Abstract
Background
Research examining the connections between individual adverse childhood experiences (ACEs) and how groupings of interrelated adversities are linked with subsequent health is scarce, limiting our understanding of risk during a period of rapid expansion of ACE screening in clinical practice. The study objective was to conduct a psychometric analysis to derive latent domains of ACEs and related life events and assess the association between each domain and health outcome.
Methods
Participants (3 months-11 years) were recruited from the University of California San Francisco Benioff’s Children Hospital Oakland Primary Care Clinic. Children were screened with the Pediatric ACEs and Related Life Events Screener (PEARLS) (n = 340), which assessed 17 total ACEs and related life events, including forms of abuse, household challenges, and social risks. Domains were constructed using confirmatory factor analysis and associations between the three identified domains and 14 health outcomes were assessed using multivariable linear and logistic regression models.
Results
Three PEARLS domains were identified: Maltreatment (ω = 0.73, ɑ=0.87), Household Challenges (ω = 0.70, ɑ=0.82), and Social Context (ω = 0.55, ɑ=0.70). Measurement invariance was supported across both gender and screening format. All domains were associated with poorer general and behavioral health and stomachaches. Maltreatment and Social Context were additionally associated with eczema while only Social Context was associated with increased odds of reporting headaches and somatic symptoms.
Conclusion
In an underserved, urban west-coast pediatric population, the PEARLS found three adversity domains of Maltreatment, Household Challenges, and Social Context that all had an independent statistically significant association with poorer child health. The results provide a timely and more nuanced representation of risk that can inform clinical practice and policy using more targeted resources and interventions.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12887-023-04163-2.
Keywords: ACEs, Adverse childhood experiences, PEARLS, Factor analysis, Child abuse
Background
Studies have consistently shown that adverse childhood experiences (ACEs) are associated with chronic conditions and proximal poorer health outcomes in childhood/adolescence and later in adulthood [1–3]. Racial/ethnic and socioeconomic disparities exist in ACEs exposure, where Black, Hispanic, and multiracial individuals and those with lower income and education are disproportionately burdened with ACEs [4]. The toxic stress response, which includes neuro-endocrine-immune and genetic regulatory alterations, is considered an important mechanism of how cumulative exposures to early adversities increase risk of morbidity and mortality throughout the life course [5–7]. Cumulative lifetime exposure to social risk factors, such as poverty, discrimination, and unsafe neighborhoods, may trigger similar pathways to toxic stress as traditional ACEs [8]; thus, explicitly including these measures into adversity constructs can have meaningful impact on screening and intervention, especially in safety-net systems that care for underserved populations. Although screening for risk factors for toxic stress has been recommended by the American Academy of Pediatrics [7], screening is only now being more widely incorporated into primary care practice [9].
ACE assessments and related stressful life events have been traditionally implemented and applied as either single adversities or as a cumulative ACE score (i.e., numeric count of total adversities experienced), the latter of which is a powerful tool in assessing risk of toxic stress [2]. However, complementary work examining empirical groupings of individual ACEs (e.g., domains or areas of adversity) and their impact on health remains scarce. Among studies that have examined for domains in assessments of childhood adversity, most have focused solely on the traditional ACE items of maltreatment and household challenges [10–14]. Few have incorporated a wider range of social factors and only examined measurement invariance across sociodemographic characteristics [15–18]. When confirmatory factor analysis is used (i.e., confirming construct validity of factors), measurement invariance across factors can be established if the same questionnaire used in different groups, e.g., gender, shows the factors operate in the same way in each group [19]. As screening for ACEs in primary care settings increases, the urgency to understand the inter-connections between both traditional ACEs and broader social factors, as well as their relationships with health, has been amplified. For example, determining adversity domains may uncover patterns and co-occurrence of ACEs/social risks and mechanisms through which specific combinations of adversities might impact health outcomes [20]. Thus, validation of adversity domains in actively used screening tools, such as the Pediatric ACEs and Related Life Events Screener (PEARLS) [21], has immediate potential impacts on intervention programs and policy aimed at preventing poor health outcomes. Alongside the cumulative ACE score approach – focused on cumulative risk, the identification and application of adversity domains (i.e., how different adversities group together) provides an additional opportunity to more precisely target interventions, strengthen linkages to referrals and resources for patients, and support clinicians in implementing more appropriate referrals.
The Pediatric ACEs and Related Life Event Screener (PEARLS) was developed to measure both ACEs and related life events, including multiple social risk factors [21]. Previous research using this screener has documented that both lifetime exposure to traditional ACEs and to common social risks have a similar and negative cumulative risk to child health [22]. No psychometric properties have been developed for PEARLS so far. To extend these findings and support application and alignment of the PEARLS, toxic stress mitigation, and resource linkage in primary care, the aims of the current study were to: (1) conduct a psychometric analysis to derive a set of latent domains from the PEARLS; (2) demonstrate that the domains maintain measurement invariance across key factors for pediatric care (e.g., age groups, gender, and screening format); and (3) assess the association between domains and pediatric clinical, mental, and behavioral outcomes.
Methods
Study population and design
We used data from the Pediatric ACEs and Resiliency Study, a randomized control study designed to: (1) examine the relationship between ACEs and health outcomes in children and caregivers over time, (2) validate an ACEs screening in a pediatric health care setting, and (3) assess preventative interventions for children with or at risk for toxic stress. Primary results and details of the study design have been presented elsewhere [21, 22]. Briefly, from March 2017 to October 2018, 555 participants ages 3 months to 11 years and their caregivers were enrolled in the study, and 367 were screened for adverse events. Recruitment occurred during well-child checks at the University of California San Francisco Benioff’s Children Hospital Oakland (BCH Oakland) Primary Care Clinic, a safety-net practice that provides care to medically underserved or underinsured populations. Eligibility criteria included: not in foster care, English and/or Spanish speaking, had a primary caregiver ≥ 18 years, and not a sibling of an existing study participant. Participation in the larger parent study included four study visits for survey completion (i.e., surveys asked about a plethora of information such as demographics, social needs, physical and mental health, child regulation, and stress), biospecimen collection (i.e., blood, nasal and buccal swabs, and stool), and participation in a social or psychosocial intervention. Participants were compensated up to $300 for their time participating in the entire study (12 months). The 555 participants had a mean age of 5.9 years (standard deviation [SD] = 3.5) and were predominantly male (52.4%), non-Hispanic Black (56.0%), had caregivers with some college education (65.1%), and were low-income. Caregivers were asked about the child’s ACEs using the PEARLS. Responses were collected in item-level screening format (n = 185) (i.e., caregivers disclosed specific adversities their child has experienced), and aggregate-level screening format (n = 182) (i.e., caregivers reported the total number of adversities their child has experienced). Those screened for aggregate-level responses were later asked to provide item-level responses (n = 155, 85.2%). We limited the present analysis to those with item-level responses, yielding a final sample of 340 children. Written informed consent and where appropriate, oral consent, was obtained. The study was approved by the university institutional review board.
