Abstract
Background
Family-centered care has evolved into patient and family-centered care. Although this is not a new concept; however, its application to nursing practice is very challenging among nurses due to its ambiguity.
Objective
This study aimed to clarify the concept of patient and family-centered care for children.
Methods
Walker and Avant’s concept analysis method was used. A literature search was also done using the following databases: Google Scholar, ProQuest, ScienceDirect, and Scopus, for articles published from 2011 to 2021.
Results
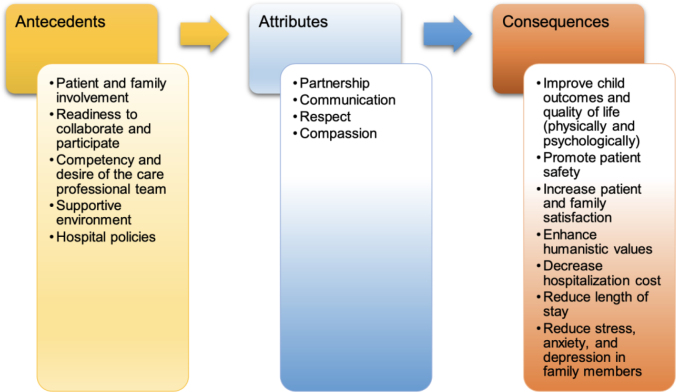
The defining attributes of patient and family-centered care are partnership, communication, respect, and compassion. Antecedents include patient and family involvement, readiness to collaborate and participate, competency and desire of the care professional team, supportive environment, and policies. Consequences of the patient and family-centered care include improved child outcomes and quality of life, promotion of patient safety, increased patient and family satisfaction, enhancement of humanistic values, reduction of hospitalization cost and length of stay, and decreased stress, anxiety, and depression in family members.
Conclusion
Four attributes of patient and family-centered care, its antecedents, and consequences may aid researchers in better understanding the concept and its application in nursing practice. This concept can also be used to establish quality care delivery strategies and promote professional relationships between nurses, patients, and families in clinical settings.
Keywords: children, concept analysis, family-centered care, patient-centered care, nurse
Background
One crucial aspect of the development in children’s healthcare in recent years has been the realization of the importance of patient and family involvement (National Association of Pediatric Nurse Practitioners, 2013). Patient and family-centered care (PFCC) integrates patient-centered and family-centered care in the healthcare system primarily to improve health outcomes (Committee on Hospital Care and Institute for Patient-and Family-Centered Care, 2012). Historically, PFCC was established in 1992 as an evolution from family-centered care (Rawson & Moretz, 2016). The concept of patient and family-centeredness is used to indicate the focus of care. Patient-centered care (PCC) is focused on the patient as an individual, whereas family-centered care (FCC) prioritizes the family as the child’s primary social support system (Coyne et al., 2018).
PFCC is defined as a way to design, implement, and assess health services based on commonly beneficial cooperation between patients, families, and healthcare professionals (Institute for Patient- and Family-Centered Care (IPFCC), 2017). PFCC practices encourage nurses to be active in involving children and their relatives in the care process, such as in terms of sharing information about parents’ experiences, participation in decision-making, and effective communication between them (Uhl et al., 2013). To effectively promote patient and family engagement in care, nurses can take the lead as one of the teams implementing patient and family-centered care (Grant & Johnson, 2019).
Several studies have found that PFCC is considered to enhance the quality of service for children, such as increasing patient and family satisfaction, improving physical and mental health, decreasing the length of stay and medical error, and reducing treatment costs (Clay & Parsh, 2016; Everhart et al., 2019; Hassanian et al., 2018). However, some obstacles are reportedly encountered in its implementation arising from the nurse healthcare professional such as the desire of the nurse to implement PFCC, knowledge possessed, and emotional support of nurses (Abraham & Moretz, 2012; Mulyaningsih et al., 2021). In addition, nurses find it challenging to comprehend how to involve patients’ relatives in the treatment process, it primarily due to competing ideas about their job as a nurse, such as the notions that nurses are professionals, that nurses have legal accountability to care for the children, and that nurses must first determine the competence of parents before allowing them to participate (Harrison, 2010). Besides, the nurse assumes that the presence of the family 24 hours a day is considered annoying and tiring, especially when the family asks many questions when providing nursing care (Coats et al., 2018).
One of the essential strategies for removing current obstacles is emphasizing leadership while developing a PFCC culture (Lloyd et al., 2018). Fostering knowledge of PFCC and its benefits is a crucial leadership role for facilitating nursing staff (Grant & Johnson, 2019). Understanding the PFCC framework in clinical nursing, including the basic concepts and its development, is necessary to provide for nurses through concept analysis. Previous studies have discussed the concept analysis of FCC and PCC in separate concepts. Most studies that identified the concept of FCC found that the family is the main focus of child care by advancing participation and collaboration with health professionals (Hutchfield, 1999; Mikkelsen & Frederiksen, 2011; Moradian, 2018; Smith, 2018). In contrast, PCC focus on the patient as the individual in care by encouraging caring, respect, and empowerment during the nursing process (Lusk & Fater, 2013; Morgan & Yoder, 2012).
PFCC is not a new concept in nursing, considering that FCC and PCC have been widely discussed through concept analysis. However, there are differences in both concepts, which lie in their conceptual focus and central characteristics (Coyne et al., 2018). When the two concepts are combined and applied in nursing care, this difference becomes a barrier for nurses due to the ambiguity in its concept and implementation (Prior & Campbell, 2018). Therefore, reviewing the PFCC through concept analysis is essential to promote clarity while providing mutual understanding within nursing.
