Abstract
Background:
Wound healing is a complicated biological process that leads to the regeneration of damaged skin tissue. Determining the methods to promote wound healing has become a hot topic in medical cosmetology and tissue repair research. Mesenchymal stem cells (MSCs) are a group of stem cells with the potential of self-renewal and multi-differentiation. MSCs transplantation has a broad application prospect in wound healing therapy. Many studies have demonstrated that the therapeutic capacity of MSCs is mainly mediated by paracrine actions. Exosomes (EXOs), which are nanosized vesicles carrying a variety of nucleic acids, proteins and lipids, are an important component of paracrine secretion. It has been demonstrated that exosomal microRNAs (EXO-miRNAs) play a key role in the function of exosomes.
Methods:
In this review, we focus on current research on miRNAs from MSC-derived exosomes (MSC-EXO miRNAs) in terms of sorting, releasing and function and their effects on inflammation regulation, epidermal cell function, fibroblast function, and extracellular matrix formation. At last, we discuss the current attempts to improve the treatment of MSC-EXO-miRNAs.
Results:
Many studies have demonstrated that MSC-EXO miRNAs play a key role in promoting wound healing. They have been shown to regulate inflammation response, enhance epidermal cell proliferation and migration, stimulate fibroblast proliferation and collagen synthesis, and regulate extracellular matrix formation. Besides, there have been a number of strategies developed to promote MSC-EXO and MSC-EXO miRNAs for wound healing treatment.
Conclusion:
Utilizing the association of exosomes from MSCs with miRNAs may be a promising strategy to promote trauma healing. MSC-EXO miRNAs may provide a new approach to promote wound healing and improve the quality of life for patients with skin injuries.
Keywords: Mesenchymal stem cells, Exosome, microRNA, Wound healing, Therapeutics
Introduction
The skin is a complex organ that acts as an active and passive immune barrier, protecting the body from external damage, and has functions such as perception and controlling body temperature [1]. However, the skin is often damaged by various causes, such as burns, infections and diseases such as diabetic ulcers. Poorly healed wounds often leave visible scars and even functional impairments, which cause a great burden on the patient's life. Conventional treatment methods, such as skin grafts and synthetic dressings, often suffer from limited autologous skin sources and rejection [2]. Therefore, it is important to find better ways to promote wound healing through trauma research.
The application of MSCs has made great strides in the field of wound repair in recent decades. MSCs come from a wide range of sources and can be derived from bone marrow, fat, umbilical cord, amniotic fluid and other sources [3]. Increasingly, studies suggest that the therapeutic effects of MSCs are based on exosome-mediated paracrine effects [4]. Exosomes are closed vesicles with a lipid bilayer, usually 50–200 nm in diameter, rich in a variety of lipids, proteins and nucleic acids (including mRNA, lncRNA, miRNA and circRNA) [5]. Exosomes are found in body fluids, including urine, blood plasma, cerebrospinal fluid, milk, and saliva, and can be secreted by a variety of mammalian cell types, including MSCs, cancer cells, immune cells, and neurons [6]. Exosomes act by transferring cargo to receptor cells and have a unique lipid bilayer structure that protects their contents from degradation [7]. They have been shown to facilitate skin wound healing, modulate inflammatory response, and promote angiogenesis and cell proliferation, among other processes [8].
Many studies have shown that miRNAs play a crucial role in the function of exosomes [9]. miRNAs are a class of evolutionarily conserved endogenous small noncoding RNAs approximately 22 nucleotides in length. miRNAs are known as mRNA regulators that bind the 3′ untranslated or 5′ untranslated regions of target mRNAs, thereby promoting mRNA degradation or translational silencing and negatively regulating the expression of many genes at the posttranscriptional level [10]. Some miRNAs are known to bind to coding regions in addition to untranslated regions [11].
A growing number of studies in recent years have demonstrated that MSC-EXO-derived miRNAs (MSC-EXO miRNAs) may play a therapeutic role in wound healing. In this review, we summarize the process by which miRNA are sorted into exosomes, the role of MSC-EXO miRNAs in wound healing, and current attempts to improve MSC-EXO miRNA treatment (Table 1).
Table 1.
Effects of mesenchymal stem cell-EXO-miRNAs in wound healing
| Effect in wound healing | Exosome source | Nomenclature | Related MSC-EXO miRNAs | Target genes/proteins | Regulation of target gene (up/down) | Outcome | References |
|---|---|---|---|---|---|---|---|
| Regulation of the inflammatory response | Human umbilical cord (UC)-MSCs | Exosomes | let-7b |
TLR4/NF-κB STAT3/Akt |
Down Up |
Induced M2 macrophage polarization and alleviated wound inflammation in rats | [67] |
| Hypoxic preconditioned dental pulp stem cell(DPSC) | Small extracellular vesicles | miR-210-3p | NF-κB1 | Down | Induced M2 macrophage polarization | [68] | |
| Human UC-MSCs | Exosomes | miR-181c | TLR4/ NF- κB/P65 | Down |
Induced M2 macrophage polarization TNF-α, IL-1β, TLR4↓ IL-10 ↑ |
[70] | |
| MSCs after IL-1β pretreatment | Extracellular vesicles | miR-21 | Programmed cell death factor 4 (PDCD4) | Down | Induced M2 macrophage polarization | [71] | |
| Human jaw bone marrow-derived MSCs and bone marrow MSCs | Exosomes | miR-223 | Pknox1 | Down |
Induced M2 macrophage polarization TNF-α ↓ IL-10, RELM-α,arginase 1 (Arg1)↑ |
[73] | |
| Promoting angiogenesis | Human adipose-derived MSCs (adMSC-Exo) | Exosomes | miR-125a | Angiogenic inhibitor delta-like 4 (DLL4) | Down | Promoted endothelial cells angiogenesis | [75] |
| Human adipose-derived MSCs (hADSCs) | Exosomes | miR-125a-3p | PTEN | Down | Promoted HUVEC viability and migration | [76] | |
| Human adipose-derived MSCs (hADSCs) | Exosomes | miR-423-5p | Suppressor of fused(Sufu) | Down | Promoted angiogenesis | [77] | |
| Deferoxamine pretreated BM-MSCs | Exosomes | miRNA- 126 |
PTEN PI3K/Akt |
Down Up |
Promoted angiogenesis | [78] | |
| Bone marrow MSC | Exosomes | miRNA-126 | PIK3R2/PI3K/Akt | Up | Enhanced the formation of new capillaries at the site of skin wounds in mice | [79] | |
| Human umbilical cord blood plasma (UCB-Exos) | Exosomes | miR-21-3p | PTEN and SPRY1 | Down | Promote fibroblast and endothelial cells proliferation and migration | [80] | |
| Human umbilical cord (UC)-MSCs | Exosomes | miR-21 | NOTCH1/DLL4 pathway | Up | Promote proliferation and migration of endothelial progenitor cells (EPCs) | [81] | |
| Promoting skin cell proliferation and migration | Human amnion mesenchymal stem cells | Exosomes | miR-135a | LATS2 | Down | Promoted fibroblast proliferation and migration | [83] |
| human amniotic mesenchymal stem cell (hAMSC) | Exosomes | miR-135a | E-cadherin, N-cadherin, LATS2 | Down | Promoted fibroblast proliferation and migration | [84] | |
| MSC | Exosomes | miR-138-5p | SIRT1 | Down | Inhibited fibroblast growth | [85] | |
| Human adipose-derived MSCs (hADSCs) | Exosomes | miR-126-3p | PIK3R2 | Down | Promoted fibroblast proliferation and migration | [86] | |
| Adipose derived stem cell | Exosomes | miRNA-21 | PI3K / AKT/ MMP-9 | up | ↑MMP-9, enhanced migration and proliferation of HaCaT cell | [87] | |
| Promoting collagen remodeling and apoptosis | Human adipose-derived MSCs (hADSCs) | Exosomes | miRNA-29a | TGF-β2/Smad3 | Down | ↓α-SMA, Col-I, Col-III, reduced scar formation | [89] |
| Human umbilical cord (UC)-MSCs | Exosomes | miR-21, -23a, -125b, -145 | TGF-β/SMAD2 | Down | Inhibited collagen deposition, reduced scar formation | [90] | |
| Human adipose-derived MSCs (hADSCs) | Exosomes | miRNA-192-5p | IL-17RA/Smad | Down | ↓Col1, Col3, α-SMA, p-Smad2/p-Smad3, reduced scar formation | [91] | |
| human amniotic fluid stem cell(hAFSC) | Exosomes | let-7-5p, miRNA-22-3p, miRNA-27a-3p, miRNA-21-5p, miRNA-23a-3p | TGF-β1/2 | Down | Prevented fibroblasts from differentiating into myofibroblasts and reduced scar formation | [93] |
MSCs Mesenchymal stem cells; EXOs exosomes; miRNA: microRNA; EVs Extracellular vesicles; ILVs Intraluminal vesicles; IL Interleukin; MVBs Multivesicular bodies; EGF Epidermal growth factor; PDGF Platelet-derived growth factor; TGF-β Transforming growth factor; VEGF Vascular endothelial growth factor; BMSC Bone marrow-derived stem cells; MMP Matrix metalloproteinases; FGFs Fibroblast growth factors; TIMP1 Tissue inhibitor of metalloproteinase 1; TNF-a Tumor necrosis factor alpha; IFNs Interferons; ECM Extracellular matrix; hUC Human umbilical cord; hBM Human bone marrow; BM-MSC Bone marrow MSC; JMMSC Jaw bone marrow MSC; HDFs Human dermal fibroblasts; HaCaTs Human keratinocytes; LPS Lipopolysaccharide; ASC Human adipose mesenchymal stem cell; HUVECs Human umbilical vein endothelial cells; DLL4 Delta-like 4
The process of wound healing
The healing process of skin wounds consists of four overlapping phases: hemostasis, inflammation, proliferation, and remodeling [12].
