Abstract
The transition to parenthood is a stressful period for most parents as individuals and as couples, with variability in parent mental health and couple relationship functioning linked to children’s long-term emotional, mental health, and academic outcomes. Few couple-focused prevention programs targeting this period have been shown to be effective. The purpose of this study was to test the short-term efficacy of a brief, universal, transition-to-parenthood intervention (Family Foundations) and report the results of this randomized trial at 10 months postpartum. This was a randomized controlled trial; 399 couples expecting their first child were randomly assigned to intervention or control conditions after pretest. Intervention couples received a manualized nine-session (five prenatal and four postnatal classes) psychoeducational program delivered in small groups. Intent-to-treat analyses indicated that intervention couples demonstrated better posttest levels than control couples on more than two thirds of measures of coparenting, parent mental health, parenting, child adjustment, and family violence. Program effects on family violence were particularly large. Of eight outcome variables that did not demonstrate main effects, seven showed moderated intervention impact; such that, intervention couples at higher levels of risk during pregnancy showed better outcomes than control couples at similar levels of risk. These findings replicate a prior smaller study of Family Foundations, indicating that the Family Foundations approach to supporting couples making the transition to parenthood can have broad impact for parents, family relationships, and children’s adjustment. Program effects are consistent and benefit all families, with particularly notable effects for families at elevated prenatal risk.
Keywords: Coparenting, Intervention, Transition to parenthood
Introduction
There is substantial variability in couples’ adjustment to parenthood, but a majority of new families experience significant strains during this period (Cowan and Cowan 2000; Heinicke 2002). On average, couples’ relationship quality declines across the transition more than it does for couples who do not have children (Doss et al. 2009; Lawrence et al. 2008), and rates of relationship conflict and distress increase (Slep and O’Leary 2005). Some couples never recover from these strains, and relationship problems and conflict become the “new normal,” leading to separation and divorce. Moreover, new parents experience high levels of role overload and stress, leading to increased depression and anxiety (Lipman and Boyle 2008). These individual- and couple-level strains have been linked to diminished parenting quality (Karreman et al. 2008; Krishnakumar and Buehler 2000). Further, levels of family violence (both intimate partner violence [IPV] and parent-to-child violence [PCV]) are high, perhaps highest, when children are young (Slep and O’Leary 2005). Couple conflict, parent maladjustment, poor parenting quality, and family violence are all linked with subsequent child mental health, behavioral, and academic problems (Kaczynski et al. 2006; Zimet and Jacob 2001).
The irony is that this concentration of individual and family risk in the years following family formation occurs when children are most vulnerable. Stressors due to parent and family dysfunction during these early years pose risks to children’s rapid development in all biological systems subserving adaptive functioning (e.g., emotional regulation, social engagement, executive functioning) (McCollum and Ostrosky 2008). These risk factors are additionally linked to children’s physical health (Beijers et al. 2010).
Efficacious prevention programs at the transition to parenthood have been developed for the highest-risk families. Home visiting programs have been shown to enhance maternal adjustment and child outcomes when targeted at high-risk (e.g., low income, low education) pregnant women (Olds 2006). Yet, the strains of parenthood and consequent negative impact on children extend beyond the few percent of the population targeted by such programs. Moreover, infants and young children are susceptible to moderately elevated, not just extreme, dysfunction in the proximal family environment (Shonkoff 2010). For example, the prevalence of postpartum maternal depression is about 15 % (Segre et al. 2007); additionally, at least an equivalent proportion of new mothers experience chronically low mood (dysthymia) or subclinical levels of depression, which also likely impact parenting and child outcomes. Similarly, a large proportion of families with young children are at risk for family violence; research utilizing an anonymous reporting procedure indicates that the rate of IPV among parents and among children ages 3–7 is ~50 % (Slep and O’Leary 2005). The rate of PCV (including corporal punishment, which is linked with children’s maladjustment) in this age group is nearly 90 %; 13 % of such families demonstrate severe forms of PCV.
Public health experts recommend implementing effective universal prevention programs, in combination with more intensive and targeted programs for higher-risk parents, to reduce population-level public health problems (Sanders and Morawska 2006). Given high rates of parent and family problems in the years after birth, the logistical burden of screening expectant parents, and the imprecision of current screening tools for the emergence of such problems after birth (McDonald et al. 2012), an effective universal approach to prevention among new families is needed. Accordingly, we developed Family Foundations (FF) as a universal prevention program for first-time expectant couples that could be easily disseminated. The program consists of a series of nine classes before and after birth with a strategic focus on enhancing the coparenting relationship. This strategy was based on evidence that the coparenting relationship, defined as the way parents support and coordinate with each other in their roles as parents, is linked to parent adjustment, parenting, and child adjustment (Feinberg 2002; Feinberg 2003; Feinberg et al. 2007; Schoppe et al. 2001). The development of FF was partly based on the innovative approach of supporting couples at the transition to parenthood that was the focus of an early program developed by Philip and Carolyn Cowan (Schulz et al. 2006). However, aspects of the Cowans’ innovative approach posed obstacles for dissemination; it involved a large number of sessions (weekly meetings over 6 months); there was limited manualization of content; and high levels of knowledge, expertise, and skill were required on the part of facilitators (in the only trial, groups were led by the program developers and their graduate students).
While not replicated, the success of the Cowans’ early effort paved the way for a number of other projects and studies that have aimed to support couples at the transition. However, few if any such programs have both utilized rigorous evaluation methods and shown strong positive impact (Pinquart and Teubert 2010). For example, Shapiro and Gottman (2005) purported to show impact on parent depression and relationship quality. However, several flaws (e.g., the Gottmans served as group facilitators; the study had a small sample size; attrition occurred but was poorly described; missing data procedure employed was inappropriate) limit the validity of the study. A more rigorous study in Australia (Halford et al. 2010) found that a couple relationship intervention adapted for expectant parents had mixed results on measures of couple relationship quality and little to no impact on parental stress and parenting. The very large (N = 6500) Building Strong Families study tested adaptations of leading couple-focused prevention programs for low- and moderate-income couples at the transition to parenthood (Wood et al. 2012). Although the interventions were intensive and included group sessions as well as caseworker support, there was no overall impact on participants.
In contrast to null or limited evidence of impact in the aforementioned couple-focused transition to parenthood prevention trials, an initial efficacy trial of FF with 169 couples at two hospitals yielded significant impact on all targeted domains (with moderate to strong effect sizes), coparenting, parent stress and maternal depression, and parenting quality by parent and observer ratings through 3 years after birth (Feinberg et al. 2010). Moreover, teachers of children at age 7 reported significantly fewer emotional problems and (for boys) externalizing problems; among families with higher levels of prenatal couple conflict, intervention effects also included better academic adjustment and fewer externalizing problems for both boys and girls (Feinberg et al. 2014). Although not hypothesized as an outcome originally, recent evidence that stress, depression, and anxiety are linked to adverse birth outcomes led us to investigate program impact on such outcomes. Indeed, among mothers who displayed moderate to high levels of prenatal cortisol levels, exposure to the intervention was associated with less preterm birth and low birth weight, as well as shorter duration of hospital stay after birth (Feinberg et al. 2015a, b).
However, replication of results is needed as experience indicates that promising results from a first intervention trial are often followed by disappointing results in a second trial (Ioannidis 2005). Thus, this paper reports results from a second efficacy trial of FF with a larger sample. A change made in the intervention was to incorporate childbirth education material into the prenatal FF classes in order to reduce the need for parents to enroll in more than one prenatal preparation program; to accommodate this material, we condensed some of the prenatal Family Foundations class material presented in the first trial. We have recently reported results from this second trial that replicate findings from the first trial of program impact on birth outcomes (Feinberg et al. 2015a, b). In the current paper, we report the results of this second trial at posttest (10 months postpartum), based on parent-reported and observational measures of parent mental health, coparenting and couple relations, parenting quality, and child adjustment. We hypothesized that participation in FF would predict better outcomes in all targeted domains, coparenting, parent stress and depression, and parenting quality. Moreover, given the tendency in prevention trials for the strongest effects to emerge for those at highest risk (e.g., Spoth et al. 2007; but see Markman et al. 2013), we hypothesized that where FF participation did not predict better outcomes for the whole subsample, follow-up analyses would demonstrate program effects for families at higher risk for a poor transition to parenthood. Based on our prior research (Feinberg et al. 2014; Kan and Feinberg 2015; Kan and Feinberg 2014), we operationalized risk in terms of prenatal (pretest) level of observed couple conflict and parent depressive symptoms. These two risk factors pose substantial challenges to parents and impact both parenting quality and child adjustment (Feinberg 2003).
