Abstract
Thyroid hormone status has long been implicated in cancer development. Here we investigated the role of thyroxine (T4) in colorectal cancer cell lines HCT 116 (APC wild type) and HT-29 (APC mutant), as well as the primary cultures of cancer cells derived from patients. Cell proliferation was evaluated with standard assay and proliferation marker expression. β-Catenin activation was examined according to nuclear β-catenin accumulation and β-catenin target gene expression. The results showed that T4 increased colorectal cancer cell proliferation while cell number and viability were elevated by T4 in both established cell lines and primary cells. Moreover, the transcriptions of proliferative genes PCNA, CCND1, and c-Myc were enhanced by T4 in the primary cells. T4 induced nuclear β-catenin accumulation, as well as high cyclin D1 and c-Myc levels compared to the untreated cells. In addition, the β-catenin-directed transactivation of CCND1 and c-Myc promoters was also upregulated by T4. CTNNB1 transcription was raised by T4 in HCT 116, but not in HT-29, while the boosted β-catenin levels were observed in both. Lastly, the T4-mediated gene expression could be averted by the knockdown of β-catenin. These results suggested that T4 promotes β-catenin activation and cell proliferation in colorectal cancer, indicating that an applicable therapeutic strategy should be considered.
Electronic supplementary material
The online version of this article (10.1007/s12672-018-0324-y) contains supplementary material, which is available to authorized users.
Keywords: Thyroid Hormone Status, Colorectal Cancer Cell Lines, Proliferation Marker Expression, Proliferating Cell Nuclear Antigen (PCNA)
Introduction
Annually, colorectal cancer resulted in an estimated 694,000 deaths and nearly 1.4 million cases were reported worldwide [1]. In spite of recent advances in the understanding of molecular pathogenesis and the development of targeted treatments, colorectal cancer has remained one of the most frequently occurring and deadly cancers for more than 40 years.
Being the crucial hormones regulating growth, metabolism, and various physiological processes in human bodies, thyroid hormones l-thyroxine (T4) and triiodothyronine (T3) have long been implicated in cancer risks and tumor developments [2, 3]. In a prospective study of 29,691 people, circulating thyrotropin level suggestive of hyperthyroid function was related to an increased cancer risk [4]. The elevated cancer risk was mainly due to risks for colon (hazard ratio 1.38), lung (hazard ratio 2.34), breast (hazard ratio 1.20), and prostate (hazard ratio 1.97) cancers. In a later nested case-control study using a large population-based medical records database, hyperthyroidism (adjusted odds ratio 1.21), along with untreated hypothyroidism (adjusted odds ratio 1.16), were also associated with the increased risk of colorectal cancer [5]. Furthermore, T4 significantly raised tumor incidence in an animal model with chemically induced colorectal cancer, possibly resulting from its proliferation promoting effect in the colon mucosa epithelial cells during carcinogen administration [6]. In the colorectal cancer cell lines, the expressions of several proliferation markers including proliferating cell nuclear antigen (PCNA), cyclin D1, and c-Myc were enhanced in response to T4 exposure at both mRNA and protein levels [7]. Consequently, non-agonist T4 analogues were able to suppress the proliferation of these colorectal cancer cells.
