Abstract:
Demodex blepharitis is a common disease of the eyelid, affecting approximately 25 million Americans. This article reviews what is known about the mechanisms and impact of Demodex blepharitis, risk factors, signs and symptoms, diagnostic techniques, current management options, and emerging treatments. Demodex mites contribute to blepharitis in several ways: direct mechanical damage, as a vector for bacteria, and by inducing hypersensitivity and inflammation. Risk factors for Demodex blepharitis include increasing age, rosacea, and diabetes. The costs, symptom burden, and psychosocial effects of Demodex blepharitis are considerable. The presence of collarettes is pathognomonic for Demodex blepharitis. Redness, dryness, discomfort, foreign body sensation, lash anomalies, and itching are also hallmarks of the disease. Although a number of oral, topical, eyelid hygiene and device-based options have been used clinically and evaluated in studies for the management of Demodex blepharitis, none have been FDA approved to treat the disease. Recent randomized controlled clinical trials suggest that lotilaner ophthalmic solution, 0.25%, is a topical treatment with the potential to eradicate Demodex mites and eliminate collarettes and eyelid redness for an extended period.
Key Words: Demodex, Blepharitis, Ocular surface disease
Blepharitis is a chronic inflammation of the eyelid margin characterized by erythema, ocular irritation and discomfort, discharge and debris on the eyelids and lashes, and eyelash anomalies.1,2 In more advanced stages, there may be corneal involvement, such as punctate epithelial erosions, infiltrates, epithelial defects, or keratitis.
Although blepharitis can have various etiologies, including allergic, staphylococcal, and seborrheic, one of the most common etiologies is Demodex mite infestation.3,4 The presence of Demodex mites in eyelid tissue was first reported in 1876, and its association with blepharitis was established in 1967, but the number of published articles on Demodex blepharitis has increased dramatically in the past 5 years.5
This literature review presents the available evidence and knowledge about Demodex blepharitis. We review what is known about the epidemiology, mechanisms and impact of the disease, risk factors, signs and symptoms, diagnostic techniques, current management options, and emerging treatments.
EPIDEMIOLOGY
It has long been accepted that the prevalence of Demodex increases with age, affecting more than 80% of those older than 60 years and 100% of those older than 70 years.6 Among younger, university-based populations, Demodex prevalence has been reported as consistently low, between 2% and 27%.7–9
Researchers who have studied patient populations with clinical signs and symptoms of blepharitis find high rates of Demodex infestation, with prevalence ranging from 29% to 90%.4 Most authors in the past 5 years report that Demodex blepharitis accounts for ≥60% of those with blepharitis.3,10–13
Recently, two studies independently reported similar rates of Demodex blepharitis among patients of all ages visiting US eye care clinics.14,15 The Titan study, a multicenter retrospective chart review, found that 58% of 1,032 consecutive patients (and 69% of those with a blepharitis diagnosis) presented with collarettes—waxy, cylindrical debris at the base of the lashes that are the pathognomonic sign of Demodex blepharitis.14 Similarly, Teo et al.15 found that 55% of all patients and 62% of blepharitis patients examined in two tertiary care clinics presented with Demodex based on lash epilation.
Demodex blepharitis is equally prevalent in both sexes.10,14 Among older Americans referred to a Veterans Administration (VA) Medical Center dry eye clinic, the rate of Demodex infestation was similar regardless of ethnicity, with 72% of white patients, 65% of black patients, and 69% of Hispanic patients affected.3
MECHANISMS OF DISEASE
Demodex mites, the most common ectoparasite on humans, have been implicated in blepharitis. Two species, Demodex folliculorum and Demodex brevis, are found in human skin, especially the cheeks, nose, and eyelids. Both species are translucent, elongated microscopic mites with four pairs of short, clawed legs. Demodex folliculorum (Fig. 1) is approximately 0.3 to 0.4 mm in length and can be found in clusters around the lash root and lash follicle, where D. folliculorum feeds on sebum and follicular epithelial cells.16 Demodex brevis is shorter, more solitary, and prefers sebaceous glands.16 Although Demodex mites are found on healthy, asymptomatic individuals of all ages,10 it has been suggested that the mites may play a pathogenic role at higher density, when the mites reach a state of demodicosis.16
FIG. 1.

Demodex folliculorum is found in human skin, especially the cheeks, nose, and eyelids. Image courtesy of Patrick Vollmer, OD.
Demodex folliculorum is believed to be more active and therefore more implicated in type 1 allergic reactions.17 Researchers have surmised that male and female mites mate outside the follicles or glands, after which the female mites lay their eggs inside the hair follicles or sebaceous glands.18
Demodex mites secrete digestive enzymes onto nearby tissues to break down the epithelial cells to consume as food.16 Although it has previously been reported that digested material is retained in the gut and spilled onto surrounding tissues at the end of the life cycle,17 a recent microbiology report suggests that is not the case and that digested material may be excreted.19 The full life cycle of a mite is estimated to be from 14 to 23 days, progressing from egg to larva to nymph and finally to the adult stage.18,20
There are several plausible mechanisms by which Demodex contribute to blepharitis, including direct damage, acting as a vector for bacteria, and inducing hypersensitivity and inflammation.17,21,22
Direct Damage
As Demodex mites consume epithelial cells at the hair follicle, their sharp claws cause microabrasions, inducing epithelial hyperplasia.4,16,21 The presence of D. folliculorum is strongly associated with hair follicle duct dilatation and hyperkeratinization and perifollicular nongranulomatous inflammation.23 Additionally, as the mites clump and lay their eggs at the base of the lashes, the follicles become distended.16 Higher numbers of mites in the lash follicles are associated with reactive conjunctivitis and keratitis.24 As Demodex infestation affects the structure of the hair follicles, lashes may be lost or become misdirected.17
Mites deposit debris consisting of digestive enzymes, epithelial cells, keratin, and eggs onto human host tissue. Proteases and lipases present in this debris may cause direct surface irritation and inflammation, a type 1 allergic response.16,17
Demodex brevis has been implicated in meibomian gland disease (MGD), including meibomian gland loss.4,25 The build-up of decomposing mite remains, including their chitinous exoskeletons, is believed to contribute to physical blockage of the meibomian glands,4 possibly leading to changes in gland architecture over time.4,25 Changes in meibum secretion or lipid composition in MGD may promote the cycle by making the ocular environment more favorable for Demodex.4,26
Bacterial Dysbiosis
The relationships among Demodex mites and the skin, gut, and ocular microbiota are complex. Historically, anterior blepharitis has often been believed to have a primarily bacterial origin. Eyelashes of patients with blepharitis have significantly higher microbial counts than healthy control subjects.13 Fu et al.27 recently reported that Demodex infestation may reduce the diversity of the microbiome in the conjunctival sac, thereby destabilizing it.
