Abstract
Background and Objectives
There has been conflicting evidence regarding the association between seasonal changes and daylight saving time (DST) and sleep disorders. This topic is of particular interest currently because the United States and Canada are considering the elimination of seasonal clock changes. The aim of this study was to compare sleep symptoms among participants who were interviewed in different seasons and before/after the transition into DST and standard time (ST).
Methods
A total of 30,097 people aged 45–85 years taking part in the Canadian Longitudinal Study on Aging were studied. Participants completed a questionnaire on sleep duration, satisfaction, sleep-onset insomnia, sleep-maintenance insomnia, and hypersomnolence symptoms. Sleep disorders were compared between participants who were interviewed during different seasons and at different times of the year (DST/ST). Data were analyzed using χ2, analysis of variance, binary logistic, and linear regression tests.
Results
Among participants interviewed in different seasons, we found no difference in dissatisfaction with sleep, sleep onset, sleep maintenance, and hypersomnolence. Those interviewed in summer had slightly shorter sleep duration compared with those in winter (6.76 ± 1.2 vs 6.84 ± 1.3 hours). Participants interviewed 1 week before vs 1 week after DST transition showed no difference in sleep symptoms, except for a 9-minute decrease in sleep duration a week after transition. However, those who were interviewed a week after transition to ST compared with a week before reported more dissatisfaction with sleep (28% vs 22.6%, adjusted odds ratio [aOR] 1.34, 95% CI 1.02–1.76), higher sleep-onset insomnia (7.1% vs 3.3%, aOR 2.26, 95% CI 1.19–4.27), higher sleep-maintenance insomnia (12.9% vs 8.2%, aOR 1.64, 95% CI 1.02–2.66), and more hypersomnolence with adequate sleep (7.3% vs 3.6%, aOR 2.08, 95% CI 1.14–3.79).
Discussion
We found small seasonal variations in sleep duration but no difference in other sleep symptoms. The transition from DST to ST was associated with a transient increase in sleep disorders.
Sleep plays an essential role in maintaining good health, mood, cognition, job performance, and social activity. Physiologic processes that affect sleep behavior are influenced by the circadian rhythm. Circadian rhythms are roughly 24-hour physiologic cycles which are mediated by the suprachiasmatic nucleus of the hypothalamus and serve as the main driving force behind sleep-wake cycles. The circadian rhythm organizes several endogenous factors, such as core body temperature, releasing of melatonin and other hormones, and cell division.1,2 It also receives input from several exogenous factors, also known as zeitgebers, which include light exposure, ambient temperature, physical/mental activity, meals, etc.2-4
Of these exogenous influences, light exposure is one of the most important modulators of circadian rhythms. Because low core body temperature and the absence of light induce sleep, sleep may vary across seasons, with longer sleep durations documented in winter and shorter durations in summer.5 Light exposure early in the night delays the circadian phase while light exposure in the morning advances the phase, leading to earlier bedtimes and awakenings.3,6
When exogenous factors do not align with one's endogenous circadian rhythms, people experience circadian malalignment. Jet lag, night shifts, and the transitions between the daylight saving time (DST) and the standard time (ST) are common situations associated with circadian malalignment.7-9 Jet lag and the transitions between DST and ST cause temporary circadian malalignment as individuals eventually adapt to their new schedule.7,9 Nevertheless, such malalignment has been associated with sleep disruption, neurocognitive dysfunction, fatigue, sleepiness, and decreased mood. For example, it has been estimated that sleep problems also account for roughly 13% of workplace injuries.10 According to the American Sleep Society, drowsy driving results in over 1,500 deaths and 40,000 injuries each year in the United States alone.11 Some studies suggest possible chronic effects on negative health and performance outcomes,7,9 metabolic dysfunction (i.e., diabetes, obesity, proinflammatory states),12 cardiovascular disease, and increased mortality.13
The transitions to and from DST have been associated with higher rates of car accidents14 as well as an increased risk of stroke and hospital visits,15,16 myocardial infarction,17,18 and general accidents.16 In a recent survey conducted by the American Academy of Sleep Medicine, respondents were most likely to use the “extra hour” gained in the Fall, during the transition to ST, to catch up on sleep.19 Is this increased sleep duration responsible for these negative outcomes? Are sleep disturbances different when transitioning to DST in spring as compared with ST in the Fall?
