Abstract
Background:
Military sexual trauma (MST) is linked to a range of deleterious health outcomes. Extant literature has focused disproportionately on mental health sequelae. Yet, additional research is needed to better understand the extent to which MST contributes to another key issue facing service members: alcohol misuse and related problems. Additionally, sex differences in the nature and prevalence of MST may impact sequelae. The present research examined (a) MST history prevalence among female and male service members, (b) relations between MST history and risk for alcohol misuse and related problems, and (c) potential sex differences in these experiences and outcomes.
Methods:
Data from current/previous service members (334 males, 70 females) were drawn from Operation: SAFETY (Soldiers and Families Excelling Through the Years), a longitudinal study of U.S. Army Reserve/National Guard soldiers and partners. Analyses examined prevalence and types of MST experienced, relations between MST history and three alcohol-related variables (total consumption, heavy drinking frequency, alcohol problems), and differences by sex.
Results:
Approximately one-third (33.7%) of service members reported MST history. Females (61.4%) reported MST history at more than twice the rate of males (27.8%). Interactions between MST and sex were significant for all alcohol variables. For males, MST history was related to 70% higher alcohol consumption, 86% higher heavy drinking frequency, and 45% higher alcohol problem scores. MST history was unrelated to alcohol variables for females.
Conclusion:
Findings suggest higher prevalence of MST among USAR/NG service members than is often reported in the literature, particularly for males. MST history was associated with higher and more hazardous/harmful current alcohol consumption for male service members, highlighting need for greater screening, prevention, and intervention among a population already at high risk for problematic alcohol use. Results underscore MST as an important and prevalent experience requiring greater study alongside more traditional notions of service-connected trauma.
Keywords: military sexual trauma, alcohol misuse, heavy drinking, sex differences, service-connected trauma
Introduction
Military sexual trauma (MST)—unwanted physical contact (e.g., touching, assault, rape) and verbal remarks (e.g., comments, coercion, threats) of a sexual nature—represents a pressing public health issue within the military. Not only is MST associated with its own negative health sequelae (Kimerling et al., 2007), but there is also potential for compounding effects with service members’ experience of other stressors and mental and behavioral health issues. With this in mind, there are important gaps in the MST literature that warrant further study. In particular, relations between MST and mental health sequelae have been well studied (Kimerling et al., 2007, Kimerling et al., 2010), but additional work is needed to better understand the extent to which MST exposure contributes to one of the top issues facing recent service members: alcohol misuse and related problems (Seal et al., 2011). Additionally, important sex differences in the nature and prevalence of MST may have implications for sequelae. Yet, a predominant focus on female victims in the literature can interfere with a more complete understanding of sex differences in prevalence, nature of MST-related experiences, and potential sequelae. The present research aims to shed light on these important issues.
The U.S. Army has identified sexual assault/sexual harassment as one of key harmful behaviors—along with suicide, discrimination, racism, and extremism—that undermines trust and negatively impacts force readiness (U.S. Army, October 2019). This increased focus has been accompanied by a wave of new prevention programs and reforms to how MST cases are handled across all branches. On July 2nd, 2021, following release of a report by the Independent Review Commission on Sexual Assault in the Military (2021), U.S. Secretary of Defense, General (retired) Lloyd Austin, introduced initiatives to remove investigation of MST cases from the chain of command, add sexual harassment as an offense under the Uniform Code of Military Justice (UCMJ), and establish dedicated offices to handle prosecution (Austin, July 2021a). Following this announcement, the Department of Defense (DoD) has moved quickly to begin implementing these policies (Austin, September 2021b). With these recent changes, it is expected that more victims will feel comfortable coming forward and reporting their experiences. Greater understanding of sex differences in relations between MST and alcohol misuse, as well as in overall prevalence and nature of MST experiences—the focus of the present research—is critical for effectively supporting these victims and targeting resources.
MST and Alcohol Use
MST increases service members’ risk for a range of deleterious health outcomes (O’Brien and Sher, 2013). To date, much of the focus in the literature has been on associated mental health symptoms (Kimerling et al., 2007, Kimerling et al., 2010, Klingensmith et al., 2014), but MST may relate to other negative health-related outcomes, such as substance use and associated problems. Relations between sexual assault and substance use are well-established in the civilian literature (see Burnam et al., 1988, Stewart, 1996, Konkolÿ Thege et al., 2017); however, less attention has been paid to these links within military populations. Some evidence suggests an association between MST history and greater odds of substance use disorder diagnosis among Veterans Health Administration (VHA) patients (Kimerling et al., 2007, Kimerling et al., 2010, Beckman et al., 2021). However, these findings cannot speak to the nature of problematic use outside clinical diagnoses and treatment-seeking VHA populations. Given the eligibility limitations for VHA care for many reserve soldiers, and increasing rates of seeking care through civilian providers (Rose et al., 2021), further examination of these potential connections is warranted.
Alcohol misuse is a pressing issue among U.S. military personnel. Alcohol use is higher among U.S. service members than among sex- and age-matched civilians (Ames and Cunradi, 2004). Alcohol misuse presents a range of intrapersonal consequences for service members and hinders operational readiness (Harwood et al., 2009). Previous research estimates that alcohol misuse among active-duty personnel alone costs the DoD approximately $1.2 billion per year in medical care and reduced operational readiness (Harwood et al., 2009). Furthermore, prior work demonstrates that service members may use drinking in an attempt to self-medicate and cope with service-connected trauma (e.g., combat exposure, PTSD; Blakey et al., 2021, Hawn et al., 2020).
Indeed, the authors’ prior research in this vein found that deployment-related MST predicted subsequent heavy episodic drinking and alcohol problems among U.S. Army Reserve and National Guard (USAR/NG) soldiers (Fillo et al., 2018). Due to the original design and focus of the parent study utilized for those analyses, we were only able to examine MST experienced by male service members during their most recent deployment (Fillo et al., 2018). Yet, MST may occur in various contexts of service outside of deployment, and it was not possible to examine sex differences in experiences or outcomes. Additional measures were added to subsequent waves of the parent study to enable broader examination of MST and potential sequelae. The present research aims to broaden understanding of the relationship between MST and alcohol by: examining MST experienced at any point during service; teasing apart total alcohol consumed, heavy drinking frequency, and alcohol problems; and examining sex differences in these experiences and sequelae.
Sex Differences in MST
MST research has historically focused on female service members (Allard et al., 2011, Wolfe et al., 1998), due to their high risk of sexual victimization in both civilian and military contexts. Men, particularly in the military, are also at high risk of sexual victimization (Kimerling et al., 2010, Matthews et al., 2018), yet their experiences are less often studied (Allard et al., 2011, O’Brien et al., 2015). Given sex differences in exposure and responses to other forms of service-connected trauma (e.g., Maguen et al., 2012, MacGregor et al., 2020), more research examining exposure to MST simultaneously among male and female service members is needed to evaluate relative prevalence and potential sex differences in types of MST experienced and sequelae. Accordingly, the present research will examine sex differences in MST prevalence, types of MST experienced, and the relation between MST and risk for alcohol misuse.
National Guard and Reserve Components
While the extant U.S. military literature has relied heavily on active-duty service members and VHA-using veteran samples, the present study utilized a sample of USAR/NG. Reserve and National Guard components are underrepresented overall in the military-related research literature, despite comprising approximately 37% of the U.S. Armed Forces (U.S. Department of Defense, Defense Manpower Data Center, June 2022). Additionally, they are at higher risk for alcohol misuse (Cohen et al., 2015, Jacobson et al., 2008) and overall need for mental health treatment (Milliken et al., 2007) than their active-duty counterparts. This elevated risk may be due to their more limited access to DoD and VA healthcare benefits (U.S. Department of Veterans Affairs, VETERANS BENEFITS ADMINISTRATION, 2012), less access to support services, and stress due to repeated transitions between military and civilian roles (Milliken et al., 2007). These factors also have the potential to exacerbate MST-related sequelae.
