Abstract
Background
Patient experience is a core component of healthcare quality. Patient-reported experience measures (PREMs) are increasingly used to assess this, but there are few paediatric PREMs. This paper reports the first stage of developing two such measures, one for children and young people (0–18 years) (CYP) with a life-threatening or life-shortening condition (LT/LSC), and one for their parents. It comprised parallel scoping reviews of qualitative evidence on the elements of health service delivery and care that matter to, or impact on, CYP (Review 1) and parents (Review 2).
Methods
Medline and PsychINFO (1/1/2010 – 11/8/2020) and CINAHL Complete (1/1/2010 – 4/7/2020) were searched and records identified screened against inclusion criteria. A thematic approach was used to manage and analyse relevant data, informed by existing understandings of patient/family experiences as comprising aspects of staff’s attributes, their actions and behaviours, and organisational features. The objective was to identity the data discrete elements of health service delivery and care which matter to, or impact on, CYP or parents which, when organised under higher order conceptual domains, created separate conceptual frameworks.
Results
18,531 records were identified. Sparsity of data on community-based services meant the reviews focused only on hospital-based (inpatient and outpatient) experiences. 53 studies were included in Review 1 and 64 in Review 2. For Review 1 (CYP), 36 discrete elements of healthcare experience were identified and organized under 8 higher order domains (e.g. staff’s empathetic qualities; information-sharing/decision making; resources for socializing/play). In Review 2 (parents), 55 elements were identified and organized under 9 higher order domains. Some domains were similar to those identified in Review 1 (e.g. professionalism; information-sharing/decision-making), others were unique (e.g. supporting parenting; access to additional support).
Conclusions
Multiple and wide-ranging aspects of the way hospital healthcare is organized and delivered matters to and impacts on CYP with LT/LSCs, and their parents. The aspects that matter differ between CYP and parents, highlighting the importance of measuring and understanding CYP and parent experience seperately. These findings are key to the development of patient/parent experience measures for this patient population and the resultant conceptual frameworks have potential application in service development.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12887-023-04151-6.
Keywords: Healthcare experiences, Patient experiences, Patient-reported experience measures, Children, Young people, Parents, Paediatrics, Life-threatening condition, Life-shortening condition, Scoping review
Background
There is now wide recognition that, in addition to outcomes and safety, patient experience is a core component of healthcare quality and should be subject to the same degree of monitoring and bench-marking [1–3]. Dominant theoretical understandings, based almost exclusively on research with adult patients and their family members, have specified the dimensions of healthcare delivery which matter to patients and affect how they experience using healthcare. Broadly similar across conceptual models, these include: respect for patient values and preferences; coordination and integration of care; information and communication; physical comfort; emotional support and involvement of family and friends [4, 5]. These dimensions of experience are found in many of the patient-reported experience measures (PREMs) which have been developed in recent years (e.g. [6–9]).
However, some have questioned whether the dominant frameworks properly capture what really matters to patients and families [10, 11]. Others have critiqued the frameworks (and the associated PREMs) as focusing on experiences of the functional aspects of care (e.g. timely administration of medication, availability of information, ward facilities) and neglecting the relational dimension of patient experience. That is, how interactions and relationships with healthcare staff are experienced. In response, a number of smaller bodies of literature (and resultant PREMs) have emerged focusing on relational experience [12–14].
The conceptual and measurement limitations described above are as true for PREMs used in paediatric settings as they are for those used with adult and older patients. However, within the paediatric context, there are additional concerns. In terms of measuring the child’s experience, the majority of paediatric PREMs are parent proxy, rather than child—report [15]. In addition, among the child-report measures which do exist, many have not been developed from research with children, with some simply a re-wording of an adult PREM into ‘child-friendly’ text and response formats, with no investigation into whether these aspects of the care experience matter to children and young people (CYP), or indeed whether what matters differs according age and cognitive ability (e.g. [16]. Furthermore, attempts to develop measures of parents’ own experiences have, to date, been extremely limited [17]. This is somewhat surprising given the core and essential roles parents play as medical, physical and emotional care providers, decision-makers and care navigators. The origins of PREMs in adult medicine are likely to have contributed to the neglect, or lack of recognition, of this aspect of healthcare experience. To date, attempts to develop robust and meaningful parent experience measures (PaREMs) have been hampered by developers failing to adhere to measure development guidelines, and are typically specific to particular healthcare settings (e.g. critical care) [17].
Within the paediatric population, the heaviest users of healthcare are CYP with life-threatening illnesses (e.g. cancers; severe congenital heart disease) and conditions which shorten life expectancy due to the degenerative nature of the condition, or because the condition significantly increases the risk of health complications (e.g. seizures, severe respiratory infections). Life expectancy can be very short—within minutes or hours of birth (e.g. Edwards’ syndrome (trisomy 18)) – through to the likelihood of death occurring sometime during the childhood years or adulthood (e.g. Duchenne muscular dystrophy; severe cerebral palsy) [18–20]. Given the frequency and intensity of health service use among this population and the fact that, given the prognosis, healthcare experiences are likely to be even more salient, there is a strong case for better understanding their experiences, and for developing a CYP’s PREM and PaREM for this population.
This paper describes the first stage in the development of a PREM for CYP with a life-threatening or life-shortening condition (LT/LSC), and a PaREM for parents of such children. It comprised parallel scoping reviews of qualitative studies investigating: (1) the healthcare experiences of CYP (aged 0–18 years) with a LT/LSC and (2) the healthcare experiences of their parents in their role as parent (referred to as Review 1 and Review 2 respectively).
Methods
The overall objective of the reviews was to identify and define aspects (or elements) of health service delivery and care that matter to, or impact on, CYP aged 0–18 years with a LT/LSC or their parents, and to present these as conceptual frameworks. A second objective (added early in the data extraction stage) was to identify and synthesise evidence on the ways health service delivery and care impact on CYP and parents. The reviews, carried out in accordance with current guidance, are reported according to the PRISMA extension for scoping reviews [21, 22].
Review questions
Review 1:
What aspects (or elements) of health service delivery and care matter to, or impact, CYP aged 0–18 years with a LT/LSC?
Review 2:
What aspects (or elements) of health service delivery and care matter to, or impact, parents of CYP aged 0–18 years with a LT/LSC in their caring role?
In addition, there were two cross-cutting questions:
Do the aspects of health service delivery and care that matter differ between CYP and parents?
Do the aspects of health service delivery and care that matter differ according to age and/or developmental stage of the CYP?
At the time the reviews were conducted, PROSPERO was not registering scoping reviews. The protocol was therefore published in an alternative repository [23].
Parent and professional involvement
Two advisory groups supported the reviews. The first was the Martin House Research Centre’s Family Advisory Board (www.york.ac.uk/healthsciences/research/public-health/projects/martinhouse/mh-ppi/fab/) which is comprised of parents of CYP with LT/LSC, including bereaved parents. Consulted at study outset, the group confirmed the importance of including studies where parents were acting as proxies for their children (due to significant cognitive impairment and/or health status/medical fragility). They were also consulted during data analysis when emergent findings were presented, particularly for the purpose of checking data interpretation. A second advisory group comprised clinicians and academics/researchers working in the field of paediatric palliative care. This group was consulted on three occasions during data analysis and the development of the conceptual frameworks.
Eligibility criteria
Inclusion criteria were:
concerns CYP up to 18 years of age diagnosed with a LT/LSC as specified in the search strategy;
study focus is experiences of using a health service(s);
reports primary research using qualitative methods or mixed methods in which qualitative data is reported separately;
data gathered directly from CYP and/or parents;
sample size of at least 5;
published in English in a peer-reviewed journal;
published in 2010 or more recently.
Exclusion criteria were:
no data collected on experiences of using a healthcare service (e.g. studies of lived experience, evaluations of specific interventions etc.);
only concerned with one or more of the following types of healthcare: cancer long-term follow-up, ante-natal, maternity, bereavement, ambulance services;
only concerned with the diagnostic process, adult healthcare and/or the transfer to adult healthcare, or does not report paediatric and adult healthcare experiences separately;
Masters / Doctoral Dissertations, books, book chapters, conference posters, and unpublished studies;
studies conducted in non-OECD countries;
published before 2010.
Information sources and search strategy
The following databases were searched: Medline and PsychINFO (search date ranges: 1/1/2010 – 11/8/2020, and CINAHL Complete (1/1/2010 – 4/7/2020). Search strategies were constructed around the following concepts: [LT/LSCs (specific diagnoses, diagnostic categories)]; [healthcare setting or healthcare staff]; [study design (qualitative or mixed methods] and [population (children and/or parent)]. LT/LSCs (n = 282) included in searches was based on previous work. Full search strategies are provided in Supplementary File 1.
Quality appraisal
As this was a scoping review a quality appraisal of included studies was not undertaken.
Study selection
Once de-duplicated, search outputs were uploaded into Covidence, an online software designed for managing systematic reviews [24]. Two reviewers independently screened all records by title and abstract. A third reviewer was consulted when differences of opinion regarding inclusion/exclusion could not be resolved. Full texts of retained articles were retrieved and the same screening process implemented and reasons for exclusion recorded. At this point it was noted that, for both reviews, almost all retained articles concerned hospital (inpatient and outpatient) healthcare experiences, as opposed to community-based health services. Furthermore, an initial review of the themes reported in studies revealed the healthcare experiences reported in the community-based health service studies were quite different to those reported elsewhere, focusing primarily on access to services and the skills of those providing them. The decision was therefore taken to limit the reviews to hospital (inpatient and outpatient) experiences only.
Data extraction and analysis
Data analysis used the core devices of a thematic approach to qualitative data analysis: data immersion, data display, data reduction and analytical writing [25].
Data extraction
All members of the review team (SM, NR, BB) were involved in developing the data extraction templates. In terms of study characteristics, the following data was extracted for both reviews: study aims, country, research design, method(s), study population (e.g. parent vs CYP (Review 1 only), gender, CYP’s age, type ofLT/LSC, ethnicity, healthcare setting, stages(s) in condition trajectory, and sample size.
Data extraction templates (or thematic frameworks) for research findings were informed by existing conceptual models of healthcare experience [4, 5, 26], domains measured by existing adult and CYP PREMs, and scrutiny of sub-sets of included studies (at least 10 per review) purposively selected to represent different study objectives, a range of diagnoses, and stages of the illness trajectory. For Review 1, the sub-set also included CYP versus parent study participant. Once drafted, initial templates were subject to an iterative process of testing and revising, involving all three reviewers using the same sub-set of studies. Final versions of the data extraction frameworks are provided in Supplementary File 2.
Relevant data from the included articles was extracted ad verbatim (i.e. original author’s text, study participant quotes). Data was deemed relevant if study authors reported an experience of health service delivery or care as mattering to one or more study participants: that is, it was of importance or significance to the CYP or parent, and/or had positive or negative impacts.
For both reviews, two researchers (SM, NR) independently extracted from 10% of included studies to confirm shared understanding of themes. Data from remaining included studies were extracted by one reviewer. Once completed, one reviewer (SM) scrutinised data extraction for both reviews to check for accuracy and consistency of allocation of data to themes. All reviewers (SM, NR, BB) then met to resolve queries and inconsistencies.
Main analysis
For both reviews, our approach to analysis was informed by the work of Entwistle et al. [10] who argue that conceptual frameworks underpinning the measurement of patient experience need to be more fine-grained if they are to be useful in identifying what needs to be done to improve service quality. They also make the case that, to better understand the relational dimension of patient experience, measures should focus on staff attributes (i.e. characteristics, inherent qualities) and actions, and not the feelings which interactions, or relationships, with staff generate.
To start, the completed data extraction templates were independently examined by all members of the review team. Following this the team met to discuss the next analytical iteration. For both reviews it was agreed that, within each theme, extracted data could usefully be categorised as describing one or more of the following: staff attributes, staff actions and organisational features (i.e. features of service organisation or delivery, hospital facilities).
Individual thematic tables were therefore constructed which, along a row, presented the ad verbatim data and summaries of that data organised into descriptions of staff attributes, descriptions of staff actions and descriptions of organisational features, see Table 1. One reviewer (SM) coded and summarised all the extracted data into these categories. Other members of the review team (NR, BB) then independently checked the summaries in terms of coding and the closeness to the original data. The team then met to discuss the summaries, after which corrections and changes were implemented by SM.
Table 1.
Structure of thematic tables
| Theme title: | ||||
| Study ID | Verbatim data extract | Review team summaries of data extract | ||
| Staff attributes | Staff actions | Organisational features | ||
Following this, an overarching summary of the data contained within a theme was drafted by one reviewer (SM) which described the discrete elements of health service delivery and care identified by the analysis. Summaries were reviewed and commented on at least once by at least one other member of the team.
