Brain death, more recently called death determination by neurologic criteria,1 is at the nexus of current controversy as the US Uniform Law Commission (ULC) seeks to revise the Uniform Determination of Death Act (UDDA). The UDDA was developed in 1980 by the ULC, then called the National Conference of Commissioners for Uniform State Laws, in conjunction with the American Bar Association, the American Medical Association, and the President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research.2 The UDDA was designed with 2 principal goals: to enhance the uniformity of death determination among states and to codify the new determination of death based on the irreversible cessation of all functions of the brain, a condition that had been concisely and popularly, though infelicitously, termed “brain death.”3 The President's Commission's first report in 1981, Defining Death, provided the conceptual justification for the UDDA and showed how brain death determination should be best incorporated into a model statute of death.4 The ULC effort was extremely successful because a large majority of states enacted the UDDA verbatim or with only minor modifications.5
Over the past 40 years, the medical and legal acceptance of brain death has grown steadily to the point that it is now practiced widely throughout the developed and developing world, as exhaustively chronicled by the recent World Brain Death Project.6 The components of the brain death examination have been formalized into well-accepted evidence-based clinical practice guidelines issued by the American Academy of Neurology (AAN) and other medical specialty societies.7 These guidelines are taught using lectures, video teaching tools, and training simulations in which residents and fellows learn how to perform and record each element of the examination and how to optimally communicate with and counsel grieving family members.8 Brain death determination procedures now are routinely incorporated into hospital policies, many of which require physicians to complete brain death checklists to enhance best practice compliance and uniformity.9
Brain death determination has been fully standardized into clinical practice, notwithstanding frustratingly persistent practice variations among neurologists.10 Its principal medical controversies now center on the fine points of brain death determination, such as the boundaries of allowable metabolic or toxic confounders,11 the role of ancillary testing,12 and whether 1 or 2 examinations are necessary.13 Most neurologists conducting brain death determinations regard it as an essential element of their routine medical practice and are unaware of or unconcerned by its critiques. In my lectures on conceptual issues in brain death to neurology departments of medical centers and to philosophy departments of universities, I am struck by the stark contrast in reception between the 2 audiences: There is nearly general acceptance from clinicians but major criticism from philosophers.14
Despite its widespread medical acceptance, since the time of its first description, brain death has generated opponents who, for conceptual or religious reasons, reject it as human death. The cohort of brain death skeptics has grown in recent years from a handful of philosophers and religious authorities to a larger and more varied and vocal cadre of scholars. Although the controversies they raise initially were restricted to academic settings, now they have extended into the public arena. The skeptics' cause has been supplemented by several high-profile medicolegal cases that have garnered widespread media attention and by some high court judicial rulings that have led a few states to amend their death statutes.15 Some of these scholars reject brain death outright on the conceptual ground that it is a contrived and nonbiological death determination16 or that it is a legal fiction to permit organ donation.17 And a few of these critics have urged the ULC to exclude brain death from the revised UDDA.
Even supporters of brain death have identified specific shortcomings of the UDDA. These deficits include (1) ambiguities raised by the UDDA's dual criteria of death that could be mitigated by providing a single brain criterion that could be tested by physicians in 2 ways, depending on the presence of technologic support18; (2) documented inconsistencies between the criterion and accepted tests of death resulting from the UDDA's reliance on the whole-brain criterion19,20; and (3) ambiguities in the interpretation of the circulatory-respiratory criterion of death because of its requirement for the irreversible cessation of vital organ function rather than for its permanent cessation.21 Despite the UDDA's widespread acceptance and popularity over the past 40 years, the legal ramifications of these critiques convinced the ULC to consider revising it.
Accordingly, in 2021, the ULC embarked on a multiyear study-revision process, following its established internal procedures. First, the ULC empaneled a Study Committee of commissioners and observers (consultants) to scrutinize and weigh the merits of each claim of a shortcoming in the UDDA, to decide whether they warranted a revision. After a year of analysis, the Study Committee concluded that revising the UDDA was justified and recommended the empaneling of a Drafting Committee, also composed of commissioners and observers, to rewrite the UDDA. The Drafting Committee met throughout 2022 and plans to have a final redrafted UDDA ready for review by the Style Committee in 2023 and thereafter submitted to a vote by the entire ULC. If the ULC approves the revised UDDA, they will initiate an implementation process that requires negotiations between ULC commissioners and state legislators in all 50 states, with the goal of replacing each state's death statute with the revised UDDA. Given the present contentious political climate in many state legislatures and the controversies inherent in any death statute, it seems likely that widespread state approval of a revised UDDA will be a much more challenging feat than the one the ULC successfully accomplished 40 years ago.