Concept Analysis of PFCC
A concept analysis approach was used for assessing the PFCC concept in nursing and the healthcare system. Concepts provide the ability to classify, formulate, label, discuss and effect a phenomenon of interest in a particular discipline. The analysis is the initial step or a heuristic in helping the authors to employ the studies’ findings in various ways to aid future scientific and research endeavors (Rodgers et al., 2018). The authors used Walker and Avant’s concept analysis method (Walker & Avant, 2014), described as follows.
Selecting the Concept
The concept was chosen based on interest in a topic related to the discipline (Walker & Avant, 2014). In this article, the authors intend to analyze the concept of PFCC, particularly for children, based on a literature review. Compared to patient-centered care, which focuses more on the individual patient, family-centered care is more concerned with the family as a whole (Coyne et al., 2018). The significance of fostering children’s physical and psychosocial development and families’ contribution to improving their children's health and well-being have benefited from PFCC approaches in recent years (Deepika & Rahman, 2020). Pediatric nurses are expected to provide PFCC in health services because the presence of the relative has been found to help in a child’s healing process, even during the COVID-19 pandemic (Goldschmidt & Mele, 2021).
Determining All Uses of the Concept
A literature review was used to determine how this concept was being used. The concept was identified by a literature search on the databases: Google Scholar, ProQuest, ScienceDirect, and Scopus, published from 2011 to 2021. The authors also used the dictionary as a source of literature on this concept. The authors consider not limiting all use of concepts from various disciplines such as nursing, medicine, psychology, and others (Walker & Avant, 2014). The keywords used during the literature search were: (patient and family-centered care) AND (children OR pediatric). Based on the literature search, the identified concepts can be seen through definitions from several existing sources (Table 1).
Table 1.
Patient and family-centered care concept definitions
| Authors (Year) | Field | Definition |
|---|---|---|
| Institute for Patient- and Family-Centered Care (IPFCC) (2017) | Medicine | PFCC is defined as a way to design, implement and assess health services based on commonly useful cooperation between patient, family, and healthcare provider |
| Fernandes et al. (2021) | Nursing | An important element in improving the quality of nursing care because it can raise humanistic values such as empathy, partnership, respect, service, and communication between patients, families, and nurses while in childcare |
| Committee on Hospital Care and Institute for Patient-and Family-Centered Care (2012) | Medicine | A method for improving health outcomes by integrating patient-centered care and family-centered care throughout the health care system, whereby patients and families are partners in health care primarily in the provision of information for medical decision-making considerations |
| Park et al. (2018) | Nursing | A critical approach that positively impacts patients (increases knowledge, self-care behavioral, satisfaction, and reduces the length of stay) and families (increases satisfaction, reduces anxiety) by involving them in the health care system |
| DiGioia Iii and Greenhouse (2016) | Medicine | Treating patients and their families with care and respect, seeing them as partners and collaborators, and upholding their worth |
| Brown et al. (2015) | Medicine | A collaborative effort to improve healthcare quality, safety, and delivery by health professionals, patients, and their relatives in every healthcare system. Involving the patient and families in the health care system by appreciating the value and treating them with great affection |
| Grant and Johnson (2019) | Nursing | A useful approach for health workers, patients, and their families in planning, implementing and evaluating based on partnerships across all disciplines |
| Rawson and Moretz (2016) | Medicine | A method of providing treatment in which the patient’s family and healthcare professional work together |
| American College of Emergency Physicians (2019) | Medicine | A strategy used in the healthcare system that acknowledges the family’s crucial role and promotes collaboration between patients, families, and healthcare teams |
| Mitchell et al. (2016) | Medicine | A strategy to deliver comprehensive care that recognizes the patient as a member of the family and they are jointly involved in the health care |
| Abney-Roberts and Norman (2012) | Nursing | A concept that is familiar to most healthcare professionals and is essential in improving patient satisfaction, quality, and safety through the involvement of infants and their mothers during their inpatient stay |
| Dudley et al. (2015) | Medicine | A strategy for enhancing the health and well-being of children and their families through associations, collaborations, and communications that are advantageous for patients, families, and medical providers |
| Palokas et al. (2015) | Nursing | An approach that involves children and their families in the care process through a collaborative process, and effective communication among health workers, stakeholders, patients, and their families to promote service quality |
| Deepika and Rahman (2020) | Nursing | An effective strategy for raising awareness among patients, families, and health workers of the significance of children’s physical and psychosocial development and the part that families play in fostering their health and happiness. Respect for every child and family is one of the principles of the PFCC |
| Uhl et al. (2013) | Nursing | PFCC practices encourage nurses to play a proactive role in involving children and families in the care process, such as in terms of sharing information about parents’ experiences, participation in decision-making, and effective communication between parents and the team |
Determining the Defining Attributes
Walker and Avant state that attributes are established by attempting to demonstrate the attribute clusters most frequently connected to the concept and that permit a study of broader insights into the concept (Walker & Avant, 2014). At this step, the authors try to find the word that appears the most frequently among all the existing definitions. Further, the authors grouped the possible words with similar meanings into keyword clusters. Finally, the authors determine the name or attribute of the concept that represents each of the existing keyword clusters (Walker & Avant, 2014). From 15 sources of articles that were relevant to the patient and family-centered care, the authors obtained four key attributes: partnership, communication, respect, and compassion (Table 2).