Methods
Three-hundred and ninety-nine heterosexual couples who were living together and expecting their first child were recruited into the study. Recruitment took place through childbirth education programs and OB/GYN clinics located in or near one of five hospitals in three Mid-Atlantic states and one southern state (three hospitals were in urban areas and two suburban). Each participant was required to be at least 18 years of age. At enrollment, the mean age of expectant mothers and fathers was 29.1 years (SD = 4.4) and 31.1 years (SD = 5.4), respectively; mean education level was 15.7 years (SD = 1.5); median household income was $87,500; 87 % of couples were married; and 81 % of participants were non-Hispanic white, 7 % Hispanic, 6 % black, 4 % Asian, and 2 % multiple race/ethnicities.
Procedures
The study was approved by university and hospital IRBs, and participants provided informed consent. Project staff collected pretest data during a home visit during pregnancy (mothers averaged 22.8-week gestation, SD = 5.5). The research assistant video-recorded couple interactions and asked each expectant parent to complete a set of questionnaires in private. After the visit, each couple was randomly assigned to condition by the project manager using a randomized block design (see Fig. 1). Posttest data were collected in a second home visit at 10 months after birth with similar procedures. Videotaped observation included triadic family interaction. Data collection took place from 2008 to 2014.
Fig. 1.
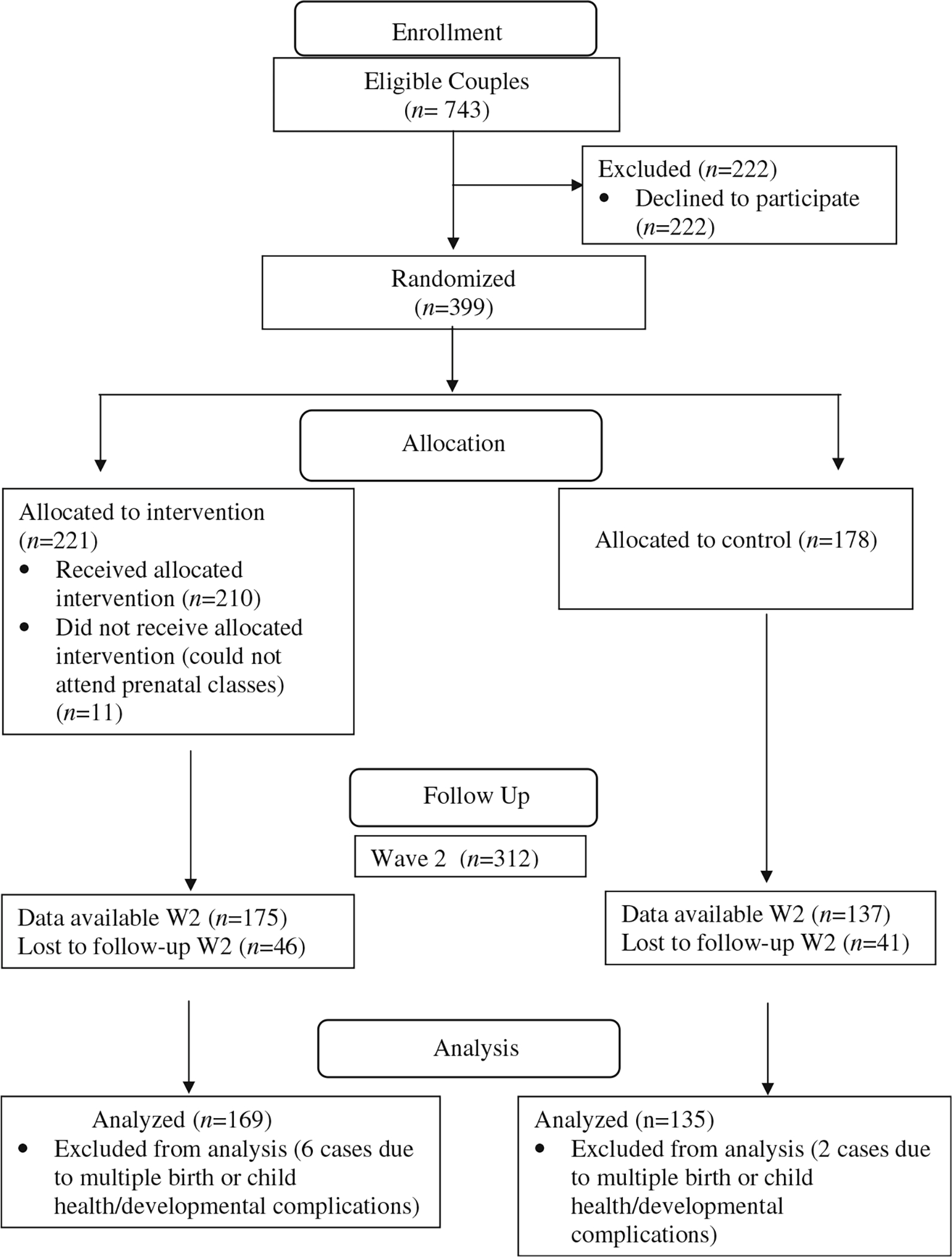
Family Foundations consort flow diagram
Baseline equivalence was assessed by examining group differences on over 60 measured preintervention variables (including demographic characteristics and pretest versions of study outcomes). We found no patterns of statistical differences between groups from this assessment. Twenty-two percent of the sample did not participate at posttest. We conducted logistic regressions examining multivariable prediction of posttest participation; interaction terms between condition and specific predictors were examined as representing differential attrition. Predictors included baseline parent and couple characteristics representing stress, mental health, and relationship qualities. We found no evidence of differential attrition between conditions.
To accommodate missing data, we employed multiple imputation (MI) techniques involving standard procedures (Graham 2012; Yuan 2011) and 60 imputed datasets. Missing data models were carried out separately by intervention group and involved many baseline characteristics including SES, mental health/stress levels, couple relationship quality, and other demographic factors. We excluded eight families (six intervention and two control) due to severe parent or infant medical problems (e.g., severe congenital defect, poor maternal health), developmental disorders (e.g., autism, Down syndrome), or multiple births. We note that results from complete case analyses and analyses using MI models were very similar. Because of the amount of missing data at posttest, we present results using MI in the “Results” section below.
Intervention and Control Conditions
The FF intervention program consisted of five classes before birth (3 h each) and four after birth (2 h each), focusing on coparental conflict resolution and problem solving, communication, and mutual support strategies. Classes (with 8 to 12 couples) were held at health care facilities and involved a range of instructional modalities, including presentations, discussion, couple and group skill-building exercises (e.g., role plays), and the viewing of video vignettes. The FF prenatal classes included standard childbirth education material. Classes were led by a team of male-female facilitators who were employees of the hospitals or contracted to the research team. Training consisted of three full days at each site, and supervision was provided by the research team after each session until facilitators had achieved familiarity and competence in the model. Control group families were mailed written materials on selecting quality child care and the stages of child development. Intervention couples attended an average of 4.4 (SD = 1.2) prenatal classes and 2.3 (SD = 1.7) postnatal classes, for a total average attendance of 6.7 of the 9 classes. More than half of couples attended at least eight of the nine classes. For each cohort, one prenatal and one postnatal class were videotaped and rated by a trained, reliable observer for implementation quality. Observer ratings indicated high-implementation fidelity, with an average of 90 % of content delivered as planned.
Observational Measures
Undergraduate research assistants were trained to code videotaped interactions according to a global coding system utilizing five- to seven-point scales. The codes for coparenting, parenting, child behavior, and couple interaction were developed for this project or adapted from codes utilized in prior work (Britner et al. 2005; Feinberg et al. 2009; Malik and Lindahl 2004; Margolin et al. 2004; McHale et al. 2001). One experienced coder served as a criterion coder. Extensive training consisted of study of the coding manual and ongoing coding tutorial sessions. Coders were blind to intervention condition. Separate teams of coders focused on each domain, coparenting, parenting, child behavior, and dyadic couple behaviors. All cases were coded by a single rater with between 10 and 25 % of cases coded by at least two raters to assess reliability. Interrater intraclass correlations ranged from 0.66 to 0.85. Aggregation of codes into index variables was guided by conceptual models and empirical assessment of covariance. Individual scales were standardized (mean = 0) before combining into composite scores. Further details for all measures are available in the Appendix.