Along with many of the other authors of this series of Neurology® articles, I serve as an observer participating in the meetings of ULC Study and Drafting Committees. This role has given us direct input into the commissioners' analysis of critiques and recommendations as well as front row seats to observe the committees' processes. The commissioners have asked many of the observers to offer their opinions and justifications on how the UDDA should be revised. At times, the physician observers have given conflicting opinions and debated each other during meetings. Several of the observers have independently submitted their opinions on how the committee should rewrite the UDDA for publication in Neurology22 and other journals.23-25
To explain the context and content of these issues for practicing neurologists, Neurology Editor, José Merino commissioned a series of articles on the UDDA and brain death of which this is the first. Here I outline the history and critiques of the UDDA and try impartially to provide the context for the debates over how it should be revised. These articles include the following: What is the ideal brain criterion of death: clinical and practical considerations by Nathaniel Robbins; What is the ideal brain criterion of death: nonclinical considerations by Michael Rubin; Must hypothalamic neurosecretory function cease for brain death determination? Yes by Michael Nair-Collins and No by Panayiotis Varelas; Should the criterion for brain death require irreversible or permanent cessation of function? Irreversible by Ari Joffe and Permanent by Dale Gardiner and Andrew McGee; Should the brain death exam with apnea test require surrogate informed consent? Yes by Ivor Berkowitz and No by David Greer. The series ends with 2 essays that pose and resolve challenges to the clinical determination of brain death: Potential threats and impediments to the clinical practice of brain death determination by Ariane Lewis and Matthew Kirschen and Re-thinking brain death: Why “dead enough” is not good enough by Daniel Sulmasy and Christopher DeCock.
The Uniform Determination of Death Act
The UDDA of 1980 is a concise model death statute that provides:
An individual who has sustained either (1) irreversible cessation of circulatory and respiratory functions, or (2) irreversible cessation of all functions of the entire brain, including the brain stem, is dead. A determination of death must be made in accordance with accepted medical standards.2
In the book Defining Death, the President's Commission thoughtfully discussed the evolution of American death statutes and explained why they selected the specific language of the UDDA.4 The Commission purposely chose dual criteria of death to reassure physicians that they could continue to use the circulatory-respiratory criterion in the overwhelming percentage of death determinations in which tracheal positive-pressure ventilation (TPPV) was not provided. The new brain criterion was afforded equal status as an alternate criterion of death to be applied in those relatively few cases in which TPPV was provided. Although the succinct nature of the UDDA did not allow clarifying the relationship between the 2 criteria of death, the discussion in Defining Death supported the contingent account my colleagues and I had offered: that the circulatory-respiratory criterion became a valid criterion of death when it led directly to the fulfillment of the more fundamental brain criterion.18,26
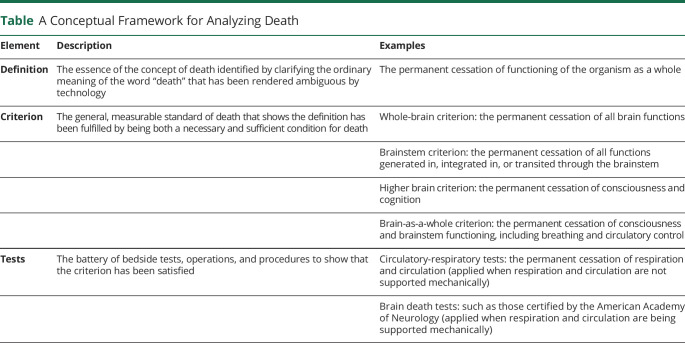
In the first critical analysis of Defining Death and the UDDA, published a few months after the President's Commission's report was issued, my colleagues and I applauded the arguments justifying brain death but showed that the structure of the UDDA did not follow logically from those claims.26 We argued that rather than offering 2 criteria of death, the UDDA should have provided a single criterion of death—the irreversible cessation of the functions of the entire brain—but state that the criterion could be satisfied by 2 different sets of tests depending on the clinical circumstance. When no device supported ventilation, the irreversible cessation of circulation and ventilation served as a sufficient test for death. When a device supported ventilation, specific brain death tests needed to be used. The Table provides a conceptual framework delineating the relationship of the criteria and tests of death.
Table.
A Conceptual Framework for Analyzing Death
Although 40 years ago this critique probably carried greater theoretical than practical import, recent technologic developments in the postmortem re-establishment of organ donor circulation, such as by using extracorporeal membrane oxygenation (ECMO)27 and normothermic regional perfusion,28 have made the precise relationship between the circulatory and brain criteria of the UDDA more consequential.29 Of historical interest, the Law Reform Commission of Canada also published a model death statute in 1981 featuring a single brain criterion of death that could be tested in 2 ways—exactly paralleling our proposed statute.30 However, in ironic contrast to the UDDA's success in the United States, neither Parliament nor any Canadian province except Manitoba adopted it.