Table 2.
Attributes of patient-and family-centered care
| Keyword Clusters | Sources | Attributes |
|---|---|---|
|
(Abney-Roberts & Norman, 2012; American College of Emergency Physicians, 2019; Committee on Hospital Care and Institute for Patient-and Family-Centered Care, 2012; DiGioia Iii & Greenhouse, 2016; Dudley et al., 2015; Fernandes et al., 2021; Grant & Johnson, 2019; Institute for Patient- and Family-Centered Care (IPFCC), 2017; Mitchell et al., 2016; Palokas et al., 2015; Park et al., 2018; Rawson & Moretz, 2016; Uhl et al., 2013) | Partnership |
|
(Committee on Hospital Care and Institute for Patient-and Family-Centered Care, 2012; Dudley et al., 2015; Fernandes et al., 2021; Palokas et al., 2015; Park et al., 2018; Uhl et al., 2013) | Communication |
|
(Brown et al., 2015; Deepika & Rahman, 2020; DiGioia Iii & Greenhouse, 2016; Fernandes et al., 2021) | Respect |
|
(Brown et al., 2015; Deepika & Rahman, 2020; DiGioia Iii & Greenhouse, 2016; Fernandes et al., 2021) | Compassion |
Partnership
In nursing, partnership means the ability to develop a relationship, coexist, and collaborate among patients, families, and nurses during healthcare delivery. The responsibility of nurses is to make sure that the child’s family can collaborate on a therapeutic plan (Kenyon & Barnett, 2001). Partnership in nursing refers to a relationship that consists of at least two people who work together to improve a patient’s health status, increase patient satisfaction, and a growing sense of well-being and sense of belonging by nurses (Jones et al., 2008).
Communication
Communication is exchanging knowledge, especially when doing so fosters understanding between individuals or organizations (Cambridge Dictionary, 2020a). Besides, the Merriam-Webster Dictionary (2022a) defines communication as transferring information between individuals using a shared set of gestures, symbols, or attitudes. In nursing practice, communication is a process that begins with establishing initial contact and lasts throughout the therapeutic relationship between nurses and patients (Kourkouta & Papathanasiou, 2014). During communication, nurses play a role in identifying patient needs, providing health information, providing comfort, and winning the patient’s trust (Fakhr-Movahedi et al., 2016). In hospitalized children, the family is an inseparable part of the child’s care, where the family is essential in providing support during the patient’s recovery and healing process. Communication establishes and maintains relationships between children and their families. Communication with children is conducted by listening, understanding, respecting, and offering them what they want and what their parents feel about them using appropriate vocabulary (Runcan et al., 2012).
Respect
Respect is paying close attention to anything or something in a situation. In addition, respect can also be interpreted as worthy of high regard (Merriam-Webster Dictionary, 2022b). In nursing, respect for people is characterized by attitudes, manners, and behaviors sensitive to each person’s dignity (Subramani & Biller-Andorno, 2022). Respect is a fundamental human right and morality based on human decency, worthiness, individuality, and self-determination. Respect is shown by unconditionally accepting, recognizing, and acknowledging the principles above in everyone as a guiding principle for behavior toward others (Browne, 1997).
Compassion
The definition of compassion is having empathy for the suffering or misfortune of others and a desire to assist them (Cambridge Dictionary, 2022b). Compassion refers to traits of warmth, goodness, and tenderness. Moreover, compassion is a trait that humans emerged for parenting and creating the ties of connection and cooperation necessary for group survival (Cole-King & Gilbert, 2011). Compassionate care is essential in providing nursing care that develops through experience and adaptation of existing nursing theories (Power, 2016). Compassionate care focuses on caring and providing care the way the person prefers. Nursing practice’s application of compassionate care entails negotiating the relationship between patients’ physical and emotional welfare to the nurses as the nursing care provider (Dewar et al., 2014).
Model Case
A girl, R, aged nine years, is a patient who confirmed positive for coronavirus and treated in the PICU room. Patient R underwent treatment due to respiratory distress. The nurse reported R’s progress on an ongoing basis to the physician and provided recommendations for what action could be taken next. As a result, physiotherapy and positioning intervention was implemented for R by involving family during practice by physiotherapist and nurse (partnership). Before the intervention, the nurse explained the aim of clinical procedures (communication) and allowed R’s parents to stay by her side during the process to reduce her fear (respect). Nurses interacted with children and their families during therapy with great warmth and promoted mutual caring (compassion).
Borderline Case
A boy, S, aged five years, was admitted to the pediatric ward with pneumonia. A nurse assessed S’s condition by touching him warmly and gently (compassion). S’s parents said their son had been coughing for three weeks and had started feeling short of breath one day ago (communication). The doctor examined S to confirm the assessment report obtained by the nurse. Next, the doctor and nurse provided joint planning for administering oxygen, nebulizer, and chest physiotherapy (partnership). Finally, the nurse explained the rationale behind the planned clinical procedure to R and his family.