Coparenting
An aggregate index of coparenting positivity was created as an average of the following three codes: coparental warmth, cooperation, and inclusiveness. Measures of coparenting negativity included separate ratings of coparental withdrawal, competition, and hostility; these codes were not combined into an overall negativity aggregate due to low internal consistency. We also included a code representing overall triadic relationship quality and a code assessing parent’s positive endorsement of the partner’s parenting.
Couple Relationship Quality
A positive communication aggregate comprised codes for listening, problem solving, and support for the partner. Negative communication was comprised of an average of codes for aggression and anger. The pretest negative communication composite served as a moderator of intervention effects, as described in the “Results” section; the posttest negative communication composite served as a study outcome.
Parenting Quality
Parenting positivity combined the following three codes: affection, sensitivity, and support for exploration. Negativity was created from codes for parental rejection and negative affect. Autonomy support combined (reversed) codes for intrusiveness and pressure to achieve.
Parent-Report Measures
Coparenting and Couple Relations
Coparenting quality as perceived by parents was represented through a total score on the 33-item Coparenting Relationship Scale (Feinberg et al. 2012) (α = 0.85 for mothers, α = 0.83 for fathers). In addition to coparenting, we assessed general relationship satisfaction with the Quality of Marriage Index (Norton 1983) (α = 0.96 for mothers and fathers).
Parent Adjustment
Depressive symptoms at posttest were assessed with the CES-Depression Scale (Radloff 1977) (α = 0.85 for mothers, α = 0.83 for fathers). Depression measured at pretest served as a moderator of intervention effects; posttest depression served as a study outcome. We measured anxiety using the 10-Item Trait Scale from the State-Trait Anxiety Inventory Scale (Spielberger et al. 1983) (α = 0.90 for mothers, α = 0.88 for fathers), as well as the total score from the Penn State Worry Questionnaire (Beck et al. 1995; Meyer et al. 1990) (α = 0.94 for mothers and α = 0.93 for fathers). Parenting stress was assessed with 27 items of the brief version of the Parenting Stress Index (Abidin 1995) (α = 0.91 for mothers and fathers).
Child Outcomes
Parents reported on two scales of the Infant Behavior Questionnaire, child soothability and duration of orientation (i.e., attention span) (Gartstein and Rothbart 2003). Alphas for soothability and duration of orientation were 0.77 and 0.78 among mothers and 0.75 and 0.83 among fathers, respectively. Mothers only reported on the following three items from the Child Sleep Questionnaire (Seifer et al. 1996): the number of nighttime wakings, difficulty going back to sleep, and total duration of child nighttime sleep.
Family violence was assessed using the Conflict Tactics Scale (Straus et al. 1996) for IPV and the Parent-Child Conflict Tactics Scale (Straus et al. 1998). Two scores represented psychological aggression and physical assault (in counts of behaviors in the past year) on each measure. To prevent undue influence of extreme values, we capped counts of psychological aggression items at 60 instances per year (affecting 3 extreme cases for IPV) and counts of physical violence items at 45 (affecting 3 extreme cases for both IPV and PCV).
Control variables utilized in all analytic models included design factors and participant background, including study site, parent age, parent gender, family income, marital status, and reported financial strain. A measure of social desirability was included to control for potential response bias (Crowne and Marlow 1960; Marlow and Crowne 1961) for self-report outcomes (α = 0.64 for mothers and 0.65 for fathers). We included the corresponding pretest measure of each outcome as a control variable if available (parenting or child outcomes were not measured at pretest). For coparenting and dyadic couple variables, we utilized a measure of couple efficacy—the degree to which partners felt that their relationship was resilient—as a proxy pretest control variable (Fincham and Bradbury 1987) (α = 0.85 for mothers and 0.84 for fathers). Child age (in months) was included in analyses of child outcomes.
Analytic Models
We used separate regression models to test the main effect of the condition (1 = intervention; 0 = control) for each outcome. For parent-specific outcomes nested within dyad, we used multilevel regression models with a random intercept specified to represent couple-level shared variance (Goldstein 2011). We used ordinary regression models for outcomes available only at the family level, mother-reported child sleep (fathers did not report on child sleep) and observed triadic relationship quality. The number of violent incidents was modeled with negative-binomial regression models. Prior research of FF has demonstrated moderated intervention impact where no main effects were evident (Feinberg et al. 2014). We focused on the following two moderators measured separately for each parent at pretest: observed negative communication and self-reported depression.
Results
Table 1 contains full descriptive information (means and standard deviations) on the pretest control variables and posttest outcomes, separately by intervention condition. Table 2 shows the results of the tests of main effects of the intervention determined using regression models. Regression coefficients (b) are provided along with effect sizes (Durlak 2009) that enable assessment of standardized group differences on the outcomes. The latter were determined using model-adjusted group mean differences enabling Cohen’s d, except for results from count models for which we provide incidence rate ratios (IRR). We found evidence of statistically significant main effects of intervention condition on numerous outcomes, spanning all outcome domains. For outcomes available separately for each parent, we found no evidence of significant moderation of intervention effects based on parent sex (not tabled). This was determined through inclusion of a gender X intervention status interaction term that was removed in final models.
Table 1.
Sample descriptive statistics, by gender and intervention status
| Measures | Mothers |
Fathers |
||||||
|---|---|---|---|---|---|---|---|---|
| Intervention |
Control |
Intervention |
Control |
|||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
|
| ||||||||
| Observed family interaction | ||||||||
| Coparenting positivity aggregate | 0.06 | 0.64 | −0.07 | 0.58 | 0.08 | 0.64 | −0.10 | 0.52 |
| Coparenting withdrawal | 0.03 | 0.84 | −0.03 | 0.77 | −0.02 | 0.91 | 0.03 | 0.84 |
| Coparenting competition | −0.11 | 0.71 | 0.12 | 0.92 | −0.09 | 0.75 | 0.12 | 0.94 |
| Coparenting hostility | −0.06 | 0.62 | 0.08 | 1.01 | −0.07 | 0.54 | 0.09 | 0.95 |
| Overall triadic relationship quality | 0.13 | 0.92 | −0.17 | 0.89 | ||||
| Positive endorsement of partner parenting | 0.06 | 0.82 | −0.09 | 0.79 | 0.12 | 0.79 | −0.16 | 0.85 |
| Dyadic couple positive communication | −0.02 | 0.82 | 0.01 | 1.02 | −0.03 | 0.90 | 0.01 | 0.89 |
| Dyadic couple negative communication | 0.05 | 0.75 | −0.08 | 0.80 | 0.09 | 0.76 | −0.13 | 0.78 |
| Parenting positivity aggregate | 4.49 | 0.50 | 4.42 | 0.51 | 4.16 | 0.58 | 3.97 | 0.69 |
| Parenting negativity aggregate | 1.10 | 0.32 | 1.13 | 0.29 | 1.12 | 0.36 | 1.16 | 0.35 |
| Parent report of family relations and own adjustment | ||||||||
| Coparenting scale (total score) | 5.04 | 0.82 | 5.09 | 0.78 | 5.03 | 0.59 | 1.84 | 0.54 |
| Quality of Marriage Index | −0.11 | 0.97 | 0.13 | 0.83 | −0.03 | 0.94 | 0.08 | 0.84 |
| Depressive symptoms | 0.40 | 0.36 | 0.43 | 0.39 | 0.36 | 0.31 | 0.42 | 0.38 |
| Anxiety (STAIT) | 17.54 | 5.08 | 17.79 | 5.70 | 16.83 | 4.52 | 17.62 | 5.4 |
| Anxiety (Penn State Worry Questionnaire) | 13.73 | 5.57 | 15.16 | 6.72 | 10.89 | 4.50 | 11.68 | 5.75 |
| Parenting Stress Index—abbreviated | 1.80 | 0.46 | 1.81 | 0.58 | 1.73 | 0.45 | 1.85 | 0.51 |
| Parent report of family violence | ||||||||
| Interparent psychological violence | 10.57 | 13.83 | 12.89 | 14.45 | 9.97 | 13.23 | 10.94 | 13.07 |
| Interparent physical violence | 0.92 | 3.51 | 1.58 | 6.58 | 0.50 | 3.29 | 1.21 | 5.50 |
| Parent-child psychological violence | 1.22 | 2.97 | 2.09 | 5.65 | 1.39 | 3.36 | 2.56 | 6.15 |
| Parent-child physical violence | 0.87 | 2.34 | 2.23 | 8.11 | 1.40 | 4.98 | 2.43 | 6.34 |
| Child outcomes (parent report) | ||||||||
| Soothability | 5.52 | 0.86 | 5.29 | 0.95 | 5.13 | 0.88 | 4.97 | 1.08 |
| Duration of orienting | 3.59 | 1.10 | 3.45 | 1.12 | 3.26 | 1.09 | 2.98 | 1.11 |
| Number of night wakings | 1.07 | 1.23 | 1.35 | 1.38 | ||||
| Difficulty going back to sleep | 1.61 | 0.88 | 1.79 | 1.11 | ||||
| Hours child sleeps at night | 10.15 | 1.46 | 10.02 | 2.03 | ||||
Table 2.