To shed some light on these questions, we conducted a cross-sectional study using data collected as part of the Canadian Longitudinal Study on Aging (CLSA). Specifically, the goal of this study was to (1) assess whether participants reported seasonal variations in sleep satisfaction, quantity, and sleep disorders and (2) determine whether transitions in and out of DST/ST were associated with different levels of sleep disturbances. Because the United States and Canada have recently begun to discuss the possibility of removing the time changes indefinitely, this topic has taken on an even greater significance.
Methods
Study Population
The CLSA is a comprehensive nationwide study in Canada, involving 30,097 participants aged 45–85 years, who were randomly selected from 7 provinces (recruitment methods are described elsewhere). Data were collected through a combination of in-home visits, on-site visits, and telephone interviews. This analysis focuses on the baseline data gathered between 2011 and 2015.20
Standard Protocol Approvals, Registrations, and Patient Consents
The CLSA protocol received approval from 13 research ethics boards across Canada.21 All participants provided their informed consent before participation.20
Measurements of Sleep Symptoms
At baseline, participants were questioned about their sleep satisfaction, number of hours they slept per day, the presence of sleep-onset and maintenance insomnia disorders, and the presence of hypersomnolence disorder. These questions were based on the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Details of the questionnaires can be found in our previous study22 and in the eMethods (links.lww.com/WNL/C788).
Sleep pattern dissatisfaction was determined by the question “How satisfied or dissatisfied are you with your current sleep pattern?”23 recorded on a 5-point Likert scale. Participants were then divided into 2 categories: dissatisfied (those answering “very dissatisfied” or “dissatisfied”) vs not dissatisfied (those answering “neutral,” “satisfied,” or “very satisfied”).
Number of hours of actual nighttime sleep in the past month (numeric variable).
Difficulty initiating sleep was queried as “Over the last month, how often did it take you more than 30 minutes to fall asleep?”24 Those reporting this symptom ≥3 nights per week were considered to have difficulty initiating sleep. Sleep-onset insomnia disorder was defined as sleep dissatisfaction, along with difficulty initiating sleep ≥3 nights per week that moderately or severely affected their function and lasted ≥3 months. Note that to accurately assess the acute changes in sleep after the transition to DST/ST, we excluded “duration ≥3 months” from all criteria of sleep disorders (i.e., sleep-onset insomnia, sleep-maintenance insomnia, and hypersomnolence disorders) for comparisons before vs after the transition to DST/ST.
Difficulty maintaining sleep was assessed by asking “Over the last month, how often did you wake in the middle of the night or too early in the morning and found it difficult to fall asleep again?”24 Participants who reported this ≥3 nights per week were considered to have symptoms of sleep-maintenance insomnia. Sleep-maintenance insomnia disorder was defined as dissatisfaction with the sleep pattern and difficulty maintaining sleep for a minimum of 3 nights per week that moderately or severely affected the participant's ability to function and lasted ≥3 months.
Difficulty staying awake was queried as “Over the last month, how often do you find it difficult to stay awake during your normal waking hours when you want to?”24 Participants who reported this happening at least 3 times per week were considered to have symptoms of excessive sleepiness. Hypersomnolence with adequate sleep was defined as this difficulty staying awake for ≥3 days per week despite reporting at least 7 hours of sleep, lasting ≥3 months (owing to a low number of participants reporting dysfunction from difficulty staying awake, the requirement of dysfunction was not included in the definition of this disorder). In this study, hypersomnolence disorder was termed “hypersomnolence with adequate sleep” to avoid confusion with standard definitions of hypersomnolence disorder.
Date of Interview
The sleep module of CLSA was evaluated as part of the in-home interview, and the interview date was recorded. We correlated each interview date with the season during which it was conducted.
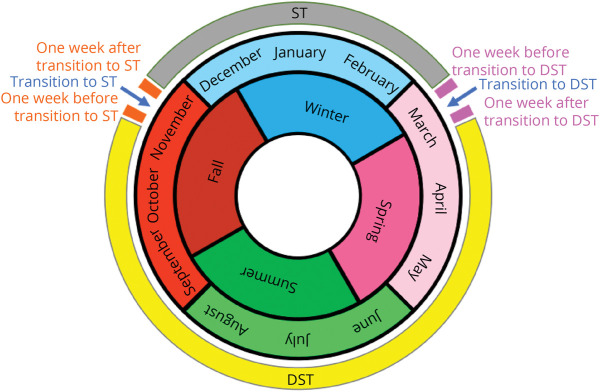
Similarly, according to the National Research Council, the second Sunday in March marks the beginning of DST (clocks turn forward by 1 hour) and the first Sunday of November marks the beginning of ST (clocks turn backward by 1 hour).25 We analyzed 6 time periods: (1) 1 week before transition to DST, (2) 1 week after transition to DST, (3) established DST, (4) 1 week before transition to ST, (5) 1 week after transition to ST, and (6) established ST (Figure). The exact dates of these transitions are presented in eTable 1 (links.lww.com/WNL/C788).
