Abstract
Background
The scapholunate interosseous ligament (SLIL) is an important contributor to wrist stability and functionality. SLIL injury is debilitating and therefore many surgical techniques have been proposed, but the optimal treatment modality remains debated.
This meta-analysis reviews the available literature comparing surgical techniques used in the treatment of chronic SLIL to determine the best approach.
Methods
An electronic search of the literature was conducted to identify all randomized controlled trials and cohort studies published before January 2019 that evaluated clinical outcomes of capsulodesis reconstruction, the modified Brunelli technique, and the reduction and association of the scaphoid and lunate (RASL) procedure for treatment of chronic SLIL. A chi-square analysis was performed to identify possible differences between each technique for several outcome measures.
Results
A total 20 studies encompassing 409 patients met inclusion criteria. Average age among patients was 36.7 years, and 68.2% of patients were male. Reductions in visual analog scale pain scale; Disabilities of Arm, Shoulder, and Hand (DASH) scores; and increases in grip strength and range of motion were observed for all techniques. Capsulodesis was superior to the modified Brunelli technique regarding preserved range of motion.
Conclusions
No significant differences were observed among any of the techniques for pain, DASH score, and grip strength outcomes. Capsulodesis, modified Brunelli, and RASL surgical techniques for the treatment of chronic SLIL injuries may all be seen as reliable methods of treatment of chronic SLIL injuries. While future trials directly comparing these methods are needed, this study suggests there is no superiority of one technique over another.
Keywords: Hand, Wrist, Clinical, Outcomes, Ligament, Scapholunate
Introduction
Scapholunate interosseous ligament (SLIL) injuries are commonly seen in young and active individuals. Such injuries often occur during a fall on an outstretched, extended, and ulnarly deviated hand and can result in wrist dysfunction and chronic complications, such as osteoarthritis.1,3 Normal wrist function depends on the intricate anatomy and mobility of osseoligamentous structures of the joint, and central to this system is the scaphoid, acting as the mediator between proximal and distal rows of the carpal bones.4 The SLIL provides structural support and prevents diastasis and malrotation of the scaphoid and lunate bones. Given its importance to normal wrist functionality, great emphasis has been placed on surgical intervention in scapholunate injuries.
The goals of surgical management are reduction of pain and restoration of normal kinematics. Numerous surgical techniques have been proposed with these goals in mind. A 2004 survey of the American and Canadian Hand Surgeons regarding management of scapholunate instability showed that the majority of surgeons favor scapholunate repair combined with a capsulodesis for acute cases, while Blatt capsulodesis, capsulodesis combined with a scapholunate ligament repair, or scaphotrapezium-trapezoid arthrodesis are reserved for chronic cases.2 Still other authors have advocated the use of the reduction and association of the scaphoid and lunate (RASL) procedure. They have shown the procedure to be a safe and effective treatment for chronic, static scapholunate dissociation as it realigns the scaphoid and lunate, restores function, reduces pain, and may be robust over time.3
Studies attempting to create algorithms for arthroscopic surgical techniques based on the Geissler classification have suggested that the degree of injury is the principal determining factor for optimal choice of procedure.5,6 Despite such studies, management is largely influenced by individual preference rather than objective consensus among hand specialists.
Investigations of 3 commonly used surgical approaches for chronic SLIL injury, including capsulodesis, modified Brunelli procedure, and the RASL procedure, have reported conflicting data on surgical outcomes.7,9 The modified Brunelli procedure is described as ligamentous reconstruction using the flexor carpi radialis tendon by a combined dorsal and volar approach, which has been shown to have promising short-term results.10 Due to a lack of consensus on optimal treatment among hand surgeons, the authors have conducted a systematic review and meta-analysis to investigate differences in outcomes of these 3 surgical techniques used for chronic SLIL repair.
Methods
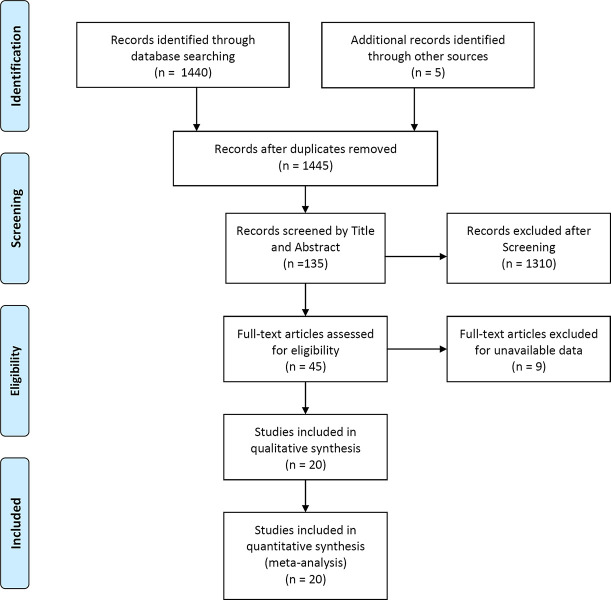
A systematic review and meta-analysis was performed according to the methods of the Cochrane Handbook for Systematic Reviews of Interventions.11 The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Statement was followed for data collection and reporting (Figure 1).12
Figure 1.