ACEs and related life events
ACEs and related life events were measured using the PEARLS, a 17-item pediatric ACEs screen developed for use in clinical practice [21, 22]. The screen included the ten original ACEs categories, plus related life events including children’s lifetime exposure to: discrimination, food insecurity, housing instability, community violence, physical illness/disability of a caregiver, death of a caregiver, and forced separation from caregiver (each item was dichotomized as yes [coded 1] or no [coded 0]) (refer to Fig. 1 for a list of all 17 ACEs and related life events measured). One of the ten ACEs categories includes exposure to domestic violence, which refers to a child witnessing domestic violence.
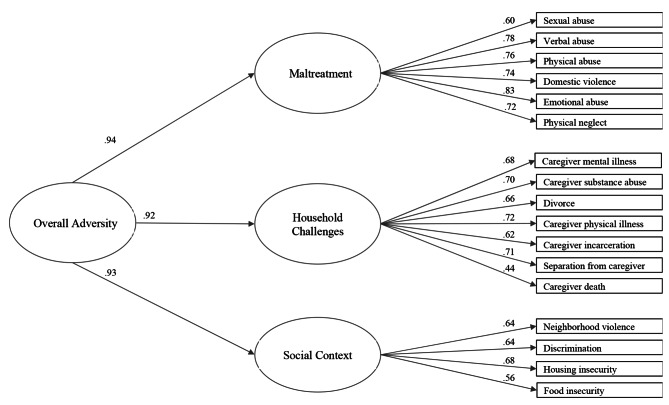
Fig. 1.
Diagram of Confirmatory Three-Factor Model of the Pediatric ACEs and Related Life Events Screener
Outcomes assessment
We assessed key pediatric clinical, mental, and behavioral health outcomes frequently observed in other ACE literature. Child general health was measured via the Patient-Reported Outcomes Measurement Information System (PROMIS) Global 7-item questionnaire that assessed caregiver-reported physical, mental, and social health, pain, fatigue, and perceived quality of life. Each item response was categorized as excellent (coded 5), very good (coded 4), good (coded 3), fair (coded 2), and poor (coded 1), and the scores were summed across the seven items and analyzed as a continuous variable. Total continuous raw scores were converted into t-scores and norm-referenced, in which lower t-scores represent poorer general health (t-score range 14.7 to 66.1) [23]. We also measured caregiver-reported missed school days due to health (1–9 days [coded 0] vs. ≥10 days [coded 1]) and electronic health record (EHR)-based measures for the 12 months preceding recruitment for emergency department (ED) visits and hospitalizations (any visit [coded 1] vs. none [coded 0]). We assessed child behavioral health as a dichotomous variable using the Behavior Rating Inventory of Executive Function (BRIEF 2/P versions administered to appropriate age group) tool, in which a Global Executive Composite scale t-score ≥ 65 was considered clinically significant for poor executive functioning (< 65 [coded 0] vs. ≥ 65 [coded 1]) [24]. Attention Deficit Hyperactivity Disorder (ADHD) diagnosis was based on International Classification of Diseases (ICD)-10 codes in the 12 months prior to recruitment (ADHD coded 1 vs. no ADHD coded 0). Presence of asthma, allergic rhinitis, and atopic dermatitis was obtained using the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire, which was validated and standardized for international use (presence of atopic disease coded 1 vs. no disease coded 0). Height and weight were obtained from clinical exam, and sex- and age-specific body mass index z-scores and percentiles were calculated using 2000 Centers for Disease Control and Prevention growth charts (≥ 95th percentile classified as obese [coded 1] vs. not obese [coded 0]). We used caregiver-reported data on presence of headaches/dizziness and stomachaches in the previous 12 months. EHR ICD-10 codes were retrieved to determine the presence of: (1) acute infections (upper and lower respiratory infection, sinusitis, bronchiolitis, pneumonia, influenza and other viral infections, scarlet fever, otitis media, conjunctivitis, and urinary tract infections); and (2) somatic symptoms (headache, nausea, abdominal pain, epigastric pain, colic, constipation, and migraine) in the 12 months prior to recruitment (presence of conditions [coded 1] vs. no condition [coded 0]).
Covariates assessment
Socio-demographic covariates were identified a priori based on existing literature on childhood adversities and health outcomes, and they were child age (continuous), sex (male coded as 0 vs. female coded as 1), race/ethnicity (categorized as non-Hispanic White [coded 0], Hispanic [coded 1], non-Hispanic Black [coded 2], and other [coded 3]), caregiver education (categorized as some high school or less [coded 0], high school [coded 1], some college [coded 2], and college [coded 3]), and family income ($25,000 or less coded as 0 vs. greater than $25,000 coded as 1) [25].
Statistical analysis
Confirmatory factor analysis (CFA) was used to model the latent structure of the PEARLS items using mean- and variance-adjusted weighted least squares estimation (WLSMV) on the tetrachoric correlations of binary PEARLS screen responses [26]. These latent domains are thus derived from the 17 PEARLS items. Standardized factor loadings ≥ 0.40 were used as an inclusion cut-off. One to three-factor models were tested. Model fit was evaluated using indices of absolute fit and standard guidelines of indices, including the model chi-squared statistics, comparative fit index (CFI ≥ 0.95), Tucker Lewis index (TLI ≥ 0.95), and root mean square error of approximation (RMSEA ≤ 0.06) [27–29]. Given the intercorrelation of the PEARLS items and the aggregate and cumulative scoring of ACEs commonly found in the literature [22], a second order factor structure was included in the CFA to represent an overarching summary measure of adversity. Cronbach’s α and McDonald’s ω were used to determine the internal consistency and reliability of the domains. After domains have been determined, composite scores for each PEARLS domain were computed for each participant by summing the number of affirmative responses within a domain.
