Abstract
Introduction
Booster sessions can improve cardiopulmonary resuscitation (CPR) skill retention among healthcare providers; however, the optimal timing of these sessions is unknown. This study aimed to explore differences in skill retention based on booster session timing.
Methods
After ethics approval, healthcare providers who completed an initial CPR training course were randomly assigned to either an early booster, late booster, or no booster group. Participants’ mean resuscitation scores, time to initiate compressions, and time to successfully provide defibrillation were assessed immediately post-course and four months later using linear mixed models.
Results
Seventy-three healthcare professionals were included in the analysis. There were no significant differences by randomization in the immediate post-test (9.7, 9.2, 8.9) or retention test (10.2, 9.8, and 9.5) resuscitation scores. No significant effects were observed for time to compression. Post-test time to defibrillation (mean ± SE: 112.8 ± 3.0 sec) was significantly faster compared to retention (mean ± SE: 120.4 ± 2.7 sec) (p = 0.04); however, the effect did not vary by randomization.
Conclusion
No difference was observed in resuscitation skill retention between the early, late, and no booster groups. More research is needed to determine the aspects of a booster session beyond timing that contribute to skill retention.
Abstract
Introduction
Des séances de rappel peuvent favoriser le maintien des compétences en réanimation cardio-pulmonaire (RCP) chez les professionnels de la santé; toutefois, le moment optimal pour offrir ces séances est inconnu. Cette étude visait à explorer les différences dans le maintien des compétences en fonction du moment où intervient la séance de rappel.
Méthodes
Après avoir obtenu une approbation éthique, nous avons réparti au hasard des professionnels de la santé ayant suivi une formation initiale en RCP entre un groupe qui a reçu un rappel précoce, un groupe qui a eu un rappel tardif et un groupe qui n’a pas reçu de séance de rappel. Les scores moyens de réussite de la réanimation, le temps moyen pris avant de commencer les compressions et le temps moyen pris pour effectuer avec succès une défibrillation ont été évalués immédiatement après la séance et quatre mois plus tard, à l’aide de modèles mixtes linéaires.
Résultats
Les données de 73 professionnels de la santé ont été analysées. Il n’y a pas eu de différences significatives à la suite de la randomisation dans les scores de réanimation au post-test immédiat (9,7; 9,2; 8,9) et au test sur le maintien des compétences (10,2; 9,8 et 9,5). Aucun effet significatif n’a été observé en lien avec le délai avant d’entamer les compressions. Le délai de défibrillation était significativement plus court après la séance (moyenne ± SE : 112,8 ± 3,0 sec) que lors du test de maintien des compétences (moyenne ± SE : 120,4 ± 2,7 sec) (p=0,04); cependant, l’effet n’a pas été différent d’un groupe à un autre.
Conclusion
Aucune différence n’a été observée sur le plan du maintien des compétences en réanimation entre les groupes avec rappel précoce, avec rappel tardif et sans rappel. De plus amples travaux sont nécessaires pour déterminer les caractéristiques d’une séance de rappel, autres que le moment où elle intervient, qui contribueraient au maintien des compétences.
Introduction
Cardiac arrest is a major cause of mortality.1–4 Prompt and effective cardiopulmonary resuscitation (CPR) following cardiac arrest has been shown to double the odds of survival.5,6 Course participants are encouraged to renew their Basic Life Support (BLS) certification every year. However, studies show that CPR skills can deteriorate much sooner than this recommended timeframe, as early as three months.2,7–11
Refresher, or booster sessions, have been shown to effectively improve CPR skill retention,12–15 in line with information processing theory.16 According to information processing theory, when material is first perceived, it is temporarily stored in short-term memory. To successfully “learn” the material, it must move to long-term memory.16 One of the key ways that information moves from our short-term memory to our long-term memory is through repetition.16 However, the optimal timing for repetition remains unclear. While some studies found that a repetition soon after initial teaching was more effective, others found that delayed repetition was more effective for long-term skill retention.18,19
Though there has yet to be consensus as to the optimal timing of booster sessions for CPR skill retention among healthcare professionals, literature from other fields suggests this value may be 10-30% of the number of days between the initial training and retention test.20 We aimed to determine the optimal timing of booster sessions for CPR skill retention after completion of a BLS course, with sessions offered at two different timepoints within this suggested interval (i.e., 10-30%).
Materials & methods
Ethical approval was obtained from the Montfort Hospital Research Ethics Board (#18-19-08-020). This paper is reported according to the CONSORT checklist.21
Design
We conducted a prospective randomized control trial.
