Abstract
Objective
This study aims to investigate the 10-year trends and disparities in underweight, overweight, and obesity among older adults aged 65 years and older in China from 2008 to 2018.
Methods
We used four waves (2008, 2011, 2014, and 2018) of data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), a national community-based cross-sectional survey conducted every 2–3 years. Body weight and height were measured by trained assessors following standardized procedures. BMI was calculated and divided into underweight (< 18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0-29.9 kg/m2), obese (≥ 30.0 kg/m2) according to WHO reference. Multinomial logistic regression models were used to examine factors related with abnormal BMI groups, after adjusting for potential confounders.
Results
Among 46,543 older adults in China, the prevalence rates of underweight decreased with each survey year from 2008 to 2018, declining from 20.05 to 7.87% (p < 0.001). In contrast, the prevalence rates of overweight and obesity showed an increasing trend (all p < 0.001). Specifically, the prevalence of overweight rose from 12.82% to 2008 to 28.45% in 2018, and the prevalence of obesity increased from 1.62% to 2008 to 4.95% in 2018. In the multinomial logistic regression model, survey year, gender, residence, marital status, economic status, numbers of chronic diseases, smoking status, sleep quality, and functional disability were factors related with obesity.
Conclusion
The prevalence rates of overweight and obesity were increasing while the prevalence of underweight and normal weight significantly decreased from 2008 to 2018 among older adults in China, which poses a huge challenge for chronic disease. There is an urgent need for intervention policy planning and early prevention of abnormal body weight for the preparation of an aging society.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-16310-6.
Keywords: Underweight, Overweight, Obesity, Older adults, Observational study
Background
Overweight and obesity represent significant global public health concerns [1]. The prevalence of obesity worldwide has nearly tripled over the past approximately 50 years, reaching alarming levels. This poses a significant threat to public health as it is closely associated with various leading causes of morbidity and mortality, including coronary heart disease, cancers, hypertension, and type 2 diabetes mellitus [1–3]. A recent study combined conventional age-period projections with the concept of a wave-shaped obesity epidemic to predict the long-term prevalence of obesity in 18 European countries and the United States. The study indicated that obesity prevalence is expected to peak between 2026 and 2054, with the USA and UK reaching the highest maximum levels initially [4]. Although the USA and Europe currently have the highest obesity prevalence rates, obesity has also emerged as a significant public health issue in China, leading to substantial national healthcare expenditures [5].
Previous studies have demonstrated that average body weight steadily increases with age and reaches its peak between the ages of 50 to 65 years [2, 6]. However, the results of different countries were quite different [6, 7]. Considerable attention should be paid to the study of body weight issues among older adults because of the accelerated aging progress across the world [8]. As the most important developing country with the largest number of elderly people in the world, China is also confronted with the challenges of population aging [9]. The national prevalence estimates for overweight and obesity in adults aged ≥ 18 years old in China for the period 2015-19 were 34.3% and 16.4%, respectively, and the prevalence varied based on sex, age group, and geographical location [5]. Findings from the China Chronic Disease and Risk Factors Surveillance program, which was established in 2004, showed that the obesity prevalence among participants aged 18–69 years increased from 3.1% to 2004 to 8.1% in 2018 [10]. However, there is insufficient evidence focusing on trends in overweight and obesity prevalence among older adults in China. The Chinese Longitudinal Healthy Longevity Survey (CLHLS), which is another national tracking study focusing on the health status of older adults in China, provides us with the opportunity to better address the issues of underweight, overweight, and obesity among older adults [11].
In this study, we aimed to investigate the trends and disparities in body weight change among older adults aged 65 years and older in China from 2008 to 2018 and provide some information for more targeted policies, using the national cross-sectional data from eight representative health surveys among older adults conducted in China in 2008, 2011, 2014, and 2018.
Methods
Study population and data source
This is a national observational study using data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS). The CLHLS aimed at investigating the determinants of healthy longevity among the older Chinese population aged 65 + and covered 22 of 31 provinces in mainland China [12, 13]. The survey was conducted randomly in about half of the cities/counties in 22 out of 31 provinces in mainland China, covering about 85% of the national population. The surveys investigated socio-economic information, history of health, life habits, and other information by questionnaire and health status by physical examinations. It began in 1998 and continued in 2000, 2002, 2005, 2008, 2011, 2014, and 2018, with about a 90% response rate for each wave [14]. Nearly one-third of participants from each wave were from the previous wave, and the rest were new recruits because of the mixed longitudinal design of CLHLS. To reduce the selection bias in different waves and ensure the consistency of the study population, new recruits were selected based on the similarities in gender, age, and general characteristics with those who were lost during the follow-up. More details of the CLHLS study design can be found elsewhere [12–14].
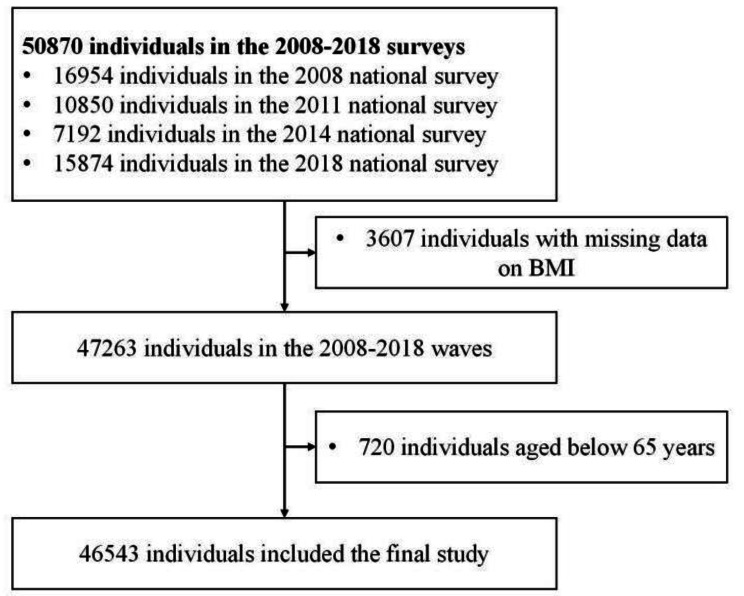
There was a total of 50,870 participants in the four waves included in our study (16,954 in 2008, 10,850 in 2011, 7,192 in 2014, and 15,874 in 2018). Among them, we excluded 3,607 participants who had missing data on Body Mass Index (BMI) and 720 participants aged below 65 years, yielding 46,543 participants (91.49%) in the final study (Fig. 1). Of which participants aged ≤ 79 years old accounted for 81.93%, 80–89 years old accounted for 16.33%, 90–99 years old accounted for 1.70%, and ≥ 100 years old accounted for 0.04%.