In colorectal tumorigenesis, aberrant Wnt/β-catenin signaling is a major force driving uncontrolled cell growth and proliferation [8]. β-Catenin is normally phosphorylated and destined for proteasomal degradation by a cytoplasmic complex comprising axin, adenomatous polyposis coli (APC), and glycogen synthase kinase 3β (GSK3β). Upon stimulation, the stabilized β-catenin accumulates in cytoplasm and migrates into nucleus, where it functions as a transcriptional co-activator for responding targets such as cell cycle genes cyclin D1 and c-Myc. Mounting evidence points that Wnt/β-catenin pathway, which is involved in both tissue homeostasis and oncogenic progression, is linked to thyroid hormone and its downstream signaling. In the intestinal epithelial cells, T3-activated nuclear thyroid hormone receptor α1 (TRα1) directly modulated murine β-catenin gene ctnnb1 at transcriptional level and β-catenin pathway [9, 10]. However, T3-bound nuclear thyroid hormone receptor β1 (TRβ1) inhibited the transactivation of CCND1 (cyclin D1 gene) promoter through Tcf/Lef-1 site in a β-catenin dependent manner [11]. In addition, type 3 deiodinase (D3) that inactivates both T4 and T3 was found to be a direct transcriptional target of β-catenin and to be over-expressed in intestinal adenomas and carcinomas [12]. Without D3, excessive T3 reduced proliferation and enhanced differentiation via E-cadherin induction in both colorectal cancer cell lines and xenograft models. In agreement with the previous reports, recent microarray data showed that T3 treatment downregulated the transcription of Wnt targets and upregulated the transcription of Wnt negative regulators in the colorectal cancer stem cells; at the same time, lower tumorigenic potential and higher sensitivity to conventional chemotherapeutics were also observed [13].
The contradicting results indicate that the interplay between thyroid hormones, β-catenin signaling, and colorectal cancer is not yet fully understood to date. In the present study, we sought to investigate whether T4 could promote colorectal cancer cell proliferation and activate β-catenin, a crucial driver in proliferative process. The effects of T4 on proliferation in both colorectal cancer cell lines and primary cultures of cancer cells were examined based on proliferation assays and proliferation marker expressions. The activation of β-catenin in response to T4 exposure was evaluated according to the nuclear accumulation of β-catenin and the expression of β-catenin target genes. Expression profiles of β-catenin under T4 treatment in the colorectal cancer cell lines with different APC mutation status were also addressed. The study demonstrated the proliferation-accelerating role of T4 in the colorectal cancer cells and suggested that the thyroid hormone status and an applicable therapeutic strategy should be considered in colorectal cancer.
Materials and Methods
Cell Culture
Human colorectal cancer cell lines HCT 116 (ATCC® CCL-247™) and HT-29 (ATCC® HTB-38™) were obtained from American Type Culture Collection (ATCC) (Manassas, VA, USA). Cells were routinely maintained in RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS), as well as 1× penicillin-streptomycin, and grown under an atmosphere of 5% CO2/95% air at 37 °C. Prior to T4 (T1775 SIGMA, Sigma-Aldrich, St. Louis, MO, USA) treatments, cells were serum-starved for 48 h and serum-free medium was then replaced by the 10% hormone-stripped FBS containing medium.
The human colorectal cancer cells for primary culture were obtained from colorectal cancer patients admitted according to the standardized diagnostic criteria (Division of Colorectal Surgery, Department of Surgery, Shuang-Ho Hospital, Taipei Medical University, Taipei, Taiwan). The enrolled patients received no chemotherapy or radiation therapy prior to surgeries and provided the written informed consents to protocol approved by Taipei Medical University-Joint Institutional Review Board (TMU-JIRB) (TMU-JIRB number: N201603078) (Supplementary Material-JIRB Approval, with original certificate in Chinese on page 1 and the translated certificate in English on page 2). All experiments were performed in accordance with relevant guidelines and regulations. In brief, clinical samples (biopsies) were washed with phosphate buffered saline supplemented with 5× penicillin-streptomycin-amphotericin B, cut into 0.5–2.0 mm3 pieces, and then incubated with digestion medium containing 300 units/ml of type I collagenase and 20 μg/ml of hyaluronidase at 37 °C for 3 h. Subsequently, cell suspensions were filtered through 70 μm cell strainers (Thermo Fisher Scientific, Waltham, MA, USA), washed with culture medium, and then incubated with ammonium chloride-Tris solution (pH 7.2) at 4 °C to remove erythrocyte contamination. Finally, the recovered cell populations were maintained for treatments as the established cell lines and studied within five passages while cell morphology remained unchanged.
Cell Count Analysis
The human colorectal cancer cell lines (105 cells per well) or the primary cells (104 cells per well) were seeded onto six-well plates. At the indicated time points, the treated cells were collected and cell number in each well was calculated using Countess™ cell counting chamber slides and the automated cell counter (Invitrogen, Carlsbad, CA, USA).