Next the summaries were refined into one or more short statements, each describing a discrete element of health service care and delivery, and categorised as either a staff attribute, staff action or organisational feature. Mindful that these statements would form the basis of a PREM, a specific rubric was used to guide how they were worded, see Table 2.
Table 2.
Statements describing the elements of healthcare experience: writing style rubric
| • One sentence describing a single construct |
| • Simple, unambiguous wording |
| • Positively phrased |
| • Where possible using words/phrases commonly found in verbatim quotes |
| • No colloquialisms |
| • Applicable to any hospital healthcare setting or staff group |
| • Worded so as not to imply a particular age or developmental stage |
| • Non-gendered |
Finally, for each review, all the ‘elements of healthcare experience’ statements which had been generated were subject to an iterative process of review and discussion by the team with the objective of grouping them under higher order concepts, or domains of health service care and delivery. This process was continued until the team was satisfied with the conceptual validity of the frameworks.
Secondary analysis: mapping the impacts of healthcare experiencess
Extracted data was re-examined for descriptions of the impact(s) of the elements of health service delivery and care on CYP (Review 1) and parents’ (Review 2). An additional column was added to the thematic tables into which one reviewer (SM) entered a summary of any impact(s) reported by a study. For an example of a thematic table, with data extracted into it (including illustrative quotations) and impact summaries, please see Supplementary File 3.
Once completed the entire team reviewed the summaries and, through an iterative process, higher order concepts (or themes)—each capturing different types of impact—were agreed (see Supplementary Files 4 and 5). Impact summaries were then coded and coded data organized under these higher order concepts.
Results
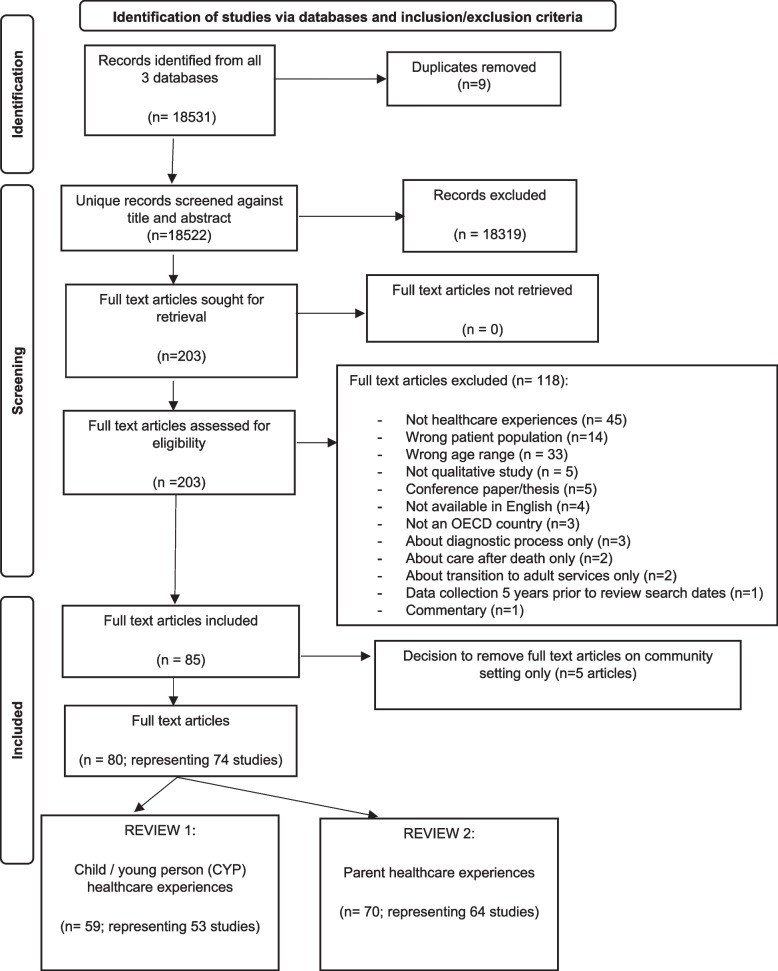
A total of 18,531 records were initially screened for Review 1 and/or Review 2, with 18,328 excluded. Full text articles for all remaining records (n = 203) were retrieved, of which 85 met inclusion criteria. As previously discussed (see methods section), at this stage the decision was taken to exclude 5 articles (representing 4 studies) only reporting on experiences of community-based health services, thereby making hospital healthcare experiences the focus of the review. Of the 80 articles (74 studies) taken forward into the review, 59 articles (representing 53 studies) were included in Review 1, and 70 articles (representing 64 studies) included in Review 2, see Fig. 1. Characteristics of included studies are set out in Table 3. Findings from the two reviews are reported sequentially.
Fig. 1.
PRISMA 2020 flow diagram for scoping review
Table 3.
Characteristics of included studies
| Review | Diagnosis | Setting reported on | Point(s) in trajectory | Focus on particular experience? | Study design, no. sites | Data collection method(s) | Child sample: Sample size, age range | Parent sample: Sample size, age range of children | |
|---|---|---|---|---|---|---|---|---|---|
|
Anderson et al. (2018)[27] Australia |
1,2 | Neutropenia | Inpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview | n/a |
N = 9 (n = 8 mothers, n = 1 father) 0 – 14 yrs |
|
Angstrom -Brannstrom et al. (2014)[28] Sweden |
1 | Cancers | Inpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview |
N = 9 (n = 5 boys, n = 4 girls) 3 – 9 yrs |
n/a |
|
Baenzinger et al. (2020)[29] Australia |
1,2 | Cancers | Inpatient, Outpatient | Treat/ manage | No | Cross-sectional, Multi-centre (n = 8) | Interview | n/a |
N = 58 (n = 52 mothers, n = 6 fathers) 0 – 15 yrs |
|
Bergviken & Nilsson (2019)[30] Sweden |
2 | Cancers | Outpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview | n/a |
N = 17 (n = 11 mothers, n = 6 fathers) 1–15 yrs |
|
Bailey-Pearce et al. (2018) [31] UK |
2 | Mixed LT/LSCs | Inpatient | Not reported | No | Cross-sectional, Single centre | Interview | n/a |
N = 7 (n = 7 fathers) Child age: not reported |
|
Baird et al. (2015, 2016)[32, 33] USA |
1,2 | Mixed LT/LSCs | Inpatient (PICU) | Critical episode | R’ships with staff | Cross-sectional, Single centre | Interview | n/a |
N = 7 (n = 5 mothers, n = 2 fathers) 0 – 15 yrs |
|
Ballantyne et al. (2019)[34] Canada |
2 | Cerebral palsy | Inpatient | Diagnosis; treat/ manage | No | Cross-sectional, Single centre | Interview | n/a |
N = 18 (n = 13 mothers, n = 5 fathers) Child age: not reported |
|
Baugham et al. (2017)[35] USA |
2 | Mixed LT/LSCs | Inpatient(NICU) | End of life; end stage | No | Cross-sectional, Single centre | Interview | n/a |
N = 45 (n = 29 mothers, n = 16 fathers) Mean age at death: 41 days |
|
Brooten et al. (2013) [36] USA |
1,2 | Mixed LT/LSCs | Inpatient (NICU, PICU) | End stage | No | Cross-sectional, Multi-centre (n = 5) | Interview | n/a |
N = 63 (n = 44 mothers, n = 19 fathers) Mean age at death: 43 mos |
|
Brouwer et al. (2020)[37] Netherlands |
1,2 | Mixed LT/LSCs | Inpatient, Outpatient | Treat/ manage; end of life; end stage | No | Cross-sectional, Multi-centre (no. sites not reported) | Interview | n/a |
N = 64 ( parent unspecified) 1–12 yrs |
|
Butler et al. (2018a, 2018b, 2018c, 2019)[38–41] Australia |
1,2 | Mixed LT/LSCs | Inpatient (PICU) | End stage | R’ships with staff | Cross-sectional, Multi-centre (n = 4) | Interview | n/a |
N = 26 (n = 18 mothers, n = 8 fathers) Child age: not reported |
|
Callans et al. (2016) [42] USA |
1,2 | Not specified (healthcare technology-dependent) | Inpatient | Not reported | Care transitions | Cross-sectional, Single centre | Focus group | n/a |
N = 18 (n = 16 mothers, n = 2 fathers) Child age: not reported |
|
Carnevale (2013)[43] Canada |
1 | Mixed LT/LSCs | Inpatient (PICU) | Critical episode | Care transitions | Cross-sectional, Single centre | Interview |
N = 12 (n = 8 boys, n = 4 girls) 3 – 17 yrs |
n/a |
|
Carnevale et al. (2011)[44] Italy |
1,2 | Mixed LT/LSCs | Inpatient (PICU) | Critical episode | Decision-making | Cross-sectional, Multi-centre (n = 2) | Interview, focus group | n/a |
N = 7 (n = 7 mothers) 1 mos – 14 yrs |
|
Cicero-Cinecto et al. (2017) [45] Mexico |
1,2 | Cancers | Inpatient | End of life; end stage | Decision making | Cross-sectional, Multi-centre (n = 3) | Interview |
N = 6 (n = 4 boys, n = 2 girls) 13 – 18 yrs |
N = 13 (n = 10 mothers, n = 3 fathers) Child age: not reported |
|
Coats et al. (2016)[46] USA |
2 | Not specified (Bone marrow transplant recipients) | Inpatient, Outpatient | Treat/ manage; end of life | Decision-making | Cross-sectional, Single centre | Interview | n/a |
N = 7) (n = 5 mothers, n = 2 fathers) 2 – 8 yrs |
|
Conway et al. (2017)[47] USA |
1,2 | Cancers | Inpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview | n/a |
N = 50 (n = 48 mothers, n = 2 fathers) Child age: not reported |
|
Coyne et al. (2014)[48] Ireland |
1,2 | Cancers | Inpatient, Outpatient | Treat/ manage | Decision-making | Cross-sectional, Single centre | Interview |
N = 20 (n = 11 boys, n = 9 girls) 7 – 16 yrs |
N = 22 (n = 17 mothers, n = 5 fathers) Child are: not reported |
|
Dahav et al. (2018)[49] Sweden |
1,2 | Mixed LT/LSCs | Inpatient (PICU) | Critical episode | No | Cross-sectional, Single centre | Interview | n/a |
N = 15 (n = 10 mothers, n = 5 fathers) 0 – 16 mos |
|
Darbyshire et al. (2015)[50] Italy |
2 | Mixed LT/LSCs | Inpatient, Outpatient | Diagnosis; end stage | No | Cross-sectional, Multi-centre (no. sites not reported) | Interview, qualitative survey | n/a |
N = 33 (n = 17 mothers, n = 16 fathers) Child age: not reported |
|
Davies et al. (2017)[51] UK |
1,2 | Cancer: leukaemia | Outpatient | Treat/ manage | R’ships with staff |
Longitudinal Multi-centre (n = 6) |
Interview | n/a |
N = 20 (n = 8 mothers, n = 12 fathers) 1–12 yrs |
|
Engler et al. (2020)[52] Germany |
1,2 | Not specified (Received paediatric palliative care) | Inpatient | End of life; end stage | No | Cross-sectional, Single centre | Interview | n/a |
N = 13 (n = 9 mothers, n = 4 fathers) 4 mos – 17 yrs |
|
Engvall et al. (2016)[53] Sweden |
1 | Cancers | Outpatient | Treat/ manage | No | Cross-sectional, Multi-centre (n = 3) | Interview |
N = 13 (n = 6 boys, n = 7 girls) 5 – 15 yrs |
n/a |
|
Enskar et al. (2020)[54] Sweden |
1,2 | Cancers | Inpatient, Outpatient | Diagnosis; treat/ manage | Nurses’ caring practices |
Longitudinal Single centre |
Interview |
N = 25 (n = 10 boys, n = 15 girls) 3—6 yrs |
N = 38 (n = 24 mothers, n = 14 fathers) 1 – 6 yrs |
|
Falck et al. (2016)[55] USA |
1,2 | Mixed LT/LSCs | Inpatient (NICU) | Critical episode | No | Cross-sectional, Single centre | Interview | n/a |
N = 6 (n = 6 mothers) 25–34 wks |
|
Falkenburg et al Netherlands |
1,2 | Mixed LT/LSCs | Inpatient (PICU) | End of life; end stage | Environment/ R’ships with staff | Cross-sectional, Single centre | Interview | n/a |
N = 36 (n = 19 mothers, n = 17 fathers) 2 wks – 14 yrs |
|
Fixter et al. (2017)[58] UK |
2 | Cystic fibrosis | Inpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview | n/a |
N = 12 (n = 10 mothers, n = 2 fathers) 2–14 yrs |
|
Gabriel et al. (2019)[59] Australia |
1,2 | Cancers | Inpatient, Outpatient | Treat/ manage | Receiving surgery | Cross-sectional, Multi-centre (n = 11) | Interview |
N = 17 (n = 7 boys, n = 10 girls) Age not reported |
N = 15 (n = 7 mothers, n = 8 fathers) 0–15 yrs |
|
Gilmer et al. (2013)[60] USA |
2 | Mixed LT/LSCs | Inpatient (inc. PICU, NICU) | End of life | No | Cross-sectional, Multi-centre (n = 3) | Interview | n/a |
N = 15 (n = 1 mother, n = 14 fathers) “Infants to 14 yrs” |
|
Greenway et al. (2019)[61] USA |
1,2 | Not specified (Admitted to PICU) | Inpatient (PICU) | Critical episode | Communication | Cross-sectional, | Interview | n/a |
N = 52 (n = 33 mothers, n = 15 fathers, n = 4 legal guardians) 2 days—12 yrs |
|
Guttman et al. (2020)[62] USA |
2 | Cerebral palsy | Inpatient | Diagnosis; critical episode | Communication | Cross-sectional, Multi-centre (n = 2) | Qualitative survey | n/a |
N = 266(parent unspecified) Child age: not reported |
|
