Abstract
Childhood obesity is a public health problem globally as well as in Poland. This paper aimed to provide age- and sex-specific waist circumference, hip circumference, waist-to-height ratio and waist-to-hip ratio normative values for Polish children and adolescents aged 3 − 18 years for more precise monitoring of abdominal fat accumulation. The waist circumference, hip circumference, waist-to-height ratio and waist-to-hip ratio references were constructed with the lambda-mu-sigma (LMS) method using data from two nationally representative health surveys: the OLA study and the OLAF study, the largest available paediatric surveys in Poland which provided measured height, weight, waist, hip and blood pressure for 22,370 children and adolescents aged 3 − 18 years. The predictive ability of newly established references for overweight/obesity as defined by the International Obesity Task Force criteria and elevated blood pressure was tested with receiver operating characteristic. Abdominal obesity cut-offs linked to adult cardiometabolic cut-offs were established. Reference values for waist circumference, hip circumference, waist-to-height ratio and waist-to-hip ratio are presented, as well as waist circumference, waist-to-height ratio and waist-to-hip ratio cut-off values linked to adult’s cut-offs of cardiometabolic risk. The predictive value for overweight and obesity of population-based waist, hip and waist-to-height ratio references was outstanding–area under the receiver operating characteristic curve > 0.95 in both sexes, whereas with regard to the elevated blood pressure predictive ability was low—area under the receiver operating characteristic curve < 0.65.
Conclusion: This paper presents the first waist, hip, waist-to-height ratio and waist-to-hip ratio references for Polish children and adolescents aged 3–18 years. The 90th and 95th percentile and cut-offs linked to adult thresholds for cardiometabolic risk are proposed as cut-offs for abdominal obesity.
|
What is Known: • Waist circumference, waist-to-height ratio and waist-to-hip ratio are used to assess abdominal obesity in children and adults. • In Poland, there is no abdominal obesity and hip circumference references for children and adolescents from 3 to 18 years of age. | |
|
What is New: • Population-based references of central obesity indices and hip references for children and youth aged 3–18 years and cardiometabolic risk thresholds for children and adolescents linked to adult’s cut-offs were established. |
Supplementary Information
The online version contains supplementary material available at 10.1007/s00431-023-05001-4.
Keywords: Abdominal obesity, References, Children, Poland, Waist circumference, Hip circumference
Introduction
The prevalence of childhood overweight (OW) and obesity (OB) has increased worldwide from 1975 to 2015 [1]. In a large Pan-European cohort of preschool children, the prevalence of OW and OB ranged from 10 to 21% [2], whereas among European adolescent boys, it reached 22 to 27% [3]. In Poland, the prevalence of OW, including OB, reached 30% among primary school boys [4]. Although body mass index (BMI) is a widely accepted measure of general adiposity in children [5], it is not a marker of body fat distribution. In adults and children, cardiovascular risk factors are related to central obesity [6–12]. The measurement of waist circumference (WC) is a simple method to assess abdominal adiposity [13]. In children and adolescents WC, compared to BMI, had a stronger positive correlation with systolic and diastolic blood pressure [14] and was a better predictor of plasma triglyceride alterations and high insulin levels [15]. Moreover, a decrease in WC was the main predictor of regression of left ventricular hypertrophy and subclinical arterial injury in hypertensive children [16]. Although waist circumference reference percentiles are available in many countries [17–19], only a few cover the age range from preschool to adolescence [20–22]. Waist-to-height ratio (WHtR), as a measure of central obesity, is also useful in predicting cardiovascular risk factors in both children and adults [11, 23]. Age-related cut-offs are required for the anthropometric traits which change with age. Similar to adults, WHtR cut-off of 0.5 was proposed for children [10, 24] but according to others [25, 26], age-specific WHtR cut-offs are required. The WHtR cut-offs for children may potentially be established by linking adult’s cut-off at age of 18 years with younger ages providing a broad age range in the sample. The waist-to-hip ratio (WHR) cut-offs have been used especially in adults, to define the distribution of body fat as “pear shape” or “apple shape” [27]. The reference systems of WHR for children have been established in a few countries [28–30] and enable assessing abdominal and hip fat distribution [31]. Research conducted by Gillum showed that WHR was positively associated with the ratio of total serum cholesterol to high-density lipoprotein (HDL) cholesterol in pre- and post-pubertal girls [32]. In 2020, international waist circumference percentile cut-offs for central obesity in children were published [33]. However, results of studies comparing different normative values across populations indicate a better discriminatory ability of national over international references [34, 35].
This study aimed to establish age- and sex-specific normative values of waist circumference, hip circumference (HC), WHtR and WHR for Polish children and adolescents aged 3–18 years. It also assessed the discriminatory power of each of the indices of central obesity as predictors of overweight, obesity and elevated blood pressure.
Subjects and methods
The analysis was carried out using data from two nationally representative health surveys—the OLA study and the OLAF study—the largest available paediatric surveys in Poland which measured height, weight, waist circumference, hip circumference and blood pressure (BP) for 22,370 children and adolescents aged 2.5 − 18.5 years (11,611 girls and 10,759 boys) [14, 36–38]. In the case of the OLAF study (PL0080), field examinations of school-aged children and adolescents were conducted in 416 schools between November 2007 and November 2009. In the case of the OLA study (N R13 0002 06), field examinations of preschool children were conducted in 81 family medicine outpatient clinics between November 2010 and May 2012. Informed consent in writing was obtained from a parent of each participating child under 18 years of age, and, in addition, written consent was also obtained from all subjects over 16 years of age. Approvals to conduct both studies were granted by the Children’s Memorial Health Institute Ethics Committee before the studies commenced (approval number: 104/KBE/2007 date: 2007-10-10 and 177/KBE/2008 date 2008-10-12).
Sampling
Study participants were randomly selected using two-stage sampling. Primary sampling units—family medicine outpatient clinics, in the case of the OLA study, and schools, in the case of the OLAF study—were sampled from a list of family medicine outpatient clinics and an all-schools-in-Poland sampling frame provided by the Regional Offices of the National Health Fund and the Polish Ministry of Education, respectively. Sampling was stratified by province (in Polish: voivodeship). In the second stage, all children in the required age range within the sampled family medicine outpatient clinics and sampled schools comprised the sampling frame. The inclusion criteria for the study were signed informed consent and age in the range from 2.5 to 18.5 years. The exclusion criterion was pregnancy and in the case of blood pressure analysis, exclusion criteria included diseases that influence BP (for example congenital heart defects, renal disease, history of hypertension) or treatment with medication that influence BP (antihypertensive, antiarrhythmic, systemic steroids).
Measurements
All measurements were performed by trained staff according to the standard protocol. Height, weight and blood pressure measurement techniques have been described in detail elsewhere [14, 36–38]. Briefly, height and weight were recorded in duplicate. Height was measured using a SECA 214 stadiometer (Seca GmbH & Co. KG, Hamburg, Germany), with the subject in the standing upright position (no shoes), with hips and shoulders perpendicular to the central axis, heels against the footboard, knees together, arms hanging loosely at the sides and the head in the Frankfurt plane. Height was recorded to the nearest millimetre, if a difference between measurements exceeded 4 mm, a third measurement was taken, and the two closest measurements were averaged. Body weight was measured in light underwear to the nearest 0.05 kg, using a digital medical scale (Radwag WPT 100/200, Poland). In the case of a difference between measurements of 0.3 kg or more, a third measurement was taken, and the two closest measurements were averaged. BP was measured using a Datascope Accutor Plus (Datascope Corp., Fairfield, New Jersey, USA), an automated oscillometric device. The appropriate cuff size (bladder width at least 40% of arm circumference and length 80–100% of arm circumference) was determined by measuring the mid-upper arm circumference; four cuff sizes were available (child cuff, small adult cuff, adult cuff and large adult cuff). BP was measured in triplicate at 1- to 2-min intervals after a 5–10 min rest in the sitting position with the arm and back supported, cuff at the level of the heart, feet on the floor and legs uncrossed. The mean of the second and third measurements was used for analysis [14, 38–40]. Waist and hip circumferences were measured in duplicate using a non-stretch anthropometric tape which was applied horizontally with subjects in a standing position. Waist circumference was measured over the naked skin, at the minimum circumference midway between the lowest rib and the iliac crest, at the end of normal expiration. HC was measured at the maximum protuberance of the buttocks. Readings were recorded to the nearest millimetre. If a difference between the two measurements exceeded 3 cm, a third measurement was taken, and the two closest measurements were averaged. There were 247 subjects with missing or invalid data, and data from these subjects were excluded from the analysis.