Contrary Case
A 7-year-old boy, M, was being treated in the pediatric ward two days ago with a medical diagnosis of pneumonia. When the nurse conducted a respiratory check, the nurse asked M’s parents to stay away from the child to minimize distractions (no partnership). Next, the nurse gave oxygen insertion intervention to the patient, but suddenly the child looked scared and cried (no compassion). M’s mother asked the nurse what happened to her son and why no information was conveyed beforehand (no communication). However, the nurse did not respond to the parents’ questions and quickly left the room (no respect).
Antecedents
An antecedent is an event or set of related events that must occur or exist before an idea manifests (Walker & Avant, 2014). The antecedents of PFCC include patient and family involvement in the care process, patient and family readiness to collaborate and participate with caregivers, the competence of the care professional team and their desire to involve patients and their families in care, supportive environment, and hospital policies. Patient and family involvement includes aspects related to the presence, participation, needs, and advantages for the child and parents, their information needs, sense of responsibility and right to health, performance of care activities, and assistance given to health providers (Melo et al., 2014).
A professional team’s goal to support parents in healthcare contexts is based on the family’s involvement in their child’s long-term condition (Smith et al., 2015). However, involving patients’ families in the healthcare system might be difficult. The attitudes and behaviors of healthcare workers hinder parents’ engagement in inpatient child care (Power & Franck, 2008). Pediatric nurses in Jordan were found to have considerably more positive opinions toward dealing with children than with their parents (Razeq et al., 2021). Moreover, parents assumed that their engagement in pediatric care was influenced by the physical and cultural environment of the room (Hill et al., 2019). Hospital policies are thought to have an impact on how PFCC is implemented (Baird et al., 2015).
Consequences
Consequences are events or happenings that take place as a result of the concept’s manifestation (Walker & Avant, 2014). Several studies report that PFCC positively impacts patients and their families. The consequences of PFCC significantly improve child outcomes, including quality of life in the physical and psychological domains (Minooei et al., 2016), promote patient safety (Khan et al., 2018), and reduce the length of stay and hospitalization costs (Nurhaeni et al., 2018; Turchi et al., 2014). In addition, the impact of PFCC significantly increases family satisfaction (Hassanian et al., 2018; Rostami et al., 2015), promotes humanistic values (Fernandes et al., 2021), and reduces stress, anxiety, and depression in family members (Park et al., 2018). The consequences of implementing PFCC are illustrated in Figure 1.
Figure 1.
Antecedents, attributes, and consequences of PFCC
Empirical Referents
The selection of empirical referents is the last step in concept analysis. Empirical referents are a class for actual events whose presence serves as an example of the context in which the idea is used. Empirical referents are intended to measure attributes and are not tools to measure concepts (Walker & Avant, 2014). The use of attributes for the partnership can be found in the instrument of the Pediatric Nurse Parent Partnership Scale (PNPPS) (Choi & Uhm, 2022; Choi & Bang, 2013), the Partnership Self-Assessment Tool (PSAT) (Center for the Advancement of Collaborative Strategies in Health, 2022; Weiss et al., 2002), and the Family – Professional Partnership Scale (FPPS) (Summers et al., 2005). The attribute of communication is found on the Health Professionals Communication Skills Scale (HP-CSS) (Juliá-Sanchis et al., 2020; Leal-Costa et al., 2016) and Communication Skill Attitude Scale (Panczyk et al., 2019; Rees et al., 2002). Meanwhile, attribute for respect and compassion are found on the Scale of Perception of Respect for and Maintenance of the Dignity of the Inpatient (CUPDPH) (Campillo et al., 2020) and the Compassion Competence Scale (Lee & Seomun, 2016). PNPPS is an instrument that mostly reflects the attributes of PFCC. However, the attributes of respect and compassion in PNPPS have yet to be fully explored. Therefore, modifying existing instruments or developing new tools that comprehensively represent all attributes is recommended.
Implications to Nursing Knowledge and Practice
The analysis concept of PFCC has implications for nursing knowledge and clinical nursing practice, especially for children during hospitalization. This review has four attributes: partnership, communication, respect, and compassion. The implications for nursing knowledge, this attribute can be an essential element for nurses in developing a care delivery model. The development of this care delivery model focuses on improving the relationship between the nurse, child, and caregiver. Meanwhile, in clinical nursing, nurses can provide care for the parents to assist children’s effective coping and address their comprehensive psychological requirements (Handayani & Daulima, 2020). In addition, this analysis can increase awareness among nurses to promote compassion and mutual respect between children and their families while providing nursing care.
Conclusion
Partnership, Communication, Respect, and Compassion were identified as the four attributes of PFCC for children. This review found that the implementation of PFCC had a positive impact on children and their families during hospitalization. However, an understanding of the factors influencing this implementation is an aspect that needs to be considered by healthcare providers. Therefore, nurses as a team in implementing PFCC can play a role in supporting the involvement of children and their families in the nursing care process. These findings recommend modifying existing instruments or creating new tools that comprehensively represent all attributes.
Acknowledgment
The authors acknowledge Universitas Indonesia and Universitas Hasanuddin for their tremendous support during the study.
Declaration of Conflicting Interest
The authors have no conflict of interest regarding this article.
Funding
Educational Fund Management Institution (LPDP Scholarship) - Ministry of Finance, Republic of Indonesia. Recipient: First author.
Authors’ Contributions
All authors contributed equally to this study, and they read and approved the final manuscript and were accountable and entirely responsible for its content.