Present Research
To fill important gaps in this literature, the present research aims to: 1) estimate prevalence and types of MST experienced at any point during military service among both female and male service members; 2) examine relations between MST history and current alcohol consumption, heavy drinking frequency, and alcohol problems; and 3) examine sex differences in these experiences and outcomes. Aim 1 is descriptive. For Aim 2, we hypothesized that MST history would be associated with greater alcohol consumption, more frequent heavy drinking, and greater alcohol problems. For Aim 3, we hypothesized that females would report higher MST history rates than males. However, as prior research is mixed regarding sex differences in MST-related health sequelae, we make no specific predictions regarding differences in alcohol-related correlates.
Materials and Methods
Participants and Procedure
Data were drawn from Operation: SAFETY (Soldiers And Families Excelling Through the Years), an ongoing longitudinal study examining health and well-being among USAR/NG soldiers and their spouses/partners. Participants were recruited from units across New York State. Eligible participants included: (a) couples who were married or living as if married, (b) one partner was a current USAR/NG soldier at the time of study enrollment, (c) the soldier was 18 to 45 years of age, (d) both partners spoke and understood English, (e) both partners were willing and able to participate in the study, and (f) both partners had at least one alcoholic beverage in the previous year. The original study included a baseline survey and two annual follow-up waves. Participants were assured their responses would not be shared with their partners, nor would the military be able to know about their participation. The protocol was approved by the University at Buffalo Institutional Review Board, Army Human Research Protections Office, Office of the Chief, Army Reserve, and Adjutant General of the National Guard. Additional study details have been published previously (Fillo et al., 2018).
The parent study sample at baseline included current service members and spouses/partners (N = 411 couples/822 individuals). Of these, 478 individuals were current or previous service members, due to 67 dual-military couples (current or previous service). The analytic sample for the present analyses comprised 404 service members (334 male, 70 female) who (a) completed questions at 1-year and/or 2-year follow-ups about MST experienced at any point during military service, or (b) reported deployment-related MST at any study wave. Demographic characteristics for the analytic sample at baseline are presented in Table 1.
Table 1.
Demographic characteristics of analytic sample at study baseline (n = 404)
| Variable | Males n = 334 % (n) or M(SD) |
Females n = 70 % (n) or M(SD) |
|---|---|---|
| Age | 31.8 (6.6) | 29.9 (5.3) |
| Race\Ethnicity | ||
| Non-Hispanic White | 79.9% (267) | 80.0% (56) |
| Non-Hispanic Black | 6.3% (21) | 2.9% (2) |
| Hispanic | 7.8% (26) | 7.1% (5) |
| Other | 4.2% (14) | 7.1% (5) |
| No Response | 1.8% (6) | 2.9% (2) |
| Education | ||
| <HS-HS Grad | 14.4% (48) | 4.3% (3) |
| Some College | 56.6% (189) | 52.9% (37) |
| College + | 29.0% (97) | 42.9% (30) |
| Relationship Status | ||
| Married | 66.5% (222) | 61.4% (43) |
| Cohabitating | 33.5% (112) | 38.6% (27) |
| Income (median) | $60,000 to $79,999 | $40,000 - $59,999 |
| Military Service History | ||
| Years Served | 10.0 (6.3) | 7.8 (4.9) |
| Ever Deployed | ||
| Yes | 65.9% (220) | 42.9% (30) |
| No | 34.1% (114) | 57.1% (40) |
| Number of Deployments | 1.7 (0.9) | 1.4 (0.5) |
Descriptive statistics for income correspond to the median income bracket endorsed by participants.
Measures
MST history.
MST history was a composite of multiple MST exposure assessments across waves. MST was measured at baseline, 1-year follow-up, and 2-year follow-up using the 8-item sexual harassment subscale of the Deployment Risk and Resilience Inventory-2 (DRRI-2; Vogt et al., 2012). This subscale examines service members’ experience of unwanted sexual contact or verbal conduct of a sexual nature during deployments (see Figure 1 for item wording). This was administered in its original form at baseline to assess MST experienced during service members’ most recent deployment, and at 1-year and 2-year follow-ups to assess MST experienced during deployment since the previous wave, as applicable. Additionally, the measure was adapted to assess any MST experienced during military service more generally—not limited to deployment—over the prior year, as well as outside of the past year. Wording of all items remained the same; only the response timeframe and context changed. The adapted version was administered to all participants with current or previous military service at 1-year and 2-year follow-ups. To create an indicator corresponding to VHA criteria for a positive MST screen, responses were aggregated across waves into a binary measure of MST history (1 = any, 0 = none), as well as binary variables for each type of MST assessed.
Figure 1.
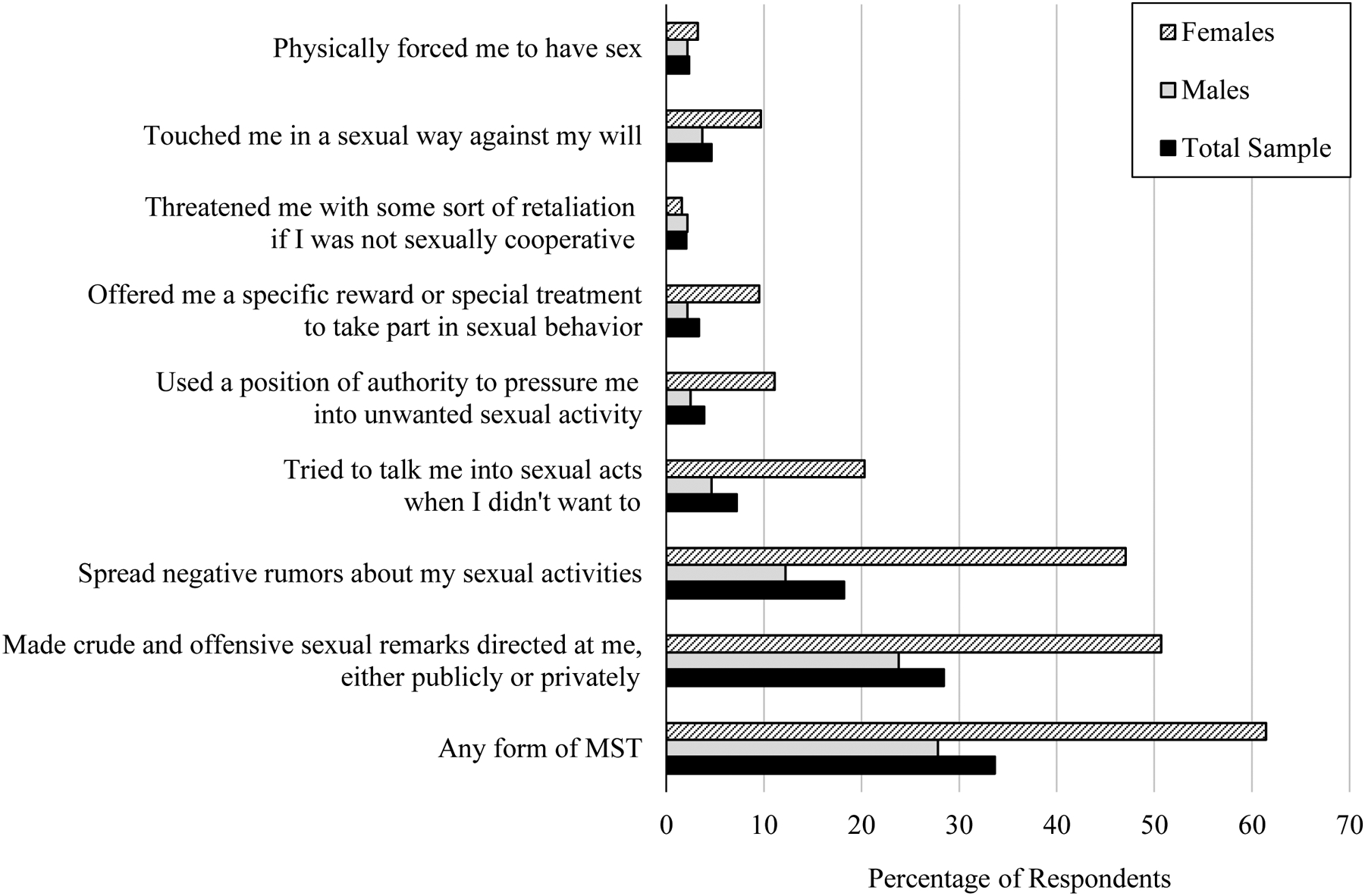
Prevalence of types of MST experienced by female and male U.S. Army Reserve and National Guard service members at any point during military service. Brackets and stars indicate differences in prevalence between males and females within each type of MST. *p < .05. **p < .01. MST = Military Sexual Trauma
Total alcohol consumption.