Statistical analyses
BMI was calculated as body weight divided by height in meters squared (kg/m2). WHR and WHtR were calculated as WC (cm) divided by HC (cm) and height (cm), respectively. References for waist and hip circumference, WHR and WHtR were constructed separately for each sex using the lambda-mu-sigma (LMS) method [41] and LMSChartMaker Pro version 2.42 software [42]. Based on the criteria < −4 standard deviation (SD) and > +4 SD from the median, nineteen waist or hip outliers (0.08% of the sample) were excluded from the analysis. A Box-Cox power transformation was used to normalise the data at each age. Natural cubic splines with knots at each distinct age t were fitted by maximum penalised likelihood to obtain three smooth curves: L(t) the Box-Cox power, M(t) the median and S(t) the coefficient of variation.
The LMS parameters as defined by the International Obesity Task Force (IOTF) were used to calculate BMI standard deviation score (SDS), and IOTF BMI SDS cut-offs were applied to classify children and adolescents as OW and OB [43]. In this study, OW includes OB. Elevated BP was defined as systolic blood pressure (SBP) or diastolic blood pressure (DBP) ≥ 95 percentile according to the national references [14, 38]. Using the obtained LMS parameters of the constructed references, waist and hip circumferences, WHR and WHtR measurements were converted to standard deviation scores (SDS). The difference between boys and girls in terms of waist and hip circumferences, WHtR and WHR was analysed with the Mann–Whitney test. The relation between waist circumference-SDS, hip circumference-SDS, WHtR-SDS, WHR-SDS, overweight, obesity and elevated blood pressure was investigated with receiver operating characteristic (ROC) analysis. The discriminating power of the WC-, HC-, WHtR- and the WHR-SDS to detect excessive body weight and elevated BP were expressed as the area under the curve (AUC). The Youden’s index was calculated to find the best cut-off points. Areas under the ROC curves were compared using DeLong’s test [44]. The cut-offs for abdominal obesity indices (WC, WHtR and WHR) were established by linking percentile curves with adult cut-off points at age 18 years, using the method described by Cole and Lobstein [43]. This approach, that paediatric percentiles identified in late adolescence (18 years of age) by adult WC, WHtR and WHR cut-offs, should constitute the cut-off points for the identification of childhood central obesity, is per analogy to the approach to adult BMI cut-off for establishing childhood BMI cut-offs [45]. The following adult cut-offs were applied in this study: for waist circumference, 94 cm in the case of males and 80 cm in the case of females, for WHR, 0.90 for males and 0.85 for females [46], and for WHtR, 0.5 for both sexes [23]. Finally, study participants were grouped according to their abdominal obesity status: with and without abdominal obesity, and, with the use of Student’s t-test, systolic and diastolic blood pressure z-scores were compared between groups. A multiple logistic regression model was used to investigate the association between the elevated blood pressure and abdominal obesity category with adjustments for age and sex. Statistical analyses, apart from fitting LMS percentiles models, were performed using SAS 9.4 software (SAS Institute Inc., Cary, NC) and Statistica 13.3 TIBCO Software Inc. P value of < 0.05 was considered statistically significant.
Results
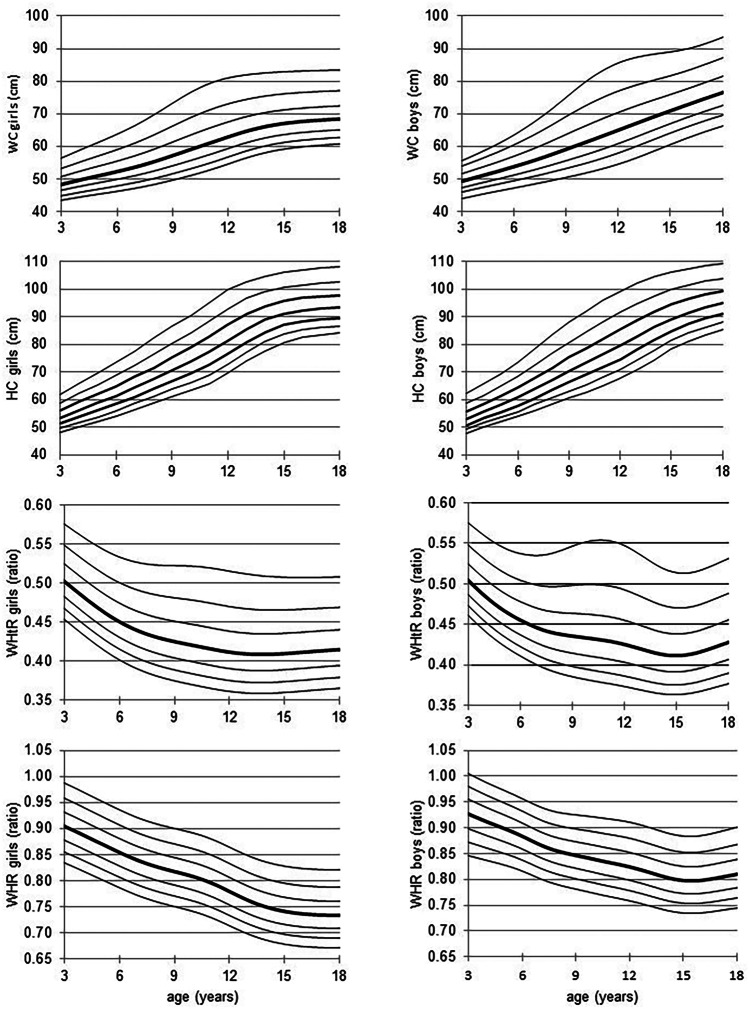
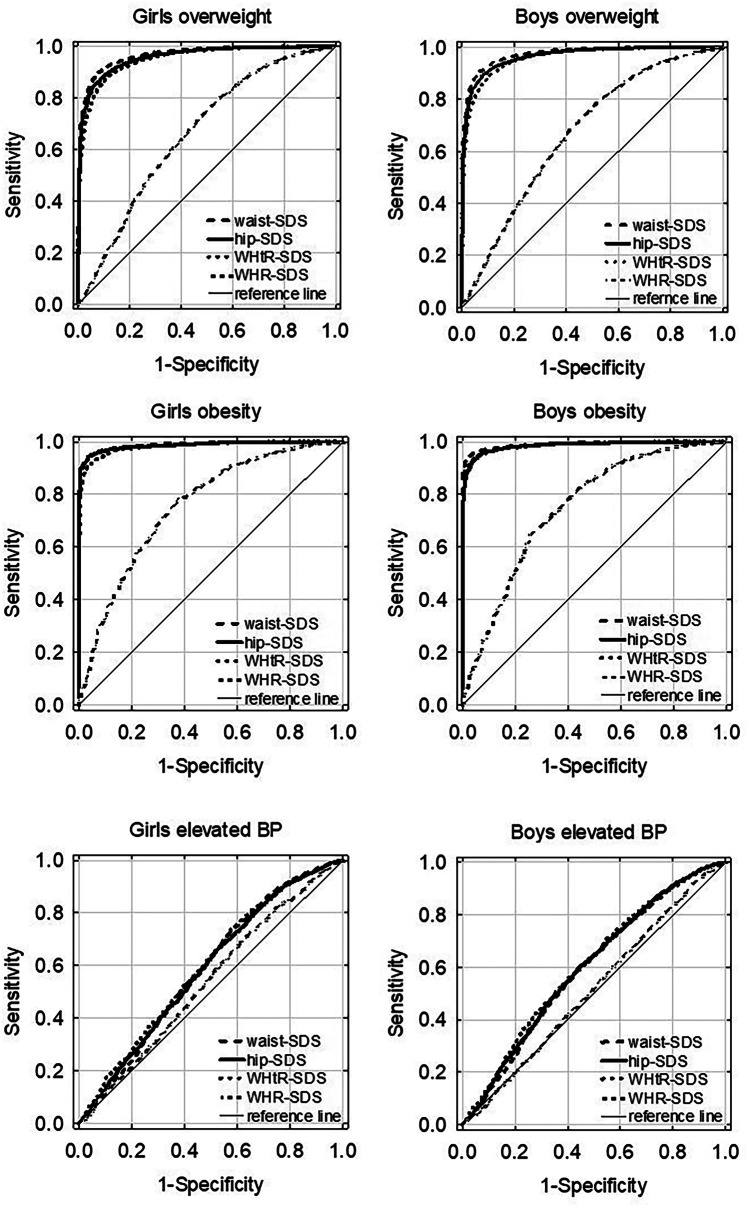
The values of waist and hip circumference increased with age (Fig. 1). The median WC was higher in boys than in girls (p < 0.05) and the difference increased with age up to 8 cm at the age of 18 years (Table 1). The adult abdominal obesity cut-off, WC of 80 cm in the case of females and 94 cm in the case of males [46, 47], at the age of 18 years was z-score + 1.57 (corresponding to the 94th percentile) and z-score + 1.85 (corresponding to the 97th percentile), for girls and boys, respectively. The median hip circumference for the age from 3 to 16 years was higher in girls compared to boys. The difference was statistically significant from 11 to 16 years of age (p < 0.01). However, in 17- and 18-year-olds, HC was higher in boys compared to girls, and the difference was significant in 18-year-olds (p < 0.01) (Table 2). The WHtR decreased in girls from 3 to 14 years of age and then levelled off (Fig. 1). In boys, with advancing age, WHtR decreased until the age of 15 years and then slightly increased (Fig. 1, Table 3). WHtR was higher in boys compared to girls, and the difference was statistically significant from age 5 to 14 years and age 17–18 years (p < 0.05). The adult WHtR cut-off: 0.5, at age 18 years was z-score + 1.76 (corresponding to the 96th percentile) and z-score + 1.48 (corresponding to the 93rd percentile), for females and males, respectively. In girls, WHR decreased with advancing age, while in boys decreased until a minimum was reached at 14 years of age and then increased (Fig. 1, Table 4). WHR was significantly higher in boys compared to girls (p < 0.01). The adult WHR cut-off in males 0.9 was z-score + 1.87 (corresponding to the 97th percentile) and for females, z-score + 2.39 (corresponding to the 99th percentile). Figure 1 shows population-based, age-specific, LMS-smoothed percentiles of waist and hip circumferences, WHtR and WHR for boys and girls (see also: Online Resource 1). The age- and sex-specific LMS parameters of abdominal obesity indices 90th and 95th percentile and cut-offs for increased cardiometabolic risk are presented in Tables 1, 3 and 4. The age- and sex-specific LMS parameters of HC and 90th and 95th percentile are presented in Table 2. The discriminating power to detect IOTF overweight and obesity, as estimated by the ROC curve, was very high for WC- as well as for HC- and WHtR-SDS, in both girls and boys (Table 5). The ROC curves demonstrate that, in comparison with HC-, WHtR- and WHR-SDS, WC-SDS was the most accurate predictor for OW (p < 0.01) in both sexes and OB in the case of boys (Fig. 2, Table 5). The second and third best predictors for OW and OB were HC-SDS and WHtR-SDS, respectively, whereas WHR-SDS had the lowest predictive ability for OW and OB (Table 5). The predictive abilities for elevated BP were low (AUC ROC < 0.61) in the case of all four anthropometric indices under study; however, their predictive ability was better than chance: AUC ROC confidence intervals did not include 0.5 (Table 5, Fig. 2).