Literature review flow chart.
Search Strategy
An electronic literature search of PubMed, Embase, Ovid, and the Cochrane Library was performed in January 2019 using the search terms scapholunate ligament and scapholunate instability. Queries for titles and abstracts from the initial search were used to identify original articles that measured outcomes for these 3 procedures utilized in the surgical repair of SLIL injuries. The bibliographies of these articles were then reviewed for other potentially relevant studies based on their titles. No start publication date was established; any article identified that was published before January 1, 2019, was considered for inclusion. In addition, reference lists of previous reviews of similar topics were searched for relevant studies.
Study Selection
Two authors independently conducted the initial search, involving screening the titles and abstracts for relevance and deleting duplicate records. Systematic reviews, animal, cadaveric, and non-English studies, as well as studies that did not report outcomes data, were excluded. All studies included in the final analysis were those that (1) evaluated the outcomes of patients with SLIL who underwent surgery with capsulodesis, modified Brunelli, or the RASL procedure; (2) were a randomized controlled trial, prospective cohort study, or retrospective cohort study; and (3) provided data on at least one of the following outcomes on both a preoperative and postoperative basis: flexion/extension range of motion; grip strength; level of pain; and/or Disabilities of Arm, Shoulder, and Hand (DASH) score. Comparing changes in grip strength along with overall flexion and extension allowed for measurements of physiologic function. The DASH was used as a measure because it has been demonstrated to be an adequate assessor of upper-limb (including wrist) function and symptomology with good reliability, validity, and responsiveness.8
Data on the year of publication, level of evidence, number of patients in study, number of patients receiving surgery, average age, sex, level of pain, range of motion, grip strength, DASH score, and length of follow-up were extracted. Outcomes data were collected from the final follow-up for each study included in the analysis.
Quality Assessment
The scientific quality of each included study was assessed according to the Oxford Centre for Evidence-based Medicine Levels of Evidence.13 The studies ranged from level 1 to level 5 based on the judgments for the outcome regarding risk of bias, inconsistency, indirectness, and imprecisions.
Statistical Analysis
Data were pooled for meta-analysis using a random-effects model to accommodate heterogeneity among study results. Continuous outcomes data (ie, level of pain, grip strength, range of motion, and DASH score) were expressed as the mean difference between values before and after surgery. The differences between groups were then tested using a chi-square test or a pairwise chi-square test when appropriate. Significance was defined as P < .05. The results of the meta-analysis were analyzed using the R statistical computing environment v3.3.1 with the meta package (R Foundation for Statistical Computing).
Results
Search Results
A total of 1440 articles were identified in the initial literature search. Five additional studies were identified using the references from other articles and abstract searches. After initial screening of titles and abstracts, 45 articles were further assessed for inclusion. After evaluation of the full text of these articles, 20 studies involving 409 patients met the inclusion criteria for the meta-analysis (Figure 1 ; Table).
Table.
Study Characteristics
| First author | Year | Study Design | Intervention | Patients, N | Mean age, y | % male | Mean follow-up, mo |
|---|---|---|---|---|---|---|---|
| Links7 | 2008 | Retrospective | Modified Brunelli | 23 | 30 | 65.2 | 29 |
| Ellanti21 | 2014 | Prospective | Modified Brunelli | 13 | 35 | 69.2 | 12 |
| Elgammal22 | 2015 | Retrospective | Modified Brunelli | 20 | 43 | 95.0 | 24 |
| Ross23 | 2013 | Prospective | Modified Brunelli | 11 | 36 | 81.8 | 14 |
| Pauchard24 | 2013 | Prospective | Three-ligament tenodesis | 19 | 42.8 | 78.9 | 25 |
| Deshmukh14 | 1999 | Prospective | Blatt capsulodesis | 44 | 29 | 54.5 | 22 |
| Misra15 | 2003 | Retrospective | Blatt capsulodesis | 19 | 36 | 63.2 | 22 |
| Muermans26 | 1999 | Retrospective | Blatt capsulodesis | 16 | 30 | 37.5 | 30 |
| Pomerance16 | 2006 | Retrospective | Blatt capsulodesis | 17 | 36 | 70.6 | 66 |
| Luchetti17 | 2010 | Prospective | Modified Mayo capsulodesis | 18 | 35 | 50.0 | 45 |
| Wintman18 | 1995 | Retrospective | Blatt capsulodesis | 20 | 28 | 35.0 | 34 |
| Moran30 | 2005 | Retrospective | Blatt/Mayo capsulodesis | 31 | 38 | 64.5 | 54 |
| Gray31 | 2015 | Retrospective | Bone-ligament-bone graft + dorsal capsulodesis | 24 | 46 | 91.7 | 98 |
| Papadogeorgou32 | 2010 | Retrospective | Dorsal capsulodesis modified with ECRB | 32 | 39 | 71.9 | 50 |
| Szabo27 | 2002 | Prospective | Dorsal intercarpal ligament capsulodesis | 22 | 41 | 81.8 | 25 |
| Gajendran28 | 2007 | Prospective | Dorsal intercarpal ligament capsulodesis | 15 | 42 | 80.0 | 86 |
| Degeorge19 | 2017 | Retrospective | Mayo capsulodesis | 15 | 34.3 | 60.0 | 20 |
| Lavernia29 | 1992 | Retrospective | Blatt capsulodesis | 21 | N/A | 61.9 | 33 |
| De Carli20 | 2017 | Retrospective | Combined dorsal tenodesis-capsulodesis | 20 | 40 | 85.0 | 67 |
| Caloia25 | 2012 | Prospective | RASL | 9 | 44.5 | 88.9 | 35 |
Abbreviations: ECRB, extensor carpi radialis brevis (ligamentoplasty); N/A, not available; RASL, reduction and association of the scaphoid and lunate.
