Abstract
BACKGROUND
Besides disease-modifying therapies, various pharmacologic agents are frequently prescribed to people with multiple sclerosis (MS) for symptom treatment and for comorbid conditions. The present study aims to investigate the types and frequencies of agents prescribed to people with MS in Greece using records from the nationwide digital prescription database.
METHODS
Prescription records for 21,218 people (65.9% women) with MS were included in the study. The criterion for study inclusion was a minimum of 3 months of continuous prescription of an agent. Identified treatments were further examined by age group.
RESULTS
Antispasticity agents (17.5%) and fampridine (14.5%) were the most regularly prescribed symptomatic medications. Antihypertensives (21.1%) and drugs for affective disorders, including antidepressants (36.1%) and anxiolytics (16.2%), were the most frequently prescribed medications for comorbid conditions. Antidepressants were prescribed at almost equally high rates among individuals older than 40 years. Hypertension was one of the leading comorbidities among the study sample, with rates rising significantly after age 40 years and plateauing after age 60 years. Polypharmacy was observed in 22.5% of the study sample, with a higher incidence among people with MS older than 60 years (46.98%).
CONCLUSIONS
Agents prescribed for the treatment of disease symptoms and other medical conditions are expected to positively affect quality of life in people with MS. However, polypharmacy seems to be particularly high, especially in the aged population. The potential implications of polypharmacy in the disease course should further be explored.
Keywords: pharmacoepidemiology, comorbidity, multiple sclerosis, olypharmacy, quality of life
Multiple sclerosis (MS) is a chronic demyelinating and neurodegenerative disease of the central nervous system. People with MS may experience periods of relapse and remission or a chronic progressive disease course. Currently, numerous disease-modifying therapies (DMTs) are available to reduce disease activity. Early initiation and adherence to therapy may be crucial for the achievement of relapse rate reduction and for the prevention of disability accumulation.1
Besides DMTs, various pharmacologic agents (PAs) are frequently prescribed to people with MS for symptomatic treatment of spasticity, fatigue, ophthalmologic complications, and sexual and bladder/bowel dysfunction, among other symptoms.2,3 Adequate treatment with PAs may lead to higher functionality, better working ability, and, consequently, a better quality of life.4
Beyond symptoms directly related to MS, typical comorbid conditions often diagnosed in people with MS include hyperlipidemia, hypertension, gastrointestinal disease, chronic lung disease, thyroid disease, obesity, and neuropsychiatric disorders.5 Comorbid conditions impact the disease course and affect treatment selection, adherence, and outcome. In this sense, several intertwined issues emerge concerning diagnostic delay, degree of disability progression, and additive effect on mortality.3–5 Early diagnosis of comorbid conditions in clinical practice is of paramount importance to prevent a negative effect on MS.5 Unfortunately, people with MS with comorbidities, as well as older patients with MS, are often excluded from clinical trials, making it difficult to study the impact of comorbid conditions on MS and the interactions between DMTs and other medications.6
Comorbidity and polypharmacy (defined as the use of ≥5 prescribed medications daily) pose major challenges to treating physicians by increasing the complexity of MS management.2,4 Despite the acknowledged benefit-to-risk equilibrium of individual treatments, polypharmacy is an independent risk factor closely associated with adverse drug reactions and contributes to an increased risk of nonadherence, hospitalization, and mortality, especially among older adults.4 Therefore, polypharmacy has developed into a major public health concern.4,7 It is estimated that adverse drug reactions are the cause of more than 10% of all hospital admissions among the elderly in the general population.7
Pharmacoepidemiological data regarding the prescribed PAs in people with MS are scarce. In the present study, we aim to investigate the types and frequencies of prescribed PAs and the extent of polypharmacy in people with MS in Greece by using records from the national digital prescription database.