Fig. 1.
The LMS smoothed curves of the 3rd, 10th, 25th, 50th, 75th, 90th and 97th percentiles of waist circumference (WC) (cm), hip circumference (HC) (cm), waist-to-height ratio (WHtR) and waist to hip ratio (WHR). L, skewness; M, median; S, coefficient of variation
Table 1.
Waist circumference LMS parameters, 90th and 95th percentile by sex and age and cut-offs linked to waist 80 and 94 cm in girls and boys, respectively, at age 18 years
| Age | Girls | Boys | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| L | M | S | Cut-offs (waist cm) | L | M | S | Cut-offs (waist cm) | |||||
| Percentile | Cut-off adult 80 cm | Percentile | Cut-off adult 94 cm | |||||||||
| 90th | 95th | 90th | 95th | |||||||||
| 3.0 | −2.7714 | 48.4171 | 0.0657 | 53.3 | 55.1 | 54.7 | −3.2654 | 49.2057 | 0.0617 | 53.9 | 55.7 | 56.8 |
| 4.0 | −2.8222 | 49.8008 | 0.0704 | 55.3 | 57.3 | 56.9 | −3.2911 | 50.7158 | 0.0657 | 56.0 | 58.0 | 59.3 |
| 5.0 | −2.8631 | 51.0858 | 0.0750 | 57.2 | 59.5 | 59.0 | −3.3097 | 52.1768 | 0.0704 | 58.1 | 60.4 | 61.9 |
| 6.0 | −2.8939 | 52.3672 | 0.0795 | 59.1 | 61.7 | 61.2 | −3.3151 | 53.7172 | 0.0759 | 60.4 | 63.1 | 64.9 |
| 7.0 | −2.9133 | 53.768 | 0.0842 | 61.2 | 64.2 | 63.6 | −3.2869 | 55.3446 | 0.0822 | 63.0 | 66.2 | 68.4 |
| 8.0 | −2.9183 | 55.3973 | 0.0891 | 63.6 | 67.1 | 66.4 | −3.2106 | 57.1629 | 0.0894 | 65.9 | 69.7 | 72.4 |
| 9.0 | −2.9110 | 57.2563 | 0.0937 | 66.4 | 70.2 | 69.4 | −3.0898 | 59.1160 | 0.097 | 69.2 | 73.6 | 76.8 |
| 10.0 | −2.9043 | 59.1739 | 0.0969 | 69.0 | 73.3 | 72.4 | −2.9544 | 61.0594 | 0.103 | 72.2 | 77.2 | 80.9 |
| 11.0 | −2.9176 | 61.0813 | 0.0973 | 71.3 | 75.8 | 74.8 | −2.8335 | 63.0168 | 0.1059 | 74.8 | 80.1 | 83.9 |
| 12.0 | −2.9596 | 62.9769 | 0.0945 | 73.2 | 77.5 | 76.6 | −2.7486 | 65.0261 | 0.1055 | 77.0 | 82.3 | 86.1 |
| 13.0 | −3.0242 | 64.7288 | 0.0898 | 74.6 | 78.7 | 77.9 | −2.7231 | 67.0767 | 0.1014 | 78.7 | 83.8 | 87.3 |
| 14.0 | −3.0901 | 66.0883 | 0.0856 | 75.6 | 79.5 | 78.7 | −2.7465 | 69.0525 | 0.0956 | 80.2 | 84.8 | 88.0 |
| 15.0 | −3.1436 | 67.0355 | 0.0824 | 76.2 | 80.0 | 79.2 | −2.7827 | 70.9893 | 0.0899 | 81.6 | 85.9 | 88.8 |
| 16.0 | −3.1801 | 67.6398 | 0.0805 | 76.6 | 80.3 | 79.6 | −2.8105 | 72.8855 | 0.0862 | 83.2 | 87.3 | 90.1 |
| 17.0 | −3.2060 | 68.0580 | 0.0792 | 76.9 | 80.6 | 79.8 | −2.8201 | 74.8000 | 0.0845 | 85.1 | 89.2 | 92.0 |
| 18.0 | −3.2268 | 68.3872 | 0.0781 | 77.2 | 80.7 | 80.0 | −2.8039 | 76.5658 | 0.0842 | 87.1 | 91.2 | 94.0 |
L skewness, M median, S coefficient of variation
Table 2.
Hip circumference LMS parameters, 90th and 95th percentile by sex and age
| Age | Girls | Boys | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| L | M | S | Percentiles (hip cm) | L | M | S | Percentiles (hip cm) | |||
| 90th | 95th | 90th | 95th | |||||||
| 3.0 | −1.9397 | 53.5983 | 0.0658 | 58.8 | 60.5 | −3.2603 | 53.0025 | 0.0659 | 58.5 | 60.6 |
| 4.0 | −2.1057 | 56.2253 | 0.0719 | 62.3 | 64.4 | −3.1759 | 55.6182 | 0.0684 | 61.6 | 63.9 |
| 5.0 | −2.1656 | 58.7635 | 0.0760 | 65.6 | 68.0 | −3.0797 | 58.0905 | 0.0723 | 64.8 | 67.4 |
| 6.0 | −2.2500 | 61.3785 | 0.0786 | 68.8 | 71.5 | −2.9630 | 60.7661 | 0.0773 | 68.3 | 71.3 |
| 7.0 | −2.3606 | 64.2733 | 0.0811 | 72.4 | 75.4 | −2.8015 | 63.8612 | 0.0826 | 72.4 | 75.8 |
| 8.0 | −2.3283 | 67.3299 | 0.0849 | 76.3 | 79.7 | −2.5724 | 67.0931 | 0.0881 | 76.7 | 80.4 |
| 9.0 | −2.0251 | 70.5600 | 0.0889 | 80.3 | 83.9 | −2.2849 | 70.2462 | 0.0936 | 80.8 | 84.9 |
| 10.0 | −1.6627 | 73.7811 | 0.0925 | 84.2 | 87.9 | −1.9891 | 73.3126 | 0.0978 | 84.7 | 89.0 |
| 11.0 | −1.4607 | 77.3026 | 0.0958 | 88.5 | 92.5 | −1.7364 | 76.3859 | 0.0998 | 88.3 | 92.7 |
| 12.0 | −1.4382 | 81.4061 | 0.0939 | 92.9 | 96.9 | −1.5586 | 79.6072 | 0.0990 | 91.7 | 96.1 |
| 13.0 | −1.2088 | 85.7057 | 0.0867 | 96.6 | 100.2 | −1.5012 | 82.9675 | 0.0949 | 94.9 | 99.1 |
| 14.0 | −1.2133 | 88.9870 | 0.0783 | 99.0 | 102.4 | −1.5893 | 86.2848 | 0.0878 | 97.7 | 101.7 |
| 15.0 | −1.7312 | 91.1207 | 0.0714 | 100.7 | 103.9 | −1.7882 | 89.2425 | 0.0795 | 99.9 | 103.6 |
| 16.0 | −2.1214 | 92.2983 | 0.0679 | 101.6 | 104.8 | −2.0177 | 91.5519 | 0.0728 | 101.5 | 105.0 |
| 17.0 | −2.3828 | 93.0326 | 0.0659 | 102.2 | 105.5 | −2.2243 | 93.3512 | 0.0678 | 102.8 | 106.1 |
| 18.0 | −2.5376 | 93.4618 | 0.0649 | 102.6 | 105.8 | −2.4012 | 94.8197 | 0.0638 | 103.9 | 107.0 |
L skewness, M median, S coefficient of variation
Table 3.
