Abstract
Although widespread support favors prospective planning for altered standards of care during mass casualty events, the literature includes few, if any, accounts of groups that have formally addressed the overarching policy considerations at the state level. We describe the planning process undertaken by public health officials in the Commonwealth of Massachusetts, along with community and academic partners, to explore the issues surrounding altered standards of care in the event of pandemic influenza. Throughout 2006, the Massachusetts Department of Public Health and the Harvard School of Public Health Center for Public Health Preparedness jointly convened a working group comprising ethicists, lawyers, clinicians, and local and state public health officials to consider issues such as allocation of antiviral medications, prioritization of critical care, and state seizure of private assets. Community stakeholders were also engaged in the process through facilitated discussion of case scenarios focused on these and other issues. The objective of this initiative was to establish a framework and some fundamental principles that would subsequently guide the process of establishing specific altered standards of care protocols. The group collectively identified 4 goals and 7 principles to guide the equitable allocation of limited resources and establishment of altered standards of care protocols. Reviewing and analyzing this process to date may serve as a resource for other states.
Keywords: altered standards of care, ethics, public health preparedness, allocation of scarce resources
Large-scale disasters can quickly overwhelm even the most sophisticated of health care systems. With respect to the next influenza pandemic, a host of issues now center on how the United States can best augment current health care capacity to respond to the projected 9.9 million people who may require hospital-level care.1 In anticipation of such mass casualties, federal and state public health officials, health care providers (HCPs), and regulatory bodies must confront the need to alter the ways in which health care is administered. Specifically, maximizing the total number of lives saved may require prioritizing scarce equipment, supplies, and personnel, providing care in nonconventional settings, and changing thresholds for critical care.2 The military has traditionally upheld protocols to achieve the greatest good for the greatest number during mass casualty incidents, using well-established and accepted practices for utilitarian triage to deploy resources. However, the patient-centered model of civilian medicine in the United States is much less familiar with such decision making.
Confronting these issues raises many ethical and legal questions. Some may argue that the fundamental public health ideologies of protecting the most vulnerable individuals/groups and striving for social justice are inherently incompatible with a utilitarian approach.3 Moreover, HCPs are strongly motivated by a professional code of ethics that centers on their duty to care.4–9 Although typically this mission can be supported, in a disaster individual HCPs may be forced to make independent decisions to prioritize scarce resources. Clearly, the weight of such decisions has the potential to cause great stress and significant liability concerns for HCPs. Furthermore, as evidenced by the legal action faced by HCPs who responded to the 2005 Gulf Coast hurricanes, such decisions introduce significant legal and professional implications if not addressed in advance.10,11
Prospective attention to situations in which altered standards of care may be required is not only important for supporting and protecting HCPs but also critical to ensuring the optimal functioning of health care systems and upholding public trust. Different hospitals providing different standards of care could easily lead to negative outcomes. Dissatisfied consumers may “shop” to find hospitals where they are eligible to receive care, resulting in an uneven distribution of burden and ineffective use of resources across the health care system. Moreover, inconsistent standards of care would undermine public confidence. The threat of an influenza pandemic underscores the need for prospectively establishing a systematic process for developing altered standards of care to provide some measure of order, guidance, and basic equity.
We describe the state planning process undertaken by the Commonwealth of Massachusetts, involving public health officials along with community and academic partners, to begin to explore the issues surrounding altered standards of care (ASC) in the event of pandemic influenza. The objective of this initiative was to establish a framework and some fundamental principles that would subsequently guide the process of establishing specific protocols for HCPs to make decisions about equitable allocation of scarce resources.
The term altered standards of care has been used to describe standards that are acceptable when adequate resources are not available to meet the usual standard of care provided by HCPs. Some find the term inaccurate because the concept of the standard of care always includes consideration of the circumstances during which the care is delivered. Others have suggested the use of terms such as situational standards of care, which may be problematic as well because the situation is already factored into the standard of care when questions of medical malpractice are determined. We used ASC because this is the term used by many working in this area, understanding that a more accurate, universally accepted, and recognized term may arise in the future.
RATIONALE
Attention to ASC began in 2004 when the Massachusetts Statewide Surge Committee, under the auspices of the Massachusetts Department of Public Health (MDPH), engaged in pandemic influenza planning. This committee—comprising approximately 35 professionals representing state and local public health, hospital and community-based HCPs, and health advocacy groups—noted that a pandemic could cause illness in up to 2 million Massachusetts residents, 80,000 of whom could require hospital-level care.12 In this context, MPDH officials recognized the importance of addressing the following provider questions: What standards of care would be expected when staff, equipment, and medications are insufficient to meet demand and to provide the level of medical care that is expected during non-emergency times? What guidance could be made available to HCPs to assist them in making fair and responsible decisions under these circumstances?