Figure. Schematic Diagram of Time Periods.
One week before transition to daylight saving time (DST), 1 week after transition to DST, getting used to DST, 1 week before transition to standard time (ST), 1 week after transition to ST, and getting used to ST.
To examine the seasonal variation of sleep disorders and the association between time zone and sleep disorders, we compared sleep variables among participants who were interviewed during different seasons and time zones. Primary and secondary objectives are as follows:
Comparison of sleep disorders among participants who were interviewed in different seasons;
Comparison of sleep disorders among participants interviewed during 1 week before vs 1 week after transition to DST; and
Comparison of sleep disorders among participants interviewed during 1 week before vs 1 week after transition to ST.
Further sensitivity and secondary analyses are presented in eResults (eTables 2–6, links.lww.com/WNL/C788).
Statistical Analysis
Statistical analysis was conducted using SPSS version 24. Descriptive results were presented as mean and standard deviation for continuous variables and frequency for categorical variables.
To compare sleep symptoms in the 4 seasons, we used the χ2 test for categorical variables and the analysis of variance test for continuous variables.
Binary logistic regression and linear regression were used to compare sleep symptoms and sleep duration between participants interviewed 1 week before vs after DST, before vs after ST, and DST vs ST, adjusting for age, sex, and province. The odds ratio and 95% CI are presented in tables.
Data Availability
Data are available from the CLSA webpage (clsa-elcv.ca) for researchers who meet the criteria for access to deidentified CLSA data.
Furthermore, the opinions expressed in this article are of the author's own and do not reflect the views of the CLSA.
Results
Seasonal Variation
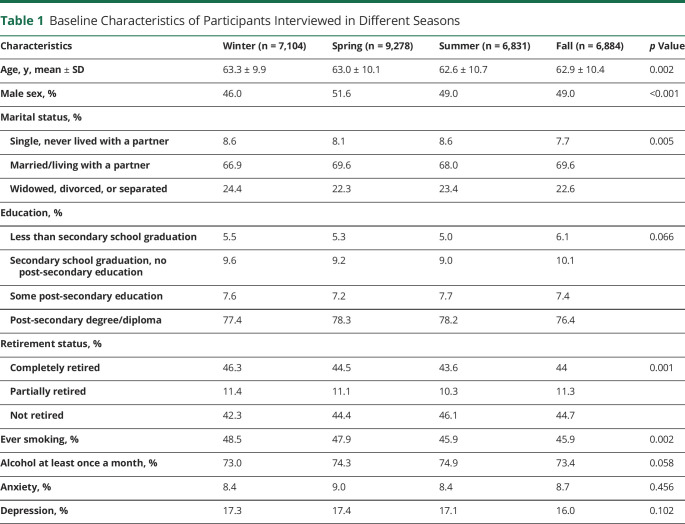
Among the 30,097 included participants, 7,104 were interviewed during winter (46% male, average age ± SD: 63.3 ± 9.9 years), 9,278 during spring (51.6% male, age: 63.0 ± 10.1 years), 6,831 during summer (49% male, age: 62.6 ± 10.7 years), and 6,884 during Fall (49% male, age: 62.9 ± 10.4 years). Further baseline characteristics are reported in Table 1.
Table 1.
Baseline Characteristics of Participants Interviewed in Different Seasons
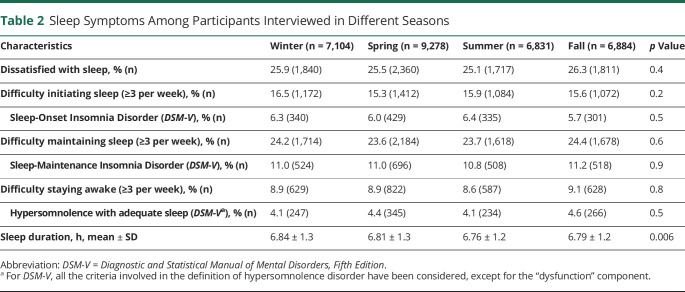
We found no difference between dissatisfaction with sleep, difficulty initiating sleep, difficulty maintaining sleep, and difficulty staying awake during the day among participants who were interviewed in different seasons. We found a modest difference in sleep duration; participants who were interviewed in summer had the shortest sleep durations (6.76 ± 1.2 hours) while those who were interviewed in winter reported the longest sleep durations (6.84 ± 1.3 hours). See Table 2 for details.