Hemsley et al. (2013)[63] Australia |
1 | Cerebral palsy | Inpatient, Outpatient | Not reported | Communication | Cross-sectional, Multi-centre: no. sites not reported | Focus group |
N = 6 (n = 4 boys, n = 2 girls) 13 – 18 yrs |
N = 10 (n = 9 mothers, n = 1 father) Child age: not reported |
|
Hooghe et al. (2018)[64] Belgium |
2 | Cancers | Inpatient Outpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview, focus group | n/a |
N = 16 (n = 9 mothers, n = 7 fathers) Age range: 9 mos – 15 yrs |
|
Inglin et al. (2011)[65] Switzerland |
1,2 | Mixed LT/LSCs | Inpatient, Outpatient | Diagnosis; treat/ manage; end stage | No | Cross-sectional, Multi-centre (n = 4) | Interview | n/a |
N = 17 (n = 15 mothers, n = 2 fathers) 1—18 yrs |
|
Iversen et al. (2013)[66] Norway |
1,2 | Cerebral palsy | Inpatient | Treat/ manage | Surgery | Cross-sectional, Single centre | Interview | n/a |
N = 12 (n = 6 mothers, n = 6 fathers) 8—16 yrs |
|
Kelly et al. (2017)[67] USA |
1 | Cance | Inpatient, Outpatient | Not reported | Decision-making | Cross-sectional, Single centre | Interview |
N = 29 (n = 15 boys, n = 14 girls) 9 – 17 yrs |
n/a |
| Kilicarslan-Toruner and Akgun- Citak (2013) [68] Turkey | 2 | Cancers | Inpatient, Outpatient | Treat/ manage | Decision-making | Cross-sectional, Single centre | Interview | n/a | N = 15 (n = 13 mothers, 2 fathers). 2–18 years |
|
Lamiani et al. (2013)[69] Italy |
2 | Mixed LT/LSCs | Inpatient (PICU) | End of life; end stage | No | Cross-sectional, | Interview | n/a |
N = 8 (n = 5 mothers, n = 3 fathers) 2mos – 13 yrs |
|
Linder et al. (2017)[70] USA |
1 | Cancers | Inpatient | Treat/ manage | “Sources of bother” | Cross-sectional, Single centre | Qualitative survey |
N = 50 (n = 23 boys, n = 27 girls) 7–18 yrs |
n/a |
|
Livesley and Long (2013)[71] UK |
1 | Mixed LT/LSCs | Inpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview |
N = 16 (n = 7 boys, n = 9 girls) 5–16 yrs |
n/a |
|
Mack et al. (2017)[72] USA |
1,2 | Cancers | Inpatient | Not reported | R’ships with staff | Cross-sectional, Multi-centre (n = 2) | Interview | n/a |
N = 29 (n = 18 mothers, n = 10 fathers, n = 1 missing data) Child age: not reported |
|
Markwalter et al. (2019)[73] USA |
2 | Not specified (Admitted to PICU) | Inpatient (PICU) | Critical episode | Care transitions | Cross-sectional, Single centre | Interview | n/a |
N = 25 (n = 25 mothers) 7 mos – 9yrs |
|
McNamara et al. (2020)[74] USA |
2 | Mixed LT/LSCs | Inpatient | Treat/ manage | Religious & spiritual care | Cross-sectional, Single centre | Interview | n/a |
N = 19 (n = 19 mothers) Child age: not reported |
|
Mitchell et al. (2019)[75] UK |
1,2 | Mixed LT/LSCs | Inpatient (PICU) | End of life; end stage | Decision-making | Cross-sectional, Single centre | Interview | n/a |
N = 17 (n = 11 mothers, n = 6 fathers) 5 mos—18 yrs |
|
Murrell et al. (2018)[76] USA |
1,2 | SMA: Type 1 | Inpatient, Outpatient | Not reported | No | Cross-sectional, Multi-centre (no. sites not reported) | Interview | n/a |
N = 29 (n = 18 mothers, n = 11 fathers) 6 mos – 14 yrs |
|
Nicholas et al. (2016)[77] Canada |
2 | Mixed LT/LSCs | Inpatient | Diagnosis; treat/ manage; end of life; end stage | No | Cross-sectional, Single centre | Interview, focus group | n/a |
N = 18 (n = 18 fathers) Child-age: not reporte d |
|
Nyborn et al. (2016)[78] USA |
1,2 | Cancers | Outpatient | Critical episode | Communication | Cross-sectional, Single centre | Interview | n/a |
N = 28 (n = 26 mothers, n = 2 fathers) 2.5 – 17.5 yrs |
|
Obas et al. (2016)[79] Canada |
1,2 | Cardiac disease | Inpatient (PICU) | Treat/ manage | Care transitions | Cross-sectional, Single centre | Interview | n/a |
N = 9 (parent unspecified) 2 mos – 14 yrs |
|
October et al. (2014)[80] UK |
2 | Mixed LT/LSCs | Inpatient (PICU) | Critical episode | Decision-making | Cross-sectional, Single centre | Qualitative survey | n/a |
N = 43 (n = 25 mothers, n = 18 fathers) 1.4 – 10 yrs |
|
Orioles et al. (2013)[81] USA |
1,2 | Mixed LT/LSCs | Inpatient(inc. PICU) | Diagnosis | Communication | Cross-sectional, Single centre | Interview | n/a |
N = 13 (n = 12 mothers, n = 1 father) “Infants”—18 yrs |
|
Oxley (2015)[82] UK |
2 | Not specified (Admitted to PICU) | Inpatient (PICU) | Critical episode | No | Cross-sectional, Single centre | Interview | n/a |
N = 7 (n = 6 mothers, n = 1 father) Child age: not reported |
|
Pinto-Taylor et al. (2020)[83] USA |
1,2 | Mixed LT/LSCs | Inpatient (inc PICU), Outpatient | Diagnosis; end of life; end stage | Decision-making | Cross-sectional, Single centre | Interview | n/a |
N = 9 (parent unspecified) Child age: not reported |
|
Robertson et al. (2019)[84] Australia |
1,2 | Cancers | Inpatient, Outpatient | Not reported | Decision-making | Cross-sectional, Single centre | Interview |
N = 5 (n = 4 boys, n = 1 girl) 11—15 yrs |
N = 25 (= 23 mothers, n = 2 fathers) 8mos – 11 yrs |
|
Roscigno et al. (2016)[85] USA |
1,2 | Traumatic brain injury | Inpatient | Critical episode | Nurses’ caring practices |
Longitudinal Single centre |
Interview | n/a |
N = 29 (n = 25 mothers, n = 4 fathers) 6- 18 yrs |
|
Ruhe et al. (2016)[86] Switzerland |
1 | Cancers | Outpatient | Treat/ manage | Decision-making |
Cross sectional Multi-centre (n = 9) |
Interview |
N = 17 (n = 11 boys, n = 6 girls) 9—17yrs |
n/a |
|
Saetrang et al. (2019)[87] Norway |
1,2 | Duchenne muscular dystrophy | Outpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview | n/a |
N = 14 (n = 7 mothers, n = 7 fathers) 7 – 17 yrs |
|
Salmon et al. (2012)[88] UK |
1,2 | Cancer: leukaemia | Outpatient | Not reported | No |
Longitudinal Multi-centre (n = 6) |
Interview | n/a |
N = 53 (n = 31 mothers, n = 22 fathers) 1 – 12 yrs |
|
Skirko et al. (2020)[89] USA |
2 | Pierre Robin Sequence | Inpatient, Outpatient | Not reported | No | Cross-sectional, Single centre | Interview, focus group | n/a |
N = 16 (n = 11 mothers, n = 5 fathers) “ < 5 yrs” |
|
Smith et al. (2015)[90] UK |
1,2 | Hydro-cephalus | Inpatient, Outpatient | Diagnosis; treat/ manage | Decision-making | Cross-sectional, Multi-centre (n = 2) | Interview | n/a |
N = 25 (n = 15 mothers, n = 10 fathers) 2 – 13 yrs |
|
Smith et al. (2018)[91] UK |
2 | Renal disease | Inpatient | Treat/ manage | Decision-making | Cross-sectional, Single centre | Interview | n/a |
N = 10 (n = 6 mothers, n = 4 fathers) 18 – 28 mos |
|
Snaman et al. (2016)[92] USA |
1,2 | Cancers | Inpatient | End of life | Communication | Cross-sectional, Single centre | Focus group | n/a |
N = 12 (parent unspecified) Child age: not reported |
|
Spalding et al. (2016)[93] UK |
1,2 | Not specified (transferred to hospice services) | Inpatient | Not reported | No | Cross-sectional, Single centre | Interview, focus group |
N = 7 (n = 5 boys, n = 2 girls) 8 – 14 yrs |
N = 5( mothers) Child age: not reported |
|
Spratling et al. (2012)[94] USA |
1 | Not specified (required respiratory assistance) | Outpatient | Treat/ manage | No | Cross-sectional, Single centre | Interview |
N = 11 (n = 5 boys, n = 6 girls) 13 – 18 yrs |
n/a |
|
Steele et al. (2013)[95] USA & Canada |
1,2 | Cancers | Inpatient | End of life; end stage | No | Cross-sectional, Multi-centre (n = 3) | Interview | n/a |
N = 60 (n = 36 mothers, n = 24 fathers) 8 – 17 yrs |
|
Sullivan et al. (2014)[96] Australia |
2 | Mixed LT/LSCs | Inpatient | End of life; end stage | Decision-making | Cross-sectional, Single centre | Interview | n/a |
N = 25 (parent unspecified) Age at death: 3 mos – 12 yrs |
|
Tenniglo et al. (2017)[97] Netherlands |
2 | Cancers | Inpatient, Outpatient |
Treat/ manage |
Decision-making | Cross-sectional, Multi-centre (n = 2) | Focus group |
N = 11 (n = 6 boys, n = 5 girls) 12 – 18 yrs |
N = 18 (n = 9 mothers, n = 9 fathers) 0 – 18 yrs |
|
Thienprayoon et al. (2016)[98] USA |
1,2 | Cancers | Inpatient | End of life; end stage | No | Cross-sectional, Single centre | Interview | n/a |
N = 34 (n = 18 mothers, n = 13 fathers, n = 3 ‘other family caregiverr’) 2 – 18 yrs |
|
Tong et al. (2010)[99] Australia |
1,2 | Renal disease | Inpatient, Outpatient | Diagnosis; treat/ manage | No | Cross-sectional, Multi-centre (n = 2) | Interview | n/a |
N = 20 (n = 15 mothers, n = 5 fathers) 0 – 18 yrs |
|
Wangmo et al. (2016)[100] Switzerland |
1,2 | Cancers | Inpatient, Outpatient | Diagnosis; treat/ manage | No | Cross-sectional, Single centre | Interview |
N = 17 (n = 11 boys, n = 6 girls) 9 – 17 yrs |
N = 19 (n = 15 mothers, n = 4 fathers) Child age: not reported |
|
Watt et al. (2011)[101] USA |
1,2 | Cancers | Inpatient, Outpatient | Diagnosis, treat/ manage | No | Cross-sectional, Multi-centre (no. of sites not reported) | Interview | n/a |
N = 50 (n = 37 mothers, n = 13 fathers) Child age: not reported |
|
Weidner et al. (2011)[102] USA |
1,2 | Mixed LT/LSCs | Inpatient | End of life | No | Cross-sectional, Single centre | Interview, focus group | n/a |
N = 29 (n = 20 mothers, n = 9 fathers Child age: not reported |
|
Young et al. (2011, 2013)[103, 104] UK |
1,2 | Cancers | Inpatient, Outpatient | Treat/ manage | Decision-making |
Longitudinal Multi-centre (n = 6) |
Interview | n/a |
(2011) N = 53 (n = 33 mothers, n = 20 fathers) (2013) N = 67 (n = 40 mothers, n = 27 fathers) 1–12 yrs |
|
Yuen et al. (2012)[105] Netherlands |
1,2 | Lethal Epi. Bullosa (LAEB) | Inpatient, Outpatient | Diagnosis; end stage | No | Cross-sectional, Single centre | Interview | n/a |
N = 16 (parent unspecified) 0.1 – 32.6 mos |
|
Zitzelsberger et al. (2014)[106] Canada |
1 | Renal disease | Inpatient | Treat /manage | Environment | Cross-sectional, Single centre | Interviews |
N = 11 (n = 6 boys, n = 5 girls) 7 – 17 yrs |
n/a |
Review 1: The hospital healthcare experiences of children and young people with life-threatening or life-shortening conditions
Characteristics of included studies
A total of 53 studies reported data on CYP’s experiences of hospital healthcare, either self-reported or via proxy reporting from parents, see Table 3 (additional details in Supplementary File 6). Nine studies recruited only CYP, 8 recruited CYP and parents, and 36 recruited only parents. This represents a total of 271 CYP (n = 142 boys, n = 129 girls) and 1,202 parents (n = 743 mothers, n = 302 fathers, 7 ‘family caregivers/legal guardians’, n = 150 not specified).