Intervention condition main effect regression coefficients (from multilevel regression models on data for both parents, except where mother-only report)
| Outcome measures (posttest) | Coefficient (b) | SE | Effect size/IRR |
|---|---|---|---|
|
| |||
| Observed family interaction | |||
| Coparenting positivity aggregate | 0.20** | 0.07 | 0.47 |
| Coparenting withdrawal | 0.02 | 0.08 | |
| Coparenting competition | −0.22** | 0.08 | 0.37 |
| Coparenting hostility | −0.13 | 0.08 | 0.22 |
| Overall triadic relationship quality | 0.33** | 0.11 | 0.37 |
| Positive endorsement of partner parenting | 0.23** | 0.08 | 0.34 |
| Dyadic couple positive communication | 0.20* | 0.09 | 0.38 |
| Dyadic couple negative communication | −0.10 | 0.08 | |
| Parenting positivity aggregate | 0.22** | 0.07 | 0.41 |
| Parenting negativity aggregate | −0.04 | 0.06 | |
| Parenting autonomy aggregate | −0.17* | 0.07 | 0.26 |
| Parent report of family relations and own adjustment | |||
| Coparenting scale (total score) | −0.03 | 0.07 | |
| Quality of Marriage Index | −0.22** | 0.08 | −0.27 |
| Depressive symptoms | −0.06* | 0.03 | 0.20 |
| Anxiety (STAIT) | −0.73 | 0.40 | |
| Anxiety (Penn State Worry Questionnaire) | −1.34** | 0.41 | 0.29 |
| Parenting Stress Index—abbreviated | −0.08 | 0.05 | |
| Parent report of family violence | |||
| Interparent psychological violence | −0.23 | 0.14 | 0.79 |
| Interparent physical violence | −0.84** | 0.32 | 0.43 |
| Parent-child psychological violence | −0.27* | 0.13 | 0.76 |
| Parent-child physical violence | −0.49** | 0.16 | 0.62 |
| Child outcomes (parent report) | |||
| Soothability | 0.19* | 0.08 | 0.21 |
| Duration of orienting | 0.22* | 0.11 | 0.20 |
| Number of night wakings | −0.02* | 0.01 | 0.27 |
| Difficulty going back to sleep | −0.24* | 0.12 | 0.23 |
| Hours child sleeps during night | 0.01 | 0.17 | |
All models include controls for site location and pretest characteristics of informant, family income, economic strain, parent age, and social desirability. Models for coparenting and observed dyadic variables include a control for pretest couple efficacy. Child sleep variables include a control for child age. Multilevel models were used if data available from each parent. Effect sizes are Cohen’s d (model-adjusted standardized group mean differences) except for family violence variables, which are count variables; for family violence, multilevel negative binomial regression models were used and IRRs given for effect size
IRR incidence rate ratio
p < 0.05
p < 0.01
Main Effects
For observed family interaction, we found main effects of intervention status on most variables with generally moderate to strong effect sizes. In all cases, the intervention condition demonstrated more positive or less negative behaviors (Table 2). In the coparenting domain, this included observed positivity (b = 0.20; p < 0.01), competition (b = −0.22; p < 0.01), endorsement of partner’s parenting (b = 0.23; p < 0.01), and observed overall triadic relationship quality (b = 0.33; p < 0.01). In the parenting domain, intervention parents displayed more positivity (b = 0.22; p < 0.01) and lower levels of autonomy (b = −0.17; p < 0.05). In separate observation of the dyad, intervention parents demonstrated more positive communication (b = 0.20; p < 0.05). For a few of the observed family interaction variables for which we did not find significant main effects, such as coparenting withdrawal and parenting negativity, there were low average scores (Table 1), leading to difficulty in establishing program impact. In addition, coparenting hostility was lower in the intervention group but at a marginally non-significant level (p < 0.10).
For parent-report variables, we also found beneficial intervention effects for the majority of variables. This included intervention impact on self-reported levels of worry (b = −1.34; p < 0.01), depression (b = −0.06; p < 0.05), child soothability (b = 0.19; p < 0.05), child duration of orientation (b = 0.22; p < 0.05), number of child wakings during the night (b = −0.02; p < 0.05), and difficulty in child falling back to sleep (b = −0.24; p < 0.05). In contrast to the observed data findings, there was not a significant main effect for self-reported coparenting. Main effects also were not found in analyses of satisfaction with division of labor or amount of time child sleeps during the night. One main effect was found in a direction counter to other results; self-reported relationship satisfaction was significantly lower among intervention couples (b = −0.22; p < 0.01).
We found evidence of significant intervention impact with large effect sizes for three of the four violence outcomes. Intervention participants indicated significantly lower levels of physical IPV (b = −0.84; p < 0.01) and psychological (b = −0.27; p < 0.05) and physical PCV (b = −0.49; p < 0.01). Psychological IPV demonstrated a similar pattern but with a marginally non-significant finding.
Moderated Intervention Effects
We assessed whether the intervention was effective for subgroups of families based on prenatal risk, parent negative communication and depression. (For testing the moderated effect on child sleep outcomes—reported on only by mothers—we used mother’s prenatal depression and averaged across parents for negative communication.) Full results are available in the Appendix. In Table 3, we present results for the eight outcomes that did not show main intervention effects. For seven of the eight, evidence of moderated intervention impact (i.e., a significant interaction term) was found for at least one moderator. We carried out post hoc probes of moderator by condition interaction terms with postestimation tests of linear combinations of the component interaction terms controlling for other model covariates (Wald tests determined whether linear combinations were significantly different from zero). For negative communication as the moderator, we found a similar pattern of findings for observed parenting negativity (b = −0.35; p < 0.01), parenting stress (b = −0.14; p < 0.05), and nighttime sleep duration (b = 0.71; p < 0.01), the intervention reduced or eliminated an association in the control group between pretest risk and the outcome. For parent depression as the moderator, there was a buffering effect of the intervention for observed coparenting withdrawal (b = −0.47; p < 0.05), observed negative communication within the couple (b = −0.47; p < 0.05), anxiety (b = −2.10; p < 0.05), and self-reported coparenting (b = 0.35; p < 0.05). Figure 2 provides an illustrative example of the interaction effects we detected, in this case for preintervention levels of conflict moderating the intervention effect on observed negative parenting styles at posttest. We note that other interaction effects demonstrated similar patterns as that shown in this figure.
Table 3.
Regression coefficients and standard errors for moderated intervention effects
| Intervention condition X pretest negative communication | ||||||
| Negative communication | Condition | Negative communication X condition | ||||
| Outcome measures (posttest) | Coefficient | SE | Coefficient | SE | Coefficient | SE |
| Observed parenting negativity | 0.33 | 0.06 | −0.05 | 0.07 | −0.35** | 0.08 |
| Parenting stress index | 0.12** | 0.04 | −0.07 | 0.05 | −0.14* | 0.06 |
| Hours child sleeps during night | −0.65** | 0.16 | 0.02 | 0.16 | 0.71** | 0.22 |
| Intervention condition X pretest depression | ||||||
| Depression | Condition | Depression X condition | ||||
| Outcome measures (posttest) | Coefficient | SE | Coefficient | SE | Coefficient | SE |
| Observed coparenting withdrawal | 0.31 | 0.19 | 0.00 | 0.11 | −0.47* | 0.23 |
| Observed couple negative communication | 0.54** | 0.19 | 0.10 | 0.12 | −0.47* | 0.21 |
| Coparenting scale | −0.51** | 0.17 | −0.04 | 0.07 | 0.35* | 0.16 |
| Anxiety (STAIT) | 4.10** | 1.00 | −0.74 | 0.39 | −2.10* | 1.06 |
All models include controls for pretest family income, pretest economic strain, pretest parent age, pretest social desirability, and site location. Coparenting and observed dyadic variables contain an additional control for pretest couple efficacy. Multilevel models were used for all reported results
p < 0.05
p < 0.01
Fig. 2.