Table 2.
Sleep Symptoms Among Participants Interviewed in Different Seasons
One Week Before vs One Week After Transition to DST
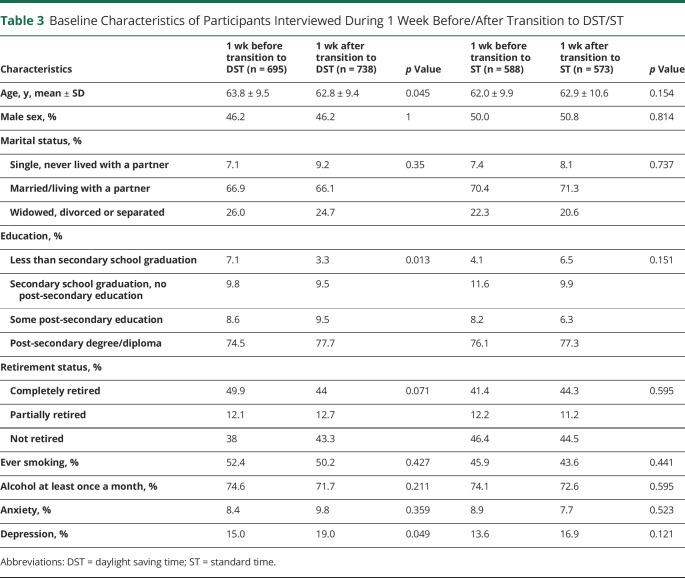
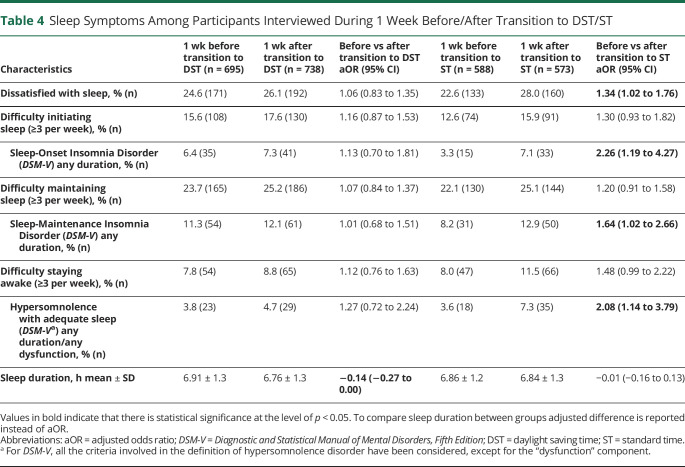
Comparing the 695 participants who were interviewed a week before transition to DST and 738 interviewed a week after transition, no sex difference was observed, but a 1-year age difference was noted (63.8 ± 9.5 vs 62.8 ± 9.4) (Table 3). Sleep-onset and maintenance insomnia disorders and hypersomnolence with adequate sleep were similar between the 2 groups. Those who were interviewed a week before transition to DST reported 9-minute longer sleep duration than those who were interviewed a week after transition (6.91 ± 1.3 vs 6.76 ± 1.3, adjusted difference −0.14, 95% CI −0.27 to 0.00) (Table 4 and eTable 2, links.lww.com/WNL/C788).
Table 3.
Baseline Characteristics of Participants Interviewed During 1 Week Before/After Transition to DST/ST
Table 4.
Sleep Symptoms Among Participants Interviewed During 1 Week Before/After Transition to DST/ST
One Week Before vs One Week After Transition to ST
A total of 588 participants were interviewed a week before transition, and 573 were interviewed a week after transition to ST. No age or sex difference was observed between these groups (Table 3). Unlike the DST findings, those who were interviewed a week after transition to ST reported more dissatisfaction with sleep (28% vs 22.6%, adjusted odds ratio [aOR] 1.34, 95% CI 1.02–1.76), higher sleep-onset insomnia (7.1% vs 3.3%, aOR 2.26, 95% CI 1.19–4.27), higher sleep-maintenance insomnia (12.9% vs 8.2%, aOR 1.64, 95% CI 1.02–2.66), and more hypersomnolence with adequate sleep (7.3% vs 3.6%, aOR 2.08, 95% CI 1.14–3.79) (Table 4 and eTable 2, links.lww.com/WNL/C788). This increase in sleep disturbances was transient; all symptoms were no longer increased in those interviewed 1 week later (i.e., 2 weeks after transition) (eTable 3).
