; 95% CI [−38,940.5, −11,773.0]). However, there was not a significant reduction in the number of care activities at the start of the pandemic, compared with what was expected for that month (Coef. = −8,933.6; p = .696; 95% CI [−55,338.9, 37,471.7]). On the other hand, during the pandemic, there was an upward trend in the average number of health appointments and care activities. That is, between March 2020 and October 2021, each month there were 2,055.3 more health appointments on average (p = .002; 95% CI [836.8, 3,273.8]; see Figure 2(a)) and 4,723.4 more care activities on average (p = .018; 95% CI [856.6, 8,590.1]; see Figure 2(b)), compared to the previous month in all CMHCs. The average number of health appointments and care activities per month, according to each sociodemographic variable can be found in supplementary materials 1 and 2, respectively.
Figure 2.
Interrupted time series analysis for the number of health appointments and care activities per month: (a) analysis for the health appointments per month and (b) analysis for care activities per month.
Discussion
This study showed a decrease in the number of users served, of health appointments and care activities per month, in 58 CMHCs in Peru, during the first 2 months of the COVID-19 pandemic. This decrease may be due to the strict movement restrictions and social isolation measures implemented by the Peruvian government to prevent the spread of COVID-19 (Ministerio de Salud, 2020e). In addition, during the early stages of the pandemic, some mental health services were completely closed to prevent the transmission and spread of COVID-19, CMHCs canceled outpatient consultations, and emergency services were limited due to a lack of protective equipment for medical staff (Salazar Vega, 2020). Furthermore, users may have experienced fear of COVID-19 when approaching CMHCs (Sotomayor-Beltran et al., 2021). The closure of mental health services that occurred in Peru during the early months of the pandemic was also implemented in different countries around the world (Duden et al., 2022), and coincided with a decline in the referrals and presentations of users to community mental health services in different settings (Sheridan Rains et al., 2021).
However, after this initial and brief decrease, there was a sustained upward trend from March 2020 to October 2021 in the number of users served, health appointments, and care activities per month performed by the CMHCs. The increasing trend in the number of users served during the pandemic could be explained by the implementation of mental health policies and guidelines from the second month of the pandemic, which established procedures and recommendations for offering virtual care (telemedicine) in CMHCs in the context of the COVID-19 pandemic (Ministerio de salud, 2020a, 2020b). Also, the public healthcare system implemented strategies such as increasing the budget available for mental health (Ministerio de Salud, 2020e), adapting health centers for staff mental health care (EsSalud, 2020); equipping health centers with technological resources such as computers, cell phones and telephone lines, and personal protection equipment (Ministerio de salud, 2020a); training health personnel in the use of technology (Ministerio de salud, 2021a); and hiring new personnel to strengthen mental health care (Ministerio de Salud, 2021b). All these strategies could have favored a return to face-to-face activities complemented by remote services. In addition, it is noteworthy that this increasing trend coincided with an increase in the prevalence of mental disorders in the general population, as occurred with depression, anxiety, and stress during the COVID-19 pandemic at 33%, 31.9%, and 29.6%, respectively (Salari et al., 2020), exceeding the prevalence prior to the pandemic (Salari et al., 2020), or as has been described, that confinement in COVID-19 resulted in significant levels of stress and anxiety in individuals (Brooks et al., 2020). This increase in the percentage of the population suffering mental distress may have been reflected in a gradual increase in the demand for mental health services, which may have been facilitated by the implementation of telehealth services and the progressive resumption of face-to-face activities in the CMHCs.
Our study reveals that, at the very beginning of the pandemic, the CMHCs included in the study reduced their capacity to provide care, but they managed to recover their previous capacity to provide care in November 2020, 9 months after the pandemic started, and even exceeded their pre-pandemic capacity. These findings suggest that, as a whole, that CMHCs managed to cope with the difficulties that the COVID-19 pandemic produced in mental health services. Our results are consistent with a population-based study that found a trend toward an increase in people with depressive symptoms in Peru who had access to treatment during the pandemic (Villarreal-Zegarra et al., 2023).