Fig. 1.
Flowchart of the inclusion of participants. Notes: BMI, Body Mass Index
Body mass index
All information was obtained in the homes of participants through face-to-face questionnaire interviews and physical health examinations by trained investigators. Body weight (in kilograms) and height (in centimeters) were measured by trained assessors following standardized procedures. BMI was calculated by using the unified formula in National Center for Health Statistics as bodyweight (kg) divided by squared body height (m2). Participants were divided into four groups according to their BMI using the standard weight status categories from WHO reference, including underweight (BMI < 18.5 kg/m2), normal (BMI 18.5–24.9 kg/m2), overweight (BMI 25.0-29.9 kg/m2), obese (BMI ≥ 30.0 kg/m2).
Explanatory variables
Following previous studies [14–17], we included explanatory variable groups derived from the CLHLS in this study, such as wave indicators (investigation years), demographic factors, socioeconomic status, lifestyle habits, and health conditions variables. Demographic factors included region (urban or rural), gender (male or female), age groups (≤ 79 years,80–89,90–99 or ≥ 100 years), marital status (unmarried, married, or divorced or widowed), and living patterns (living with family members, living in an institution, or living alone). Socioeconomic status included years of schooling (0 years or ≥ 1 years), economic status compared with other local people (poor, fair, or rich). Lifestyle habits included smoking status (never, previous, or current), alcohol intaking status (never, previous, or current), regular exercise (never, previous, or current), dietary diversity (poor, moderate, or good), participating in organized social activities (almost every day, sometimes, or never). Dietary diversity was evaluated as poor (0–3), moderate [4–6], or good [7–9] by the calculated dietary diversity score (0–9) reflecting the consumption numbers of nine types of food groups (meat, vegetables, fish, eggs, fruits, legumes, milk, tea, and nuts) [18]. Health status included body mass index(BMI) (underweight, normal weight, overweight, or obesity), numbers of chronic diseases (0, 1, or ≥ 2), functional disability (no or yes), sleeping quality (good or bad), sleeping length(<5 h, 5–9 h, or ≥ 9 h), self-reported health (good, fair, or poor), self-reported quality of life (good, fair, or poor). Functional disability was defined as the self-reported difficulty with any of the following activities of daily living (ADL) items, such as dressing, eating, bathing, continence, toileting and cleaning, or indoor movement [18].
Statistical analysis
Baseline characteristics were presented as proportions for categorical variables. Pearson Chi-square tests for trends were used to compare the prevalence rates of abnormal body weights between different baseline characteristics groups, such as survey year, gender, age groups. The multinomial logistic regression model was used to further assess the association between abnormal body weight and potential related factors. In the multinomial logistic regression model, we included survey year, gender, age groups, marital status, residence, economic status, living pattern, education level, numbers of chronic diseases, smoking status, alcohol intaking status, regular exercise, dietary diversity, sleeping quality, sleeping length, housework, outdoor activities, functional disability, self-reported quality of life, self-reported health. In the sensitive analysis, we divided age by per 5 years (65–69, 70–74, 75–79, 80–84, 85–89, ≥ 90 years old) instead of 10 years to examine the robust of the results in the models. A two-tailed P-value of less than 0.05 was considered statistically significant. All the analyses above were performed using Statistical Product and Service Solutions (SPSS 25.0).
Results
Characteristics of the study participants
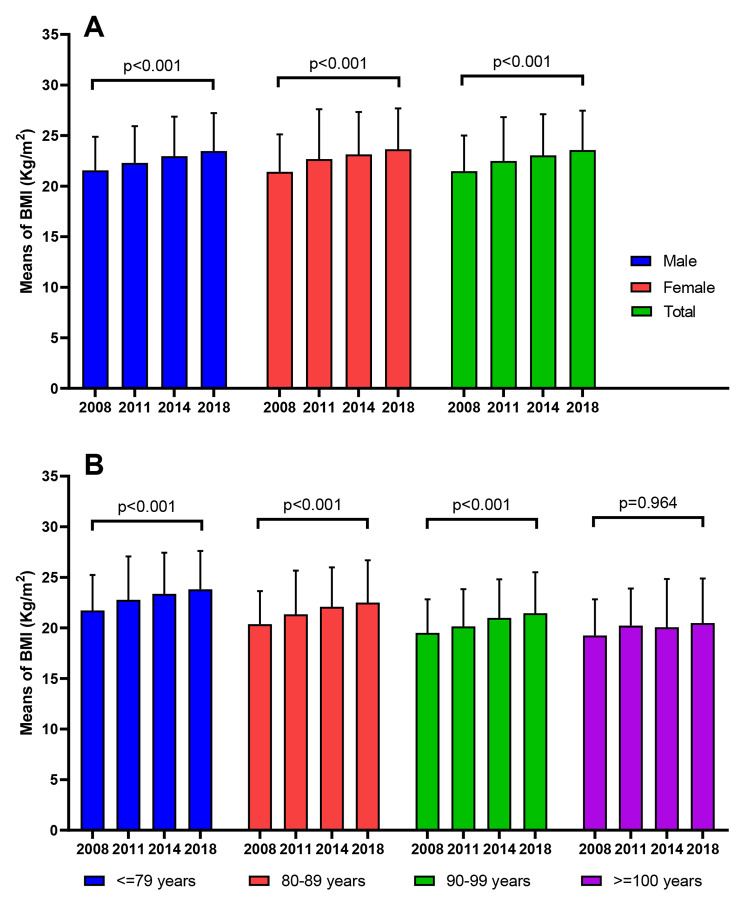
We included a total of 46,543 participants in four waves of CLHLS surveys in 2008, 2011, 2014 and 2018 (supplemental Table 1). The mean BMI of all subjects was 22.56 ± 3.98 kg/m2, with 22.51 ± 3.69 kg/m2 for males and 22.61 ± 4.23 kg/m2 for females. BMI increased over the years from 2008 to 2018 in both men, women and the all subjects (p < 0.001) in Fig. 2A. Significant differences were observed in the distribution of survey year, gender, living area, family economic status, living pattern, education level, number of chronic diseases, smoking, drinking, regular exercise, dietary diversity score, sleep duration, sleep quality, housework, outdoor sports and other factors in different years (all p < 0.001). Except for the ≥ 100 years old group, BMI in other age groups also showed a trend of increasing with the years (p < 0.001) in Fig. 2B.