Discussion
We conducted a cross-sectional study, using data collected from a cohort of middle-aged and older participants across Canada (i.e., the CLSA) between 2011 and 2015 to determine whether sleep symptoms varied by season and during transitions in and out of DST/ST. We found only modest differences in sleep duration by season. Although transition to DST was not associated with reported sleep disruption, the transition back to ST was associated with several sleep disorder symptoms.
We found that people reported somewhat longer sleep during winter and shorter sleep during summer, although there were no seasonal variations in sleep dissatisfaction, difficulty initiating sleep, difficulty maintaining sleep, nor difficulty staying awake during the day. These findings are consistent with some previous studies that found seasonal variations in sleep duration,26,27 although current evidence remains quite mixed. For example, a recent publication supported a shorter sleep duration in spring relative to winter, while some other studies had found no seasonal differences.5,28,29 One hypothesis for these discrepancies pertains to the varying measures used to assess sleep across these studies. Some used self-reported data while others used more objective measures such as wearable devices. Furthermore, the previously cited studies took place in different countries, which differ in their seasonal zeitgeber variations, including the timing of light exposure. Of note, seasonal variations in light are high in Canada compared with many other countries. Even with these large differences, we found only small seasonal variations in sleep duration.26
Regarding sleep disorders, some studies have also found no difference in sleep problems across the seasons.30,31 In other studies, winter has been linked with increased reports of sleep disorders30 and decreased early awakenings,32 and some studies found less disturbed sleep in spring.32 These studies vary widely in their methodology, population, and setting, which may also account for the mixed nature of the evidence. Of note, many factors that can greatly influence sleep disorders tend to remain constant throughout the year (e.g., sleep hygiene habits, other disorders that may be causing the sleep disorders, medications), perhaps explaining the absence of differences seen in our study.
Relative to 1 week before transition from ST to DST, the prevalence of sleep-onset insomnia, sleep-maintenance insomnia, and hypersomnolence with adequate sleep was similar when assessed 1 week after transition. However, when looking at the transition from DST to ST, participants reported being more dissatisfied with sleep, having higher sleep-onset and sleep-maintenance insomnia, and having more hypersomnolence with adequate sleep 1 week after transition. These findings are partly unexpected because it is during the transition from DST to ST that there is an “extra hour” of sleep.
In a study of 469 teenagers in Germany, transition to DST was associated with higher daytime sleepiness until the third week after the transition. This effect was more prominent in older students who were evening-type individuals.33 According to a UK study on 120 young participants, sleep latency and efficiency deteriorated during the week after the transition to ST.34 In another study conducted on 10 individuals using wrist-worn accelerometers during sleep, the transition to DST between 2003 and 2004 resulted in a 60-minute shortening of sleep duration and a 10% reduction in sleep efficiency.35 In another study during 1983–2006 on the National Institute of Occupational Safety and Health, workers slept 40 minutes less on Mondays after the transition to DST and faced higher levels of injuries, but no significant changes were observed in sleep or injury on Mondays after the transition to ST.36 From the shift work literature, it is well-documented that phase advancing (i.e., transitioning to DST) is typically harder and associated with more disturbances in sleep and alertness, than phase delay (i.e., transitioning to ST).3,4 These results are unlikely to simply be due to seasonal variations in sleep disorders because we did not find any evidence of seasonal variations in this sample.
One explanation for these findings may be the differences in the available light required for adjustment. When looking at light exposure in Montreal, for example, the day before the transition from ST to DST, sunrise occurs at roughly 6 am while sunset occurs around 6 pm. After the transition, sunrise occurs at 7 am and sunset occurs around 7 pm.37 The opportunity for natural morning light exposure, which facilitates phase advancing,3 is thus still available after the transition. Conversely, when people in Montreal must transition from DST to ST, they would benefit from evening/nighttime light exposure and morning light avoidance to facilitate their circadian phase delay.3,38 However, natural light exposure occurs roughly from 8 am to 6 pm before the transition and from 7 am to 5 pm after the transition.39 This timing of light exposure could, therefore, make it harder for circadian rhythms to phase delay. Relative to the transition from ST to DST, shifting from DST to ST may result in slower circadian adaptation (i.e., prolonged circadian misalignment) and thus explain the transiently higher reports in sleep disorders that we found.