Participants
Frontline healthcare providers across four hospitals in Ottawa, ON, Canada were included as long as they had not taken a BLS course in the previous six months.
Intervention
Booster sessions followed a standardized ten-minute format. The initial portion involved performing a two-minute resuscitation scenario in front of an experienced instructor who shares immediate feedback based on performance gaps. The scenario involved entering a room in the hospital and noticing a patient lying unconscious on the floor. A mannequin with feedback capabilities was used to provide participants with real-time feedback on their performance (e.g., compression depth, rate, and recoil).
Outcomes
The primary outcome was participants’ mean score on a standardized Heart and Stroke Foundation resuscitation checklist (Appendix A), which has demonstrable face validity as it is used by CPR certification organizations (maximum score of 13 points).22 High-quality compression (i.e., appropriate depth and speed) was indicated by the appearance of a green light on the mannequin. The participants needed 30 high quality compressions in the allotted 15 to 18 seconds to pass. The two secondary outcomes were the time to initiate compressions and the time to successfully provide a defibrillation. Participants were videotaped once immediately after their resuscitation scenario and again four months later during the retention test. The retention test used the same resuscitation scenario as the initial test. To account for potential scheduling difficulties, a window of five days before or after the desired date was considered acceptable.
Sample size
Assuming an alpha error of 0.05 and conservatively high correlation between repeated measures of 0.8, based on findings from a previous BLS study,23 a total sample size of 54 subjects (i.e., 19 per group) would provide 80% power for finding a significant inter-group difference. Factoring in a 40% dropout rate before the retention test, we calculated 90 subjects at recruitment (i.e., 30 per group) would be the total sample size.
Randomization
Participants were randomly assigned to one of three groups using the randomize function in Microsoft Excel: early booster (three weeks post-course), late booster (eight weeks post-course), or no booster (control group).
Blinding
Outcomes were assessed by video raters with BLS expertise, who underwent initial standardization (intra-class correlation = 0.988). Video raters were blinded both to the participants’ assigned groups as well as to whether a video was the immediate post-test or the retention test. Participants were made aware of their group assignment after completing the immediate post-test.
Statistical methods
Data were analyzed using linear mixed model repeated measures with SPSS 17.0 (SPSS Inc., Chicago, IL). The mean of the two raters’ scores was considered the dependent variable, the test’s timing was the within-subjects factor (immediate post-test or retention test), and the between-subjects factor was the group assignment (control, early booster, or late booster). A p-value of 0.05 was considered statistically significant.
Results
Eighty-six participants were randomized, of which 73 completed the study and were included in the analysis: 34 participants in the control group, 23 in the early booster group, and 16 in the late booster group (Appendix B). Demographic characteristics of participants are provided in Table 1. The inter-rater reliability between raters assessing participants’ performance was 0.83.
Table 1.
Demographic data.
| Control (n = 34) | Early Booster (n = 23) |
Late Booster (n = 16) |
|
|---|---|---|---|
| Gender: n (%) | |||
| Male | 7 (20.6) | 6 (26.1) | 4 (25.0) |
| Female | 27 (79.4) | 17 (73.9) | 12 (75.0) |
| Age: mean±SD | 42.4±10.8 | 43.3±13.9 | 43.3±12.8 |
| Primary language: n (%) | |||
| English | 119 (55.9) | 15 (65.2) | 8 (50.0) |
| Other | 15 (44.1) | 8 (34.8) | 8 (50.0) |
| Education: n (%) | |||
| PhD | 12 (35.3) | 6 (26.1) | 7 (43.8) |
| Masters | 11 (32.4) | 10 (43.5) | 7 (43.8) |
| Bachelor | 4 (11.8) | 1 (4.3) | 1 (6.3) |
| College | 4 (11.8) | 4 (17.4) | 1 (6.3) |
| High School | 3 (8.8) | 2 (8.7) | 0 (0) |
| Occupation: n (%) | |||
| Nurse | 17 (50.0) | 13 (56.5) | 9 (56.3) |
| Respiratory therapist | 2 (5.9) | 3 (13.0) | 1 (6.3) |
| Physician | 9 (26.5) | 5 (21.7) | 4 (25.0) |
| Porter | 0 (0.0) | 1 (4.3) | 0 (0.0) |
| Anesthesia assistant | 6 (17.6) | 1 (4.3) | 2 (12.5) |
| Physiotherapist | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Prior CPR training: n (%) | |||
| Yes | 32 (94.1) | 23 (100.0) | 16 (100.0) |
| No | 2 (5.9) | 0 (0) | 0 (0) |
| BLS training > 6 months ago: n (%) | |||
| Yes | 34 (100.0) | 23 (100.0) | 16 (100.0) |
| No | 0 (0) | 0 (0) | 0 (0) |
| No response | 0 (0) | 0 (0) | 0 (0) |
Primary outcome results
Immediate post-test scores were not statistically different among control, early booster, and late booster groups (9.7, 9.2, 8.9) (Figure 1). Retention test scores in the three groups were also not statistically different (10.2, 9.8, and 9.5). Combining all participants together, the mean retention test score (mean ± SE: 9.8 ± 0.2) was significantly higher than the immediate post-test score (mean ±SE: 9.3 ± 0.2) (mean difference: 0.6 ± 2.4; p=0.02). There was no effect of the groups on the mean score (i.e., the resulting increase in mean scores were consistent in all groups).