METHODS
We previously analyzed anonymized data from a 2-year period from the nationwide digital prescription database and identified 21,218 patients with MS (13,994 or 65.9% females; mean age, 46.6 ± 13.5; range, 8–95).8 In this study, we further analyzed records regarding all prescribed PAs in the identified population. The inclusion criterion for PA identification was at least 3 months of continuous prescription of the agent. The analysis was performed on the basis of active substances to avoid disease coding misclassifications.9 The identified PAs were then classified into various categories according to the World Health Organization’s Anatomical Therapeutic Chemical classification system.10 Identified cases were further divided into 4 age groups (<18, 18–39, 40–60, >60 years), and the number as well as percentage of people with MS under treatment were calculated within each PA category. Finally, we calculated the extent of polypharmacy in each population.
This study was performed according to the ethical standards of the Helsinki Declaration and in accordance with national data protection legislation of Greece. The study received ethical approval from the Greek Ministry of Health. Informed consent of the participants was not required according to national legislation on data protection. We used the Strengthening the Reporting of Observational Studies in Epidemiology guidelines in reporting the findings of this study.
RESULTS
Overall, 15,520 people with MS (73.1%) were treated at least once with a DMT during this study period. The most frequently prescribed drugs for symptomatic treatment were antispasticity agents (n = 3721, 17.5%) and fampridine (n = 3092, 14.5%). Antihypertensives (n = 4483, 21.1%) and drugs for affective disorders such as antidepressants (n = 7660, 36.1%) and anxiolytics (n = 3444, 16.2%) were the most commonly prescribed PAs for comorbid conditions. Antiepileptic (n = 2936, 13.8%), antiulcer (n = 2919, 13.7%), and urinary antispasmodic (n = 2308, 10.9%) drugs were also frequently prescribed (TABLE; FIGURE S1, available online at IJMSC.org). As expected, except for DMTs, prescriptions of PAs in the group younger than 18 years were uncommon, whereas the percentage of people with MS under treatment in all other PA categories increased with age. Regarding prescriptions for comorbid conditions, 10,491 people with MS (49.4%) were not prescribed any PAs, 4455 (21.0%) were prescribed PAs for 1 category, 2949 (13.9%) were prescribed PAs for 2 categories, and 3323 (15.6%) were prescribed PAs for 3 or more categories. Polypharmacy was observed in 4775 people with MS (22.5%), with a higher incidence in those older than 60 years (n = 1644 of 3499, 46.98%) (FIGURE).
TABLE.
Number and Percentage of Each Age Group With Most Frequent Pharmacologic Agents
| Drug classification | Age group, No. (%) | ||||
|---|---|---|---|---|---|
|
| |||||
| <18 y (n = 133) | 18–39 y (n = 6342) | 40–60 y (n = 11,244) | >60 y (n = 3499) | Overall (N = 21,218) | |
| Disease-modifying therapies | 125 (94.0) | 5633 (88.8) | 8304 (73.8) | 1458 (41.7) | 15,520 (73.1) |
| Antidepressants | 6 (4.5) | 1095 (17.3) | 4748 (42.2) | 1811 (51.7) | 7660 (36.1) |
| Antihypertensives | 0 | 172 (2.7) | 2344 (20.8) | 1966 (56.2) | 4482 (21.1) |
| Antispasmodics | 2 (1.5) | 375 (5.9) | 2170 (19.3) | 1174 (33.5) | 3721 (17.5) |
| Anxiolytics/sedatives | 1 (0.7) | 471 (7.4) | 2058 (18.3) | 914 (26.1) | 3444 (16.2) |
| Fampridine | 0 | 386 (6.1) | 2008 (17.8) | 697 (19.9) | 3091 (14.6) |
| Antiepileptics | 6 (4.5) | 421 (6.6) | 1756 (15.6) | 753 (21.5) | 2936 (13.8) |
| Antiulcers | 22 (16.5) | 595 (9.4) | 1589 (14.1) | 713 (20.4) | 2919 (13.7) |
| Urinary antispasmodics | 0 | 317 (5.0) | 1448 (12.9) | 543 (15.5) | 2308 (10.9) |
| Painkillers | 2 (1.5) | 224 (3.5) | 1068 (9.5) | 525 (15.0) | 1819 (8.6) |
| Modafinil | 0 | 147 (2.3) | 671 (6.0) | 237 (6.8) | 1055 (5.0) |
| Antithyroids | 0 | 94 (1.5) | 458 (4.1) | 321 (9.2) | 873 (4.1) |