Next, we estimated a series of nested multiple group CFAs to determine configural (i.e., factor loading pattern and item thresholds are similar and there is overall acceptable model fit in both groups), metric (i.e., factor loadings are constrained to be equal across groups and fits equally as well as the model with the parameters freely estimated), and scalar (i.e., loadings and item thresholds constrained to be equal) measurement invariance by age group (< 6 vs. ≥ 6 years based on school age), gender, and PEARLS screening format (item-level vs. aggregate-level screening). This approach is consistent with the procedure recommended for use with categorical measures outlined by Svetina et al. (2020).
Multivariable logistic and linear regressions were used to examine the relationship between each PEARLS domain and each health outcome, adjusting for covariates. As exploratory analyses, we included all three domains into one model for each of the outcome models to assess collinearity of the domains.
We performed multiple imputation with iterative chained equations to impute missing socio-demographic covariate data (104 participants had missing data for one or more covariates. Missingness across study variables ranged from 1.5 to 30.6%) [31]. Thirty imputed datasets were generated, and we obtained averaged results from the repeated analyses. Participants missing PEARLS or outcome data were excluded from the analyses. The number of missingness for each measured outcome is different (number and percentages of missingness for each outcome are shown in Table 1).
Table 1.
Child and Caregiver Characteristics
| Characteristic | N (%) Total N = 340 |
|
|---|---|---|
| Age, mean (SD) | 5.8 (3.5) | |
| Sex | ||
| Male | 182 (53.5) | |
| Female | 158 (46.5) | |
| Race | ||
| Non-Hispanic White | 14 (4.1) | |
| Hispanic | 62 (18.2) | |
| Non-Hispanic Black | 188 (55.3) | |
| Other | 76 (22.4) | |
| Caregiver Education | ||
| Some high school or less | 30 (8.8) | |
| High school | 82 (24.1) | |
| Some college | 119 (35.0) | |
| College | 104 (30.6) | |
| Missing | 5 (1.5) | |
| Income | ||
| 25,000 or less | 143 (42.1) | |
| Greater than 25,000 | 93 (27.4) | |
| Missing | 104 (30.6) | |
| PROMIS t-score, mean (SD) | 50.5 (8.7) | |
| Missing | 79 (23.2) | |
| Missed School Days Due to Health | ||
| Less than 10 days | 175 (51.5) | |
| 10 days or more | 44 (12.9) | |
| Missing | 121 (35.6) | |
| ED visit in the past year | ||
| No | 189 (55.6) | |
| Yes | 151 (44.4) | |
| Hospitalization in the past year | ||
| No | 328 (96.5) | |
| Yes | 12 (3.5) | |
| ADHD | ||
| No | 299 (87.9) | |
| Yes | 41 (12.1) | |
| BRIEF-P Global Executive Composite T score, mean (SD) | 55.4 (12.7) | |
| Missing | 148 (43.5) | |
| Stomach Aches | ||
| No | 283 (83.2) | |
| Yes | 46 (13.5) | |
| Missing | 11 (3.2) | |
| Headaches/Dizziness | ||
| No | 293 (86.2) | |
| Yes | 36 (10.6) | |
| Missing | 11 (3.2) | |
| Asthma | ||
| No | 189 (55.6) | |
| Yes | 140 (41.2) | |
| Missing | 11 (3.2) | |
| Rhinitis | ||
| No | 184 (54.1) | |
| Yes | 145 (42.6) | |
| Missing | 11 (3.2) | |
| Eczema | ||
| No | 177 (52.1) | |
| Yes | 151 (44.4) | |
| Missing | 12 (3.5) | |
| Obesity | ||
| No | 257 (75.6) | |
| Yes | 82 (24.1) | |
| Missing | 1 (0.3) | |
| Infections | ||
| No | 174 (51.2) | |
| Yes | 166 (48.8) | |
| Somatic symptoms | ||
| No | 284 (83.5) | |
| Yes | 56 (16.5) | |
| Total ACES score, mean (SD) | 3.2 (3.2) | |
For sensitivity analysis, we compared the averaged results from the multiple imputation to the complete case analysis. Statistical significance was set at p ≤ .05. All analyses were performed with R 3.3.2 [32], STATA version 16 [33], SPSS 26 [34], and Mplus 8.5 [35].
Results
Our study sample (n = 340) was predominantly non-Hispanic Black (n = 188, 55.3%) and low-income (n = 143, 42.1%), with a mean age of 5.8 years (SD = 3.5). Majority of the participants’ caregivers had some college education (n = 223, 65.6%). Participants reported experiencing an average of 3.2 ACEs and related life events (SD = 3.2) (Table 1).
Confirmatory factor analysis structure
Model fit statistics from the CFA demonstrated that a three-factor model with a second order summary factor adequately fit the data (RMSEA = 0.03; CFI and TLI = 0.99) (Table 2), and exhibited better fit compared to the one and two-factor models (Additional File Table S1). The latent structure is depicted in Fig. 1. Domain 1, labeled as Maltreatment, consisted of six items including exposure to sexual abuse, verbal abuse, physical abuse, domestic violence, emotional abuse, and physical neglect (score range 0–6). Exposure to domestic violence was included in the Maltreatment domain because literature suggests that a child just witnessing domestic violence has been recognized as a type of child maltreatment [36–38]. Domain 2, labeled Household Challenges, consisted of seven items that describe the disturbances in the child’s household: caregiver mental illness, caregiver substance abuse, divorce or separation, caregiver physical illness, caregiver incarceration, death of caregiver, and child separation from caregiver (score range 0–7). Domain 3, labeled Social Context, captures four items in the PEARLS that may influence the child’s social environment: neighborhood violence and whether the child experienced discrimination, housing insecurity, or food insecurity (score range 0–4).
Table 2.