WHtR LMS parameters, 90th and 95th percentile by sex and age and cut-offs linked to WHtR 0.5 at age 18 years
| Age | Girls | Boys | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| L | M | S | Cut-offs (ratio) | L | M | S | Cut-offs (ratio) | |||||
| Percentile | Cut-off adult 0.5 | 90th | Cut-off adult 0.5 | |||||||||
| 90th | 95th | 90th | 95th | |||||||||
| 3.0 | −2.4564 | 0.5022 | 0.0620 | 0.549 | 0.565 | 0.570 | −3.3777 | 0.5038 | 0.0558 | 0.547 | 0.562 | 0.555 |
| 4.0 | −2.6240 | 0.4826 | 0.0647 | 0.530 | 0.547 | 0.553 | −3.4072 | 0.4846 | 0.0596 | 0.529 | 0.546 | 0.538 |
| 5.0 | −2.7660 | 0.4645 | 0.0676 | 0.513 | 0.530 | 0.537 | −3.4370 | 0.4684 | 0.0634 | 0.515 | 0.533 | 0.525 |
| 6.0 | −2.8890 | 0.4495 | 0.0708 | 0.499 | 0.518 | 0.525 | −3.4659 | 0.4558 | 0.0676 | 0.505 | 0.524 | 0.516 |
| 7.0 | −3.0004 | 0.4383 | 0.0744 | 0.490 | 0.510 | 0.518 | −3.4905 | 0.4461 | 0.0724 | 0.499 | 0.520 | 0.510 |
| 8.0 | −3.0909 | 0.4305 | 0.0780 | 0.485 | 0.507 | 0.515 | −3.5077 | 0.4397 | 0.0776 | 0.497 | 0.521 | 0.510 |
| 9.0 | −3.1639 | 0.4251 | 0.0813 | 0.482 | 0.506 | 0.515 | −3.5135 | 0.4359 | 0.0823 | 0.497 | 0.524 | 0.511 |
| 10.0 | −3.2243 | 0.4206 | 0.0839 | 0.480 | 0.505 | 0.514 | −3.5061 | 0.4329 | 0.0860 | 0.498 | 0.526 | 0.513 |
| 11.0 | −3.2697 | 0.4158 | 0.0852 | 0.476 | 0.502 | 0.511 | −3.4859 | 0.4297 | 0.0880 | 0.496 | 0.526 | 0.511 |
| 12.0 | −3.2853 | 0.4113 | 0.0852 | 0.471 | 0.496 | 0.506 | −3.4533 | 0.4253 | 0.0885 | 0.491 | 0.521 | 0.507 |
| 13.0 | −3.2681 | 0.4088 | 0.0846 | 0.467 | 0.492 | 0.502 | −3.4087 | 0.4197 | 0.0876 | 0.483 | 0.512 | 0.498 |
| 14.0 | −3.2220 | 0.4083 | 0.0837 | 0.466 | 0.490 | 0.499 | −3.3508 | 0.4145 | 0.0860 | 0.476 | 0.502 | 0.490 |
| 15.0 | −3.1608 | 0.4096 | 0.0826 | 0.466 | 0.489 | 0.498 | −3.2786 | 0.4126 | 0.0847 | 0.472 | 0.497 | 0.485 |
| 16.0 | −3.0995 | 0.4114 | 0.0816 | 0.467 | 0.489 | 0.498 | −3.1951 | 0.4150 | 0.0838 | 0.473 | 0.498 | 0.486 |
| 17.0 | −3.0708 | 0.4132 | 0.0810 | 0.468 | 0.490 | 0.499 | −3.1045 | 0.4209 | 0.0836 | 0.479 | 0.504 | 0.492 |
| 18.0 | −3.0735 | 0.4147 | 0.0806 | 0.470 | 0.492 | 0.500 | −3.0090 | 0.4281 | 0.0836 | 0.487 | 0.511 | 0.500 |
L skewness, M median, S coefficient of variation, WHtR waist-to-height ratio
Table 4.
WHR LMS parameters, 90th and 95th percentile by sex and age and cut − offs linked to WHR 0.85 and 0.9 in the case of girls and boys, respectively, at age 18 years
| Age | Girls | Boys | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| L | M | S | Cut-offs (ratio) | L | M | S | Cut-offs (ratio) | |||||
| Percentile | Cut-off adult 0.85 | 90th | Cut-off adult 0.9 | |||||||||
| 90th | 95th | 90th | 95th | |||||||||
| 3.0 | −1.2336 | 0.9034 | 0.0447 | 0.959 | 0.976 | 1.013 | 1.2953 | 0.9268 | 0.0448 | 0.980 | 0.994 | 1.004 |
| 4.0 | −1.2869 | 0.8869 | 0.0450 | 0.942 | 0.959 | 0.996 | 0.8351 | 0.9122 | 0.0436 | 0.963 | 0.978 | 0.987 |
| 5.0 | −1.3211 | 0.8699 | 0.0455 | 0.924 | 0.941 | 0.978 | 0.3820 | 0.8987 | 0.0427 | 0.949 | 0.963 | 0.972 |
| 6.0 | −1.3365 | 0.8532 | 0.0460 | 0.907 | 0.924 | 0.961 | −0.0611 | 0.8838 | 0.0423 | 0.933 | 0.948 | 0.957 |
| 7.0 | −1.3554 | 0.8380 | 0.0467 | 0.892 | 0.909 | 0.946 | −0.4863 | 0.8672 | 0.0426 | 0.917 | 0.931 | 0.941 |
| 8.0 | −1.3932 | 0.8260 | 0.0474 | 0.880 | 0.897 | 0.934 | −0.8906 | 0.8547 | 0.0434 | 0.905 | 0.920 | 0.930 |
| 9.0 | −1.4508 | 0.8165 | 0.0480 | 0.871 | 0.888 | 0.926 | −1.2649 | 0.8466 | 0.0446 | 0.898 | 0.914 | 0.925 |
| 10.0 | −1.5299 | 0.8070 | 0.0487 | 0.862 | 0.879 | 0.917 | −1.5945 | 0.8392 | 0.0459 | 0.893 | 0.909 | 0.920 |
| 11.0 | −1.6430 | 0.7945 | 0.0495 | 0.850 | 0.867 | 0.906 | −1.8697 | 0.8318 | 0.0469 | 0.887 | 0.904 | 0.915 |
| 12.0 | −1.8004 | 0.7779 | 0.0503 | 0.833 | 0.851 | 0.891 | −2.0832 | 0.8243 | 0.0477 | 0.880 | 0.898 | 0.910 |
| 13.0 | −1.9945 | 0.7612 | 0.0510 | 0.816 | 0.834 | 0.875 | −2.2387 | 0.8147 | 0.0482 | 0.871 | 0.889 | 0.901 |
| 14.0 | −2.1787 | 0.7483 | 0.0516 | 0.804 | 0.822 | 0.864 | −2.3471 | 0.8045 | 0.0483 | 0.860 | 0.878 | 0.890 |
| 15.0 | −2.3124 | 0.7401 | 0.0519 | 0.796 | 0.814 | 0.856 | −2.4201 | 0.7981 | 0.0484 | 0.854 | 0.872 | 0.884 |
| 16.0 | −2.3915 | 0.7353 | 0.0521 | 0.791 | 0.809 | 0.852 | −2.4686 | 0.7983 | 0.0486 | 0.854 | 0.873 | 0.885 |
| 17.0 | −2.4265 | 0.7333 | 0.0522 | 0.789 | 0.807 | 0.851 | −2.4950 | 0.8036 | 0.0491 | 0.860 | 0.879 | 0.892 |
| 18.0 | −2.4375 | 0.7326 | 0.0522 | 0.788 | 0.807 | 0.850 | −2.5042 | 0.8100 | 0.0496 | 0.868 | 0.887 | 0.900 |
L skewness, M median, S coefficient of variation, WHR waist-to-hip ratio
Table 5.