| Antilipidemics | 0 | 18 (0.3) | 464 (4.1) | 375 (10.7) | 857 (4.0) |
| Antiplatelets | 0 | 34 (0.5) | 385 (3.4) | 413 (11.8) | 832 (3.9) |
| Antipsychotics | 0 | 116 (1.8) | 442 (3.9) | 240 (6.8) | 798 (3.8) |
| Bronchodilators | 2 (1.5) | 79 (1.2) | 269 (2.4) | 188 (5.4) | 538 (2.5) |
| Antiosteoporotics | 0 | 42 (0.7) | 251 (2.2) | 161 (4.6) | 454 (2.1) |
| Anticoagulants | 1 (0.7) | 25 (0.4) | 186 (1.6) | 152 (4.3) | 364 (1.7) |
| Antidiabetics | 0 | 9 (0.1) | 170 (1.5) | 189 (5.4) | 368 (1.7) |
FIGURE.
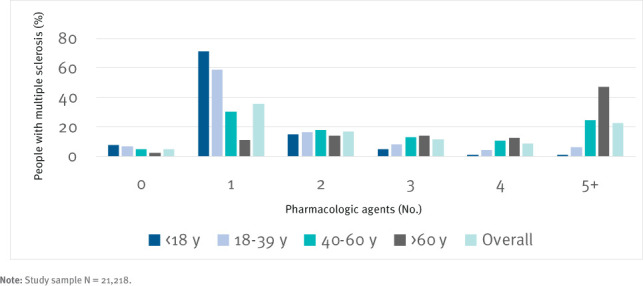
Number of Pharmacologic Agents by Study Participant Age
DISCUSSION
According to the current literature, the prevalence of comorbidities varies across different age groups. The prevalence of psychiatric comorbidities is almost equivalent across age groups, and the occurrence of physical comorbidities shows a relationship with age, with younger patients (aged 20–59 years) more frequently facing comorbid psychiatric manifestations (predominated by affective disorders) and older people with MS (aged >60 years) more often presenting with cardiovascular, neuropsychiatric, and metabolic disorders (hypertension, hyperlipidemia, depression, heart disease, and diabetes, in order of frequency).5 The findings of the present study are in line with these observations. Antidepressants were the most commonly prescribed medications in the entire sample (36.1%) and across the age groups up to 60 years; in the patients with MS older than 60 years, the most commonly prescribed treatments were antihypertensives (56.1%). Antidepressants were prescribed in almost equally high rates among participants older than 40 years (42%–52%). Data about the prevalence of mental disorders in the Greek general population are scarce. According to a 2021 study, 9.4% of Greek adults had a diagnosis of clinical depression, a trend in the general population with a recorded escalation from 3.3% in 2008 to 6.8% in 2009 and 8.2% in 2011.11 Therefore, rates of clinically significant mental comorbidity in MS seem to be much higher than in the general population in Greece.12
Vascular comorbidity, including hypertension, is strongly associated with a more rapid progression of disability in MS because cardiovascular risk factors and serum lipid profile changes are linked with an elevated lesion burden, advanced neurodegeneration, and more severe brain atrophy rates, especially if left untreated.13–15 According to this study, hypertension seems to be a leading comorbidity among people with MS in this sample (21.1%), with rates that escalate significantly after age 40 years and peak after age 60 years (56.1%). Similar results were seen by Marrie et al16 in a study of the age-specific prevalence of vascular comorbid conditions in adult Canadians with MS. Marrie et al estimated overall hypertension rates among people with MS to be 20.8% and among the general population to be 22.5% and generated comparative rates in the age groups of 20 to 44 years (people with MS, 7.71%; general population, 6.89%), 45 to 59 years (people with MS, 24.7%; general population, 24.7%), and older than 60 years (people with MS, 46.0%; general population, 55.5%). The same study estimated overall hyperlipidemia prevalence among people with MS to be 10.8% and among the general population to be 12.7%, and for those older than 60 years, hyperlipidemia was observed in 20.1% of those with MS and in 28.6% of the general population. Furthermore, diabetes rates among people with MS were found to be 7.62%, comparable with those among the general population (8.31%) and by age group.16 According to a 2020 study of cardiovascular risk factors among Greek adults, the prevalence of hypertension was estimated to be 39.2% (29.9% among those <70 years old); hyperlipidemia, 60.2%; and diabetes, 11.6%.17 However, an estimated 40% of the Greek population with hypertension may be untreated,18 and in the case of comorbidity with MS, this might be an additional challenge.