Total alcohol consumption over the past year was measured with an adapted version of the Alcohol Quantity-Frequency Index (QFI; Straus and Bacon, 1953). This is computed by multiplying two items together. The first item assessed frequency of typical alcohol consumption on a 9-point scale from Did not drink beer, wine, wine coolers, or hard liquor in the last 12 months to Every day. For those who endorsed any drinking, a second item assessed typical quantity consumed on each occasion over the past 12 months. Typical quantity was measured on a 10-point scale from 1 drink to 18 or more drinks. Drinking frequency responses were converted to the total number of drinking days in the past year,1 and quantity responses were converted to number of drinks per drinking occasion, prior to multiplying the items. Resulting values represent total number of drinks consumed over the past year.
Heavy drinking frequency.
In line with previous research (Homish and Leonard, 2007), past year heavy drinking frequency was measured as the maximum report of two items: 1) frequency of five or more drinks (males)/four or more drinks (females) in a single setting, and 2) frequency of getting drunk. Responses were rescaled to number of heavy drinking instances per year.1
Alcohol problems.
Alcohol problems were measured using the 10-item Alcohol Use Disorders Identification Test (AUDIT; Babor and Del Boca, 1992). Example items include “have you or someone else been injured because of your drinking” and “how often during the last year have you had a feeling of guilt or remorse after drinking.” Each item is rated from 0 (Never) to 4 (Daily or almost daily). Total scores are summed across items (range: 0 – 40; α = .78).
Covariates.
Participant age and PTSD symptoms were also assessed and included in models as covariates. PTSD symptoms were assessed using the 20-item, self-report PTSD Checklist (PCL-5; Bovin et al., 2016). Each item is rated from 0 (Not at all) to 4 (Extremely). Responses are summed across items, with higher total scores indicating greater PTSD symptom severity (range: 0 – 80; α = .95).
Data Analytic Plan
Descriptive statistics were computed to characterize focal variables. Prevalence of MST history and each type of MST was calculated for the total analytic sample and for males and females separately. Tests of two proportions were used to examine sex differences in overall MST history prevalence and each specific type of MST.
Actor-Partner Interdependence Modeling (APIM) was used for inferential analyses to appropriately account for the fact that the analytic sample included couples in which both spouses/partners had military history. APIM is a dyadic data analysis technique that models the non-independence that naturally exists between individuals in interpersonal relationships (Kenny et al., 2006). Couple members are nested within dyad, which is treated as the unit of analysis.
Distributions of alcohol variables were examined prior to conducting focal analyses. As is often the case with count variables in the context of substance use, all of the alcohol variables demonstrated positive skew. To properly account for the distribution of these variables, focal inferential models were conducted in Stata version 17.0 (StataCorp, 2021) using multilevel mixed-effects negative binomial regression. For all models, adjusted risk ratios (aRR) are reported to provide effect sizes and aid interpretability of results. Analyses examined the extent to which MST history was associated with total alcohol consumption, heavy drinking frequency, and alcohol problems, assessed at the 2-year follow-up wave. All models included participant sex (−0.5 = male, 0.5 = female). All models controlled for participant age (grand mean-centered) and PTSD symptoms (grand mean-centered). PTSD symptoms were included as a covariate because it is highly comorbid with substance use disorders and is a particularly salient issue among military personnel (Debell et al., 2014). Because the measure used to assess alcohol problems (AUDIT) contains consumption-related items, models predicting alcohol problems additionally controlled for overall alcohol consumption (QFI). For all alcohol variables, a second set of models included the interaction between MST history and participant sex to examine potential sex differences. All models were calculated using robust standard errors.
Results
Preliminary Analyses
Descriptive statistics and correlations, broken down by sex, are presented in Table 2 . On average, over the past year, participants reported consuming 4.3 drinks per week (M = 221.3 drinks/year, SD = 335.1) and heavy drinking 1.6 times per month (M = 18.9 times/year, SD = 40.5), with 10.7% reporting drinking heavily weekly or more. The average AUDIT score (M = 4.4, SD = 4.0) fell below the established cutoff (AUDIT ≥ 8) for clinically significant harmful drinking, but 14.4% of the sample scored 8 or higher.
Table 2.
Descriptive statistics and correlations among focal variables.
| 1 | 2 | 3 | 4 |
Males M (SD) or % (n) |
Females M (SD) or % (n) |
|
|---|---|---|---|---|---|---|
| 1. MST History (0/1) | - | .12* | .14* | .22*** | 27.8% (93) | 61.4% (43) |
| 2. Total Alcohol Consumption | −.02 | - | .65*** | .67*** | 234.1 (347.5) | 157.6 (258.0) |
| 3. Heavy Drinking Frequency | −.15 | .77*** | - | .65*** | 18.7 (39.7) | 19.7 (44.9) |
| 4. Alcohol Problems | .02 | .81*** | .67*** | - | 4.5 (4.1) | 3.7 (3.6) |
p < .05.
p < .001.
MST = Military Sexual Trauma. Correlations among variables for male service members presented above the diagonal. Correlations among variables for female service members presented below the diagonal. Relations between continuous variables are Pearson correlations. Correlations involving a binary variable (i.e., MST history) are point-biserial correlations.
Focal Analyses
MST prevalence and types.
Figure 1 depicts prevalence of any MST history and each specific type assessed. This includes average prevalence for the total sample, as well as broken down separately for males and females. MST history was common; 33.7% of service members reported experiencing some form of MST during the course of military service. The most common types reported were being the target of crude or offensive sexual remarks (28.4%, n = 114) and others spreading negative rumors about one’s sexual activities (18.2%, n = 72). Additionally, 2.3% (n = 9) reported being physically forced to have sex. Female service members reported more than double the rate of MST (61.4%) than did male service members (27.8%; z = −5.41, p <.001). Female service members also reported significantly higher rates of most types of MST. The two exceptions were for threats of retaliation if not sexually cooperative (z = 0.27, p = 0.782) and being physically forced to have sex (z = −0.51, p = 0.613).
Total alcohol consumption.