Hemostasis occurs in the first stage of wound injury. After vascular injury, exposed subendothelial collagen in the vessel activates nearby platelets, leading to the formation of a “platelet plug” [13]. The coagulation cascade is activated, and fibrinogen is converted to fibrin by thrombin, forming a fibrin network and eventually a clot [14]. The clot not only effectively stops bleeding but also acts as a scaffold for immune cells during the inflammatory phase. Platelet degranulation releases many cytokines, including platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF) and transforming growth factor-β (TGF-β), which promote inflammatory cell infiltration and induce the proliferation and migration of vascular endothelial cells and fibroblasts [15] (Fig. 1)
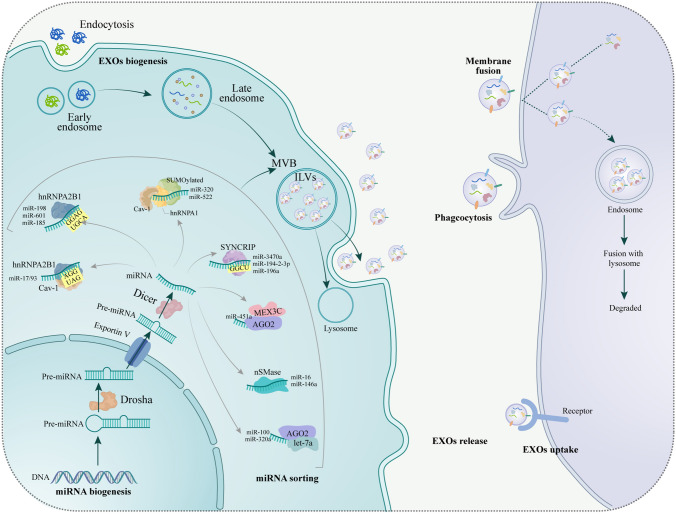
Fig. 1.
Biogenesis, sorting, releasing and uptaking of miRNAs from MSC-derived exosomes. After miRNAs and EXOs are generated, some miRNAs specifically bind to RNA-binding proteins or membrane proteins according to specific motifs in miRNAs and are transported to EXOs by them. An RNA-binding proteins or membrane proteins can bind to different miRNAs with the same motifs. An RNA-binding proteins or membrane proteins also bind to more than one motif miRNA. EXOs are released extracellular through exocytosis, and miRNA can be protected from extracellular degradation under the protection of EXOs. Recipient cells absorb released EXOs through three mechanisms. (1) Direct fusion with the plasma membrane, (2) Phagocytosis, (3) Receptor-mediated endocytosis
The key cells in the inflammatory phase are neutrophils and macrophages [16]. In the initial phase of inflammation, neutrophils rapidly migrate to the site of injury to clear microorganisms and subsequently recruit macrophages [17]. In the later stages of inflammation, proinflammatory M1-type macrophages are replaced with anti-inflammatory M2 macrophages [18]. Wound healing moves from the inflammatory phase to the proliferative phase, which is a critical step in normal wound healing. M2 macrophages produce anti-inflammatory factors that promote skin cell proliferation, stimulate extracellular matrix (ECM) synthesis and remodeling, and promote angiogenesis [19]. During this phase, the release of inflammatory cytokines promotes angiogenesis and recruits keratinocytes and fibroblasts to the site of damage [20].
In the proliferation phase, fibroblast growth factor (FGF) and VEGF mediate endothelial cell proliferation, migration, and formation of new blood vessels [21]. In addition, fibroblasts proliferate and migrate to the site of injury with the help of TGF-β and VEGF to produce type I and type III collagen and form ECM, which together with new capillaries and inflammatory cells form granulation tissue. Some fibroblasts also differentiate into myofibroblasts, causing contraction of the wound margins [22]. In addition, fibroblasts secrete growth factors that stimulate the proliferation and migration of keratinocytes, promoting wound re-epithelialization and reestablishing the skin epidermal barrier (Fig. 2).
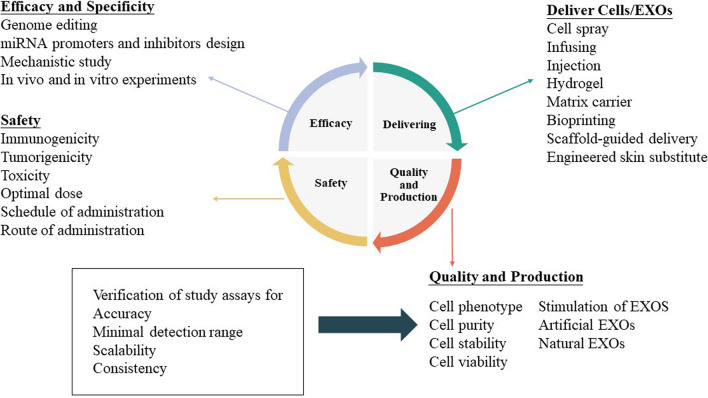
Fig. 2.
The current and future direction of exosomal miRNAs. Now many researchers are studying and future directions will focus on efficacy and specificity, delivery, safety, quality and production. How to design suitable miRNA promoters and miRNA inhibitors, and how to use gene modification to make MSC-exos more effective and safer. To further explore the mechanism of exosomeal miRNA, conduct in vivo and in vitro experiments to prepare for clinical use. In terms of safety, immunogenicity, tumorigenicity and toxicity should be concerned, and the optimal dose, route of administration schedule and route of administration should be determined. Quality consistency and mass production capacity require constant attention, and remarkable results have been achieved so far. Strategies for Delivering Cells/EXOs currently include cell spray, infusing, injection, hydrogel, matrix carrier, bioprinting, scaffold-guided delivery, engineered skin substitute
During the remodeling phase, myofibroblast apoptosis makes room for ECM remodeling [23]. During ECM remodeling, old ECM is degraded by matrix metalloproteinases (MMPs), and collagen III is converted to collagen I, thereby reducing scar size and improving tensile strength [24].
Role of MSC-EXOs in wound healing
A large body of literature suggests that MSC-EXOs or MSC-EVs can accelerate wound healing by targeting the different stages of wound healing.
Anti-inflammatory and immunomodulatory functions
The inflammatory response is an important phase that regulates wound repair, and multiple inflammatory cells and inflammatory factors are synergistically involved in the inflammatory response against infection. However, prolonged inflammation can lead to excessive wound scar formation, as in the case of chronic refractory wounds in diabetes. Macrophages play a crucial role in the late phase of inflammation, especially the polarization of M1-type macrophages into M2-type macrophages. If the M1-M2 phenotypic transition does not occur, the wound becomes chronically refractory [25]. Many publications have shown that MSC-Exos can induce M2 macrophage polarization and reduce the persistent inflammation that leads to prolonged wound healing [26–28]. Melatonin (MT)-pretreated MSC-EXOs increased the ratio of M2 to M1 polarization by activating the PTEN/AKT signaling pathway and accelerated the healing of skin injury in diabetic mice by inhibiting the expression of the proinflammatory factors IL-1β and TNF-α and promoting the expression of the anti-inflammatory factor IL-10 [26]. Hypoxic ADSC-EXOs delivering circ-Snhg11 induced M2 macrophage polarization and enhanced wound healing in diabetic mice by binding miR-144-3p to promote HIF-1α expression [27].
Promoting angiogenesis
The angiogenic phase of skin healing is largely dependent on the proliferation of endothelial cells and the action of angiogenesis-related factors. MSC-EXOs can serve as a direct signal for endothelial cells to initiate angiogenesis. VEGF is a potent proangiogenic factor that can act at the early stage of angiogenesis to promote endothelial cell proliferation and migration. Han et al. [29] found that hADSC-EXOs under hypoxia could promote neovascularization in mice by regulating VEGF/VEGF-R. Liu et al. [30] found that exosomes derived from Huc-MSC-EXOs improved wound healing in rats with deep second-degree burns by transferring angiopoietin-2 to promote the migration and tube-forming ability of vascular endothelial cells.
Regulating the migration and proliferation of skin cells
Cell proliferation and migration form the basis of wound repair. Wound healing requires the migration of fibroblasts and epithelial cells to the wound site to perform specific functions, such as fibroblasts filling tissue defects and synthesizing ECM and epithelial cells gradually covering the wound [31]. Many studies have shown that MSC-EXOs can regulate the proliferation and migration of fibroblasts and affect collagen synthesis by regulating the expression of growth factors and related genes. Li et al. [32] found that lncRNA H19 in hBMSC-EXOs binds to miR-152-3p in fibroblasts and inhibits the expression of phosphatase and tensin homolog (PTEN) while activating the PI3K/AKT signaling pathway, promoting fibroblast proliferation and migration and inhibiting their apoptosis to accelerate the healing of diabetic foot skin ulcers. On the other hand, Bin et al. [33] suggested that under high cell density, human umbilical cord MSC-derived exosomes (hUC-MSC-EXOs) inhibit fibroblast proliferation and migration by delivering protein 14–3-3ζ, which induces YAP phosphorylation and thus inhibits the Wnt/β-catenin signaling pathway to prevent tissue overproliferation.