According to the findings of a 2016 nationwide study based on prescription data, the overall prevalence of medication-prescribed diabetes in the general Greek population was estimated to be 7.0%, ranging from 0.08% among minors to 8.2% among adults and 30.3% among individuals older than 75 years.18,19 The aforementioned data are useful to place the present data into order of magnitude, thus indicating that vascular risk factors among people with MS are slightly lower in overall prevalence compared with the general population, as also shown by Marrie et al,16 but still play a pivotal role in clinical outcome.
Spasticity affects 60% to 84% of people with MS, contributing to gait disturbances, falls, sleep disturbances, pain, and motor disability. Spasticity in MS is generally treated with a combination of medications, physical therapy, and exercise. According to previous studies, up to 78% of people with MS receive monotherapy for spasticity, and 46% receive combination therapy with 2 or more spasticity drugs.20–22 In the present study, the most frequently prescribed medications for symptomatic treatment were antispasticity agents (17.5%) and fampridine (14.5%), indicating that spasticity and gait disturbances are major complications of the disease.
Lower urinary tract dysfunction has been reported to occur in up to 90% of people with MS during the first 18 years after disease onset.23 The most often observed urologic complications are urgency, frequency, neurogenic detrusor overactivity (34%–99%), detrusor sphincter dyssynergia (43%), and atonic bladder (12%).24–26 The present study is in line with the previously mentioned data, with urinary antispasmodics used by 11% of the sample and increasing need for administration after age 40 years (12.8%–15.5%).
The prevalence of polypharmacy rises among older people with MS because the presentation and progression of overlapping chronic health conditions is associated with age.4 At the same time, an increase in the aging MS population has been noted worldwide because the life expectancy of people with MS has been prolonged.27 Furthermore, MS occurrence and diagnosis have also shifted older, therefore multiplying the risk of comorbidity and, consequently, polypharmacy.28,29 Depending on the study, an estimated 15% to 59% of hospital admissions of people with MS is attributed to polydrug reactions.7,30,31 Polypharmacy is significantly associated with comorbidity, increased disability, increased hospitalization rates, and lower quality of life.7 The risk of improper dosing and other forms of nonadherence may be especially magnified among people with MS who experience depression and cognitive decline.4 Conversely, polypharmacy itself is an additional stand-alone risk factor for functional (iatrogenic fatigue) and cognitive declines, which are common symptoms among people with MS regardless of age.32 Another practical issue imposed by polypharmacy in relation to the use of DMTs and especially among older people with MS is the fact that their use is associated with increased propensity for falls, compromised driving ability, increased traffic accidents, and mortality.33 The implications of polypharmacy are still an underresearched topic among people with MS. The present study findings highlight the issue of polypharmacy among people with MS older than 60 years. In this age group, rates of therapy administration of 5 or more PAs have doubled compared with the average of the entire sample and have quadrupled compared with the rates across all other categories of therapy administration of up to 4 PAs in the same age group.