Results of ROC analysis for the optimal waist-SDS, hip-SDS, WHtR-SDS and WHR-SDS for predicting IOTF overweight/obesity and elevated BP in girls and boys
| AUC ROC (95% CI) | Cut-off | Sensitivity | Specificity | Youden index | p valuea | |
|---|---|---|---|---|---|---|
| Girls – overweight | ||||||
| Waist-SDS | 0.969 (0.964 0.972) | 0.7414 | 92.4% | 89.7% | 0.821 | < 0.01b |
| Hip-SDS | 0.960 (0.956 0.964) | 0.7042 | 90.8% | 87.9% | 0.787 | < 0.05c |
| WHtR-SDS | 0.954 (0.948 0.957) | 0.6972 | 89.7% | 87.3% | 0.770 | < 0.01d |
| WHR-SDS | 0.667 (0.652 0.682) | 0.4839 | 52.8% | 72.9% | 0.257 | − |
| Girls – obesity | ||||||
| Waist-SDS | 0.989 (0.986 0.991) | 1.3913 | 97.4% | 93.9% | 0.913 | < 0.01c |
| Hip-SDS | 0.987 (0.984 0.989) | 1.4039 | 96.6% | 94.4% | 0.909 | < 0.01d |
| WHtR-SDS | 0.982 (0.979 0.986) | 1.3466 | 94.6% | 93.2% | 0.878 | < 0.01d |
| WHR-SDS | 0.759 (0.732 0.786) | 0.7353 | 62.2% | 78.7% | 0.409 | − |
| Girls – elevated BP | ||||||
| Waist-SDS | 0.592 (0.571 0.614) | 0.5849 | 41.2% | 74.4% | 0.156 | < 0.01d |
| Hip-SDS | 0.591 (0.570 0.613) | 0.3627 | 48.3% | 65.6% | 0.139 | < 0.01d |
| WHtR-SDS | 0.598 (0.578 0.617) | 0.7443 | 42.4% | 73.6% | 0.160 | < 0.01d |
| WHR-SDS | 0.541 (0.520 0.562) | 0.5102 | 38.0% | 70.7% | 0.091 | − |
| Boys – overweight | ||||||
| Waist-SDS | 0.975 (0.972 0.978) | 0.6887 | 93.0% | 90.8% | 0.838 | < 0.01b |
| Hip-SDS | 0.967 (0.963 0.970) | 0.6609 | 92.2% | 89.1% | 0.814 | < 0.05c |
| WHtR-SDS | 0.961 (0.956 0.965) | 0.6675 | 89.6% | 89.1% | 0.787 | < 0.01d |
| WHR-SDS | 0.677 (0.662 0.691) | 0.3393 | 58.8% | 69.0% | 0.278 | − |
| Boys – obesity | ||||||
| Waist-SDS | 0.991 (0.989 0.992) | 1.3670 | 98.1% | 94.4% | 0.924 | < 0.01b |
| Hip-SDS | 0.986 (0.983 0.989) | 1.2332 | 96.4% | 92.6% | 0.890 | < 0.01d |
| WHtR-SDS | 0.986 (0.984 0.989) | 1.2935 | 96.4% | 93.3% | 0.896 | < 0.01d |
| WHR-SDS | 0.753 (0.728 0.778) | 0.3367 | 73.7% | 65.8% | 0.395 | − |
| Boys – elevated BP | ||||||
| Waist-SDS | 0.594 (0.573 0.616) | 0.1994 | 54.7% | 60.7% | 0.154 | < 0.01d |
| Hip-SDS | 0.599 (0.577 0.620) | 0.2172 | 55.2% | 60.8% | 0.160 | < 0.01d |
| WHtR-SDS | 0.607 (0.586 0.628) | 0.4782 | 41.2% | 75.0% | 0.161 | < 0.01e |
| WHR-SDS | 0.524 (0.501 0.544) | 1.3379 | 13.1% | 92.2% | 0.052 | − |
AUC, area under the curve, BP blood pressure, CI confidence interval, IOTF International Obesity Task Force, ROC receiver operating characteristic, SDS standard deviation score, WHR waist-to-hip ratio, WHtR waist-to-height ratio
aresults of the DeLong’s test, only statistically significant differences are reported
bcompared to: HC-, WHtR- and WHR − SDS curve
ccompared to: WHtR − and WHR − SDS curve
dcompared to: WHR-SDS curve
ecompared to: waist- and WHR-SD
Fig. 2.
ROC curves for prediction of IOTF overweight, obesity and elevated blood pressure from waist-SDS, hip-SDS, WHtR-SDS and WHR-SDS. BP, blood pressure; IOTF, International Obesity Task Force; ROC, receiver operating characteristics; WHtR, waist-to-height ratio; WHR, waist-to-hip ratio; SDS, standard deviation score
The sensitivity, specificity and Youden index of WC-SDS, HC-SDS, WHtR-SDS and WHR-SDS for the prediction of OW, OB and elevated BP are presented in Table 5. The Youden index was higher than 0.5 in the case of WC-SDS, HC-SDS and WHtR-SDS prediction of OW and OB both in girls and boys (Table 5). In the case of WHR-SDS, the Youden index was lower than 0.5 (Table 5). All analysed anthropometric indices had a very low Youden index (< 0.17) for predicting elevated BP.
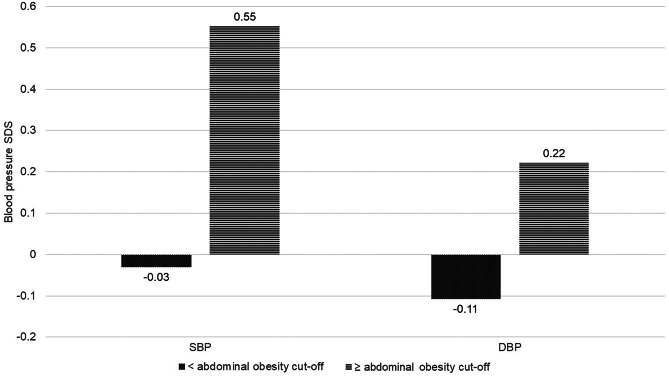
Systolic and diastolic blood pressure were significantly (Student’s t-test p < 0.0001) higher in children and adolescents with abdominal obesity compared to those without abdominal obesity (Fig. 3). According to the results of the multiple logistic regression models, children and adolescents with abdominal obesity had significantly higher odds for elevated blood pressure: OR = 2.577 (95% CI: 2.259–2.940). The effect was independent of age and sex (Table 6).
Fig. 3.
Blood pressure SDS of study participants according to abdominal obesity status: < abdominal obesity, all anthropometric indices (waist circumference, waist-to-height ratio and waist-to-hip ratio) below their cut-offs for abdominal obesity; ≥ abdominal obesity, at least one of anthropometric indices (waist circumference, waist-to-height ratio or waist-to-hip ratio) equal or over cut-off for abdominal obesity. DBP, diastolic blood pressure; SBP, systolic blood pressure; SDS, standard deviation score
Table 6.
Results of multiple logistic regression. Statistics reflects odds of elevated blood pressure as function of abdominal obesity, sex and age
| β | SE β | p value | OR | 95% | CI | |
|---|---|---|---|---|---|---|
| Intercept | −2.576 | 0.097 | < .0001 | |||
| Abdominal obesity | 0.947 | 0.067 | < .0001 | 2.577 | 2.259 | 2.940 |
| Sex | −0.014 | 0.049 | 0.77 | 0.986 | 0.896 | 1.085 |
| Age | 0.007 | 0.005 | 0.19 | 1.007 | 0.997 | 1.017 |
β regression coefficient, SE standard error, OR odds ratio, CI confidence interval
Discussion
This study presents, for the first time in the literature, age- and sex-specific references for waist and hip circumferences, WHtR and WHR of a representative sample of 22,370 Polish children and adolescents aged 3–18 years and cut-offs for abdominal obesity indices linked to adults’ cardiovascular risk thresholds. These references will allow the calculation of individual SDS for waist and hip circumferences, WHtR and WHR, which is important in paediatric healthcare practice and epidemiological studies. Longitudinal observations show that abdominal obesity status may change, as reported for children aged 4 to 9 years by Ortiz-Marrón et al. [48], and changes include both incidence or remittance, as well as the obesity status may be stable (either as obese or non-obese). This indicates the importance of systematic monitoring of child’s abdominal obesity indices using appropriate tool, namely nationally representative references from age 3 to adulthood.
Study material for this paper was collected 11 to 15 years ago. More recent studies in Poland show higher, in comparison to our material, values of waist, hip and WHtR [49, 50], what might reflect “continuing secular trend to an increase in childhood fatness” [51]. From this perspective, nationally representative sample taken several years ago is less influenced by secular trend in fatness. This approach is in line with decision taken in the UK that weight and BMI reference should be “frozen” [51].
The findings of this study concerning the outstanding predictive ability of WC- and WHtR-SDS for IOTF overweight and obesity are in line with the results of other studies [20]. The areas under the ROC for WC- and WHtR-SDS are similar. Also, HC has an outstanding predictive ability for IOTF overweight and obesity, whereas WHR-SDS has poor discrimination for overweight and acceptable discrimination for obesity in children and adolescents.