Western Blotting
To examine protein expressions, the nucleus/cytoplasm compartments were separated using NE-PER® nuclear and cytoplasmic extraction reagents (Thermo Fisher Scientific, Waltham, MA, USA) following the manufacturer’s instructions and the whole cell lysates were extracted by radioimmunoprecipitation assay buffer supplemented with 1× complete protease inhibitor cocktail (F. Hoffmann-La Roche AG, Basel, Switzerland). The equal micrograms of protein samples in equal volumes were resolved on 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis gels via electrophoresis carried out at 100 V for 2 h. Proteins were then transferred from gels onto nitrocellulose blotting membranes (GE Healthcare, Chicago, IL, USA) using Trans-Blot® SD semi-dry transfer cell (Bio-Rad Laboratories, Inc., Hercules, CA, USA). After blocking with 2% BSA in TBST at room temperature for 1 h, membranes were incubated at 4 °C overnight with the primary antibodies specific to β-catenin (BD Biosciences, Franklin Lakes, NJ, USA), Lamin B (GeneTex, Inc., Hsinchu, Taiwan), cyclin D1 (Santa Cruz Biotechnology, Inc., Dallas, TX, USA), c-Myc (Santa Cruz Biotechnology, Inc., Dallas, TX, USA), and α-tubulin (Novus Biologicals, Littleton, CO, USA). Subsequently, the corresponding horseradish peroxidase-conjugated secondary antibodies were applied onto membranes at room temperature for 1 h. Protein detection was then carried out with Amersham™ ECL™ Western Blotting Detection Reagents (GE Healthcare, Chicago, IL, USA) and Amersham™ Imager 600 (GE Healthcare, Chicago, IL, USA). In nuclear and total protein examinations, the internal controls for data quantification were Lamin B1 and α-tubulin, respectively.
ChIP
Chromatin immunoprecipitation (ChIP) study was performed as previously described [14], using Dynabeads® Protein A (Thermo Fisher Scientific, Waltham, MA, USA) following the manufacturer’s instructions. The sonicated DNA fragments were immunoprecipitated by the antibodies specific to β-catenin (BD Biosciences, Franklin Lakes, NJ, USA)/normal mouse IgG (Santa Cruz Biotechnology, Inc., Dallas, TX, USA) and purified via GenepHlow™ Gel/PCR Kit (Geneaid Biotech Ltd., New Taipei City, Taiwan), as instructed. qPCR reactions, described in detail in next section, were conducted to analyze specific DNA fragments using the previously reported primer sequences targeting the promoter regions of interests: CCND1 promoter forward 5′-CCGGGCTTTGATCTTTGCTTA-3′ and reverse 5′-TCTGCTGCTCGCTGCTACTG-3′; c-Myc promoter forward 5′-GCGGGTTACATACAGTGCACTTCA-3′ and reverse 5′-TGGAAATGCGGTCATGCACAAA-3′ [15].