CONCLUSIONS
The present study highlights the frequent concomitant use of various PAs in people with MS. Medications for comorbid affective disorders were the most frequently prescribed PAs up to age 60 years, subsequently reaching a plateau. Hypertensive agents emerged as a leading comorbidity among people with MS following a steady upward trend across all age categories, peaking after age 60 years, and surpassing rates for all other PAs. Furthermore, polypharmacy was detected in approximately one-fourth of the study sample, with incidence rising significantly in people with MS older than 60 years.
Although PAs prescribed for the treatment of other medical conditions and for MS-related symptoms are expected to positively affect quality of life and contribute to prolonged life expectancy, future studies should investigate potential drug-to-DMT interactions. In addition, as the MS population shifts toward older ages, the impact of polypharmacy on disease course should also be studied.
PRACTICE POINTS
Analysis of nationwide prescription data for people with multiple sclerosis living in Greece indicated emotional disorders as the most prevalent comorbidity up to age 60 years and hypertension as a leading comorbidity after age 60 years.
Polypharmacy may have a major effect on disease burden and quality of life due to the potential risk of pharmacologic interactions, particularly after age 60 years.
Supplementary Material
Funding Statement
FINANCIAL DISCLOSURES: Dr Bakirtzis has received travel support and/or research grants and/or lecture fees and/or advisory services from Wireless World Research Forum, the Hellenic Academy of Neuroimmunology, Novartis, Bayer, Merck, Genesis Pharma, Sanofi, Specifar, Roche, Biogen, Elpen, and Mylan. Dr Nikolaidis has received travel support and/or research grants and/or lecture fees and/or advisory services from the Hellenic Foundation for Research and Innovation, the Ministry of Education’s Education and Lifelong Learning Program, the Hellenic Neurological Society, the Hellenic Academy of Neuroimmunology, Biogen Idec, Novartis, Teva Pharmaceutical Industries, Bayer, Genesis Pharma, Sanofi, Specifar, Roche, Mylan, and Merck. Dr Boziki has received travel support and/or research grants and/or lecture fees and/or advisory services from the Hellenic Foundation for Research and Innovation, the Ministry of Education’s Education and Lifelong Learning Program, the Hellenic Neurological Society, the Hellenic Academy of Neuroimmunology, Biogen Idec,Novartis, Teva Pharmaceutical Industries, Bayer, Genesis Pharma, Sanofi, Specifar, Roche, and Merck. Dr Grigoriadis has received travel support and/or research grants and/or lecture fees and/or advisory services from Novartis, Bayer, Merck, Genesis, Sanofi, Specifar, Roche, Biogen, Teva Pharmaceutical Industries, and Mylan. FUNDING/SUPPORT: None.
Footnotes
The other authors declare no conflicts of interest.
PRIOR PRESENTATION: Parts of the study results were presented at the Sixth Middle East North Africa Committee for Research and Treatment in Multiple Sclerosis Congress; December 10 to 11, 2021; Dubai, United Arab Emirates.