Bacterial biofilms have been implicated in blepharitis, and it has been proposed that lash deposits in blepharitis may be composed of these biofilms.28 Demodex may also take advantage of the barrier defense “shield” provided by the biofilm to infiltrate the lash follicles and meibomian glands.29 Demodex mites carry concomitant bacteria such as Streptococcus and Staphylococcus species on their surface, and Bacillus oleronius inside their abdomen, producing antigens and inducing an immune response.17,20–22 In particular, studies have shown a positive correlation between Staphylococcus epidermidis and Demodex mite density.30 The mites may act as a vector for other skin and environmental microbes when patients rub their eyes to relieve blepharitis-related itching and discomfort.30
Delayed Hypersensitivity Response
In rosacea, Demodex proliferation seems to exist on a continuum, with mites triggering an inflammatory cascade, which then creates conditions for increasing mite proliferation and worsening disease.31
In Demodex blepharitis, digestive enzymes, chitin, and other mite byproducts may also trigger an inflammatory cascade by the toll-like receptor (TLR2) innate immunity pathway.11,16,18,21 There is an increase in the number of CD4+ T cells, macrophages, and Langerhans cells in patients with Demodex.16 Demodex infestation is associated with upregulation of pro-inflammatory cytokines, particularly IL-1β and IL-17,17,18,24 tear film alterations,24 and upregulation of matrix metalloproteinase-9 (MMP-9).20 Tarkowski et al.32 hypothesized that biological debris from Demodex mites may disrupt the epithelial barrier and lead to chronic inflammation and degeneration of conjunctival tissue, contributing to the development of pterygium. Activation of IL-17/MMP-9 signaling may also exacerbate corneal epithelial barrier dysfunction.33
RISK FACTORS AND ASSOCIATED CO-MORBIDITIES
Blepharitis, rosacea, diabetes, and increasing age are risk factors for Demodex blepharitis.21 Other factors that may predispose people to Demodex blepharitis include local or systemic immunosuppression, stress, higher alcohol intake, greater sun exposure, and smoking.3,20,21
Rosacea
Demodex mites have been implicated in rosacea and there are close associations between Demodex skin infestation and ocular Demodex.34,35 It is believed that once facial demodicosis develops, Demodex mites migrate and flourish around the eyes as well, contributing to ocular rosacea and/or Demodex blepharitis. Ocular rosacea is characterized by telangiectasia, lid margin irregularity, and meibomian gland dysfunction; ocular rosacea can lead to severe ocular surface disease, including cicatrizing conjunctivitis and corneal perforation.36 Patients with rosacea are more likely to have blepharitis and higher Demodex mite densities.37 Mites likely trigger an inflammatory cascade that worsens both skin and ocular conditions.31 The dermatology literature suggests that Demodex may also be associated with a multitude of skin conditions beyond rosacea, including acne vulgaris, seborrheic dermatitis, and basal cell and sebaceous carcinoma.16,38
Dry Eye Disease (DED)
In recent reports, 60% to 70% of patients with dry eye also presented with Demodex blepharitis.3,14 There is significant overlap in symptoms between Demodex blepharitis and dry eye disease. However, ocular signs associated with DED, such as staining, rapid tear break-up time, and reduced Schirmer score, do not correlate with Demodex blepharitis.17,29
A tear film compromised by DED could make conditions more hospitable for Demodex mites. Demodicosis, particularly when unrecognized or untreated, can complicate ocular surface diseases, leading to more severe symptoms.39 Patients using lifitegrast and cyclosporine were just as likely to have signs of Demodex blepharitis (60% had collarettes) as those not using topical immunomodulators, suggesting that dry eye treatments are unlikely to mitigate Demodex blepharitis.14
Meibomian Gland Dysfunction
Several authors have reported associations between Demodex infestation and MGD. Flores de Venecia et al.40 reported an 85% incidence of Demodex in patients with MGD compared with 34% in healthy control subjects (without any lid margin disease). In a similar study, Bhandari et al. reported a 60% incidence in patients with MGD compared with 18% in control subjects.41 Demodex-positive MGD patients have been shown to have statistically significantly more damage to the size and morphology of the meibomian glands, their openings, and the degree of adjacent fibrosis than Demodex-negative MGD patients.25 The intensity of Demodex infestation has been associated with the severity of MG damage: The greater the number of Demodex mites, the more serious the structural damage to the meibomian glands.25 Additionally, patients with Demodex blepharitis have been shown to have low-quality meibum24 and higher concentrations of (O-acyl)-ω-hydroxy fatty acids (OAHFAs) in their meibum,26 potentially exacerbating MGD and contributing to tear film instability.
Chalazia, Hordeola, and Pterygia
Significant associations have been reported between ocular Demodex infestation and chalazia23,42 and pterygium.32 Two recent articles have noted, in particular, the strong association between Demodex infestation and pediatric chalazia and suggested that children with recurrent chalazia should be evaluated for Demodex and that Demodex should be considered a risk factor for development of chalazia in children.43,44 It has been hypothesized that a local granulomatous reaction provoked by chitin from decomposing Demodex mites may lead to hordeolum or chalazion.4
DIAGNOSIS OF DEMODEX BLEPHARITIS
Clinical Signs
Collarettes—solidified exudative excretions that form a cylindrical collar around the base of the eyelash follicle—are the pathognomonic sign of Demodex blepharitis.18,21,24,35,39,45–49 Several robust studies have shown that all eyes with collarettes (100%) are positive for Demodex mites, identified by microscopy48 or by polymerase chain reaction genetic testing for the mite DNA.12
Often referred to in the literature as cylindrical dandruff (CD), collarettes have also been called sleeves, cuffs, crusting, or lash debris. We find the term “collarette” to be the most aptly descriptive. Collarettes are waxy in texture and composed of accumulated undigested material, keratinized cells, dead or living mites, and eggs and egg casings of mites.4,20,48 Collarettes remain at the base of the lash, differentiating the collarettes from bacterial debris that clings to the shaft of the lash as it grows.17 Not only is the presence of collarettes indicative of Demodex mites, but having a high number of collarettes has been associated with more severe mite infestation.3,46,48,50 Collarettes can be easily identified at the slitlamp by instructing patients to look down or close the eyelids, so that there is a clear view of the base of the upper lash margin (Fig. 2).14,16,21,48
FIG. 2.