Fig. 2.
Trends of BMI in different survey years of 2008, 2011, 2014, and 2018. Notes: BMI, Body Mass Index
Trends of underweight, overweight, and obesity
From 2008 to 2018, the rate of the underweight and normal weight decreased with each passing year, and the rate of overweight was increasing in the older people in China(Fig. 2B, p<0.05).The prevalence rates of overweight and obesity were higher in female than in male (overweight: 20.37% vs. 19.88%; obesity: 4.79% vs. 2.60%, p < 0.05). Furthermore, the prevalence of overweight and obesity decreased with age but increased among older adults residing in urban areas, higher economic levels, non-smokers and non-drinkers, those experiencing more than 2 chronic diseases, and older adults with higher dietary diversity scores, in comparison to their counterparts, respectively (all p < 0.05, as shown in Table 1). The rates of underweight were higher in females compared to males (15.28% vs. 12.25%, p < 0.05). Additionally, underweight rates increased with age and were also higher among divorced or widowed individuals, older adults residing in rural areas, those with poor family conditions, current smokers or drinkers, and those sleeping less than 5 h, in comparison to their counterparts, respectively (all p < 0.05).
Table 1.
Comparison of characteristics among 46,543 older adults by BMI groups
| Total | Normal | Underweight | Overweight | Obesity | p value | |
|---|---|---|---|---|---|---|
| Survey year | < 0.001 | |||||
| 2008 | 16,108 | 10,554(65.52) | 3229(20.05) | 2065(12.82) | 260(1.62) | |
| 2011 | 9166 | 5703(62.22) | 1370(14.95) | 1690(18.44) | 403(4.39) | |
| 2014 | 6390 | 4013(62.80) | 656(10.27) | 1383(21.64) | 338(5.29) | |
| 2018 | 14,879 | 8738(58.73) | 1172(7.87) | 4232(28.45) | 737(4.95) | |
| Gender | < 0.001 | |||||
| Male | 22,518 | 14,698(65.27) | 2757(12.25) | 4476(19.88) | 586(2.60) | |
| Female | 24,025 | 14,310(59.56) | 3670(15.28) | 4894(20.37) | 1151(4.79) | |
| Age groups (years) | < 0.001 | |||||
| ≤ 79 | 38,133 | 23,797(62.40) | 4522(11.86) | 8305(21.78) | 1510(3.96) | |
| 80–89 | 7599 | 4745(62.45) | 1653(21.75) | 991(13.04) | 211(2.77) | |
| 90–99 | 792 | 456(57.57) | 246(31.03) | 73(9.27) | 17(2.13) | |
| ≥ 100 | 19 | 10(53.30) | 7(38.63) | 1(5.90) | 0(2.17) | |
| Marital status | < 0.001 | |||||
| Unmarried | 591 | 369(62.51) | 95(16.08) | 119(20.11) | 8(1.30) | |
| Married | 30,498 | 19,021(62.37) | 3581(11.74) | 6777(22.22) | 1119(3.67) | |
| Divorced or widowed | 15,219 | 9474(62.25) | 2731(17.95) | 2421(15.91) | 593(3.89) | |
| Category of residence | < 0.001 | |||||
| Urban (city and town) | 21,402 | 13,128(61.34) | 2183(10.20) | 5114(23.90) | 977(4.56) | |
| Rural | 25,140 | 15,881(63.17) | 4244(16.88) | 4256(16.93) | 760(3.02) | |
| Economic status | < 0.001 | |||||
| Rich | 7305 | 4448(60.89) | 738(10.10) | 1770(24.22) | 349(4.78) | |
| Fair | 33,165 | 20,923(63.09) | 4361(13.15) | 6700(20.20) | 1181(3.56) | |
| Poor | 5875 | 3513(59.80) | 1310(22.30) | 861(14.66) | 190(3.24) | |
| Living pattern | < 0.001 | |||||
| Living with family members | 38,725 | 24,122(62.29) | 5258(13.58) | 7913(20.43) | 1432(3.70) | |
| Living in an institution | 577 | 350(60.63) | 89(15.38) | 114(19.71) | 25(4.28) | |
| Living alone | 6949 | 4396(63.26) | 1043(15.00) | 1245(17.91) | 266(3.83) | |
| Education level (years) | < 0.001 | |||||
| 0 | 18,623 | 11,512(61.82) | 3294(17.69) | 3121(16.76) | 697(3.74) | |
| ≥ 1 years | 27,919 | 17,496(62.67) | 3134(11.22) | 6250(22.38) | 1040(3.73) | |
| Numbers of chronic diseases | < 0.001 | |||||
| 0 | 15,557 | 10,559(67.87) | 2345(15.08) | 2268(14.58) | 385(2.48) | |
| 1 | 14,465 | 9002(62.23) | 2127(14.71) | 2825(19.53) | 510(3.53) | |
| ≥ 2 | 15,811 | 9007(56.97) | 1842(11.65) | 4141(26.19) | 821(5.19) | |
| Smoking status | < 0.001 | |||||
| Never | 28,867 | 17,546(60.78) | 3914(13.56) | 6115(21.18) | 1293(4.48) | |
| Previous | 6910 | 4427(64.06) | 873(12.63) | 1425(20.63) | 185(2.68) | |
| Current | 10,416 | 6851(65.77) | 1614(15.49) | 1751(16.81) | 200(1.92) | |
| Alcohol intaking status | < 0.001 | |||||
| Never | 26,997 | 16,302(60.38) | 3748(13.88) | 5718(21.18) | 1229(4.55) | |
| Previous | 4315 | 2822(65.38) | 518(12.00) | 853(19.77) | 123(2.85) | |
| Current | 10,416 | 6851(65.77) | 1614(15.49) | 1751(16.81) | 200(1.92) | |
| Regular exercise | < 0.001 | |||||
| Never | 24,526 | 15,525(63.30) | 3867(15.77) | 4344(17.71) | 790(3.22) | |
| Previous | 3219 | 2021(62.77) | 599(18.61) | 493(15.33) | 106(3.29) | |
| Current | 18,370 | 11,210(61.03) | 1907(10.38) | 4433(24.13) | 820(4.46) | |
| Dietary diversity | < 0.001 | |||||
| Poor | 12,357 | 7708(62.37) | 2279(18.44) | 1964(15.90) | 406(3.28) | |
| Moderate | 23,764 | 14,957(62.94) | 3174(13.36) | 4764(20.05) | 868(3.65) | |
| Good | 10,343 | 6277(60.69) | 973(9.41) | 2631(25.44) | 462(4.46) | |