LEGAL CONTEXT
The declaration of a public health emergency by the governor would provide enhanced authority to allow the commissioner of public health to waive statutory and regulatory restrictions (FN Massachusetts General Law c.17, §2A), for example, allowing certain HCPs to practice outside their usual scope of work.13 Because issues of malpractice liability are not detailed by statute (with the exception of the Tort Claims Act for public employees and the Good Samaritan Acts [Massachusetts General Law c.112, §§ 12B,12F,12V, 12V ½, 23BB and Massachusetts General Law c.111C, §21 FN]), it is questionable whether the commissioner, by order alone, could provide additional liability protection to HCPs based on the declaration of an emergency.13 Legislation is pending in Massachusetts that may provide additional authority and protection with respect to liability; however, HCPs still require standards to guide decision making and practice during a public health emergency. These concerns further underscored the urgency that planning for ASC should begin well in advance of a possible pandemic.
METHODS
Joint MDPH-Harvard Working Group
In January 2006, MDPH and the Harvard School of Public Health Center for Public Health Preparedness (HSPH-CPHP) jointly convened a working group to make recommendations to the Commonwealth on the key ethical, legal, and practical issues regarding ASC during pandemic influenza. HSPH-CPHP is 1 of 25 national academic Centers for Public Health Preparedness funded by the US Centers for Disease Control and Prevention, collectively charged with advancing state and local preparedness for public health threats. HSPH-CPHP and MDPH had previously enjoyed a robust history of collaboration on issues of public health preparedness. Building on this partnership, leaders identified ethicists, lawyers, clinicians, and local and state public health officials to serve on the 20-member Joint Working Group (“the group”). Group members were selected based on their complementary expertise and experience, and collectively represented Massachusetts’ leaders in public health law, ethics, disaster medicine, and public health preparedness. The director of the HSPH-CPHP (H.K.K.) and the MDPH general counsel (D.L.) served as co-chairs.
Identifying Goals and Principles
The group convened 4 meetings throughout 2006. First, the group reviewed the applicable Massachusetts law with respect to emergency public health authority, as well as a selection of the current literature related to ASC during mass casualty events. Based on the multidisciplinary experiences of its members and the available scientific literature, the group concurred that prospective establishment of the principles, processes, and framework guiding decisions to alter the standard of care in the event of pandemic influenza was necessary to fully consider the complex ethical and legal elements, and allow adequate time for systematic review and revision.14–18 Because the specific clinical and epidemiological characteristics of an influenza pandemic remain unknown (eg, the virulence of the virus, its response to various treatments, the age distribution of cases), it would not be viable or prudent to make all of the necessary specific decisions or recommendations in advance.
Hence, consistent with previous literature, the group determined that ASC guidelines must include both specific recommendations that could be established in advance, as well as the flexibility to allow for the incorporation of real-time data into evidence-based decision making.19–22 Furthermore, to ensure equity and consistency and to relieve burdens on individual HCPs, the group determined that guidelines for decision making must be developed at the state level, as opposed to the local or institutional level.19,23 To this end, the group recognized the importance of including a range of key stakeholders in the decision-making process16–18,24 and ensuring transparency by making public the process and rationale.17,21,25
Developing Scenarios
To structure and provide a context for further discussion to inform the development of guidelines consistent with the above-described criteria, HSPH-CPHP created a series of 5 scenarios to illustrate the specific considerations of categories of ASC defined by the group: allocation of scarce resources, prioritization of critical care (2 scenarios), government seizure of private assets,26 and provider duty to care. Each scenario was accompanied by a series of discussion questions, intended to evoke reactions that would illuminate any widely held social and ethical norms regarding distribution of limited resources. Then, the scenarios and questions were discussed at length by the group and continuously refined by HSPH-CPHP.
Engaging Stakeholders
To garner feedback from a more diverse audience, the authors recruited resident stakeholders to deliberate over the scenarios and the issues raised by them. Two stakeholder meetings (for consumers and HCPs, respectively) were held in July 2006, each attended by approximately 15 Massachusetts residents. Each meeting lasted 4 hours, during which time the stakeholders engaged in professionally facilitated discussions of the 5 scenarios. A summary of the scenarios and the stakeholders’ reactions to each is shown in Table 1, and several key findings are noted below.
TABLE 1.