Demographics
Outcomes were reported at a mean follow-up of 41 months (range, 12-98 months), with an average sample size of 20.5 patients (range, 9-44 patients). Weighted average age in the modified Brunelli, capsulodesis, and RASL groups were 37.4, 36.2, and 44.5 years, respectively. Weighted average age among all patients included in this study was 36.7 years. Among the modified Brunelli cohort, 77.9% of patients were male; in comparison, 65.0% and 88.9% of patients were male in the capsulodesis and RASL groups, respectively. Across all groups, 68.2% of patients were male. The weighted average time to surgery was 20.0 months.
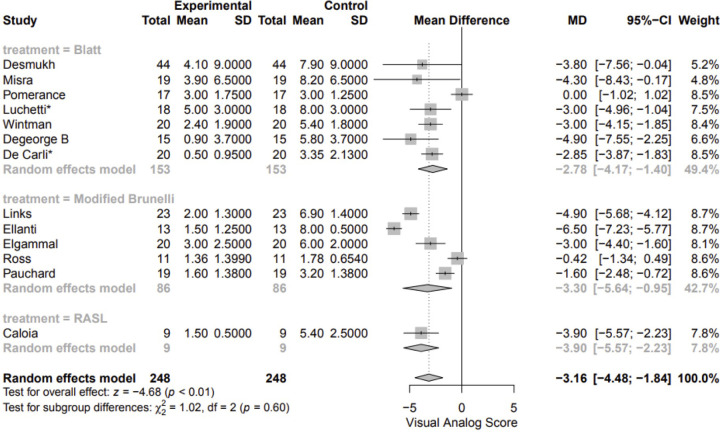
Pain
Pain scores were reported in 13 studies involving 248 patients (Figure 2).7,14,25 For all studies, pain data were measured on a 10-point visual analog scale. Data were available for capsulodesis (n = 7 studies, 153 patients), the modified Brunelli approach (n = 5 studies, 86 patients), and RASL (n = 1 study, 9 patients). Of the 12 studies that provided information about static versus dynamic injury, 75 were static or scapholunate advanced collapse (SLAC) and 164 were dynamic or pre-dynamic. Of the 7 capsulodesis studies, techniques included Blatt (n = 4 studies, 100 patients), Mayo (n = 1 studies, 15 patients), modified Mayo (n = 1 study, 18 patients), and combined dorsal tenodesis-capsulodesis (n = 1 study, 20 patients). The mean postoperative pain improvement for the capsulodesis method was 2.78 points (95% confidence interval [CI], 1.40-4.17 points). The mean pain improvement for the modified Brunelli method was 3.30 points (95% CI, 0.95-5.64 points). The mean improvement for RASL method was 3.90 points (95% CI, 2.23-5.57 points). A 3.16-point improvement in pain was noted after pooling all surgical interventions (95% CI, 1.84-4.48 points; P < .001). Subgroup analysis demonstrated no significant difference among the 3 techniques with respect to pain improvement (P = .60), even after power analysis.
Figure 2.
Pain forest plot.