| Sleeping quality | < 0.001 | |||||
| Good | 28,303 | 17,790(62.85) | 3495(12.35) | 5981(21.13) | 1038(3.67) | |
| Poor | 18,240 | 11,219(61.51) | 2932(16.08) | 3390(18.58) | 700(3.84) | |
| Sleeping length | < 0.001 | |||||
| < 5 h | 2951 | 1733(58.73) | 538(18.24) | 578(19.58) | 102(3.44) | |
| 5–9 h | 36,701 | 23,006(62.69) | 4813(13.12) | 7499(20.43) | 1382(3.76) | |
| > 9 h | 6680 | 4137(61.92) | 1047(15.67) | 1248(18.68) | 249(3.73) | |
| Housework | < 0.001 | |||||
| Almost everyday | 30,679 | 19,069(62.16) | 3979(12.97) | 6408(20.89) | 1223(3.99) | |
| Sometimes | 6556 | 4283(65.32) | 849(12.94) | 1237(18.87) | 188(2.87) | |
| Never | 9224 | 5616(60.89) | 1590(17.23) | 1695(18.38) | 323(3.50) | |
| Outdoor activities | < 0.001 | |||||
| Almost everyday | 24,540 | 15,461(63.00) | 2897(11.80) | 5344(21.78) | 838(3.41) | |
| Sometimes | 14,045 | 8578(61.08) | 1902(13.54) | 2915(20.76) | 649(4.62) | |
| Never | 7875 | 4920(62.47) | 1623(20.61) | 1084(13.77) | 248(3.15) | |
| Functional disability | < 0.001 | |||||
| No | 42,506 | 26,730(62.88) | 5733(13.49) | 8528(20.06) | 1515(3.56) | |
| Yes | 2958 | 1611(54.47) | 595(20.13) | 589(19.92) | 162(5.48) | |
| Self-reported quality of life | < 0.001 | |||||
| Good | 57,528 | 17,888(62.19) | 3233(11.24) | 6478(22.52) | 1165(4.05) | |
| Fair | 30,606 | 9741(63.66) | 2486(16.24) | 2577(16.84) | 499(3.26) | |
| Poor | 4037 | 1126(55.77) | 558(27.66) | 271(13.44) | 63(3.13) | |
| Self-reported health | < 0.001 | |||||
| Good | 22,492 | 14,467(64.32) | 2454(10.91) | 4811(21.39) | 760(3.38) | |
| Fair | 16,824 | 10,476(62.27) | 2290(13.61) | 3341(19.86) | 717(4.26) | |
| Poor | 6771 | 3812(56.29) | 1532(22.62) | 1176(17.37) | 251(3.71) | |
Notes: BMI, Body Mass Index
Factors associated with underweight
In the multinomial logistic regression model, older adults in China were significantly more likely to be underweight from 2008 to 2014 compared to the participants in 2018, with a decreasing risk though (OR = 2.33 in 2008, 95% CI: 2.13–2.55; OR = 1.81 in 2011, 95% CI: 1.64–2.01; OR = 1.25 in 2014, 95% CI: 1.11–1.41), after adjusted for other factors (as shown in Table 2). Moreover, male participants were less likely to be underweight compared to female (OR = 0.73, 95% CI: 0.67–0.80). Older adults living in urban areas (OR = 0.72, 95% CI: 0.68–0.77), the currently married (OR = 0.86, 95% CI: 0.80–0.93) and those with good sleep quality (OR = 0.86, 95% CI: 0.80–0.92) had a lower chance of being underweight compared to counterparts, respectively. When comparing the good dietary diversity scores, the results showed that the elderly with poor and fair scores were more likely to be underweight (OR = 1.35, 95% CI: 1.22–1.48; OR = 1.16, 95% CI: 1.06–1.26).
Table 2.
Multinomial logistic regression model a
| Underweight | Overweight | Obesity | ||||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |||
| Survey year | ||||||||
| 2008 | 2.33(2.13–2.55) | < 0.001 | 0.42(0.39–0.45) | < 0.001 | 0.33(0.28–0.39) | < 0.001 | ||
| 2011 | 1.81(1.64–2.01) | < 0.001 | 0.63(0.58–0.68) | < 0.001 | 0.93(0.79–1.08) | 0.328 | ||
| 2014 | 1.25(1.11–1.41) | < 0.001 | 0.79(0.72–0.86) | < 0.001 | 1.35(1.15–1.58) | < 0.001 | ||
| 2018 | 1.00 | 1.00 | 1.00 | |||||
| Gender | ||||||||
| Male | 0.73(0.67–0.80) | < 0.001 | 0.88(0.82–0.95) | 0.001 | 0.60(0.51–0.70) | < 0.001 | ||
| Female | 1.00 | 1.00 | 1.00 | |||||
| Age groups (years) | ||||||||
| ≤ 79 | 0.31(0.09–1.02) | 0.054 | 3.08(0.25–37.22) | 0.377 | 2.42(0.05-127.69) | 0.663 | ||
| 80–89 | 0.54(0.16–1.79) | 0.314 | 1.87(0.15–22.64) | 0.623 | 1.44(0.03–75.94) | 0.858 | ||
| 90–99 | 0.84(0.25–2.82) | 0.782 | 1.50(0.12–18.40) | 0.752 | 1.00(0.02–54.88) | > 0.999 | ||
| ≥ 100 | 1.00 | 1.00 | 1.00 | |||||
| Marital status | ||||||||
| Unmarried | 1.24(0.95–1.62) | 0.115 | 1.48(1.15–1.89) | 0.002 | 0.52(0.23–1.20) | 0.125 | ||
| Married | 0.86(0.80–0.93) | < 0.001 | 1.19(1.11–1.28) | < 0.001 | 0.97(0.84–1.11) | 0.650 | ||
| Divorced or widowed | 1.00 | 1.00 | 1.00 | |||||
| Category of residence | ||||||||
| Urban (city and town) | 0.72(0.68–0.77) | < 0.001 | 1.23(1.16–1.30) | < 0.001 | 1.26(1.12–1.42) | < 0.001 | ||
| Rural | 1.00 | 1.00 | 1.00 | |||||
| Economic status | ||||||||
| Rich | 0.80(0.71–0.91) | 0.001 | 1.12(1.00-1.26) | 0.052 | 1.06(0.85–1.32) | 0.621 | ||
| Fair | 0.80(0.73–0.87) | < 0.001 | 1.06(0.96–1.17) | 0.261 | 0.82(0.68–0.99) | 0.037 | ||
| Poor | 1.00 | 1.00 | 1.00 | |||||
| Living pattern | ||||||||
| Living with family members | 1.25(1.14–1.38) | < 0.001 | 1.00(0.91–1.09) | 0.988 | 1.16(0.97–1.38) | 0.115 | ||
| Living in an institution | 1.45(1.07–1.95) | 0.015 | 0.67(0.50–0.89) | 0.006 | 0.84(0.49–1.44) | 0.525 | ||
| Living alone | 1.00 | 1.00 | 1.00 | |||||
| Education level (years) | ||||||||
| 0 | 1.07(1.00-1.15) | 0.042 | 0.88(0.82–0.93) | < 0.001 | 0.92(0.82–1.05) | 0.216 | ||