Finally, it is important to note the relative transience of the sleep disruptions that we observed after the shift to ST.3,40 Any increase in sleep disturbance was no longer evident only 1 week later (i.e., 2 weeks after transition). This suggests that, as disruptive as these transitions may feel in the short term, there may be less long-term chronic sleep implications of the repeated switch back and forth from DST to ST.
Some limitations should be noted. This is a cross-sectional study using self-reported measures—we cannot establish any causal links. Self-report may be subject to expectation biases or to general mood effects (e.g., shift to ST is associated with the onset of an often-difficult Canadian winter). In addition, although our participant groups were similar in their demographics, this remains a between-group design, and thus, we cannot conclude with certainty that the higher frequencies of sleep disorders reported 1 week after the transition to ST were directly due to the transition. Future studies with repeated individual assessment, with correlation with objective sleep measures, and including those living in areas with different light/seasonal changes would be of considerable interest. Our sample only includes middle-aged/older adults; the results may have been different if younger individuals had been included in the sample. In addition, even within the same time zone, sunset and sunrise differ according to the meridian. However, we attempted to reduce the confounding effect of this variable by adjusting for provinces. For future studies, it would be helpful to evaluate the consequences of transitioning from ST to DST and vice versa on possible accidents, sick leave, and cognitive impairments. Another weakness of the study is the lack of information on the specific temperature and precipitation on the days that the questionnaires were administered. However, because the study was conducted over a period of 3 years with participants randomly selected from 9 cities in a very large country, it is considered unlikely that local weather patterns may have a significant effect on the results. Efforts were made to account for any residual confounding factors by adjusting for the participant's province, which could account for differences in latitude and climate patterns.
On the other hand, this study has many strengths. First, it has a large sample size and, therefore, allows for more precise estimates. Second, it is one of the few studies to assess the seasonality of a wide range of sleep parameters and sleep disorders as well as their relation to DST and ST transitions.
Our findings suggest that there may be small seasonal variations in sleep duration, without any difference in insomnia or somnolence prevalence. In addition, the transition from DST to ST is associated with a transient increase in self-reported sleep disruption.
Acknowledgment
This research was made possible using the data/biospecimens collected by the Canadian Longitudinal Study on Aging (CLSA). This research has been conducted using the CLSA Baseline Comprehensive Dataset version 5.1, under Application Number 1906008. The CLSA is led by Drs. Parminder Raina, Christina Wolfson, and Susan Kirkland.
Glossary
- aOR
adjusted odds ratio
- CLSA
Canadian Longitudinal Study on Aging
- DST
daylight saving time
- ST
standard time
Appendix. Authors
Footnotes
Infographic links.lww.com/WNL/C863
CME Course: NPub.org/cmelist
Study Funding
Funding for the Canadian Longitudinal Study on Aging (CLSA) is provided by the Government of Canada through the Canadian Institutes of Health Research (CIHR) under grant reference: LSA 94473, and the Canada Foundation for Innovation, as well as the following provinces: Newfoundland, Nova Scotia, Quebec, Ontario, Manitoba, Alberta, and British Columbia.
Disclosure
S. Zolfaghari, M. Cyr, and A. Pelletier have nothing to disclose. R.B. Postuma reports grants and personal fees from the Fonds de Recherche du Québec–Santé, grants from the Canadian Institutes of Health Research, grants from the Parkinson Society of Canada, grants from Weston-Garfield Foundation, grants from Michael J. Fox Foundation, grants from Webster Foundation, grants from the National Institutes of Health, personal fees from Takeda, personal fees from Roche/Prothena, personal fees from Teva Neurosciences, personal fees from Novartis Canada, personal fees from Biogen, personal fees from Boehringer Ingelheim, personal fees from Theranexus, personal fees from GE HealthCare, personal fees from Jazz Pharmaceuticals, personal fees from AbbVie, personal fees from Janssen, personal fees from Otsuko, personal fees from Phytopharmics, personal fees from Inception Sciences, others from Parkinson Canada, and personal fees from Curasen, outside the submitted work. Go to Neurology.org/N for full disclosures.