qPCR
Total RNA was extracted using illustra RNAspin Mini RNA Isolation Kit (GE Healthcare, Chicago, IL, USA), following the manufacturer’s instructions. One microgram of total RNA (genomic DNA-free) was reverse-transcribed by RevertAid H Minus First Strand cDNA Synthesis Kit (Thermo Fisher Scientific, Waltham, MA, USA) into cDNA, which was later used as PCR templates as instructed. Reactions were performed via QuantiNova™ SYBR® Green PCR Kit (Qiagen, Hilden, Germany) and a CFX Connect™ Real-Time PCR Detection System (Bio-Rad Laboratories, Inc., Hercules, CA, USA), according to the provided protocols. Primer sequences were as follows: 18S rRNA forward 5′-GTAACCCGTTGAACCCCATT-3′ and reverse 5′-CCATCCAATCGGTAGTAGCG-3′ (accession no.: NR_003286.2); CTNNB1 forward 5′-CTGGTCCTTTTTGGTCGAGGA-3′ and reverse 5′-GCAAGGCTAGGGTTTGCTAAAT-3′ (accession no.: NM_001904.3); PCNA forward 5′-TCTGAGGGCTTCGACACCTA-3′ and reverse 5′-TCATTGCCGGCGCATTTTAG-3′ (accession no.: NM_002592.2); CCND1 forward 5′-CAAGGCCTGAACCTGAGGAG-3′ and reverse 5′-GATCACTCTGGAGAGGAAGCG-3′ (accession no.: NM_053056.2); c-Myc forward 5′-TTCGGGTAGTGGAAAACCAG-3′ and reverse 5′-CAGCAGCTCGAATTTCTTCC-3′ (accession no.: NM_002467.4). Relative gene expression normalized to the internal control 18S rRNA was calculated based on ΔΔCT method, and the fidelity of PCR reactions was determined using melting temperature analysis.
siRNA Transfection
The human colorectal cancer cells were seeded onto six-well plates (105 cells per well). Prior to transfections, culture medium was replaced by serum-free medium and cells were transfected with 100 nM of SignalSilence® Control siRNA or SignalSilence® β-Catenin siRNA I (Cell Signaling Technology, Danvers, MA, USA) using Lipofectamine® 3000 Transfection Kit (Invitrogen, Carlsbad, CA, USA) following the manufacturer’s instructions. The 10% hormone-stripped FBS containing medium was added 6 h after transfections, and cells were incubated as usual for 48 h. Medium was then refreshed, and T4 was applied 24 h before sample collections.
Data Analysis and Statistics
Data were analyzed using IBM SPSS Statistics 19 (SPSS, Inc., Chicago, IL, USA) and graphed by GraphPad Prism 6 (GraphPad Software, Inc., La Jolla, CA, USA). Statistical significance was determined by applying Mann-Whitney U test for qPCR data and Student’s t test for the rest of experiments. The results with P value ≤ 0.05 were considered significant.
Results
Thyroid Hormone T4 Promotes Cell Proliferation in Colorectal Cancer Cell Lines HCT 116 and HT-29
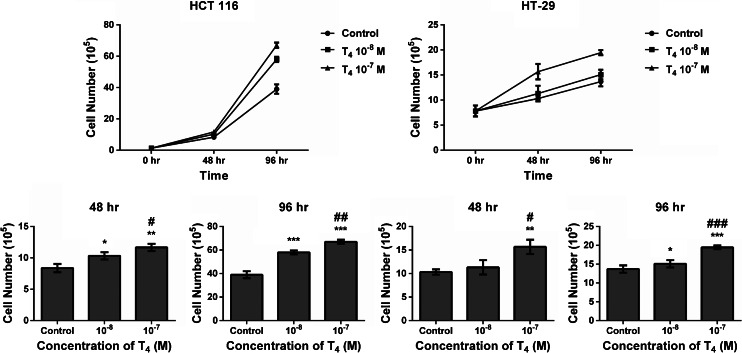
Given that T4 altered the expressions of numerous proliferative and pro-apoptotic genes [7], we first examined the effects of thyroid hormone T4 on cell number and viability over time in colorectal cancer cell lines HCT 116 and HT-29 (Fig. 1). In both cell lines, the numbers of live cells in the T4 (10−8 and 10−7 M)-treated groups were substantially higher than the control cells after 48 and 96 h while 10−7 M of T4 significantly elevated cell numbers more than 10−8 M of T4 (Fig. 1). With an alternative method MTT assay (Supplementary Materials and Methods), the exposures to 10−8 and 10−7 M of T4 in HCT 116 cells also significantly increased absorbance, an index of mitochondria activity, to 1.27- and 1.43-fold compared to the control cells (Supplementary Fig. 1, left panel). In HT-29 cells, absorbance was significantly raised to 1.27- and 1.41-fold in the T4 (10−8 and 10−7 M)-treated cells compared to the control cells (Supplementary Fig. 1, right panel). T4 at 10−7 M exhibited greater effects than 10−8 M, but statistical significance was only observed in HCT 116 cells (Supplementary Fig. 1).