For the models predicting total alcohol consumption, results revealed a significant interaction between MST history and service member sex (see Table 3). Follow-up analyses (see Figure 2) revealed that, for male service members, MST history was associated with consuming 70% more drinks per year (aRR = 1.70, p = 0.004), compared to male service members with no MST history. However, there was no relation between MST history and drinks per year for female service members (aRR = 0.61, p = .193). Among those with MST history, male service members’ total alcohol consumption was more than triple that of female service members (aRR = 0.32, p < .001). There were no sex differences in total alcohol consumption among those with no MST history (aRR = 0.88, p = .664).
Table 3.
Multilevel negative binomial regression models examining the relation between MST history and alcohol use variables at study wave 3
| Total alcohol consumption | Heavy drinking frequency | Alcohol problems | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Main effects model | Interaction model | Main effects model | Interaction model | Main effects model | Interaction model | |||||||
| Variable | aRR | 95% CI | aRR | 95% CI | aRR | 95% CI | aRR | 95% CI | aRR | 95% CI | aRR | 95% CI |
| Intercept | 78.12*** | [60.24, 101.31] | 96.13*** | [71.75, 128.79] | 10.03*** | [7.63, 13.18] | 12.81*** | [9.36, 17.54] | 3.38*** | [3.05, 3.74] | 3.67*** | [3.28, 4.11] |
| MST History | 1.37† | [0.96, 1.95] | 1.02 | [0.65, 1.59] | 1.47* | [1.04, 2.07] | 1.02 | [0.66, 1.56] | 1.20* | [1.05, 1.38] | 1.07 | [0.90, 1.26] |
| Age | 1.00 | [0.97, 1.02] | 1.00 | [0.98, 1.03] | 0.99 | [0.96, 1.02] | 0.99 | [0.96, 1.03] | 0.99** | [0.98, 0.99] | 0.99* | [0.98, 0.99] |
| PTSD Symptoms | 1.03*** | [1.02, 1.04] | 1.03*** | [1.02, 1.04] | 1.04*** | [1.03, 1.05] | 1.04*** | [1.03, 1.05] | 1.01*** | [1.01, 1.02] | 1.01*** | [1.01, 1.02] |
| Alcohol Consumption | - | - | - | - | - | - | - | - | 1.01*** | [1.01, 1.01] | 1.01*** | [1.01, 1.01] |
| Sex | 0.50** | [0.33, 0.75] | 0.88 | [0.50, 1.55] | 0.79 | [0.50, 1.25] | 1.48 | [0.78, 2.80] | 0.84† | [0.71, 1.01] | 1.05 | [0.83, 1.32] |
| MST history × sex | - | - | 0.36** | [0.17, 0.76] | - | - | 0.30** | [0.12, 0.74] | - | - | 0.69* | [0.49, 0.97] |
p < .10.
p < .05.
p < .01.
p < .001.
aRR = Adjusted Risk Ratio. 95% CI = 95% Confidence Interval. MST = Military Sexual Trauma. PTSD = Posttraumatic Stress Disorder. Sex variable is effect coded (-0.5 = male, 0.5 = female).
Figure 2.

Interactive effects of MST history and service member sex in model of total alcohol consumption. Brackets and stars indicate significant differences between participant subgroups. **p < .01. ***p < .001. MST = Military Sexual Trauma
Heavy drinking frequency.
For the models predicting heavy drinking frequency, results revealed a significant interaction between MST history and service member sex (see Table 3). Follow-up analyses (see Figure 3) revealed that, for male service members, MST history was associated with 86% more heavy drinking instances per year (aRR = 1.86, p = .002), compared to male service members with no MST history. However, there was no relation between MST history and heavy drinking frequency for female service members (aRR = 0.56, p = .150). Among those with MST history, male service members engaged in heavy drinking at more than double the rate of female service members (aRR = 0.44, p = .010). There were no sex differences in heavy drinking frequency among those with no MST history (aRR = 1.48, p = .227).
Figure 3.
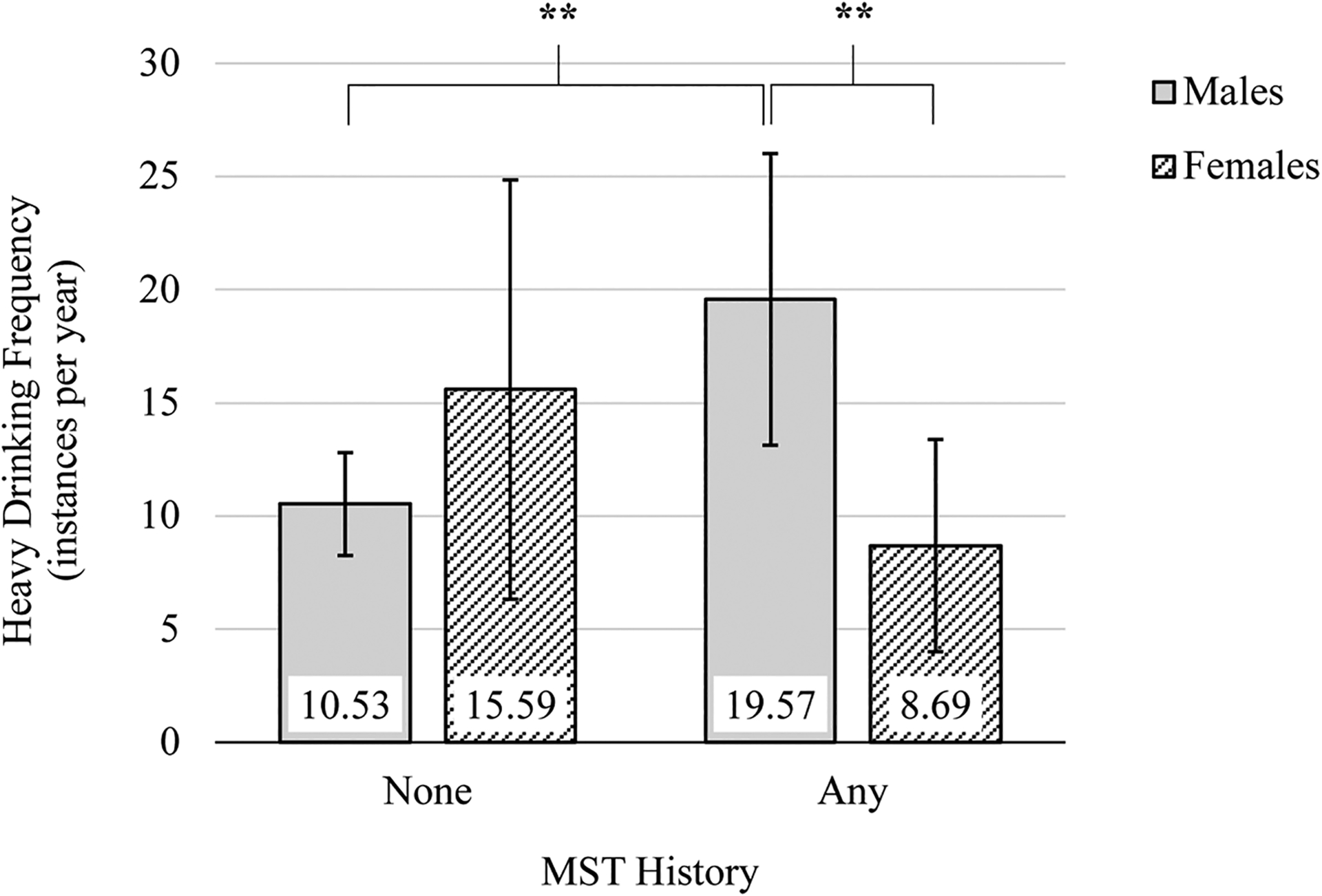
Interactive effects of MST history and service member sex in model of heavy drinking frequency. Brackets and stars indicate significant differences between participant subgroups. **p < .01. MST = Military Sexual Trauma
Alcohol use problems.