Factor Loadings and Scale Reliability Estimates for the Second Order CFA Model
| Loading* | Reliability | |||||
|---|---|---|---|---|---|---|
| Factor | Indicator | % Exposed | β | ω | ɑ | |
| First-order | ||||||
| Maltreatment | Sexual Abuse | 4 | 0.60 | 0.73 | 0.87 | |
| Verbal Abuse | 14 | 0.78 | ||||
| Physical Abuse | 6 | 0.76 | ||||
| Domestic Violence | 34 | 0.74 | ||||
| Emotional Abuse | 18 | 0.83 | ||||
| Physical Neglect | 9 | 0.72 | ||||
|
Household Challenges |
Mental Illness | 39 | 0.68 | 0.70 | 0.82 | |
| Substance Abuse | 20 | 0.70 | ||||
| Divorce | 30 | 0.66 | ||||
| Physical Illness | 14 | 0.72 | ||||
| Incarceration | 23 | 0.62 | ||||
| Separation from Caregiver | 11 | 0.71 | ||||
| Caregiver Death | 9 | 0.44 | ||||
|
Social Context |
Neighborhood Violence | 24 | 0.64 | 0.55 | 0.70 | |
| Discrimination | 15 | 0.64 | ||||
| Housing Insecurity | 24 | 0.68 | ||||
| Food Insecurity | 19 | 0.56 | ||||
| Second-order | ||||||
| Overall Adversity | Maltreatment | 0.94 | ||||
| Household Challenges | 0.92 | |||||
| Social Context | 0.93 | |||||
| Model fit indices: Χ2(116) = 139.68, p = .07; RMSEA = 0.03 [90% CI: 0.00, 0.04]; CFI = 0.99; TLI = 0.99 | ||||||
*All loadings were statistically significant, p < .05
Correlations among the three domains ranged from 0.85 to 0.88. The subscales had acceptable internal consistency and reliability, with alphas ranging from 0.70 to 0.87 and omegas from 0.55 to 0.73 (Table 2). The average number of exposures for each domain was as follows: 0.8 for Maltreatment (SD = 1.2), 1.5 for Household Challenges (SD = 1.6), and 0.8 for Social Context (SD = 1.0).
Measurement invariance for age, gender, and screening format
A summary of the fit statistics for the multiple group CFAs for age group, gender, and PEARLS screening format is shown in Table 3. Configural invariance was established for age, gender, and screening format. Metric invariance was substantiated for gender and screening format, but not for age group. There was a decrease in the mean scores across all three domains for 5-year-olds (Additional File Figure S1). Finally, we observed scalar invariance for gender and screening format when comparing the model with constrained loadings and item thresholds to the previous less constrained model (Table 3).
Table 3.
Summary of Fit Statistics of Measurement Invariance Models across Age, Gender, and PEARLS Screening Format
| Chi-square | Degrees of freedom | p-valuea | RMSEA | CFI | TLI | ||
|---|---|---|---|---|---|---|---|
| Child age (< 6 v 6 + years) | |||||||
| Configural | 268.26 | 232 | -- | 0.03 | 0.96 | 0.96 | |
| Constrain thresholds | 393.42 | 249 | < 0.001 | 0.06 | 0.85 | 0.83 | |
| Constrain thresholds + loadings | 399.02 | 266 | 0.05 | 0.05 | 0.86 | 0.86 | |
| Screening format | |||||||
| Configural | 285.10 | 232 | -- | 0.04 | 0.96 | 0.95 | |
| Constrain threshold | 309.65 | 249 | 0.07 | 0.04 | 0.95 | 0.95 | |
| Constrain thresholds + loadings | 321.08 | 266 | 0.25 | 0.04 | 0.96 | 0.96 | |
| Gender | |||||||
| Configural | 289.16 | 232 | -- | 0.04 | 0.95 | 0.94 | |
| Constrain threshold | 299.99 | 249 | 0.76 | 0.04 | 0.96 | 0.95 | |
| Constrain thresholds + loadings | 321.08 | 266 | 0.25 | 0.04 | 0.96 | 0.96 | |
aComparison between one measurement invariance model to the one above
Associations between PEARLS domains and child outcomes
After adjusting for covariates, we found statistically significant associations between the three domains and child general, mental, and physical health outcomes. All three PEARLS domains when modelled individually had a statistically significant association with lower caregiver ratings of child’s general health as assessed by PROMIS and clinically poorer Global Executive Functioning as measured by BRIEF (Table 4). For specific health outcomes, there were increased odds of stomachaches with greater exposure to Maltreatment, Household Challenges, and adverse Social Context factors. The Social Context domain was additionally associated with headaches (odds ratio [OR] = 1.55; 95% confidence interval [95% CI] [1.10, 2.18]) and somatic symptoms (OR = 1.40; 95% CI [1.05, 1.86]). There was a positive association between eczema and both the Maltreatment (OR = 1.24; 95% CI [1.02, 1.52]) and SocialContext domains (OR = 1.49; 95% CI [1.17, 1.89]) (Table 4).
Table 4.