Current Controversies Over the UDDA
Here I briefly provide the context that frames the debates on several of the principal controversies over the UDDA, all of which have been discussed during the meetings of the ULC Study and Drafting Committees. Subsequent articles in this series address some, but not all, of these debates, the soundness of whose arguments readers can assess for themselves.
Is Brain Death Biological Death?
A fundamental question is whether brain death is truly biological death or rather is a nonbiological schema16 or a contrived legal fiction17 that permits physicians to conduct unilateral withdrawal of life-sustaining therapy and multiorgan procurement for transplantation from severely brain-damaged patients. While this question has been raised repeatedly by several ULC observers, it will not be featured in this Neurology debate series for 2 reasons: (1) It is not directly relevant to practicing neurologists who largely accept brain death, do not question its conceptual basis, understand its legality, and routinely practice its determination as they have been trained, and (2) the ULC Drafting Committee has already rejected the idea of removing the brain criterion of death from any revised UDDA. Their summary rejection is unsurprising given that a primary purpose of the original UDDA in 1980 was to provide the legal foundation for physicians to incorporate brain death determination into their clinical practices. Nevertheless, this conceptual question continues to be debated within the halls of academia where it remains a source of heated controversy. In addition, the ULC Drafting Committee is considering the inclusion of an opt-out option that will allow family members who believe brain death is not truly death to prohibit physicians from declaring it.
The principal justification for regarding brain death as biological death is that it marks the cessation of the human organism as a whole. The organism as a whole refers not to the whole organism (the sum of its parts) but rather to the essential defining characteristics of the human organism that are generated autonomously by the natural interaction of its parts but are not localized to any part. The intrinsic interrelationship of the organism's innate ensemble of parts creates holistic emergent functions that comprise the coherent unity of the human organism and that maintain its life and health. Organ support technology obviously sustains the continued life of many parts of the brain-dead organism despite the cessation of the organism as a whole. Thus, brain death, the cessation of the organism as a whole, has a biological rationale as the organism's death, which has become necessary to clarify in our current era in which technology can support individual organs. Opponents to this claim, while generally agreeing that death is the cessation of the organism as a whole, maintain that the organism as a whole remains intact despite brain death. Interested readers can consult the accounts of both the conceptual justification of brain death as human death31,32 and the critiques rejecting their alleged equivalence.33,34
What Is the Ideal Brain Criterion of Death? Must Hypothalamic Neurosecretory Function Cease for Brain Death Determination?
The UDDA endorsed the whole-brain criterion of death by requiring the irreversible cessation of all brain functions. The President's Commission importantly clarified the distinction between brain functions and brain activities. Brain functions are physical signs of brain operations that are observable on neurologic examination, such as breathing, movements, and the reflexes conducted by the cranial nerves. Brain activities are neuronal cellular actions that, when isolated, do not coordinate distributed neural networks sufficiently to generate an observable function.4 The President's Commission held that the appropriate physiologic standard for brain death determination was at the macroscopic level of the cessation of brain functions, not at the microscopic level of cessation of brain neuronal activities. Thus, for brain death determination, brain functions must cease but some brain neuronal cellular activities may persist. In the prototypic case of brain death, a global brain insult from trauma, stroke, or cardiac arrest leads to massive cerebral edema with transtentorial herniation and intracranial hypertension which exceeds mean arterial blood pressure and produces intracranial circulatory arrest. Diffuse neuronal death then ensues diffusely throughout the brain.