An increased amount of body fat tissue, especially visceral fat, plays a major role in the pathogenesis of insulin resistance and causes significant metabolic changes in lipid and carbohydrate metabolism [9]. From the perspective of the presence of metabolic disturbances, youth with obesity are not a homogeneous group. Obese children with normal glucose levels, blood pressure and lipid levels constitute a metabolically healthy obesity (MHO) subgroup [52], while metabolically unhealthy obesity (MUO) involves cardiometabolic abnormalities in obese individuals, thus increasing their health risk [53, 54]. The MUO phenotype, as compared to the MHO phenotype, is linked to higher waist circumference and WHtR [54–56], which makes it possible to identify higher risk phenotype using waist measurement, a convenient, simple and inexpensive tool. While waist circumference and WHtR optimal cut-offs are available for the detection of MHO and MUO phenotypes in adults [57, 58], according to the best authors’ knowledge, such uniform cut-offs have not been established, so far, for children and adolescents. To predict increased cardiometabolic risk in children and adolescents, WC-SDS in the range of 0.5 − 1.28 and WHtR ratio in the range of 0.41 − 0.60 is proposed [29, 33, 47, 59–61].
Some authors proposed a fixed and equaled value of WHtR ratio = 0.5 as a criterion for abdominal obesity in children and adolescents, regardless of age. The research presented in this paper has indicated that WHtR changes with age, which is in line with observations by other authors [10, 11, 13, 20–25], and there are differences between boys and girls. Taking these observations into account, it seems that, across a wide age range of children and adolescents, WHtR cut-offs based on age- and sex-specific WHtR-SDS would be more appropriate. The data obtained show that in younger ages (3–7 years of age), WHtR cut-offs, based on percentile 96 and 93 in the case of girls and boys, respectively, were in the range 0.52–0.57 and in older ages 0.49–0.51 to reach a ratio of 0.5 at the age of 18 years. Abdominal obesity references proposed by this paper may be useful in future works on tools which would enable distinction between MHO and MUO in childhood and adolescence.
In adults, in contrast to higher waist circumference and WHtR, higher hip circumference is associated with a lower risk of type 2 diabetes and cardiovascular disease [62]. According to the authors’ knowledge, such data is not available for children. It may be related to scarce reference data on the hip circumference in children and adolescents [28, 63, 64]. LMS parameters for hip circumference for children and youth aged 3–18 years, presented for the first time in this paper, enable hip SDS calculation. Our results show that HC-SDS has outstanding discrimination for overweight and obesity, giving way only to WC-SDS. HC references, established by the presented study, can be of use in future works on cardiometabolic risk assessment among children.
Although blood pressure was higher in children and adolescents with abdominal obesity and odds for elevated blood pressure were higher in the abdominal obesity group, all anthropometric indices under study had a similar and low predictive ability for elevated blood pressure. These results are in line with other researchers’ findings [65–67].
Strengths
The present paper has several strengths. First, the study’s random sample was large (22,370 participants) and nationally representative. The study involved children and adolescents aged 3–18 years. BP measurements were included as a component of cardiometabolic risk assessment. The data were derived using the same standardised procedure. Percentile curves were constructed using the LMS method, and cardiometabolic risk cut-offs were linked to adult cardiometabolic risk cut-offs.
Limitations
The study did not include blood lipids, insulin and glucose for cardiometabolic risk assessment and had a cross-sectional design.
Conclusions
In conclusion, waist and hip circumferences-SDS and WHtR-SDS could be used as non-invasive and low-cost indices of central obesity and cardiometabolic risk in children and adolescents. Moreover, proposed abdominal obesity references may be useful in future works on tools which would enable the distinction between metabolically healthy and metabolically unhealthy obesity in childhood and adolescence. Longitudinal studies, including also blood lipids, insulin and glucose, could be helpful to determine whether WHtR, WC and HC changes are associated with cardiometabolic risk in youth.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- AUC
Area under the curve
- BMI
Body mass index
- BP
Blood pressure
- CI
Confidence interval
- DBP
Diastolic blood pressure
- HC
Hip circumference
- IOTF
The International Obesity Task Force
- LMS
Lambda-mu-sigma
- MHO
Metabolically healthy obesity
- MUO
Metabolically unhealthy obesity
- OB
Obesity
- OW
Overweight
- ROC
Receiver operating characteristic
- SBP
Systolic blood pressure
- SDS
Standard deviation score
- WC
Waist circumference
- WHR
Waist-to-hip ratio
- WHtR
Waist-to-height ratio
Authors’ Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Zbigniew Kułaga, Anna Świąder-Leśniak and Aneta Kotowska. The first draft of the manuscript was written by Zbigniew Kułaga, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The OLAF study was supported by a grant from Iceland, Liechtenstein, and Norway through the EEA Financial Mechanism and the Norwegian Financial Mechanism, and the Ministry of Science and Higher Education of Poland; grant number: PL0080. The OLA study was supported by a grant from the National Centre for Research and Development; grant number: N R13 0002 06.
Data availability
Data are available upon reasonable request sent to the corresponding author. Sharing of data might be considered for specific research projects, based upon study protocol ethically accepted.
Declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approvals to conduct both studies were granted by the Children’s Memorial Health Institute Ethics Committee before the studies commenced (approval number: 104/KBE/2007 date: 2007-10-10 and 177/KBE/2008 date 2008-10-12).
Consent to participate
Informed consent in writing was obtained from a parent of each participating child under 18 years of age, and, in addition, written consent was also obtained from all subjects over 16 years of age.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.González-Álvarez MA, Lázaro-Alquézar A, Simón-Fernández MB (2020) Global trends in child obesity: are figures converging? IJERPH 17(24):9252. 10.3390/ijerph17249252 [DOI] [PMC free article] [PubMed]
- 2.Manios Y, Androutsos O, Katsarou C, Vampouli EA, Kulaga Z, Gurzkowska B, Iotova V, Usheva N, Cardon G, Koletzko B, Moreno LA, De Bourdeaudhuij I (2018) Prevalence and sociodemographic correlates of overweight and obesity in a large Pan-European cohort of preschool children and their families: the ToyBox study. Nutrition 55–56:192–198. 10.1016/j.nut.2018.05.007 [DOI] [PubMed]
- 3.Inchley J, Currie D, Budisavljevic S, Torsheim T, Jåstad A, Cosma A, Kelly C, Arnarsson ÁM, Samdal O (2022) Spotlight on adolescent health and well-being. Findings from the 2017/2018 health behaviour in school-aged children (HBSC) survey in Europe and Canada. International report Published online 2022
- 4.Kułaga Z, Grajda A, Gurzkowska B, Wojtyło M, Góźdź M, Litwin M. The prevalence of overweight and obesity among Polish school- aged children and adolescents. Przegl Epidemiol. 2016;70(4):641–651. [PubMed] [Google Scholar]
- 5.Reilly JJ (2006) Diagnostic accuracy of the BMI for age in paediatrics. Int J Obes 30(4):595–597. 10.1038/sj.ijo.0803301 [DOI] [PubMed]
- 6.Dobbelsteyn C, Joffres M, MacLean D, Flowerdew G (2001) A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors. The Canadian Heart Health Surveys. Int J Obes 25(5):652–661. 10.1038/sj.ijo.0801582 [DOI] [PubMed]
- 7.Lee CMY, Huxley RR, Wildman RP, Woodward M (2008) Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol 61(7):646–653. 10.1016/j.jclinepi.2007.08.012 [DOI] [PubMed]