REFERENCES
- 1.Burkhard A, Toliver J, Rascati K. Association between multiple sclerosis disease severity and adherence to disease-modifying therapies. J Manag Care Spec Pharm . 2021;27(7):915–923. doi: 10.18553/jmcp.2021.27.7.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Magyari M, Sorensen PS. Comorbidity in multiple sclerosis. Front Neurol . 2020;11:851. doi: 10.3389/fneur.2020.00851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bede P, Finegan E, Chipika RH et al. Occulomotor neural integrator dysfunction in multiple sclerosis: insights from neuroimaging. Front Neurol . 2018;9:691. doi: 10.3389/fneur.2018.00691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thelen J, Zvonarev V, Lam S, Burkhardt C, Lynch S, Bruce J. Polypharmacy in multiple sclerosis: current knowledge and future directions. Mo Med . 2021;118(3):239–245. [PMC free article] [PubMed] [Google Scholar]
- 5.Marrie RA. Comorbidity in multiple sclerosis: implications for patient care. Nat Rev Neurol . 2017;13(6):375–382. doi: 10.1038/nrneurol.2017.33. [DOI] [PubMed] [Google Scholar]
- 6.Marrie RA, Miller A, Sormani MP et al. The challenge of comorbidity in clinical trials for multiple sclerosis. Neurology . 2016;86(15):1437–1445. doi: 10.1212/WNL.0000000000002471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frahm N, Hecker M, Zettl UK. Polypharmacy among patients with multiple sclerosis: a qualitative systematic review. Expert Opin Drug Saf . 2020;19(2):139–145. doi: 10.1080/14740338.2020.1720646. [DOI] [PubMed] [Google Scholar]
- 8.Bakirtzis C, Grigoriadou E, Boziki MK et al. The administrative prevalence of multiple sclerosis in Greece on the basis of a nationwide prescription database. Front Neurol . 2020;11:1012. doi: 10.3389/fneur.2020.01012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Högg T, Zhao Y, Gustafson P et al. Adjusting for differential misclassification in matched case-control studies utilizing health administrative data. Stat Med . 2019;38(19):3669–3681. doi: 10.1002/sim.8203. [DOI] [PubMed] [Google Scholar]
- 10.ATC/DDD Index 2022. WHO Collaborating Centre for Drug Statistics Methodology. Last updated December 14, 2021. Accessed May 18, 2022. https://www.whocc.no/atc_ddd_index.
- 11.Michas G, Magriplis E, Micha R et al. Sociodemographic and lifestyle determinants of depressive symptoms in a nationally representative sample of Greek adults: the Hellenic National Nutrition and Health Survey (HNNHS) J Affect Disord . 2021;281:192–198. doi: 10.1016/j.jad.2020.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Skapinakis P, Bellos S, Koupidis S, Grammatikopoulos I, Theodorakis PN, Mavreas V. Prevalence and sociodemographic associations of common mental disorders in a nationally representative sample of the general population of Greece. BMC Psychiatry . 2013;13:163. doi: 10.1186/1471-244X-13-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kappus N, Weinstock-Guttman B, Hagemeier J et al. Cardiovascular risk factors are associated with increased lesion burden and brain atrophy in multiple sclerosis. J Neurol Neurosurg Psychiatry . 2016;87(2):181–187. doi: 10.1136/jnnp-2014-310051. [DOI] [PubMed] [Google Scholar]
- 14.Uher T, Fellows K, Horakova D et al. Serum lipid profile changes predict neurodegeneration in interferon-β1a-treated multiple sclerosis patients. J Lipid Res . 2017;58(2):403–411. doi: 10.1194/jlr.M072751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marrie RA, Rudick R, Horwitz R et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology . 2010;74(13):1041–1047. doi: 10.1212/WNL.0b013e3181d6b125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marrie RA, Yu BN, Leung S et al. Rising prevalence of vascular comorbidities in multiple sclerosis: validation of administrative definitions for diabetes, hypertension, and hyperlipidemia. Mult Scler . 2012;18(9):1310–1319. doi: 10.1177/1352458512437814. [DOI] [PubMed] [Google Scholar]