CYP study participants were aged 3–18 years, with one study failing to report the age range of CYP involved. For the studies which only recruited parents as proxy informants, the age range of their children was reported in 31/44 studies, with CYP aged 0–18 years represented. Participant ethnicity was reported by 24/53 studies but there was considerable variability in how it was categorised. Overall, the great majority of study participants were described as white or Caucasian. Only two studies investigated the impact of ethnicity on CYP’s healthcare experiences.
With respect to study design, almost all studies were cross-sectional (n = 48) and used interviews to collect data (n = 49). Other methods included focus groups (n = 6), and qualitative survey (n = 1). Over half (n = 36) were single site studies. Where studies recruited CYP, the CYP sample size ranged from 5 to 50 (median 13), and for studies recruiting parents, the parent sample size ranged from 5 to 67 (median = 21).
Over half (n = 33) the studies focused on a single diagnosis/diagnostic group, most frequently cancer (n = 22), followed by cerebral palsy (n = 2) and renal disease (n = 2), and with seven concerned with the following other diagnoses: cardiac disease; Duchenne muscular dystrophy; hydrocephalus; lethal acantholytic epidermolysis bullosa (LAEB); neutropenia; spinal muscular atrophy (type 1); and traumatic brain injury. The remaining studies (n- = 20) recruited samples with a number of different LT/LSCs: none compared differences in experience according to condition.
Studies covered all the stages of condition trajectory, from the period following diagnosis, through to treatment and management, critical episodes, end of life and end stage/death, with thirty focussed on a specific stage. The majority (n = 46) reported on inpatient experiences, of which 13 concerned experiences in intensive care. Just under half (n = 24) reported on outpatient experiences, with 7 studies only investigating this setting. Where the studies focused on a particular aspect of the healthcare experience (n = 29/53), this was most commonly decision making (n = 10), followed by relationships with staff (n = 5) and communication (n = 4). Just 2 studies investigated the impact of age on healthcare experience.
Twenty-three studies were North American, 7 were conducted in Australia and the same number in the UK. The remaining studies (n = 17) were conducted in other European countries (n = 15) and Mexico (n = 1).
Elements of health service delivery and care that matter to children and young people
The review identified 36 discrete aspects (or elements) of health service delivery and care that matter to CYP with a LT/LSC. These can be organised into a conceptual framework comprising 8 broad domains: two concerned with staff attributes; three concerned with staff actions; and three concerned with organisational features, see Table 4. One of these domains (‘Physical and sensory environment during inpatient stays’) is specific to inpatient hospital stays. In an additional two domains (‘Meeting emotional and social needs’ and ‘Resources for socialising and play’), there are some elements which were only reported in studies of inpatient hospital stays (e.g. ‘Staff ensure that the CYP has time alone when they want it’, ‘There is access to technology so that CYP can stay in contact with friends outside’ etc.).
Table 4.
Elements of hospital health service delivery and care that matter to children and young people with a life-threatening or life-shortening condition: a conceptual framework
| STAFF ATTRIBUTES: Empathetic qualities |
| • Staff are kind (n = 10) |
| • Staff are encouraging (n = 2) |
| STAFF ATTRIBUTES: Professionalism |
| • Staff are knowledgeable and skilled in managing the CYP's condition (n = 15) |
| • Staff are thorough and careful (n = 7) |
| • Staff are calm (n = 3) (PO) |
| STAFF ACTIONS: Sharing medical information and decision making |
| • Staff offer the CYP a choice as to how much information they are given about their health, treatment & care (n = 8) |
| • Staff explain medical information using words that the CYP understands (n = 8) |
| • Staff offer the CYP a choice about involvement in discussions about decisions which may affect their health (n = 5) |
| • Staff provide medical information in a caring way (n = 3) |
| • Staff pace the provision of medical information to meet the CYP’s needs (n = 2) |
| STAFF ACTIONS: Delivering clinical and personal care |
| • Staff minimise the CYP’s pain and discomfort (n = 12) |
| • Staff notice and respond to the CYP's requests for help (n = 9) |
| • Staff explain what is going to happen to the CYP (n = 9) |
| • Staff consult the CYP about how they want clinical procedures and care tasks to be carried out (n = 7) |
| • Staff ensure treatments and medications are provided to the CYP on time (n = 3) |
| • Staff notice and respond to the CYP’s non-verbal signals that they need attention (n = 3) (PO) |
| • Staff make sure the CYP is clean (n = 3) (PO) |
| • Staff are prepared for the CYP's admission to or attendance on the unit/ward (n = 2) (CYPO) |
| • Staff look after or help with the CYP’s appearance (n = 2) (PO) |
| STAFF ACTIONS: Meeting emotional and social needs |
| • Staff take time to get to know the CYP (e.g. their interests, life outside hospital etc.) (n = 25) |
| • Staff take the CYP’s whole life into account when arranging medical treatment and care (n = 3) |
| • Staff help the CYP to access toys, games, and other sources of entertainment (n = 2) |
| • Staff do all they can to ensure the CYP is calm and free from anxiety (n = 1) (PO) |
| • Staff ensure that the CYPs has time alone when they want it (n = 1) (CYPO) (Inpatient only) |
| ORGANISATIONAL FEATURES: Resources for socialising and play |
| • There is a supply of games, toys and other sources of entertainment suitable for the CYP (n = 3) (CYPO) |
| • There is access to technology so that the CYP can stay in contact with friends outside hospital (n = 1) (Inpatient only) |
| ORGANISATIONAL FEATURES: Physical and sensory environment during inpatient stays |
| • The layout of the ward allows the CYP to spend time with other CYP (n = 3) (CYPO) |
| • There are facilities so that parents can stay overnight (n = 3) |
| • The room/ward is not too noisy (n = 2) |
| • The room/ward is a comfortable temperature (n = 1)(CYPO) |
| • The beds are comfortable (n = 1) (CYPO) |
| • Ward facilities are accessible if using medical equipment or a wheelchair (n = 1) |
| • There are single rooms available for the CYP (n = 1) (PO) |
| • There is sufficient storage for the CYP’s property (n = 1) (CYPO) |
| • The food is appetising (n = 1) |
| ORGANISATIONAL FEATURES: Continuity of care |
| • Staff are familiar to the CYP (n = 12) |
Figures in brackets indicate the number of papers reporting that the experience matters to children and young people
PO = Element reported as mattering by parents only
CYPO = Element reported as mattering by CYP only
There was considerable variation in the number of studies reporting each of the elements as mattering to CYP, see also Table 4. The element most frequently reported as mattering to CYP was ‘Staff take time to get to know the CYP’ (n = 25/53), followed by ‘Staff are knowledgeable and skilled in managing the CYP’s condition’ (n = 15/53). All other elements were reported by ten studies or fewer. Whilst most elements (n = 24) were identified as mattering to CYP by both CYP and parents, some were only described by CYP (n = 7), and others only by parents (n = 6), see also Table 4.
The impact of health service delivery and care on children and young people
Most of the included studies in which CYP were study participants (n = 15/17) reported CYP’s descriptions of how health service delivery and care affected them. Impacts were wide-ranging with seven areas of impact identified: emotional well-being (e.g. frustration, panic, shock, sadness), physical well-being (e.g. pain, sleeplessness), trust in staff, how comfortable CYP felt with staff, understanding of the situation being faced, sense of empowerment and control, and being at ease with (versus regretting) treatment decisions. For further details on the nature of these impacts see Supplementary File 4.
Table 5 presents the results of mapping out connections between elements of health service delivery and care (grouped into the 8 domains described above) and impact(s). All domains of health service delivery and care were identified as impacting emotional wellbeing. Domains having the widest range of impacts on CYP’s lives were staff actions with respect to sharing of medical information and decision-making, and the delivery of clinical and personal care.
Table 5.
Impacts of health service delivery and care on children and young people
| Impact on children and young people | |||||||
|---|---|---|---|---|---|---|---|
| Domain of health service delivery & care | Emotional wellbeing | Physical wellbeing | Trust in staff | Feeling (un) comfortable with staff | Understanding of situation being faced | Empowerment & control | At ease with (versus regretting) treatment decisions |
| STAFF ACTIONS | |||||||
| Sharing medical information & decision making | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Delivering clinical & personal care | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Meeting emotional & social needs | ✓ | ✓ | |||||
| ORGANISATIONAL FEATURES | |||||||
| Resources for socialising & play | ✓ | ||||||
| Physical & sensory environment during inpatient stays | ✓ | ✓ | |||||
| Continuity of care | ✓ | ✓ | |||||
The findings of this review, and resultant conceptual framework, were shared with the Family Advisory Board. Parents endorsed the conceptual framework, reporting either that they were aware of these elements mattering to their CYP, or would not be surprised if they did.
Review 2: The hospital healthcare experiences of parents of a child/young person with a life-threatening or life-shortening condition
Characteristics of included studies
Sixty-four studies reported on parents’ experiences of hospital healthcare in their parenting role, representing a total of 1,892 parents (n = 948 mothers, n = 436 fathers, 7 family caregivers/legal guardians, n = 501 not specified), see Table 3 (additional details in Supplementary File 6). In 45/64 studies the age of their child with a LT/LSC was reported, with children aged 0–18 years represented. Parents’ ethnicity was reported by 30/64 studies, and in these a large majority were described as white or Caucasian. Only two studies investigated the impact of ethnicity on parents’ healthcare experiences.
The majority of studies were cross-sectional (n = 59), with most using interviews to collect data (n = 58). Other methods used included focus groups (n = 9), qualitative surveys (n = 2). Most (n = 42) were single site studies. The sample size ranged from 5 to 266 (median = 19).
Over half (n = 35) the studies concerned a single diagnosis/diagnostic group, most frequently cancer (n = 21), followed by cerebral palsy (n = 3). Other conditions represented in single diagnosis studies (n = 11) were cardiac disease, cystic fibrosis, Duchenne muscular dystrophy, hydrocephalus, neutropenia, lethal epidermolysis bullosa, Pierre robin sequence, renal disease, SMA type 1 and traumatic brain injury. The remainder (n = 29) either recruited parents of CYP with a number of different LT/LSCs (n = 22), or the sample was defined in terms of the paediatric service or medical treatment required (e.g. paediatric palliative care, bone marrow transplant etc.) (n = 7). Overall, studies covered all stages in the condition trajectory, with 30 focussing on a specific stage. The majority of studies (n = 59) reported on inpatient experiences, of which 18 reported on experiences of intensive care. Twenty-five studies reported on outpatient experiences, with 5 investigating this healthcare context only. Where the studies focused on a particular aspect of the healthcare experience (n = 32/64), this was most commonly decision making (n = 14), followed by communication (n = 5). Only one study investigated the impact of the child’s age on parents’ experiences.
Twenty-seven studies were North American, 11 were conducted in the UK, 7 in Australia and 1 in Mexico. The remainder (n = 18) were conducted in other European countries.
Elements of health service delivery and care that matter to parents
The review identified 55 elements of health service delivery and care that matter to parents who have a CYP with a LT/LSC. These can be organised into 9 broad domains: two concerned with staff attributes; four with staff actions; and three with organisational features, see Table 6. One of these domains is specific to situations in which the CYP is a hospital inpatient (‘Physical environment during hospital inpatient stays’). In an additional two domains (‘Supporting coping’, ‘Supporting parenting’), there are some elements only reported in situations in which the CYP was a hospital inpatient.
Table 6.