Summary of Scenarios and Stakeholder Reactions
| Scenario 1: Allocation of Scarce Resources | |
|---|---|
| Context: Your community is in the midst of influenza pandemic, and oseltamivir phosphate (ie, Tamiflu) is the only drug that may effectively reduce mortality of ill patients and limit infection of exposed people. Issue: Supplies of Tamiflu are limited, and hospitals across the country are independently making decisions to govern allocation of antiviral medications. The 4 major hospitals in a given geographic area have recently established different protocols regarding prioritization of antivirals: Hospital A: Prophylaxis of staff who are exposed while caring for influenza patients. Hospital B: Treatment of the sickest influenza patients. Hospital C: Treatment of the patients most likely to benefit, namely those who present within 48 h of symptom onset. Hospital D: Prophylaxis of exposed staff and treatment of all probable and confirmed cases, regardless of severity. |
Stakeholder Reactions: Consumers supported the approach of reserving antiviral medications for those most likely to benefit. Providers did not reach consensus in support of a particular approach, but strongly advocated for the protection of health care providers and first responders as a top priority. Both groups agreed that decisions governing the prioritization of scarce resources must be unified at the state level. Both groups agreed that, for this strategy to be effective, it must be accompanied by aggressive risk communication to health care providers and the public. |
| Scenario 2: Prioritization of Critical Care | |
| Context: You are 6 wk into the pandemic, and the health care system has been taxed beyond capacity, with every hospital bed full, every ventilator in use, and all health care providers working extended shifts. To increase the number of available beds to accommodate the surge of influenza patients, all scheduled operations have been postponed for the past 2 wk. Issue: The postponed procedures include diagnostic and palliative operations for patients with pancreatic cancer, ovarian cancer, and malignant brain tumors, among other diseases. For many of these patients, their expected survival is <6 mo, but without immediate operations, they will likely die within 2 wk. As a result of the pandemic, medical resources are scarce, and the usual critical care that would follow those operations cannot be provided to all in need. Hospitals across the country are independently making decisions to govern how to modify standards of critical care to provide limited but high-yield critical care interventions and processes for many additional patients. Hospital A: Providing critical care according to usual standards on a first-come, first-served basis. Hospital B: Providing key critical care interventions only to those patients with an expected survival of >6 mo. |
Stakeholder Reactions: Both consumers and providers strongly opposed the approach of maximizing life-years saved by only providing key critical care interventions to patients with an expected survival of >6 mo. Providers felt that triage on a case-by-case basis would be more realistic and ethically sound, whereas consumers were strongly and emotionally opposed to any model of limiting critical care interventions. Providers also favored individual hospitals having ultimate authority over such decisions, using an institutional review board model, and identifying a small committee to which these decisions could be referred. |
| Scenario 3: Government Control of Private Institutions | |
| Context: You are 2 mo into the pandemic, and all health care facilities are challenged by continuing to provide care with increasingly limited resources. The large medical centers have managed to cope, but many community hospitals have been struggling to continue providing care. Issue: An effective community response to the pandemic requires that all health care facilities be mobilized to their fullest potential, but these community hospitals require outside logistical support and supplies to continue operating. Anticipating these problems, states across the country are establishing laws to govern seizure of private assets. State A: After trying without success to persuade the large medical centers to provide some of their ventilators and expert staff to community hospitals, state A seized and redistributed ventilators. State B: Fearing that it would create a disincentive for preparedness among hospitals in the future, state B did not seize hospital resources. As a result, several of the smaller community hospitals in state B are no longer able to staff available beds due to shortages of personnel and resources. |
Stakeholder Reactions: Both consumers and providers opposed state seizure and redistribution of hospital-owned ventilators. Providers felt that it would be more practical to transfer patients to hospitals with available resources rather than to move ventilators and other resources. Consumers were concerned that seizure and redistribution of resources would be a disincentive to hospital preparedness. Both groups were strongly in favor of state tracking of ventilators and other health care resources. |
| Scenario 4: Provider Safety vs Duty to Care | |
| Context: Dr Smith is a surgeon at hospital B. Ever since his hospital’s cache of N-95 respirators was depleted last week, a number of Dr Smith’s colleagues have contracted influenza. Issue: Dr Smith fears for his own safety in the absence of appropriate personal protective equipment, and is also concerned about exposing his wife and 2 young children to influenza. His wife insists that he stay home from work rather than risking exposure, but Dr Smith has a deep commitment to his profession and feels a strong duty to care for his patients. In light of his concerns, Dr Smith is torn between his personal desire to protect himself and his family and his professional mission to use his skills and expertise to help the patients who need him. |
Stakeholder Reactions: Both consumers and providers believed that Dr Smith should continue to work, despite his concerns about his personal safety. Providers emphasized the importance of the ethical code governing physician duty to care, and noted that failing to care for patients may result in legal and/or licensing issues. Both groups strongly supported prospective action on behalf of hospitals to protect their staff and families of staff so that issues such as this do not arise, for example, stockpiling personal protective equipment, promoting personal/family emergency preparedness, and providing emergency accommodations for staff who do not want to go home and risk infecting their families. |
| Scenario 5: Prioritization of Critical Care—The Provider’s Perspective | |
| Context: As a surgeon, Dr Smith deeply opposes hospital B’s decision to provide key critical care interventions only to those patients with an expected survival of >6 mo. Issue: This new rule requires that Dr Smith cancel a bowel obstruction surgery scheduled for later this week. Without surgery, his patient—a 36-y-old mother of 3 with ovarian cancer—will die within 2 wk. Dr Smith is considering performing the operation in violation of hospital rules, potentially risking his career. In light of his disagreement with recent hospital policies, Dr Smith is torn between his professional mission to use his skills and expertise to help the patients who need him, and his obligation to observe the rules of his institution. |
Stakeholder Reactions: Although both groups expressed the importance of health care providers serving as advocates for their patients, providers particularly opposed Dr Smith violating hospital policy. Providers acknowledged that a surgeon’s decision to violate hospital rules would implicate a number of others in the process. Providers identified the need for improved systems within hospitals to support physicians in the event that rules governing the allocation of critical care interventions are introduced, for example, liability protection, mental health support. |
The first scenario in the table focused on allocation of scarce resources. When asked to consider a range of strategies for allocating antiviral medications, consumers supported the approach of reserving antivirals for those most likely to benefit. HCPs did not reach consensus in support of a particular approach, but strongly advocated for the protection of HCPs and first responders as a top priority. Both groups agreed that decisions governing the prioritization of scarce resources must be unified at the state level, requiring aggressive risk communication to HCPs and the public to be effective.
