Dear Editor,
ROHHADNET syndrome comprises rapid-onset obesity, hypothalamic dysfunction, hypoventilation, and autonomic dysfunction.[1,2] We present a case of ROHHADNET syndrome posted for excision of thoracic ganglioneuroma thoracoscopically, after receiving written and informed consent from the parents.
A 4.5-year-old girl weighing 22.4 kg and of 98 cm height was diagnosed with ROHHADNET syndrome. She presented with rapid weight gain, untreated stage II hypertension, and right eye divergent squint. Magnetic resonance imaging (MRI) revealed a left thoracic paravertebral neural crest tumour close to the aortic arch and left subclavian artery, from thoracic vertebrae D2 to D5 (2.3 × 2.5 × 3.8 cm), with extradural spinal cord extension and diffuse cerebellar atrophy [Figure 1]. Thoracoscopic excision was planned, given the progression of the disease to paraneoplastic cerebellitis and impending spinal cord compression.
Figure 1.
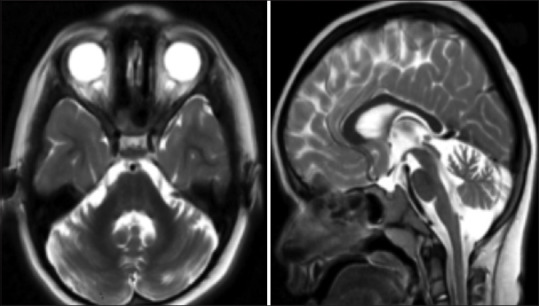
Axial and sagittal view of the brain revealing diffuse cerebellar atrophy and paraneoplastic cerebellitis
The child was premedicated with intravenous ketamine 0.5 mg/kg, glycopyrrolate 0.005 mg/kg, and midazolam 0.02 mg/kg and underwent monitoring in the preoperative area. Anaesthesia induction with intravenous fentanyl 0.002 mg/kg, propofol 2 mg/kg, and atracurium 0.5 mg/kg followed by tracheal intubation with a microcuff endotracheal tube of 4.5- mm internal diameter was done. The right radial artery and right internal jugular vein were cannulated, and an epidural catheter was placed at T7-8 interspace. For deflation of the left lung, the endotracheal tube was passed into the right mainstem bronchus over a neonatal bronchoscope having an internal diameter of 2.8 mm (Karl Storz -Endoskope. KARL STORZ SE & Co. KG. 3478532 Tuttlingen/Germany) and was fixed at 15 cm at the angle of the mouth after confirmation of air entry. The child was laid in the semi-prone position with adequate padding of pressure points [Figure 2]. Intrathoracic pressure was maintained between 4 and 6 cm H2O. Anaesthesia was maintained using 1.2% sevoflurane with oxygen and air and atracurium boluses. Positive pressure ventilation was maintained with an inspiratory pressure of 20 cm H2O, positive end expiratory pressure of 5 cm H2O, fractional inspired oxygen of 1 (to begin with and which was then reduced to 0.7), a respiratory rate of 30 breaths/min (targeting an oxygen saturation of 93%–95%), and end-tidal carbon dioxide of 35–40 mm Hg. Serial arterial blood gas analysis was done to confirm the adequacy of ventilation. The patient’s haemodynamics remained stable throughout the five-hour surgery, with the patient experiencing a blood loss of 100 ml. An intercostal drain was inserted on the left side, and surgical incisions were sutured. The tracheal tube was withdrawn, fixed at 13 cm, and bilateral lung ventilation was confirmed. Lung recruitment was done using continuous positive airway pressure of 30 cm H2O for 20 seconds. The child was shifted to the paediatric critical care unit and extubated after an hour.
Figure 2.

Positioning of the child with adequate padding
The multiorgan involvement associated with ROHHADNET syndrome offers a set of challenges for an anaesthesiologist, including airway difficulty (owing to obesity), autonomic dysfunction, adrenocortical insufficiency, etc.[3,4] Judicious use of premedication is needed as these patients are prone to experiencing hypoventilation due to a lack of neural responsiveness to hypoxemia and hypercarbia. Drugs which are opioid sparing, have shorter half life and that have minimal respiratory depressant effect should be preferred.
Neuraxial blocks should be given cautiously to patients with autonomic dysfunction because sympathetic blockade may lead to profound hypotension and bradycardia. Other concerns include hypothermia or hyperthermia, delayed gastric emptying, inadequate response to blood loss, and resistance to vasopressors/inotropes.[1] Invasive monitoring and strict vigilance are required due to an increased risk of sudden cardiorespiratory arrest.[3] Due to adrenocortical insufficiency, they may require perioperative steroid coverage.[5] Postoperative monitoring in critical care setup is advisable because of the increased risk of postoperative hypoventilation with carbon dioxide retention, thermal dysregulation, and labile haemodynamics.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lazea C, Sur L, Florea M. ROHHAD (Rapid-onset obesity with hypoventilation, hypothalamic dysfunction, autonomic dysregulation) syndrome—What every pediatrician should know about the etiopathogenesis, diagnosis and treatment: A review. Int J Gen Med. 2021;14:319–26. doi: 10.2147/IJGM.S293377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ibanez-Mico S, Marcos Oltra AM, de Murcia Lemauviel S, Ruiz Pruneda R, Martínez Ferrández C, Domingo Jiménez R. Rapid-onset obesity with hypothalamic dysregulation, hypoventilation, and autonomic dysregulation (ROHHAD syndrome): A casereport and literature review. Neurología. 2017;32:616–22. doi: 10.1016/j.nrl.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Isasa EE, Rodríguez PMA, Bambaren AI, Viñas MC, Mayo GD, Pérez DF, et al. Anesthesia in a pediatric patient with ROHADD syndrome. Rev Esp Anestesiol Reanim (Engl Ed) 2018;65:525–529. doi: 10.1016/j.redar.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Solanki SL, Karan N, Parab SY. Obstructive sleep apnoea and its knowledge and attitude among Indian anaesthesiolgists - A survey study. Indian J Anaesth. 2019;63:648–52. doi: 10.4103/ija.IJA_183_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goykhman A, Fitch J, Tobias JD. Perioperative care of a child with ROHHADNET syndrome. J Med Cases. 2013;4:710–4. [Google Scholar]