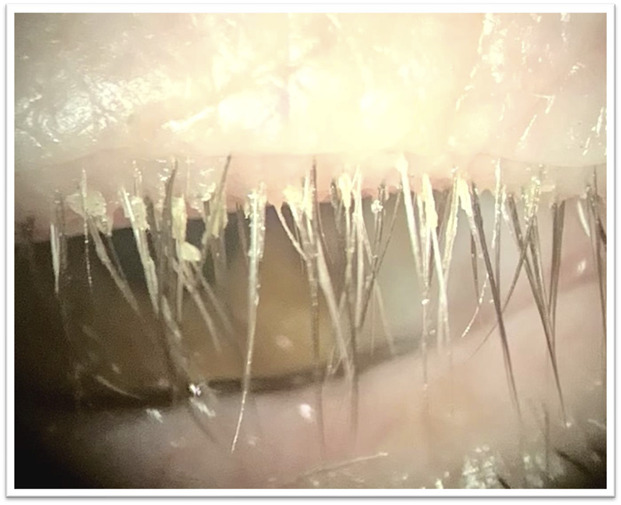
Collarettes, the pathognomonic sign of Demodex blepharitis, can be readily identified at the base of the upper lash margin on downward gaze at the slitlamp. Image courtesy of Patrick Vollmer, OD.
An epilated eyelash sample viewed under a microscope can enable further confirmation of the presence of Demodex. However, there is no universally accepted method for sampling lashes and quantifying Demodex mite density, making accurate comparisons difficult.51 In the two recent prevalence studies discussed at the beginning of this review, US researchers found nearly identical rates of demodicosis, regardless of whether the researchers defined demodicosis by the presence of collarette14 or by lash epilation with mite counts.15 Outside of clinical trials, lash epilation and microscopy are often impractical. In our experience, observing the presence of collarettes at the slitlamp can be the sole diagnostic indicator for Demodex blepharitis in clinical practice because the collarettes are pathognomonic. Furthermore, Zhang et al.4 recently concluded that positive identification of collarettes (CD), along with eyelash manipulation at the slitlamp (without epilation), may be the most suitable method for diagnosis of Demodex blepharitis in clinical settings and that collarettes alone should alert the practitioner to the high likelihood of ocular demodicosis.
Lash anomalies are another important clinical sign of Demodex blepharitis. Trichiasis, or eyelash misdirection, is common.17,20 Madarosis, or eyelash loss, occurs in more advanced cases20,35 and is predictive of Demodex blepharitis. Sędzikowska et al.52 found a 4.30 odds ratio that patients complaining of eyelash loss would have Demodex. Nicholls et al.20 have also described a less common finding, in which the lash thickness abruptly changes, with a terminal thinning and twisted or split ends, which attribute to the consumption of lash cortex by Demodex mites. Given that the purpose of the eyelashes is to protect the ocular surface and direct airflow away from it, mite-induced follicular damage that results in lash misdirection or loss may make patients more symptomatic or negatively impact ocular surface health.14
Eyelid margin erythema and telangiectasia are also commonly seen in Demodex blepharitis22,49,53 and may contribute to patients' perception of a negative cosmetic appearance.53
Symptoms
Ocular itching is the symptom most commonly associated with Demodex blepharitis,11,35,50–53 and evidence suggests that patients consider ocular itching to be one of the most bothersome symptoms associated with the disease.53 Demodex-related itching may be more likely to occur at night or early morning after periods of mite activity,5,35 distinguishing it from daytime, allergy-related itching. Dry eye or blepharitis patients with Demodex are significantly more likely to report itching than those without Demodex,3,11 and the frequency of itching complaints increases with higher Demodex density.3,10 Individuals who report itching have a 2.6-fold higher risk of having Demodex.52 Demodex-related ocular itching may be propagated through nonhistamine itching pathways.3
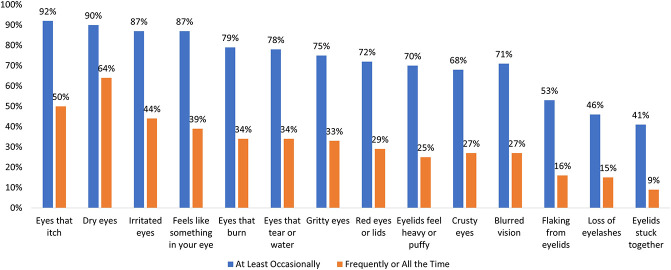
In addition to itching, those with Demodex blepharitis often present with a range of other symptoms, including dryness, discharge, eye redness, burning, tearing, foreign body sensation, pain, and blurred (or fluctuating) vision (Fig. 3).53
FIG. 3.
Symptoms reported by patients with confirmed Demodex blepharitis ( N=301).53
Impact of Demodex Blepharitis
The symptom burden and psychosocial effects of Demodex blepharitis are considerable, according to a recent study of 311 patients with confirmed Demodex blepharitis.53 One-third of the patients reported making multiple visits to a doctor to resolve their symptoms and more than half of the patients reported being bothered by symptoms “frequently” or “all of the time.”53 Approximately half (51%) of the patients had been experiencing symptoms for at least four years, and more than half (58%) of the patients had not previously received a correct diagnosis.53 Eighty percent of the patients said that blepharitis had negatively affected daily life, with impacts on driving at night, daily hygiene routines, contact lens discomfort and, for women, difficulty wearing makeup or artificial lashes.53 It has previously been reported that patients with blepharitis have a 67% higher risk of anxiety and 52% higher risk of depression compared with those without blepharitis.54
Clinicians may want to have a heightened suspicion of Demodex blepharitis in specific patient populations. Contact lens wear, by altering the ocular surface microbiome, may increase susceptibility to Demodex.55 Perhaps more importantly for clinical practice, however, Demodex may be a significant factor in contact lens intolerance and dropout. Approximately half (51%) of contact lens wearers have Demodex.14 In a study of Asian female contact lens wearers examined by confocal microscopy, Demodex was found in 90% of lens wearers compared with 65% of nonwearers (P=0.06).56 Symptomatic lens wearers have been shown to have higher Demodex mite density.57 Tarkowski et al.58 found that a high percentage of contact lens–intolerant subjects (93%) had Demodex infestation compared with only 6% of asymptomatic wearers. Given the positive correlation between the presence of Demodex and intolerance to soft contact lenses, Demodex mites may exacerbate symptoms of contact lens discomfort.