Elements of hospital health service delivery and care that matter to parents of children with a life-threatening or life-shortening condition: a conceptual framework
| STAFF ATTRIBUTES: Empathetic qualities |
| • Staff are kind (n = 7) |
| • Staff are patient (n = 4) |
| STAFF ATTRIBUTES: Professionalism |
| • Staff are honest (n = 24) |
| • Staff are knowledgeable and skilled in managing the CYP’s condition (n = 22) |
| • Staff are committed to caring for the child (n = 10) |
| • Staff are polite (n = 3) |
| • Staff are calm (n = 2) |
| • Staff are respectful of cultural and religious beliefs (n = 2) |
| STAFF ACTIONS: Sharing medical information and decision making with parents |
| • Staff involve the parent to the extent that they want in decisions about treatment and care (n = 26) |
| • Staff explain things in ways the parent understands (n = 23) |
| • Staff give difficult or bad news sensitively (n = 22) |
| • Staff give the parent all the information they want about the child’s condition, treatment and care (n = 18) |
| • Staff are willing to answer questions (n = 13) |
| • Staff pace the provision of medical information according to the parent’s readiness and capacity for information at the time (n = 12) |
| • Staff make themselves available to talk to the parent (n = 12) |
| • Staff keep the parent updated on changes in their child’s condition, treatment and care (n = 10) |
| • Staff give difficult or bad news in private (n = 4) |
| • Staff give the parent time to think about significant decisions (n = 4) |
| • Staff check with the parent about discussing medical information in front of their child (n = 3) |
| • Staff check with the parent about how much they tell their child (n = 1) |
| STAFF ACTIONS: Management of the child’s condition |
| • Staff listen to and respect the parent’s views on their child’s condition, treatment and care (n = 24) |
| • Staff give the child the same level of care and attention as other children (n = 5) |
| • Staff on the ward/unit communicate with each other about the CYP’s treatment and care (n = 4) |
| • Staff agree about the CYP’s treatment and care (n = 3) |
| • Staff take information and advice from other specialisms into account when deciding on treatment and care (n = 3) |
| • Staff take family circumstances into account when arranging treatment and care (n = 2) |
| • Staff are willing to be questioned about the child’s treatment and care (n = 1) |
| STAFF ACTIONS: Supporting coping |
| • Staff acknowledge the impact of the situation on the parent (n = 13) |
| • Staff allow the parent to be hopeful (n = 11) |
| • Staff take time to talk to and get to know the parent as an individual (n = 10) |
| • Staff ask the parent how they are feeling (n = 6) |
| • Staff prepare the parent for any changes they might see in their child (n = 6) |
| • Staff give the parent information on hospital facilities (e.g. where to get food, washed) (n = 5) (Inpatient only) |
| • Staff encourage the parent to take care of themselves (e.g. rest, eat etc.) (n = 4) (Inpatient only) |
| • Staff comfort the parent (n = 3) |
| • Staff allow the parent to be on the ward as much as is possible (n = 3) (Inpatient only) |
| • Staff offer to introduce the parents to other parents on the unit/ward (n = 3) (Inpatient only) |
| • Staff talk to the parent about life outside the hospital (n = 2) (Inpatient only) |
| STAFF ACTIONS: Supporting parenting |
| •Staff support the parent to care for their child as much as they would like to (e.g. changing clothes, washing, feeding etc.) (n = 13) (Inpatient only) |
| • Staff make sure the parent can be physically close to and/or hold their child (n = 7) |
| • Staff support the parent to take on any medical responsibilities they want to be involved in (n = 6) (Inpatient only) |
| • Staff do their best to ensure the parent has as much time with their child as they want (n = 5) (Inpatient only) |
| • Staff support the parent with talking to siblings about the child’s health problems (n = 3) |
| • Staff ensure the parent has opportunities for privacy with their child (n = 1) (Inpatient only) |
| • Staff support the parent with explaining difficult or bad news to their child (n = 1) |
| • Staff give the parent information on how the ward/unit operates (e.g. staff roles, shift patterns, visiting hours etc.)(n = 1) |
| ORGANISATIONAL FEATURES: Physical environment during inpatient stays |
| • There are toilets on the ward for the parent (n = 2) |
| • There is a room for the parent to use when they need a break (n = 2) |
| • The layout of the room allows the parent to have time alone with their child (n = 2) |
| ORGANISATIONAL FEATURES: Continuity and coordination of care |
| • Staff are familiar to the parent (n = 18) |
| • There is a staff member responsible for coordinating treatment and care (n = 10) |
| ORGANISATIONAL FEATURES: Access to additional support |
| • Psychological support services are available to the parent (n = 9) |
| • Spiritual care services are available to the parent (e.g. chaplains, faith leaders etc.) (n = 4) |
| • Information on welfare/benefits advice is available to the parent (n = 1) |
| • Interpreters are available to the parent (n = 1) |
Figures in brackets indicate the number of papers reporting that the experience matters to parents
The elements of health service delivery and care most frequently reported as mattering to parents (n > 20 studies reporting) were: ‘Staff are knowledgeable and skilled in managing the CYP’s condition’; ‘Staff are honest with parents’; ‘Staff involve parents to the extent that they want when significant decisions are being made’; ‘Staff give difficult or bad news sensitively’; ‘Staff explain things in ways the parent understands’; and ‘Staff listen to and respect parent’s views about their child’s condition and care’.
Two further elements of health service delivery and care which some parents had reported as valuing were identified in 8 studies. Both staff actions, these elements had been labelled: ‘staff behaving in ways that indicated high levels of emotional distress about child’s/family’s situation’ (e.g. openly weeping), and ‘staff making themselves available to a family beyond usual or expected practice’ (e.g. going into work on a day off to see a family; flying home from holiday early to be with a family at end of life). The research team discussed the inclusion of these elements in the conceptual framework with the project’s clinical/academic advisory group. With respect to the first element (‘Staff behaving in ways that indicated high levels ….’), the advisory group agreed that the data coded under this element was different to that coded under other staff attributes or actions which captured empathetic care. They also agreed that, whilst conveying distress at the suffering/situations patients/families face is natural and appropriate, there are limits to this and uncontrolled displays of emotion are not professional.
In terms of the second element (‘Staff making themselves available…..’), the advisory group agreed that such actions/behaviours could not be expected to implemented into routine service provision. In addition, it potentially indicated a favouring of particular patients/families: something directly in conflict to principles of equity of care (and something which the project’s parent advisory group had identified as very important). It was therefore agreed that the conceptual framework should not include these two elements.
The impacts of health service delivery and care on parents
Most included studies (n = 61/64) described how these elements of health service delivery and care affected parents. Together, they indicate that multiple areas of parents’ lives can be affected by health service delivery and care, including (and most commonly) emotional well-being (e.g. anxiety, anger, fear etc.), being able to parent in the way they want and parent’s trust in staff, see Table 7. For further details on the nature of these impacts see Supplementary File 5.
Table 7.
Impacts of health service delivery and care on parents
| Impact on parents | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Domain of health service delivery & care | Emotional wellbeing | Ability to parent child in way they want | Trust in staff | Care burden | Empowerment & control | Understanding of situation being faced | Partnership (versus conflict) with staff | Maintenance of usual family routine | At ease with (versus regretting) treatment & care decisions | Satisfaction with treatment & care | Sense of hope | Physical wellbeing |
| STAFF ACTIONS | ||||||||||||
| Sharing medical information & decision making | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Management of child’s condition | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Supporting coping | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Supporting parenting during inpatient stays | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||
| ORGANISATIONAL FEATURES | ||||||||||||
| Physical environment during inpatient stays | ✓ | ✓ | ✓ | ✓ | ||||||||
| Continuity & coordination of care | ✓ | ✓ | ✓ | ✓ | ||||||||
| Access to additional support | ✓ | ✓ | ✓ | |||||||||
Table 7 also presents findings from the analysis which mapped connections between the specific elements of health service delivery and care (grouped into the 9 domains set out in Table 6) and the various potential impacts on parents’ lives. All domains of service delivery and care were found to be reported as impacting on emotional wellbeing, and almost all domains (7/8) on being able to parent in the way they want. The domains having the widest range of impacts on parents’ lives are staff actions, both in terms of sharing medical information and decision making, and management of the child’s condition. This is closely followed by supporting parenting during impatient stays and supporting coping.
Discussion
This paper reports parallel scoping reviews of qualitative evidence on the health service experiences of CYP with LT/LSC and their parents, and the resultant conceptual frameworks, setting out the elements of hospital (inpatient and outpatient) health service delivery and care that matter to, and impact on, CYP with a LT/LSC and their parents. Both frameworks are comprised of elements of hospital health service delivery and care (36 for CYP, 55 for parents) which are conceptually distinct. The generation of these conceptual frameworks is the first stage in the development of a CYP PREM and PaREM which, it is intended, can be used to assess both experiences of specific episodes of care (e.g. inpatient admission) and longer-term periods of care under a particular service or specialism. While some elements are specific to inpatient experiences only, none are specific to a particular staff group, stage in the illness trajectory or child’s age/developmental stage. This fits with recent calls for paediatric measures to be developed which are applicable to the multiple service providers in a child’s network of care and across the child’s illness experience [17].
Compared to many existing patient experience frameworks, the frameworks we have developed are deliberately organised around a number of domains of care (e.g. clinical and personal care, the physical and sensory environment etc.), rather than cross-cutting concepts (e.g. respect for patient values and preferences, physical wellbeing), something critiqued by other researcher as limiting the way PREMs can inform service evaluation and service improvement activities, and allow meaningful comparisons by research studies [10, 11].
Similar to previous work [10, 11], the scoping reviews have identified specific staff attributes, and actions or behaviours, that matter to and impact CYP’s and parents’ health service experience, alongside physical and sensory features, and the availability of various facilities and sources of support. To our knowledge this is the first conceptual framework of patient experience developed for CYP with a LT/LSC, and the first conceptual framework of parent experience (across any paediatric population) which is grounded in parents’ views and accounts.
It is recognized globally that, relative to adult patients, attempts to collect CYP’s experiences and views on healthcare provision is very limited [107–110]. This is a critical gap given parent-proxy reporting does not accurately reflect the experiences of CYP, with parents tending to rate experiences more positively than their child [111–113]. Furthermore, our own review highlights differences between CYP and parents in the aspects of the CYP’s healthcare which matter to them. Specifically, findings from direct research with CYP reveals the importance of multiple aspects of the physical and sensory environment, resources for socializing and play, and meeting social and emotional needs to CYP (e.g. ‘the layout of the ward allows the CYP to spend time with other CYP’, ‘the bed are comfortable’, ‘staff ensure the CYP has time alone when they want it’ etc.) which do not emerge from research with parents on their child’s healthcare experiences. These findings reinforce the importance of researchers exercising caution in relying on proxy data.
In addition, we have argued for the need to assess both CYP and parent experience given that a parent’s wellbeing and associated ability to parent is highly likely to impact their child [114–117]. It is notable that key domains identified as important by parents themselves include supporting parenting whilst the child is an inpatient, and supporting coping with the emotional impact and practical implications of their child’s condition and hospital admission.
Finally, a novel and important aspect of both scoping reviews is the identification of the way experiences of using health services impact on multiple areas of CYP’s and parents’ lives. These impacts included: emotional and physical wellbeing; trust in and relationships with staff; understanding of the situation being faced; and satisfaction with treatment, care and decision-making. Importantly, for each type of impact, multiple and diverse elements of health service delivery and care were implicated. This raises questions about the utility of patient experience frameworks (and associated PREMs) which solely focus on measuring impacts, given that they do not yield information about what has caused these experiences.
Limitations
Despite an inclusive search strategy, just 4 studies were identified which reported on experiences of using community health services. Given this very small number, and that a reading of the articles revealed that healthcare experiences reported were quite different to those reported in hospital based studies, a decision was taken to limit the scoping reviews, and therefore the resultant conceptual frameworks, to hospital healthcare experiences. The limited body of research on experiences of community-based health care for CYP with LT/LSCs, and their parents, is concerning and highlights the need for further research on this topic.
Across the two reviews that were undertaken, a range of different types of LT/LSCs were represented. However, a high proportion of studies were concerned with CYP with cancer (21/53 in Review 1; 21/64 in Review 2). The relative lack of evidence on CYP with diagnoses requiring the involvement of multiple specialisms, or which carry implications in terms of cognitive and physical abilities, may mean not all elements of healthcare mattering to CYP with LT/LSC and their parents have been identified and described by existing research. Additional research is needed to investigate this further. In both conceptual frameworks the number of studies identifying each element of health delivery and care are reported (see Tables 4 and 6). This information gives an indication of the depth of data on a particular element. However, these figures should not be taken as an indication of the relative importance of elements since over half the studies in Review 1 and 2 focused on a specific aspect of health service delivery and care (e.g. decision making, communication etc.). Finally, requiring a sample size of 5 or more could have led to us excluding studies taking an Interpretative Phenomenological Analysis (IPA) approach. However, no studies were excluded solely on the basis of sample size. We also note that, whilst there is no firm consensus around minimum sample sizes for IPA, sample sizes of n > 6–8 are generally encouraged for studies not being undertaken for educational (undergraduate/postgraduate studies) purposes.