| ≥ 1 | 1.00 | 1.00 | 1.00 | |||||
|
Numbers of chronic diseases |
||||||||
| 0 | 1.26(1.16–1.36) | < 0.001 | 0.47(0.43–0.50) | < 0.001 | 0.45(0.39–0.52) | < 0.001 | ||
| 1 | 1.28(1.18–1.38) | < 0.001 | 0.68(0.64–0.73) | < 0.001 | 0.64(0.56–0.73) | < 0.001 | ||
| ≥ 2 | 1.00 | 1.00 | 1.00 | |||||
| Smoking status | ||||||||
| Never | 0.55(0.48–0.63) | < 0.001 | 1.18(1.04–1.32) | 0.007 | 1.47(1.12–1.93) | 0.006 | ||
| Previous | 0.67(0.59–0.76) | < 0.001 | 1.11(0.99–1.23) | 0.064 | 1.12(0.86–1.47) | 0.400 | ||
| Current | 1.00 | 1.00 | 1.00 | |||||
| Alcohol intaking status | ||||||||
| Never | 1.27(1.13–1.44) | < 0.001 | 1.13(1.02–1.25) | 0.023 | 1.21(0.97–1.52) | 0.093 | ||
| Previous | 1.10(0.89–1.37) | 0.371 | 1.02(0.76–1.36) | 0.167 | 1.15(0.65–2.03) | 0.118 | ||
| Current | 1.00 | 1.00 | 1.00 | |||||
| Regular exercise | ||||||||
| Never | 1.08(1.00-1.16) | 0.041 | 0.87(0.82–0.92) | < 0.001 | 0.76(0.67–0.86) | < 0.001 | ||
| Previous | 1.18(1.05–1.33) | 0.005 | 0.78(0.69–0.88) | < 0.001 | 0.79(0.62–1.01) | 0.060 | ||
| Current | 1.00 | 1.00 | 1.00 | |||||
| Dietary diversity | ||||||||
| Poor | 1.35(1.22–1.48) | < 0.001 | 0.72(0.66–0.78) | < 0.001 | 0.70(0.59–0.83) | < 0.001 | ||
| Moderate | 1.16(1.06–1.26) | 0.001 | 0.86(0.80–0.91) | < 0.001 | 0.87(0.76–0.99) | 0.041 | ||
| Good | 1.00 | 1.00 | 1.00 | |||||
| Sleeping quality | ||||||||
| Good | 0.86(0.80–0.92) | < 0.001 | 1.24(1.17–1.32) | < 0.001 | 1.26(1.11–1.42) | < 0.001 | ||
| Poor | 1.00 | 1.00 | 1.00 | |||||
| Sleeping length | ||||||||
| < 5 h | 1.08(0.93–1.24) | 0.311 | 1.08(0.94–1.24) | 0.284 | 0.85(0.64–1.13) | 0.272 | ||
| 5–9 h | 1.00(0.91–1.09) | 0.944 | 0.96(0.89–1.04) | 0.327 | 0.91(0.77–1.07) | 0.260 | ||
| > 9 h | 1.00 | 1.00 | 1.00 | |||||
| Housework | ||||||||
| Almost everyday | 0.89(0.82–0.97) | 0.010 | 1.09(1.00-1.18) | 0.043 | 1.09(0.92–1.28) | 0.347 | ||
| Sometimes | 0.83(0.75–0.93) | 0.001 | 0.95(0.86–1.04) | 0.269 | 0.79(0.63–0.99) | 0.042 | ||
| Never | 1.00 | 1.00 | 1.00 | |||||
| Outdoor activities | ||||||||
| Almost everyday | 0.88(0.81–0.96) | 0.005 | 1.09(1.00-1.20) | 0.052 | 1.02(0.84–1.23) | 0.880 | ||
| Sometimes | 1.04(0.95–1.14) | 0.436 | 0.97(0.88–1.06) | 0.465 | 1.48(1.22–1.80) | < 0.001 | ||
| Never | 1.00 | 1.00 | 1.00 | |||||
| Functional disability | ||||||||
| No | 0.98(0.86–1.11) | 0.706 | 0.79(0.70–0.89) | < 0.001 | 0.58(0.47–0.71) | < 0.001 | ||
| Yes | 1.00 | 1.00 | 1.00 | |||||
| Self-reported quality of life | ||||||||
| Good | 0.70(0.61–0.80) | < 0.001 | 1.15(0.98–1.36) | 0.088 | 1.01(0.73–1.39) | 0.966 | ||
| Fair | 0.78(0.68–0.88) | < 0.001 | 0.90(0.77–1.06) | 0.201 | 0.91(0.66–1.24) | 0.538 | ||
| Poor | 1.00 | 1.00 | 1.00 | |||||
| Self-reported health | ||||||||
| Good | 0.57(0.51–0.62) | < 0.001 | 1.01(0.92–1.10) | 0.881 | 0.87(0.72–1.04) | 0.134 | ||
| Fair | 0.67(0.61–0.73) | < 0.001 | 0.96(0.88–1.05) | 0.353 | 1.01(0.85–1.19) | 0.951 | ||
| Poor | 1.00 | 1.00 | 1.00 | |||||
Notes: BMI, Body Mass Index; OR, odds ratio; CI, Confidence Interval
a Participates with normal weight as the reference group in the multinomial logistic regression model. In the multinomial logistic regression model, we included survey year, gender, age groups, marital status, residence, economic status, living pattern, education level, numbers of chronic diseases, smoking status, alcohol intaking status, regular exercise, dietary diversity, sleeping quality, sleeping length, housework, outdoor activities, functional disability, self-reported quality of life, self-reported health
Factors associated with overweight and obesity
Compared to female, male participants were less likely to be overweight or obese (OR = 0.88, 95% CI: 0.82–0.95; OR = 0.60, 95% CI: 0.51–0.70, as shown in Table 2). When comparing the dietary diversity scores and the ADL groups, the results showed that older adults with poor and medium scores (OR = 0.72, 95% CI: 0.66–0.78; OR = 0.86, 95% CI: 0.80–0.91) and those without any functional disability (OR = 0.79, 95% CI: 0.70–0.89) had a lower likelihood of being overweight or obese (poor dietary diversity scores: OR = 0.70, 95% CI: 0.59–0.83; medium dietary diversity scores: OR = 0.87, 95% CI: 0.76–0.99; Independent: OR = 0.58, 95% CI: 0.47–0.71) compared to counterparts, respectively. Compared with the divorced or widowed, the married and the unmarried were more likely to be overweight (OR = 1.19, 95% CI: 1.11–1.28; OR = 1.48, 95% CI: 1.15–1.89). The regression analysis also revealed that older adults living in urban areas (OR = 1.23, 95% CI: 1.16–1.30; OR = 1.26, 95% CI: 1.12–1.42) and with good sleep quality (OR = 1.24, 95% CI: 1.17–1.32; OR = 1.26, 95% CI: 1.11–1.42) had more chances of being overweight or obesity compared to counterparts respectively. The results were similar in the sensitive analysis (supplemental Tables 2–4).