Demodex blepharitis is common in the cataract surgery age population. Using light microscopy, researchers in Poland evaluated the eyelashes of 73 consecutive patients presenting for cataract surgery and found Demodex infestation in nearly half of the patients; those patients had lower Schirmer scores and faster tear break-up times.59 The Titan study also found that 56% of cataract patients demonstrated Demodex blepharitis.14 A healthy ocular surface is critical for successful intraocular lens (IOL) power calculation and good visual outcomes and satisfaction after cataract or refractive surgery, so it is important to screen preoperative patients for ocular surface and lid disease, including Demodex blepharitis.
DISEASE MANAGEMENT
There are currently no FDA-approved treatments for Demodex blepharitis. Although a number of over-the-counter and office-based device options have been used clinically and evaluated in relatively small studies, none has yet been established as clearly effective at eradicating mites and eliminating signs of Demodex blepharitis.4,60 Side effects and tolerability should be taken into consideration because successful management of this disease is dependent on patient convenience and compliance, neither of which are ideal with current options. A recent multicenter, randomized controlled study has demonstrated that lotilaner ophthalmic solution, 0.25% (TP-03, Tarsus Pharmaceuticals, Irvine, CA), shows significant improvements in mite eradication, collarette elimination, and eyelid erythema reduction compared with vehicle.61
Current Management Approaches
In the decades since Demodex blepharitis was first identified, many agents have been evaluated to better manage the disease, including selenium, antiparasitics, topical and oral antibiotics, and many naturally derived products.5,18 The most well-studied approaches are described below and in Table 1.
TABLE 1.
Current and Emerging Management Approaches to Demodex Blepharitis
| Agent or Procedure | Form and Dosing | Demonstrated Effects in Demodex Blepharitis | Limitations |
| Ivermectin2,45,62,63,65 | Acaricide | ||
| Oral or topical | Improves signs and symptoms | Hypersensitivity reactions and drug interactions | |
| Established dermatological treatment | Reduces mite density | More severe side effects with oral use | |
| Metronidazole45,62,64,65 | Broad anti-inflammatory and antiparasitic | ||
| Oral or topical | Improves signs and symptoms | Hypersensitivity reactions and drug interactions | |
| Established dermatological treatment | Reduces mite density | More severe side effects with oral use | |
| Tea tree oil (TTO) and derivatives, especially terpinene 4-ol (T4O)2,16,18,21,46,47,60,62,66–71 | Over-the-counter and prescription formulations (3% to 100%) available in gel, shampoo, ointment, lid wipe or scrub, and other | Improves signs and symptoms | Contact dermatitis, ocular irritation, allergic reactions, epithelial cell toxicity |
| Broad-spectrum antimicrobial and acaricide | Some formulations achieve modest levels of mite eradication | ||
| Intense pulsed light (IPL)72–75 | In-office treatment | Reduces mean Demodex mite density | Contraindicated in Fitzpatrick V and VI skin tones, cost |
| Improves ocular surface parameters | |||
| Microblepharoexfoliation (MBE)2,29,76 | In-office treatment to remove lid and lash debris | Helpful adjunct to at-home lid hygiene | Mild discomfort, irritation, or redness |
| Improves symptoms | |||
| Reduces mite density but does not eradicate mites | |||
| Lotilaner ophthalmic solution, 0.25%61,78–83 | Investigational drug (0.25%) | High rates of mite eradication, collarette cure, and erythema cure | Mild instillation site pain was the most commonly reported adverse event |
| Topical acaricide | |||
| 2 drops per day dosing for 6 weeks |
Other agents that have been evaluated but for which there is limited evidence in the literature include selenium, topical and oral antibiotics, permethrin cream, manuka honey, okra-derived compounds, mugwort volatile oil, and castor oil.
Ivermectin and Metronidazole
Ivermectin and metronidazole have long been used safely by dermatologists to treat Demodex-related skin conditions. In a recent meta-analysis, Martinez-Pulgarin et al.62 reported that the combination of systemic and topical ivermectin and metronidazole had been shown to reduce mite counts in Demodex blepharitis, as well. In-office application of topical ivermectin-metronidazole gel therapy has also recently been tested,45 but larger studies are needed. Ivermectin is known to have an acaricidal effect,63 and metronidazole has a broad anti-inflammatory effect through neutrophil-mediated reduction of reactive oxygen species and T lymphocytes.64 However, the effects of these agents may only temporarily alleviate Demodex infestation, and side effects are possible.5,62,65
Tea Tree Oil and Other Natural Products
Tea tree oil (TTO) and its derivatives (including terpinen 4-ol or T4O) exhibit broad-spectrum antimicrobial activity against bacteria and fungi through the disruption of the cytoplasmic membrane and have demonstrated acaricidal properties, although the exact mechanism of action against Demodex viability has not been identified.66 Products containing various concentrations of TTO (from 3% to 100%) in the form of a gel, shampoo, ointment, face wash, or lid wipe have been shown to be effective in improving signs and symptoms of blepharitis.18,60,67,68 However, their efficacy for mite eradication remains uncertain.47 Higher concentrations of TTO (50%+) are more effective66 but are not considered safe for home use and must be applied in the clinic.
In a stratified meta-analysis, there were no significant subgroup differences between TTO-derived and non-TTO-derived products in mite counts, total eradication, or CD score reduction.62 Koo et al.69 reported an overall Demodex mite eradication rate of 23.6% in patients using TTO for 1 month. However, in this study, patients underwent a relatively arduous regimen of weekly in-office eyelid scrubs with high-concentration TTO in addition to twice-daily, at-home eyelid scrubs. Researchers have acknowledged that alternative treatments with improved side-effect profiles and less toxicity would be desirable.21
The primary side effects associated with TTO and T4O use are contact dermatitis, ocular irritation, and allergic reactions.16,46,47,70 Until recently, T4O was believed to be less irritating than TTO. However, an in vitro study found that even very low 0.1% and 0.01% concentrations of T4O are toxic to human meibomian gland epithelial cells.71
Other natural products that have been proposed for topical use to address Demodex blepharitis include Manuka honey, okra-derived compounds, mugwort volatile oil, and castor oil, but robust studies on their effectiveness are lacking.