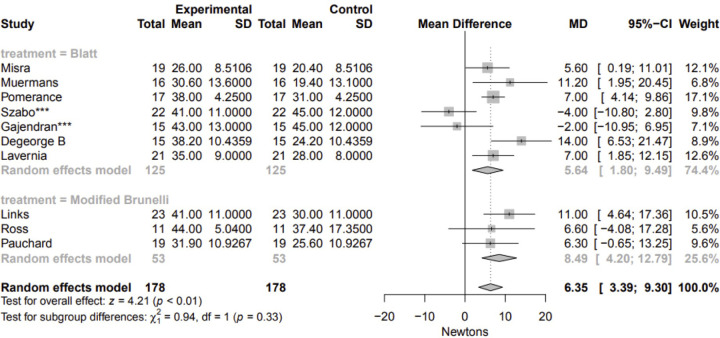
Grip Strength
Data on grip strength were reported in 10 overall studies involving 178 patients undergoing either capsulodesis or the modified Brunelli approach (Figure 3).7,15,16,19,23,24,26,29 Of the 9 studies that provided information about static versus dynamic injury, 84 were static or SLAC and 74 were dynamic or pre-dynamic. Of the 7 capsulodesis studies, techniques included Blatt (n = 4 studies, 73 patients), dorsal intercarpal ligament capsulodesis (n = 2 studies, 37 patients), and Mayo (n = 1 studies, 15 patients). A mean improvement of 6.35 N of grip strength was reported after pooling all surgical interventions (95% CI, 3.39-9.30 N; P < .001). Subgroup analysis demonstrated no significant difference in grip strength improvement for either approach (P = .332). RASL was excluded due to the limited number of studies reporting on grip strength.
Figure 3.
Grip strength forest plot.
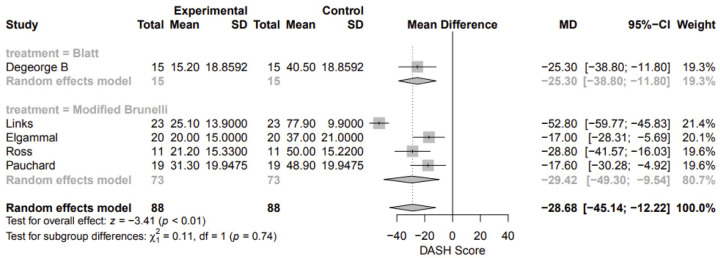
DASH Score
DASH scores were reported in 5 studies involving 88 patients undergoing either capsulodesis (n = 1 studies, 15 patients) or the modified Brunelli approach (n = 4 studies, 73 patients).7,19,22,24 Of these, 50 injuries were static or SLAC, and 38 were dynamic or pre-dynamic. The one capsulodesis study evaluated the Mayo technique. Mean postoperative decrease in DASH score after capsulodesis was 25.30 (95% CI, 11.80-38.80). Mean postoperative decrease after the modified Brunelli approach was 29.42 (95% CI, 9.54-49.30). Pooled results demonstrated a 28.68 decrease in DASH score subsequent to surgery (95% CI, 12.22-45.14). There was no significant difference in DASH scores between these 2 techniques (P = .737). RASL was excluded due to the limited number of studies reporting DASH scores (Figure 4).
Figure 4.
DASH score forest plot.
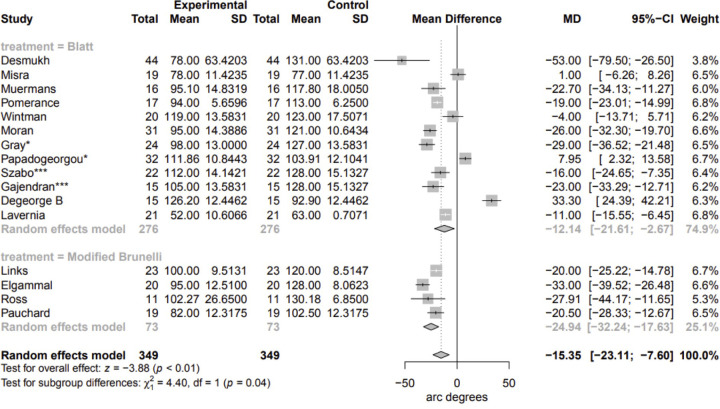
Flexion/Extension
Data on flexion and extension was reported in 16 studies involving 349 patients undergoing either capsulodesis (n = 12 studies, 276 patients) or the modified Brunelli approach (n = 4 studies, 73 patients; Figure 5).7,14,16,18,19,22,24,26,32 Of the 14 studies that provided information about static versus dynamic injury, 122 were static or SLAC and 177 were dynamic or predynamic. Of the 12 capsulodesis studies, techniques included Blatt (n = 6 studies, 137 patients), dorsal intercarpal ligament capsulodesis (n = 2 studies, 37 patients), Mayo (n = 1 study, 15 patients), a mix of Blatt and Mayo techniques (n = 1 study, 31 patients), a combination of bone-ligament-bone graft and dorsal capsulodesis (n = 1 study, 24 patients), and dorsal capsulodesis modified with extensor carpi radialis brevis ligamentoplasty (n = 1 study, 32 patients). On average, the capsulodesis technique resulted in a mean decrease of 12.14° of arc postoperatively (95% CI, 2.67°-21.61°). The modified Brunelli technique resulted in a mean decrease of 24.94° of arc (95% CI, 17.63°-32.24°). Pooled results demonstrated a mean decrease of 15.35° of arc subsequent to any surgical intervention (95% CI, 17.63°-23.11°). Subgroup analysis by intervention demonstrated that capsulodesis resulted in a statistically significant improvement in preservation of 12.80° of arc compared with that seen with the modified Brunelli technique (P = .036). RASL was excluded from the analysis due to the limited number of studies reporting on this variable.