Two of the scenarios focused on prioritization of critical care (1 from the consumer’s perspective and 1 from the provider’s perspective) and provoked the most intense discussion. Both consumers and HCPs strongly opposed the approach of maximizing life-years saved by providing key critical care only to patients with an expected survival greater than 6 months. HCPs believed that triage on a case-by-case basis would be more realistic and ethically sound, whereas consumers were strongly and emotionally opposed to any model of limiting critical care. HCPs also favored individual hospitals having ultimate authority over such decisions, using an ethics review board model, and identifying a small committee to which these decisions could be referred.
The third scenario focused on government control of private assets. Both consumers and providers opposed state seizure and redistribution of hospital-owned ventilators. The fourth scenario focused on HCP duty to care. Most consumers and HCPs support the idea that HCPs have an obligation to keep working in the event of a pandemic, and everyone strongly supported prospective action on behalf of hospitals to protect their staff and families of staff (ie, reciprocity).
Establishing Guidelines for Altered Standards of Care in a Pandemic
The group convened its last in-person meeting in October 2006 to reach final consensus on the development of Massachusetts’ Guidelines for the Development of Altered Standards of Care for Influenza Pandemic. During this meeting, the findings from the stakeholder meetings were presented, and areas where the stakeholder reactions differed from the opinions of the group members were discussed at length. Following extensive deliberation, the group collectively identified 4 goals and 7 principles to guide the allocation of limited resources and establishment of ASC protocols (described below). The group also recommended that MDPH convene a multidisciplinary advisory committee to advise on specific protocols and decisions.
The guidelines were drafted by the MDPH general counsel in November 2006, and were vetted through the group before presentation to the Massachusetts Statewide Surge Committee later that month. Feedback from all interested parties was solicited, and the draft guidelines underwent 2 subsequent rounds of revision between November 2006 and June 2007. The purpose of the guidelines is to establish the principles necessary to guide the drafting of ASC priorities and protocols and the process for implementing them during a public health emergency. An overview of the process by which ASC would be implemented is shown in Figure 1. The guidelines are described in Results.
FIGURE 1.
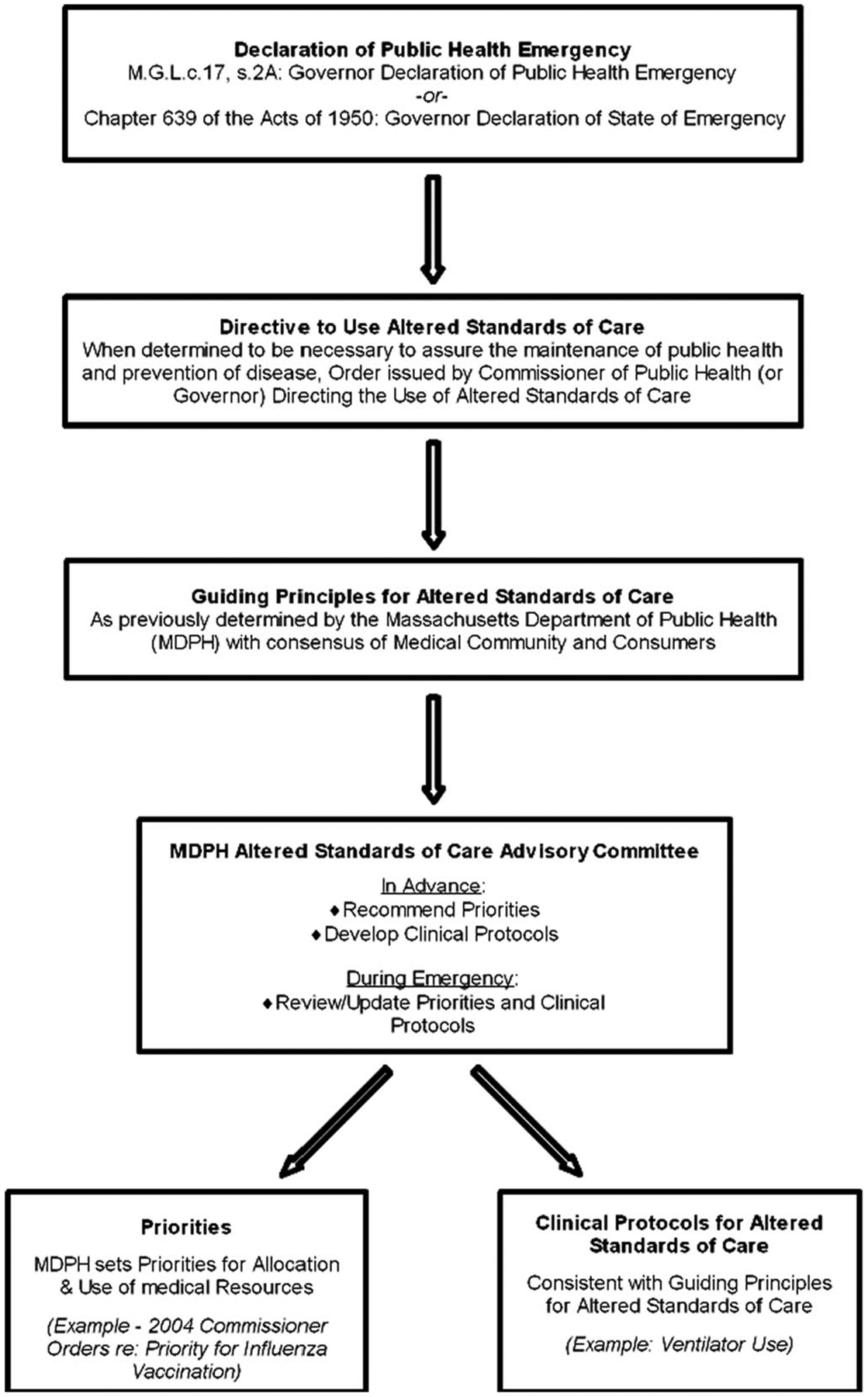
Massachusetts’ process for the development of altered standards of care for pandemic influenza
RESULTS
Public Health Goals
In the event of an influenza pandemic in which public health and health care needs may potentially exceed available resources, Massachusetts public health authorities will ensure that all actions and decisions are aligned with the following 4 goals:
Control the pandemic to the extent possible: protect the public from mass outbreak of disease and resultant morbidity and mortality.
Maximize positive patient outcomes when health care needs exceed available resources.
Establish principles and guidelines to assist HCPs to continue to provide care in an ethical manner during circumstances that make delivery of health care services in the normal course difficult, if not impossible.