In-Office Procedures
Intense pulsed light (IPL) has been proposed as an adjunctive procedure for managing demodicosis. The heat transfer may be beneficial in killing the Demodex mites and for MGD, softening meibum, and reducing inflammatory mediators.72,73 Two recent reports have shown that a series of IPL treatments can reduce mean mite counts and improve ocular surface parameters but the effect on Demodex mite density seems to be variable.74,75 Some limitations of IPL include cost and the fact that IPL cannot be performed on patients with darker skin tones (Fitzpatrick V or VI).
Microblepharoexfoliation (MBE) removes debris on the surface of the eyelids and lashes and has been used in combination with daily at-home eyelid hygiene. Although results were better than eyelid hygiene alone, the results were not clinically meaningful at eliminating Demodex.29,76 An effective treatment for Demodex blepharitis would likely decrease the need for mechanical intervention such as MBE or lid scrubs.77
Measures of Efficacy
Various measures have been proposed for evaluating treatment efficacy. Luo et al.51 proposed that a reduction of 1 mite per lash should be considered the clinical standard for treatment efficacy but there is no global consensus on the number of mites that constitutes infestation or treatment success.4,17 Recently, an expert panel concluded that patients with more than 10 collarettes should be treated, irrespective of symptoms, with reductions in collarettes used to evaluate treatment efficacy.77
A few studies have used collarette or CD scoring or classification systems to evaluate treatment efficacy. Karakurt et al.,67 for example, graded CD qualitatively as none (0), light (1), moderate (2), or severe (3). In a recent phase 2b/3 randomized controlled clinical trial of lotilaner ophthalmic solution, 0.25%, for Demodex blepharitis, collarettes were graded separately for the upper and lower eyelids according to the quantitative scale shown in Table 2.61 Grade 2 (>10 collarettes) or higher on this scale for the upper eyelid was required for inclusion in the study. Grade 0, or “collarette cure,” was considered the primary outcome measure, whereas a reduction in collarettes to 10 lashes or less (grade 0 or 1) was considered clinically meaningful because this level of change in collarettes had previously been associated with reduced mite density.48
TABLE 2.
Collarette Grading Scale62
| 0 | 0–2 lashes with collarettes |
| 1 | 3–10 lashes with collarettes |
| 2 | >10 but less than one third of lashes with collarettes |
| 3 | One third of lashes or more but less than two thirds of lashes with collarettes |
| 4 | Two thirds or more of lashes with collarettes |
Emerging Treatments
Lotilaner ophthalmic solution, 0.25% (TP-03), an acaricide of the isoxazoline parasiticide class, has completed late-stage clinical trials. Lotilaner is a veterinary medication approved for use in several countries, including the United States and European Union, for the treatment of ticks and fleas in pets. Lotilaner is lipophilic, making lotilaner well-suited to reach the oily lash follicles where mites reside. Ectoparasites exposed to isoxazolines exhibit a spastic paralysis leading to their starvation and death.78
In four phase 2 studies, this eye drop was found to be effective in reducing collarettes and Demodex density and well tolerated.79–82 The Mars single-arm pilot study evaluated 28 days of twice-daily dosing through 90 days of follow-up in participants with confirmed Demodex blepharitis.79 These results were confirmed in a randomized controlled trial, the Jupiter study, which found statistically significant decreases in collarettes and mite density in the lotilaner-treated group compared with vehicle.80 The Io and Europa studies, in which TP-03 dosing was extended to 6 weeks, demonstrated high rates of collarette cure and mite eradication, again with statistically significant differences compared with a vehicle control group.81,82
Most recently, in the pivotal phase 2b/3 Saturn-1 trial, the group treated with TP-03 achieved a statistically significantly higher proportion of patients with clinically meaningful reduction in collarettes to 10 or less (81.3% vs. 23.0%; P<0.0001), collarette cure (44.0% vs. 7.4%; P<0.0001, primary endpoint), mite eradication (67.9% vs. 17.6%; P<0.0001), and erythema cure (19.1% vs. 6.9%; P=0.0001) compared with the vehicle control group.61 This randomized, controlled, double-masked trial enrolled 421 patients with Demodex blepharitis; results were confirmed in a second phase 3 study with an additional 412 patients.83 All patients in both studies presented with Demodex blepharitis confirmed by lash epilation and mite count and were required to have collarettes and eyelid erythema to be included in the trial.61,83 Nearly 92.0% of Saturn-1 patients rated the study drop as neutral to comfortable. All ocular adverse events in the study group were mild, with the most common being instillation site pain.61
CONCLUSION
Demodex blepharitis has the potential to impair visual quality and ocular comfort and have a substantial impact on quality of life. The symptoms negatively affect patients, prompting many visits to healthcare practitioners and unsuccessful attempts at relief. Additionally, Demodex contributes to ocular surface disorders that may blur vision and may lead to corneal damage, suboptimal surgical outcomes, or contact lens intolerance. Demodex blepharitis is likely an underdiagnosed significant public health burden; additional studies are needed to accurately assess its socioeconomic impact.
Current options for the management of Demodex blepharitis are burdensome, inconvenient, and may be ineffective and/or toxic to ocular tissues. Recent randomized controlled trials suggest that lotilaner ophthalmic solution, 0.25%, is a topical treatment with the potential to significantly reduce or eliminate Demodex mites and collarettes, the pathognomonic sign of Demodex blepharitis. The development of a more effective, tolerable, safe, convenient, and regulatory body–approved treatment for Demodex blepharitis would benefit patients and provide practitioners with the first targeted tool to combat this prevalent disease.
ACKNOWLEDGMENTS
The authors thank J. Beiting of Wordsmith Consulting who provided professional medical writing support funded by Tarsus Pharmaceuticals.
Footnotes
M. Barnett, D. K. Dhaliwal, I. B. Gaddie, P. Karpecki, K. K. Nichols, C. J. Rapuano, and E. Yeu are consultants for Tarsus Pharmaceuticals. P. Karpecki is also a consultant for Azura, BioTissue, Bruder, Oasis Medical, OCuSOFT, Scope, and Thea. K. K. Nichols is also a consultant for Bruder and Thea. A. Chan, P. Karpecki, J. Mun, and E. Yeu have equity interests in Tarsus Pharmaceuticals. A. Chan and J. Mun are employees of Tarsus Pharmaceuticals. F. S. Mah and M. K. Rhee report no conflicts of interest related to the content of this article.