Figure 5.
Arc of motion forest plot.
Discussion
Damage to the SLIL is the most common form of traumatic wrist instability and occurs when excessive force is applied to the wrist while it is extended with ulnar deviation, spurring the capitate in between the scaphoid and lunate bones.33 This may occur abruptly through a fall on the outstretched hand or chronically through consistent and repeated weight-bearing on the wrist. An SLIL injury classically presents as pain along the radial and dorsal aspects of the wrist and is commonly associated with pain, loss of range of motion, and decreased grip strength, drastically impacting a patient's quality of life.34,35 SLIL tears may also progress to arthritis in nearly a quarter of all cases.10 As such, early recognition and treatment of this injury is a priority among hand surgeons.
Numerous surgical approaches have been described in the treatment of SLIL injuries. There is general consensus of the preferred surgical approach in setting of acute scapholunate instability, with primary scapholunate ligament repair with or without augmentation with capsulodesis as the preferred technique.2 In the treatment of chronic scapholunate instability, Blatt capsulodesis is the most common surgical technique, although there is considerably more variability in treatment methods among practicing surgeons than is seen in acute injury.2 Each strategy varies in its efficacy of reducing pain and restoration of normal biomechanical function, and no consensus exists about an optimal treatment method.30,36 The majority of the existing literature comparing different surgical approaches is limited to small-scale, isolated studies.7 The current analysis shows that patients who underwent capsulodesis had increased flexion and extension compared with those receiving the modified Brunelli. Additionally, there was no difference observed in DASH score or grip strength between the modified Brunelli approach and capsulodesis, and no significant difference in pain was seen among patients undergoing the modified Brunelli, capsulodesis, and RASL approaches.
Capsulodesis was first described for the treatment of SLIL in 1987 and is currently one of the most commonly utilized surgical methods aimed at preventing subluxation of the scaphoid.26,37 Wintman et al demonstrated the effectiveness of this method in decreasing pain while restoring functionality by assessing patients’ performances of common tasks, such as jar opening, throwing, and shoveling.18 In a study by Misra et al, 13 of 15 patients who underwent capsulodesis experienced excellent or good clinical results and were able to return to their original levels of activity.15 Additionally, this procedure has been shown to decrease pain for both dynamic and static SL instability at the cost of decreased range of motion.30 The current analysis shows that this approach is superior to the modified Brunelli approach, solely in terms of flexion and extension. As none of the included studies provided direct comparisons between capsulodesis and RASL in terms of range of motion, conclusions between these approaches cannot be drawn for this outcome. This is also true when comparing RASL with the modified Brunelli technique.
The modified Brunelli approach, a revised method of the original Brunelli technique, has persisted over the last 2 decades as one of the primary modes for SLIL instability treatment.38 This surgical approach consists, in part, of removing the formed scar between the scaphoid and lunate bones and subsequently passing a segment of the flexor carpi radialis through the scaphoid bone and attaching it to the lunate.10 Numerous alternatives that make variations of the technique have also been established.39 Ellanti et al showed that this technique was able to drastically reduce preoperative pain levels (from 8 to 1.5 on the visual analog scale) and increase preoperative grip strength (from 40% to 75%) in their study.21 Given the vast literature on the modified Brunelli and its related techniques, as well as the numerous trials that have sought to determine the efficacy of them, its inclusion in this analysis was paramount.22,40,41
The most recently developed of the 3 methods at the focus of this study, RASL, originally used the Herbert screw to buttress the connection between the scaphoid and lunate long enough for soft tissue healing to occur between the two.42 Though reported to produce symptomatic relief, there have been concerns of improper carpal alignment.43 A study by Koehler et al illustrated that, despite overall reductions in pain and increases in grip strength, 7 of 18 patients experienced complications and 4 underwent revision surgeries.44
Data show that all 3 of these surgical approaches—the modified Brunelli, capsulodesis, and RASL—are associated with significant decreases in pain. Lower DASH scores, increases in grip strength, and increases in flexion and extension were seen in patients who were treated with the modified Brunelli or capsulodesis approaches. Notably, there is a lack of data on RASL for these outcomes. Collectively, however, these data suggest that they are all reliable and sufficient ways to treat chronic SLIL injuries. Furthermore, the only difference in outcomes between approaches was seen in flexion and extension, with capsulodesis being superior to the modified Brunelli. Though these results reached statistical significance, the similarities measured among the other outcomes suggest that there is likely little clinical significance to this finding. Therefore, the authors believe that the decision regarding which surgical approach to use in the treatment of chronic SLIL injuries may be appropriately based on physician preference.