Moreover, Wang et al. [34] suggested that ADSC-EXOs could inhibit scar formation by acting on fibroblasts and adjusting the type III/type I collagen ratio. In conclusion, the above studies suggest that the regulatory function of MSC-EXOs on fibroblasts can play a dual role in promoting wound healing and inhibiting scar formation during the wound repair process.
The promoting effect of MSC-EXOs on human immortalized epidermal HaCaT cells has also been reported. In one study, ADSC-EXOs were found to inhibit HaCaT cell apoptosis by activating Wnt/β-catenin signaling [35]. Human amniotic MSCs (hAMSCs) and hAMSC conditional medium (CM) inhibit heat stress-induced HaCaT cell apoptosis through the PI3K/AKT signaling pathway, thereby accelerating wound re-epithelialization in rats with skin burns [36]. In another study, adipose stem cell-derived microvesicles (ASC-MVs) were found to enhance HaCaT cell function through the AKT and ERK signaling pathways [37].
Regulating extracellular matrix remodeling
Insufficient or excessive ECM formation can lead to failure of wound healing or scar formation, and the key to ECM remodeling is collagen synthesis and degradation. In the early stages of wound healing, MSC-EXOs promote wound healing by promoting collagen I (Col-1) and III (Col-3) deposition [38]. In contrast, MSC-EXOs can inhibit collagen synthesis and thus reduce scar formation in the late stage of wound healing [39]. HADSC-EXOs inhibited the production of ECM in keloids by suppressing the production of Col-1 and Col-3 [40]. The effect of MSC-EXOs in inhibiting collagen synthesis was associated with upregulation of MMP family expression levels. In the presence of TGF-β1, hADSC-EXO treatment resulted in an upregulation of MMP1 and MMP3 expression levels and a significant downregulation of COL-1 and COL-3 expression levels in fibroblasts [41]. Furthermore, uncontrolled accumulation of myofibroblasts in wounds leads to scar formation. HADSC-EXOs reduce scarring by blocking the differentiation of fibroblasts to myofibroblasts and increasing the ratios of Col-1 to Col-3, TGFβ3 to TGFβ1, and MMP3 to TIMP1 [34]. One study found that hUC-MSC-EXOs reduce Col-1 and Col-3 production in part by inhibiting the TGF-β1/Smad2/3 signaling pathway, a pathway that also inhibits fibroblast differentiation into myofibroblasts [42].
miRNAs in exosomes
Biogenesis of microRNAs and exosomes
miRNAs are first transcribed in the nucleus, and then the resulting pri-miRNAs are converted into pre-miRNAs by Drosha and transferred from the nucleus to the cytoplasm by Transportin-5. The pre-miRNA becomes a single-stranded miRNA under Dicer processing. A portion of the miRNA then binds to RNA-binding proteins and membrane proteins according to the specific sequence of the miRNA. miRNAs function in EXOs mainly in the biofunctional pre-miRNA form rather than in the mature form [43].
During the biogenesis of exosomes, the cytoplasmic membrane invaginates, gathering some extracellular components and cell membrane proteins to form early endosomes. Early endosomal membranes invade inward and form intraluminal vesicles (ILVs) with the involvement of endosomal-sorting complexes required for transport (ESCRTs). These early endosomes may exchange material with other organelles or fuse between different early endosomes to form late endosomes that mature into multivesicular bodies (MVBs). MVBs fuse with the cell membrane and secrete ILVs outside the cell, and the released ILVs are called exosomes. A portion of the MVB may also be degraded by fusion with autophagosomes or lysosomes [44].
miRNAs are sorted into exosomes
Many studies have shown that miRNAs can be selectively secreted into exosomes. One study compared the miRNA content between MSC-EVs and their parent MSCs. In another study, the level of miR-21-5p in exosomes was found to be 100-fold higher than that in hUC-MSCs [45]. One study found that the five most abundant miRNAs in MSC exosomes were miR-21, let-7 g, miR-1246, miR-381 and miR-100 compared with MSCs [46]. In addition, miRNAs in exosomes from different MSC sources differ. For example, the most abundant miRNAs in BM-MSC exosomes are miR-143-3p, miR-10b-5p, miR-486-5p, miR-22-3p and miR-21-5p, whereas the most common miRNAs in adipose-derived MSC (ASC) exosomes are miR-486-5p, miR-10a-5p, miR-10b- 5p, miR-191-5p and miR-222-3p [47]. In conclusion, these studies suggest the existence of mechanisms that control the active sorting of miRNAs into exosomes.
To elucidate the specific mechanism of miRNA sorting into exosomes, researchers have analyzed the sequences of relevant miRNAs and identified numerous miRNA motifs associated with miRNA sorting. Changing the motifs of specific miRNAs can alter the enrichment of miRNAs in exosomes. In addition, researchers have identified specific proteins that regulate the entry of miRNAs into exosomes, and the feasibility of adding specific motifs to miRNAs to promote their enrichment in exosomes has been demonstrated [48].
Different RNA-binding proteins, such as hnRNP and AGO2, bind to miRNAs according to specific sequences in the miRNA and transport them into exosomes. The hnRNP-binding protein family is an important player in miRNA sorting into exosomes. Interestingly, the same hnRNP can bind to miRNAs containing different specific motifs. For example, hnRNPA2B1 binds miR-198, miR-601 and miR-185 via the GGAG/UGCA motif and is then transported to the exosome [49, 50]. Another report showed that hnRNPA2B1 can also bind miR-17/93 via the AGG/UAG motif [51]. hnRNPA2B1 can also negatively regulate the exosomal sorting of microRNAs, such as by inhibiting the exosomal export of miR-503 in endothelial cells [52]. SUMOylated hnRNPA1 binds miR-17/93 via caveolin-1 (CAV1) and is involved in sEV-miRNA loading with the help of miR-196a, miR-320 and miR-522 [53]. In addition, SYNCRIP, also known as hnRNP-Q, can bind to miRNAs containing GGCU sequences, such as miR-3470a and miR-194–2-3p, loading them into exosomes [54]. AGO2, a core component of the miRISC complex, can bind to let-7a, miR-100 and miR-320a through the KRAS-MEK-ERK signaling pathway and lead to exosome sorting [55]. In addition, AGO2 may act as an intermediary between MEX3C and miR-451a, assisting the targeting of MEX3C by siRNA molecules and leading to decreased exosomal miR-451a [56]. In conclusion, many RNA binding proteins were shown to be associated with miRNA sorting into exosomes, such as La protein, LIN28, SRP9/14, QKI, TERT, ELAVL1, IGF2BP1, ANXA2, ALIX, Nucleolin, and FUS/TDP-43.
Different membrane proteins can also bind to miRNAs based on specific sequences in the miRNA to transport them into exosomes. nSMase2 was the first molecule reported to be associated with miRNA secretion into exosomes. nSMase2 can specifically sort miR-16 and miR-146a into EVs [57]. CAV1 is a membrane-bound protein that binds miRNAs and loads them into exosomes via the AsUGnA motif [58]. In addition, CAV1 can mediate the encapsulation of hnRNPA1 and its bound miRNA into microvesicles [53]. Cav-1 can also form a complex with hnRNPA2B1, which enhances hnRNPA2B1 binding to mir-17/93 and directs the complex into exosomes [51]. The mechanism of sEV cargo loading by CAV1 is related to the sEV-miRNA sorting protein YBX1. Although several molecular mediators have been identified, the mechanism of miRNA selective sorting into EVs remains elusive.
Uptake of miRNA-containing exosomes by recipient cells
Exosomes can protect miRNAs from degradation during transport to target cells. Chen-Yu Zhang's team proposed two models [59] to explain the stability of extracellular miRNAs: protection of miRNAs by EV membrane structures and stabilization of miRNAs by forming protein–miRNA complexes.
Receptor cells take up the released exosomes through three different mechanisms: (1) direct fusion with the plasma membrane, (2) phagocytosis, and (3) receptor-mediated endocytosis.
The contents of phagocytosed exosomes may be released directly into the cytoplasm and exert a regulatory effect, or they may enter the endosome and subsequently fuse with lysosomes, whose contents are degraded. Additionally, exosomes may naturally contain some endosomal escape mechanisms, which may trigger a functional response once the miRNA in the exosome escapes the degradation pathway. However, to date, these mechanisms remain unknown. There is still controversy about whether exosomal miRNAs can enter recipient cells to affect recipient cell function. In one study, it was suggested that microRNAs in extracellular vesicles are rarely delivered to target cells [60]. However, there are limitations to the study: EBV-infected primary human B-cell activity is affected, and all experiments were performed in vitro using artificial setups, which is not a completely accurate representation of the in vivo situation. Another issue is the use of viral miRNA, which may not fully reflect the host cell-secreted miRNA contained in EV, and only a limited number of cell line-derived extracellular vesicles were studied, which is not of general interest. It has been shown that exosomal miRNAs can be transferred to recipient cells and thus affect the function of the recipient cells. In 2007, Valadi et al. first demonstrated that exosomal miRNAs can be transferred to another cell [61]. One investigator cocultured miRNA-126-3p-transfected hUC-MSCs with HUVECs and showed that miRNA affects the function of HUVECs through exosomal transfer between cells [62].