The United Kingdom, largely through the influence of Christopher Pallis, conceptualized brain death as the widespread cessation of brainstem function: the brainstem criterion of death.35 Pallis emphasized that the brainstem was the center of the capacity for consciousness, respiration, and circulatory tone, that nearly all sensory input and motor output traversed the brainstem and that most of the bedside tests for brain death assessed brainstem functions. In practice, applying the brainstem criterion or the whole-brain criterion yield nearly identical determinations, with a very high level of diagnostic congruence.36 The relatively few instances in which the 2 criteria yield divergent results are cases of primary brainstem catastrophes sparing the cerebral hemispheres.37
For years, experienced neurologists have observed that not all patients determined to be brain dead had diabetes insipidus, suggesting the preservation of some degree of hypothalamic neurosecretion of vasopressin peptide prohormone to the posterior pituitary gland, despite the cessation of all other brain functions. One explanation for this conserved island of minor brain function is that the pituitary gland and adjacent hypothalamic neuroendocrine inputs often have a parallel and primarily extracranial blood supply which may be spared from the lethal effects of marked intracranial hypertension. Recent studies have shown that up to half of patients fulfilling the AAN criteria for brain death determination retain a degree of hypothalamic neurosecretory function that is sufficient to prevent diabetes insipidus. This finding of a single preserved brain function highlights the fact that, although these patients satisfy the AAN test battery for brain death, they do not fulfill the UDDA's all-encompassing requirement for the cessation of “all functions of the entire brain” resulting from its reliance on the whole-brain criterion of death.38
In addressing this issue, the AAN Ethics Law & Humanities Committee asserted that this isolated preserved hypothalamic neurosecretory function is inconsequential and remains fully consistent with brain death by fulfilling the AAN test battery.39 But despite this authoritative reassurance that reflects a consensus within the neurology professional community, the ULC remains concerned that, because the discrepancy between accepted medical practices and the plain language of the statute has led to high court judicial decisions questioning the validity and reliability of brain death, it may require an alteration of the whole-brain criterion in the UDDA. The ULC study and drafting committees agreed that when a prevailing and accepted best medical practice diverges from statutory law (such as the UDDA), generally, the requirements of the law should be changed to align with the accepted best medical practice—not vice versa.
One approach to better align the law with prevailing medical practice would be to modestly change the whole-brain criterion to the brain-as-a-whole criterion. While the brain-as-a-whole criterion remains in an early stage of refinement, it probably entails cessation of all major brain functions required by the whole-brain criterion, particularly those of the brainstem, but not of relatively minor functions such as hypothalamic neurosecretion and, perhaps, random, disorganized EEG activity.32 A group of ULC observers proposed an analogous modest modification of the whole-brain criterion they called the neurorespiratory criterion.22 An additional benefit of the whole-brain criterion modification approach is that it better aligns the criterion of death with how many neurologists personally conceptualize brain death—as requiring the cessation of most but not all brain functions.40
A complementary approach would be to tighten the test battery for brain death by, for example, requiring the neuroimaging demonstration of complete cessation of intracranial circulation.19 This approach would likely decrease the mismatch between the accepted AAN tests and the whole-brain criterion of death required by the UDDA but likely would be resisted by authoritative neurologists who maintain that brain death is fundamentally a clinical, not a radiologic, diagnosis.6,41 Such a requirement also would raise the question of the accuracy of neuroimaging tests, given the minimal data currently available on their positive and negative predictive values in confidently proving the complete cessation of intracranial blood flow.42 Finally, because such a requirement would significantly reduce the number of brain-dead organ donors, it likely would be opposed by the organ donation community.
The final potential brain criterion of death, the higher-brain formulation, requires only the permanent cessation of consciousness and cognition.43 This formulation, long popular within academic circles and the popular media, has been uniformly and consistently rejected by medical societies and laws throughout the world because it is a contrived, radical redefinition of death that classifies as dead, people in longstanding vegetative states who are regarded as alive everywhere in the world. This criterion was soundly rejected by the President's Commission in Defining Death in 1981.4 Given the great concern that ULC committee members expressed during the discussion of consciousness, over the difficulty of accurately ascertaining covert awareness in apparently unconscious patients in the intensive care unit44 and in vegetative states,45 it seems extremely unlikely that the ULC will recommend any version of the higher-brain formulation in a revised UDDA.
Should the Criteria for Brain Death Require Irreversible or Permanent Cessation of Function?
The UDDA states that the relevant vital functions must cease irreversibly, yet the tests to determine death issued by the medical consultants to the President's Commission in Appendix F of Defining Death required only the permanent cessation of these vital functions.4 Although the words “irreversible” and “permanent” at first seem synonymous, they carry an important distinction that becomes important in death determination. Irreversible cessation of a vital function means that, once it ceases, it cannot be restored with available technology because doing so is impossible (practically, not theoretically). By contrast, permanent cessation of a vital function means that, once it ceases, it will not be restored because it will neither restart itself (“autoresuscitation”) nor will physicians attempt to restart it with resuscitative interventions.21
Although the UDDA uses the word “irreversible” to describe the cessation of vital functions, the word is not defined in the statute or in Defining Death. Ambiguity over the precise meaning of the word “irreversible” in the UDDA has led to a controversy in death determination, centered on the precise moment of death in organ donation after the circulatory determination of death (DCDD).46,47 Although many people simply assume that the authors of the UDDA intended the strictest construal of “irreversible” (impossible), Alexander Capron, the Executive Director of the staff of the President's Commission, told me that, when writing Defining Death and endorsing the UDDA, they did not appreciate the distinction between the words irreversible and permanent and used them interchangeably. When he later became aware of the distinction between them, he commented that, although they chose the word irreversible for the UDDA, their intended meaning was permanent.