References
- 1.Huang W, Ramsey KM, Marcheva B, Bass J. Circadian rhythms, sleep, and metabolism. J Clin Invest. 2011;121(6):2133-2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harrington J. Health effects of shift work and extended hours of work. Occup Environ Med. 2001;58(1):68-72. [Google Scholar]
- 3.Smith MR, Eastman CI. Shift work: health, performance and safety problems, traditional countermeasures, and innovative management strategies to reduce circadian misalignment. Nat Sci Sleep. 2012;4:111-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eastman CI. Circadian rhythms and bright light: recommendations for shift work. Work Stress. 1990;4(3):245-260. [Google Scholar]
- 5.Mattingly SM, Grover T, Martinez GJ, et al. The effects of seasons and weather on sleep patterns measured through longitudinal multimodal sensing. NPJ Digit Med. 2021;4(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gooley JJ. Light resetting and entrainment of human circadian rhythms. In: Kumar V, ed. Biological Timekeeping: Clocks, Rhythms and Behaviour. Springer India; 2017:297-313. [Google Scholar]
- 7.Reid KJ, Abbott SM. Jet lag and shift work disorder. Sleep Med Clin. 2015;10(4):523-535. [DOI] [PubMed] [Google Scholar]
- 8.Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23(1-2):497-509. [DOI] [PubMed] [Google Scholar]
- 9.Roenneberg T, Winnebeck EC, Klerman EB. Daylight saving time and artificial time zones: a battle between biological and social times. Front Physiol. 2019;10:944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uehli K, Mehta AJ, Miedinger D, et al. Sleep problems and work injuries: a systematic review and meta-analysis. Sleep Med Rev. 2014;18(1):61-73. [DOI] [PubMed] [Google Scholar]
- 11.American Sleep Association. Sleep and Sleep Disorder Statistics [online]. Accessed September 30, 2022. sleepassociation.org/about-sleep/sleep-statistics. [Google Scholar]
- 12.Grandner MA. Sleep, health, and Society. Sleep Med Clin. 2017;12:1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huyett P, Siegel N, Bhattacharyya N. Prevalence of sleep disorders and association with mortality: results from the NHANES 2009-2010. Laryngoscope. 2021;131(3):686-689. [DOI] [PubMed] [Google Scholar]
- 14.Hicks RA, Lindseth K, Hawkins J. Daylight saving-time changes increase traffic accidents. Percept Mot Skills. 1983;56(1):64-66. [DOI] [PubMed] [Google Scholar]
- 15.Sipilä JO, Ruuskanen JO, Rautava P, Kytö V. Changes in ischemic stroke occurrence following daylight saving time transitions. Sleep Med. 2016;27-28:20-24. [DOI] [PubMed] [Google Scholar]
- 16.Ferrazzi E, Romualdi C, Ocello M, et al. Changes in accident & emergency visits and return visits in relation to the enforcement of daylight saving time and photoperiod. J Biol Rhythms. 2018;33(5):555-564. [DOI] [PubMed] [Google Scholar]
- 17.Janszky I, Ljung R. Shifts to and from daylight saving time and incidence of myocardial infarction. N Engl J Med. 2008;359(18):1966-1968. [DOI] [PubMed] [Google Scholar]
- 18.Manfredini R, Fabbian F, De Giorgi A, et al. Daylight saving time and myocardial infarction: should we be worried? A review of the evidence. Eur Rev Med Pharmacol Sci. 2018;22(3):750-755. [DOI] [PubMed] [Google Scholar]
- 19.Darien I. When daylight saving time ends, 41% plan to ‘fall back’ to sleep [online]. Accessed September 30, 2022. aasm.org/when-daylight-saving-time-ends-people-plan-to-sleep.
- 20.Raina PS, Wolfson C, Kirkland SA, et al. The Canadian Longitudinal Study on Aging (CLSA). Can J Aging. 2009;28(3):221-229. [DOI] [PubMed] [Google Scholar]
- 21.Hoch CC, Reynolds CF III, Nebes RD, Kupfer DJ, Berman SR, Campbell D. Clinical significance of sleep-disordered breathing in Alzheimer's disease. Preliminary data. J Am Geriatr Soc. 1989;37(2):138-144. [DOI] [PubMed] [Google Scholar]
- 22.Zolfaghari S, Yao CW, Wolfson C, Pelletier A, Postuma RB. Sleep disorders and future diagnosis of parkinsonism: a prospective study using the Canadian Longitudinal Study on Aging. J Parkinsons Dis. 2022;12(1):257-266. [DOI] [PubMed] [Google Scholar]
- 23.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297-307. [DOI] [PubMed] [Google Scholar]
- 24.Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. [DOI] [PubMed] [Google Scholar]
- 25.Canada NRC. Time zones and daylight saving time [online]. Accessed September 30, 2022. nrc.canada.ca/en/certifications-evaluations-standards/canadas-official-time/time-zones-daylight-saving-time.