Establish processes directed by MDPH for determining priorities for the use of limited health care resources and to establish ASC clinical protocols for HCPs, including health care practitioners at all levels and all institutions and entities that deliver health care. To the extent possible, this includes having in place these priorities and ASC protocols before an influenza pandemic, and establishing a process for reevaluating these priorities and ASC protocols during an influenza pandemic to reflect changing conditions and circumstances. It is anticipated that the principles in these guidelines will remain constant and that any changes in priorities or ASC protocols will be made in conformity with these principles.
Process for Decision Making on Allocation of Limited Resources and ASC Protocols
Massachusetts public health authorities will observe the following decision-making processes regarding the prioritization of limited health care resources and related ASC protocols:
Following a declaration by the governor that there is an emergency that is detrimental to the public’s health, the commissioner of public health may, if he or she deems such action necessary to ensure the maintenance of public health during such period of emergency, order adherence to the ASC priorities and protocols.
Priorities for distribution of limited medications and other supplies not addressed by ASC protocols will be determined by MDPH with input from an advisory committee. See below for principles to guide prioritization of certain groups.
ASC protocols will be prepared by the members of the ASC Advisory Committee in consultation with MDPH.
Priorities and ASC protocols will be set in advance of an influenza pandemic to the extent possible; based on principles of distribution of limited resources outlined below; proportional to the existing conditions; implemented only as necessary; consistent across the Commonwealth with appropriate local control and implementation as well as HCP discretion; implemented at provider or institution level in conformance with guidelines; and subject to continuous review and reassessment by MDPH and the ASC Advisory Committee.
Principles for Allocation of Limited Resources and ASC Protocols
The guidelines are intended to support the accelerated decision making necessary to effectively control the pandemic and maximize patient outcomes. To ensure that this is accomplished in an ethical manner, the guidelines include the 7 guiding principles agreed upon by the group and supported by the stakeholders. In summary, these principles state the following:
Limited resources will be allocated so as to maximize the number of lives saved (determined on the basis of the best available medical information, implemented in a manner that provides equitable treatment of any individual or group of individuals based on the best available clinical knowledge and judgment, and implemented without discrimination or regard to sex, sexual orientation, race, religion, ethnicity, disability, age, income, or insurance status). Age and/or disability may be considered along with other risk factors in allocating resources to save as many lives as possible, but the importance of saving older adults or people with disabilities is the same as for others. The assessment of risk factors should be made on the basis of the best available medical information, clinical knowledge, and clinical judgment. This principle ensures that people are not denied medical care based solely on their age or disability. It does allow for the consideration of risk factors, however, based on the individual’s medical condition. This medical condition can be the consequence of the aging process or of a particular disability and could affect the individual’s ability to benefit from, withstand, and survive the scarce medical intervention needed by others. This consideration is in conformance with the overarching principle of maximizing the number of lives saved. Note that there is no inclusion for the principle of maximizing life-years saved or of the “life-cycle” or “fair innings principle,”27 although these ethical concepts may be considered and included as the guidelines evolve.