- 8.Brenner DR, Tepylo K, Eny KM, Cahill LE, El-Sohemy A (2010) Comparison of body mass index and waist circumference as predictors of cardiometabolic health in a population of young Canadian adults. Diabetol Metab Syndr 2(1):28. 10.1186/1758-5996-2-28 [DOI] [PMC free article] [PubMed]
- 9.Katzmarzyk PT, Srinivasan SR, Chen W, Malina RM, Bouchard C, Berenson GS (2004) Body mass index, waist circumference, and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescents. Pediatr 114(2):e198–e205. 10.1542/peds.114.2.e198 [DOI] [PubMed]
- 10.Maffeis C, Banzato C, Talamini G (2008) Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr 152(2):207–213.e2. 10.1016/j.jpeds.2007.09.021 [DOI] [PubMed]
- 11.Campagnolo PDB, Hoffman DJ, Vitolo MR (2011) Waist-to-height ratio as a screening tool for children with risk factors for cardiovascular disease. Ann Hum Biol 38(3):265–270. 10.3109/03014460.2010.526147 [DOI] [PubMed]
- 12.Muñoz-Hernando J, Escribano J, Ferré N, Closa-Monasterolo R, Grote V, Koletzko B, Gruszfeld D, ReDionigi A, Verduci E, Xhonneux A et al (2022) Usefulness of the waist-to-height ratio for predicting cardiometabolic risk in children and its suggested boundary values. Clin Nutr 41(2):508–516. 10.1016/j.clnu.2021.12.008 [DOI] [PubMed]
- 13.Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, Santos RD, Arsenault B, Cuevas A, Hu FB et al (2020) Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol 16(3):177–189. 10.1038/s41574-019-0310-7 [DOI] [PMC free article] [PubMed]
- 14.Kułaga Z, Litwin M, Grajda A, Kułaga K, Gurzkowska B, Góźdź M, Pan H (2012) Oscillometric blood pressure percentiles for Polish normal-weight school-aged children and adolescents. J Hypertens 30(10):1942–1954. 10.1097/HJH.0b013e328356abad. [DOI] [PubMed]
- 15.Bassali R, Waller JL, Gower B, Allison J, Davis CL (2010) Utility of waist circumference percentile for risk evaluation in obese children. Int J Pediatr Obes 5(1):97–101. 10.3109/17477160903111722 [DOI] [PMC free article] [PubMed]
- 16.Litwin M, Niemirska A, Śladowska-Kozlowska J, Wierzbicka A, Janas R, Wawer Z T, Wisniewski A, Feber J (2010) Regression of target organ damage in children and adolescents with primary hypertension. Pediatr Nephrol 25(12):2489–2499. 10.1007/s00467-010-1626-7 [DOI] [PMC free article] [PubMed]
- 17.Bacopoulou F, Efthymiou V, Landis G, Rentoumis A, Chrousos GP (2015) Waist circumference, waist-to-hip ratio and waist-to-height ratio reference percentiles for abdominal obesity among Greek adolescents. BMC Pediatr 15(1):50. 10.1186/s12887-015-0366-z [DOI] [PMC free article] [PubMed]
- 18.Bojanic D, Ljubojevic M, Krivokapic D, Gontarev S (2020) Waist circumference, waist-to-hip ratio, and waist-to-height ratio reference percentiles for abdominal obesity among Macedonian adolescents. Nutr Hosp. 10.20960/nh.03006 [DOI] [PubMed]
- 19.Inokuchi M, Matsuo N, Takayama JI, Hasegawa T (2021) Population-based waist circumference reference values in Japanese children (0–6 years): comparisons with Dutch, Swedish and Turkish preschool children. J Pediatr Endocrinol Metab 34(3):349–356. 10.1515/jpem-2020-0418 [DOI] [PubMed]
- 20.Brannsether B, Roelants M, Bjerknes R, Júlíusson P (2011) Waist circumference and waist-to-height ratio in Norwegian children 4–18 years of age: reference values and cut-off levels: WC and WHtR: reference values. Acta Paediatr 100(12):1576–1582. 10.1111/j.1651-2227.2011.02370.x [DOI] [PubMed]
- 21.Khadilkar A, Ekbote V, Chiplonkar S, Khadilkar V, Kajale N, Kulkarni S, Parthasarathy L, Arya A, Bhattacharya A, Agarwal S (2014) Waist circumference percentiles in 2–18 year old Indian children. J Pediatr 164(6):1358–1362.e2. 10.1016/j.jpeds.2014.02.018 [DOI] [PubMed]
- 22.Kweon S, Kim Y, Jang M, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K (2014) Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 43(1):69–77. 10.1093/ije/dyt228 [DOI] [PMC free article] [PubMed]
- 23.Ashwell M, Gunn P, Gibson S (2012) Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis: Waist-to-height ratio as a screening tool. Obes Rev 13(3):275–286. 10.1111/j.1467-789X.2011.00952.x [DOI] [PubMed]
- 24.McCarthy HD, Ashwell M (2006) A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message – ‘keep your waist circumference to less than half your height’. Int J Obes 30(6):988–992. 10.1038/sj.ijo.0803226 [DOI] [PubMed]
- 25.Sung RY, So HK, Choi KC, Choi KC., Nelson EA, Li AM, Yin JA, Kwok CW, Ng PC, Fok TF (2008) Waist circumference and waist-to-height ratio of Hong Kong Chinese children. BMC Public Health 8(1):324. 10.1186/1471-2458-8-324 [DOI] [PMC free article] [PubMed]
- 26.Roswall J, Bergman S, Almqvist-Tangen G, Alm B, Niklasson A, Nierop AF, Dahlgren J (2009) Population-based waist circumference and waist-to-height ratio reference values in preschool children. Acta Paediatr 98(10):1632–1636. 10.1111/j.1651-2227.2009.01430.x [DOI] [PubMed]
- 27.Fu J, Hofker M, Wijmenga C (2015) Apple or pear: size and shape matter. Cell Metab 21(4):507–508. 10.1016/j.cmet.2015.03.016 [DOI] [PubMed]
- 28.Fredriks AM, van Buuren S, Fekkes M, Verloove-Vanhorick SP, Wit JM (2005) Are age references for waist circumference, hip circumference and waist-hip ratio in Dutch children useful in clinical practice? Eur J Pediatr 164(4):216–222. 10.1007/s00431-004-1586-7 [DOI] [PubMed]
- 29.Mushtaq MU, Gull S, Abdullah HM, Shahid U, Shad MA, Akram J (2011) Waist circumference, waist-hip ratio and waist-height ratio percentiles and central obesity among Pakistani children aged five to twelve years. BMC Pediatr 11(1):105. 10.1186/1471-2431-11-105 [DOI] [PMC free article] [PubMed]
- 30.Bamoshmoosh M (2013) Central obesity in Yemeni children: a population based cross-sectional study. World J Cardiol 5(8):295. 10.4330/wjc.v5.i8.295 [DOI] [PMC free article] [PubMed]
- 31.Rönnecke E, Vogel M, Bussler S, Grafe N, Jurkutat A, Schlingmann M, Koerner A, Kiess W (2019) Age- and sex-related percentiles of skinfold thickness, waist and hip circumference, waist-to-hip ratio and waist-to-height ratio: results from a population-based pediatric cohort in Germany (LIFE Child). Obes Facts 12(1):25–39. 10.1159/000494767 [DOI] [PMC free article] [PubMed]
- 32.Gillum R. (1999) Distribution of waist-to-hip ratio, other indices of body fat distribution and obesity and associations with HDL cholesterol in children and young adults aged 4–19 years: The Third National Health and Nutrition Examination Survey. Int J Obes 23(6):556–563. 10.1038/sj.ijo.0800866 [DOI] [PubMed]
- 33.Xi B, Zong X, Kelishadi R, Litwin M, Hong YM, Poh BK, Steffen LM, Galcheva SV, Herter-Aeberli I, Nawarycz T et al (2020) International waist circumference percentile cutoffs for central obesity in children and adolescents aged 6 to 18 years. J Clin Endocrinol Metab 105(4):e1569–e1583. 10.1210/clinem/dgz195 [DOI] [PMC free article] [PubMed]
- 34.Hocquette A, Durox M, Wood R, Klungsøyr K, Szamotulska K, Berrut S, Rihs T, Kyprianou T, Sakkeus L, Lecomte A et al (2021) International versus national growth charts for identifying small and large-for-gestational age newborns: a population-based study in 15 European countries. Lancet Reg Health Eur 8:100167. 10.1016/j.lanepe.2021.100167 [DOI] [PMC free article] [PubMed]
- 35.Lee K (2019) Comparison of body mass index percentiles to detect metabolic syndrome using the Korean, United States centers for disease control and prevention, and World Health Organization references in Korean children aged 10–16 years. Metab Syndr Relat Disord 17(4):210–216. 10.1089/met.2018.0126 [DOI] [PubMed]
- 36.Kułaga Z, Litwin M, Tkaczyk M, Palczewska I, Zajączkowska M, Zwolińska D, Krynicki T, Wasilewska A, Moczulska A, Morawiec-Knysak A et al (2011) Polish 2010 growth references for school-aged children and adolescents. Eur J Pediatr 170(5):599–609. 10.1007/s00431-010-1329-x [DOI] [PMC free article] [PubMed]
- 37.Kułaga Z, Grajda A, Gurzkowska B, Góźdź M, Wojtyło M, Świąder A, Różdżyńska-Świątkowska A, Litwin M (2013) Polish 2012 growth references for preschool children. Eur J Pediatr 172(6):753–761. 10.1007/s00431-013-1954-2 [DOI] [PMC free article] [PubMed]