For the models predicting alcohol use problems, results revealed an interaction between MST and service member sex (see Table 3). Follow-up analyses (see Figure 4) revealed that, for male service members, MST history was associated with significantly more alcohol problems (aRR = 1.28, p = .001) compared to male service members with no MST history. However, there was no relation between MST history and alcohol problems for female service members (aRR = 0.88, p = .427). Among those with MST history, male service members experienced more alcohol problems than did female service members (aRR = 0.72, p = .009). There were no sex differences in alcohol problems among those with no MST history (aRR = 1.05, p = .709).
Figure 4.

Interactive effects of MST history and service member sex in model of alcohol problems. Brackets and stars indicate significant differences between participant subgroups. **p < .001. AUDIT alcohol use disorders identification test; MST = Military Sexual Trauma
Discussion
The present study sought to advance the literature on MST by examining: (1) prevalence and types of MST experienced throughout military service among USAR/NG service members, (2) relations between MST history and alcohol misuse and alcohol problems in this population, and (3) sex differences in MST exposure and alcohol-related outcomes. Results revealed that approximately 1 in 3 service members had experienced MST at some point during the course of their military service. However, there were sex differences in overall MST history prevalence, prevalence of specific types experienced, and the relation between MST and alcohol variables. Female service members (61.4%) reported MST history at higher rates than did males (27.8%). These differences held across most types of MST experiences, but the overall pattern of experiences for male and female service members was similar. Additionally, there were no sex differences for threats of retaliation and forced sex, but it is worth noting that these were the least common types of MST reported in the sample.
MST prevalence estimates vary widely in the literature (0.4% - 71%) due to variations across studies in the definition of MST being used, assessment methods, context or time period examined, and type of sample (Suris and Lind, 2008, Wilson, 2018). Additionally, research on MST is hampered by underreporting (Morral et al., 2015, U.S. Department of Defense, 2018). Victims of sexual assault are typically reluctant to report the events (Morgan and Thompson, October 2021). This is especially true in the case of MST reporting due to service members’ fears of retaliation as well as potential punishment under UCMJ for other factors at play at the time of the event (e.g., substance use, adultery; Morral et al., 2015, U.S. Department of Defense, 2021). It is estimated that only 15 to 33 percent of sexual assaults in the military are officially reported (Morral et al., 2015, U.S. Department of Defense, 2018). Together, these factors hinder a more complete understanding of prevalence, types, and consequences of MST.
The MST history prevalence found in the present study is at the high end among studies in the literature using self-administered surveys (e.g., 17%−30%), and higher than would be expected from a sample not seeking treatment or VA benefits (Suris and Lind, 2008). In particular, the rate of MST history reported by male service members in the present sample (27.8%) was considerably higher than the mean prevalence reported in the literature (3.9%; Wilson, 2018). Participants may have been more comfortable reporting their experiences in the present study due to the self-administered, confidential nature of the research, and the fact that it was conducted outside of the purview of the DoD and VHA. Indeed, recent research found that male veterans’ endorsement of MST history was 11 times higher when assessed using a self-administered survey—in fact, the same measure used in the present research—compared to the standard VHA screen (Bovin et al., 2019). Given that male victims are more reluctant to endorse MST exposure and seek related care, ensuring privacy around screening is essential for accurate assessment of MST history (Bovin et al., 2019, Wilson, 2018).
The present findings also revealed that MST history was a risk factor for greater overall alcohol consumption, heavy drinking frequency, and alcohol problems. This was particularly true for male service members. Male service members with MST history reported approximately 70 % higher current overall alcohol consumption and 86 % more frequent heavy drinking than did males without MST history. Accordingly, male service members with MST history also reported greater alcohol problems. Among service members with MST history, males reported higher alcohol consumption, more frequent heavy drinking, and more alcohol problems than did females. In contrast, results demonstrated no differences in any of the analyses for women based on MST history, nor differences in any of the alcohol variables between males and females without MST history. The present findings are consistent with the patterns found in our prior work on MST during a single prior deployment and subsequent alcohol use among male service members (Fillo et al., 2018). Furthermore, the present research builds upon that work by suggesting that the link between MST and alcohol misuse and related problems exists for MST more generally—not just within the context of deployment. However, they also suggest that these patterns may be specific to male service members.
Elevated alcohol use is a widely recognized health problem among recent service members, particularly within reserve and National Guard components (Jacobson et al., 2008, Seal et al., 2011). And male service members report significantly higher overall consumption and hazardous/disordered drinking than do female service members (Meadows et al., 2018). The present findings reveal that MST history may further exacerbate heavy drinking among a population already at considerable risk. Whereas prior research has shown relations between MST and greater odds of a substance use disorder diagnosis among VHA patients (Kimerling et al., 2010, Beckman et al., 2021), the present findings demonstrate that these relations extend to multiple indicators of alcohol misuse and related problems among male service members even in a non-clinical, non-treatment-seeking sample.
These drinking patterns are also concerning because they may put service members at increased risk for revictimization. Consuming alcohol has been linked to increased risk for sexual victimization and perpetration (see Testa and Livingston, 2018, Abbey et al., 2014). Indeed, the 2014 RAND Military Workplace Study found that one third of military sexual assault victims reported that they had been drinking prior to the assault (Morral et al., 2015). Furthermore, evidence suggests that alcohol use is a risk factor for revictimization (see Classen et al., 2005 for a review). In civilian populations, heavy alcohol use has been found to mediate the relation between victimization and revictimization (Testa et al., 2010, Norris et al., 2021). Therefore, not only are the observed patterns concerning in their own right due to the potential consequences for the health and well-being of service members and their families, but also because they have the potential to create a vicious cycle whereby the effects of MST may increase risk for experiencing MST again in the future. There has been growing attention to examining risk factors for sexual revictimization among service members and veterans in recent years (e.g., Scoglio et al., 2022, Tirone et al., 2020), but further examination of male victims’ risk and the specific role of alcohol misuse is needed.
Taken together, findings provide valuable epidemiological information about the prevalence of MST, sex differences in these experiences, and the extent to which MST exposure is a risk factor for alcohol misuse. In examining MST and related risk at the population level, the present research takes a different approach compared to more clinically-oriented MST research. Whereas results demonstrate alarming prevalence of MST for female and male service members, simply experiencing these events does not necessarily mean all such individuals will have a trauma response or require treatment. Indeed, greater understanding of factors that predict more or less severe responses to the same MST experiences is an important direction for future research. However, it is worth noting that the size of the effects found in the present research suggest that any exposure to MST serves as a risk factor for alcohol misuse among male service members, irrespective of individual differences in response to those events across persons (i.e., PTSD symptoms). Furthermore, the fact that some individuals are less affected by these experiences in no way diminishes the severity of the problem or the fact that sexual harassment and sexual assault represent a pressing concern within the U.S. Armed Forces.
Clinical Implications
The present research demonstrates that both female and male reserve and National Guard service members are at risk for MST victimization, and these experiences are not restricted to deployment. Attention to MST, particularly in female service members, grew from their increasing role in the first Gulf War (Wolfe et al., 1998). Yet, our findings illustrate that male service members are also at considerable risk for MST. In fact, because males make up the vast majority of military personnel, they constitute approximately 60 % of MST victims annually (Morral et al., 2015). Therefore, prevention efforts should be developed with the understanding that the experience and negative effects of MST are relevant to all service members—female and male—in various contexts of military service and across all components.