To overcome these limitations in care imposed by the pandemic, health services were reorganized, mainly through the provision of remote health services (telemedicine) in order to reduce COVID-19 infections; thus, services provided by CMHCs were also gradually transformed into online or telehealth services in the following months (Cavero, et al., 2022). However, mental telemedicine access and care present challenges to consider, such as that most CMHC users come from low-income areas with limited access to technology (Weigel et al., 2020), and that technological disparities among patients primarily affect low-income persons (Schriger et al., 2022). Considering that people in highest income quintile in Peru are five times more likely to access mental health treatment than those in the lowest income quintile (Villarreal-Zegarra et al., 2020); it is highly likely that low-income groups were the most affected by access to and receipt of telemedicine services during the pandemic and thus suffered the greatest impact on their well-being. Thus, although the implementation of telemedicine services may have facilitated access to mental health services, as reflected by the increase in the number of users served by this modality (Villarreal-Zegarra et al., 2020), it does not necessarily mean that the remote services provided were the most appropriate. For example, telemedicine service could mean not being able to fully see the patient’s reactions, dealing with privacy problems at the time of care (Villarreal-Zegarra et al., 2022), and lacking the adequate technological resources to properly deliver and receive remote mental care (Schriger et al., 2022). Similarly, having little training in the use of technology and not having a stable internet connection, could have had a negative impact on the implementation of telemedicine and affect the impact of remote therapies (Schriger et al., 2022; Villarreal-Zegarra et al., 2022). Additionally, our study did not obtain telemedicine data from the HIS, so it is not possible to assess its evolution during the pandemic.
On the other hand, both the initial reduction and the subsequent increase in the trend of users attended, as well as appointments and activities performed in CMHCs reported in this study coincided with studies conducted in others mental health systems, where the same analysis (uninterrupted time series analysis) was used to estimate changes in user care in different health centers. One study in South Africa found that the levels of hospital admissions and outpatient consultations were reduced from the COVID-19 blocking measures, and during the pandemic there was a gradual recovery process in the number of hospital admissions (Wettstein et al., 2022). In other study performed in South-East England, the trend was similar to the previous study, outpatient and community care in mental health services decreased since the application of COVID-19 confinement, followed by a gradual recovery of care (Penington et al., 2022).
Implications for public health
Based on the above, the adaptation to remote services promoted by the Peruvian health system through policies, guidelines, and mental health plans (Ministerio de salud, 2020a, 2020d), was an adequate alternative to maintain the continuity of service in the CMHCs. Therefore, maintaining and strengthening the use of remote care may help to respond to the increasing demands of users for mental health service. In addition, new policies and guidelines could reinforce the complementarity of face-to-face and distance services. This hybrid care could be a feasible and effective option for mental health facilities in LMICs, as it would help to tailor the offer to the services’ resources and the circumstances of each user. This could also allow the health system to respond faster and more effectively to future emergencies in which traditional face-to-face services are disrupted. Also, frameworks for the implementation of teleconsultation and digital health services in mental health now exist (Villarreal-Zegarra et al., 2022), which could help decision-makers to guide the implementation process. Finally, new health policies should also focus on overcoming the current technological constrains of the public services as well as the barriers among users, especially among those with fewer resources that face more challenges to access remote services.
Strengths and limitations
Our study has a number of strengths to highlight. First, the study included information from 58 facilities, representing almost 25% of all the Peru CMHCs, which allows us to obtain a nationwide idea of the provision of mental health care during the pandemic. Second, by using data covering the pre-pandemic and pandemic periods, the study allows a comparison of changes in the trend in the number of care visits in the pandemic period with the trend predicted by the pre-pandemic data.