Associations between PEARLS Factors Modelled Individually and Child Health
| Health outcomes | Maltreatment OR (95% CI)a |
Household challenges OR (95% CI)a |
Social context OR (95% CI)a |
|---|---|---|---|
| PROMISb | -2.29 (-3.14, -1.44) | -1.51 (-2.15, -0.87) | -2.32 (-3.30, -1.33) |
| Missed school days | 1.19 (0.91, 1.56) | 1.21 (0.98, 1.49) | 1.33 (0.97, 1.83) |
| ED visits | 0.85 (0.70, 1.04) | 0.96 (0.83, 1.11) | 1.07 (0.86, 1.34) |
| Hospitalization | 0.61 (0.28, 1.32) | 1.06 (0.72, 1.57) | 0.62 (0.29, 1.34) |
| ADHD | 1.17 (0.89, 1.52) | 1.20 (0.98, 1.48) | 1.09 (0.77, 1.53) |
| BRIEF | 2.48 (1.75, 3.51) | 1.59 (1.26, 2.01) | 2.35 (1.64, 3.37) |
| Stomachaches | 1.38 (1.08, 1.78) | 1.31 (1.08, 1.59) | 1.45 (1.07, 1.96) |
| Headaches | 1.24 (0.94, 1.64) | 1.15 (0.93, 1.42) | 1.55 (1.10, 2.18) |
| Asthma | 1.07 (0.86, 1.33) | 1.16 (0.99, 1.37) | 1.21 (0.94, 1.57) |
| Rhinitis | 1.15 (0.93, 1.42) | 1.13 (0.97, 1.32) | 1.21 (0.95, 1.55) |
| Eczema | 1.24 (1.02, 1.52) | 1.10 (0.95, 1.27) | 1.49 (1.17, 1.89) |
| Obesity | 0.98 (0.79, 1.22) | 0.99 (0.84, 1.17) | 1.09 (0.84, 1.40) |
| Infections | 0.85 (0.70, 1.04) | 0.97 (0.84, 1.13) | 1.02 (0.81, 1.29) |
| Somatic symptoms | 1.01 (0.78, 1.31) | 1.04 (0.85, 1.26) | 1.40 (1.05, 1.86) |
aModels adjusted for child’s age, sex, race/ethnicity, caregiver’s educational level, family income, and screening format. Race/ethnicity was categorized as Non-Hispanic White, Non-Hispanic Black, Hispanic, or other; caregiver’s educational level was categorized as some high school or less, high school graduate, some college, college or greater; family income was dichotomized as <$25,000 vs. ≥ $25,000 annually based on the sample distribution and approximation of federal poverty level for a family of four
bResults are mean differences (95% CI)
When all three domains were included simultaneously in a model, some associations with child health were attenuated. Only Maltreatment remained significantly associated with PROMIS, and both Maltreatment and Social Context were independently associated with poorer Global Executive Functioning. Only Social Context remained significantly associated with physical health symptoms of headaches, eczema, and somatic symptoms (Additional File Table S2).
In sensitivity analyses, the pattern of results from the complete case and multiple imputation analyses was virtually identical.
Discussion
In this psychometric analysis of the PEARLS used in a pediatric population of a safety-net primary care clinic, the findings revealed a three-domain structure with Maltreatment, Household Challenges, and Social Context dimensions as well as a higher order general domain of cumulative child adversity. Findings also demonstrated measurement equivalence across both gender and PEARLS screening format. All three domains were associated with poorer general and behavioral health as well as with stomachaches. Both the Maltreatment and Social Context domains were associated with eczema, while the Social Context domain was additionally associated with headaches. Findings support the presence of three PEARLS domains with practical implications for resource linkage and intervention and demonstrate that each unique relational pattern in the PEARLS items may have an impact on health outcomes. Our validation of the three distinct domains offers a more psychometrically robust approach that is content-specific with immediate clinical applicability to strengthen tailored responses including better identification and distribution of subsequent resources in the clinical, research, and policy settings for exposed individuals that align with each domain.
Findings for the PEARLS domains are consistent with related literature to date [39]. Other studies have similarly derived Maltreatment and Household Challenges subdomains within the traditional ACE categories [1, 40]. Using confirmatory factor analysis, a Canadian study of adolescents found that child maltreatment and household challenges domains were associated with poor mental and physical health, but did not identify a social-environmental factor [41]. A birth cohort study in the United Kingdom derived a “socioeconomic and material disadvantage” (16 p396) domain from the National Survey of Health and Development and found that it was associated with poorer general health in later life [16], similar to our finding with the Social Context domain and outcomes. Although no other study has assessed the same three subdomains of Maltreatment, Household Challenges, and Social Context as latent constructs, one study of court-involved youth looked at three similar theory-derived domains of maltreatment, family dysfunction, and social disadvantage and found similar increased risks for mental health problems with maltreatment and household dysfunction [42].
Findings from the current study additionally support PEARLS domain measurement invariance, which has been largely left out of most of the previous assessments of childhood adversity constructs [11, 13–17, 41, 43–45]. Establishing measurement invariance allows more confident ascertainment of true group differences in a given construct instead of differences based on measurement bias or differences in measure interpretation [19]. We established measurement invariance across both gender and screening format, suggesting that meaningful comparison of domain scores can be made across males and females and across item-level and aggregate-level response ACE screening. We were not able to demonstrate measurement invariance across age groups. There are several possible reasons for this finding. First, a pattern was present in the mean scores across all three domains, in which there was a dip in all domain scores for 5-year-olds, suggesting there may not be static changes in these domains with development. Furthermore, we chose age six as an arbitrary but meaningful cut-point based on school-age and choosing another cut-point might show different results. Whether the PEARLS subscales should be interpreted differently for these age groups requires further investigation that is outside the scope of this analysis.
While all three domains were associated with child health outcomes, our exploratory analyses in which all three domains were included in one model suggest specific independent associations. All three domains were associated with PROMIS score as demonstrated by the three separate models, with Maltreatment capturing additional variance that is not measured by Household Challenges nor Social Context as shown by the exploratory model, as statistical significance was only retained for Maltreatment. We also observed this with eczema, in which statistical significance was only retained for Social Context. This pattern of results is not unexpected given the collinearity between the domains and adversities. The observed pattern of relatedness among the domains suggests that a higher-order overall PEARLS domain exists, which we accounted for using a second order model, and have previously reported on the cumulative risk association with health outcomes [22]. While all three PEARLS domains may be statistically related to some outcomes, suggesting that a broad set of adversities may account for the associations, other outcomes may be associated with fewer domains with different patterns of associations, suggesting that a more specific set of adversities may play a role. Given the diversity of outcomes found to be associated with ACEs, screening across all domains may improve the detection of a child at risk for poor health outcomes. Future research should build evidence on which interventions or resources best support each domain and develop clinical workflows that facilitate support for children and families exposed to each domain.
Establishing domains within the PEARLS as predictors of various health outcomes has immediate implications for clinical practice and policymaking. First, distinct domains provide the opportunity for targeted and tailored treatment and linkage to referrals and resources. Limited accessible supports for children and families who experience adversity and following up positive endorsements of adversities with appropriate, specific interventions and resources are two of the biggest barriers to clinicians supporting trauma screening [46, 47]. If supports can be targeted based on latent domains, more tailored resource and referral linkages can be provided thus maximizing use of often limited resources while avoiding overwhelming services with well-meaning but mis-targeted referrals. Second, clinicians may be less likely to miss or overlook resource linkage opportunities among children with relatively lower cumulative scores if they observe that the few items that are endorsed all fall within one domain. Third, domain scores may also enhance screening by streamlining clinical workflows, while acknowledging that the specific resource within that workflow will depend on the specific adversity. Domains may help point to follow-up screening required for current risk. For example, after administering the initial PEARLS, if clinicians find that their patients endorse one or multiple items within a single domain, they may further investigate the patients’ exposure to similar adversities as part of a more focused follow-up. Use of the distinct domains in this manner may help tailor the response and expedite referral and access to resources. For example, in addition to clinician involvement and anticipatory guidance and follow-up for any ACE exposure, if a patient has a high score for Maltreatment, a clinician may directly refer to an in-house social worker, child protective services (CPS), or mental health resources.
