Abstract
Background
Nasogastric tube syndrome is a rare but life‐threatening complication of nasogastric tube placement due to acute upper airway obstruction caused by bilateral vocal cord paresis.
Case Presentation
An 86‐year‐old woman was brought to the emergency department with acute stridor. She had been diagnosed with stroke 106 days prior, and an 8F nasogastric tube was placed on the day following the diagnosis. A laryngeal fiberscopy revealed bilateral laryngeal edema and bilateral vocal cord palsy. Nasogastric tube removal and intubation were carried out, and the stridor disappeared. Two days later, a tracheostomy was performed. Unfortunately, the patient's vocal cord function had not improved at the 1 month follow‐up upon assessment with a laryngeal fiberscope.
Conclusion
Long‐term small‐bore nasogastric tube placement can cause upper airway obstruction due to bilateral vocal cord palsy.
Keywords: airway obstruction, endoscopy, intubation, tracheostomy, vocal cord paralysis
Nasogastric tube syndrome (NGTS) is a rare but lethal complication of nasogastric tube placement. Nasogastric tube syndrome can be fatal due to upper airway obstruction caused by vocal cord paresis. We report a woman who was diagnosed with NGTS caused by long‐term use of small‐bore nasogastric tube.
INTRODUCTION
Nasogastric tube syndrome (NGTS) is a rare but life‐threatening complication of nasogastric tube placement. Nasogastric tube syndrome was first described by Sofferman et al. in 1990 as the triad of nasogastric tube placement with throat pain and vocal cord paresis. 1 Although its incidence is unknown, NGTS is potentially fatal due to acute upper airway obstruction caused by bilateral vocal cord paresis. The clinical risk of developing NGTS other than nasogastric tube insertion is not clear, and it remains unclear which patients we should be concerned about regarding the development of the disease. In this report, we present a case of NGTS that developed after prolonged placement, despite the nasogastric tube diameter being as small as 8F. This case represents a rare occurrence of NGTS in an adult who underwent placement of a nasogastric tube with a very small diameter.
CASE REPORT
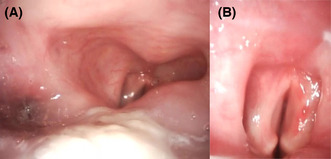
An 86‐year‐old woman was brought to the emergency department with acute stridor. She had previously been diagnosed with stroke, right‐sided hemiparesis, and aphagia due to left middle cerebral artery occlusion 106 days earlier. Her National Institutes of Health Stroke Scale score had been 16/42. Emergency cerebrovascular mechanical thrombectomy was carried out. Scattered cerebral infarcts were observed in the left middle cerebral artery region. Evaluation after treatment revealed no dysarthria but dysphagia, and an 8F nasogastric tube was inserted for nutrition on the day following the diagnosis. At the time of discharge, her neurological condition was assessed as Glasgow Coma Scale E4V4M6, dysphagia present, no dysarthria, right upper extremity Manual Muscle Test score 1, and right lower extremity Manual Muscle Test score 2. No observations were made regarding the vocal cords. She was transferred to the hospital for rehabilitation for dysphagia and right‐sided paralysis and continued rehabilitation. On presentation, there was no sign of trauma, and her vital signs were as follows: heart rate, 96 b.p.m.; blood pressure, 152/123 mmHg; oxygen saturation, 97% on 2 L oxygen through a nasal cannula; respiratory rate, 18 breaths/min; body temperature, 36.5°C; and Glasgow Coma Scale score, E4V2M6. She did not have throat pain. Laryngeal fiberscopy revealed the nasogastric tube passing through the right side of the hypopharynx, bilateral laryngeal edema without ulcer, and bilateral vocal cord palsy (Figure 1). Nasogastric tube removal and intubation were carried out, and the stridor disappeared. There were no significant changes on neurological examination or head computed tomography; hence, we diagnosed NGTS. Two days later, a tracheostomy was undertaken. Unfortunately, the patient's vocal cord function had not improved at the 1 month follow‐up upon assessment with a laryngeal fiberscope. She was transferred to a rehabilitation hospital on day 58.
FIGURE 1.
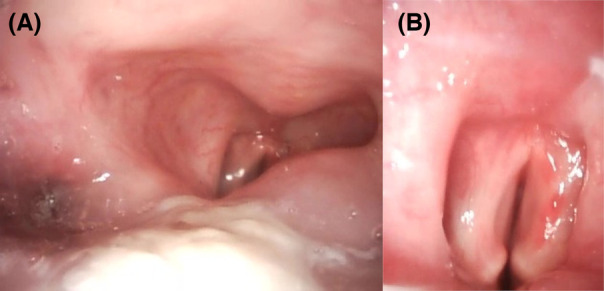
Laryngeal fiberscopy in an 86‐year‐old woman with long‐term small‐bore nasogastric tube placement. (A) Bilateral laryngeal edema. (B) Bilateral vocal cord palsy at inspiratory phase.
DISCUSSION
Considering the clinical findings of our patient, we discovered the following: (i) long‐term small‐bore nasogastric tube placement can induce NGTS; (ii) NGTS is life‐threatening due to upper airway obstruction with bilateral vocal cord palsy; and (iii) bilateral vocal cord palsy might not improve in all cases.