Finally, our study has some limitations. First, the HIS does not distinguish between face-to-face and virtual activities. Therefore, we do not know if how much of the increase in visits is due to teleconsultations. Second, the HIS data are completed by health professionals; however, recording criteria may vary between different CMHCs and between different professionals. Therefore, there may be cases with inadequate data collection. Third, our study is observational; therefore, no claims of causality can be made.
Conclusions
This study examined changes and trends in the monthly number of users served, health appointments, and activities performed in 58 community mental health centers (CMHCs) in Peru, before and during the COVID-19 pandemic (from March 2019 to October 2021). The study found a significant reduction in the number of users served and health care appointments at the 58 CMHCs studied in March 2020, the month in which the closure measures were declared to reduce COVID-19 infections in Peru. This reduction was followed by an upward trend in the number of users, appointments and activities during the pandemic. The CMHCs were able to regain care capacity 1 year after the pandemic and made efforts to respond to mental health needs in the context of a global health crisis.
As a final recommendation, the authors urge policymakers to consider strengthening mental health services in the short and medium term. Likewise, we recommend the use of alternative health services such as telemedicine to improve the public health system, to be better prepared for future health emergencies.
Supplemental Material
Supplemental material, sj-docx-1-isp-10.1177_00207640231185026 for Provision of community mental health care before and during the COVID-19 pandemic: A time series analysis in Peru by David Villarreal-Zegarra, Piero Segovia-Bacilio, Rubí Paredes-Angeles, Ana Lucía Vilela-Estrada, Victoria Cavero and Francisco Diez-Canseco in International Journal of Social Psychiatry
Acknowledgments
The authors thank Percy Soto and Akram Hernández for their support and assistance in the development of the data analysis.
Footnotes
Author contributions: David Villarreal-Zegarra: Conceptualization, Methodology, Software, Formal analysis, Data Curation, Writing – Original Draft, Visualization. Piero Segovia-Bacilio: Methodology, Formal analysis, Investigation, Writing – Original Draft, Visualization. Rubí Paredes-Angeles: Investigation, Data Curation, Writing – Review & Editing. Ana Lucía Vilela-Estrada: Conceptualization, Investigation, Writing – Review & Editing, Supervision. Victoria Cavero: Conceptualization, Investigation, Writing – Review & Editing, Supervision. Francisco Diez-Canseco: Conceptualization, Writing – Review & Editing, Supervision.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental material: Supplemental material for this article is available online.
Availability of data and materials: The data were provided by the Peruvian Ministry of Health and were requested through the Transparency Portal. The request is free and can be made through the web page https://www.gob.pe/432-acceso-a-la-informacion-publica.
Ethics approval and consent to participate: The study protocol was approved by the institutional ethics committee of Universidad Peruana Cayetano Heredia in Lima, Peru (Approval record 573-33-20). The ethical risk for the participants is minimal since the data are the product of a secondary analysis of a publicly accessible database. No prospective data collection of participants was performed, all data used was retrospective and collected by the Peruvian Ministry of Health. As this was a retrospective evaluation of an open-access database (anonymous), our study did not require formal consent from participants. Hence, conducting this analysis did not represent an ethical hazard since there was no access to confidential data.