Figure 1.
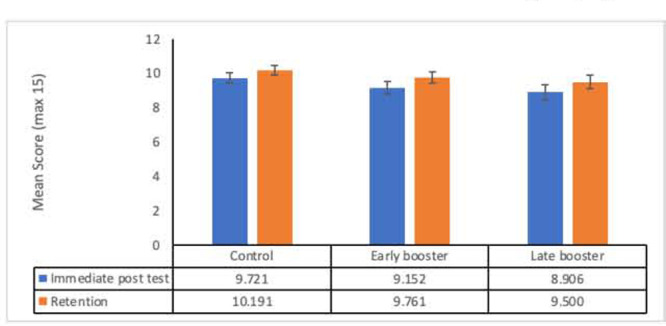
Mean score with standard errors between groups
Secondary outcome results
There was no significant effect of test (immediate post-test vs. retention) between groups nor interactions (tests X groups) for time to compression. There was no statistically significant difference in times when comparing the groups to each other.
For time to defibrillation, the immediate post-test score (mean ± SE: 112.8 ± 3.0 sec) was significantly lower compared to the retention score (mean ± SE: 120.4 ± 2.7 sec) (mean difference 7.6 ± 3.7; p=0.04). There was no effect of the groups (Control, Early and Late Booster) or interaction (tests X groups) on the defibrillation time. We also compared these outcomes by profession and found no significant effects.
When comparing mean scores by profession, we found lower immediate post-test scores among respiratory therapists (mean = 7.4) compared to the post-test and retention test scores of nurses (post-test mean = 9.8; retention mean=10.0) and physicians (post-test mean = 9.7; retention mean=9.9) (p < 0.05).
Discussion
Contrary to our hypothesis, we did not find any significant differences in scores across the three groups (early, late or control [i.e. no booster]). It remains unclear, as to what the optimal timing for BLS booster sessions may be given there was no difference in the performance between the early booster and late booster groups.
Our results contradict prior research showing that skills fade rapidly within the first three months after initial training.10 This could be due to our small sample size. Another potential reason is that five among the thirteen possible points on the scoring grid are directly related to using the Automated Emergency Defibrillator (AED). During the booster sessions, much of the feedback offered to participants pertained to the AED sequence. As such, those who had received feedback on these items during their booster may have been more likely to focus on these elements during the retention test. This raises the question as to whether it is the feedback received during a booster session that may be more impactful than the specific timing of the session. This is supported by a recent scoping review founding more evidence on the benefit of feedback for maintaining CPR skills, rather than on the timing of booster sessions.24 Our study is aligned with information processing theory, showing that any practice repetition helps to move new materials to long-term memory.16 Although our control group did not receive any booster, they were exposed to the immediate post-test so that we measured their immediate short-term learning. This immediate post-test may have acted as a repetition according to information processing theory. Future research should compare feedback vs. no feedback using various booster session timeframes. Professional experience may also be a factor to explore further as respiratory therapists appeared to score lower than nurses and physicians.
Strengths and limitations
One of the main strengths of this study is that it includes a variety of practising healthcare providers, rather than a single profession or experience level 15,2518,26 We also recruited healthcare professionals who were at least six months from their certification to avoid contamination of our retention data.
A limitation was that the immediate post-test may have reinforced retention through the testing effect, and that the same scenario was used at all time points. However, this method was the most rigorous to answer our research question and avoid additional uncontrolled variables related to using various scenarios. It should also be noted that it is resource-intensive to schedule booster sessions for each participant.