Discussion
China has the highest number of older adults globally, with approximately 180 million individuals aged 65 years and older, a significant portion of whom suffer from one or more chronic diseases, accounting for 75% of this population [19]. Abnormal body weight is known to be associated with various chronic conditions, leading to significant national healthcare expenditures [20]. We found that obesity prevalence was increasing in all age groups and genders, regardless of geographical location, race or socioeconomic status and especially in the elderly, which was similar to the trends of obesity in other age groups [5, 20]. Our results also show that the prevalence of overweight and obesity increased along with year, which is consistent with other studies [5, 21]. Ampofo et al. [21] utilized prophet models and time-series data from the WHO Global Health Observatory data repository to forecast the prevalence of obesity in 185 countries. They found that obesity prevalence in China was predicted to be 12% in 2030, and called for more urgent attention and effective future interventions.
The obesity prevalence rate found in our study in 2018 (4.95%) was slightly higher than that reported in some Asian countries, such as 4.3% in Japan and 4.7% in Korea [22]. However, it was significantly lower than the rates reported in Western countries, such as 23.1% in the Russian Federation, 28.3% in Canada, 42.8% in the USA, 23.1% in Germany, 20.8% in France, and 20.9% in Spain [22–25]. In the China Chronic Disease and Risk Factors Surveillance program, the prevalence of obesity among adults aged 18–69 years was reported as 8.1%, which was higher than the findings in our study. This difference could be attributed to variations in the age groups targeted in the two national studies. Additionally, the rates of obesity varied widely across different regions and countries, likely influenced by environmental factors that promote obesity. Factors such as improved living conditions, which may lead to improved nutrition and increased calorie intake, the presence of chronic conditions like arthritis that can limit mobility, and the popularity of indoor recreational activities that reduce outdoor physical activities, among others, contribute to this variation [5, 26, 27]. In our results, the rates of overweight and obesity increase among older adults living in the urban areas, rich families, who never smoke or drink, suffering from more than 2 chronic diseases and older adults with good dietary diversity score compared to their counterparts respectively. Our result is consistent with the possible reasons proposed above. In the regression models, we found that adults with poor and medium dietary diversity scores and those without any functional disability had a lower likelihood of being overweight or obese compared to counterpart. Dietary and physical activity has been well-reported to be factors related with obesity. Interestingly, we found that older adults with good sleep quality had higher risk of being overweight and obese. One possible explanation is that older adults with good sleep quality might spend more time in bed and lead to reduced physical activity levels and lower energy expenditures, which might contribute to weight gain over time. Further research is needed to fully understand the mechanisms behind the association between sleep quality and the risk of overweight and obesity among older adults.
For the problem of obesity of the older adults, except for the possible macro sociological and demographic factors, the core biological factors are also significant for effective interventions. Many studies have demonstrated the age-related changes in metabolism and body composition and the presence of chronic disease that develop with the ageing process are the core biological mechanisms and targets [28–30]. In sum, the developing trend of abnormal body weight in older adults is a multifactorial problem with complex interactions among biological mechanisms, sociocultural, environmental factors. There is significant heterogeneity of phenotypes among overweight and obese individuals such as visceral or central obesity, peripheral obesity or metabolically healthy obesity [31]. It limited to classify abnormal body weight only based on BMI value, which may hinder the early identification of metabolic abnormalities. The European Association for obesity research (EASO) stressed that there need to be an improvement in the diagnostic criteria of obesity based on the etiology, degree and health risk [32]. Hopefully, there are more markers or indicators that could help in the subgroup’s classification such as VAT, WHtR and fat mass, or better detection technology for assessment of body composition like dual-energy X-ray [26, 33, 34]. Important progress has been made in identifying subtypes of obesity and what is important is to apply these advances to health management of the older adults.
Compared with most western countries faced with medical burden of obesity, many low-income and middle-income countries are now facing a double burden of disease on underweight, overweight and obesity, especially in Asian countries [35, 36]. Recent evidence has come to a new concept of “obesity paradox” based on the U- or J-shaped relationship between mortality and BMI, which means increased risk of excess mortality were observed in the underweight/normal weight population [37, 38]. Although there has been a slight decrease in the prevalence of underweight, it was estimated that 462 million adults are underweight in 2019[39]. Similarly, in our results, the prevalence rate of the underweight decreased with each passing year from 2008 to 2018 with lowest rate of 7.87% in 2018. Then a multinomial logistic regression model was further performed to explore the influencing factors associated with the underweight. The results show that older adults living in urban areas, married and those with good sleep quality had a lower chance of being underweight compared to counterparts, respectively. Based on our results and other studies, the reasons lying behind the facts can be summarized into two aspects: inadequate food supply and reduced intake [40]. Economic disadvantage, reduced capacity of purchase, psychosocial factors caused by widowhood, divorce, the loss of identity and loss of social roles can result in inadequate food supply [41]. And reduced intake can be result of dementia, polypharmacy, constipation, poor appetite or reduced masticatory efficiency caused by oral health problems [42]. Though being underweight increases the risk of death, dementia, fractures, insulin resistance and higher hospitalization or emergency room visits, less attention appears to be paid to the underweight compared with the overweight and obesity [43–46]. Thus, improvements are needed in public infrastructure and social support, and interventions on nutrition should be given to underweight older adults for healthy aging.