Contributor Information
Michelle K. Rhee, Email: mkrhee@msn.com.
Melissa Barnett, Email: drbarnett00@gmail.com.
Christopher J. Rapuano, Email: cjrapuano@willseye.org.
Deepinder K. Dhaliwal, Email: dkdhaliwal@mac.com.
Kelly K. Nichols, Email: nicholsk@uab.edu.
Paul Karpecki, Email: karpecki@karpecki.com.
Francis S. Mah, Email: Mah.Francis@Scrippshealth.org.
Arthur Chan, Email: Arthur@tarsusrx.com.
James Mun, Email: jmun@tarsusrx.com.
Ian Benjamin Gaddie, Email: ibgaddie@me.com.
REFERENCES
- 1.Putnam CM. Diagnosis and management of blepharitis: An optometrist’s perspective. Clin Optom (Auckl) 2016;8:71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amescua G, Akpek EK, Farid M, et al. Blepharitis preferred practice Pattern®. Ophthalmology 2019;126:PP56-93. [DOI] [PubMed] [Google Scholar]
- 3.Cheng AM, Hwang J, Dermer H, et al. Prevalence of ocular demodicosis in an older population and its association with symptoms and signs of dry eye. Cornea 2021;40:995–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang AC, Muntz A, Wang MTM, et al. Ocular demodex: A systematic review of the clinical literature. Ophthalmic Physiol Opt 2020;40:389–432. [DOI] [PubMed] [Google Scholar]
- 5.Shah PP, Stein RL, Perry HD. Update on the management of demodex blepharitis. Cornea 2022;41:934–939. [DOI] [PubMed] [Google Scholar]
- 6.Cheng AMS, Sheha H, Tseng SCG. Recent advances on ocular Demodex infestation. Curr Opin Ophthalmol 2015;26:295–300. [DOI] [PubMed] [Google Scholar]
- 7.Correa Fontt J, Mena Oliva M, Pérez Campos C, et al. Prevalence of Demodex spp. in eyelashes of a university's population in Santiago, Chile. Archivos de la Sociedad Española de Oftalmología (English Edition) 2020;95:159–163. [DOI] [PubMed] [Google Scholar]
- 8.Murphy O, O'Dwyer V, Lloyd-McKernan A. The effect of lid hygiene on the tear film and ocular surface, and the prevalence of Demodex blepharitis in university students. Cont Lens Anterior Eye 2020;43:159–168. [DOI] [PubMed] [Google Scholar]
- 9.Vargas-ARzola J, Segura-Salvador A, Torres-Aguilar H, et al. Prevalence and risk factors to Demodex folliculorum infection in eyelash follicles from a university population of Mexico. Acta Microbiologica et Immunologica Hungarica 2020;67:156–160. [DOI] [PubMed] [Google Scholar]
- 10.Biernat MM, Rusiecka-Ziółkowska J, Piątkowska E, et al. Occurrence of demodex species in patients with blepharitis and in healthy individuals: A 10-year observational study. Jpn J Ophthalmol 2018;62:628–633. [DOI] [PubMed] [Google Scholar]
- 11.Kabatas N, Dogan AS, Kabatas EU, et al. The effect of Demodex infestation on blepharitis and the ocular symptoms. Eye Contact Lens 2017;43:64–67. [DOI] [PubMed] [Google Scholar]
- 12.Kasetsuwan N, Kositphipat K, Busayarat M, et al. Prevalence of ocular demodicosis among patients at tertiary care center, Bangkok, Thailand. Int J Ophthalmol 2017;10:122–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu M, Cheng C, Yi H, et al. Quantitative analysis of the bacteria in blepharitis with Demodex infestation. Front Microbiol 2018;9:1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trattler W, Karpecki P, Rapoport Y, et al. The prevalence of Demodex blepharitis in US eye care clinic patients as determined by collarettes, a pathognomonic sign. Clin Ophthalmol 2022;16:1153–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teo A, Rosenberg E, Jacobson A. Prevalence of Demodex colonization in patients presenting to an outpatient clinic. Invest Ophthalmol Vis Sci 2021;62:1236. [Google Scholar]
- 16.Fromstein SR, Harthan JS, Patel J, et al. <em>Demodex </em>blepharitis: Clinical perspectives. Clin Optom (Auckl) 2018;10:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bitton E, Aumond S. Demodex and eye disease: A review. Clin Exp Optom 2021;104:285–294. [DOI] [PubMed] [Google Scholar]
- 18.Lam NSK, Long XX, Li X, et al. Comparison of the efficacy of tea tree (melaleuca alternifolia) oil with other current pharmacological management in human demodicosis: A systematic review. Parasitology 2020;147:1587–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith G, Manzano-Marín A, Reyes-Prieto M, et al. Human follicular mites: Ectoparasites becoming symbionts. Mol Biol Evol 2022;39:msac125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicholls SG, Oakley CL, Tan A, et al. Demodex species in human ocular disease: New clinicopathological aspects. Int Ophthalmol 2017;37:303–312. [DOI] [PubMed] [Google Scholar]
- 21.Luo X, Li J, Chen C, et al. Ocular demodicosis as a potential cause of ocular surface inflammation. Cornea 2017;36:S9–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol 2010;10:505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schear MJ, Milman T, Steiner T, et al. The association of demodex with chalazia: A histopathologic study of the eyelid. Ophthalmic Plast Reconstr Surg 2016;32:275–278. [DOI] [PubMed] [Google Scholar]
- 24.Rabensteiner DF, Aminfar H, Boldin I, et al. Demodex mite infestation and its associations with tear film and ocular surface parameters in patients with ocular discomfort. Am J Ophthalmol 2019;204:7–12. [DOI] [PubMed] [Google Scholar]
- 25.Cheng S, Zhang M, Chen H, et al. The correlation between the microstructure of meibomian glands and ocular demodex infestation.: A retrospective case-control study in a Chinese population. Medicine (Baltimore) 2019;98:e15595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gao H, Chen H, Xie HT, et al. Changes in meibum lipid composition with ocular Demodex infestation. Transl Vis Sci Technol 2021;10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fu Y, Wu J, Wang D, et al. Metagenomic profiling of ocular surface microbiome changes in Demodex blepharitis patients. Front Cell Infect Microbiol 2022;12:922753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rynerson JM, Perry HD. DEBS – a unification theory for dry eye and blepharitis. Clin Ophthalmol 2016;10:2455–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Epstein IJ, Rosenberg E, Stuber R, et al. Double-masked and unmasked prospective study of terpinen-4-ol lid scrubs with microblepharoexfoliation for the treatment of Demodex blepharitis. Cornea 2020;39:408–416. [DOI] [PubMed] [Google Scholar]