As noted in the results, across both reviews the impact of ethnicity on what matters to CYP was poorly investigated, with just over half the papers reporting participants’ ethnicity, and only 2 studies investigating the issue. Where ethnicity was reported, it was often inadequately described, with the majority of participants said to be White or Caucasian, with no further information on their ethnic or cultural background provided. We therefore currently have no evidence as to whether there are ethnic differences in the elements of health delivery and care that matter to CYP or parents. We must also be mindful of the fact that the research reviewed was undertaken in OECD countries; it cannot be assumed that the frameworks apply to other settings.
In relation to Review 1, just 17/53 of the included studies recruited CYP. Whilst recruiting parents to research on the experiences of CYP with LT/LSCs is necessary given that some CYP may be limited in their ability to participate due to cognitive or communication difficulties or feeling too unwell, this does mean that we need to treat the emergent conceptual framework as, potentially, incomplete. We also note that the CYP’s framework, reflecting the themes that emerged from Scoping Review 1, is relatively thin with regards to the provision of emotional support, with no direct reference to healthcare professionals offering CYP opportunities to talk about worries and fears. This is somewhat surprising given that previous research with CYP with LT/LSCs has found they have psychological and psychosocial concerns, and research prioritization exercises involving CYP suggest emotional and spiritual support is a priority [118, 119]. However, undertaking qualitative research with CYP is challenging [120, 121] and it is entirely possible that the lack of data on this issue reflects difficulties experienced by researchers in interviewing research participants about the more distressing aspects of living with a LT/LSC. Future research will need to address this issue, albeit sensitively. Finally, most studies recruited CYP across a very broad range of ages and just two investigated age differences in experience. We were therefore unable to draw unable conclusions as to whether the elements of health service delivery and care that matter differ according to age and/or developmental stage of the CYP.
One of the strengths of these reviews is that the research team consulted both a family and a professional advisory group about the review design, preliminary findings, and the resultant conceptual fameworks. It also provided an initial validation of the CYP’s conceptual framework. Further validation work for both frameworks, including very importantly children and young people, will be an essential next step in the development of the PREM, as well as the PaREM. In undertaking this work, special attention will need to be paid to ensuring a range of diagnoses (and particularly those under-represented in existing studies), CYP age groups, disease stages and ethnic/cultural groups are represented.
Conclusions
Following a comprehensive and rigorous review of the qualitative research on the health care experiences of CYP with a LT/LSC and their parents, two conceptual frameworks have been developed which delineate the elements of health service delivery and care that matter to CYP with a LT/LSC as inpatients and outpatients, and their parents. In addition, the impact of attending (or not) to these elements of care have been mapped out. The findings make it clear that while there are some overlaps between what matters to CYP and parents, they also have their own distinct and specific needs. Going forward, these frameworks will be used to develop measures of healthcare experience for CYP and parents for use in service evaluation, service improvement projects and research.
Supplementary Information
Additional file 1: Supplementary File 1. Literature review search strategies.
Additional file 2: SupplementaryFile 2. Final versions of data extraction frameworks.
Additional file 3: Supplementary File 3. Extract from a thematic table used for main analysis.
Additional file 4: Supplementary File 4. The impacts of health service delivery and care on children and young people - List of codes and their definitions.
Additional file 5: Supplementary File 5. The impacts of health service delivery and care on parents- List of codes and their definitions.
Additional file 6: Supplementary File 6. Additional study characteristics.
Acknowledgements
We would like to express our thanks to Kath Wright (retired), formerly information specialist at the Centre for Reviews and Dissemination, University of York, for her expertise in devising the search strategies and conducting the searches. Dr Julia Hackett contributed to initial screening of records. We would also like to thank our two advisory groups for their thoughtful reflections on the review design and findings. Finally, we would like to acknowledge the invaluable advice provided by Professor Lorna Fraser, Professor Richard Harding, and Professor Fliss Murtagh with regard to the scope and focus of the review.
Abbreviations
- CYP
Children and young people
- LT/LSC
Life-threatening or life-shortening condition
- PREM
Patient-reported experience measure
- PaREM
Parent-reported experience measure
Authors’ contributions
SM and BB developed the scoping review protocol and were responsible for study selection. SM and NR undertook data extraction and checking. All authors contributed to data analysis, wrote sections of the manuscript, and reviewed the final manuscript.
Funding
This study was funded by the Martin House Research Centre: a partnership between the Universities of York and Leeds Martin House Hospice Care for Children and Young People.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reference
- 1.Bull C, Byrnes J, Hettiarachchi R, Downes M. A systematic review of the validity and reliability of patient-reported experience measures. Health Serv Res. 2019;54(5):1023–1035. doi: 10.1111/1475-6773.13187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anhang Price R, Elliott MN, Zaslavsky AM, Hays RD, Lehrman WG, Rybowski L, et al. Examining the role of patient experience surveys in measuring health care qualit. Med Care Res Rev. 2014;71(5):522–54. doi: 10.1177/1077558714541480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.OECD . Putting people at the centre of health care: PaRIS survey of patients with chronic conditions. 2019. [Google Scholar]
- 4.Coulter A, Cleary PD. Patients’ Experiences With Hospital Care In Five Countries. Health Aff. 2001;20(3):244–52. doi: 10.1377/hlthaff.20.3.244. [DOI] [PubMed] [Google Scholar]
- 5.Medicine Io. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington DC: National Academy Press; 2001.10.17226/10027. [PubMed]
- 6.Lunt LE, Shoop-Worrall S, Smith N, Cleary G, McDonagh J, Smith AD, et al. Validation of novel patient-centred juvenile idiopathic arthritis-specific patient-reported outcome and experience measures (PROMs/PREMs) Pediatr Rheumatol Online J. 2020;18(1):91. doi: 10.1186/s12969-020-00481-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toomey SL, Zaslavsky AM, Elliott MN, Gallagher PM, Fowler FJ, Jr, Klein DJ, et al. The Development of a Pediatric Inpatient Experience of Care Measure: Child HCAHPS. Pediatrics. 2015;136(2):360–9. doi: 10.1542/peds.2015-0966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murrells T, Robert G, Adams M, Morrow E, Maben J. Measuring relational aspects of hospital care in England with the 'Patient Evaluation of Emotional Care during Hospitalisation' (PEECH) survey questionnaire. BMJ Open. 2013;3(1).10.1136/bmjopen-2012-002211. [DOI] [PMC free article] [PubMed]
- 9.Gan C, Campbell KA, Snider A, Cohen S, Hubbard J. Giving Youth a Voice (GYV): a measure of youths' perceptions of the client-centredness of rehabilitation services. Can J Occup Ther. 2008;75(2):96–104. doi: 10.1177/000841740807500205. [DOI] [PubMed] [Google Scholar]
- 10.Entwistle V, Firnigl D, Ryan M, Francis J, Kinghorn P. Which experiences of health care delivery matter to service users and why? A critical interpretive synthesis and conceptual map. J Health Serv Res Policy. 2012;17(2):70–8. doi: 10.1258/jhsrp.2011.011029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bastemeijer CM, Voogt LP, van Ewijk H, Hazelzet JA. What do patient values and preferences mean? A taxonomy based on a systematic review of qualitative papers. Patient Educ Counsel. 2017;100(5):871–81. doi: 10.1016/j.pec.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 12.Mercer SW, Maxwell M, Heaney D, Watt GC. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. 2004;21(6):699–705. doi: 10.1093/fampra/cmh621. [DOI] [PubMed] [Google Scholar]
- 13.Williams AM, Lester L, Bulsara C, Petterson A, Bennett K, Allen E, et al. Patient Evaluation of Emotional Comfort Experienced (PEECE): developing and testing a measurement instrument. BMJ Open. 2017;7(1):e012999. doi: 10.1136/bmjopen-2016-012999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Graham C KS, Cooper R, King J, Sizmur S, Jenkinson C, et al.. An evaluation of a near real-time survey for improving patients' experiences of the relational aspects of care: a mixed-methods. Health Services Delivery Research 2018;6(15). 10.3310/hsdr06150. [PubMed]
- 15.Bele S, Teela L, Zhang M, Rabi S, Ahmed S, van Oers HA, et al. Use of patient-reported experience measures in pediatric care: a systematic review. Front Pediatr. 2021;9. 10.3389/fped.2021.753536. [DOI] [PMC free article] [PubMed]
- 16.Arigliani M, Castriotta L, Pusiol A, Titolo A, Petoello E, Brun Peressut A, et al. Measuring empathy in pediatrics: validation of the Visual CARE measure. BMC Pediatr. 2018;18(1):57. doi: 10.1186/s12887-018-1050-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ang FJL, Finkelstein EA, Gandhi M. Parent-reported experience measures of care for children with serious illnesses: a scoping review. Pediatr Crit Care Med. 2022;23(9):e416–3. 10.1097/PCC.0000000000002996. [DOI] [PubMed]
- 18.Fraser LK, Parslow R. Children with life-limiting conditions in paediatric intensive care units: a national cohort, data linkage study. Arch Dis Child. 2018;103(6):540–7. doi: 10.1136/archdischild-2017-312638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boyden JY, Curley MAQ, Deatrick JA, Ersek M. Factors associated with the use of U.S. community-based palliative care for children with life-limiting or life-threatening illnesses and their families: an integrative review. J Pain Symptom Manag. 2018;55(1):117–31. doi: 10.1016/j.jpainsymman.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 20.Kim CH, Song IG, Kim MS, Lee JY, Lim NG, Shin HY. Healthcare utilization among children and young people with life-limiting conditions: Exploring palliative care needs using National Health Insurance claims data. Scientific Reports. 2020;10(1):2692. doi: 10.1038/s41598-020-59499-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Internal Med. 2018;169(7):467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 22.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–26. doi: 10.11124/jbies-20-00167. [DOI] [PubMed] [Google Scholar]
- 23.Available from: https://eprints.whiterose.ac.uk/175542/.
- 24.Innovation VH. Covidence Systematic Review Software Melbourne, Australia Available from: www.covidence.org.