There are several limitations to this study. First, most information like living patterns, lifestyle habits and health status including sleeping quality etc. were collected through face-to-face questionnaire interviews, which may lead to biases in the process of data collection. Moreover, we did not calculate the weighted prevalence of overweight and obesity because of the unavailable survey weights. Second, though this study covered older adults in 22 of 31 provinces in mainland China, limiting the generalization of our results to the geographically or ethnically distinct groups or younger population. Third, based on the cross-sectional study design, our results could not infer the causal relationship between research factors and abnormal weight among older adults.
Conclusions
In conclusion, the prevalence of overweight/obesity was increasing while the prevalence of underweight and normal weight significantly decreased from 2008 to 2018 among older adults in China after adjustment for demographic confounding factors. This study provided basic information for understanding the changes in body weight and the risk factors of overweight/obesity and underweight in the elderly in China. Future research on abnormal body weight of the elderly in China should consider the use of better detection technology for assessment of body composition and the subgroups classification, fully considering the impact of psychosocial and socioeconomic factors. With the rapidly increasing aging population, the growing overweight/obese older population in China poses a huge challenge for chronic disease and our study directly support intervention policy planning and prevention to the preparation of an aging society.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the members of the CLHLS study group for data collection and all the participants.
Authors’ contributions
Conception and design: Liyuan Tao, Jue Liu; Administrative support: Jue Liu; Provision of study materials or patients: Dina Jiesisibieke, Yuting Feng, Zhu Liduzi Jiesisibieke; Collection and assembly of data: Yuting Feng; Data analysis and interpretation: Dina Jiesisibieke, Liyuan Tao, Zhu Liduzi Jiesisibieke; Manuscript writing: All authors; Final approval of manuscript: All authors.
Funding
This study was funded by the National Natural Science Foundation of China (82004210, 72122001), the National Key R&D Program of China (2018YFC1704400). No payment was received by any of the co-authors for the preparation of this article.
Data availability
The datasets generated and/or analysed during the current study are available in the https://opendata.pku.edu.cn/dataverse/CHADS;jsessionid=f69ff64e099fa5139e1708177eec.
Declarations
Ethics approval and consent to participate
Ethical approval for all the CHARLS waves was granted from the Institutional Review Board (IRB) of Peking University (IRB00001052-11015). Informed consent was obtained from all participants, including legal representatives of illiterate participants. All methods were performed in line with the relevant guidelines and regulations as stipulated in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jue Liu, Email: jueliu@bjmu.edu.cn.
Liyuan Tao, Email: tendytly@163.com.
References
- 1.Blüher M. Obesity: global epidemiology and pathogenesis. Nat reviews Endocrinol. 2019;15(5):288–98. doi: 10.1038/s41574-019-0176-8. [DOI] [PubMed] [Google Scholar]
- 2.Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metab Clin Exp. 2019;92:6–10. doi: 10.1016/j.metabol.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, Sherry B, et al. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42(6):563–70. doi: 10.1016/j.amepre.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 4.Janssen F, Bardoutsos A, Vidra N. Obesity prevalence in the long-term future in 18 european countries and in the USA. Obes Facts. 2020;13(5):514–27. doi: 10.1159/000511023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. The lancet Diabetes & endocrinology. 2021;9(6):373–92. doi: 10.1016/S2213-8587(21)00045-0. [DOI] [PubMed] [Google Scholar]
- 6.Mensink GB, Schienkiewitz A, Haftenberger M, Lampert T, Ziese T, Scheidt-Nave C. [Overweight and obesity in Germany: results of the german health interview and examination survey for adults (DEGS1)]. Bundesgesundheitsblatt, Gesundheitsforschung. Gesundheitsschutz. 2013;56(5–6):786–94. doi: 10.1007/s00103-012-1656-3. [DOI] [PubMed] [Google Scholar]
- 7.Hajek A, Lehnert T, Ernst A, Lange C, Wiese B, Prokein J, et al. Prevalence and determinants of overweight and obesity in old age in Germany. BMC Geriatr. 2015;15:83. doi: 10.1186/s12877-015-0081-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United Nations DoEaSA, Population Division. World Population Prospects: The 2019 Revision, Key Findings and Advance Table 2019.
- 9.Liu L. China Geriatric Health Research Report (2018) Beijing, China: Social Sciences Literature Press; 2019. [Google Scholar]
- 10.Wang L, Zhou B, Zhao Z, et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004-18. Lancet. 2021;398(10294):53–63. doi: 10.1016/S0140-6736(21)00798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang Y, Meng Y. Is China moving toward healthy aging? A Tracking Study based on 5 phases of CLHLS Data. Int J Environ Res Public Health. 2020;17(12). [DOI] [PMC free article] [PubMed]
- 12.Li T, Zhang Y, Wang J, et al. All-cause mortality risk associated with long-term exposure to ambient PM2.5 in China: a cohort study. Lancet Public Health. 2018;3(10):e470–7. doi: 10.1016/S2468-2667(18)30144-0. [DOI] [PubMed] [Google Scholar]
- 13.Ji JS, Zhu A, Bai C, Wu CD, Yan L, Tang S, et al. Residential greenness and mortality in oldest-old women and men in China: a longitudinal cohort study. Lancet Planet health. 2019;3(1):e17–e25. doi: 10.1016/S2542-5196(18)30264-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gao M, Kuang W, Qiu P, Wang H, Lv X, Yang M. The time trends of cognitive impairment incidence among older chinese people in the community: based on the CLHLS cohorts from 1998 to 2014. Age Ageing. 2017;46(5):787–93. doi: 10.1093/ageing/afx038. [DOI] [PubMed] [Google Scholar]
- 15.Du M, Tao L, Zhu L, Liu J. Association between biomass fuel use and the risk of cognitive impairment among older populations in China: a population-based cohort study. Environ Health. 2021;20(1):21. doi: 10.1186/s12940-021-00706-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Du M, Tao L, Liu M, Liu J. Tourism experiences and the lower risk of mortality in the chinese elderly: a national cohort study. BMC Public Health. 2021;21(1):996. doi: 10.1186/s12889-021-11099-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Du M, Liu M, Liu J. The association between sleep duration and risk of mortality in chinese older adults: a national cohort study. J Clin Sleep Med. 2021;17(9):1821–9. doi: 10.5664/jcsm.9278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tao LY, Xie Z, Tao H. Dietary diversity and all-cause mortality among chinese adults aged 65 or older: a community-based cohort study. Asia Pac J Clin Nutr. 2020;29(1):152–60. doi: 10.6133/apjcn.202003_29(1).0020. [DOI] [PubMed] [Google Scholar]
- 19.Chengfu LI, Liu H, Liang Y, Wang H, Qianhui LIJPJ. Study on International Comparison of Healthy Life Expectancy and Prediction of Healthy Life Expectancy in China. J Popul. 2018;40(1):5–17. [Google Scholar]
- 20.Hajek A, Brettschneider C, van der Leeden C, Lühmann D, Oey A, Wiese B, et al. Prevalence and factors associated with obesity among the oldest old. Arch Gerontol Geriatr. 2020;89:104069. doi: 10.1016/j.archger.2020.104069. [DOI] [PubMed] [Google Scholar]
- 21.Ampofo AG, Boateng EB. Beyond 2020: modelling obesity and diabetes prevalence. Diabetes Res Clin Pract. 2020;167:108362. doi: 10.1016/j.diabres.2020.108362. [DOI] [PubMed] [Google Scholar]
- 22.Prevalence of obesity. among adults, BMI > = 30 (age-standardized estimate) (%).