- 26.Suzuki M, Taniguchi T, Furihata R, et al. Seasonal changes in sleep duration and sleep problems: a prospective study in Japanese community residents. PLoS One. 2019;14(4):e0215345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de la Iglesia HO, Fernández-Duque E, Golombek DA, et al. Access to electric light is associated with shorter sleep duration in a traditionally hunter-gatherer community. J Biol Rhythms. 2015;30(4):342-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Connell SE, Griffiths PL, Clemes SA. Seasonal variation in physical activity, sedentary behaviour and sleep in a sample of UK adults. Ann Hum Biol. 2014;41:1-8. [DOI] [PubMed] [Google Scholar]
- 29.Wehr TA, Giesen HA, Moul DE, Turner EH, Schwartz PJ. Suppression of men's responses to seasonal changes in day length by modern artificial lighting. Am J Physiol. 1995;269(1 pt 2):R173-R178. [DOI] [PubMed] [Google Scholar]
- 30.Johnsen MT, Wynn R, Allebrandt K, Bratlid T. Lack of major seasonal variations in self reported sleep-wake rhythms and chronotypes among middle aged and older people at 69 degrees North: the Tromsø Study. Sleep Med. 2013;14(2):140-148. [DOI] [PubMed] [Google Scholar]
- 31.Sivertsen B, Overland S, Krokstad S, Mykletun A. Seasonal variations in sleep problems at latitude 63°-65° in Norway: the Nord-Trondelag Health Study, 1995-1997. Am J Epidemiol. 2011;174(2):147-153. [DOI] [PubMed] [Google Scholar]
- 32.Titova OE, Lindberg E, Elmståhl S, Lind L, Benedict C. Seasonal variations in sleep duration and sleep complaints: a Swedish cohort study in middle-aged and older individuals. J Sleep Res. 2022;31(1):e13453. [DOI] [PubMed] [Google Scholar]
- 33.Schneider AM, Randler C. Daytime sleepiness during transition into daylight saving time in adolescents: are owls higher at risk? Sleep Med. 2009;10(9):1047-1050. [DOI] [PubMed] [Google Scholar]
- 34.Harrison Y. Individual response to the end of Daylight Saving Time is largely dependent on habitual sleep duration. Biol Rhythm Res. 2013;44(3):391-401. [Google Scholar]
- 35.Lahti TA, Leppämäki S, Lönnqvist J, Partonen T. Transition to daylight saving time reduces sleep duration plus sleep efficiency of the deprived sleep. Neurosci Lett. 2006;406(3):174-177. [DOI] [PubMed] [Google Scholar]
- 36.Barnes CM, Wagner DT. Changing to daylight saving time cuts into sleep and increases workplace injuries. J Appl Psychol. 2009;94(5):1305-1317. [DOI] [PubMed] [Google Scholar]
- 37.Montréal, Quebec, Canada: Sunrise, Sunset, and Daylength, March 2022 [online]. Accessed September 30, 2022. timeanddate.com/sun/canada/montreal?month=3&year=2022. [Google Scholar]
- 38.Cyr M, Artenie DZ, Al Bikaii A, Borsook D, Olson JA. The effect of evening light on circadian-related outcomes: a systematic review. Sleep Med Rev. 2022;64:101660. [DOI] [PubMed] [Google Scholar]
- 39.Montréal, Quebec, Canada: Sunrise, Sunset, and Daylength, November 2022 [online]. Accessed September 30, 2022. timeanddate.com/sun/canada/montreal?month=11&year=2022. [Google Scholar]
- 40.Aschoff J, Hoffmann K, Pohl H, Wever R. Re-entrainment of circadian rhythms after phase-shifts of the Zeitgeber. Chronobiologia. 1975;2(1):23-78. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the CLSA webpage (clsa-elcv.ca) for researchers who meet the criteria for access to deidentified CLSA data.
Furthermore, the opinions expressed in this article are of the author's own and do not reflect the views of the CLSA.