ASC protocols will permit flexibility for physician discretion, exercised in good faith, under circumstances that warrant exception from the protocols and subject to prior expedited review process. Health care institutions will establish capacity for expeditious review of exceptions.
Health care institutions will be responsible for developing mutual aid plans on a regional basis.
ASC protocols will recognize any changes in practice necessary to provide care under conditions of scarce resources or overwhelming demand for care; an expanded scope of practice for HCPs; the use of alternate care sites, such as influenza specialty care units at facilities other than hospitals; and reasonable, practical standards for documentation of delivery of care.
HCPs will be responsible for adhering to the protocols to protect the public’s health.
Patient care will be provided within the context and limitations necessitated by the public health emergency.
The Commonwealth and individual employers have a duty to prioritize the care and protection of HCPs.
Communication
During an influenza pandemic, Massachusetts public health authorities will observe transparency of decision making, and public outreach should stress MDPH’s existing and ongoing collaboration with the universe of HCPs, hospitals, and others in developing protocols and procedures. Moreover, public health officials should disclose as much information as necessary to protect public health without releasing personal identifying information in a manner that is consistent with state and federal law.
Individual Rights
During an influenza pandemic, Massachusetts public health authorities will take all measures to ensure that civil liberties and patients’ rights are protected to the greatest extent possible. It is recognized, however, that the protection of the public’s health during an influenza pandemic may require limitations on these liberties and rights.
Provider Liability
The guidelines state that during an influenza pandemic, health care providers who deliver care in accordance with the priorities and ASC protocols developed by MDPH and the ASC Advisory Committee, including care provided outside their scope of practice or scope of license, will be considered to have provided care at the level at which the average, prudent HCP in a given community would practice. In addition, the guidelines state that any individual patient to whom an approved ASC is provided should have no basis to assert in a medical malpractice claim against the HCP that an appropriate level of care was not provided. Moreover, the HCP, having met the requisite standard of care, should not be held liable in a malpractice action based on the provision of care in accordance with an approved ASC.
Next Steps
Per the recommendation of the MDPH-Harvard Joint Working Group, the ASC Advisory Committee has been convened. Committee members include physicians, nurses, ethicists, lawyers, hospital administrators, and emergency services personnel. The advisory committee has reviewed all available resources from ASC work done at the federal and state levels and has been assigned the task of making more specific recommendations for resource allocation and ASC. These recommendations will then be vetted with an expanded committee whose members will include other disciplines and representatives of other interested groups. Ultimately, the recommendations will be released for public comment, and final priorities and ASC will be the subject of broad educational and community outreach efforts. Initial recommendations should be finalized by June 2009. These recommendations, as accepted by MDPH, will be the basis for the ongoing policy decisions with respect to implementation of ASC during a public health emergency. In the interim, MDPH and HSPH intend to use these final ASC priorities and protocols as the subject of further research and collaboration with other states and the federal government in an effort to achieve consistent shared knowledge and understanding.
To identify best practices and promote the sharing of resources, HSPH-CPHP and MDPH have contacted state health departments across the United States to assess the extent of planning for ASC that has occurred. In this effort, 2 HSPH-CPHP representatives attempted to contact all 50 state health departments and arrange a 30-minute structured interview regarding ASC planning. HSPH-CPHP and MDPH intend to distribute the results of their analyses and resources identified to their fellow states at the conclusion of the project.
DISCUSSION
Organizations across the United States have paid increasing attention to ASC planning.28,29 The Centers for Disease Control and Prevention and the Agency for Healthcare Research and Quality, among others, have published relevant recommendations and guidance.15,20,30 Others have published clinical decision support tools and recommendations.16,31–33 These resources present important frameworks, but they would require consistency in adoption and enforcement to be effective and equitable. Because federal authorities can provide only general guidance, the responsibility falls to state public health authorities to develop standards for equitable allocation of care. A recent report from the Government Accountability Office stated that only 7 of the 20 states surveyed had adopted or were drafting standards of medical care for a mass casualty event, and only 3 of those 7 had adopted some altered standards of care guidelines.34 To our knowledge, this article is among the first to describe the planning process for ASC at the state level.
Consistent with the literature, 3 central themes resounded throughout our discussions: the value of accountability for reasonableness while engaging in ASC planning, the importance of reciprocity for HCPs, and the need for mechanisms to ensure equity throughout the process.