- 17.Touloumi G, Karakosta A, Kalpourtzi N et al. High prevalence of cardiovascular risk factors in adults living in Greece: the EMENO National Health Examination Survey. BMC Public Health . 2020;20(1):1665. doi: 10.1186/s12889-020-09757-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michas G, Karvelas G, Trikas A. Cardiovascular disease in Greece; the latest evidence on risk factors. Hellenic J Cardiol . 2019;60(5):271–275. doi: 10.1016/j.hjc.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Liatis S, Dafoulas GE, Kani C et al. The prevalence and treatment patterns of diabetes in the Greek population based on real-world data from the nation-wide prescription database. Diabetes Res Clin Pract . 2016;118:162–167. doi: 10.1016/j.diabres.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 20.Rizzo MA, Hadjimichael OC, Preiningerova J, Vollmer TL. Prevalence and treatment of spasticity reported by multiple sclerosis patients. Mult Scler . 2004;10(5):589–595. doi: 10.1191/1352458504ms1085oa. [DOI] [PubMed] [Google Scholar]
- 21.Haselkorn JK, Loomis S. Multiple sclerosis and spasticity. Phys Med Rehabil Clin N Am . 2005;16(2):467–481. doi: 10.1016/j.pmr.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 22.Sosnoff JJ, Gappmaier E, Frame A, Motl RW. Influence of spasticity on mobility and balance in persons with multiple sclerosis. J Neurol Phys Ther . 2011;35(3):129–132. doi: 10.1097/NPT.0b013e31822a8c40. [DOI] [PubMed] [Google Scholar]
- 23.Aharony SM, Lam O, Corcos J. Evaluation of lower urinary tract symptoms in multiple sclerosis patients: review of the literature and current guidelines. Can Urol Assoc J . 2017;11(1–2):61–64. doi: 10.5489/cuaj.4058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Sèze M, Ruffion A, Denys P, Joseph PA, Perrouin-Verbe B;, GENULF The neurogenic bladder in multiple sclerosis: review of the literature and proposal of management guidelines. Mult Scler . 2007;13(7):915–928. doi: 10.1177/1352458506075651. [DOI] [PubMed] [Google Scholar]
- 25.Phé V, Chartier-Kastler E, Panicker JN. Management of neurogenic bladder in patients with multiple sclerosis. Nat Rev Urol . 2016;13(5):275–288. doi: 10.1038/nrurol.2016.53. [DOI] [PubMed] [Google Scholar]
- 26.Wein AJ, Dmochowski RR. Neuromuscular dysfunction of the lower urinary tract. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. CampbellWalsh Urology . 11th ed. Elsevier Mosby; 2016. pp. 1761–1795. [Google Scholar]
- 27.Sanai SA, Saini V, Benedict RH et al. Aging and multiple sclerosis. Mult Scler . 2016;22(6):717–725. doi: 10.1177/1352458516634871. [DOI] [PubMed] [Google Scholar]
- 28.Louapre C, Papeix C, Lubetzki C, Maillart E. Multiple sclerosis and aging. Geriatr Psychol Neuropsychiatr Vieil . 2017;15(4):402–408. doi: 10.1684/pnv.2017.0685. [DOI] [PubMed] [Google Scholar]
- 29.Prosperini L, Lucchini M, Ruggieri S et al. Shift of multiple sclerosis onset towards older age. J Neurol Neurosurg Psychiatry . 2022 doi: 10.1136/jnnp-2022-329049. jnnp-2022-329049. [DOI] [PubMed] [Google Scholar]
- 30.Beiske GA, Holmøy T, Beiske AG, Johannessen SI, Johannessen Landmark C. Antiepileptic and antidepressive polypharmacy in patients with multiple sclerosis. Mult Scler Int . 2015;2015:317859. doi: 10.1155/2015/317859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jelinek GA, Weiland TJ, Hadgkiss EJ, Marck CH, Pereira N, van der Meer DM. Medication use in a large international sample of people with multiple sclerosis: associations with quality of life, relapse rate and disability. Neurol Res . 2015;37(8):662–673. doi: 10.1179/1743132815Y.0000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thelen JM, Lynch SG, Bruce AS, Hancock LM, Bruce JM. Polypharmacy in multiple sclerosis: relationship with fatigue, perceived cognition, and objective cognitive performance. J Psychosom Res . 2014;76(5):400–404. doi: 10.1016/j.jpsychores.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 33.Marrie RA, Fisk JD, Walld R et al. Use of benzodiazepines and Z-drugs in multiple sclerosis. Front Neurol . 2022;13:874724. doi: 10.3389/fneur.2022.874724. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