- 38.Grajda A, Kułaga Z, Gurzkowska B, Wojtyło M, Góźdź M, Litwin M. (2017) Preschool children blood pressure percentiles by age and height. J Hum Hypertens 31(6):400–408. 10.1038/jhh.2016.90 [DOI] [PubMed]
- 39.Leung AA, Daskalopoulou SS, Dasgupta K, McBrien K, Butalia S, Zarnke KB, Nerenberg K, Harris KC, Nakhla M, Cloutier R et al (2017) Hypertension Canada’s 2017 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults. Can J Cardiol 33(5):557–576. 10.1016/j.cjca.2017.03.005 [DOI] [PubMed]
- 40.Castro AV, Fragoso AS, Moreno FJA, Sánchez Pérez M, Rodríguez Padial L, Rodríguez Roca GC (2019) Mean blood pressure of the general population with the mean of three measurements versus the mean of the second and third measurements. Ricarto Study. High Blood Press Cardiovasc Prev 26(5):391–397. 10.1007/s40292-019-00338-0 [DOI] [PubMed]
- 41.Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr. 1990;44(1):45–60. [PubMed] [Google Scholar]
- 42.Pan H, Cole TJ (2000) LMSchartmaker, a program to construct growth references using the LMS method Version 2.42. Published online 2000. Accessed 25 Apr 2010. http://www.healthforallchildren.co.uk
- 43.Cole TJ, Lobstein T (2012) Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity: extended international BMI cut-offs. Pediatr Obes 7(4):284–294. 10.1111/j.2047-6310.2012.00064.x [DOI] [PubMed]
- 44.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–845. doi: 10.2307/2531595. [DOI] [PubMed] [Google Scholar]
- 45.Dietz WH, Robinson TN (1998) Use of the body mass index (BMI) as a measure of overweight in children and adolescents. J Pediatr 132(2):191–193. 10.1016/S0022-3476(98)70426-3 [DOI] [PubMed]
- 46.World Health Organization (2008) Waist circumference and waist-hip ratio : report of a WHO expert consultation, Geneva, 8–11 December 2008. Published online 2011. Accessed 15 Feb 2023. https://apps.who.int/iris/handle/10665/44583
- 47.Alberti G, Zimmet P, Kaufman F, Tajima N, Martin S, Arslanian S, Wong G, Bennett P, Shaw J, Caprio S (2007) The IDF consensus definition of the metabolic syndrome in children and adolescents. International Diabetes Federation [DOI] [PubMed]
- 48.Ortiz-Marrón H, Cabañas Pujadas G, Ortiz-Pinto MA, Garcia AM, Matesanz Martinez C, Del Castillo MAM, Cortes Rico M, Galan I (2023) Changes in general and abdominal obesity in children at 4, 6 and 9 years of age and their association with other cardiometabolic risk factors. Eur J Pediatr 182(3):1329–1340. 10.1007/s00431-022-04802-3 [DOI] [PMC free article] [PubMed]
- 49.Klimek-Piotrowska W, Koziej M, Hołda MK, Piątek K, Wszołek K, Tyszka A, Kmiotek E, Pliszko M, Śliwińska A, Krauss K et al (2015) Anthropometry and body composition of adolescents in Cracow, Poland. PLoS ONE 10(3):e0122274. 10.1371/journal.pone.0122274 [DOI] [PMC free article] [PubMed]
- 50.Zadarko-Domaradzka M, Sobolewski M, Nizioł-Babiarz E, Barabasz Z, Warchoł K, Niewczas-Czarna K, Zadarko E (2023) An investigation of the utility of waist circumference predicting cardiorespiratory fitness in school children: a cross-sectional study. Int. J. Environ. Res. Public Health 20(1):851. 10.3390/ijerph20010851 [DOI] [PMC free article] [PubMed]
- 51.Wright CM. Booth IW, Buckler JMH, Cameron M, Cole TJ, Healy MJR, Hulse JA, Preece MA, Reilly JJ, Williams AF (2002) Growth reference charts for use in the United Kingdom. Arch Dis Child 86(1):11–14. 10.1136/adc.86.1.11 [DOI] [PMC free article] [PubMed]
- 52.Damanhoury S, Newton AS, Rashid M, Hartling L, Byrne JLS, Ball GDC (2018) Defining metabolically healthy obesity in children: a scoping review: MHO definition in Children. Obes Rev 19(11):1476–1491. 10.1111/obr.12721 [DOI] [PubMed]
- 53.Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, Urbina EM, Ewing LJ, Daniels SR (2013) Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation 128(15):1689–1712. 10.1161/CIR.0b013e3182a5cfb3 [DOI] [PubMed]
- 54.Genovesi S, Antolini L, Orlando A, Gilardini L, Bertoli S, Giussani M, Invitti C, Nava E, Battaglino MG, Leone A et al (2020) Cardiovascular risk factors associated with the metabolically healthy obese (MHO) phenotype compared to the metabolically unhealthy obese (MUO) phenotype in children. Front Endocrinol 11:27. 10.3389/fendo.2020.00027 [DOI] [PMC free article] [PubMed]
- 55.Aldhoon-Hainerová I, Hainer V, Zamrazilová H (2017) Impact of dietary intake, lifestyle and biochemical factors on metabolic health in obese adolescents. Nutr Metab Cardiovasc Dis 27(8):703–710. 10.1016/j.numecd.2017.05.002 [DOI] [PubMed]
- 56.Vukovic R, Dos Santos TJ, Ybarra M, Atar M (2019) Children with metabolically healthy obesity: a review. Front Endocrinol 10:865. 10.3389/fendo.2019.00865 [DOI] [PMC free article] [PubMed]
- 57.Bermúdez V, Rojas J, Salazar J, Añez R, Toledo A, Bello L, Apruzzese V, González R, Chacín M, Cabrera M et al (2015) Sensitivity and specificity improvement in abdominal obesity diagnosis using cluster analysis during waist circumference cut-off point selection. J Diabetes Res 2015:1–14. 10.1155/2015/750265 [DOI] [PMC free article] [PubMed]
- 58.Guzmán-García JM, Romero-Saldaña M, Molina-Recio G, Álvarez-Fernández C, Raya-Cano E, Molina-Luque R (2022) Diagnostic accuracy of the waist-to-height ratio and other anthropometric indices for metabolically healthy obesity in the working population. Front Nutr 9:962054. 10.3389/fnut.2022.962054 [DOI] [PMC free article] [PubMed]
- 59.Buchan DS, Boddy LM, Grace FM, Brown E, Sculthorpe N, Cunningham C, Murphy MH, Dagger R, Foweather L, Graves LEF et al (2017) Utility of three anthropometric indices in assessing the cardiometabolic risk profile in children. Am J Hum Biol 29(3). 10.1002/ajhb.22934 [DOI] [PubMed]
- 60.Ezzatvar Y, Izquierdo M, Ramírez‐Vélez R, Pozo Cruz B, García‐Hermoso A (2022) Accuracy of different cutoffs of the waist‐to‐height ratio as a screening tool for cardiometabolic risk in children and adolescents: a systematic review and meta‐analysis of diagnostic test accuracy studies. Obes Rev 23(2). 10.1111/obr.13375 [DOI] [PubMed]
- 61.Eslami M, Pourghazi F, Khazdouz M, Tian J, Pourrostami K, Esmaeili-Abdar Z, Ejtahed HS, Qorbani M (2023) Optimal cut-off value of waist circumference-to-height ratio to predict central obesity in children and adolescents: a systematic review and meta-analysis of diagnostic studies. Front Nutr 9:985319. 10.3389/fnut.2022.985319 [DOI] [PMC free article] [PubMed]
- 62.Cameron AJ, Romaniuk H, Orellana L, Dallongeville J, Dobson AJ, Drygas W, Ferrario M, Ferrieres J, Giampaoli S, Gianfagna F et al (2020) Combined influence of waist and hip circumference on risk of death in a large cohort of European and Australian adults. J Am Heart Assoc 9(13):e015189. 10.1161/JAHA.119.015189 [DOI] [PMC free article] [PubMed]
- 63.Moreno LA, Mesana MI, González-Gross M, Gil CM, Ortega FB, Fleta J, Wärnberg J, León J, Marcos A, Bueno M (2007) Body fat distribution reference standards in Spanish adolescents: the AVENA Study. Int J Obes 31(12):1798–1805. 10.1038/sj.ijo.0803670 [DOI] [PubMed]
- 64.McCarthy HD, Rigby RA, Stasinopoulos DM (2010) Hip circumference percentile curves for the UK child and youth population. Proc Nutr Soc 69(OCE6):E424. 10.1017/S0029665110002879
- 65.Li Y, Zou Z, Luo J, Ma J, Ma Y, Jing J, Zhang X, Lou C, Wang H, Zhao C et al (2020) The predictive value of anthropometric indices for cardiometabolic risk factors in Chinese children and adolescents: a national multicenter school-based study. PLoS ONE 15(1):e0227954. 10.1371/journal.pone.0227954 [DOI] [PMC free article] [PubMed]
- 66.Chiolero A, Paradis G, Maximova K, Burnier M, Bovet P (2013) No use for waist-for-height ratio in addition to body mass index to identify children with elevated blood pressure. Blood Press 22(1):17–20. 10.3109/08037051.2012.701376 [DOI] [PubMed]
- 67.Arellano-Ruiz P, García-Hermoso A, García-Prieto JC, Sánchez-López M, Martínez Vizcaíno V, Solera-Martínez M (2020) Predictive ability of waist circumference and waist-to-height ratio for cardiometabolic risk screening among Spanish children. Nutrients 12(2):415. 10.3390/nu12020415 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request sent to the corresponding author. Sharing of data might be considered for specific research projects, based upon study protocol ethically accepted.