There are some limitations to consider when interpreting these results. First, our study, similar to many other ACEs studies, relied on caregiver-report. Some questions, such as those related to child abuse, may be sensitive and anxiety-inducing to report, potentially leading to underreporting of ACEs [48]. This may also lead to common method variance bias, which occurs when there is variance due to measurement method rather than to the constructs the measures are assumed to represent. However, the observed screening format invariance provides some evidence that differences observed are not due to measurement mode. Also, generalizability of the results is limited because this study focused on pediatric patients in an urban, primary care center that cares for mostly underserved families; thus, further validation is needed in more diverse populations with other age groups and settings. However, these findings can still serve as preliminary construct validation of the PEARLS. In addition, because of the small sample size, our study may be underpowered to detect significant differences. Participants with missing PEARLS or outcome data were excluded from the study, limiting the sample size, and these participants may be different from those who had this data. We also had a large percentage of missingness for the income variable, which we addressed with multiple imputation and the results between the complete case and multiple imputation analyses were similar. Lastly, the timing of certain measurements may have also impacted our results, specifically the EHR data that was collected 12 months prior to recruitment. Some of the younger children may not have as much time to have codes for certain health outcomes reported in the EHR or may not be able to express their exact condition compared to older children, but we attempted to address this by adjusting for age. Also, the PEARLS assesses lifetime prevalence of adversities rather than for exposures that occur at specific time-points after recruitment. Given the cross-sectional design of the analysis, causation cannot be determined. As such, future studies should focus on the longitudinal effects of these adversity domains on health outcomes and how timing and duration of adversity exposure can also impact disease risk. Future studies should also assess how providing tailored responses based on domain positivity moves us toward patient-centered care and helps prevent poor health outcomes.
Conclusion
As a prevention tool, PEARLS screening early in childhood offers an opportunity to link families to resources prior to the onset of negative health outcomes and to mitigate and decrease exposures to childhood adversity. The PEARLS is an efficient way to cumulatively assess Maltreatment, Household Challenges, and Social Context domains while also tailor referral and intervention needs based on domain positivity. All three domains were associated with poorer health in children and complement the current practice of assessing cumulative risk of childhood adversity which can help guide clinical practice and policy.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank our families for sharing and trusting us with their personal experiences and sensitive information. We would also like to acknowledge our study coordinators without whom the study would not be possible: Nitasha Sharma, Cherri Harris, Roberto Mok, Nai Pharn.
Abbreviations
- ACEs
Adverse Childhood Experiences
- PEARLS
Pediatric ACEs and Related Life Events Screener
- BCH Oakland
Benioff’s Children Hospital Oakland
- PROMIS
Patient-Reported Outcomes Measurement Information System
- EHR
Electronic health record
- ED
Emergency department
- BRIEF
Behavior Rating Inventory of Executive Function
- ADHD
Attention Deficit Hyperactivity Disorder
- ICD
International Classification of Diseases
- ISAAC
International Study of Asthma and Allergies in Childhood
- CFA
Confirmatory factor analysis
- WLSMV
Mean- and variance-adjusted weighted least squares estimation
- CFI
Comparative fit index
- TLI
Tucker Lewis index
- RMSEA
Root mean square error of approximation
- SD
Standard deviation
- OR
Odds ratio
- CI
confidence interval
- CPS
Child protective services
Author contributions
M.Y. drafted the initial manuscript, conducted the data analyses, and reviewed and revised the manuscript. N.T., D.H., and D.F. helped with the data analyses. N.T., D.H., D.L., and N.B.H. conceptualized and designed the study. M.B., K.K., and M.B. coordinated all study operations. All the authors reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
This work was supported in part by the TARA Health Foundation, Genentech Corporate Giving, and National Heart, Lung, and Blood Institute (NHLBI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data Availability
The de-identified datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request and on signing of a data-sharing agreement.
Declarations
Competing interests
NT has unexercised stock options in Genentech Inc. Other authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. All methods in our study were performed in accordance with the relevant guidelines and regulations. The study was approved by the Benioff’s Children Hospital Oakland institutional review board. Written informed consent and where appropriate, oral consent, was obtained from all study participants. Informed consent was taken from legally authorized representatives and/or guardians of all minor participants.
Consent for publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Morgan Ye, Email: morganyafang.ye@ucsf.edu.
Danielle Hessler, Email: danielle.hessler@ucsf.edu.
Derek Ford, Email: dcf6e@virginia.edu.
Mindy Benson, Email: mindy.benson@ucsf.edu.
Kadiatou Koita, Email: kadiatoukoita1@gmail.com.
Monica Bucci, Email: mbucci@centerforyouthwellness.org.
Dayna Long, Email: dayna.long@ucsf.edu.
Nadine Burke Harris, Email: nadineburkeharris@gmail.com.
Neeta Thakur, Email: Neeta.Thakur@ucsf.edu.
References
- 1.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245–58. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention . Preventing adverse childhood experiences: leveraging the best available evidence. Atlanta, GA: National Center for Injury Prevention and Control; 2019. [Google Scholar]
- 3.Liming KW, Grube WA. Wellbeing Outcomes for Children Exposed to Multiple Adverse Experiences in Early Childhood: A Systematic Review. Child Adolesc Soc Work J [Internet]. 2018;35(4):317–35. Available from: 10.1007/s10560-018-0532-x.