Accountability for Reasonableness
The group recognizes that its work will neither preclude all difficult decisions nor align with every viewpoint that may emerge. As described by ethicist Norman Daniels17,35 (a member of the group) and widely referenced in the context of disaster preparedness and response: “We are likely to find reasonable disagreement about principles that should govern priority setting. In the absence of consensus on principles, a fair process allows us to agree on what is legitimate and fair.”17 As described above, the group strove to meet the spirit of “accountability for reasonableness,” namely, “transparency about the grounds for decisions; appeals to rationales that all can accept as meaningful and relevant to meeting health needs fairly; and procedures for revising decisions in light of challenges to them.”17
Reciprocity
The issue of reciprocity for HCPs, 1 of the 7 guiding principles included in the guidelines, was especially highlighted in the severe acute respiratory syndrome epidemic when more than 20% of those infected in 2003 were HCPs.36 Despite protection measures for them, HCPs working during an influenza pandemic will likely assume an elevated risk for infection while carrying out their duty to care. Per Thompson and colleagues, “Reciprocity requires that society supports those who face a disproportionate burden in protecting the public good and takes steps to minimize their impact as far as possible.”22 Additional consideration is required to determine how best to put this principle into practice.
Ensuring Equity
The decision to prioritize scarce resources and critical care to maximize lives saved also runs the risk of further marginalization of those who are already disadvantaged with respect to access to health care. Hence, the goals and principles reflected the importance of tempering a utilitarian approach with nonmalfeasance, proportionality, respect for people, and justice.20 Ongoing efforts are examining ways to functionally incorporate checks and balances in support of these ends in our process. In addition, Massachusetts’ work on ASC coincides with broader statewide efforts to improve preparedness for vulnerable populations.37
CONCLUSIONS
We recognize that our experience in Massachusetts has provided only the first step: the basic principles and a framework for establishing the actual ASC and the method for implementing them. It will be more difficult to determine the priorities for the allocation of limited health care resources and creating the specific ASC protocols. We will continue to engage a diverse range of stakeholders in a transparent discussion of difficult topics, using the 7 guiding principles while noting that “public health officials have a responsibility to maximize preparedness to minimize the need to make allocation decisions later.”20 It is our hope that such stewardship will guide public health for the future.
Acknowledgments
This activity was supported under a cooperative agreement from the Centers for Disease Control and Prevention, grant U90/CCU124242-03.
Footnotes
The article was written before Dr Koh’s appointment as the Assistant Secretary of Health and does not necessarily represent the views of DHHS or the United States.
The contents of this manuscript do not necessarily reflect the views of the Centers for Disease Control and Prevention.
Authors’ Disclosures
The authors report no conflicts of interest.
Contributor Information
Donna Levin, Massachusetts Department of Public Health.
Rebecca Orfaly Cadigan, Center for Public Health Preparedness, Division of Public Health Practice, Harvard School of Public Health.
Paul D. Biddinger, Department of Emergency Medicine, Massachusetts General Hospital.
Suzanne Condon, Massachusetts Department of Public Health.
Howard K. Koh, Harvard School of Public Health, is currently the Assistant Secretary of Health in the US Department of Health and Human Services (DHHS).
REFERENCES
- 1.Trust for America’s Health. A Killer Flu. June 2005. http://healthyamericans.org/reports/flu/Flu2005.pdf. Accessed July 14, 2008.
- 2.Mehta S. Disaster and mass casualty management in a hospital: how well are we prepared? J Postgrad Med. 2006;52:89–90. [PubMed] [Google Scholar]
- 3.Gostin LO, Powers M. What does social justice require for the public’s health? Public health ethics and policy imperatives. Health Affairs. 2006;25:1053–1060. [DOI] [PubMed] [Google Scholar]
- 4.Huber SJ, Wynia MK. When pestilence prevails Physician responsibilities in epidemics. Am J Bioethics. 2004;4:W5–W11. [DOI] [PubMed] [Google Scholar]
- 5.Reid L Diminishing returns? Risk and the duty to care in the SARS epidemic. Bioethics. 2005;19:348–361. [DOI] [PubMed] [Google Scholar]
- 6.Ruderman C, Tracy CS, Bensimon CM, et al. On pandemics and the duty to care: whose duty? Who cares? BMC Medical Ethics. 2006;7:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singer PA, Benatar SR, Bernstein M, et al. Ethics and SARS: lessons from Toronto. BMJ. 2003;327:1342–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sokol DK. Virulent epidemics and scope of healthcare workers’ duty of care. Emerg Infect Dis. 2006;12:1238–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.University of Toronto Joint Center for Bioethics (Working Group). Ethics and SARS: Learning Lessons from the Toronto Experience. http://www.yorku.ca/igreene/sars.html. Accessed August 21, 2007.
- 10.Nossiter A Grand Jury Won’t Indict Doctor in Hurricane Deaths. New York Times. July 25, 2007. http://www.nytimes.com/2007/07/25/us/25doctor.html?scp[H11005]1&sq[H11005]Grand%20Jury%20Won%92t%20Indict%20Doctor%20in%20Hurricane%20Deaths&st[H11005]cse. Accessed May 4, 2009. [Google Scholar]
- 11.Okie S Dr. Pou and the hurricane—implications for patient care during disasters. New Engl J Med. 2008;358:1–5. [DOI] [PubMed] [Google Scholar]
- 12.US Centers for Disease Control and Prevention. FluSurge. http://www.cdc.gov/flu/flusurge.htm. Accessed November 27, 2006.