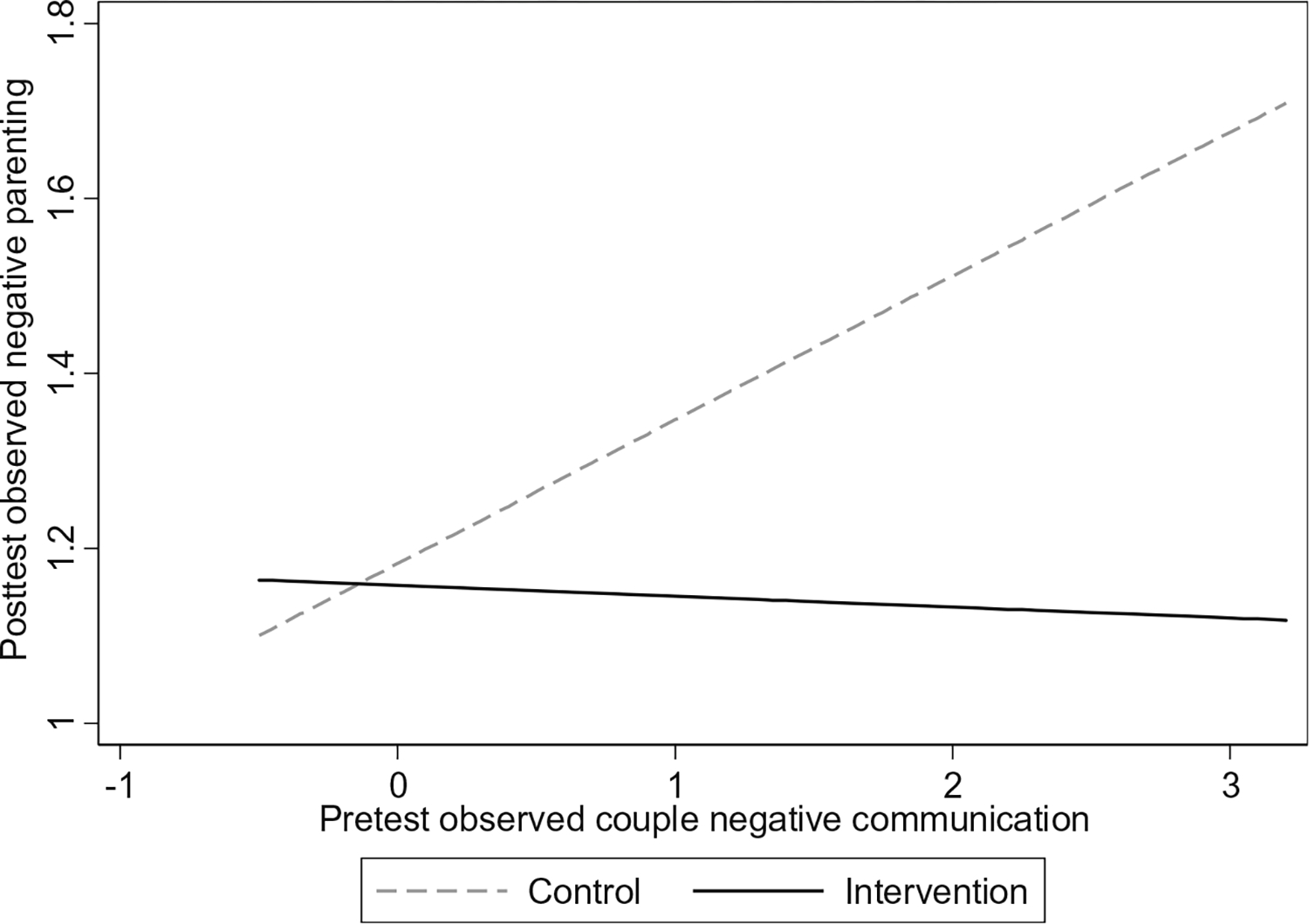
Moderation of pretest observed negative couple communication by intervention on posttest observed negative parenting
Discussion
The transition to parenthood is stressful for the majority of families, and the strains of this period are linked to parent and family relationship dysfunction (Doss et al. 2009; Perren et al. 2005). However, success in supporting families making the transition has been limited in the past to strategies focusing on the highest-risk families (Olds 2006). Prior work focused beyond the highest-risk families has resulted in null results, small effects, and mixed findings (Halford et al. 2010; Pinquart and Teubert 2010; Wood et al. 2012). We developed FF as a universal program with a strategic target on the coparenting relationship and with a strategic delivery approach through an existing universal, non-stigmatizing framework. With this replication of the first trial of FF, we are closer to being able to support the successful transition of all families across the great divide of parenthood.
As in the first trial of FF (Feinberg et al. 2010; Feinberg et al. 2009; Soli et al. 2010), we found significant positive impact across all domains of outcomes examined, parent mental health and adjustment, coparenting and couple relations, parenting quality, family violence, and early indicators of child self-regulation (soothability, attention, sleep). Several factors bolster the validity of these findings. First, effects were found by both parent self-report and observational methods. Second, in contrast to the first trial, in which two hospital sites were located close to the investigative team, this trial was implemented across five hospital sites; only one of which was in close proximity to the research team. Although we provided in-person training to all facilitators and follow-up supervision remotely by telephone, the greater number of sites and their distance increased the independence of local implementation and made this trial closer to an effectiveness trial than the first efficacy trial.
The magnitude of effects between the first trial and this second one are comparable, although in some cases—particularly for parent depression—the effect size in the first trial (0.56) was larger. However, in the first trial, the effect size for depression is for mothers only, as mother and fathers showed significantly different results, and there was no significant effect for fathers. Here, the effect size of d = 0.20 reflects an effect for both parents as there was no significant difference between mothers and fathers.
Relatively large effects were found for reductions in family violence, an outcome not measured in the first trial. It is difficult to translate effect sizes for continuous scaled variables into practical terms, but the family violence measures were collected as counts of violent incidents over the past year and are thus easier to interpret. For IPV and parent-to-child violence, there were roughly half as many incidents reported for intervention families as for control families. For psychological aggression, both between parents and from parents to children, there were roughly one quarter as many incidents in the intervention as in the control condition. Given that FF does not target family violence per se, but rather aims to reduce risk factors for violence (e.g., parent stress and depression, couple conflict, harsh parenting), these findings may indicate that the program has a cumulative impact on family violence through a range of intermediate targets. Future mediational analyses may help clarify the pathways to such effects.
Although we found significant impact on most outcomes, eight hypothesized outcome measures did not demonstrate overall program impact. The relatively well-educated and high-functioning nature of the sample may have reduced the potential for finding overall preventive intervention impact. Thus, we followed up with moderator analyses to examine whether higher-risk couples experienced positive benefits from the program on those outcomes. We found that either or both prenatal depression and couple conflict moderated program impact for seven of the eight variables. These results indicate that in most cases, where there was no overall program impact, there were benefits for families at higher levels of prenatal risk (as depicted in Fig. 2). These moderation results can also be interpreted as a protective effect of the intervention. As depicted in Fig. 2, assignment to the intervention reduced or eliminated the association between the prenatal risk factor and outcome in the control group. Thus, in the example depicted by the figure, assignment to FF protected infants from negative parenting associated with prenatal risk.
Against the findings of positive benefits due to FF across all domains, we found one result of negative impact due to program assignment on self-reported relationship quality. If not a chance finding, it may be the case that the program increased couples’ expectations of relationship quality, by which they judged their own relationship quality. However, no other outcomes, including those for coparenting, manifested a negative result. Thus, we consider this likely to be a chance finding but will examine this outcome again in future follow-up work.
Future research should continue to follow this sample in order to determine the persistence of the effects over a longer period of time, as we have done in the first FF trial. Further, mediation analyses should examine the pathways through which intervention effects develop. In this regard, it is important for the field to look inside the “black box” of family process. Our global measures of family relationships, even our global coding of videotape observation, typically do not yield much information about the impact of interventions on family interaction patterns. Accordingly, we are pursuing dynamical system-inspired analysis of micro-coded family interaction data to more precisely understand the impact of preventive intervention on family interaction patterns, which may mediate longer-term changes in parent and youth well-being (Feinberg, M. E., Xia, M., Fosco, G., & Chow, S.: Family Foundations Effects on Couple Interaction Across the Transition to Parenthood, submitted).