Revising the UDDA could clarify this point because whether death determination requires the irreversible or permanent cessation of circulatory function spells the difference between whether, at the moment of organ donation, DCDD donors are legally dead or remain alive. This ambiguity exists because, in a typical DCDD protocol, at the moment the organ donor's death is declared (usually 5 minutes after complete circulatory cessation), circulation and respiration have ceased permanently but not yet irreversibly.20
The traditional medical practice of death determination using the circulatory-respiratory criterion requires only the permanent cessation standard. When physicians determine death after the cessation of heartbeat, circulation, and respiration in a terminally ill patient with a do-not-resuscitate (DNR) order, they require only that the cessation of circulation and respiration is permanent. Given the presence of the DNR order, no attempt will be made to resuscitate, and physicians are not required to prove that the cessation of vital functions is irreversible because permanent cessation is sufficient. Therefore, in the absence of resuscitative efforts, physicians can declare death immediately after circulation and ventilation cease.21
Proving the irreversibility of circulatory cessation from cardiac arrest is demanding; it would require attempting resuscitation and showing that it failed and now even may require an unsuccessful trial of ECMO because this treatment has provided time to permit the spontaneous return of heartbeat after several days of asystole in a few remarkable cases of intractable cardiac arrest after myocardial infarction.48 A similar problem exists in proving the irreversible cessation of brain functions. Would proving that standard require aggressive medical and surgical treatment in even futile cases before the brain injury could be judged irreversible? Despite the attraction of its categorical ring, irreversible cessation of circulatory or brain function is a subtle and complex phenomenon and proving it is often unachievable or undesirable in contemporary medical practice.
The permanent irreversible distinction is applied less often to the brain criterion of death. From its beginning, brain death always has required the irreversible cessation of brain functions. But this strict requirement is an artifact of the retrospective nature of brain death determination: Testing for the cessation of brain functions is conducted long after the pathophysiologic process responsible for the brain damage has occurred. This retrospective timing of brain death testing contrasts with the typically prospective determination of cessation of circulation and respiration. However, there is no justification requiring irreversible cessation of brain function for brain death determination in controlled DCDD. Although there is no compelling reason to change brain death testing to requiring only permanent cessation, it may become necessary for emerging protocols of uncontrolled DCDD.49
Should the Brain Death Examination With Apnea Test Require Surrogate Informed Consent?
A more recent controversy surrounds the question of whether physicians have the duty to obtain informed consent from a lawful surrogate decision-maker to perform the brain death examination, just as they must routinely to perform invasive procedures. Initially, the consent issue was raised because of the alleged dangers of the apnea test,50 but more recently, critics have generalized the duty to obtain consent to the entire brain death determination.51 Debates over this claim have been published,52,53 and this issue will be debated in a later article in this series. To some extent, the consent issue turns on the precise risk of performing the apnea test and other interventions, in that the risk of a procedure is usually directly correlated with the requirement for consent. A recent scoping review of apnea testing in brain death showed a wide variability in apnea test procedures and their attendant risks.54 Everyone engaged in the debate should agree that, irrespective of the consent issue, if the apnea test is to be performed, it should be conducted properly according to the highest standards of accuracy, efficacy, and patient safety.
Should the UDDA Permit Religious or Other Exemptions From Brain Death Determination?
The need for a formalized exemption from brain death determination was promoted decades ago by some religious authorities in Orthodox Judaism and Islam who rejected brain death as violating their traditional religious teaching about the nature of death. Although both Judaism and Islam have internally varied and conflicting religious opinions about brain death,6 the strictest traditional authorities in both religions oppose it. In 1991, largely as a result of lobbying by the Orthodox Jewish community, New Jersey became the first state to provide a statutory exemption to brain death determination which is activated if the patient's family can document that their religion formally rejects it.55 In such validly documented cases, physicians declaring death must rely only on the permanent cessation of circulation and respiration. Several other states require physicians to provide the less restrictive standard of making a “reasonable accommodation” to a family's beliefs in the context of a brain death determination.
Of course, religion is not the only or even the most common source of family member disagreement with brain death. Some family members reject that the patient is dead on conceptual grounds and therefore demand continued treatment. Another common cause is a family's inability or emotional unwillingness to accept the finality of brain death, particularly in tragic cases of young, previously healthy patients with devastating traumatic brain injuries. In responses to such instances of family opposition, physicians should try to practice the virtues of compassion, tolerance, patience, willingness to compromise, and excellent communication skills.56 The ULC is currently debating whether to insert a clause in the revised UDDA providing exemptions to brain death declaration on religious, conceptional, or other grounds. This issue, and other practical management topics that arise in communicating with the family of the brain-dead patient and mediating disputes, will be explored in the penultimate article in this series.