Limitations
This study has several important limitations. There is the possibility that some articles have been missed during the authors’ systematic review and thus would alter the true overall results for that method. Additionally, there were only 3 studies that had data on RASL, limiting the conclusions that can be drawn using this approach. Furthermore, the limited number of studies in RASL involved patients whose mean age was higher than that of patients in the capsulodesis and modified Brunelli groups and therefore may negatively impact comparison. Surgeons in these studies may also have chosen one procedure over another on the basis of other clinical variables that were not examined in this study. There is a spectrum of scapholunate injury severity, as shown by the mix of static and dynamic injuries, which may have influenced surgical decision-making and ultimately outcomes. Additionally, capsulodesis is inherently diverse, and therefore varying methods may add to variability. Lastly, this study does not report follow-up data beyond 4 years that may have provided clinically relevant information regarding the optimal treatment.
Conclusions
This analysis demonstrates that capsulodesis, modified Brunelli, and RASL procedures are all reliable strategies for treating chronic SLIL injuries. The only difference identified among approaches was the improved flexion and extension range of motion with capsulodesis compared with the modified Brunelli technique. Otherwise, each approach significantly decreased pain levels and DASH scores while improving range of motion and grip strength. While the difference in range of motion was statistically significant, this does not suggest that this will always translate to a difference in a clinical setting. Further trials with direct comparisons that account for other clinical variables are needed to identify which method is superior.
Acknowledgments
Ethics: Institutional Review Board approval was not required for completion of this manuscript. There is no information in this manuscript that can be used to identify patients.
References
- 1.Mathoulin C, Dauphin N, Wahegaonkar A. Arthroscopic dorsal capsuloligamentous repair in chronic scapholunate ligament tears. Hand Clin. 2011;27(4):563-572, xi. doi:10.1016/j.hcl.2011.07.003 10.1016/j.hcl.2011.07.003 [DOI] [PubMed] [Google Scholar]
- 2.Zarkadas P, White N, Bertrand P. A survey of the surgical management of acute and chronic scapholunate instability. J Hand Surg. 2004; 29A(5):848-857. doi:10.1016/j.jhsa.2004.05.008 10.1016/j.jhsa.2004.05.008 [DOI] [PubMed] [Google Scholar]
- 3.Mathoulin C. Treatment of dynamic scapholunate instability dissociation: contribution of arthroscopy. Hand Surg Rehabil. 2016;35(6):377-392. doi:10.1016/j.hansur.2016.09.002 10.1016/j.hansur.2016.09.002 [DOI] [PubMed] [Google Scholar]
- 4.Manuel J, Moran S. The diagnosis and treatment of scapholunate instability. Hand Clin. 2010;26(1):129-144. doi:10.1016/j.hcl.2009.08.006 10.1016/j.hcl.2009.08.006 [DOI] [PubMed] [Google Scholar]
- 5.Alonso Rasgado T, Zhang Q, Jimenez Cruz D, et al. Analysis of tenodesis techniques for treatment of scapholunate instability using the finite element method. Int J Numer Method Biomed Eng. 2017;33(12):e2897. doi:10.1002/cnm.2897 10.1002/cnm.2897 [DOI] [PubMed] [Google Scholar]
- 6.Harvey E, Berger R, Osterman A, Fernandez D, Weiss A. Bone-tissue-bone repairs for scapholunate dissociation. J Hand Surg Am. 2007;32(2):256-264. doi:10.1016/j.jhsa.2006.11.011 10.1016/j.jhsa.2006.11.011 [DOI] [PubMed] [Google Scholar]
- 7.Links A, Chin S, Waitayaawinyu T, Trumble T. Scapholunate interosseous ligament reconstruction: results with a modified Brunelli technique versus four-bone weave. J Hand Surg Am. 2008;33(6):850-856. doi:10.1016/j.jhsa.2008.02.010 10.1016/j.jhsa.2008.02.010 [DOI] [PubMed] [Google Scholar]
- 8.Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop. 2008;32(1):1-6. doi:10.1007/s00264-007-0368-z 10.1007/s00264-007-0368-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michelotti B, Adkinson J, Chung K. Chronic scapholunate ligament injury: techniques in repair and reconstruction. Hand Clin. 2015;31(3):437-449. doi:10.1016/j.hcl.2015.04.013 10.1016/j.hcl.2015.04.013 [DOI] [PubMed] [Google Scholar]