Fig. 1.
Thyroid hormone T4 promotes cell proliferation in colorectal cancer cell lines HCT 116 and HT-29. Cells treated with/without T4 were collected at the indicated time points and counted. Data represent at least three independent experiments performed in replicates and are presented as mean ± sd (n = 3). *P ≤ 0.05, **P ≤ 0.01, and ***P ≤ 0.001 compared to the control group. #P ≤ 0.05, ##P ≤ 0.01, and ###P ≤ 0.001 compared to the T4 (10−8 M) group
Thyroid Hormone T4 Modulates β-Catenin Activation and Expression in Colorectal Cancer Cell Lines HCT 116 and HT-29
To evaluate T4 effects on β-catenin pathway, we measured the nuclear accumulation of β-catenin, the levels of β-catenin target genes, and the transactivation of β-catenin target promoters in response to T4 treatment in colorectal cancer cell lines HCT 116 (APC wild type) and HT-29 (APC mutant) (Fig. 2). The results showed that the addition of 10−8 and 10−7 M of T4 to HCT 116 cells significantly elevated nuclear β-catenin to 1.28- and 1.58-fold compared to the control cells (Fig. 2a, left panel). β-Catenin abundances in nucleus in HT-29 cells were 1.13- and 1.61-fold significantly higher in the T4 (10−8 and 10−7 M)-treated cells (Fig. 2a, right panel). The T4-induced increases of nuclear β-catenin occurred with T4 dosages in both cell lines (Fig. 2a). Moreover, the levels of cyclin D1 and c-Myc significantly increased with T4 concentrations (10−8 and 10−7 M) compared to the control cells in both HCT 116 and HT-29 cells (Fig. 2b). In APC wild-type HCT 116 cells, T4 (10−7 M) was able to significantly raise the interaction between β-catenin and CCND1 promoter region to 2.80-fold compared to the control cells, whereas WNT3A recombinant protein (25 ng/ml) caused a 3.47-fold enhancement (Fig. 2c, left panel). The interactions between β-catenin and c-Myc promoter region were also significantly boosted by T4 and WNT3A to 2.58- and 3.14-fold, respectively (Fig. 2c, right panel).
Fig. 2.
Thyroid hormone T4 induces β-catenin activation in colorectal cancer cell lines HCT 116 and HT-29. a Cells treated with/without T4 were collected after 24 h for western blotting and the nuclear fractions were examined. Images are representative, with statistics from at least three independent experiments shown below (HCT 116 n = 6; HT-29 n = 7). Data are normalized to the internal control Lamin B1 and presented as mean ± sd. *P ≤ 0.05 and ***P ≤ 0.001 compared to the control group. #P ≤ 0.05, ##P ≤ 0.01, and ###P ≤ 0.001 compared to the T4 (10−8 M) group. C control. b Cells treated with/without T4 were collected after 24 h for western blotting, and the whole cell lysates were examined. Images are representative, with statistics from at least three independent experiments shown below (HCT 116 n = 5; HT-29 n = 7). Data are normalized to the internal control α-tubulin and presented as mean ± sd. *P ≤ 0.05 and ***P ≤ 0.001 compared to the control group. ##P ≤ 0.01 and ###P ≤ 0.001 compared to the T4 (10−8 M) group. C control. c HCT 116 cells treated with either T4 (10−7 M) or WNT3A (25 ng/ml) were evaluated after 24 h by ChIP study. Data are normalized to the control cells and presented as mean ± sd from at least three independent experiments performed in replicates (n = 10). *P ≤ 0.05 and ***P ≤ 0.001 compared to the control group
Being a Wnt/β-catenin target itself, the mRNA expression of CTNNB1 (β-catenin gene) was significantly elevated by T4 at 10−8 and 10−7 M to 1.14- and 1.41-fold compared to the control cells in APC wild-type HCT 116 cells (Fig. 3a, left panel) whereas expression was unchanged in HT-29 cells bearing APC mutation (Fig. 3a, right panel). The higher concentration of T4 (10−7 M) presented a significantly stronger effect than the lower concentration of T4 (10−8 M) (Fig. 3a, left panel). Nevertheless, the considerable increases of total β-catenin levels in response to 10−8 and 10−7 M of T4 were observed in both HCT 116 and HT-29 cells (Fig. 3b).