Without doubt, the most flexible public policy approach would be to allow patients the liberty to choose their own personal death criteria and to extend that right of choice to lawful surrogate decision-makers such as durable powers of attorney for health care. This libertarian approach, proposed in detail by Veatch and Ross,57,58 holds that patients' constitutionally protected rights to consent and refuse treatment should encompass the ultimate right to be declared dead according to one's own choice of death criteria. Although permitting personal choice in medical conditions is appealing in a liberty-respecting society, the idea of personal choice in death criteria strikes me as difficult to implement in clinical practice and one that carries the potential for creating chaos in intensive care units. Furthermore, by adding such extraordinary flexibility to a death statute, it risks bending the statute beyond the breaking point and fracturing its consistency and applicability. Therefore, although it is possible the ULC will insert an opt-out clause in the revised UDDA, I find it unlikely that they will incorporate an unrestricted right of choice of a death criterion.
Future Directions
The precise language of the ULC's revision of the UDDA and their choice for the brain criterion of death will not be known, at least until mid-2023. While tweaks to the UDDA language could resolve some of its perceived shortcomings, any changes to well-established law also carries the potential of raising new and controversial issues. Therefore, a few skeptical ULC commissioners have warned that altering a successful law in the current era of contentious state legislatures might be playing with fire and could paradoxically and unintentionally trigger greater discord and controversy than by simply leaving it alone.
In any event, neurologists will continue to play an indispensable advisory role in the ULC's UDDA revision process. We can inform the commissioners' work with our explanations of brain death, our accounts of the accuracy, reliability, and acceptability of its determination, our depictions of the successes and problems of its determination in clinical practice, and our predictions about the impact of future changes in the UDDA on medical practice. The design of an optimal statute of death is a prime example of the benefits to society that result from a close and respectful collaboration among lawyers, lawmakers, and physicians when drafting laws governing health care.
Glossary
- AAN
American Academy of Neurology
- DCDD
donation after the circulatory determination of death
- DNR
do-not-resuscitate
- ECMO
extracorporeal membrane oxygenation
- TPPV
tracheal positive-pressure ventilation
- UDDA
Uniform Determination of Death Act
- ULC
Uniform Law Commission
Appendix. Author
Study Funding
No targeted funding reported.
Disclosure
The author reports no relevant disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Lewis A, Bernat JL, eds. Death Determination by Neurologic Criteria: Areas of Controversy and Consensus. Springer Nature; 2022. [Google Scholar]
- 2.Uniform Determination of Death Act. Uniform Law Acts. 1980;12:589. [Google Scholar]
- 3.Ad Hoc Committee. A definition of irreversible coma: report of the Ad Hoc Committee of the Harvard Medical School to examine the definition of brain death. JAMA. 1968;205(6):337-340. [PubMed] [Google Scholar]
- 4.President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Defining Death. Medical, Ethical, and Legal Issues in the Determination of Death. US Government Printing Office; 1981. [Google Scholar]
- 5.Pope TM. Legal briefing: brain death and total brain failure. J Clin Ethics. 2014;25(3):245-247. [PubMed] [Google Scholar]
- 6.Greer DM, Shemie SD, Lewis A, et al. Determination of brain death/death by neurological criteria: the World Brain Death Project. JAMA. 2020;324(11):1078-1097. [DOI] [PubMed] [Google Scholar]
- 7.Wijdicks EFM, Varelas PN, Gronseth GS, Greer DM. Evidence-based guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010:74(23):1911-1918. [DOI] [PubMed] [Google Scholar]
- 8.MacDougall BJ, Robinson JD, Kappus L, Sudikoff SN, Greer DM. Simulation-based training in brain death determination. Neurocrit Care. 2014;21(3):383-391. [DOI] [PubMed] [Google Scholar]
- 9.Young GB. Checklist for brain death. Can Med Assoc J. 1991;145(4):294-295. [PMC free article] [PubMed] [Google Scholar]