Additionally, it is important to understand sex differences in the nature of these experiences and potential sequelae, so that prevention and intervention efforts can be targeted appropriately. Indeed, present findings highlight sex differences in prevalence of MST and its relation to alcohol misuse and alcohol problems. Female service members were more likely to have experienced most forms of MST, except for forced sex and threats of retaliation. However, MST history appeared to put male service members at considerably higher risk for heavier and more hazardous alcohol use, as well as alcohol problems. Whereas previous research on sex differences in the relative strength of relations between MST and alcohol use is mixed, the lack of any relation between MST and alcohol use variables for females in this sample was still somewhat surprising. Although speculative, the stronger effect among males may suggest they are more likely to drink to cope with the stress of their experiences (Dolan and Ender, 2008). Perhaps female victims’ struggles to cope manifests in different ways (e.g., depression, anxiety, or other forms of internalizing symptoms; Maguen et al., 2012). Indeed, recent research found that the increased risk for PTSD and depression associated with MST was greater among female veterans compared to males (Tannahill et al., 2020). This is just one possibility; the explanation behind sex differences in coping with MST is likely multifaceted. It is also possible that the lack of association between MST and alcohol variables in our female sample may have been due to low power. Given the growing role of female service members in the U.S. Armed Forces, the present findings provide important information for helping to meet the needs of current and future generations of service members and veterans. Future work should examine resiliency and coping related to MST, including potential sex differences in these processes.
As the recent DoD-wide policy changes related to MST continue to be implemented, it is reasonable to expect that victims will feel more comfortable reporting and seeking related care. However, ongoing changes in patterns of healthcare utilization among service members and veterans indicate that greater understanding of MST risk and related sequelae will particularly be important for civilian healthcare providers. While the VHA currently conducts universal MST screening for all veterans seen for care, this approach misses numerous veterans, including many former National Guard and reserve, who cannot receive VHA services due to eligibility requirements (U.S. Department of Veterans Affairs, VETERANS BENEFITS ADMINISTRATION, 2012). Additionally, more than half of eligible veterans do not utilize VHA benefits (U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics, 2020). Even among eligible veterans who do utilize VHA benefits, the VA Choice Act (2014) led to an increase in veterans’ access to and utilization of civilian healthcare providers (Rose et al., 2021). This use is expected to continue to grow with the passing of the VA MISSION Act (2018), which further expands veterans’ ability to seek care outside the VHA system. However, civilian healthcare providers do not consistently ask about military service history and may need support in identifying military-related health concerns, such as MST (Vest et al., 2018, Vest et al., 2019). Taken together, these changes underscore the importance of civilian providers asking patients about military service, screening for MST among other common service-connected issues, and being knowledgeable about health-related risks for MST victims.
Strengths and Limitations
Strengths of the present work include using an inclusive measure of MST capturing the full range of MST experiences that correspond to VHA criteria, as well as broadening the scope of exposure contexts in which these experiences are examined (i.e., entire service history). Given that duties and service experiences can change from year to year—particularly in reserve and National Guard components—this approach allows for more comprehensive evaluation of MST exposure in this large, important, and often understudied population. Using self-report, confidential surveys administered outside the DoD or VHA likely increased participant comfort with reporting such sensitive information (Bovin et al., 2019). Furthermore, simultaneously investigating the types, prevalence, and correlates of MST in both female and male service members allowed for examination of sex differences, which can have important implications for appropriately targeting prevention, screening, and treatment efforts.
The present research is not withstanding of limitations. This study examined MST experienced at any point during military service, but we were not able to ascertain time since the event(s) or other features of the event(s). We also do not have information regarding participants’ alcohol use prior to MST exposure or the start of service. Each of these factors may have implications for the severity of sequelae. Together, they also mean that we cannot make definitive conclusions about the direction of causality. Indeed, relations between MST and alcohol misuse are likely reciprocal. Results likely underestimate lifetime prevalence, as the sample included current service members who may still experience MST in the future. Additionally, eligibility criteria for the parent study included being married or cohabiting (as if married). This may limit the generalizability of the present findings. However, it is worth noting that approximately half (48%) of US service members are married (U.S. Department of Defense, Office of the Deputy Assistant Secretary of Defense for Military Community And Family Policy, 2021), with a further 10–20% living with a non-marital partner (U.S. Census Bureau, 2021). The use of only male-female couples in the present analyses may also limit the generalizability of the findings with respect to LGBTQIA+ service members. Finally, due to low overall rates of certain experiences, we were not able to examine whether different types of MST had stronger links to alcohol misuse and related problems compared to others, nor sex differences in those relations. These are important questions for future research.
Conclusions
The present research revealed that approximately 1 in 3 USAR/NG soldiers experience MST at some point during military service. In turn, this MST exposure is associated with greater risk for higher overall alcohol consumption, more frequent heavy drinking, and more alcohol problems among male service members. Findings underscore the need for universal prevention, screening, and intervention for female and male, current and previous, service members across all branches and components of the U.S. Armed Forces. Additionally, findings highlight the need for these efforts to be sensitive to sex differences in the nature, prevalence, and health-related consequences of MST, so care can be better matched with victims’ needs. Although MST is distinct from other types of trauma commonly experienced by service members (e.g., combat exposure, severe injury), it is associated with some of the same negative sequelae. Thus, the present results call attention to MST as an important and prevalent experience among service members, and one that warrants greater study alongside more traditional notions of service-connected trauma.
Acknowledgments
Research reported in this manuscript was supported by the National Institute on Drug Abuse [R01DA034072; PI: GGH] and by the National Center for Advancing Translational Sciences [UL1TR001412; University at Buffalo]. Preparation of this article was partially supported by the National Institute on Alcohol Abuse and Alcoholism [T32AA007583; PIs: Kenneth E. Leonard, GGH] and [K01AA027547; PI: JF] in support of Jennifer Fillo, and by the National Institute on Drug Abuse [T32DA007292; PI: Brion Maher] in support of Erin M. Anderson Goodell. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no conflicts of interest to declare.
Overall alcohol consumption frequency and heavy drinking frequency were rescaled from their original Likert responses into count variables reflecting the number of instances per year represented by each scale point, as follows: Every day (1 × 365 days = 365), Almost every day ([(5 + 6) / 2] × 52 weeks = 286), 3–4 times a week ([(3 + 4) / 2] × 52 weeks = 182), 2 times a week (2 × 52 weeks = 104), Once a week (1 × 52 weeks = 52), 2–3 times per month ([(2 + 3) / 2] × 12 months= 30), About once a month (1 × 12 months = 12), Less than once a month, but at least once in the past year ([11 + 1] / 2 = 6), Did not drink beer, wine, wine coolers, or hard liquor in the last 12 months (0). This approach was adopted to more accurately reflect the count nature of the constructs, and it enabled parametric analysis of overall alcohol consumption and heavy drinking frequency responses by putting them on an interval scale.