Authors’ Biographies
Tuti Seniwati, S.Kep.,Ns., M.Kes is a Pediatric Nursing Lecturer at the Department of Pediatric Nursing, Faculty of Nursing, Universitas Hasanuddin, Makassar, Indonesia. Currently, she is studying in the Doctoral Nursing Program at the Faculty of Nursing, Universitas Indonesia. Her research interests focus on children with critical care, children with emergency care, child developmental care, and disaster areas.
Prof. Yeni Rustina, S.Kp., M.App.Sc., Ph.D is a Professor at the Department of Pediatric Nursing, Faculty of Nursing, Universitas Indonesia. Her research interest focuses on the area of neonatology, particularly in the care of infants with low body weight.
Dr. Nani Nurhaeni, S.Kp., MN is an Associate Professor at the Department of Pediatric Nursing, Faculty of Nursing, Universitas Indonesia. Her research area in pediatrics includes infectious diseases, especially pneumonia, growth and development, family empowerment, stunting, and health promotion.
Dessie Wanda, S.Kp., M.N., Ph.D is an Associate Professor at the Department of Pediatric Nursing, Faculty of Nursing, Universitas Indonesia. Her research interests are in the area of pediatric nursing, clinical education, reflective practice, and qualitative research.
Ethical Consideration
Not applicable.
Data Availability
Not applicable.
References
- Abney-Roberts, S. E., & Norman, C. (2012). Patient family centered care: It's more than open visitation. Journal of Obstetric, Gynecologic & Neonatal Nursing, 41, S107. 10.1111/j.1552-6909.2012.01361_80.x [DOI] [Google Scholar]
- Abraham, M., & Moretz, J. G. (2012). Implementing patient-and family-centered care: Part I-understanding the challenges. Pediatric Nursing, 38(1), 44-47. [PubMed] [Google Scholar]
- American College of Emergency Physicians . (2019). Patient- and family-centered care and the role of the emergency physician providing care to a child in the emergency department. Annals of Emergency Medicine, 73(3), e29-e31. 10.1016/j.annemergmed.2018.11.006 [DOI] [PubMed] [Google Scholar]
- Baird, J., Davies, B., Hinds, P. S., Baggott, C., & Rehm, R. S. (2015). What impact do hospital and unit-based rules have upon patient and family-centered care in the pediatric intensive care unit? Journal of Pediatric Nursing, 30(1), 133-142. 10.1016/j.pedn.2014.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, S. M., Rozenblum, R., Aboumatar, H., Fagan, M. B., Milic, M., Lee, B. S., Turner, K., & Frosch, D. L. (2015). Defining patient and family engagement in the intensive care unit. American Journal of Respiratory and Critical Care Medicine, 191(3), 358-360. 10.1164/rccm.201410-1936LE [DOI] [PubMed] [Google Scholar]
- Browne, A. J. (1997). A concept analysis of respect applying the hybrid model in cross-cultural settings. Western Journal of Nursing Research, 19(6), 762-780. 10.1177/019394599701900605 [DOI] [Google Scholar]
- Cambridge Dictionary . (2020a). Meaning of communication. In https://dictionary.cambridge.org/dictionary/english/communication
- Cambridge Dictionary . (2022b). Meaning of compassionate. In https://dictionary.cambridge.org/dictionary/english/compassionate
- Campillo, B., Corbella, J., Gelpi, M., Martinez, E., Viciana, M. A., & Alonso, M. (2020). Development and validation of the scale of perception of respect for and maintenance of the dignity of the inpatient [CuPDPH]. Ethics, Medicine and Public Health, 15, 100553. 10.1016/j.jemep.2020.100553 [DOI] [Google Scholar]
- Center for the Advancement of Collaborative Strategies in Health . (2022). Partnership Self-Assessment Tool Questionnaire. https://atrium.lib.uoguelph.ca/xmlui/bitstream/handle/10214/3129/Partnership_Self-Assessment_Tool-Questionnaire_complete.pdf?sequence=1&isAllowed=y
- Choi, M.-Y., & Uhm, J.-Y. (2022). Factorial validity of the Pediatric Nurse Parent Partnership Scale—Pediatric Nurses (PNPPS-PN). Healthcare, 10, 991. 10.3390/healthcare10060991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, M. Y., & Bang, K.-S. (2013). Development and testing of a pediatric nurse parent partnership scale. Journal of Korean Academy of Nursing, 43(2), 194-202. 10.4040/jkan.2013.43.2.194 [DOI] [PubMed] [Google Scholar]
- Clay, A. M., & Parsh, B. (2016). Patient-and family-centered care: It’s not just for pediatrics anymore. AMA Journal of Ethics, 18(1), 40-44. 10.1001/journalofethics.2016.18.1.medu3-1601 [DOI] [PubMed] [Google Scholar]
- Coats, H., Bourget, E., Starks, H., Lindhorst, T., Saiki-Craighill, S., Curtis, J. R., Hays, R., & Doorenbos, A. (2018). Nurses’ reflections on benefits and challenges of implementing family-centered care in pediatric intensive care units. American Journal of Critical Care, 27(1), 52-58. 10.4037/ajcc2018353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole-King, A., & Gilbert, P. (2011). Compassionate care: The theory and the reality. Journal of Holistic Healthcare, 8(3), 29-37. [Google Scholar]