Four mechanisms have been proposed for the pathogenesis of NGTS: (i) the rubbing force between the fixed tube and movable structures of the larynx; (ii) gravitational compression on the tube by the cricoid cartilage against the vertebral column in the supine position; and (iii) the pressure of tonic contraction of the cricopharyngeal muscle on the tube. 1 Ulcers formed through these mechanisms are assumed to cause inflammation around the posterior cricoarytenoid muscle, resulting in vocal cord palsy. The fourth mechanism proposed by Isozaki et al. concerning cases without ulcer formation is that posterior cricoarytenoid muscle ischemia results from compression. 2 Considering these hypotheses, it has been speculated that tube diameter influences the pathogenesis of NGTS. 3 The nasogastric tube sizes reported previously were 16–18F, and it is not clear how large a tube should be to induce NGTS. In addition to the size, the material of the nasogastric tube is suspected to affect NGTS because of plasticizer elution, which alters tube flexibility. 3 Therefore, it is possible that the onset of NGTS cannot be avoided even with a small diameter of 8F. In addition, given that the involvement of size is relative, the fact that the patient was small and thin (150 cm, 45 kg) might have contributed to NGTS development. In this case, a polyurethane feeding tube without a plasticizer was used. Although NGTS commonly occurs between 12 h and 2 weeks after nasogastric tube insertion, 4 only three cases were diagnosed between 2 weeks and 2 years after nasogastric tube insertion. 2 Similarly, our patient had a prolonged NGTS development time of 105 days. The mechanism by which NGTS occurred in this case is assumed to be as follows. As the posterior cricoarytenoid muscle is a thin tissue that exists behind the cricoid cartilage, even with a small tube diameter, the repeated rubbing force of the tube over a long period of time, and the pressure exerted by the cricoid cartilage, vertebral body, and nasogastric tube in the supine position could have disrupted the perfusion of the posterior cricoarytenoid muscle, and induced muscle ischemia, as proposed by Isozaki et al. 2 Our case is unique in that it developed after long‐term implantation, despite using the smallest‐bore soft tube in an adult patient. 1 , 3 , 5 These facts indicate that NGTS is an unavoidable complication of nasogastric tube insertion. This case suggests that NGTS might not be avoidable, even with small‐diameter tubes. As a mechanism has been proposed in which tube stimulation is the trigger, shortening the duration of nasogastric indwelling might be effective in reducing the chances of stimulation and preventing NGTS. Clinicians should be aware of the risk of NGTS development in all patients requiring nasogastric tube placement and should undertake appropriate observations. Nasogastric tube syndrome could be fatal and is an acute complication due to bilateral vocal cord palsy, 77% of which requires tracheostomy. Given that only diagnosed cases have been reported, there could be undiagnosed cases that were treated as sudden deaths. Although most NGTS patients have good vocal cord function recovery within 2 months, some cases in which there was no improvement have been reported. 4 , 6 , 7 This difference might be due to pathological variations. Differences in prognosis according to pathophysiology remain unelucidated.
Nasogastric tube placement is one of the most commonly performed procedures. Nasogastric tube syndrome is caused by nasogastric tube placement and can lead to upper airway obstruction due to vocal cord palsy. Airway obstruction can be fatal within minutes; thus, patients with suspected NGTS should be treated by an experienced medical team for airway management. Considering that palsy might be irreversible, physicians should be aware of the risks of NGTS and carry out appropriate observations for patients who undergo nasogastric tube placement.
CONCLUSION
Long‐term small‐bore nasogastric tube placement can cause upper airway obstruction due to bilateral vocal cord palsy.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: This report has been approved by our institutional Ethical Committee. The approval number is SKEC‐23‐6.
Informed consent: Written informed consent was obtained from the patient to publish this case report and accompanying images.
Registry and registration no. of the study/trial: N/A.
Animal studies: N/A.
Nihira T, Fukaguchi K, Taguchi A, Fukui H, Sekine I, Yamamoto D, et al. Bilateral vocal cord palsy induced by long‐term use of small‐bore nasogastric tube. Acute Med Surg. 2023;10:e872. 10.1002/ams2.872
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Sofferman RA, Haisch CE, Kirchner JA, Hardin NJ. The nasogastric tube syndrome. Laryngoscope. 1990;100(9):962–8. [DOI] [PubMed] [Google Scholar]
- 2. Isozaki E, Tobisawa S, Naito R, Mizutani T, Hayashi H. A variant form of nasogastric tube syndrome. Intern Med. 2005;44(12):1286–90. [DOI] [PubMed] [Google Scholar]
- 3. Kanbayashi T, Tanaka S, Uchida Y, Hatanaka Y, Sonoo M. Nasogastric tube syndrome: the size and type of the nasogastric tube may contribute to the development of nasogastric tube syndrome. Intern Med. 2021;60(12):1977–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brousseau VJ, Kost KM. A rare but serious entity: nasogastric tube syndrome. Otolaryngol Head Neck Surg. 2006;135(5):677–9. [DOI] [PubMed] [Google Scholar]
- 5. Nehru VI, Al Shammari HJ, Jaffer AM. Nasogastric tube syndrome: the unilateral variant. Med Princ Pract. 2003;12(1):44–6. [DOI] [PubMed] [Google Scholar]
- 6. Nayak G, Virk RS, Singh M, Singh M. Nasogastric tube syndrome: a diagnostic dilemma. J Bronchology Interv Pulmonol. 2018;25(4):343–5. [DOI] [PubMed] [Google Scholar]
- 7. Apostolakis LW, Funk GF, Urdaneta LF, McCulloch TM, Jeyapalan MM. The nasogastric tube syndrome: two case reports and review of the literature. Head Neck. 2001;23(1):59–63. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