ORCID iD: David Villarreal-Zegarra  https://orcid.org/0000-0002-2222-4764
https://orcid.org/0000-0002-2222-4764
References
- Baum C. F., Schaffer M. E., Stillman S. (2007). Enhanced routines for instrumental variables/generalized method of moments estimation and testing. The Stata Journal, 7(4), 465–506. [Google Scholar]
- Brooks S. K., Webster R. K., Smith L. E., Woodland L., Wessely S., Greenberg N., Rubin G. J. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet, 395(10227), 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo-Martell H., Cutipé-Cárdenas Y. (2019). Implementation, initial results, and sustainability of the mental health services reform in Peru, 2013–2018. Revista Peruana de Medicina Experimental y Salud Publica, 36(2), 326–333. [DOI] [PubMed] [Google Scholar]
- Cavero V., Vilela-Estrada A. L., Paredes-Angeles R., Cusihuaman-Lope N., Villarreal-Zegarra D., Diez-Canseco F. (2022). Peruvian health government response to mental health care in the context of the COVID-19 pandemic: A scoping review and policy document analysis. OSF. [Google Scholar]
- Coronavirus Resource Center. (2023). Mortality analyses. https://coronavirus.jhu.edu/data/mortality
- COVID-19 Mental Disorders Collaborators. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet, 398(10312), 1700–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duden G. S., Gersdorf S., Stengler K. (2022). Global impact of the COVID-19 pandemic on mental health services: A systematic review. Journal of Psychiatric Research, 154, 354–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EsSalud. (2020). Recomendaciones clínicas para la prevención y manejo de problemas de salud mental en personal de salud en el marco de la pandemia por COVID-19. [Google Scholar]
- Kola L., Kohrt B. A., Hanlon C., Naslund J. A., Sikander S., Balaji M., Benjet C., Cheung E. Y. L., Eaton J., Gonsalves P., Hailemariam M., Luitel N. P., Machado D. B., Misganaw E., Omigbodun O., Roberts T., Salisbury T. T., Shidhaye R., Sunkel C. . . ., Patel V. (2021). COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry, 8(6), 535–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathieu E., Ritchie H., Rodés-Guirao L., Appel C., Giattino C., Hasell J., Macdonald B., Dattani S., Beltekian D., Ortiz-Ospina E., Roser M. (2020). Coronavirus Pandemic (COVID-19). Our World in Data. [Google Scholar]
- Ministerio de Salud. (2018). Plan Nacional de Fortalecimiento de Servicios de Salud Mental Comunitaria 2018–2021. [Google Scholar]
- Ministerio de Salud. (2020. a). Guía Técnica para el cuidado de la salud mental de la población afectada, familias y comunidad, en el contexto del COVID-19, Resolución Ministerial N°186-2020-MINSA C.F.R. [Google Scholar]
- Ministerio de Salud. (2020. b). Guía Técnica para el cuidado de la Salud Mental de la Población Afectada, Familias y Comunidad, en el contexto del COVID-19: Especificaciones para la atención de la salud mental de mujeres víctimas de la violencia de género. [Google Scholar]
- Ministerio de Salud. (2020. c). Guía técnica para el cuidado de la salud mental del personal de la salud en el contexto del COVID-19. [Google Scholar]
- Ministerio de Salud. (2020. d). Plan de salud mental en el contexto de COVID-19. [Google Scholar]
- Ministerio de Salud. (2020. e). Resolución Ministerial N.° 678-2020-MINSA. https://www.gob.pe/institucion/minsa/normas-legales/1129992-678-2020-minsa
- Ministerio de salud. (2021. a). Lineamientos para la Asistencia Técnica y supervisión del Ministerio de Salud a los Gobiernos Regionales para el fortalecimiento de la respuesta frente a la pandemia para la COVID-19. [Google Scholar]
- Ministerio de Salud. (2021. b). Norma Técnica de Salud para la Adecuación de los Servicios de Salud del Primer Nivel de Atención de Salud frente a la pandemia por COVID-19 en el Perú. [Google Scholar]
- Miranda J. J., Diez-Canseco F., Araya R., Cutipe Y., Castillo H., Herrera V., Galea J., Brandt L. R., Toyama M., Cavero V. (2017). Transitioning mental health into primary care. Lancet Psychiatry, 4(2), 90–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newey W. K., West K. D. (1987). A simple, positive semi-definite, heteroskedasticity and autocorrelation consistent covariance matrix. Econometrica, 55(3), 703–708. [Google Scholar]