References
- ABBEY A, WEGNER R, WOERNER J, PEGRAM SE & PIERCE J 2014. Review of survey and experimental research that examines the relationship between alcohol consumption and men’s sexual aggression perpetration. Trauma Violence Abuse, 15, 265–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ALLARD CB, NUNNINK S, GREGORY AM, KLEST B & PLATT M 2011. Military sexual trauma research: A proposed agenda. Journal of Trauma & Dissociation, 12, 324–345. [DOI] [PubMed] [Google Scholar]
- AMES G & CUNRADI C 2004. Alcohol use and preventing alcohol-related problems among young adults in the military. Alcohol Research & Health, 28, 252–257. [Google Scholar]
- AUSTIN LJ (July 2, 2021a). Department of Defense actions and implementation guidance to address sexual assault and sexual harassment in the military. US Department of Defense. Available: https://media.defense.gov/2021/Jul/02/2002755437/−1/−1/0/IRC-FULL-REPORT-FINAL-1923-7-1-21.PDF. [Accessed 22nd February 2022] [Google Scholar]
- AUSTIN LJ (September 22, 2021b). Commencing DoD actions and implementation to address sexual assault and sexual harassment in the military. US Department of Defense. Available: https://www.armyresilience.army.mil/ard/images/pdf/DOD-ACTIONS-AND-IMPLEMENTATION-TO-ADDRESS-SEXUAL-ASSAULT-AND-SEXUAL-HARRASSMENT-IN-THE-MILITARY.PDF. [Accessed 22nd February 2022] [Google Scholar]
- BABOR TF & DEL BOCA FK 1992. Just the facts: Enhancing measurement of alcohol consumption using self-report methods. In: LITTEN RZ & ALLEN JP (eds.) Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press. [Google Scholar]
- BECKMAN KL, WILLIAMS EC, HEBERT PL, FROST MC, RUBINSKY AD, HAWKINS EJ, LITTMAN AJ & LEHAVOT K 2021. Associations among military sexual trauma, opioid use disorder, and gender. American Journal of Preventive Medicine, 62, 377–386. [DOI] [PubMed] [Google Scholar]
- BLAKEY SM, TSAI J & ELBOGEN EB 2021. Drinking to cope with posttraumatic stress: A nationally representative study of men with and without military combat experience. Journal of Dual Diagnosis, 17, 101–112. [DOI] [PubMed] [Google Scholar]
- BOVIN MJ, BLACK SK, KLEIMAN SE, BROWN ME, BROWN LG, STREET AE, ROSEN RC, KEANE TM & MARX BP 2019. The impact of assessment modality and demographic characteristics on endorsement of military sexual trauma. Women’s Health Issues, 29, S67–S73. [DOI] [PubMed] [Google Scholar]
- BOVIN MJ, MARX BP, WEATHERS FW, GALLAGHER MW, RODRIGUEZ P, SCHNURR PP & KEANE TM 2016. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28, 1379–1391. [DOI] [PubMed] [Google Scholar]
- BURNAM MA, STEIN JA, GOLDING JM, SIEGEL JM, SORENSON SB, FORSYTHE AB & TELLES CA 1988. Sexual assault and mental disorders in a community population. Journal of Consulting and Clinical Psychology, 56, 843–850. [DOI] [PubMed] [Google Scholar]
- CLASSEN CC, PALESH OG & AGGARWAL R 2005. Sexual revictimization: A review of the empirical literature. Trauma, Violence, & Abuse, 6, 103–129. [DOI] [PubMed] [Google Scholar]
- COHEN GH, FINK DS, SAMPSON L & GALEA S 2015. Mental health among reserve component military service members and veterans. Epidemiologic Reviews, 37, 7–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DEBELL F, FEAR NT, HEAD M, BATT-RAWDEN S, GREENBERG N, WESSELY S & GOODWIN L 2014. A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49, 1401–1425. [DOI] [PubMed] [Google Scholar]
- DOLAN CA & ENDER MG 2008. The coping paradox: Work, stress, and coping in the U.S. Army. Military Psychology, 20, 151–169. [Google Scholar]
- FILLO J, HEAVEY SC, HOMISH DL & HOMISH GG 2018. Deployment-related military sexual trauma predicts heavy drinking and alcohol problems among male reserve and National Guard soldiers. Alcoholism: Clinical and Experimental Research, 42, 111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HARWOOD HJ, ZHANG Y, DALL TM, OLAIYA ST & FAGAN NK 2009. Economic implications of reduced binge drinking among the military health system’s TRICARE Prime plan beneficiaries. Military Medicine, 174, 728–736. [DOI] [PubMed] [Google Scholar]
- HAWN SE, CUSACK SE & AMSTADTER AB 2020. A systematic review of the self-medication hypothesis in the context of posttraumatic stress disorder and comorbid problematic alcohol use. Journal of Traumatic Stress, 33, 699–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOMISH GG & LEONARD KE 2007. The drinking partnership and marital satisfaction: The longitudinal influence of discrepant drinking. Journal of Consulting and Clinical Psychology, 75, 43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- INDEPENDENT REVIEW COMMISSION ON SEXUAL ASSAULT IN THE MILITARY 2021. Hard truths and the duty to change: Recommendations from the Independent Review Commission on Sexual Assault in the Military. Available: https://media.defense.gov/2021/Jul/02/2002755437/−1/−1/0/IRC-FULL-REPORT-FINAL-1923-7-1-21.PDF/IRC-FULL-REPORT-FINAL-1923-7-1-21.PDF. [Accessed 2nd February 2022]
- JACOBSON IG, RYAN MA, HOOPER TI, SMITH TC, AMOROSO PJ, BOYKO EJ, GACKSTETTER GD, WELLS TS & BELL NS 2008. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA, 300, 663–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KENNY DA, KASHY DA & COOK WL 2006. Dyadic data analysis, New York, NY, Guilford Press. [Google Scholar]
- KIMERLING R, GIMA K, SMITH MW, STREET A & FRAYNE S 2007. The Veterans Health Administration and military sexual trauma. American Journal of Public Health, 97, 2160–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KIMERLING R, STREET AE, PAVAO J, SMITH MW, CRONKITE RC, HOLMES TH & FRAYNE SM 2010. Military-related sexual trauma among Veterans Health Administration patients returning from Afghanistan and Iraq. American Journal of Public Health, 100, 1409–1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KLINGENSMITH K, TSAI J, MOTA N, SOUTHWICK SM & PIETRZAK RH 2014. Military sexual trauma in US veterans: Results from the National Health and Resilience in Veterans study. Journal of Clinical Psychiatry, 75, e1133–e1139. [DOI] [PubMed] [Google Scholar]
- KONKOLŸ THEGE B, HORWOOD L, SLATER L, TAN MC, HODGINS DC & WILD TC 2017. Relationship between interpersonal trauma exposure and addictive behaviors: A systematic review. BMC Psychiatry, 17, 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MACGREGOR AJ, DYE JL & DOUGHERTY AL 2020. Gender differences in mental health screening outcomes among US Marines in combat support occupations. Womens Health Issues, 30, 470–476. [DOI] [PubMed] [Google Scholar]
- MAGUEN S, LUXTON DD, SKOPP NA & MADDEN E 2012. Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. Journal of Psychiatric Research, 46, 311–316. [DOI] [PubMed] [Google Scholar]
- MATTHEWS M, FARRIS C, TANKARD M & DUNBAR MS 2018. Needs of male sexual assault victims in the U.S. Armed Forces. Santa Monica, CA: RAND Corporation. Available: https://www.rand.org/pubs/research_reports/RR2167.html. [PMC free article] [PubMed] [Google Scholar]
- MEADOWS SO, ENGEL CC, COLLINS RL, BECKMAN RL, CAFALU M, HAWES-DAWSON J, DOYLE M, KRESS AM, SONTAG-PADILLA L, RAMCHAND R & WILLIAMS KM 2018. 2015 Department of Defense Health Related Behaviors Survey. Santa Monica, CA: RAND Corporation. Available: https://www.rand.org/pubs/research_reports/RR1695.html. [PMC free article] [PubMed] [Google Scholar]