- 25.J. MMHAS . Quallitative Data Analysis: A Methods Sourcebook. 4th. Thousand Oaks: Sage Publications; 2019. [Google Scholar]
- 26.Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care. 2002;14(5):353–8. doi: 10.1093/intqhc/14.5.353. [DOI] [PubMed] [Google Scholar]
- 27.Anderson KJ, Bradford NK, Clark JE. Through Their Eyes: Parental Perceptions on Hospital Admissions for Febrile Neutropenia in Children With Cancer. J Pediatr Oncol Nurs. 2018;35(5):342–52. doi: 10.1177/1043454218777719. [DOI] [PubMed] [Google Scholar]
- 28.Angstrom-Brannstrom C, Norberg A. Children undergoing cancer treatment describe their experiences of comfort in interviews and drawings. J Pediatr Oncol Nurs. 2014;31(3):135–46. doi: 10.1177/1043454214521693. [DOI] [PubMed] [Google Scholar]
- 29.Baenziger J, Hetherington K, Wakefield CE, Carlson L, McGill BC, Cohn RJ, et al. Understanding parents' communication experiences in childhood cancer: a qualitative exploration and model for future research. Support Care Cancer. 2020;28(9):4467–76. doi: 10.1007/s00520-019-05270-6. [DOI] [PubMed] [Google Scholar]
- 30.Bergviken H, Nilsson S. Focusing on the hospital stay or everyday life with cancer: Parents' experiences of choosing a central access device for their child with cancer. J Specialists Pediatr Nurs. 2019;24(3):e12261. doi: 10.1111/jspn.12261. [DOI] [PubMed] [Google Scholar]
- 31.Bailey-Pearce O, Stedmon J, Dallos R, Davis G. Fathers' experiences of their child's life-limiting condition: An attachment narrative perspective. Clin Child Psychol Psychiatry. 2018;23(3):381–97. doi: 10.1177/1359104517730115. [DOI] [PubMed] [Google Scholar]
- 32.Baird J, Davies B, Hinds PS, Baggott C, Rehm RS. What Impact Do Hospital and Unit-Based Rules Have Upon Patient and Family-Centered Care in the Pediatric Intensive Care Unit? J Pediatr Nurs. 2015;30(1):133–42. doi: 10.1016/j.pedn.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baird J, Rehm RS, Hinds PS, Baggott C, Davies B. Do You Know My Child? Continuity of Nursing Care in the Pediatric Intensive Care Unit. Nurs Res. 2016;65(2):142–50. doi: 10.1097/nnr.0000000000000135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ballantyne M, Bernardo S, Sozer A, Orava T, A CM, Church P, et al. A whole new world: a qualitative investigation of parents' experiences in transitioning their preterm child with cerebral palsy to developmental/rehabilitation services. Dev Neurorehabil. 2019;22(2):87–97. doi: 10.1080/17518423.2018.1434698. [DOI] [PubMed] [Google Scholar]
- 35.Baughcum AE, C.A, Winning AM, Shultz EL, Keim MC, Humphrey LM, Schlegel AB, Gerhardt CA. Perspectives from bereaved parents on improving end of life care in the NICU. Clin Pract Pediatr Psychol. 2017;5:392–403. [Google Scholar]
- 36.Brooten D, Youngblut JM, Seagrave L, Caicedo C, Hawthorne D, Hidalgo I, et al. Parent’s Perceptions of Health Care Providers Actions Around Child ICU Death: What Helped, What Did Not. Am J Hospice Palliat Med. 2013;30(1):40–9. doi: 10.1177/1049909112444301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brouwer M, Maeckelberghe ELM, van der Heide A, Hein I, Verhagen E. Barriers in care for children with life-threatening conditions: a qualitative interview study in the Netherlands. BMJ Open. 2020;10(6):e035863. doi: 10.1136/bmjopen-2019-035863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Butler AE, Hall H, Copnell B. The changing nature of relationships between parents and healthcare providers when a child dies in the paediatric intensive care unit. J Adv Nurs (John Wiley & Sons, Inc) 2018;74(1):89–99. doi: 10.1111/jan.13401. [DOI] [PubMed] [Google Scholar]
- 39.Butler AE, Hall H, Copnell B. Becoming a Team: The Nature of the Parent-Healthcare Provider Relationship when a Child is Dying in the Pediatric Intensive Care Unit. J Pediatr Nurs. 2018;40:e26–e32. doi: 10.1016/j.pedn.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 40.Butler AE, Copnell B, Hall H. “Some were certainly better than others” – Bereaved parents’ judgements of healthcare providers in the paediatric intensive care unit: a grounded theory study. Intensive Crit Care Nurs. 2018;45:18–24. doi: 10.1016/j.iccn.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 41.Butler AE, Copnell B, Hall H. Welcoming expertise: Bereaved parents' perceptions of the parent–healthcare provider relationship when a critically ill child is admitted to the paediatric intensive care unit. Australian Crit Care. 2019;32(1):34–9. doi: 10.1016/j.aucc.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 42.Callans KM, Bleiler C, Flanagan J, Carroll DL. The Transitional Experience of Family Caring for Their Child With a Tracheostomy. J Pediatr Nurs. 2016;31(4):397–403. doi: 10.1016/j.pedn.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 43.Carnevale FA, Gaudreault J. The experience of critically ill children: A phenomenological study of discomfort and comfort. Dynamics (Pembroke, Ont) 2013;24(1):19–27. [PubMed] [Google Scholar]
- 44.Carnevale FA, Benedetti M, Bonaldi A, Bravi E, Trabucco G, Biban P. Understanding the private worlds of physicians, nurses, and parents: a study of life-sustaining treatment decisions in Italian paediatric critical care. J Child Health Care. 2011;15(4):334–49. doi: 10.1177/1367493511420183. [DOI] [PubMed] [Google Scholar]
- 45.Cicero-Oneto CE, Valdez-Martinez E, Bedolla M. Decision-making on therapeutic futility in Mexican adolescents with cancer: a qualitative study. BMC Med Ethics. 2017;18(1):74. doi: 10.1186/s12910-017-0231-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coats H, Rishel CJ. Journeys of Hope. J Hosp Palliat Nurs. 2016;18(5):436–42. doi: 10.1097/njh.0000000000000269. [DOI] [Google Scholar]
- 47.Conway MF, Pantaleao A, Popp JM. Parents' Experience of Hope When Their Child Has Cancer: Perceived Meaning and the Influence of Health Care Professionals. J Pediatr Oncol Nurs. 2017;34(6):427–34. doi: 10.1177/1043454217713454. [DOI] [PubMed] [Google Scholar]
- 48.Coyne I, Amory A, Kiernan G, Gibson F. Children's participation in shared decision-making: Children, adolescents, parents and healthcare professionals' perspectives and experiences. Eur J Oncol Nurs. 2014;18(3):273–80. doi: 10.1016/j.ejon.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 49.Dahav P, Sjöström-Strand A. Parents' experiences of their child being admitted to a paediatric intensive care unit: a qualitative study–like being in another world. Scand J Caring Sci. 2018;32(1):363–70. doi: 10.1111/scs.12470. [DOI] [PubMed] [Google Scholar]
- 50.Darbyshire P, Mischo-Kelling M, Lochner L, Messerschmidt-Grandi C. 'Fighting for care': parents' perspectives of children's palliative care in South Tyrol, Italy. Int J Palliat Nurs. 2015;21(11):542–7. doi: 10.12968/ijpn.2015.21.11.542. [DOI] [PubMed] [Google Scholar]
- 51.Davies S, Salmon P, Young B. When trust is threatened: Qualitative study of parents' perspectives on problematic clinical relationships in child cancer care. Psycho-Oncology. 2017;26(9):1301–6. doi: 10.1002/pon.4454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Engler J, Gruber D, Engler F, Hach M, Seipp H, Kuss K, et al. Parents' Perspectives on Hospital Care for Children and Adolescents with Life-Limiting Conditions: A Grounded Theory Analysis of Narrative Interviews. J Palliat Med. 2020;23(4):466–74. doi: 10.1089/jpm.2019.0245. [DOI] [PubMed] [Google Scholar]
- 53.Engvall G, Angstrom-Brannstrom C, Mullaney T, Nilsson K, Wickart-Johansson G, Svard AM, et al. It Is Tough and Tiring but It Works–Children's Experiences of Undergoing Radiotherapy. PLoS One. 2016;11(4):e0153029. doi: 10.1371/journal.pone.0153029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Enskar K, Darcy L, Bjork M, Knutsson S, Huus K. Experiences of Young Children With Cancer and Their Parents With Nurses' Caring Practices During the Cancer Trajectory. J Pediatr Oncol Nurs. 2020;37(1):21–34. doi: 10.1177/1043454219874007. [DOI] [PubMed] [Google Scholar]
- 55.Falck AJ, Moorthy S, Hussey-Gardner B. Perceptions of Palliative Care in the NICU. Adv Neonatal Care. 2016;16(3):191–200. doi: 10.1097/ANC.0000000000000301. [DOI] [PubMed] [Google Scholar]
- 56.Falkenburg JL, Tibboel D, Ganzevoort RR, Gischler S, Hagoort J, van Dijk M. Parental Physical Proximity in End-of-Life Care in the PICU. Pediatr Crit Care Med. 2016;17(5):e212–e7. doi: 10.1097/pcc.0000000000000682. [DOI] [PubMed] [Google Scholar]
- 57.Falkenburg JL, Tibboel D, Ganzevoort RR, Gischler SJ, van Dijk M. The Importance of parental connectedness and relationships with healthcare professionals in end-of-Life Care in the PICU. Pediatr Crit Care Med. 2018;19(3):e157–e63. doi: 10.1097/pcc.0000000000001440. [DOI] [PubMed] [Google Scholar]
- 58.Fixter V, Butler C, Daniels J, Phillips S. A qualitative analysis of the information needs of parents of children with cystic fibrosis prior to first admission. J Pediatr Nurs. 2017;34:e29–e33. doi: 10.1016/j.pedn.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 59.Gabriel MG, Wakefield CE, Vetsch J, Karpelowsky JS, Darlington AE, Cohn RJ, et al. Paediatric surgery for childhood cancer: lasting experiences and needs of children and parents. Eur J Cancer Care. 2019;28(5):e13116. doi: 10.1111/ecc.13116. [DOI] [PubMed] [Google Scholar]
- 60.Gilmer MJ, Foster TL, Bell CJ, Mulder J, Carter BS. Parental perceptions of care of children at end of life. Am J Hosp Palliat Med. 2013;30(1):53–8. doi: 10.1177/1049909112440836. [DOI] [PubMed] [Google Scholar]
- 61.Greenway TL, Rosenthal MS, Murtha TD, Kandil SB, Talento DL, Couloures KG. Barriers to Communication in a PICU: A qualitative investigation of family and provider perceptions. Pediatr Crit Care Med. 2019;20(7). 10.1097/pcc.0000000000002070. [DOI] [PubMed]
- 62.Guttmann K, Flibotte J, DeMauro SB, Seitz H. A mixed methods analysis of parental perspectives on diagnosis and prognosis of neonatal intensive care unit graduates with cerebral palsy. J Child Neurol. 2020;35(5):336–43. doi: 10.1177/0883073820901412. [DOI] [PubMed] [Google Scholar]
- 63.Hemsley B, Kuek M, Bastock K, Scarinci N, Davidson B. Parents and children with cerebral palsy discuss communication needs in hospital. Dev Neurorehabil. 2013;16(6):363–74. doi: 10.3109/17518423.2012.758187. [DOI] [PubMed] [Google Scholar]
- 64.Hooghe A, Rosenblatt PC, De Jongh S, Bakker E, Nijkamp M, Rober P. "The child is our focus": on couple issues in child oncology treatment. Psycho-Oncology. 2018;27(10):2482–7. doi: 10.1002/pon.4855. [DOI] [PubMed] [Google Scholar]
- 65.Inglin S, Hornung R, Bergstraesser E. Palliative care for children and adolescents in Switzerland: a needs analysis across three diagnostic groups. Eur J Pediatr. 2011;170(8):1031–8. doi: 10.1007/s00431-011-1398-5. [DOI] [PubMed] [Google Scholar]
- 66.Iversen AS, Graue M, Raheim M. At the edge of vulnerability–lived experience of parents of children with cerebral palsy going through surgery. Int J Qual Stud Health Well-being. 2013;8:1–10. doi: 10.3402/qhw.v8i0.20007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kelly KP, Mowbray C, Pyke-Grimm K, Hinds PS. Identifying a conceptual shift in child and adolescent-reported treatment decision making: "Having a say, as I need at this time". Pediatr Blood Cancer. 2017;64(4):04. doi: 10.1002/pbc.26262. [DOI] [PubMed] [Google Scholar]
- 68.Kilicarslan-Toruner E, Akgun-Citak E. Information-seeking behaviours and decision-making process of parents of children with cancer. Eur J Oncol Nurs. 2013;17(2):176–83. doi: 10.1016/j.ejon.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 69.Lamiani G, Giannini A, Fossati I, Prandi E, Vegni E. Parental experience of end-of life care in the pediatric intensive care unit. Minerva Anestesiologica. 2013;79(12):1334–43. [PubMed] [Google Scholar]
- 70.Linder LA, Seitz M. Through their words: sources of bother for hospitalized children and adolescents with cancer. J Pediatr Oncol Nurs. 2017;34(1):51–64. doi: 10.1177/1043454216631308. [DOI] [PubMed] [Google Scholar]
- 71.Livesley J, Long T. Children's experiences as hospital in-patients: voice, competence and work. Messages for nursing from a critical ethnographic study. Int J Nurs Stud. 2013;50(10):1292–303. doi: 10.1016/j.ijnurstu.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 72.Mack JW, Ilowite M, Taddei S. Difficult relationships between parents and physicians of children with cancer: a qualitative study of parent and physician perspectives. Cancer. 2017;123(4):675–81. doi: 10.1002/cncr.30395. [DOI] [PubMed] [Google Scholar]
- 73.Markwalter DW, Murphy MA, Turnbull JM, Fanning JB. Framing the future: Family preparedness for care transitions of critically ill children. Fam Syst Health. 2019;37(3):212–23. doi: 10.1037/fsh0000431. [DOI] [PubMed] [Google Scholar]