- 30.Yan Y, Yao Q, Lu Y, et al. Association between Demodex infestation and ocular surface microbiota in patients with Demodex blepharitis. Front Med (Lausanne) 2020;7:592759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Forton FMN. The pathogenic role of demodex mites in rosacea: A potential therapeutic target already in erythematotelangiectatic rosacea? Dermatol Ther (Heidelb) 2020;10:1229–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tarkowski W, Moneta-Wielgoś J, Młocicki D. Do Demodex mites play a role in pterygium development? Med Hypotheses 2017;98:6–10. [DOI] [PubMed] [Google Scholar]
- 33.Zhang XB, Ding YH, He W. The association between demodex infestation and ocular surface manifestations in meibomian gland dysfunction. Int J Ophthalmol 2018;11:589–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gonzalez-Hinojosa D, Jaime-Villalonga A, Aguilar-Montes G, et al. Demodex and rosacea: Is there a relationship? Indian J Ophthalmol 2018;66:36–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ayres BD, Donnenfeld E, Farid M, et al. Clinical diagnosis and management of Demodex blepharitis: The Demodex expert panel on treatment and eyelid health (DEPTH). Eye (Lond) 2023;Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karamursel Akpek E, Merchant A, Pinar V, et al. Ocular rosacea: Patient characteristics and follow-up. Ophthalmology 1997;104:1863–1867. [PubMed] [Google Scholar]
- 37.Sarac G, Cankaya C, Ozcan KN, et al. Increased frequency of Demodex blepharitis in rosacea and facial demodicosis patients. J Cosmet Dermatol 2020;19:1260–1265. [DOI] [PubMed] [Google Scholar]
- 38.Aktaş Karabay E, Aksu Çerman A. Demodex folliculorum infestations in common facial dermatoses: Acne vulgaris, rosacea, seborrheic dermatitis. Anais Brasileiros de Dermatologia 2020;95:187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ziaja-Sołtys M, Kołodziejczyk M, Rymgayłło-Jankowska B, et al. Massive demodicosis of the eyes in a patient with Sjögren syndrome: A case report. Acta Parasitologica 2021;66:677–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flores de Venecia AB, III, Siong RLB. Demodex sp. Infestation in anterior blepharitis, meibomian-gland dysfunction, and mixed blepharitis. Philipp J Ophthalmol 2011;36:15–22. [Google Scholar]
- 41.Bhandari V, Reddy JK. Blepharitis: Always remember demodex. Middle East Afr J Ophthalmol 2014;21:317–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liang L, Ding X, Tseng SCG. High prevalence of demodex brevis infestation in chalazia. Am J Ophthalmol 2014;157:342–348. [DOI] [PubMed] [Google Scholar]
- 43.Huang J, Guo MX, Xiang DM, et al. The association of demodex infestation with pediatric chalazia. BMC Ophthalmol 2022;22:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiao Y, Gao L, Shen L, et al. High load of Demodex in young children with chalazia. J Pediatr Ophthalmol Strabismus 2022;1–7. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 45.Avila MY, Martinez-Pulgarin DF, Rizo Madrid C. Topical ivermectin-metronidazole gel therapy in the treatment of blepharitis caused by demodex spp.: A randomized clinical trial. Contact Lens and Anterior Eye 2021;44:101326. [DOI] [PubMed] [Google Scholar]
- 46.Messaoud R, El Fekih L, Mahmoud A, et al. Improvement in ocular symptoms and signs in patients with Demodex anterior blepharitis using a novel terpinen-4-ol (2.5%) and hyaluronic acid (0.2%) cleansing wipe. Clin Ophthalmol 2019;13:1043–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Savla K, Le JT, Pucker AD. Tea tree oil for Demodex blepharitis. Cochrane Database Syst Rev 2020;6:CD013333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci 2005; 46:3089–3094. [DOI] [PubMed] [Google Scholar]
- 49.Randon M, Liang H, El Hamdaoui M, et al. In vivo confocal microscopy as a novel and reliable tool for the diagnosis of Demodex eyelid infestation. Br J Ophthalmol 2015;99:336–341. [DOI] [PubMed] [Google Scholar]
- 50.Aumond S, Bitton E. Palpebral and facial skin infestation by Demodex folliculorum. Cont Lens Anterior Eye 2020;43:115–122. [DOI] [PubMed] [Google Scholar]
- 51.Luo KS, Xie A, Yang JJ, et al. Critical value of Demodex count per lash for symptomatic and clinical improvement of Demodex blepharitis. Eye (Lond) 2021;36:663–665, online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sędzikowska A, Osęka M, Grytner-Zięcina B. Ocular symptoms reported by patients infested with Demodex mites. Acta Parasitol 2016;61:808–814. [DOI] [PubMed] [Google Scholar]
- 53.O'Dell L, Dierker DS, Devries DK, et al. Psychosocial impact of Demodex blepharitis. Clin Ophthalmol 2022;16:2979–2987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chiang CC, Lin CL, Tsai YY, et al. Patients with blepharitis are at elevated risk of anxiety and depression. PLoS One 2013;8:e83335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ozkan J, Willcox MD. The ocular microbiome: Molecular characterisation of a unique and low microbial environment. Curr Eye Res 2019;44:685–694. [DOI] [PubMed] [Google Scholar]
- 56.Jalbert I, Rejab S. Increased numbers of Demodex in contact lens wearers. Optom Vis Sci 2015;92:671–678. [DOI] [PubMed] [Google Scholar]
- 57.Siddireddy JS, Vijay AK, Tan J, et al. The eyelids and tear film in contact lens discomfort. Cont Lens Anterior Eye 2018;41:144–153. [DOI] [PubMed] [Google Scholar]