- 23.Statistics Canada. Tables 13-10-0096-20 Body mass index, overweight or obese, self-reported, adult, age groups (18 years and older).
- 24.Hales CMCM, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018.NCHS Data brief, no 360. Hyattsville, MD: National Center for Health Statistics; 2020. [PubMed] [Google Scholar]
- 25.Peralta M, Ramos M, Lipert A, Martins J, Marques A. Prevalence and trends of overweight and obesity in older adults from 10 european countries from 2005 to 2013. Scand J Public Health. 2018;46(5):522–9. doi: 10.1177/1403494818764810. [DOI] [PubMed] [Google Scholar]
- 26.Batsis JA, Villareal DT. Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nat reviews Endocrinol. 2018;14(9):513–37. doi: 10.1038/s41574-018-0062-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Popkin BM. Synthesis and implications: China’s nutrition transition in the context of changes across other low- and middle-income countries. Obes Rev. 2014;15(Suppl 1):60–7. doi: 10.1111/obr.12120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. 2013;14(8):542–59. doi: 10.1016/j.jamda.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 29.Abizanda P, Romero L, Sánchez-Jurado PM, Ruano TF, Ríos SS, Sánchez MF. Energetics of aging and Frailty: the FRADEA Study. The journals of gerontology Series A, Biological sciences and medical sciences. 2016;71(6):787–96. [DOI] [PMC free article] [PubMed]
- 30.Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376(3):254–66. doi: 10.1056/NEJMra1514009. [DOI] [PubMed] [Google Scholar]
- 31.Lee MJ, Wu Y, Fried SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Aspects Med. 2013;34(1):1–11. doi: 10.1016/j.mam.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hebebrand J, Holm JC, Woodward E, Baker JL, Blaak E, Durrer Schutz D, et al. A proposal of the European Association for the study of obesity to improve the ICD-11 diagnostic criteria for obesity based on the three Dimensions Etiology, Degree of Adiposity and Health Risk. Obes Facts. 2017;10(4):284–307. doi: 10.1159/000479208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mayoral LP, Andrade GM, Mayoral EP, Huerta TH, Canseco SP, Rodal Canales FJ, et al. Obesity subtypes, related biomarkers & heterogeneity. Indian J Med Res. 2020;151(1):11–21. doi: 10.4103/ijmr.IJMR_1768_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shah NR, Braverman ER. Measuring adiposity in patients: the utility of body mass index (BMI), percent body fat, and leptin. PLoS ONE. 2012;7(4):e33308. doi: 10.1371/journal.pone.0033308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. doi: 10.1016/S0140-6736(19)32497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395(10217):75–88. doi: 10.1016/S0140-6736(19)32472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lavie CJ, De Schutter A, Milani RV. Healthy obese versus unhealthy lean: the obesity paradox. Nat reviews Endocrinol. 2015;11(1):55–62. doi: 10.1038/nrendo.2014.165. [DOI] [PubMed] [Google Scholar]
- 38.Zhu Y, Wang Q, Pang G, Lin L, Origasa H, Wang Y, et al. Association between Body Mass Index and Health-Related Quality of Life: the “Obesity Paradox” in 21,218 adults of the Chinese General Population. PLoS ONE. 2015;10(6):e0130613. doi: 10.1371/journal.pone.0130613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization., Key facts about malnutrition. 2022.
- 40.Oliveira L, Poínhos R, Vaz Almeida MD. Relating food choice determinants with sociodemographic variables, health status and nutritional risk among community living older adults. Clin Nutr. 2022;51:397–403. doi: 10.1016/j.clnesp.2022.07.012. [DOI] [PubMed] [Google Scholar]
- 41.Stajkovic S, Aitken EM, Holroyd-Leduc J. Unintentional weight loss in older adults. Can Med Assoc J. 2011;183(4):443–9. doi: 10.1503/cmaj.101471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fávaro-Moreira NC, Krausch-Hofmann S, Matthys C, Vereecken C, Vanhauwaert E, Declercq A, et al. Risk factors for Malnutrition in older adults: a systematic review of the literature based on Longitudinal Data. Adv Nutr. 2016;7(3):507–22. doi: 10.3945/an.115.011254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Minagawa Y, Saito Y. The role of underweight in active life expectancy among older adults in Japan. The journals of gerontology Series B, psychological sciences and social sciences. 2021;76(4):756–65. [DOI] [PubMed]
- 44.Park D, Lee JH, Han S. Underweight: another risk factor for cardiovascular disease? A cross-sectional 2013 behavioral risk factor Surveillance System (BRFSS) study of 491,773 individuals in the USA. Medicine. 2017;96(48):e8769. doi: 10.1097/MD.0000000000008769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Takahashi PY, Sauver JL, Olson TC, Huber JM, Cha SS, Ebbert JO. Association between underweight and hospitalization, emergency room visits, and mortality among patients in community medical homes. Risk Manage Healthc policy. 2013;6:1–6. doi: 10.2147/RMHP.S39976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen C, Winterstein AG, Fillingim RB, Wei YJ. Body weight, frailty, and chronic pain in older adults: a cross-sectional study. BMC Geriatr. 2019;19(1):143. doi: 10.1186/s12877-019-1149-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analysed during the current study are available in the https://opendata.pku.edu.cn/dataverse/CHADS;jsessionid=f69ff64e099fa5139e1708177eec.