- Committee on Hospital Care and Institute for Patient-and Family-Centered Care . (2012). Patient-and family-centered care and the pediatrician's role. Pediatrics, 129(2), 394-404. 10.1542/peds.2011-3084 [DOI] [PubMed] [Google Scholar]
- Coyne, I., Holmström, I., & Söderbäck, M. (2018). Centeredness in healthcare: A concept synthesis of family-centered care, person-centered care and child-centered care. Journal of Pediatric Nursing, 42, 45-56. 10.1016/j.pedn.2018.07.001 [DOI] [PubMed] [Google Scholar]
- Deepika, S. R., & Rahman, J. (2020). Patient and family centered care: Practices in pediatrics. International Journal of Nursing Education, 12(4), 43-47. [Google Scholar]
- Dewar, B., Adamson, E., Smith, S., Surfleet, J., & King, L. (2014). Clarifying misconceptions about compassionate care. Journal of Advanced Nursing, 70(8), 1738-1747. 10.1111/jan.12322 [DOI] [PubMed] [Google Scholar]
- DiGioia Iii, A. M., & Greenhouse, P. K. (2016). Creating value with the patient-and family-centered care methodology and practice: What trainees need to know, why, and strategies for medical education. AMA Journal of Ethics, 18(1), 33-39. 10.1001/journalofethics.2017.18.1.medu2-1601 [DOI] [PubMed] [Google Scholar]
- Dudley, N., Ackerman, A., Brown, K. M., Snow, S. K., American Academy of Pediatrics Committee on Pediatric Emergency, M., American College of Emergency Physicians Pediatric Emergency Medicine, C., Emergency Nurses Association Pediatric, C., Shook, J. E., Chun, T. H., & Conners, G. P. (2015). Patient-and family-centered care of children in the emergency department. Pediatrics, 135(1), e255-e272. 10.1542/peds.2014-3424 [DOI] [PubMed] [Google Scholar]
- Everhart, J. L., Haskell, H., & Khan, A. (2019). Patient-and family-centered care: Leveraging best practices to improve the care of hospitalized children. Pediatric Clinics, 66(4), 775-789. 10.1016/j.pcl.2019.03.005 [DOI] [PubMed] [Google Scholar]
- Fakhr-Movahedi, A., Rahnavard, Z., Salsali, M., & Negarandeh, R. (2016). Exploring nurse’s communicative role in nurse-patient relations: A qualitative study. Journal of Caring Sciences, 5(4), 267-276. https://doi.org/10.15171%2Fjcs.2016.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes, A. K., Wilson, S., Nalin, A. P., Philip, A., Gruber, L., Kwizera, E., Sydelko, B. S., Forbis, S. G., & Lauden, S. (2021). Pediatric family-centered rounds and humanism: A systematic review and qualitative meta-analysis. Hospital Pediatrics, 11(6), 636-649. 10.1542/hpeds.2020-000240 [DOI] [PubMed] [Google Scholar]
- Goldschmidt, K., & Mele, C. (2021). Disruption of patient and family centered care through the COVID-19 pandemic. Journal of Pediatric Nursing, 58, 102-103. https://doi.org/10.1016%2Fj.pedn.2021.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, S. M., & Johnson, B. H. (2019). Advancing the practice of patient- and family-centered care: the central role of nursing leadership. Nurse Leader, 17(4), 325-330. 10.1016/j.mnl.2019.05.009 [DOI] [Google Scholar]
- Handayani, A., & Daulima, N. H. C. (2020). Parental presence in the implementation of atraumatic care during children’s hospitalization. Pediatric Reports, 12(S1), 8693. 10.4081/pr.2020.8693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison, T. M. (2010). Family-centered pediatric nursing care: State of the science. Journal of Pediatric Nursing, 25(5), 335-343. 10.1016/j.pedn.2009.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassanian, Z. M., Bahrami, F., Farhadian, M., & Khalili, A. (2018). Effect of participatory care on the satisfaction of parents of children admitted to the children's wards: Clinical trial study. National Journal of Physiology, Pharmacy and Pharmacology, 8(5), 664-670. 10.5455/njppp.2018.8.1247303012018 [DOI] [Google Scholar]
- Hill, C., Knafl, K. A., Docherty, S., & Santacroce, S. J. (2019). Parent perceptions of the impact of the Paediatric Intensive Care environment on delivery of family-centred care. Intensive and Critical Care Nursing, 50, 88-94. 10.1016/j.iccn.2018.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchfield, K. (1999). Family‐centred care: A concept analysis. Journal of Advanced Nursing, 29(5), 1178-1187. 10.1046/j.1365-2648.1999.00987.x [DOI] [PubMed] [Google Scholar]
- Institute for Patient- and Family-Centered Care (IPFCC) . (2017). Advancing the practice of patient- and family-centered care in hospitals - how to get started. https://www.ipfcc.org/resources/getting_started.pdf
- Jones, J., lowe, m., Burns, C., Donaldson, P., Abbey, J., & Abbey, B. (2008). Practice Partnership Model : An innovative approach for nursing at The Prince Charles Hospital. Brisbane: Queensland Health and Queensland University of Technology. 10.13140/RG.2.1.2179.6327 [DOI] [Google Scholar]