- 13.Commonwealth of Massachusetts. The General Laws of Massachusetts. http://www.mass.gov/legis/laws/mgl/index.htm. Accessed October 3, 2008.
- 14.Challen K, Bentley A, Bright J, et al. Clinical review: mass casualty triage—pandemic influenza and critical care. Crit Care. 2007;11:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.US Department of Health and Human Services, Agency for Healthcare Research and Quality. 2005. Altered Standards of Care in Mass Casualty Events. http://www.ahrq.gov/research/altstand. Accessed May 2, 2009.
- 16.Hick JL, Rubinson L, O’Laughlin DT, et al. Clinical review: allocating ventilators during large-scale disasters—problems, planning, and process. Crit Care. 2007;11:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daniels N Accountability for reasonableness. BMJ. 2000;321:1300–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larkin GL, Arnold J. Ethical considerations in emergency planning, preparedness, and response to acts of terrorism. Prehosp Disast Med. 2003;18:170–178. [DOI] [PubMed] [Google Scholar]
- 19.Koenig KL, Cone DC, Burstein JL, et al. Surging to the right standard of care. Acad Emerg Med. 2006;13:195–198. [DOI] [PubMed] [Google Scholar]
- 20.Kinlaw K, Levine R. Ethical Guidelines in Pandemic Influenza—Recommendations of the Ethics Subcommittee of the Advisory Committee to the Director, Centers for Disease Control and Prevention. 2007. http://www.pandemicflu.utah.gov/docs/20070515-PanFluEthicGuides.pdf. Accessed May 2, 2009. [DOI] [PubMed]
- 21.Bernstein M, Hawryluck L. Challenging beliefs and ethical concepts: the collateral damage of SARS. Crit Care. 2003;7:269–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thompson AK, Faith K, Gibson JL, et al. Pandemic influenza preparedness: an ethical framework to guide decision-making. BMC Med Ethics. 2006;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pesik N, Keim ME, Iserson KV. Terrorism and the ethics of emergency medical care. Ann Emerg Med. 2001;37:642–646. [DOI] [PubMed] [Google Scholar]
- 24.Schoch-Spana M, Chamberlain A, Franco C, et al. Disease, disaster, and democracy: the public’s stake in health emergency planning. Biosecur Bioterror. 2006;4:313–319. [DOI] [PubMed] [Google Scholar]
- 25.Hawryluck L Ethics review: position papers and policies—are they really helpful to front-line ICU teams? Crit Care. 2006;10:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The Proceedings of the Public’s Health and the Law in the 21st Century: Fifth Annual Partnership Conference. J Law Med Ethics. 2007;35 (Suppl 4):11–137. [DOI] [PubMed] [Google Scholar]
- 27.White DB, Katz MH, Luce JM, et al. Who should receive life support during a public health emergency? Using ethical principles to improve allocation decisions. Ann Intern Med. 2009;150:132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hodge JG, Gostin LO, Vernick JS. The Pandemic and All-Hazards Act: improving public health emergency response. JAMA. 2007;297:1708–1711. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization. WHO Global Influenza Preparedness Plan. 2005. http://www.who.int/csr/resources/publications/influenza/GIP_2005_5Eweb.pdf. Accessed December 20, 2007.
- 30.US Department of Health and Human Services, Agency for Healthcare Research and Quality. Mass Medical Care with Scarce Resources. 2007. http://www.ahrq.gov/research/mce. Accessed May 2, 2009.
- 31.Devereaux A, Christian MD, Dichter JR, et al. Summary of suggestions from the Task Force for Mass Critical Care Summit, January 26–27, 2007. Chest. 2008;133:1S–7S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rubinson L, Nuzzo JB, Talmor DS, et al. Augmentation of hospital critical care capacity after bioterrorist attacks or epidemics: recommendations of the Working Group on Emergency Mass Critical Care. Crit Care. 2005;33:E1–E13. [DOI] [PubMed] [Google Scholar]
- 33.Hick JL, O’Laughlin DT. Concept of operations for triage of mechanical ventilation in an epidemic. Acad Emerg Med. 2006;13:223–229. [DOI] [PubMed] [Google Scholar]
- 34.US Government Accountability Office. States Are Planning for Medical Surge, but Could Benefit from Shared Guidance for Allocating Scarce Medical Resources. GAO-08–668. June 13, 2008. http://www.gao.gov/new.items/d08668.pdf. Accessed March 1, 2009. [Google Scholar]
- 35.Daniels N Just Health: Meeting Health Needs Fairly. Cambridge, UK: Cambridge University Press; 2008. [Google Scholar]
- 36.Tai DYH. SARS plague: duty to care or medical heroism? Ann Acad Med Singapore. 2006;35:374–378. [PubMed] [Google Scholar]
- 37.Nick GA, Savoia E, Elqura L, et al. Emergency preparedness for vulnerable populations: people with special health-care needs. Public Health Rep. 2009;124:338–343. [DOI] [PMC free article] [PubMed] [Google Scholar]