- 10.Braksick SA, Robinson CP, Gronseth GS, Hocker S, Wijdicks EFM, Rabinstein AA. Variability in reported physician practices for brain death determination. Neurology. 2019;92(9):e888-e894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murphy L, Wolfer H, Hendrickson RG. Toxicologic confounders of brain death determination: a narrative review. Neurocrit Care. 2021;34(3):1072-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robbins NM, Bernat JL. When do you order ancillary tests to determine brain death? Neurol Clin Pract. 2018;8(3):266-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varelas PN, Rehman M, Mehta C, et al. Comparison of 1 vs 2 brain death examinations on time to death pronouncement and organ donation: a 12-year single center experience. Neurology. 2021;96(10):e1453-e1461. [DOI] [PubMed] [Google Scholar]
- 14.Bernat JL. Whither brain death? Am J Bioethics. 2014;14(8):3-8. [DOI] [PubMed] [Google Scholar]
- 15.Lewis A, Scheyer O. Legal objections to use of neurologic criteria to declare death in the United States: 1968 to 2017. Chest. 2019;155(6):1234-1245. [DOI] [PubMed] [Google Scholar]
- 16.Shewmon DA. The brain and somatic integration: insights into the standard biological rationale for equating ‘brain death’ with death. J Med Philos. 2001;26(5):457-478. [DOI] [PubMed] [Google Scholar]
- 17.Shah SK, Miller FG. Can we handle the truth? Legal fictions in the determination of death. Am J Law Med. 2010;36(4):540-585. [DOI] [PubMed] [Google Scholar]
- 18.Bernat JL, Culver CM, Gert B. Defining death in theory and practice. Hastings Cent Rep. 1982;12(1):5-9. [PubMed] [Google Scholar]
- 19.Bernat JL, Dalle Ave AL. Aligning the criterion and tests for brain death. Cambr Q Healthc Ethics. 2019;28(4):635-641. [DOI] [PubMed] [Google Scholar]
- 20.Sulmasy DP. Whole-brain death and integration: realigning the ontological concept with clinical diagnostic tests. Theor Med Bioeth. 2019;40(5):455-481. [DOI] [PubMed] [Google Scholar]
- 21.Bernat JL. How the distinction between “irreversible” and “permanent” illuminates circulatory-respiratory death determination. J Med Philos. 2010;35(3):242-255. [DOI] [PubMed] [Google Scholar]
- 22.Omelianchuk A, Bernat J, Caplan A, et al. Revise the Uniform Determination of Death Act to align the law with practice through neurorespiratory criteria. Neurology. 2022;98(13):532-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewis A, Bonnie RJ, Pope T. It's time to revise the Uniform Determination of Death Act. Ann Intern Med. 2020;172(2):143-145. [DOI] [PubMed] [Google Scholar]
- 24.Shewmon DA. Statement in support of revising the Uniform Determination of Death Act and in opposition to a proposed revision. J Med Philos. 2021;2021:jhab014. doi: 10.1093/jmp/jhab014 [DOI] [PubMed] [Google Scholar]
- 25.Nguyen D. Does the Uniform Determination of Death Act need to be revised? Linacre Q. 2020;87(3):317-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernat JL, Culver CM, Gert B. On the definition and criterion of death. Ann Intern Med. 1981;94(3):389-394. [DOI] [PubMed] [Google Scholar]
- 27.Domínguez-Gil B, Ascher N, Capron AM, et al. Expanding controlled donation after the circulatory determination of death: statement from an international collaborative. Intensive Care Med. 2021;47(3):265-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Entwistle JW, Drake DH, Fenton KN, et al. Normothermic regional perfusion: ethical issues in thoracic organ donation. J Thorac Cardiovasc Surg. 2022;164(1):147-154. doi: 10.1016/j.jtcvs.2022.01.018 [DOI] [PubMed] [Google Scholar]
- 29.Bernat JL, Capron AM, Bleck TP, et al. The circulatory-respiratory determination of death in organ donation. Crit Care Med. 2010;38(3):963-970. [DOI] [PubMed] [Google Scholar]
- 30.Law Reform Commission of Canada. Criteria for the Determination of Death. Law Reform Commission of Canada; 1981. [Google Scholar]
- 31.Huang AP, Bernat JL. The organism as a whole in an analysis of death. J Med Philos. 2019;44(6):712-731. [DOI] [PubMed] [Google Scholar]
- 32.Bernat JL. Refinements in the organism as a whole rationale for brain death. Linacre Q. 2019;86(4):347-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shewmon DA. Constructing the death elephant: a synthetic paradigm shift for the definition, criteria, and tests for death. J Med Philos. 2010;35(3):256-298. [DOI] [PubMed] [Google Scholar]
- 34.Joffe AR, Khaira G, de Caen AR. The intractable problems with brain death and possible solutions. Philos Ethics Humanit Med. 2021;16(1):11. doi: 10.1186/s13010-021-00107-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pallis C, Harley DH. The ABC of Brainstem Death, 2nd ed. British Medical Journal Publishers; 1996. [Google Scholar]