- Juliá-Sanchis, R., Cabañero-Martínez, M. J., Leal-Costa, C., Fernández-Alcántara, M., & Escribano, S. (2020). Psychometric properties of the health professionals communication skills scale in university students of health sciences. International Journal of Environmental Research and Public Health, 17(20), 7565. 10.3390/ijerph17207565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenyon, E., & Barnett, N. (2001). Partnership in nursing care (PINC): The Blackburn model. Journal of Child Health Care: for Professionals Working with Children in the Hospital and Community, 5(1), 35-38. 10.1177/136749350100500106 [DOI] [PubMed] [Google Scholar]
- Khan, A., Spector, N. D., Baird, J. D., Ashland, M., Starmer, A. J., Rosenbluth, G., Garcia, B. M., Litterer, K. P., Rogers, J. E., & Dalal, A. K. (2018). Patient safety after implementation of a coproduced family centered communication programme: Multicenter before and after intervention study. BMJ 363, k4764. 10.1136/bmj.k4764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kourkouta, L., & Papathanasiou, I. V. (2014). Communication in nursing practice. Materia Socio-Medica, 26(1), 65-67. https://doi.org/10.5455%2Fmsm.2014.26.65-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leal-Costa, C., Tirado-González, S., Rodríguez-Marín, J., & vander-Hofstadt-Román, C. J. (2016). Psychometric properties of the health professionals communication skills scale (HP-CSS). International Journal of Clinical and Health Psychology, 16(1), 76-86. 10.1016/j.ijchp.2015.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, Y., & Seomun, G. (2016). Development and validation of an instrument to measure nurses' compassion competence. Applied Nursing Research, 30, 76-82. 10.1016/j.apnr.2015.09.007 [DOI] [PubMed] [Google Scholar]
- Lloyd, B., Elkins, M., & Innes, L. (2018). Barriers and enablers of patient and family centred care in an Australian acute care hospital: Perspectives of health managers. Patient Experience Journal, 5(3), 55-64. 10.35680/2372-0247.1270 [DOI] [Google Scholar]
- Lusk, J. M., & Fater, K. (2013). A concept analysis of patient‐centered care. Nursing Forum, 48(2), 89-98. 10.1111/nuf.12019 [DOI] [PubMed] [Google Scholar]
- Melo, E. M. d. O. P. d., Ferreira, P. L., Lima, R. A. G. d., & Mello, D. F. d. (2014). The involvement of parents in the healthcare provided to hospitalzed children. Revista Latino-Americana de Enfermagem, 22, 432-439. 10.1590/0104-1169.3308.2434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merriam-Webster Dictionary . (2022a). Definition of communication. In https://www.merriam-webster.com/dictionary/communication
- Merriam-Webster Dictionary . (2022b). Definition of respect. In https://www.merriam-webster.com/dictionary/respect
- Mikkelsen, G., & Frederiksen, K. (2011). Family‐centred care of children in hospital–a concept analysis. Journal of Advanced Nursing, 67(5), 1152-1162. 10.1111/j.1365-2648.2010.05574.x [DOI] [PubMed] [Google Scholar]
- Minooei, M. S., Ghazavi, Z., Abdeyazdan, Z., Gheissari, A., & Hemati, Z. (2016). The effect of the family empowerment model on quality of life in children with chronic renal failure: Children’s and parents’ views. Nephro-Urology Monthly, 8(4), e36854. https://doi.org/10.5812%2Fnumonthly.36854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell, M. L., Coyer, F., Kean, S., Stone, R., Murfield, J., & Dwan, T. (2016). Patient, family-centred care interventions within the adult ICU setting: An integrative review. Australian Critical Care, 29(4), 179-193. 10.1016/j.aucc.2016.08.002 [DOI] [PubMed] [Google Scholar]
- Moradian, S. T. (2018). Family-centered care: An evolutionary concept analysis. International Journal of Medical Reviews, 5(2), 82-86. 10.29252/IJMR-050207 [DOI] [Google Scholar]
- Morgan, S., & Yoder, L. H. (2012). A concept analysis of person-centered care. Journal of Holistic Nursing, 30(1), 6-15. 10.1177/0898010111412189 [DOI] [PubMed] [Google Scholar]
- Mulyaningsih, N., Yuniar, I., & Setyaningsih, E. (2021). Gambaran tingkat pengetahuan dan pemberian dukungan emosional perawat di ruang instalasi rawat intensif (IRI) RSUD dr Soedirman Kebumen [Description of the level of knowledge and providing emotional support for nurses in the intensive care unit (IRI) RSUD dr Soedirman Kebumen]. Proceeding of The 13th University Research Colloquium 2021: Kesehatan dan MIPA, Central Java, Indonesia. [Google Scholar]
- National Association of Pediatric Nurse Practitioners . (2013). NAPNAP position statement on the role of pediatric nurse practitioners in quality improvement. Journal of Pediatric Health Care, 27(4), e43-e45. 10.1016/j.pedhc.2013.03.004 [DOI] [Google Scholar]
- Nurhaeni, N., Rustina, Y., Agustini, N., & Rosuliana, N. E. (2018). Impact of family empowerment model on satisfaction and children’s length of stay in hospital. Enfermería Clínica, 28, 36-40. 10.1016/S1130-8621(18)30033-0 [DOI] [Google Scholar]
- Palokas, J. M., Northington, L., Wilkerson, R. R., & Boss, B. J. (2015). An interactive evaluation of patient/family centered rounds on pediatric inpatient units. Journal of Pediatric Nursing, 30(4), e9-e15. 10.1016/j.pedn.2014.11.005 [DOI] [PubMed] [Google Scholar]