- 74.McNamara LC, Okoniewski W, Maurer SH, Moehling K, Hall DE, Schenker Y. "Give them the door but don't push them through it": Family Attitudes Toward Physician-Led Spiritual Care in Pediatric Palliative Medicine. J Religion Health. 2020;12:12. doi: 10.1007/s10943-020-00991-z. [DOI] [PubMed] [Google Scholar]
- 75.Mitchell S, Spry JL, Hill E, Coad J, Dale J, Plunkett A. Parental experiences of end of life care decision-making for children with life-limiting conditions in the paediatric intensive care unit: a qualitative interview study. BMJ Open. 2019;9(5):e028548. doi: 10.1136/bmjopen-2018-028548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Murrell DV, Crawford CA, Jackson CT, Lotze TE, Wiemann CM. Identifying Opportunities to Provide Family-centered Care for Families With Children With Type 1 Spinal Muscular Atrophy. J Pediatr Nurs. 2018;43:111–9. doi: 10.1016/j.pedn.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 77.Nicholas DB, Beaune L, Barrera M, Blumberg J, Belletrutti M. Examining the experiences of fathers of children with a life-limiting illness. J SocWork End-Of-Life Palliat Care. 2016;12(1–2):126–44. doi: 10.1080/15524256.2016.1156601. [DOI] [PubMed] [Google Scholar]
- 78.Nyborn JA, Olcese M, Nickerson T, Mack JW. "Don't try to cover the sky with your hands": parents' experiences with prognosis communication about their children with advanced cancer. J Palliat Med. 2016;19(6):626–31. doi: 10.1089/jpm.2015.0472. [DOI] [PubMed] [Google Scholar]
- 79.Obas KA, Leal JM, Zegray M, Rennick JE. Parental perceptions of transition from intensive care following a child's cardiac surgery. Nurs Crit Care. 2016;21(3):e1–e9. doi: 10.1111/nicc.12202. [DOI] [PubMed] [Google Scholar]
- 80.October TW, Fisher KR, Feudtner C, Hinds PS. The parent perspective: "being a good parent" when making critical decisions in the PICU. Pediatr Crit Care Med. 2014;15(4):291–8. doi: 10.1097/PCC.0000000000000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Orioles A, Miller VA, Kersun LS, Ingram M, Morrison WE. "To be a phenomenal doctor you have to be the whole package": physicians' interpersonal behaviors during difficult conversations in pediatrics. J Palliat Med. 2013;16(8):929–33. doi: 10.1089/jpm.2013.0103. [DOI] [PubMed] [Google Scholar]
- 82.Oxley R. Parents' experiences of their child's admission to paediatric intensive care. Nurs Child Young People. 2015;27(4):16–21. doi: 10.7748/ncyp.27.4.16.e564. [DOI] [PubMed] [Google Scholar]
- 83.Pinto Taylor E, Doolittle B. Caregiver decision-making for terminally ill children: a qualitative study. J Palliat Care. 2020;35(3):161–6. doi: 10.1177/0825859719885947. [DOI] [PubMed] [Google Scholar]
- 84.Robertson EG, Wakefield CE, Shaw J, Darlington AS, McGill BC, Cohn RJ, et al. Decision-making in childhood cancer: parents' and adolescents' views and perceptions. Supp Care Cancer. 2019;27(11):4331–40. doi: 10.1007/s00520-019-04728-x. [DOI] [PubMed] [Google Scholar]
- 85.Roscigno CI. Parent Perceptions of How Nurse Encounters Can Provide Caring Support for the Family in Early Acute Care After Children's Severe Traumatic Brain Injury. J Neurosci Nurs. 2016;48(2):E2–E15. doi: 10.1097/jnn.0000000000000192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ruhe KM, Badarau DO, Brazzola P, Hengartner H, Elger BS, Wangmo T. Participation in pediatric oncology: views of child and adolescent patients. Psycho-Oncology. 2016;25(9):1036–42. doi: 10.1002/pon.4053. [DOI] [PubMed] [Google Scholar]
- 87.Saetrang T, Bjork IT, Capjon H, Rasmussen M. Parent-child communication and timing of interventions are challenges in the Duchenne muscular dystrophy care. Acta Paediatrica. 2019;108(3):535–40. doi: 10.1111/apa.14537. [DOI] [PubMed] [Google Scholar]
- 88.Salmon P, Hill J, Ward J, Gravenhorst K, Eden T, Young B. Faith and protection: the construction of hope by parents of children with leukemia and their oncologists. Oncologist. 2012;17(3):398–404. doi: 10.1634/theoncologist.2011-0308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Skirko JR, Pollard SH, Slager S, Hung M, Weir C. Family experience with pierre robin sequence: a qualitative study. Cleft Palate-Craniofacial J. 2020;57(6):736–45. doi: 10.1177/1055665620910331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Smith J, Cheater F, Bekker H. Parents' experiences of living with a child with hydrocephalus: a cross-sectional interview-based study. Health Expectations. 2015;18(5):1709–20. doi: 10.1111/hex.12164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Smith C, Randle-Phillips C. Parental experiences of a paediatric renal service. J Kidney Care. 2018;3(6):355–61. doi: 10.12968/jokc.2018.3.6.355. [DOI] [Google Scholar]
- 92.Snaman JM, Torres C, Duffy B, Levine DR, Gibson DV, Baker JN. Parental Perspectives of Communication at the End of Life at a Pediatric Oncology Institution. J Palliat Med. 2016;19(3):326–32. doi: 10.1089/jpm.2015.0253. [DOI] [PubMed] [Google Scholar]
- 93.Spalding J, Yardley S. 'The nice thing about doctors is that you can sometimes get a day off school': an action research study to bring lived experiences from children, parents and hospice staff into medical students' preparation for practice. BMJ Supp Palliat Care. 2016;6(4):459–64. doi: 10.1136/bmjspcare-2015-001080. [DOI] [PubMed] [Google Scholar]
- 94.Spratling R. The experiences of medically fragile adolescents who require respiratory assistance. J Adv Nurs (John Wiley & Sons, Inc) 2012;68(12):2740–9. doi: 10.1111/j.1365-2648.2012.05979.x. [DOI] [PubMed] [Google Scholar]
- 95.Steele AC, Kaal J, Thompson AL, Barrera M, Compas BE, Davies B, et al. Bereaved parents and siblings offer advice to health care providers and researchers. J Pediatr Hematol/Oncol. 2013;35(4):253–9. doi: 10.1097/MPH.0b013e31828afe05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sullivan J, Monagle P, Gillam L. What parents want from doctors in end-of-life decision-making for children. Arch Dis Childhood. 2014;99(3):216–20. doi: 10.1136/archdischild-2013-304249. [DOI] [PubMed] [Google Scholar]
- 97.Tenniglo LJA, Loeffen EAH, Kremer LCM, Font-Gonzalez A, Mulder RL, Postma A, et al. Patients' and parents' views regarding supportive care in childhood cancer. Support Care Cancer. 2017;25(10):3151–60. doi: 10.1007/s00520-017-3723-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Thienprayoon R, Marks E, Funes M, Martinez-Puente LM, Winick N, Lee SC. Perceptions of the Pediatric Hospice Experience among English- and Spanish-Speaking Families. J Palliat Med. 2016;19(1):30–41. doi: 10.1089/jpm.2015.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tong A, Lowe A, Sainsbury P, Craig JC. Parental perspectives on caring for a child with chronic kidney disease: an in-depth interview study. Child. 2010;36(4):549–57. doi: 10.1111/j.1365-2214.2010.01067.x. [DOI] [PubMed] [Google Scholar]
- 100.Wangmo T, Ruhe KM, Badarau DO, Kuhne T, Niggli F, Elger BS, et al. Parents' and patients' experiences with paediatric oncology care in Switzerland–satisfaction and some hurdles. Swiss Med Weekl. 2016;146:w14309. doi: 10.4414/smw.2016.14309. [DOI] [PubMed] [Google Scholar]
- 101.Watt L, Dix D, Gulati S, Sung L, Klaassen RJ, Shaw NT, et al. Family-centred care: a qualitative study of Chinese and South Asian immigrant parents' experiences of care in paediatric oncology. Child. 2013;39(2):185–93. doi: 10.1111/j.1365-2214.2011.01342.x. [DOI] [PubMed] [Google Scholar]
- 102.Weidner NJ, Cameron M, Lee RC, McBride J, Mathias EJ, Byczkowski TL. End-of-life care for the dying child: what matters most to parents. J Palliat Care. 2011;27(4):279–86. doi: 10.1177/082585971102700404. [DOI] [PubMed] [Google Scholar]
- 103.Young B, Ward J, Salmon P, Gravenhorst K, Hill J, Eden T. Parents' experiences of their children's presence in discussions with physicians about Leukemia. Pediatrics. 2011;127(5):e1230–8. doi: 10.1542/peds.2010-2402. [DOI] [PubMed] [Google Scholar]
- 104.Young B, Hill J, Gravenhorst K, Ward J, Eden T, Salmon P. Is communication guidance mistaken? Qualitative study of parent-oncologist communication in childhood cancer. Br J Cancer. 2013;109(4):836–43. doi: 10.1038/bjc.2013.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yuen WY, Duipmans JC, Jonkman MF. The needs of parents with children suffering from lethal epidermolysis bullosa. Br J Dermatol. 2012;167(3):613–8. doi: 10.1111/j.1365-2133.2012.10993.x. [DOI] [PubMed] [Google Scholar]
- 106.Zitzelsberger H, McKeever P, Peter E, Chambon A, Morgan KP, Spalding K. Doing 'technological time’ in a pediatric hemodialysis unit: an ethnography of children. Health Place. 2014;27:112–9. doi: 10.1016/j.healthplace.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 107.Davies C, Fraser J, Waters D. Establishing a framework for listening to children in healthcare. Journal of Child Health Care. 2019:1367493519872078.10.1177/1367493519872078. [DOI] [PubMed]
- 108.White L. Rights of children and young people in health care. J Paediatr Child Health. 2020;56(4):499–501. doi: 10.1111/jpc.14802. [DOI] [PubMed] [Google Scholar]
- 109.Hargreaves DS, Lemer C, Ewing C, Cornish J, Baker T, Toma K, et al. Measuring and improving the quality of NHS care for children and young people. Arch Dis Child. 2019;104(7):618–21. doi: 10.1136/archdischild-2017-314564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ehrich J, Namazova-Baranova L, Pettoello-Mantovani M. Introduction to “Diversity of Child Health Care in Europe: A Study of the European Paediatric Association/Union of National European Paediatric Societies and Associations”. J Pediatr. 2016;177:S1–S10. doi: 10.1016/j.jpeds.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 111.Chesney M, Lindeke L, Johnson L, Jukkala A, Lynch S. Comparison of child and parent satisfaction ratings of ambulatory pediatric subspecialty care. J Pediatr Health Care. 2005;19(4):221–9. doi: 10.1016/j.pedhc.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 112.Hargreaves DS, Sizmur S, Pitchforth J, Tallett A, Toomey SL, Hopwood B, et al. Children and young people’s versus parents’ responses in an English national inpatient survey. Arch Dis Childhood. 2018;103(5):486. doi: 10.1136/archdischild-2017-313801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mah JK, Tough S, Fung T, Douglas-England K, Verhoef M. Adolescent quality of life and satisfaction with care. J Adolesc Health. 2006;38(5):607.e1–7. doi: 10.1016/j.jadohealth.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 114.Albanese AM, Russo GR, Geller PA. The role of parental self-efficacy in parent and child well-being: A systematic review of associated outcomes. Child. 2019;45(3):333–63. doi: 10.1111/cch.12661. [DOI] [PubMed] [Google Scholar]
- 115.Pinquart M. Parenting stress in caregivers of children with chronic physical condition—A meta-analysis. Stress Health. 2018;34(2):197–207. doi: 10.1002/smi.2780. [DOI] [PubMed] [Google Scholar]
- 116.Lebowitz ER, Leckman JF, Silverman WK, Feldman R. Cross-generational influences on childhood anxiety disorders: pathways and mechanisms. J Neural Transm (Vienna) 2016;123(9):1053–67. doi: 10.1007/s00702-016-1565-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.van Santvoort F, Hosman CMH, Janssens JMAM, van Doesum KTM, Reupert A, van Loon LMA. The Impact of Various Parental Mental Disorders on Children’s Diagnoses: A Systematic Review. Clin Child Fam Psychol Rev. 2015;18(4):281–99. doi: 10.1007/s10567-015-0191-9. [DOI] [PubMed] [Google Scholar]
- 118.Aldiss S, Fern LA, Phillips R, Callaghan A, Dyker KE, Gravestock HL, et al. Research priorities for young people with cancer: a UK priority setting partnership with the James Lind Alliance. BMJ Open. 2019;9:e028119. 10.1136/bmjopen-2018-028119. [DOI] [PMC free article] [PubMed]
- 119.Beresford BBA, Fraser LK. A consultation with stakeholders about research priorities for the Martin House Research Centre. York: University of York, Martin House Research Centre; 2017. [Google Scholar]
- 120.Koller D. Right of children to be heard. BMJ Paediatrics Open. 2021;5(1):e001161. doi: 10.1136/bmjpo-2021-001161. [DOI] [Google Scholar]
- 121.Fargas-Malet M, McSherry D, Larkin E, Robinson C. research with children: methodological issues and innovative techniques. J Early Childhood Res. 2010;8(2):175–92. doi: 10.1177/1476718X09345412. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary File 1. Literature review search strategies.
Additional file 2: SupplementaryFile 2. Final versions of data extraction frameworks.
Additional file 3: Supplementary File 3. Extract from a thematic table used for main analysis.
Additional file 4: Supplementary File 4. The impacts of health service delivery and care on children and young people - List of codes and their definitions.
Additional file 5: Supplementary File 5. The impacts of health service delivery and care on parents- List of codes and their definitions.
Additional file 6: Supplementary File 6. Additional study characteristics.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.