Conclusion
No difference was observed in resuscitation skill retention between the early, late, and no booster groups. More research is needed to determine the elements of a booster session beyond timing that helps to maintain skill retention.
Appendix A. BLS scoring grid
Adult CPR and AED Skills Testing Checklist

Student Name _______________________________________Date of Test
In-Facility Scenario: “You are working in a hospital or clinic, and you see a person who has suddenly collapsed in the hallway. You check that the scene is safe and then approach the patient. Demonstrate what you would do next.”
Prehospital Scenario: “You arrive on the scene for a suspected cardiac arrest. No bystander CPR has been provided. You approach the scene and ensure that it is safe. Demonstrate what you would do next.”

Once student shouts for help, instructor says, “Here’s the barrier device. I am going to get the AED.”
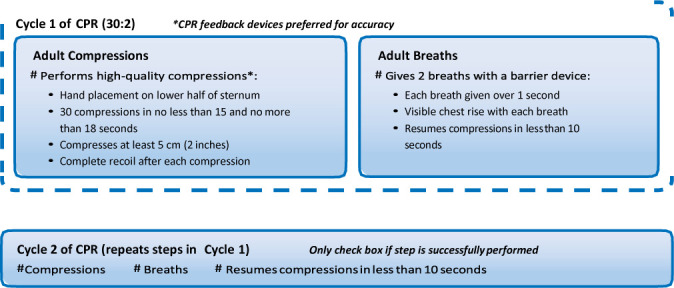
Rescuer 2 says, “Here is the AED. I’ll take over compressions, and you use the AED.”
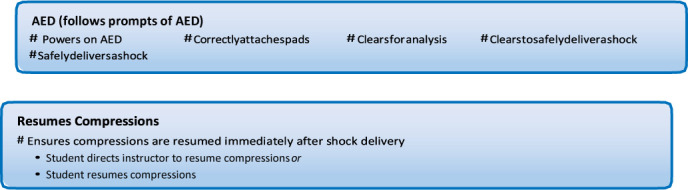
STOP TEST
|
Instructor Notes
| |
| Test Results Check PASS or NR to indicate pass or needs remediation: | PASS # NR # |
| Instructor Initials_Instructor HSF ID #_____Date _____ | |
© 2016 American Heart Association
Appendix B. CONSORT Flow Chart
Funding Statement
Funding: This project received a grant from the Association médicale universitaire de l’Hôpital Montfort (AMUHM)–Department of Family Medicine. Dr. Boet was supported by The Ottawa Hospital Anesthesia Alternate Funds Association and the Faculty of Medicine, University of Ottawa with a Tier 2 Clinical Research Chair.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132(18):S414–35. 10.1161/CIR.0000000000000259 [DOI] [PubMed] [Google Scholar]
- 2.Monsieurs KRG, Nolan JP, Bossaert LLet al. European resuscitation council guidelines for resuscitation 2015. Resuscitation 2015;95:1–80. 10.1016/j.resuscitation.2015.07.038 [DOI] [PubMed] [Google Scholar]
- 3.Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: Improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American heart association. Circulation 2013;128(4):417–35. 10.1161/CIR.0b013e31829d8654 [DOI] [PubMed] [Google Scholar]
- 4.Stiell IG, Brown SP, Nichol G, Davis DP. What is the role of chest compression depth during out of hospital. Crit Care Med 2013;40(4):1192–8. 10.1097/CCM.0b013e31823bc8bb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Heart Association . CPR facts & stats [Internet]. 2021. Available from https://cpr.heart.org/en/resources/cpr-facts-and-stats [Accessed on Dec 6, 2021].