- 4.Giano Z, Wheeler DL, Hubach RD. The frequencies and disparities of adverse childhood experiences in the U.S. BMC Public Health [Internet]. 2020 Sep 10;20(1):1327. Available from: https://pubmed.ncbi.nlm.nih.gov/32907569. [DOI] [PMC free article] [PubMed]
- 5.Berens AE, Jensen SKG, Nelson CA. Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Medicine. Volume 15. BioMed Central Ltd.; 2017. [DOI] [PMC free article] [PubMed]
- 6.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation–allostatic load and its health consequences. MacArthur studies of successful aging. Arch Intern Med. 1997/10/29. 1997;157(19):2259–68. [PubMed]
- 7.Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, Garner AS, et al. The lifelong Effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 8.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci [Internet]. 2001 Apr 10;98(8):4770 LP – 4775. Available from: http://www.pnas.org/content/98/8/4770.abstract. [DOI] [PMC free article] [PubMed]
- 9.Kerker BD, Storfer-Isser A, Szilagyi M, Stein RE, Garner AS, O’Connor KG, et al. Do Pediatricians ask about adverse childhood Experiences in Pediatric Primary Care? Acad Pediatr. 2016;16(2):154–60. doi: 10.1016/j.acap.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford DC, Merrick MT, Parks SE, Breiding MJ, Gilbert LK, Edwards VJ et al. Examination of the Factorial Structure of Adverse Childhood Experiences and Recommendations for Three Subscale Scores. Psychol Violence [Internet]. 2014 Oct;4(4):432–44. Available from: https://pubmed.ncbi.nlm.nih.gov/26430532. [DOI] [PMC free article] [PubMed]
- 11.Chegeni M, Haghdoost A, Shahrbabaki ME, Shahrbabaki PM, Nakhaee N. Validity and reliability of the Persian version of the Adverse Childhood Experiences Abuse Short Form. J Educ Health Promot [Internet]. 2020 Jun 30;9:140. Available from: https://pubmed.ncbi.nlm.nih.gov/32766325. [DOI] [PMC free article] [PubMed]
- 12.Meinck F, Cosma AP, Mikton C, Baban A. Psychometric properties of the Adverse Childhood Experiences Abuse Short Form (ACE-ASF) among Romanian high school students. Child Abuse Negl [Internet]. 2017;72:326–37. Available from: https://www.sciencedirect.com/science/article/pii/S0145213417302958. [DOI] [PubMed]
- 13.Beal SJ, Wingrove T, Mara CA, Lutz N, Noll JG, Greiner MV. Childhood Adversity and Associated Psychosocial Function in Adolescents with Complex Trauma. Child Youth Care Forum [Internet]. 2018/10/31. 2019 Jun;48(3):305–22. Available from: https://pubmed.ncbi.nlm.nih.gov/31467469. [DOI] [PMC free article] [PubMed]
- 14.Scott BG, Burke NJ, Weems CF, Hellman JL, Carrión VG. The Interrelation of Adverse Childhood Experiences within an At-Risk Pediatric Sample. J Child Adolesc Trauma [Internet]. 2013 Jul 1;6(3):217–29. Available from: 10.1080/19361521.2013.811459.
- 15.Morrill MI, Schulz MS, Nevarez MD, Preacher KJ, Waldinger RJ. Assessing within- and between-family variations in an expanded measure of childhood adversity. Psychol Assess [Internet]. 2019/01/10. 2019 May;31(5):660–73. Available from: https://pubmed.ncbi.nlm.nih.gov/30628820. [DOI] [PMC free article] [PubMed]
- 16.Caleyachetty R, Hardy R, Cooper R, Richards M, Howe LD, Anderson E et al. Modeling Exposure to Multiple Childhood Social Risk Factors and Physical Capability and Common Affective Symptoms in Later Life. J Aging Health [Internet]. 2016/12/22. 2018 Mar;30(3):386–407. Available from: https://pubmed.ncbi.nlm.nih.gov/28553793. [DOI] [PMC free article] [PubMed]
- 17.Mersky JP, Janczewski CE, Topitzes J. Rethinking the Measurement of Adversity: Moving Toward Second-Generation Research on Adverse Childhood Experiences. Child Maltreat [Internet]. 2016 Dec 5;22(1):58–68. Available from: 10.1177/1077559516679513. [DOI] [PubMed]
- 18.Cooper DK, Nickodem K. Cumulative Lifetime Adversity in a National Sample of Hispanic/Latino Immigrants: Exploring Construct Validity Across Six Hispanic/Latino Groups Using Data From the HCHS/SOL Sociocultural Ancillary Study. Eval Health Prof [Internet]. 2020 Mar 13;0163278720910470. Available from: 10.1177/0163278720910470. [DOI] [PMC free article] [PubMed]
- 19.Dimitrov DM. Testing for Factorial Invariance in the Context of Construct Validation. Meas Eval Couns Dev [Internet]. 2010 Jul 1;43(2):121–49. Available from: 10.1177/0748175610373459.
- 20.Anda RF, Porter LE, Brown DW. Inside the Adverse Childhood Experience Score: Strengths, Limitations, and Misapplications. Am J Prev Med [Internet]. 2020;59(2):293–5. Available from: https://www.sciencedirect.com/science/article/pii/S0749379720300581. [DOI] [PubMed]
- 21.Koita K, Long D, Hessler D, Benson M, Daley K, Bucci M, et al. Development and implementation of a pediatric adverse childhood experiences (ACEs) and other determinants of health questionnaire in the pediatric medical home: a pilot study. PLoS ONE. 2018;13(12):e0208088. doi: 10.1371/journal.pone.0208088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thakur N, Hessler D, Koita K, Ye M, Benson M, Gilgoff R et al. Pediatrics adverse childhood experiences and related life events screener (PEARLS) and health in a safety-net practice. Child Abuse Negl [Internet]. 2020;108:104685. Available from: https://www.sciencedirect.com/science/article/pii/S0145213420303409. [DOI] [PMC free article] [PubMed]
- 23.Rothrock NE, Amtmann D, Cook KF. Development and validation of an interpretive guide for PROMIS scores. J Patient-Reported Outcomes [Internet]. 2020;4(1):16. Available from: 10.1186/s41687-020-0181-7. [DOI] [PMC free article] [PubMed]
- 24.Foss-Feig JH, de la Fontaine N, Tsatsanis K. BRIEF (Behavior Rating Inventory of Executive Functions) BT - Encyclopedia of Autism Spectrum Disorders. In: Volkmar FR, editor. New York, NY: Springer New York; 2015. p. 1–5. Available from: 10.1007/978-1-4614-6435-8_102048-1.