In addition to the classical repressive effects of targeting mRNAs, recent evidence suggests that miRNAs can also promote gene expression under specific conditions [63]. Professor Yu's laboratory at Fudan University proposed the concept of intranuclear activated miRNAs, which can bind to enhancers in the nucleus to promote gene expression, opening up new paths in the field of miRNA research [64]. In addition, exosomal miRNAs have different roles from intracellular miRNAs. In 2012, exosomal miR-21 and miR-29a were found for the first time to have the ability to bind to Toll-like receptors (TLRs) and activate ligands in immune cells [65]. Recent studies have found that miRNAs released from injured neurons can activate TLR7/8 [66].
miRNAs in exosomes of mesenchymal stem cells regulate wound healing
Regulation of the inflammatory response
A large number of studies have focused on MSC-EXO miRNAs to promote M2 macrophage polarization and thus reduce the inflammatory response. Under simulated inflammatory conditions, let-7b specifically expressed in hUC-MSC-EXOs drives macrophage differentiation toward an anti-inflammatory phenotype by downregulating TLR4/NF-κB as well as upregulating the STAT3/Akt signaling pathway, reducing inflammatory cell infiltration in traumatic surfaces [67]. Small extracellular vesicles derived from hypoxic preconditioned dental pulp stem cells (DPSCs) inhibit NF-kB1 expression, induce M2 macrophage polarization and suppress inflammatory responses [68]. hUC-MSC-EXOs contain three specific miRNAs (miR-181c, miR-21, and miR-146a) that have a regulatory function in inflammation [69]. In a study on a mouse burn model, miR-181c in hUC-MSC-EXOs reduced the number of macrophages at the burn site, inhibited the TLR4 signaling pathway, downregulated the activity of its downstream target protein NF-κB/P65, promoted M2 macrophage polarization, blocked the release of the inflammatory factors IL-1β and TNF-α, and promoted the expression of the anti-inflammatory factor IL-10, thereby inhibiting inflammatory and immune responses and promoting burn healing [70]. It was found that miR-21 expression was significantly upregulated in MSCs and their EVs after IL-1β pretreatment, mediating macrophage polarization toward the M2 type by inhibiting the programmed cell death factor 4 (PDCD4) gene in macrophages [71]. After IL-1β stimulation, hUCBMSCs overexpress miR-146a and are loaded into exosomes, which are taken up by macrophages and then mediate the macrophage polarization toward the M2 type [72]. In addition, He et al. [73] found that miR-223 in BM-MSC-EXOs induced M2 macrophage polarization by inhibiting pknox1 protein levels, resulting in increased expression of RELM-α and arginase 1 (Arg1), increased expression levels of the inflammatory mediator IL-10, and decreased expression levels of TNF-α, which accelerated skin wound healing in mice. In another report, after treatment of fibroblast-based model of inflammation with ADSC-EXOs,the researchers observed a significant decrease in protein levels of TNF-α, IL-6 and IL-8 and increase in IL-10 concentration. Further studies found that because the combination of miR-34a-5p, miR-124-3p, miR-146a-5p, miR-132, miR-21 and miR-29a was highly expressed in ADSC-EXOs, it could reduce inflammation and enhance wound healing [74].
Promoting angiogenesis
In ADSC-EXOs, miR-125a and miR-423-5p have been shown to have angiogenic potential. Among them, miR-125a can inhibit the transcription and expression of the angiogenic repressor inhibiting delta-like 4 (DLL4), which promotes endothelial cell angiogenesis by promoting the formation of endothelial tip cells [75]. Another study found that miR-125a-3p in hADSC-EXOs promoted the viability of HUVECs and facilitated wound healing in mice by inhibiting PTEN [76]. ADSC-EXOs enriched with miR-423-5p downregulated the expression of serine kinase inhibitor (suppressor of fused, Sufu) in endothelial cells [77]. MSC-EXO miRNAs can act on the PI3K/Akt signaling pathway to affect angiogenesis. Ding et al. [78] found that miRNA-126 carried by deferoxamine-pretreated BMSC-EXOs exhibited a stronger ability to promote angiogenesis than normal BMMS exosomes in vitro and in vivo by downregulating PTEN and activating the PI3K/Akt signaling pathway, thereby accelerating wound healing in diabetic rats. Further studies found that BM-MSC-EXO miR-126 processing affected angiogenesis by targeting PIK3R2 to activate the PI3K/Akt signaling pathway, which contributes to enhanced neo-capillary formation at skin wound sites in mice [79]. Human umbilical cord blood plasma (UCB-EXOs) are highly enriched in miR-21-3p, which can downregulate the expression of PTEN and SPRY1 and thus regulate the PI3K/Akt and ERK1/2 signaling pathways to promote angiogenesis of endothelial cells [80]. Further studies revealed that miR-21 in umbilical MSC-derived exosomes (uMSCEXOs) promotes proliferation, migration of endothelial progenitor cells (EPCs), and angiogenesis in rats with cranial defects by upregulating the NOTCH1/DLL4 pathway [81].
Promoting skin cell proliferation and migration
Analysis by miRNA microarray revealed that 292 miRNAs were altered in ADSC-EXOs that promoted the proliferation and differentiation of dermal fibroblasts, of which 199 were upregulated and 93 were downregulated [82]. MiR-135a in human amnion mesenchymal stem cell (hAMSC)-EXOs downregulates LATS2 expression, thereby promoting fibroblast migration and wound healing in rat skin [83]. Further studies revealed that miR-135a in hAMSC-EXOs inhibited the expression of E-cadherin, N-cadherin, and LATS2, promoted the expression of α-SMA, and promoted fibroblast migration [84]. Additional studies found that MSC-EXOs downregulate SIRT1 through miR-138-5p delivery, thereby inhibiting fibroblast growth and protein expression and alleviating pathological scarring [85]. ADSC-derived exosome-loaded miR-126-3p promotes fibroblast proliferation and migration through downregulation of PIK3R2 expression to promote wound healing in rats [86].
Positive effects of MSC-EXO miRNAs on keratinocytes have also been reported: it was shown that adipose-derived stem cell exosomes (AD-EXOs) overexpressing miRNA-21 enhanced the migration and proliferation of HaCaT cells by increasing MMP-9 expression through the PI3K/AKT pathway [87]. The experimental results of Wang et al. [88] demonstrated that miRNA-21 was able to mediate TGF-β1 by targeting PTEN (downregulation) to promote mesenchymal transition and migration of keratinocytes during skin wound repair.
Promoting collagen remodeling and apoptosis
Excessive synthesis or insufficient degradation of collagen can lead to scar formation. MSC-EXO miRNAs can inhibit the expression of Col-I and Col-III, thereby reducing scar formation. Subcutaneous injection of ADSC-EXO with high miRNA-29a expression in a mouse skin scald model had a significant effect on promoting thermal injury healing, and the mechanism of action was that miRNA-29a suppressed the expression levels of the fibrosis genes α-SMA, Col-I, and Col-III by inhibiting the TGF-β2/Smad3 signaling pathway [89]. Similarly, Fang et al. [90] found that hUC-MSC-EXOs could reduce scar formation in skin-deficient mice by transferring microRNAs (miR-21, miR-23a, miR-125b, and miR-145) to inhibit collagen deposition through suppression of the TGF-β2/SMAD2 pathway. In addition, miRNA-192-5p, which is highly expressed in ADSC-EXOs, promoted scar-free healing of wounds by downregulating IL-17RA expression in HSFs and reducing the expression levels of Col1, Col3, α-SMA and p-Smad2/p-Smad3 [91].
Overdifferentiation of myofibroblasts leads to the formation of fibrotic scars on the trauma surface. TGF-β is an important regulator that stimulates the differentiation of fibroblasts into myofibroblasts, and MSC-EXOs can reduce scar formation by inhibiting the expression of TGF-β. Exosomal miRNA-4255p and miRNA-142-3p can inhibit the differentiation of human dermal fibroblasts to myofibroblasts by reducing TGF-β1 expression, ultimately reducing scar formation to promote wound healing [92]. Let-7-5p, miRNA-22-3p and miRNA-27a-3p in human amniotic fluid stem cell-derived exosomes (hAFSC-exo) downregulate TGF-β1, and miRNA-21-5p and miRNA-23a-3p downregulate TGF-β2, which in turn prevents fibroblasts from differentiating into myofibroblasts to reduce scar formation [93].
Current attempts to improve the treatment of MSC-exo miRNAs
Genetic modification of miRNAs by CRISPR/Cas9 technology
Because altering the motifs of specific miRNAs can change the enrichment of miRNAs in exosomes, it is possible to use CRISPR/Cas9 technology to modify miRNA sequences so that specific miRNAs can be enriched in exosomes. In one study, artificially engineered extracellular vesicles were constructed for the delivery of CRISPR/Cas9-edited miR-29b (EV-Cas9-29b) to alleviate denervation-induced muscle atrophy in mice [94]. Researchers developed an artificial exosome in which the CD63-Cas9 protein of the exosome was fused, and verified the efficiency of removing the target gene from the recipient cell [95].