- 58.Tarkowski W, Moneta-Wielgoś J, Młocicki D. Demodex sp. as a potential cause of the abandonment of soft contact lenses by their existing users. Biomed Res Int 2015;2015: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nowomiejska K, Lukasik P, Brzozowska A, et al. Prevalence of ocular demodicosis and ocular surface conditions in patients selected for cataract surgery. J Clin Med 2020;9:3069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hirsch-Hoffmann S, Kaufmann C, Banninger PB, et al. Treatment options for demodex blepharitis: Patient choice and efficacy. Klin Monbl Augenheilkd 2015;232:384–387. [DOI] [PubMed] [Google Scholar]
- 61.Yeu E, Wirta DL, Karpecki P, et al. Lotilaner ophthalmic solution, 0.25% for the treatment of Demodex blepharitis: Results of a prospective, randomized, vehicle-controlled, double-masked, pivotal trial (Saturn-1). Cornea 2023;42:435–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Martinez-Pulgarin DF, Avila MY, Rodriguez-Morales AJ. Interventions for demodex blepharitis and their effectiveness: A systematic review and meta-analysis. Cont Lens Anterior Eye 2021;44:101453. [DOI] [PubMed] [Google Scholar]
- 63.Holzchuh FG, Hida RY, Moscovici BK, et al. Clinical treatment of ocular Demodex folliculorum by systemic ivermectin. Am J Ophthalmol 2011; 151:1030–1034. [DOI] [PubMed] [Google Scholar]
- 64.Persi A, Rebora A. Metronidazole and demodex folliculorum. Acta Derm Venereol 1981;61:182–183. [PubMed] [Google Scholar]
- 65.Navel V, Mulliez A, Benoist d'Azy C, et al. Efficacy of treatments for demodex blepharitis: A systematic review and meta-analysis. Ocul Surf 2019;17:655–669. [DOI] [PubMed] [Google Scholar]
- 66.Cheung IM, Xue AL, Kim A, et al. In vitro anti-demodectic effects and terpinen-4-ol content of commercial eyelid cleansers. Cont Lens Anterior Eye 2018; 41:513–517. [DOI] [PubMed] [Google Scholar]
- 67.Karakurt Y, Zeytun E. Evaluation of the efficacy of tea tree oil on the density of demodex mites (acari: Demodicidae) and ocular symptoms in patients with demodectic blepharitis. J Parasitol 2018;104:473–478. [DOI] [PubMed] [Google Scholar]
- 68.Ergun SB, Saribas GS, Yarayici S, et al. Comparison of efficacy and safety of two tea tree oil-based formulations in patients with chronic blepharitis: A double-blinded randomized clinical trial. Ocul Immunol Inflamm 2020;28:888–897. [DOI] [PubMed] [Google Scholar]
- 69.Koo H, Kim TH, Kim KW, et al. Ocular surface discomfort and demodex: Effect of tea tree oil eyelid scrub in demodex blepharitis. J Korean Med Sci 2012; 27:1574–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ngo W, Jones L, Bitton E. Short-term comfort responses associated with the use of eyelid cleansing products to manage Demodex folliculorum. Eye Contact Lens 2018;44:S87–S92. [DOI] [PubMed] [Google Scholar]
- 71.Chen D, Wang J, Sullivan DA, et al. Effects of terpinen-4-ol on meibomian gland epithelial cells in vitro. Cornea 2020;39:1541–1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Huang X, Qin Q, Wang L, et al. Clinical results of intraductal meibomian gland probing combined with intense pulsed light in treating patients with refractory obstructive meibomian gland dysfunction: A randomized controlled trial. BMC Ophthalmol 2019;19:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Craig JP, Chen YH, Turnbull PRK. Prospective trial of intense pulsed light for the treatment of meibomian gland dysfunction. Invest Ophthamol Vis Sci 2015;56:1965–1970. [DOI] [PubMed] [Google Scholar]
- 74.Cheng SN, Jiang FG, Chen H, et al. Intense pulsed light therapy for patients with meibomian gland dysfunction and ocular Demodex infestation. Curr Med Sci 2019;39:800–809. [DOI] [PubMed] [Google Scholar]
- 75.Zhang X, Song N, Gong L. Therapeutic effect of intense pulsed light on ocular demodicosis. Curr Eye Res 2019;44:250–256. [DOI] [PubMed] [Google Scholar]
- 76.Murphy O, O'Dwyer V, Lloyd-McKernan A. The efficacy of tea tree face wash, 1,2-octanediol and microblepharoexfoliation in treating Demodex folliculorum blepharitis. Cont Lens Anterior Eye 2018;41:77–82. [DOI] [PubMed] [Google Scholar]
- 77.Farid M, Ayres BD, Donnenfeld E, et al. Delphi panel consensus regarding current clinical practice management options for Demodex blepharitis. Clin Ophthalmol 2023;17:667–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Toutain CE, Seewald W, Jung M. The intravenous and oral pharmacokinetics of lotilaner in dogs. Parasit Vectors 2017;10:522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gonzalez-Salinas R, Yeu E, Holdbrook M, et al. Safety and efficacy of topical lotilaner ophthalmic solution 0.25% for the treatment of demodex blepharitis: A pilot study. J Ophthalmol 2021;2021:3862684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gonzalez-Salinas R, Karpecki P, Yeu E, et al. Safety and efficacy of lotilaner ophthalmic solution, 0.25% for the treatment of blepharitis due to demodex infestation: A randomized, controlled, double-masked clinical trial. Cont Lens Anterior Eye 2022;45:101492. [DOI] [PubMed] [Google Scholar]
- 81.Gonzalez-Salinas R, Yeu E, Holdbrook M, et al. Collarette elimination and demodex mite eradication with topical lotilaner ophthalmic solution, 0.25%. J Ocul Pharmacol Ther 2021;37:479–484. [DOI] [PubMed] [Google Scholar]
- 82.Gonzalez-Salinas R, Yeu E, Quiroz-Mercado H, et al. Safety and efficacy of lotilaner ophthalmic solution 0.25% for the treatment of Demodex blepharitis: The EUROPA Study. Invest Ophthalmol Vis Sci 2021; 62:1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yeu E, Berdy G, Peterson J, et al. Safety and Efficacy of Lotilaner Ophthalmic Solution, 0.25% in Treating Demodex Blepharitis: Results of the Saturn-2, Pivotal, Phase III Trial. 2022. Chicago: IL: American Academy of Ophthalmology. [Google Scholar]