Future research should also examine the cost-benefit equation for this universal preventive approach. Cost-benefit considerations demand that universal prevention approaches have modest costs, as the economic (and human) benefit per family is likely to be less than that achieved by programs targeting high-risk families who have a greater likelihood, by definition, of experiencing significant and costly problems. For example, across effective models of home visiting, costs per family are almost $5000, with economic benefits estimated to be slightly more than twice that figure (Aos et al. 2004; Karoly et al. 2005). For FF, we have estimated a per-family cost of $779 based on analysis of program costs in our first trial—although the per-family cost for later cohorts (after the initial costs of program setup are no longer necessary) was estimated at $566 (Jones et al. 2014). These estimates are consistent with the costs of other multisession family programs. Our estimate of the economic benefits of the program indicates that the benefits are equivalent to roughly three times the initial cost or five times the cost for later cohorts (Jones 2015).
Limitations
The relatively well-educated and high-functioning nature of the sample may have reduced the potential for finding preventive intervention impact. Although a strength of the study is the use of multiple sources of data, some bias in measurement may exist as we relied on self-report measures and videotaped observation data based on non-naturalistic task settings.
Conclusions
These findings replicate a prior smaller study of Family Foundations, indicating that the Family Foundations approach to supporting couples making the transition to parenthood can have impact for all families and especially for families at elevated prenatal risk. Against a background of null, small, and mixed findings for other programs focused on couples at the transition to parenthood, these replicated results indicate that it is possible to provide effective support for couples at the transition that has impact on a broad range of parent, child, and family well-being domains. Moreover, given the empirically supported theoretical framework that was developed as the basis for the design of the FF program (Feinberg 2002; Feinberg 2003), these results confirm that prevention success is based, at least in part, on the careful development of conceptual models regarding malleable risk and protective factors.
Acknowledgments
We appreciate the assistance of Mary Metzger, Stephanie Rogers, and Becky Law and the facilitators in implementing the program. This study was funded by a grant from the National Institute of Child Health and Development (HD058529), Mark Feinberg, PI.
Appendix 1
Observed Family Interaction Procedures
Family interaction was videotaped at both pretest and posttest. At pretest, expectant parents engaged in two couple relationship discussion tasks. In the first task, couples were asked to talk about their day or a concern on their mind not related to their relationship. Each partner took turns with 6 min as the focal talker and 6 min as the listener. For the second task, couples were asked to talk for 120 min about three problems in their relationship that they had rated highly from a list of desired changes; they were asked to discuss the conflict and if possible to problem solve. At posttest, the couples engaged in only the second conflict-focused discussion for 12 min.
At posttest, families engaged in two interactions as a triad. First, parents and the child engaged in 12 min of joint free play on the floor with a limited set of toys provided by the interviewer. Second, parents were asked to teach their child for 6 min to accomplish a set of tasks designed to be at the limit of most infants’ developmental capacity (e.g., rolling a ball back and forth with a parent, building a tower of blocks).
Parent-Report Questionnaire Measures
Coparenting quality as perceived by parents at posttest was represented through a total score on the Coparenting Relationship Scale (Feinberg et al. 2012). The overall score was calculated as the average of the following six subscales: coparental agreement, support, partner’s parenting, closeness while parenting, undermining, and exposure of the child to conflict (α = 0.85 for mothers, α = 0.83 for fathers). A total score from the Quality of Marriage Index (Norton 1983) provided a measure of relationship satisfaction. Using a Likert response scale with six items, parents were asked about their relationship in terms of stability, feeling of partnership, and overall happiness in the relationship (α = 0.96 for mothers and fathers). Items for this measure had slightly different scales; thus, we standardized (mean= 0) before combining.
Depressive symptoms was gauged by a total score from Center for Epidemiological Studies Depression Scale (Radloff 1977). Questions are asked regarding the respondent’s feelings and outlook within the past week (Radloff 1977). We used an abbreviated 14-item scale from the original 20-item version that was been highly correlated in prior research with the full scale. Items were rated using a four-level response scale ranging from rarely/none of the time to always/most of the time, covering issues such as degree of loneliness and whether people were perceived as unfriendly (α = 0.85 for mothers, α = 0.83 for fathers).
Anxiety was assessed using the 10-Item Trait Scale from the StateTrait Anxiety Inventory Scale (Spielberger et al. 1983). Questions cover topics such as how much the respondent feels nervous, pleasant, or content, with responses given on a four-item scale ranging from “almost never” to “almost always. ” The scale has good internal consistency (α = 0.90 for mothers, α = 0.88 for fathers). A measure of anxiety was utilized from an average of the seven items in the Penn State Worry Questionnaire, reduced from the original 16-item survey (Beck et al. 1995; Meyer et al. 1990) to seven items for this project (α = 0.94 for mothers and α = 0.93 for fathers). Questions covered assessment of the generality, excessiveness, and uncontrollability of worries. Responses were made on a five-point scale ranging from “not at all typical” to “very typical. ”
Parental efficacy was measured using a total score from the Being a Parent Scale (Gibaud-Wallston and Wandersman 1978; Pedersen et al. 1989) measured at posttest. The 10-item pretest version assesses expected capability of being a parent and potential stressors about the responsibility. Two items were dropped at posttest (α = 0.77 for mothers, α = 0.78 for fathers). To measure parenting stress at posttest, we used a total score on the Parenting Stress Index (Abidin 1995) abbreviated from 36 to 27 items for this study. Parents provided responses using a five-point Likert scale, indicating level of agreement with statements about issues such as perceived problems associated with caring for a child and overall satisfaction with parenthood (α = 0.91 for mothers and for fathers).
Measures of child soothability and duration of orientation were each derived from six items in the Infant Behavior Questionnaire (Gartstein and Rothbart 2003). Soothability was comprised of items regarding how well the infant responds to parental behaviors like holding or singing. Duration of orientation was assessed with items regarding how attentive the baby was to objects such as mobiles and books. Alphas for soothability and duration of orientation were 0.77 and 0.78 among mothers and 0.75 and 0.83 among fathers, respectively. Three outcomes representing child sleep characteristics were taken from the Child Sleep Questionnaire (Seifer et al. Jul 1996), reported at posttest by mothers only.
The revised Conflict Tactics Scale (CTS2) (Straus et al. 1996) provided measures of interpartner physical and psychological aggression behaviors in the past year reported by each parent. Both parents reported on the same behaviors twice, once as perpetrator and once as victim. We utilized the highest report by either parent to represent the score for each behavior (e.g., mother hit father; father yelled at mother). Physical assault consisted of eight items such as punching, arm twisting, or throwing something at the partner. Psychological aggression was comprised of four items such as name calling or insulting the partner. Parent-child physical and psychological aggression was reported by both parents using the Parent-Child Conflict Tactics Scale (Straus et al. 1998), adapted from the Conflict Tactics Scale. The physical violence total combined seven items including shaking, pinching, and spanking. Parent-child psychological aggression consisted of five items including screaming at the child, threatening to spank, or calling the child names. Response options involved ranges of amounts (e.g., this happened 4–10 times in the past year). We utilized the midpoint count of each range in order to create average scale scores.
Control variables used in all analytic models included basic demographics such as income, age, and marital status, reported by parents at baseline. In addition, a measure of economic strain was created from three items asking how much a respondent has had to reduce standard of living recently, inability to afford certain essentials, and difficulty living on current income (α = 0.69 for mothers and 0.65 for fathers) (Howe et al. 1995; Kessler et al. 1988). A measure of social desirability was included to control for potential bias in models for self-report outcomes. We derived this score from 13 items taken from the Marlowe-Crowne short form (Crowne and Marlow 1960; Marlow and Crowne 1961). Respondents were asked whether they endorsed items such as always being courteous and willingness to admit making a mistake (α = 0.64 for mothers and 0.65 for fathers). For coparenting and dyadic measures, a seven-item measure of pretest couple efficacy (Fincham and Bradbury 1987) was used to control for the couple’s ability to manage interpersonal conflict (α = 0.85 for mothers and 0.84 for fathers).
Appendix 2
Table 4.