Use of MSC-EXOs as therapeutic miRNA delivery vehicles
The use of exosomes for noncoding RNA delivery, and thus for the treatment of diseases, has been extensively studied in the field of oncology. There are two forms of miRNA-based therapies. (1) Loading exogenous miRNA mimics that are known to promote tumor suppression. For example, miR-6785-5p mimics were loaded into human umbilical cord MSC-derived exosomes to treat gastric cancer by inhibiting INHBA gene expression and suppressing cellular angiogenesis and metastasis [96]. (2) Provide specific miRNA inhibitors to suppress tumor-promoting miRNAs. For example, delivery of LNA-antimiR-142-3p into breast cancer stem cells via BM-MSC-EXOs resulted in downregulation of miR-142-3p and miR-150, thereby reducing the proliferation capacity of breast cancer stem cells [97].
In view of the above studies, MSC-EXOs can be used as a vehicle to deliver miRNA mimics or specific miRNA inhibitors to promote wound healing.
Engineering to enhance the efficacy and production of EXOs
Current research has proposed many ways to modify MSCs or combine them with other materials to improve their therapeutic potential. Compared to normal exosomes, H2O2-ADSC-EXOs led to more improved flap survival and promoted neovascularization for cell-free therapeutic applications in flap grafts [98]. In addition, combined with selenium, the effects of ADSC-EXOs on inhibiting inflammation and promoting angiogenesis were significantly enhanced [99]. Many studies have focused on the development of optimized hydrogels for the construction of mesenchymal stem cell-derived exosome delivery platforms [100–102]. In one study, polyvinyl alcohol (PVA)/alginate (Alg) nanohydrogel was used to encapsulate hUC-MSC-exos [101]. In another study, researchers constructed gel methacrylate (GelMA)/carbohydrate-catechol (Chi-C) hydrogels to encapsulate hUC-MSC-exos [102]. The results showed that the hydrogel-bound mesenchymal stem cells were valuable in angiogenesis and the re-epithelialization of chronic wounds. These novel hydrogels can maintain the bioactivity of exosomes, improve the efficacy of exosome delivery, and enhance the ability of exosomes to promote wound healing, and they have the characteristics of low toxicity, an appropriate degradation rate, and strong plasticity. Therefore, they have promising applications.
Over the last decade, there have been a number of strategies developed to promote large scale EV generation, Including through various stimulants such as protein regulations, thermal and oxidative stress, hypoxia, pH, radiation, starvation, chemicals, and culture environment to stimulate cells to produce more exosomes. Another approach is through physical and chemical methods such as nitrogen plantations, extrusion through porous membrane, sonication, dissolving in high pH breaking the cell membrane and reconstructing the released contents to synthesize artificial EV. In addition, there are large-scale generation of natural EVs using chemicals, red blood cells, cellular nanoporation, bioreactors and 3D scaffolds [103].
Conclusion
MSC-EXOs, as intercellular communication vectors, carry miRNAs that regulate the inflammatory response and promote angiogenesis, showing encouraging applications in trauma repair. Compared with MSCs, MSC-EXOs have the advantages of high stability and safety, and more importantly, they can be engineered to enhance their trauma healing effect by regulating the miRNAs they carry. MSC-EXO miRNAs have been shown to regulate the wound healing process.
The problems that once troubled us have been gradually solved in recent years. First, “quality consistency” and “mass production capacity” used to be the two most critical points for stem cell drug development. However, MSCs differentiated from embryonic stem cells through Emstein’s patented two-step cell differentiation technique are capable of continuous homogenization and mass production [104]. This undoubtedly breaks through the barrier that adult derived MSCs are difficult to produce drugs. What’s more, MSCs spheroids can be delivered under ambient conditions for tolerating room temperature for more than 10 days [105]. Second, effectiveness and safety. Future research will focus on how to design suitable miRNA promoters and miRNA inhibitors and how to modify MSC-EXOs to make them more effective and safer. To improve biosafety, the UM team inserted a suicide gene into the stem cell genome, which can be triggered by an injection of a simple drug after wound healing to kill the remaining stem cells and their derived cells, thereby avoiding tumour fears [105]. Third, there is the issue of specificity. Natural exosomes still have some limitations as delivery platforms. For example, exosomes are not taken up only by the site of injury, and the load will be delivered nonselectively to all cell types in vivo, reducing miRNA utilization. Genetic engineering techniques need to be developed to achieve cell-specific targeting. In addition, there is a need to determine the optimal dose and schedule of MSC-EXO miRNA administration, as well as the route of administration that achieves maximum efficacy with minimal adverse effects. With the in-depth discussion of related issues and the translational application of basic research results, MSC-EXO miRNAs will become an effective biological therapy and lead to new trauma treatment options.
Acknowledgement
This work was supported by the National Natural Science Foundation of China under Grant Number 81460293.
Author contributions
JCC contributed to the investigation, data curation, and manuscript writing; LDW supervised the study.
Declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical statement
There were no animal or human subject experiments carried out for this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dyring-Andersen B, Løvendorf MB, Coscia F, Santos A, Møller LBP, Colaço AR, et al. Spatially and cell-type resolved quantitative proteomic atlas of healthy human skin. Nat Commun. 2020;11:5587. doi: 10.1038/s41467-020-19383-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu JC, Zheng CX, Sui BD, Liu WJ, Jin Y. Mesenchymal stem cell-derived exosomes: A novel and potential remedy for cutaneous wound healing and regeneration. World J Stem Cells. 2022;14:318–329. doi: 10.4252/wjsc.v14.i5.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun L, Wang F, Chen H, Liu D, Qu T, Li X, et al. Co-Transplantation of human umbilical cord mesenchymal stem cells and human neural stem cells improves the outcome in rats with spinal cord injury. Cell Transplant. 2019;28:893–906. doi: 10.1177/0963689719844525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yan L, Wu X. Exosomes produced from 3D cultures of umbilical cord mesenchymal stem cells in a hollow-fiber bioreactor show improved osteochondral regeneration activity. Cell Biol Toxicol. 2020;36:165–178. doi: 10.1007/s10565-019-09504-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu Y, Luo Y, Fang Z, Teng W, Yu Y, Tian J, et al. Mechanism of sanguinarine in inhibiting macrophages to promote metastasis and proliferation of lung cancer via modulating the exosomes in A549 Cells. Onco Targets Ther. 2020;13:8989–9003. doi: 10.2147/OTT.S261054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nair VD, Ge Y, Li S, Pincas H, Jain N, Seenarine N, et al. Sedentary and trained older men have distinct circulating exosomal microRNA profiles at baseline and in response to acute exercise. Front Physiol. 2020;11:605. doi: 10.3389/fphys.2020.00605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Imafuku A, Sjoqvist S. Extracellular vesicle therapeutics in regenerative medicine. Adv Exp Med Biol. 2021;1312:131–138. doi: 10.1007/5584_2020_599. [DOI] [PubMed] [Google Scholar]
- 8.Matsuzaka Y, Yashiro R. Therapeutic strategy of mesenchymal-stem-cell-derived extracellular vesicles as regenerative medicine. Int J Mol Sci. 2022;23:6480. [DOI] [PMC free article] [PubMed]
- 9.Grange C, Tritta S, Tapparo M, Cedrino M, Tetta C, Camussi G, et al. Stem cell-derived extracellular vesicles inhibit and revert fibrosis progression in a mouse model of diabetic nephropathy. Sci Rep. 2019;9:4468. doi: 10.1038/s41598-019-41100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fahim SA, Abdullah MS, Espinoza-Sánchez NA, Hassan H, Ibrahim AM, Ahmed SH, et al. Inflammatory breast carcinoma: elevated microRNA miR-181b-5p and reduced miR-200b-3p, miR-200c-3p, and miR-203a-3p expression as potential biomarkers with diagnostic value. Biomolecules. 2020;10:1059. [DOI] [PMC free article] [PubMed]