- Panczyk, M., Iwanow, L., Zarzeka, A., Jaworski, M., & Gotlib, J. (2019). Communication skills attitude scale: A translation and validation study in asample of registered nurses in Poland. BMJ Open, 9(5), e028691. 10.1136/bmjopen-2018-028691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, M., Lee, M., Jeong, H., Jeong, M., & Go, Y. (2018). Patient-and family-centered care interventions for improving the quality of health care: A review of systematic reviews. International Journal of Nursing Studies, 87, 69-83. 10.1016/j.ijnurstu.2018.07.006 [DOI] [PubMed] [Google Scholar]
- Power, L. (2016). Nursing theory and the delivery of compassionate care. Nursing Standard (Royal College of Nursing (Great Britain) : 1987), 30(24), 41-46. 10.7748/ns.30.24.41.s46 [DOI] [PubMed] [Google Scholar]
- Power, N., & Franck, L. (2008). Parent participation in the care of hospitalized children: A systematic review. Journal of Advanced Nursing, 62(6), 622-641. 10.1111/j.1365-2648.2008.04643.x [DOI] [PubMed] [Google Scholar]
- Prior, S. J., & Campbell, S. (2018). Patient and family involvement: A discussion of co-led redesign of healthcare services. Journal of Participatory Medicine, 10(1), e8957. 10.2196/jopm.8957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson, J. V., & Moretz, J. (2016). Patient-and family-centered care: A primer. Journal of the American College of Radiology, 13(12), 1544-1549. 10.1016/j.jacr.2016.09.003 [DOI] [PubMed] [Google Scholar]
- Razeq, N. M. A., Arabiat, D. H., & Shields, L. (2021). Nurses' perceptions and attitudes toward family-centered care in acute pediatric care settings in Jordan. Journal of Pediatric Nursing, 61, 207-212. 10.1016/j.pedn.2021.05.018 [DOI] [PubMed] [Google Scholar]
- Rees, C., Sheard, C., & Davies, S. (2002). The development of a scale to measure medical students' attitudes towards communication skills learning: The Communication Skills Attitude Scale (CSAS). Medical Education, 36(2), 141-147. 10.1046/j.1365-2923.2002.01072.x [DOI] [PubMed] [Google Scholar]
- Rodgers, B. L., Jacelon, C. S., & Knafl, K. A. (2018). Concept analysis and the advance of nursing knowledge: state of the science. Journal of Nursing Scholarship, 50(4), 451-459. 10.1111/jnu.12386 [DOI] [PubMed] [Google Scholar]
- Rostami, F., Hassan, S. T. S., Yaghmai, F., Ismaeil, S. B., & Suandi, T. B. (2015). Effects of family-centered care on the satisfaction of parents of children hospitalized in pediatric wards in a pediatric ward in Chaloos in 2012. Electronic Physician, 7(2), 1078-1084. https://doi.org/10.14661%2F2015.1078-1084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runcan, P. L., Constantineanu, C., Ielics, B., & Popa, D. (2012). The role of communication in the parent-child interaction. Procedia-Social and Behavioral Sciences, 46, 904-908. 10.1016/j.sbspro.2012.05.221 [DOI] [Google Scholar]
- Smith, J., Swallow, V., & Coyne, I. (2015). Involving parents in managing their child's long-term condition—a concept synthesis of family-centered care and partnership-in-care. Journal of Pediatric Nursing, 30(1), 143-159. 10.1016/j.pedn.2014.10.014 [DOI] [PubMed] [Google Scholar]
- Smith, W. (2018). Concept analysis of family-centered care of hospitalized pediatric patients. Journal of Pediatric Nursing, 42, 57-64. 10.1016/j.pedn.2018.06.014 [DOI] [PubMed] [Google Scholar]
- Subramani, S., & Biller-Andorno, N. (2022). Revisiting respect for persons: Conceptual analysis and implications for clinical practice. Medicine, Health Care and Philosophy, 25, 351-360. 10.1007/s11019-022-10079-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers, J. A., Hoffman, L., Marquis, J., Turnbull, A., Poston, D., & Nelson, L. L. (2005). Measuring the quality of family—professional partnerships in special education services. Exceptional Children, 72(1), 65-81. 10.1177/001440290507200104 [DOI] [Google Scholar]
- Turchi, R. M., Antonelli, R. C., Norwood, K. W., Adams, R. C., Brei, T. J., Burke, R. T., Davis, B. E., Friedman, S. L., Houtrow, A. J., & Kuo, D. Z. (2014). Patient-and family-centered care coordination: A framework for integrating care for children and youth across multiple systems. Pediatrics, 133(5), e1451-e1460. 10.1542/peds.2014-0318 [DOI] [PubMed] [Google Scholar]
- Uhl, T., Fisher, K., Docherty, S. L., & Brandon, D. H. (2013). Insights into patient and family‐centered care through the hospital experiences of parents. Journal of Obstetric, Gynecologic & Neonatal Nursing, 42(1), 121-131. 10.1111/1552-6909.12001 [DOI] [PubMed] [Google Scholar]
- Walker, L. O., & Avant, K. C. (2014). Strategies for theory construction in nursing (5th ed.). Upper Saddle River, NJ: Pearson/Prentice Hall. [Google Scholar]
- Weiss, E. S., Anderson, R. M., & Lasker, R. D. (2002). Making the most of collaboration: Exploring the relationship between partnership synergy and partnership functioning. Health Education & Behavior, 29(6), 683-698. 10.1177/109019802237938 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.