- 25.Slopen N, Shonkoff JP, Albert MA, Yoshikawa H, Jacobs A, Stoltz R, et al. Racial disparities in child adversity in the U.S.: interactions with Family Immigration History and Income. Am J Prev Med. 2016;50(1):47–56. doi: 10.1016/j.amepre.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 26.Li C-H. Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods [Internet]. 2016;48(3):936–49. Available from: 10.3758/s13428-015-0619-7. [DOI] [PubMed]
- 27.Bentler PM. Comparative fit indexes in structural models. Vol. 107, Psychological Bulletin. US: American Psychological Association; 1990. pp. 238–46. [DOI] [PubMed] [Google Scholar]
- 28.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. US: Lawrence Erlbaum; 1999. pp. 1–55. [Google Scholar]
- 29.Browne MW, Cudeck R. Alternative Ways of Assessing Model Fit. Sociol Methods & Res [Internet]. 1992;21(2):230–58. Available from: https://econpapers.repec.org/RePEc:sae:somere:v:21:y:1992:i:2:p:230-258.
- 30.Svetina D, Rutkowski L, Rutkowski D. Multiple-Group Invariance with Categorical Outcomes Using Updated Guidelines: An Illustration Using Mplus and the lavaan/semTools Packages. Struct Equ Model A Multidiscip J [Internet]. 2020 Jan 2;27(1):111–30. Available from: 10.1080/10705511.2019.1602776.
- 31.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res [Internet]. 2011 Mar 1;20(1):40–9. Available from: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed]
- 32.R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria; 2022.
- 33.StataCorp . Stata Statistical Software: release 16. College Station. TX: StataCorp LLC; 2019. [Google Scholar]
- 34.Corp IBM. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp; 2019. [Google Scholar]
- 35.Muthén LK, Muthén BO. Mplus User’s Guide. Eighth Edi. Muthén & Muthén, editor. Los Angeles, CA; 2017.
- 36.Walker-Descartes I, Mineo M, Condado LV, Agrawal N. Domestic Violence and Its Effects on Women, Children, and Families. Pediatr Clin North Am [Internet]. 2021;68(2):455–64. Available from: https://www.sciencedirect.com/science/article/pii/S0031395520301838. [DOI] [PubMed]
- 37.McTavish JR, MacGregor JCD, Wathen CN, MacMillan HL. Children’s exposure to intimate partner violence: an overview. Int Rev Psychiatry [Internet]. 2016 Sep 2;28(5):504–18. Available from: 10.1080/09540261.2016.1205001. [DOI] [PubMed]
- 38.Wathen C, Macmillan H. Children’s exposure to intimate partner violence: impacts and interventions. Paediatr Child Health. 2013 Oct;1:18:419–22. [PMC free article] [PubMed]
- 39.Liming K. Examining the Differing Effects of Economic Hardship and poor maternal wellbeing on cumulative exposure to adverse childhood experiences. J Child Adolesc Trauma. 2019 Sep 1;12. [DOI] [PMC free article] [PubMed]
- 40.Choi C, Mersky JP, Janczewski CE, Plummer Lee C-T, Davies WH, Lang AC. Validity of an expanded assessment of adverse childhood experiences: A replication study. Child Youth Serv Rev [Internet]. 2020;117:105216. Available from: https://www.sciencedirect.com/science/article/pii/S0190740920303984.
- 41.Afifi TO, Salmon S, Garcés I, Struck S, Fortier J, Taillieu T et al. Confirmatory factor analysis of adverse childhood experiences (ACEs) among a community-based sample of parents and adolescents. BMC Pediatr [Internet]. 2020 Apr 21;20(1):178. Available from: https://pubmed.ncbi.nlm.nih.gov/32316954. [DOI] [PMC free article] [PubMed]
- 42.Logan-Greene P, Tennyson RL, Nurius PS, Borja S. Adverse Childhood Experiences, Coping Resources, and Mental Health Problems among Court-Involved Youth. Child Youth Care Forum [Internet]. 2017/07/18. 2017;46(6):923–46. Available from: https://pubmed.ncbi.nlm.nih.gov/33132670. [DOI] [PMC free article] [PubMed]
- 43.Karatekin C, Hill M. Expanding the Original Definition of Adverse Childhood Experiences (ACEs). J Child Adolesc Trauma [Internet]. 2018 Nov 12;12(3):289–306. Available from: https://pubmed.ncbi.nlm.nih.gov/32318200. [DOI] [PMC free article] [PubMed]
- 44.Weller BE, Conrad JK, Wilburn VG, Ramamonjiarivelo Z, Gladden J. Adverse childhood experiences and mental health conditions among multiracial adolescents. Ethn Health [Internet]. 2021 Jan 21;1–15. Available from: 10.1080/13557858.2020.1869187. [DOI] [PubMed]
- 45.Ospina MB, Serrano-Lomelin JA, Amjad S, Hicks A, Giesbrecht GF. Latent factors of adverse childhood experiences and adult-onset asthma. J Dev Orig Health Dis [Internet]. 2020/01/15. 2021;12(1):50–7. Available from: https://www.cambridge.org/core/article/latent-factors-of-adverse-childhood-experiences-and-adultonset-asthma/C9784663434CBEFE03783B6B56BD1FEB. [DOI] [PubMed]
- 46.Finkelhor D. Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abuse Negl [Internet]. 2018;85:174–9. Available from: https://www.sciencedirect.com/science/article/pii/S0145213417302715. [DOI] [PubMed]
- 47.Garner AS, Shonkoff JP, Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care and, on D S, Siegel BP, Dobbins BS, Earls MI. MF, Early Childhood Adversity, Toxic Stress, and the Role of the Pediatrician: Translating Developmental Science Into Lifelong Health. Pediatrics [Internet]. 2012 Jan 1;129(1):e224 LP-e231. Available from: http://pediatrics.aappublications.org/content/129/1/e224.abstract. [DOI] [PubMed]
- 48.Tourangeau R, Yan T. Tourangeau, Roger: Joint Program in Survey Methodology, University of Maryland, 1218 LeFrak Hall. College Park, MD, US: American Psychological Association; 2007. Sensitive questions in surveys; pp. 859–83. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The de-identified datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request and on signing of a data-sharing agreement.