- 11.Brümmer A, Hausser J. MicroRNA binding sites in the coding region of mRNAs: extending the repertoire of post-transcriptional gene regulation. BioEssays. 2014;36:617–626. doi: 10.1002/bies.201300104. [DOI] [PubMed] [Google Scholar]
- 12.Pemmari T, Laakso J, Patrikainen MS, Parkkila S, Järvinen TAH. Carbonic anhydrase VI in skin wound healing study on Car6 knockout mice. Int J Mol Sci. 2020;21:5092. [DOI] [PMC free article] [PubMed]
- 13.Beke Debreceni I, Mezei G, Batár P, Illés Á, Kappelmayer J. Dasatinib Inhibits procoagulant and clot retracting activities of human platelets. Int J Mol Sci. 2019;20:5430. [DOI] [PMC free article] [PubMed]
- 14.de Laat-Kremers RMW, Yan Q, Ninivaggi M, de Maat M, de Laat B. Deciphering the coagulation profile through the dynamics of thrombin activity. Sci Rep. 2020;10:12544. doi: 10.1038/s41598-020-69415-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wada Y, Suzuki A, Ishiguro H, Murakashi E, Numabe Y. Chronological gene expression of human gingival fibroblasts with low reactive level laser (LLL) irradiation. J Clin Med. 2021;10:1952. [DOI] [PMC free article] [PubMed]
- 16.Sorkin M, Huber AK, Hwang C, Carson WFt, Menon R, Li J, et al, Regulation of heterotopic ossification by monocytes in a mouse model of aberrant wound healing. Nat Commun. 2020;11:722. [DOI] [PMC free article] [PubMed]
- 17.Rajendran NK, Dhilip Kumar SS, Houreld NN, Abrahamse H. Understanding the perspectives of forkhead transcription factors in delayed wound healing. J Cell Commun Signal. 2019;13:151–162. doi: 10.1007/s12079-018-0484-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ding W, Duan Y, Qu Z, Feng J, Zhang R, Li X, et al. Acidic microenvironment aggravates the severity of hepatic ischemia/reperfusion injury by modulating M1-polarization through regulating PPAR-γ signal. Front Immunol. 2021;12:697362. doi: 10.3389/fimmu.2021.697362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsieh CC, Wang CH. Aspirin disrupts the crosstalk of angiogenic and inflammatory cytokines between 4T1 breast cancer cells and macrophages. Mediators Inflamm. 2018;2018:6380643. doi: 10.1155/2018/6380643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Houseright RA, Rosowski EE, Lam PY, Tauzin SJM, Mulvaney O, Dewey CN, et al. Cell type specific gene expression profiling reveals a role for complement component C3 in neutrophil responses to tissue damage. Sci Rep. 2020;10:15716. doi: 10.1038/s41598-020-72750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Y, Tian L, Yang F, Tong W, Jia R, Zou Y, et al. Tannic acid accelerates cutaneous wound healing in rats via activation of the ERK 1/2 signaling pathways. Adv Wound Care (New Rochelle) 2019;8:341–354. doi: 10.1089/wound.2018.0853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shabestani Monfared G, Ertl P, Rothbauer M. An on-chip wound healing assay fabricated by xurography for evaluation of dermal fibroblast cell migration and wound closure. Sci Rep. 2020;10:16192. doi: 10.1038/s41598-020-73055-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li M, Hou Q, Zhong L, Zhao Y, Fu X. Macrophage related chronic inflammation in non-healing wounds. Front Immunol. 2021;12:681710. doi: 10.3389/fimmu.2021.681710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Soib HH, Ismail HF, Husin F, Abu Bakar MH, Yaakob H, Sarmidi MR. Bioassay-guided different extraction techniques of Carica papaya (Linn.) leaves on in vitro wound-healing activities. Molecules. 2020;25:517. [DOI] [PMC free article] [PubMed]
- 25.He M, Halima M, Xie Y, Schaaf MJM, Meijer AH, Wang M. Ginsenoside Rg1 Acts as a selective glucocorticoid receptor agonist with anti-inflammatory action without affecting tissue regeneration in zebrafish larvae. Cells. 2020;9:1107. [DOI] [PMC free article] [PubMed]
- 26.Liu W, Yu M, Xie D, Wang L, Ye C, Zhu Q, et al. Melatonin-stimulated MSC-derived exosomes improve diabetic wound healing through regulating macrophage M1 and M2 polarization by targeting the PTEN/AKT pathway. Stem Cell Res Ther. 2020;11:259. doi: 10.1186/s13287-020-01756-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shi R, Jin Y, Zhao S, Yuan H, Shi J, Zhao H. Hypoxic ADSC-derived exosomes enhance wound healing in diabetic mice via delivery of circ-Snhg11 and induction of M2-like macrophage polarization. Biomed Pharmacother. 2022;153:113463. doi: 10.1016/j.biopha.2022.113463. [DOI] [PubMed] [Google Scholar]
- 28.Teng L, Maqsood M, Zhu M, Zhou Y, Kang M, Zhou J, et al. Exosomes derived from human umbilical cord mesenchymal stem cells accelerate diabetic wound healing via promoting M2 macrophage polarization, angiogenesis, and collagen deposition. Int J Mol Sci. 2022;23:10421. [DOI] [PMC free article] [PubMed]
- 29.Han Y, Ren J, Bai Y, Pei X, Han Y. Exosomes from hypoxia-treated human adipose-derived mesenchymal stem cells enhance angiogenesis through VEGF/VEGF-R. Int J Biochem Cell Biol. 2019;109:59–68. doi: 10.1016/j.biocel.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 30.Liu J, Yan Z, Yang F, Huang Y, Yu Y, Zhou L, et al. Exosomes derived from human umbilical cord mesenchymal stem cells accelerate cutaneous wound healing by enhancing angiogenesis through delivering Angiopoietin-2. Stem Cell Rev Rep. 2021;17:305–317. doi: 10.1007/s12015-020-09992-7. [DOI] [PubMed] [Google Scholar]
- 31.Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341:738–746. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 32.Li B, Luan S, Chen J, Zhou Y, Wang T, Li Z, et al. The MSC-derived exosomal lncRNA H19 promotes wound healing in diabetic foot ulcers by upregulating PTEN via MicroRNA-152-3p. Mol Ther Nucleic Acids. 2020;19:814–826. doi: 10.1016/j.omtn.2019.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang B, Shi Y, Gong A, Pan Z, Shi H, Yang H, et al. HucMSC exosome-delivered 14-3-3ζ orchestrates self-control of the Wnt response via modulation of YAP during cutaneous regeneration. Stem Cells. 2016;34:2485–2500. doi: 10.1002/stem.2432. [DOI] [PubMed] [Google Scholar]
- 34.Wang L, Hu L, Zhou X, Xiong Z, Zhang C, Shehada HMA, et al. Exosomes secreted by human adipose mesenchymal stem cells promote scarless cutaneous repair by regulating extracellular matrix remodelling. Sci Rep. 2017;7:13321. doi: 10.1038/s41598-017-12919-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ma T, Fu B, Yang X, Xiao Y, Pan M. Adipose mesenchymal stem cell-derived exosomes promote cell proliferation, migration, and inhibit cell apoptosis via Wnt/β-catenin signaling in cutaneous wound healing. J Cell Biochem. 2019;120:10847–10854. doi: 10.1002/jcb.28376. [DOI] [PubMed] [Google Scholar]
- 36.Li JY, Ren KK, Zhang WJ, Xiao L, Wu HY, Liu QY, et al. Human amniotic mesenchymal stem cells and their paracrine factors promote wound healing by inhibiting heat stress-induced skin cell apoptosis and enhancing their proliferation through activating PI3K/AKT signaling pathway. Stem Cell Res Ther. 2019;10:247. doi: 10.1186/s13287-019-1366-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ren S, Chen J, Duscher D, Liu Y, Guo G, Kang Y, et al. Microvesicles from human adipose stem cells promote wound healing by optimizing cellular functions via AKT and ERK signaling pathways. Stem Cell Res Ther. 2019;10:47. doi: 10.1186/s13287-019-1152-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hu L, Wang J, Zhou X, Xiong Z, Zhao J, Yu R, et al. Exosomes derived from human adipose mensenchymal stem cells accelerates cutaneous wound healing via optimizing the characteristics of fibroblasts. Sci Rep. 2016;6:32993. doi: 10.1038/srep32993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kou X, Xu X, Chen C, Sanmillan ML, Cai T, Zhou Y, et al. The Fas/Fap-1/Cav-1 complex regulates IL-1RA secretion in mesenchymal stem cells to accelerate wound healing. Sci Transl Med. 2018;10:eaai8524. [DOI] [PMC free article] [PubMed]
- 40.Li J, Li Z, Wang S, Bi J, Huo R. Exosomes from human adipose-derived mesenchymal stem cells inhibit production of extracellular matrix in keloid fibroblasts via downregulating transforming growth factor-β2 and Notch-1 expression. Bioengineered. 2022;13:8515–8525. doi: 10.1080/21655979.2022.2051838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu J, Li F, Liu B, Yao Z, Li L, Liu G, et al. Adipose-derived mesenchymal stem cell exosomes inhibit transforming growth factor-β1-induced collagen synthesis in oral mucosal fibroblasts. Exp Ther Med. 2021;22:1419. doi: 10.3892/etm.2021.10854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hu J, Chen Y, Huang Y, Su Y. Human umbilical cord mesenchymal stem cell-derived exosomes suppress dermal fibroblasts-myofibroblats transition via inhibiting the TGF-β1/Smad 2/3 signaling pathway. Exp Mol Pathol. 2020;115:104468. doi: 10.1016/j.yexmp.2020.104468. [DOI] [PubMed] [Google Scholar]