Regression coefficients and standard errors for moderated intervention effects (full results where interactions were statistically significant)
| Intervention condition X pretest negative communication | ||||||
| Negative communication | Condition | Negative communication X condition | ||||
| Outcome measures (posttest) | Coefficient | SE | Coefficient | SE | Coefficient | SE |
| Observed parenting positivity | −0.37*** | 0.07 | 0.21** | 0.07 | 0.26** | 0.11 |
| Observed parenting negativity | 0.33 | 0.06 | −0.05 | 0.07 | −0.35*** | 0.08 |
| Depressive symptoms | 0.49*** | 0.49 | −0.06* | 0.03 | −0.08* | 0.04 |
| Parenting stress index | 0.12** | 0.04 | −0.07 | 0.05 | −0.14* | 0.06 |
| Difficulty child going back to sleep | 0.33* | 0.13 | −0.25* | 0.11 | −0.35* | 0.16 |
| Hours child sleeps during night | −0.65*** | 0.16 | 0.02 | 0.16 | 0.71** | 0.22 |
| Intervention condition X pretest depression | ||||||
| Depression | Condition | Depression X condition | ||||
| Outcome measures (posttest) | Coefficient | SE | Coefficient | SE | Coefficient | SE |
| Observed parenting positivity | −0.61*** | 0.18 | 0.22** | 0.07 | 0.58** | 0.21 |
| Observed coparenting withdrawal | 0.31 | 0.19 | 0.00 | 0.11 | −0.47* | 0.23 |
| Observed couple negative communication | 0.54** | 0.19 | 0.10 | 0.12 | −0.47* | 0.21 |
| Coparenting scale | −0.51*** | 0.17 | −0.04 | 0.07 | 0.35* | 0.16 |
| Anxiety (STAIT) | 4.10*** | 1.00 | −0.74 | 0.39 | −2.10* | 1.06 |
| Anxiety (Penn State Worry Questionnaire) | 4.85*** | 1.19 | −1.37*** | 0.40 | −3.41** | 1.29 |
All models include controls for pretest family income, pretest economic strain, pretest parent age, pretest social desirability, and site location. Coparenting and observed dyadic variables contain an additional control for pretest couple efficacy. Multilevel models were used for all reported results
p < 0.05
p < 0.01
p < 0.001
Footnotes
Conflict of interest Dr. Feinberg created Family Foundations and is the owner of a privatecompanythat disseminates the program. Dr. Feinberg’s company has been reviewed by the Institutional Review Board and the Conflict of Interest Committee at Pennsylvania State University for potential financial gain. The other authors declare no potential conflict of interest.
Compliance with Ethical Standards All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. The views expressed in this article are those of the authors and do not necessarily represent the views of NICHD or Penn State University.
Electronic supplementary material
The online version of this article (doi:10.1007/s11121-016-0674-z) contains supplementary material, which is available to authorized users.
References
- Abidin RR (1995). Parenting Stress Index (3rd ed.). Odessa: Psychological Assessment Resources. [Google Scholar]
- Aos S, Lieb R, Mayfield J, Miller M, & Pennucci A (2004). Benefits and Costs of Prevention and Early Intervention Programs for Youth. www.wsipp.wa.gov/pub.asp?docid=04-07-3901.
- Beck JG, Stanley MA, & Zebb BJ (1995). Psychometric properties of the Penn State Worry Questionnaire. Journal of Clinical Geropsychology, 1, 33–42. [Google Scholar]
- Beijers R, Jansen J, Riksen-Walraven M, & de Weerth C (2010). Maternal prenatal anxiety and stress predict infant illnesses and health complaints. Pediatrics, 126, e401–e409. [DOI] [PubMed] [Google Scholar]
- Britner PA, Marvin RS, & Pianta RC (2005). Development and preliminary validation of the caregiving behavior system: Association with child attachment classification in the pre-school strange situation. Attachment & Human Development, 7, 83–102. [DOI] [PubMed] [Google Scholar]
- Cowan CP, & Cowan PA (2000). When Partners Become Parents: the Big Life Change for Couples. Mahwah: Lawrence Erlbaum Associates, Inc., Publishers. [Google Scholar]
- Crowne DP, & Marlow D (1960). A new scale of social desirability independent of psychopathology. Journal of Consulting Psychology, 24, 349–354. [DOI] [PubMed] [Google Scholar]
- Doss BD, Rhoades GK, Stanley SM, & Markman HJ (2009). The effect of the transition to parenthood on relationship quality: an 8-year prospective study. Journal of Personality and Social Psychology, 96, 601–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durlak JA (2009). How to select, calculate, and interpret effect sizes. Journal of Pediatric Psychology, 34, 917–928. doi: 10.1093/jpepsy/jsp004. [DOI] [PubMed] [Google Scholar]
- Feinberg ME (2002). Coparenting and the transition to parenthood: a framework for prevention. Clinical Child & Family Psychology Review, 5, 173–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME (2003). The internal structure and ecological context of coparenting: a framework for research and intervention. Parenting: Science and Practice, 3, 95–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Kan ML, & Hetherington EM (2007). The longitudinal influence of coparenting conflict on parental negativity and adolescent maladjustment. Journal of Marriage and the Family, 69, 687–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Kan ML, & Goslin MC (2009). Enhancing coparenting, parenting, and child self-regulation: Effects of family foundations 1 year after birth. Prevention Science, 10, 276–285. doi: 10.1007/s11121-009-0142-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Jones DE, Kan ML, & Goslin MC (2010). Effects of family foundations on parents and children: 3.5 years after baseline. Journal of Family Psychology, 24, 532–542. [DOI] [PubMed] [Google Scholar]
- Feinberg ME, Brown LD, & Kan ML (2012). A multi-domain self-report measure of coparenting. Parenting, 12, 1–21. doi: 10.1080/15295192.2012.638870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Jones DE, Roettger ME, Solmeyer A, & Hostetler ML (2014). Long-term follow-up of a randomized trial of family foundations: Effects on children’s emotional, behavioral, and school adjustment. Journal of Family Psychology, 28, 821–831. doi: 10.1037/fam0000037. [DOI] [PubMed] [Google Scholar]
- Feinberg ME, Jones D, Roettger M, Hostetler M, Sakuma K, Paul I, & Ethrenthal D (2015a). Preventive effects on birth outcomes: Buffering impact of maternal stress, depression, & anxiety. Maternal and Child Health Journal. doi: 10.1007/s10995-015-1801-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Roettger M, Jones DE, Paul IM, & Kan ML (2015b). Effects of a psychosocial couple-based prevention program on adverse birth outcomes. Maternal and child health journal, 19, 102–111. doi: 10.1007/s10995-014-1500-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fincham FD, & Bradbury TN (1987). The assessment of marital quality: a reevaluation. Journal of Marriage & the Family, 49, 797–809. [Google Scholar]
- Gartstein MA, & Rothbart MK (2003). Studying infant temperament via the revised infant behavior questionnaire. Infant Behavior & Development, 26, 64–86. [Google Scholar]
- Gibaud-Wallston A, & Wandersman LP (1978). Development and Utility of the Parenting Sense of Competence Scale. Toronto: Paper presented at: Meetings of the American Psychological Association. [Google Scholar]
- Goldstein H (2011). Multilevel statistical models (Vol. 922). John Wiley & Sons. [Google Scholar]
- Graham JW (2012). Missing data: Analysis and design. Springer. [Google Scholar]
- Halford WK, Petch J, & Creedy D (2010). Promoting a positive transition to parenthood: a randomized clinical trial of couple relationship education. Prevention Science, 11, 89–100. [DOI] [PubMed] [Google Scholar]
- Heinicke CM (2002). The Transition to Parenting. Mahwah: Erlbaum. [Google Scholar]
- Howe GW, Caplan RD, Foster D, Lockshin M, & McGrath C (1995). When couples cope with job loss: a strategy for developing and testing preventive interventions. In Hurrell LRMJJ (Ed.), Job Stress Interventions (pp. 139–157). Washington: American Psychological Association. [Google Scholar]
- Ioannidis JPA (2005). Why most published research findings are false. PLoS Med, 2, e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DE (2015). Return on Investment from Family-Focused Prevention (Paper presented at Prevention Research Center, August 28, 2015. Penn State University). [Google Scholar]
- Jones DE, Feinberg ME, & Hostetler ML (2014). Costs to implement an effective transition-to-parenthood program for couples: Analysis of the Family Foundations program. Evaluation and Program Planning, 44, 59–67. doi: 10.1016/j.evalprogplan.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaczynski KJ, Lindahl KM, Malik NM, & Laurenceau J-P (2006). Marital conflict, maternal and paternal parenting, and child adjustment: A test of mediation and moderation. Journal of Family Psychology, 20, 199–208. [DOI] [PubMed] [Google Scholar]
- Kan ML, & Feinberg ME (2014). Can a family-focused, transition-to-parenthood program prevent parent and partner aggression among couples with young children? Violence and Victims, 29, 967–980. [DOI] [PubMed] [Google Scholar]
- Kan M, & Feinberg M (2015). Impacts of a coparenting-focused intervention on links between pre-birth intimate partner violence and observed parenting. Journal of Family Violence, 30, 363–372. doi: 10.1007/s10896-015-9678-x. [DOI] [Google Scholar]
- Karoly LA, Kilburn MR, & Cannon JS (2005). Early childhood interventions: Proven results, future promise (Vol. MG-341-PNC). Santa Monica: RAND Corporation. [Google Scholar]
- Karreman A, van Tuijl C, van Aken MAG, & Dekovic M (2008). Parenting, coparenting, and effortful control in preschoolers. Journal of Family Psychology, 22, 30–40. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Turner B, & House JS (1988). Effects of unemployment on health in a community survey: Main, modifying, mediating effects. Journal of Social Issues, 44, 69–86. [Google Scholar]
- Krishnakumar A, & Buehler C (2000). Interparental conflict and parenting behaviors: a meta-analytic review. Family Relations: Interdisciplinary Journal of Applied Family Studies, 49, 25–44. [Google Scholar]
- Lawrence E, Rothman AD, Cobb RJ, Rothman MT, & Bradbury TN (2008). Marital satisfaction across the transition to parenthood. Journal of Family Psychology, 22, 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipman EL, & Boyle MH (2008). Linking Poverty and Mental Health: a Lifespan View Ontario, Canada: The Provincial Centre of Excellence for Child and Youth Mental Health.