- 6.Idris AH, Guffey D, Pepe PE, et al. Chest compression rates and survival following out-of-hospital cardiac arrest. Crit Care Med 2015;43(4):840–8. 10.1097/CCM.0000000000000824 [DOI] [PubMed] [Google Scholar]
- 7.Hamilton R. Nurses’ knowledge and skill retention following cardiopulmonary resuscitation training: a review of the literature. J Adv Nurs 2005;51(3):288–97. 10.1111/j.1365-2648.2005.03491.x [DOI] [PubMed] [Google Scholar]
- 8.Hunt EA, Fiedor-Hamilton M, Eppich WJ. Resuscitation education: narrowing the gap between evidence-based resuscitation guidelines and performance using best educational practices. Pediatr Clin North Am 2008;55(4):1025–50. 10.1016/j.pcl.2008.04.007 [DOI] [PubMed] [Google Scholar]
- 9.Oermann MH, Kardong-Edgren SE, Odom-Maryon T. Competence in CPR. Am J Nurs 2012;112(5):43–6. 10.1097/01.NAJ.0000414320.71954.34 [DOI] [PubMed] [Google Scholar]
- 10.Yang CW, Yen ZS, McGowan JE, et al. A systematic review of retention of adult advanced life support knowledge and skills in healthcare providers. Resuscitation [Internet] 2012;83(9):1055–60. 10.1016/j.resuscitation.2012.02.027 [DOI] [PubMed] [Google Scholar]
- 11.Bhanji F, Finn JC, Lockey A, et al. Part 8: education, implementation, and teams: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2015;132:S242–68. 10.1161/CIR.0000000000000277 [DOI] [PubMed] [Google Scholar]
- 12.Wolfe H, Maltese M, Niles D, et al. Blood pressure directed booster trainings improve intensive care unit provider retention of excellent CPR skills. Pediatr Emerg Care 2015;31(11):743–7. 10.1097/PEC.0000000000000394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sutton RM, Niles D, Meaney PA, et al. Low-dose, high-frequency CPR training improves skill retention of in-hospital pediatric providers. Peds 2011;128(1). 10.1542/peds.2010-2105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kardong-Edgren S, Oermann MH, Jastrzembski TS, et al. Baseline cardiopulmonary resuscitation skill performance of nursing students is improved after one resuscitation quality improvement skill refresher. J Nurses Prof Dev 2020;36(2):57–62. 10.1097/NND.0000000000000614 [DOI] [PubMed] [Google Scholar]
- 15.Niles DE, Nishisaki A, Sutton RM, et al. Improved retention of chest compression psychomotor skills with brief “rolling refresher” training. Simul Healthc 2017;12(4):213–9. 10.1097/SIH.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 16.Schunk D. Learning Theories: An Educational Perspective. 6th ed. London, United Kingdom: Pearson; 2011. [Google Scholar]
- 17.Anderson R, Sebaldt A, Lin Y, Cheng A. Optimal training frequency for acquisition and retention of high-quality CPR skills: a randomized trial. Resuscitation 2019;135(October 2018):153–61. 10.1016/j.resuscitation.2018.10.033 [DOI] [PubMed] [Google Scholar]
- 18.Bender J, Kennally K, Shields R, Overly F. Does simulation booster impact retention of resuscitation procedural skills and teamwork? J Perinatol 2014;34(9):664. [DOI] [PubMed] [Google Scholar]
- 19.Kaczorowski K, Levitt C, Hammond M, et al. Retention of neonatal resuscitation skills and knowledge: a randomized controlled trial. Fam Med 1998;30(10):705–11. [PubMed] [Google Scholar]
- 20.Rohrer D, Pashler H. Increasing retention without increasing study time. Educ. 2007;132. [Google Scholar]
- 21.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Int J Surg. 2011;9(8):672–7. 10.1016/j.ijsu.2011.09.004 [DOI] [PubMed] [Google Scholar]
- 22.Heart and Stroke Foundation of Canada. Available at https://cpr.heartandstroke.ca/ [Accessed Mar 31, 2019].
- 23.Li Q, Zhou R hua, Liu J, et al. Pre-training evaluation and feedback improved skills retention of basic life support in medical students. Resuscitation 2013;84(9):1274–8. 10.1016/j.resuscitation.2013.04.017 [DOI] [PubMed] [Google Scholar]
- 24.Lauridsen KG, Løfgren B, Brogaard L, Paltved C, Hvidman L, Krogh K. Cardiopulmonary resuscitation training for healthcare professionals. Simul Healthc J Soc Simul Healthc 2021;Publish Ah(00):1–13. 10.1097/sih.0000000000000608 [DOI] [PubMed] [Google Scholar]
- 25.Kemery S, Kelly K, Wilson C, Wheeler CA. Brief bedside refresher training to practice cardiopulmonary resuscitation skills in the ambulatory surgery center setting. J Contin Educ Nurs 2015;46(8):370–6. 10.3928/00220124-20150721-04 [DOI] [PubMed] [Google Scholar]
- 26.Matterson HH, Szyld D, Green BR, et al. Neonatal resuscitation experience curves: simulation based mastery learning booster sessions and skill decay patterns among pediatric residents. J Perinat Med 2018;46(8):934–41. [DOI] [PubMed] [Google Scholar]