- 43.Adamo A, Brandi J, Caligola S, Delfino P, Bazzoni R, Carusone R, et al. extracellular vesicles mediate mesenchymal stromal cell-dependent regulation of B Cell PI3K-AKT signaling pathway and actin cytoskeleton. Front Immunol. 2019;10:446. doi: 10.3389/fimmu.2019.00446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee C, Han J, Jung Y. Pathological contribution of extracellular vesicles and their micrRNAs to progression of chronic liver disease. Biology (Basel). 2022;11:637. [DOI] [PMC free article] [PubMed]
- 45.Jothimani G, Pathak S, Dutta S, Duttaroy AK, Banerjee A. A comprehensive cancer-associated microRNA expression profiling and proteomic analysis of human umbilical cord mesenchymal stem cell-derived exosomes. Tissue Eng Regen Med. 2022;19:1013–1031. doi: 10.1007/s13770-022-00450-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen J, Chen J, Cheng Y, Fu Y, Zhao H, Tang M, et al. Mesenchymal stem cell-derived exosomes protect beta cells against hypoxia-induced apoptosis via miR-21 by alleviating ER stress and inhibiting p38 MAPK phosphorylation. Stem Cell Res Ther. 2020;11:97. doi: 10.1186/s13287-020-01610-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baglio SR, Rooijers K, Koppers-Lalic D, Verweij FJ, Pérez Lanzón M, Zini N, et al. Human bone marrow- and adipose-mesenchymal stem cells secrete exosomes enriched in distinctive miRNA and tRNA species. Stem Cell Res Ther. 2015;6:127. doi: 10.1186/s13287-015-0116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garcia-Martin R, Wang G, Brandão BB, Zanotto TM, Shah S, Kumar Patel S, et al. MicroRNA sequence codes for small extracellular vesicle release and cellular retention. Nature. 2022;601:446–451. doi: 10.1038/s41586-021-04234-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Villarroya-Beltri C, Gutiérrez-Vázquez C, Sánchez-Cabo F, Pérez-Hernández D, Vázquez J, Martin-Cofreces N, et al. Sumoylated hnRNPA2B1 controls the sorting of miRNAs into exosomes through binding to specific motifs. Nat Commun. 2013;4:2980. doi: 10.1038/ncomms3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Si Y, Liu F, Wang D, Fang C, Tang X, Guo B, et al. Exosomal transfer of miR-185 is controlled by hnRNPA2B1 and impairs re-endothelialization after vascular injury. Front Cell Dev Biol. 2021;9:619444. doi: 10.3389/fcell.2021.619444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee H, Li C, Zhang Y, Zhang D, Otterbein LE, Jin Y. Caveolin-1 selectively regulates microRNA sorting into microvesicles after noxious stimuli. J Exp Med. 2019;216:2202–2220. doi: 10.1084/jem.20182313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pérez-Boza J, Boeckx A, Lion M, Dequiedt F, Struman I. hnRNPA2B1 inhibits the exosomal export of miR-503 in endothelial cells. Cell Mol Life Sci. 2020;77:4413–4428. doi: 10.1007/s00018-019-03425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li Y, Zhang J, Li S, Guo C, Li Q, Zhang X, et al. Heterogeneous nuclear ribonucleoprotein A1 loads batched tumor-promoting MicroRNAs into small extracellular vesicles with the assist of Caveolin-1 in A549 cells. Front Cell Dev Biol. 2021;9:687912. doi: 10.3389/fcell.2021.687912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Santangelo L, Giurato G, Cicchini C, Montaldo C, Mancone C, Tarallo R, et al. The RNA-binding protein SYNCRIP Is a component of the hepatocyte exosomal machinery controlling MicroRNA sorting. Cell Rep. 2016;17:799–808. doi: 10.1016/j.celrep.2016.09.031. [DOI] [PubMed] [Google Scholar]
- 55.McKenzie AJ, Hoshino D, Hong NH, Cha DJ, Franklin JL, Coffey RJ, et al. KRAS-MEK signaling controls Ago2 sorting into exosomes. Cell Rep. 2016;15:978–987. doi: 10.1016/j.celrep.2016.03.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lu P, Li H, Li N, Singh RN, Bishop CE, Chen X, et al. MEX3C interacts with adaptor-related protein complex 2 and involves in miR-451a exosomal sorting. PLoS ONE. 2017;12:e0185992. doi: 10.1371/journal.pone.0185992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kosaka N, Iguchi H, Yoshioka Y, Takeshita F, Matsuki Y, Ochiya T. Secretory mechanisms and intercellular transfer of microRNAs in living cells. J Biol Chem. 2010;285:17442–17452. doi: 10.1074/jbc.M110.107821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Robinson H, Ruelcke JE, Lewis A, Bond CS, Fox AH, Bharti V, et al. Caveolin-1-driven membrane remodelling regulates hnRNPK-mediated exosomal microRNA sorting in cancer. Clin Transl Med. 2021;11:e381. doi: 10.1002/ctm2.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen X, Liang H, Zhang J, Zen K, Zhang CY. Secreted microRNAs: a new form of intercellular communication. Trends Cell Biol. 2012;22:125–132. doi: 10.1016/j.tcb.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 60.Albanese M, Chen YA, Hüls C, Gärtner K, Tagawa T, Mejias-Perez E, et al. MicroRNAs are minor constituents of extracellular vesicles that are rarely delivered to target cells. PLoS Genet. 2021;17:e1009951. doi: 10.1371/journal.pgen.1009951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 62.Qu Q, Wang L, Bing W, Bi Y, Zhang C, Jing X, et al. miRNA-126-3p carried by human umbilical cord mesenchymal stem cell enhances endothelial function through exosome-mediated mechanisms in vitro and attenuates vein graft neointimal formation in vivo. Stem Cell Res Ther. 2020;11:464. doi: 10.1186/s13287-020-01978-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tan H, Huang S, Zhang Z, Qian X, Sun P, Zhou X. Pan-cancer analysis on microRNA-associated gene activation. EBioMedicine. 2019;43:82–97. doi: 10.1016/j.ebiom.2019.03.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liang Y, Lu Q, Li W, Zhang D, Zhang F, Zou Q, et al. Reactivation of tumour suppressor in breast cancer by enhancer switching through NamiRNA network. Nucleic Acids Res. 2021;49:8556–8572. doi: 10.1093/nar/gkab626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fabbri M, Paone A, Calore F, Galli R, Gaudio E, Santhanam R, et al. MicroRNAs bind to Toll-like receptors to induce prometastatic inflammatory response. Proc Natl Acad Sci U S A. 2012;109:E2110–2116. doi: 10.1073/pnas.1209414109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wallach T, Wetzel M, Dembny P, Staszewski O, Krüger C, Buonfiglioli A, et al, Identification of CNS injury-related microRNAs as novel toll-like receptor 7/8 signaling activators by small RNA sequencing. Cells. 2020;9:186. [DOI] [PMC free article] [PubMed]
- 67.Ti D, Hao H, Tong C, Liu J, Dong L, Zheng J, et al. LPS-preconditioned mesenchymal stromal cells modify macrophage polarization for resolution of chronic inflammation via exosome-shuttled let-7b. J Transl Med. 2015;13:308. doi: 10.1186/s12967-015-0642-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tian J, Chen W, Xiong Y, Li Q, Kong S, Li M, et al. Small extracellular vesicles derived from hypoxic preconditioned dental pulp stem cells ameliorate inflammatory osteolysis by modulating macrophage polarization and osteoclastogenesis. Bioact Mater. 2023;22:326–342. doi: 10.1016/j.bioactmat.2022.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ti D, Hao H, Fu X, Han W. Mesenchymal stem cells-derived exosomal microRNAs contribute to wound inflammation. Sci China Life Sci. 2016;59:1305–1312. doi: 10.1007/s11427-016-0240-4. [DOI] [PubMed] [Google Scholar]
- 70.Li X, Liu L, Yang J, Yu Y, Chai J, Wang L, et al. Exosome derived from human umbilical cord mesenchymal stem cell mediates MiR-181c attenuating burn-induced excessive inflammation. EBioMedicine. 2016;8:72–82. doi: 10.1016/j.ebiom.2016.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yao M, Cui B, Zhang W, Ma W, Zhao G, Xing L. Exosomal miR-21 secreted by IL-1β-primed-mesenchymal stem cells induces macrophage M2 polarization and ameliorates sepsis. Life Sci. 2021;264:118658. doi: 10.1016/j.lfs.2020.118658. [DOI] [PubMed] [Google Scholar]
- 72.Song Y, Dou H, Li X, Zhao X, Li Y, Liu D, et al. Exosomal miR-146a contributes to the enhanced therapeutic efficacy of interleukin-1β-primed mesenchymal stem cells against sepsis. Stem Cells. 2017;35:1208–1221. doi: 10.1002/stem.2564. [DOI] [PubMed] [Google Scholar]
- 73.He X, Dong Z, Cao Y, Wang H, Liu S, Liao L, et al. MSC-derived exosome promotes M2 polarization and enhances cutaneous wound healing. Stem Cells Int. 2019;2019:7132708. doi: 10.1155/2019/7132708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Heo JS, Kim S, Yang CE, Choi Y, Song SY, Kim HO. Human adipose mesenchymal stem cell-derived exosomes: A key player in wound healing. Tissue Eng Regen Med. 2021;18:537–548. doi: 10.1007/s13770-020-00316-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liang X, Zhang L, Wang S, Han Q, Zhao RC. Exosomes secreted by mesenchymal stem cells promote endothelial cell angiogenesis by transferring miR-125a. J Cell Sci. 2016;129:2182–2189. doi: 10.1242/jcs.170373. [DOI] [PubMed] [Google Scholar]