- 36.Wijdicks EFM. The transatlantic divide over brain death determination and the debate. Brain. 2012;135(4):1321-1331. [DOI] [PubMed] [Google Scholar]
- 37.Varelas PN, Brady P, Rehman M, et al. Primary posterior fossa lesions and preserved supratentorial cerebral blood flow: implications for brain death determination. Neurocrit Care. 2017;27(3):407-414. [DOI] [PubMed] [Google Scholar]
- 38.Nair-Collins M, Joffe AR. Frequent preservation of neurologic function in brain death and brainstem death entails false-positive misdiagnosis and cerebral perfusion. AJOB Neurosci. 2021;2021:1-14. doi: 10.1080/21507740.2021.1973148 [DOI] [PubMed] [Google Scholar]
- 39.Russell JA, Epstein LG, Greer DM, Kirschen M, Rubin MA, Lewis A. Brain death, the determination of brain death, and member guidance for brain death accommodation requests: AAN position statement. Neurology. 2019;92(5):228-232. doi: 10.1212/WNL.0000000000006750 [DOI] [PubMed] [Google Scholar]
- 40.Joffe AR, Anton NR, Duff JP, deCaen A. A survey of American neurologists about brain death: understanding the conceptual basis and diagnostic tests for brain death. Ann Intensive Care. 2012;2(1):4. doi: 10.1186/2110-5820-2-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wijdicks EFM, The case against confirmatory tests for determining brain death in adults. Neurology. 2010;75(1):77-83. [DOI] [PubMed] [Google Scholar]
- 42.Shewmon DA, Salamon N. The MRI of Jahi McMath and its implications for the global ischemic penumbra hypothesis. J Child Neurol. 2022:37(1):35-42. [DOI] [PubMed] [Google Scholar]
- 43.Gervais K. Redefining Death. Yale University Press; 1987. [Google Scholar]
- 44.Edlow BL, Fins JJ. Assessment of covert consciousness in the intensive care unit: clinical and ethical considerations. J Head Trauma Rehabil. 2018;33(6):424-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Monti MM, Vanhaudenhuyse A, Coleman MR, et al. Willful modulation of brain activity in disorders of consciousness. N Engl J Med. 2010;362(7):579-589. [DOI] [PubMed] [Google Scholar]
- 46.Bernat JL. Point: are donors after circulatory death really dead, and does it matter? Yes and yes. Chest. 2010;138:1, 13-16. [DOI] [PubMed] [Google Scholar]
- 47.Truog RD, Miller FG. Counterpoint: are donors after circulatory death really dead, and does it matter? No and not really. Chest. 2010;138(1):16-18. [DOI] [PubMed] [Google Scholar]
- 48.Tweet MS, Schears GJ, Cassar A, Sheldon SH, McGlinch BP, Sandhu GS. Emergency cardiac support with extracorporeal membrane oxygenation for cardiac arrest. Mayo Clin Proc. 2013;88(7):761-765. [DOI] [PubMed] [Google Scholar]
- 49.Bernat JL. On noncongruence between the concept and determination of death. Hastings Cent Rep. 2013;43(6):25-33. [DOI] [PubMed] [Google Scholar]
- 50.Berkowitz I, Garrett JR. Legal and ethical considerations for requiring consent for apnea testing in brain death determination. Am J Bioeth. 2020;20(6):4-16. [DOI] [PubMed] [Google Scholar]
- 51.Paquette E, Frader J, Shah S, Tasker RC, Truog R. Beyond the apnea test: an argument to broaden the requirement for consent to the entire brain death evaluation. Am J Bioeth. 2020;20(6):17-19. [DOI] [PubMed] [Google Scholar]
- 52.Lewis A, Greer D. Point: should informed consent be required for apnea testing in patients with suspected brain death? No. Chest. 2017;152(4):700-702. [DOI] [PubMed] [Google Scholar]
- 53.Truog RD, Tasker RC. Counterpoint: should informed consent be required for apnea testing in patients with suspected brain death? Yes. Chest. 2017;152(4):702-704. [DOI] [PubMed] [Google Scholar]
- 54.Busl KM, Lewis A, Varelas PN. Apnea testing for the determination of brain death: a systematic scoping review. Neurocrit Care. 2021;34(2):608-620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Olick RS: Brain death, religious freedom, and public policy: New Jersey's landmark legislative initiative. Kennedy Inst Ethics J. 1991;1(4):275-288. [DOI] [PubMed] [Google Scholar]
- 56.Truog RD, Morrison W, Kirschen M. What should we do when families refuse testing for brain death? AMA J Ethics. 2020;22(12):986-994. [DOI] [PubMed] [Google Scholar]
- 57.Ross LF. Respecting choice in definitions of death. Hastings Cent Rep. 2018;48(suppl 4):S53-S55. [DOI] [PubMed] [Google Scholar]
- 58.Veatch RM, Ross LF. Defining Death: The Case for Choice. Georgetown University Press; 2016. [Google Scholar]