- 10.Brunelli GA, Brunelli GR. A new surgical technique for carpal instability with scapho-lunar dislocation (eleven cases). Ann Chir Main Memb Super. 1995;14(4-5):207-213. doi:10.1016/s0753-9053(05)80415-6 [DOI] [PubMed] [Google Scholar]
- 11.Higgins S. Cochrane Handbook for Systematic Reviews of Interventions. Wiley and Sons; 2005. [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman D, PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/joumal.pmed.1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atkins D, Eccles M, Flottorp S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res. 2004;4(1):38. doi:10.1186/1472-6963-4-38 10.1186/1472-6963-4-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deshmukh S, Givissis P, Belloso D, Stanley J, Trail I. Blatt's capsulodesis for chronic scapholunate dissociation. J Hand Surg Br. 1999;24(2):215-220. doi:10.1054/jhsb.1998.0183 10.1054/JHSB.1998.0183 [DOI] [PubMed] [Google Scholar]
- 15.Misra A, Hales P. Blatt's capsulodesis for chronic scapholunate instability. Acta Orthop Belg. 2003;69(3):233-238. [PubMed] [Google Scholar]
- 16.Pomerance J. Outcome after repair of the scapholunate interosseous ligament and dorsal capsulodesis for dynamic scapholunate instability due to trauma. J Hand Surg Am. 2006;31(8):1380-1386. doi:10.1016/j.jhsa.2006.07.005 10.1016/j.jhsa.2006.07.005 [DOI] [PubMed] [Google Scholar]
- 17.Luchetti R, Zorli I, Atzei A, Fairplay T. Dorsal intercarpal ligament capsulodesis for predynamic and dynamic scapholunate instability. J Hand Surg Eur Vol. 2010;35(1):32-37. doi:10.1177/1753193409347686 10.1177/1753193409347686 [DOI] [PubMed] [Google Scholar]
- 18.Wintman B, Gelberman R, Katz J. Dynamic scapholunate instability: results of operative treatment with dorsal capsulodesis. J Hand Surg Am. 1995;20(6):971-979. doi:10.1016/S0363-5023(05)80145-5 10.1016/S0363-5023(05)80145-5 [DOI] [PubMed] [Google Scholar]
- 19.Degeorge B, Coulomb R, Kouyoumdjian P, Mares O. Arthroscopic dorsal capsuloplasty in scapholunate tears EWAS 3: preliminary results after a minimum follow-up of 1 year. J Wrist Surg. 2018;7(4):324-330. doi:10.1055/s-0038-1660446 10.1055/s-0038-1660446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Carli P, Donndorff A, Torres M, Boretto J, Gallucci G. Combined tenodesis- capsulodesis for scapholunate instability: minimum 2-year follow-up. J Wrist Surg. 2017;6(1):11-21. doi:10.1055/s-0036-1583304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ellanti P, Sisodia G, Al-Ajami A, Ellanti P, Harrington P. The modified Brunelli procedure for scapholunate instability: a single centre study. Hand Surg. 2014;19(1):39-42. doi:10.1142/S0218810414500075 10.1142/S0218810414500075 [DOI] [PubMed] [Google Scholar]
- 22.Elgammal A, Lukas B. Mid-term results of ligament tenodesis in treatment of scapholunate dissociation: a retrospective study of 20 patients. J Hand Surg Eur Vol. 2016;41(1):56-63. doi:10.1177/1753193415587871 10.1177/1753193415587871 [DOI] [PubMed] [Google Scholar]
- 23.Ross M, Loveridge J, Cutbush K, Couzens G. Scapholunate ligament reconstruction. J Wrist Surg. 2013;2(2):110-115. doi:10.1055/s-0033-1341962 10.1055/s-0033-1341962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pauchard N, Dederichs A, Segret J, Barbary S, Dap F, Dautel G. The role of three- ligament tenodesis in the treatment of chronic scapholunate instability. J Hand Surg Eur Vol. 2013;38(7):758-766. doi:10.1177/1753193413475753 10.1177/1753193413475753 [DOI] [PubMed] [Google Scholar]
- 25.Caloia M, Caloia H, Pereira E. Arthroscopic scapholunate joint reduction. Is an effective treatment for irreparable scapholunate ligament tears? Clin Orthop Relat Res. 2012;470(4):972-978. doi:10.1007/s11999-011-1953-4 10.1007/s11999-011-1953-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muermans S, De Smet L, Van Ransbeeck H. Blatt dorsal capsulodesis for scapholunate instability. Acta Orthop Belg. 1999;65(4):434-439. [PubMed] [Google Scholar]