- Malik NM, & Lindahl KM (2004). System for coding interaction in dyads. In Kerig PK & Baucom DH (Eds.), Couple Observational Coding Systems. NJ: Lawrence Erlbaum. [Google Scholar]
- Margolin G, Gordis EB, & Oliver PH (2004).Links between marital and parent-child interactions: Moderating role of husband-to-wife aggression. Development and Psychopathology, 16, 753–771. [DOI] [PubMed] [Google Scholar]
- Markman H, Rhoades G, Stanley S, & Peterson K (2013). A randomized clinical trial of the effectiveness of premarital intervention: Moderators of divorce outcomes. Journal of Family Psychology, 27, 165–172. doi: 10.1037/a0031134. [DOI] [PubMed] [Google Scholar]
- Marlow D, & Crowne DP (1961). Social desirability and response to perceived situational demands. Journal of Consulting Psychology, 25, 109–115. [DOI] [PubMed] [Google Scholar]
- McCollum JA, & Ostrosky M (2008). Family roles in young children’s emerging peer related social competence. Social competence of young children, 31–59. [Google Scholar]
- McDonald S, Wall J, Forbes K, Kingston D, Kehler H, Vekved M, & Tough S (2012). Development of a prenatal psychosocial screening tool for post-partum depression and anxiety. Paediatric and Perinatal Epidemiology, 26, 316–327. [DOI] [PubMed] [Google Scholar]
- McHale JP, Kuersten-Hogan R, & Lauretti A (2001). Evaluating coparenting and family-level dynamics during infancy and early childhood: the coparenting and family rating system. In Kerig PK & Lindahl KM (Eds.), Family Observational Coding Systems: Resources for Systemic Research (pp. 151–170). Mahwah: Lawrence Erlbaum. [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the Penn State Worry Questionnaire. Behav Res Ther, 28, 488. [DOI] [PubMed] [Google Scholar]
- Norton R (1983). Measuring marital quality: a critical look at the dependent variable. Journal of Marriage and the Family, 45, 141–151. [Google Scholar]
- Olds DL (2006). The nurse–family partnership: an evidence-based preventive intervention. Infant Mental Health Journal, 27, 5–25. doi: 10.1002/imhj.20077. [DOI] [PubMed] [Google Scholar]
- Pedersen FA, Bryan Y, Huffman L, & Del Carmen R (1989). Constructions of self and offspring in the pregnancy and early infancy periods. Kansas City: Society for Research in Child Development. [Google Scholar]
- Perren S, von Wyl A, Burgin D, Simoni H, & von Klitzing K (2005). Depressive symptoms and psychosocial stress across the transition to parenthood: Associations with parental psychopathology and child difficulty. Journal of Psychosomatic Obstetrics & Gynecology, 26, 173–183. [DOI] [PubMed] [Google Scholar]
- Pinquart M, & Teubert D (2010). Effects of parenting education with expectant and new parents: a meta-analysis. Journal of Family Psychology, 24, 316–327. [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: a self-report depression scale for research in the general population. Applied psychological measurement, 1, 385–401. [Google Scholar]
- Sanders MR, & Morawska A (2006). Towards a public health approach to parenting. The Psychologist. Special Issue: Nipping criminality in the bud, 19, 476–479. [Google Scholar]
- Schoppe SJ, Mangelsdorf SC, & Frosch CA (2001). Coparenting, family process, and family structure: Implications for preschoolers’ externalizing behavior problems. Journal of Family Psychology, 15, 526–545. [DOI] [PubMed] [Google Scholar]
- Schulz MS, Cowan CP, & Cowan PA (2006). Promoting healthy beginnings: a randomized controlled trial of a preventive intervention to preserve marital quality during the transition to parenthood. Journal of Consulting and Clinical Psychology, 74, 20–31. [DOI] [PubMed] [Google Scholar]
- Segre LS, O’Hara MW, Arndt S, & Stuart S (2007). The prevalence of postpartum depression. Social Psychiatry and Psychiatric Epidemiology, 42, 316–321. [DOI] [PubMed] [Google Scholar]
- Seifer R, Sameroff AJ, Dickstein S, & Hayden LC (1996). Parental psychopathology and sleep variation in children. Child and Adolescent Psychiatric Clinics of North America, 5, 715–727. [Google Scholar]
- Shapiro AF, & Gottman JM (2005). Effects on marriage of a psycho-communicative-educational intervention with couples undergoing the transition to parenthood, evaluation at 1-year post intervention. Journal of Family Communication, 5, 1–24. [Google Scholar]
- Shonkoff JP (2010). Building a new biodevelopmental framework to guide the future of early childhood policy. Child Development, 81, 357–367. doi: 10.1111/j.1467-8624.2009.01399.x. [DOI] [PubMed] [Google Scholar]
- Slep AMS, & O’Leary SG (2005). Parent and partner violence in families with young children: Rates, patterns, and connections. Journal of Consulting and Clinical Psychology, 73, 435–444. [DOI] [PubMed] [Google Scholar]
- Soli AR, Feinberg ME, Jones DE, & Coffman D (2010). The Effects of Family Foundations on Coparenting and Child Adjustment: a Mediation Analysis. Denver: Poster presented at the Society for Prevention Research Annual Meeting. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, & Jacobs GA (1983). Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto: Consulting Psychologists Press. [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Clair S, & Feinberg M (2007). Substance-use outcomes at 18 months past baseline: the PROSPER Community-University Partnership Trial. American Journal of Preventive Medicine, 32, 395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus M, Hamby S, Boney-McCoy S, & Sugarman D (1996). The revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues, 283–316. [Google Scholar]
- Straus M, Hamby S, Finkelhor D, Moore DW, & Runyan D (1998). Identification of child maltreatment with the parent-child conflict tactics scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect, 22, 249–270. [DOI] [PubMed] [Google Scholar]
- Wood RG, Moore Q, Clarkwest A, Killewald A, & Monahan S (2012). The Long-Term Effects of Building Strong Families: a Relationship Skills Education Program for Unmarried Parents, Washington. DC: ACF, Office of Planning Research and Evaluation. [Google Scholar]
- Yuan Y (2011). Multiple imputation using SAS software. Journal of Statistical Software, 1–25. [Google Scholar]
- Zimet DM, & Jacob T (2001). Influences of marital conflict on child adjustment: Review of theory and research. Clinical Child & Family Psychology Review, 4, 319–335. [DOI] [PubMed] [Google Scholar]