- MILLIKEN CS, AUCHTERLONIE JL & HOGE CW 2007. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq War. JAMA, 298, 2141–2148. [DOI] [PubMed] [Google Scholar]
- MORGAN RE & THOMPSON A October 2021. Criminal Victimization, 2020. Department of Justice Office of Justice Programs, Bureau of Justice Statistics. Available: https://bjs.ojp.gov/library/publications/criminal-victimization-2020. [Google Scholar]
- MORRAL AR, GORE K & SCHELL TL 2015. Sexual assault and sexual harassment in the US military: Estimates for Department of Defense service members from the 2014 RAND Military Workplace Study. Santa Monica, CA: RAND Corporation. Available: https://www.rand.org/pubs/research_reports/RR870z2-1.html. [Google Scholar]
- NORRIS AL, CAREY KB, SHEPARDSON RL & CAREY MP 2021. Sexual revictimization in college women: Mediational analyses testing hypothesized mechanisms for sexual coercion and sexual assault. Journal of Interpersonal Violence, 36, 6440–6465. [DOI] [PubMed] [Google Scholar]
- O’BRIEN BS & SHER L 2013. Military sexual trauma as a determinant in the development of mental and physical illness in male and female veterans. International Journal of Adolescent Medicine and Health, 25, 269–274. [DOI] [PubMed] [Google Scholar]
- O’BRIEN C, KEITH J & SHOEMAKER L 2015. Don’t tell: Military culture and male rape. Psychological Services, 12, 357–65. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Defense, Office of the Deputy Assistant Secretary of Defense for Military Community And Family Policy. (2021) 2020 Demographics Profile of the Military Community. Available from: https://download.militaryonesource.mil/12038/MOS/Reports/2020-demographics-report.pdf [Accessed 27th October 2022]
- ROSE L, AOUAD M, GRAHAM L, SCHOEMAKER L & WAGNER T 2021. Association of expanded health care networks with utilization among Veterans Affairs enrollees. JAMA Network Open, 4, e2131141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SCOGLIO AAJ, MOLNAR BE, LINCOLN AK, GRIFFITH J, PARK C & KRAUS SW 2022. Sexual and physical revictimization in U.S. military veterans. Journal of Traumatic Stress, 35, 1129–1141. [DOI] [PubMed] [Google Scholar]
- SEAL KH, COHEN G, WALDROP A, COHEN BE, MAGUEN S & REN L 2011. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence, 116, 93–101. [DOI] [PubMed] [Google Scholar]
- STATACORP 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC. [Google Scholar]
- STEWART SH 1996. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin, 120, 83–112. [DOI] [PubMed] [Google Scholar]
- STRAUS R & BACON SD 1953. Drinking in college, New Haven, CT, Yale University Press. [Google Scholar]
- SURIS A & LIND L 2008. Military sexual trauma: A review of prevalence and associated health consequences in veterans. Trauma, Violence, & Abuse, 9, 250–269. [DOI] [PubMed] [Google Scholar]
- TANNAHILL HS, LIVINGSTON WS, FARGO JD, BRIGNONE E, GUNDLAPALLI AV & BLAIS RK 2020. Gender moderates the association of military sexual trauma and risk for psychological distress among VA-enrolled veterans. Journal of Affective Disorders, 268, 215–220. [DOI] [PubMed] [Google Scholar]
- TESTA M, HOFFMAN JH & LIVINGSTON JA 2010. Alcohol and sexual risk behaviors as mediators of the sexual victimization-revictimization relationship. Journal of Consulting & Clinical Psychology, 78, 249–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TESTA M & LIVINGSTON JA 2018. Women’s alcohol use and risk of sexual victimization: Implications for prevention. In: ORCHOWSKI LM & GIDYCZ CA (eds.) Sexual Assault Risk Reduction and Resistance. San Diego: Academic Press. [Google Scholar]
- TIRONE V, BAGLEY JM, BLAIS R, PETREY K, MEADE E & SADLER A 2020. Military sexual trauma and sexual revictimization. Psychiatric Annals, 50, 444–451. [Google Scholar]
- U.S. ARMY October 2019. The Army People Strategy. Available: https://www.army.mil/e2/downloads/rv7/the_army_people_strategy_2019_10_11_signed_final.pdf. [Accessed 2nd February 2022]
- U.S. CENSUS BUREAU 2021.TABLE UC3. OPPOSITE-SEX UNMARRIED COUPLES BY PRESENCE OF BIOLOGICAL CHILDREN UNDER 18, and Age, EARNINGS, EDUCATION, AND RACE AND HISPANIC ORIGIN OF BOTH PARTNERS: 2021. Current Population Survey, 2021 Annual Social and Economic Supplement. Available from: https://www2.census.gov/programs-surveys/demo/tables/families/2021/cps-2021/tabuc1-all.xls [Accessed 22nd October 2022] [Google Scholar]
- U.S. Department of Defense. (2018) Department of Defense Annual Report on Sexual Assault in the Military. Fiscal Year 2017. Available from: http://sapr.mil/public/docs/reports/FY17_Annual/DoD_FY17_Annual_Report_on_Sexual_Assault_in_the_Military.pdf [Accessed 2nd February 2022]
- U.S. Department of Defense. (2021) Department of Defense Annual Report on Sexual Assault in the Military. Fiscal Year 2020. Available from: https://www.sapr.mil/sites/default/files/DOD_Annual_Report_on_Sexual_Assault_in_the_Military_FY2020.pdf [Accessed 2nd February 2022]
- U.S. Department of Defense, Defense Manpower Data Center. (June 30, 2022) Number of Military and DoD appropriated fund (APF) civilian personnel: by assigned duty location and service/component. Available from: https://dwp.dmdc.osd.mil/dwp/api/download?fileName=DMDC_Website_Location_Report_2206.xlsx&groupName=milRegionCountryInsert [Accessed 5th December 2022]
- U.S. Department of Veterans Affairs, National Center for Veterans Analysis and Statistics (2020). VA utilization profile FY 2017. Available from: https://www.va.gov/vetdata/docs/Quickfacts/VA_Utilization_Profile_2017.pdf. [Accessed 30th August 2022]
- U.S. Department of Veterans Affairs, VETERANS BENEFITS ADMINISTRATION 2012. Summary of VA benefits for National Guard and reserve members and veterans. Available from: http://www.benefits.va.gov/benefits/benefits-summary/summaryofvanationalguardandreserve.pdf. [Accessed 30th August 2022]
- VEST BM, KULAK J, HALL VM & HOMISH GG 2018. Addressing patients’ veteran status: Primary care providers’ knowledge, comfort, and educational needs. Family Medicine, 50, 455–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VEST BM, KULAK JA & HOMISH GG 2019. Caring for veterans in US civilian primary care: Qualitative interviews with primary care providers. Family Practice, 36, 343–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VOGT DS, SMITH BN, KING DW & KING LA 2012. Manual for the Deployment Risk and Resilience Inventory-2 (DRRI-2): A Collection of Measures for Studying Deployment-Related Experiences of Military Veterans. Boston, MA: National Center for PTSD. [Google Scholar]
- WILSON LC 2018. The prevalence of military sexual trauma: A meta-analysis. Trauma, Violence, & Abuse, 19, 584–597. [DOI] [PubMed] [Google Scholar]
- WOLFE J, SHARKANSKY EJ, READ JP, DAWSON R, MARTIN JA & OUIMETTE PC 1998. Sexual harassment and assault as predictors of PTSD symptomatology among US female Persian Gulf War military personnel. Journal of Interpersonal Violence, 13, 40–57. [Google Scholar]