- 27.Szabo R, Slater R Jr, Palumbo C, Gerlach T. Dorsal intercarpal ligament capsulodesis for chronic, static scapholunate dissociation: clinical results. J Hand Surg Am. 2002;27(6):978-984. doi:10.1053/jhsu.2002.36523 10.1053/jhsu.2002.36523 [DOI] [PubMed] [Google Scholar]
- 28.Gajendran V, Peterson B, Slater R Jr, Szabo R. Long-term outcomes of dorsal intercarpal ligament capsulodesis for chronic scapholunate dissociation. J Hand Surg Am. 2007;32(9):1323-1333. doi:10.1016/j.jhsa.2007.07.016 10.1016/j.jhsa.2007.07.016 [DOI] [PubMed] [Google Scholar]
- 29.Lavernia C, Cohen M, Taleisnik J. Treatment of scapholunate dissociation by ligamentous repair and capsulodesis. J Hand Surg Am. 1992;17(2):354-359. doi:10.1016/0363-5023(92)90419-p 10.1016/0363-5023(92)90419-P [DOI] [PubMed] [Google Scholar]
- 30.Moran S, Cooney W, Berger R, Strickland J. Capsulodesis for the treatment of chronic scapholunate instability. J Hand Surg Am. 2005;30(1):16-23. doi:10.1016/j.jhsa.2004.07.021 10.1016/j.jhsa.2004.07.021 [DOI] [PubMed] [Google Scholar]
- 31.Gray A, Cuénod P, Papaloïzos MY. Midterm outcome of bone-ligament-bone graft and dorsal capsulodesis for chronic scapholunate instability. J Hand Surg Am. 2015;40(8):1540-1546. doi:10.1016/j.jhsa.2015.04.034 10.1016/j.jhsa.2015.04.034 [DOI] [PubMed] [Google Scholar]
- 32.Papadogeorgou E, Mathoulin C. Extensor carpi radialis brevis ligamentoplasty and dorsal capsulodesis for the treatment of chronic post-traumatic scapholunate instability. Chir Main. 2010;29(3):172-179. doi:10.1016/j.main.2010.03.006 10.1016/j.main.2010.03.006 [DOI] [PubMed] [Google Scholar]
- 33.Elsaftawy A. Proposition of a new classification for scapholunate instability. Pol Przegl Chir. 2013;85(11):676-680. doi:10.2478/pjs-2013-0103 [DOI] [PubMed] [Google Scholar]
- 34.Snider M, Alsaleh K, Mah J. Scapholunate interosseus ligament tears in elite gymnasts. Can J Surg. 2006;49(4):290-291. [PMC free article] [PubMed] [Google Scholar]
- 35.Manuel J, Moran S. The diagnosis and treatment of scapholunate instability. Orthop Clin North Am. 2007;38(2):261-277, vii. doi:10.1016/j.ocl.2007.02.003 10.1016/j.ocl.2007.02.003 [DOI] [PubMed] [Google Scholar]
- 36.Whipple T. The role of arthroscopy in the treatment of scapholunate instability. Hand Clin. 1995;11(1):37-40. 10.1016/S0749-0712(21)00024-X [DOI] [PubMed] [Google Scholar]
- 37.Blatt G. Capsulodesis in reconstructive hand surgery. Dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3(1):81-102. 10.1016/S0749-0712(21)00637-5 [DOI] [PubMed] [Google Scholar]
- 38.Van Den Abbeele KL, Loh YC, Stanley JK, Trail IA. Early results of a modified Brunelli procedure for scapholunate instability. J Hand Surg Br. 1998;23(2):258-261. doi:10.1016/s0266-7681(98)80191-5 10.1016/S0266-7681(98)80191-5 [DOI] [PubMed] [Google Scholar]
- 39.Garcia-Elias M, Lluch A, Stanley J. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006;31(1):125-134. doi:10.1016/j.jhsa.2005.10.011 10.1016/j.jhsa.2005.10.011 [DOI] [PubMed] [Google Scholar]
- 40.Chabas J, Gay A, Valenti D, Guinard D, Legre R. Results of the modified Brunelli tenodesis for treatment of scapholunate instability: a retrospective study of 19 patients. J Hand Surg Am. 2008;33(9):1469-1477. doi:10.1016/j.jhsa.2008.05.031 10.1016/j.jhsa.2008.05.031 [DOI] [PubMed] [Google Scholar]
- 41.Sousa M, Aido R, Freitas D, Trigueiros M, Lemos R, Silva C. Scapholunate ligament reconstruction using a flexor carpi radialis tendon graft. J Hand Surg Am. 2014;39(8):1512-1516. doi:10.1016/j.jhsa.2014.04.031 10.1016/j.jhsa.2014.04.031 [DOI] [PubMed] [Google Scholar]
- 42.Rosenwasser M, Miyasajsa K, Strauch R. The RASL procedure: reduction and association of the scaphoid and lunate using the Herbert screw. Tech Hand Up Extrem Surg. 1997;1(4):263-272. 10.1097/00130911-199712000-00007 [DOI] [PubMed] [Google Scholar]
- 43.Aviles A, Lee S, Hausman M. Arthroscopic reduction-association of the scapholunate. Arthroscopy. 2007;23(1):105.e1-5. doi:10.1016/j.arthro.2006.07.013 10.1016/j.arthro.2006.07.013 [DOI] [PubMed] [Google Scholar]
- 44.Koehler S, Guerra S, Kim J, Sakamoto S, Lovy A, Hausman M. Outcome of arthroscopic reduction association of the scapholunate joint. J Hand Surg Eur Vol. 2016;41(1):48-55. doi:10.1177/1753193415577335 10.1177/1753193415577335 [DOI] [PubMed] [Google Scholar]