- Penington E., Lennox B., Geulayov G., Hawton K., Tsiachristas A. (2022). The early impact of the COVID-19 pandemic on patients with severe mental illness: An interrupted time-series study in South-East England. European Psychiatry, 65(1), e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global Health, 16(1), 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar Vega E. (2020). El peso del aislamiento: la salud mental en cuidados intensivos. Lima. [Google Scholar]
- Schriger S. H., Klein M. R., Last B. S., Fernandez-Marcote S., Dallard N., Jones B., Beidas R. S. (2022). Community mental health clinicians’ perspectives on telehealth during the COVID-19 pandemic: Mixed methods study. JMIR Pediatrics and Parenting, 5(1), e29250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan Rains L., Johnson S., Barnett P., Steare T., Needle J. J., Carr S., Lever Taylor B., Bentivegna F., Edbrooke-Childs J., Scott H. R., Rees J., Shah P., Lomani J., Chipp B., Barber N., Dedat Z., Oram S., Morant N.Early impacts of the COVID-19 pandemic on mental health care and on people with mental health conditions: framework synthesis of international experiences and responses. Social Psychiatry and Psychiatric Epidemiology, 56(1), 13–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotomayor-Beltran C., Matta-Solis H., Perez-Siguas R., Matta-Solis E., Matta-Zamudio L. (2021). Fear of COVID-19 among Peruvian People Living in Disadvantaged Communities: A Cross-Sectional Study. Clin Pract Epidemiol Ment Health, 17, 19-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toyama M., Castillo H., Galea J. T., Brandt L. R., Mendoza M., Herrera V., Mitrani M., Cutipé Y., Cavero V., Diez-Canseco F., Jaime Miranda J. . (2017). Peruvian mental health reform: A framework for scaling-up mental health services. International Journal of Health Policy and Management, 6(9), 501–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarreal-Zegarra D., Alarcon-Ruiz C. A., Melendez-Torres G. J., Torres-Puente R., Navarro-Flores A., Cavero V., Huarcaya-Victoria J. (2022). Development of a framework for the implementation of synchronous digital mental health: realist synthesis of systematic reviews. JMIR Mental Health, 9(3), e34760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarreal-Zegarra D., Cabrera-Alva M., Carrillo-Larco R. M., Bernabe-Ortiz A. (2020). Trends in the prevalence and treatment of depressive symptoms in Peru: A population-based study. BMJ Open, 10(7), e036777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarreal-Zegarra D., Reátegui-Rivera C. M., Otazú-Alfaro S., Yantas-Alcantara G., Soto-Becerra P., Melendez-Torres G. J. (2023). Estimated impact of the COVID-19 pandemic on the prevalence and treatment of depressive symptoms in Peru: An interrupted time series analysis in 2014–2021. Social Psychiatry and Psychiatric Epidemiology. Advance online publication. 10.1007/s00127-023-02446-8. [DOI] [PMC free article] [PubMed]
- Weigel G., Ramaswamy A., Sobel L., Salganicoff A., Cubanski J., Freed M. (2020). Opportunities and barriers for telemedicine in the U.S. during the COVID-19 emergency and beyond. Women’s Health Policy. [Google Scholar]
- Wettstein A., Tlali M., Joska J. A., Cornell M., Skrivankova V. W., Seedat S., Mouton J. P., van den Heuvel L. L., Maxwell N., Davies M. A., Maartens G., Egger M., Haas A. D. (2022). The effect of the COVID-19 lockdown on mental health care use in South Africa: An interrupted time-series analysis. Epidemiology and Psychiatric Sciences, 31, e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2018). International statistical classification of diseases and related health problems (11th ed.). [Google Scholar]
- World Health Organization. (2020). COVID-19 disrupting mental health services in most countries, WHO survey. https://www.who.int/news/item/05-10-2020-covid-19-disrupting-mental-health-services-in-most-countries-who-surveys
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-isp-10.1177_00207640231185026 for Provision of community mental health care before and during the COVID-19 pandemic: A time series analysis in Peru by David Villarreal-Zegarra, Piero Segovia-Bacilio, Rubí Paredes-Angeles, Ana Lucía Vilela-Estrada, Victoria Cavero and Francisco Diez-Canseco in International Journal of Social Psychiatry