- 76.Pi L, Yang L, Fang BR, Meng XX, Qian L. Exosomal microRNA-125a-3p from human adipose-derived mesenchymal stem cells promotes angiogenesis of wound healing through inhibiting PTEN. Mol Cell Biochem. 2022;477:115–127. doi: 10.1007/s11010-021-04251-w. [DOI] [PubMed] [Google Scholar]
- 77.Xu F, Xiang Q, Huang J, Chen Q, Yu N, Long X, et al. Exosomal miR-423-5p mediates the proangiogenic activity of human adipose-derived stem cells by targeting Sufu. Stem Cell Res Ther. 2019;10:106. doi: 10.1186/s13287-019-1196-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ding J, Wang X, Chen B, Zhang J, Xu J. Exosomes derived from human bone marrow mesenchymal stem cells stimulated by deferoxamine accelerate cutaneous wound healing by promoting angiogenesis. Biomed Res Int. 2019;2019:9742765. doi: 10.1155/2019/9742765. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 79.Zhang L, Ouyang P, He G, Wang X, Song D, Yang Y, et al. Exosomes from microRNA-126 overexpressing mesenchymal stem cells promote angiogenesis by targeting the PIK3R2-mediated PI3K/Akt signalling pathway. J Cell Mol Med. 2021;25:2148–2162. doi: 10.1111/jcmm.16192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hu Y, Rao SS, Wang ZX, Cao J, Tan YJ, Luo J, et al. Exosomes from human umbilical cord blood accelerate cutaneous wound healing through miR-21-3p-mediated promotion of angiogenesis and fibroblast function. Theranostics. 2018;8:169–184. doi: 10.7150/thno.21234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang Y, Xie Y, Hao Z, Zhou P, Wang P, Fang S, et al. Umbilical mesenchymal stem cell-derived exosome-encapsulated hydrogels accelerate bone repair by enhancing angiogenesis. ACS Appl Mater Interfaces. 2021;13:18472–18487. doi: 10.1021/acsami.0c22671. [DOI] [PubMed] [Google Scholar]
- 82.Choi EW, Seo MK, Woo EY, Kim SH, Park EJ, Kim S. Exosomes from human adipose-derived stem cells promote proliferation and migration of skin fibroblasts. Exp Dermatol. 2018;27:1170–1172. doi: 10.1111/exd.13451. [DOI] [PubMed] [Google Scholar]
- 83.Gao S, Chen T, Hao Y, Zhang F, Tang X, Wang D, et al. Exosomal miR-135a derived from human amnion mesenchymal stem cells promotes cutaneous wound healing in rats and fibroblast migration by directly inhibiting LATS2 expression. Stem Cell Res Ther. 2020;11:56. doi: 10.1186/s13287-020-1570-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chen T, Gao S, Hao Y, Zhang F, Tang X, Wei Z, et al. Experimental study of human amniotic mesenchymal stem cell exosome promoting fibroblasts migration through microRNA-135a. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34:234–9. [DOI] [PMC free article] [PubMed]
- 85.Zhao W, Zhang R, Zang C, Zhang L, Zhao R, Li Q, et al. Exosome derived from mesenchymal stem cells alleviates pathological scars by inhibiting the proliferation, migration and protein expression of fibroblasts via delivering miR-138-5p to Target SIRT1. Int J Nanomed. 2022;17:4023–4038. doi: 10.2147/IJN.S377317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ma J, Zhang Z, Wang Y, Shen H. Investigation of miR-126-3p loaded on adipose stem cell-derived exosomes for wound healing of full-thickness skin defects. Exp Dermatol. 2022;31:362–374. doi: 10.1111/exd.14480. [DOI] [PubMed] [Google Scholar]
- 87.Yang C, Luo L, Bai X, Shen K, Liu K, Wang J, et al. Highly-expressed micoRNA-21 in adipose derived stem cell exosomes can enhance the migration and proliferation of the HaCaT cells by increasing the MMP-9 expression through the PI3K/AKT pathway. Arch Biochem Biophys. 2020;681:108259. doi: 10.1016/j.abb.2020.108259. [DOI] [PubMed] [Google Scholar]
- 88.Wang J, Qiu Y, Shi NW, Zhao JN, Wang YC, Jiang H, et al. microRNA-21 mediates the TGF-β1-induced migration of keratinocytes via targeting PTEN. Eur Rev Med Pharmacol Sci. 2016;20:3748–3759. [PubMed] [Google Scholar]
- 89.Yuan R, Dai X, Li Y, Li C, Liu L. Exosomes from miR-29a-modified adipose-derived mesenchymal stem cells reduce excessive scar formation by inhibiting TGF-β2/Smad3 signaling. Mol Med Rep. 2021;24:758. [DOI] [PMC free article] [PubMed]
- 90.Fang S, Xu C, Zhang Y, Xue C, Yang C, Bi H, et al. Umbilical cord-derived mesenchymal stem cell-derived exosomal MicroRNAs suppress myofibroblast differentiation by inhibiting the transforming growth factor-β/SMAD2 pathway during wound healing. Stem Cells Transl Med. 2016;5:1425–1439. doi: 10.5966/sctm.2015-0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Li Y, Zhang J, Shi J, Liu K, Wang X, Jia Y, et al. Exosomes derived from human adipose mesenchymal stem cells attenuate hypertrophic scar fibrosis by miR-192-5p/IL-17RA/Smad axis. Stem Cell Res Ther. 2021;12:221. doi: 10.1186/s13287-021-02290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Duan M, Zhang Y, Zhang H, Meng Y, Qian M, Zhang G. Epidermal stem cell-derived exosomes promote skin regeneration by downregulating transforming growth factor-β1 in wound healing. Stem Cell Res Ther. 2020;11:452. doi: 10.1186/s13287-020-01971-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang Y, Yan J, Liu Y, Chen Z, Li X, Tang L, et al. Human amniotic fluid stem cell-derived exosomes as a novel cell-free therapy for cutaneous regeneration. Front Cell Dev Biol. 2021;9:685873. doi: 10.3389/fcell.2021.685873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen R, Yuan W, Zheng Y, Zhu X, Jin B, Yang T, et al. Delivery of engineered extracellular vesicles with miR-29b editing system for muscle atrophy therapy. J Nanobiotechnol. 2022;20:304. doi: 10.1186/s12951-022-01508-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Park DJ, Seo YJ. Engineering of extracellular vesicles based on payload changes for tissue regeneration. Tissue Eng Regen Med. 2021;18:485–497. doi: 10.1007/s13770-021-00349-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chen Z, Xie Y, Chen W, Li T, Chen X, Liu B. microRNA-6785-5p-loaded human umbilical cord mesenchymal stem cells-derived exosomes suppress angiogenesis and metastasis in gastric cancer via INHBA. Life Sci. 2021;284:119222. doi: 10.1016/j.lfs.2021.119222. [DOI] [PubMed] [Google Scholar]
- 97.Naseri Z, Oskuee RK, Forouzandeh-Moghadam M, Jaafari MR. Delivery of LNA-antimiR-142-3p by mesenchymal stem cells-derived exosomes to breast cancer stem cells reduces tumorigenicity. Stem Cell Rev Rep. 2020;16:541–556. doi: 10.1007/s12015-019-09944-w. [DOI] [PubMed] [Google Scholar]
- 98.Bai Y, Han YD, Yan XL, Ren J, Zeng Q, Li XD, et al. Adipose mesenchymal stem cell-derived exosomes stimulated by hydrogen peroxide enhanced skin flap recovery in ischemia-reperfusion injury. Biochem Biophys Res Commun. 2018;500:310–317. doi: 10.1016/j.bbrc.2018.04.065. [DOI] [PubMed] [Google Scholar]
- 99.Heo JS. Selenium-stimulated exosomes enhance wound healing by modulating inflammation and angiogenesis. Int J Mol Sci. 2022;23:11543. [DOI] [PMC free article] [PubMed]
- 100.Zhou Y, Zhang XL, Lu ST, Zhang NY, Zhang HJ, Zhang J, et al. Human adipose-derived mesenchymal stem cells-derived exosomes encapsulated in pluronic F127 hydrogel promote wound healing and regeneration. Stem Cell Res Ther. 2022;13:407. doi: 10.1186/s13287-022-02980-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhang Y, Zhang P, Gao X, Chang L, Chen Z, Mei X. Preparation of exosomes encapsulated nanohydrogel for accelerating wound healing of diabetic rats by promoting angiogenesis. Mater Sci Eng C Mater Biol Appl. 2021;120:111671. doi: 10.1016/j.msec.2020.111671. [DOI] [PubMed] [Google Scholar]
- 102.Xu H, Wang J, Wu D, Qin D. A hybrid hydrogel encapsulating human umbilical cord mesenchymal stem cells enhances diabetic wound healing. J Mater Sci Mater Med. 2022;33:60. doi: 10.1007/s10856-022-06681-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hahm J, Kim J, Park J. Strategies to enhance extracellular vesicle production. Tissue Eng Regen Med. 2021;18:513–524. doi: 10.1007/s13770-021-00364-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jiang B, Yan L, Wang X, Li E, Murphy K, Vaccaro K, et al. Concise review: mesenchymal stem cells derived from human pluripotent cells, an unlimited and quality-controllable source for therapeutic applications. Stem Cells. 2019;37:572–581. doi: 10.1002/stem.2964. [DOI] [PubMed] [Google Scholar]
- 105.Wang X, Jiang B, Sun H, Zheng D, Zhang Z, Yan L, et al. Noninvasive application of mesenchymal stem cell spheres derived from hESC accelerates wound healing in a CXCL12-CXCR4 axis-dependent manner. Theranostics. 2019;9:6112–6128. doi: 10.7150/thno.32982. [DOI] [PMC free article] [PubMed] [Google Scholar]