Fig. 3.
Thyroid hormone T4 modulates β-catenin expression in colorectal cancer cell lines HCT 116 and HT-29. a Cells treated with/without T4 were collected after 24 h, and the mRNA expression of CTNNB1 was examined using qPCR. Data are normalized to the internal control 18S rRNA and presented as mean ± sd from at least three independent experiments performed in replicates (HCT 116 n = 5; HT-29 n = 6). *P ≤ 0.05 and **P ≤ 0.01 compared to the control group. #P ≤ 0.05 compared to the T4 (10−8 M) group. b Cells treated with/without T4 were collected after 24 h for western blotting, and the whole cell lysates were examined. Images are representative, with statistics from at least three independent experiments shown below (HCT 116 n = 4; HT-29 n = 3). Data are normalized to the internal control α-tubulin and presented as mean ± sd. *P ≤ 0.05 and **P ≤ 0.01 compared to the control group. ##P ≤ 0.01 compared to the T4 (10−8 M) group. C control
Thyroid Hormone T4 Stimulates Cell Proliferation and β-Catenin Activation in the Primary Cultures of Cancer Cells Derived from Colorectal Cancer Patients
Since T4 induced cell proliferation and β-catenin activation in colorectal cancer cell lines HCT 116 and HT-29, we determined whether these effects could be reproduced in the primary cells derived from two different colorectal cancer patients (Figs. 4 and 5). In the primary cultures of cancer cells derived from both patients, the numbers of T4 (10−7 M)-treated cells were substantially higher than the control cells after 96 h, with statistical significance achieved in the cells from patient 2 (Fig. 4). Furthermore, the mRNA expression of PCNA, CCND1, and c-Myc was significantly elevated by 10−7 M of T4 to 1.46- to 1.80-fold in comparison with the control cells from both patients (Fig. 5a). In the subsequent western blotting studies using the primary cells derived from patient 2, the T4-directed levels of nuclear β-catenin, cyclin D1, and c-Myc were 2.30-, 1.30-, and 2.15-fold markedly higher than in the control cells, respectively (Fig. 5b, c).
Fig. 4.
Thyroid hormone T4 promotes cell proliferation in the primary cultures of cancer cells derived from colorectal cancer patients. Cells treated with/without 10−7 M of T4 were collected after 96 h and counted. Data are representative from two independent experiments performed in replicates and presented as mean ± sd (patient 1 n = 2; patient 2 n = 3). ***P ≤ 0.001 compared to the control group
Fig. 5.
Thyroid hormone T4 induces β-catenin activation in the primary culture of cancer cells derived from colorectal cancer patients. a Cells treated with/without 10−7 M of T4 were collected after 24 h, and the mRNA expression of PCNA, CCND1, and c-Myc was examined using qPCR. Data are normalized to the internal control 18S rRNA and presented as mean ± sd from two independent experiments performed in replicates (n = 4). *P ≤ 0.05 compared to the control group. b Cells treated with/without 10−7 M of T4 were collected after 24 h for western blotting, and the nuclear fractions were examined. Images are representative, with statistics from two independent experiments shown below (n = 4). Data are normalized to the internal control Lamin B1 and presented as mean ± sd. *P ≤ 0.05 compared to the control group. C control. c Cells treated with/without 10−7 M of T4 were collected after 24 h for western blotting, and the whole cell lysates were examined. Images are representative, with statistics from two independent experiments shown below (n = 2). Data are normalized to the internal control α-tubulin and presented as mean ± sd. *P ≤ 0.05 compared to the control group. C control
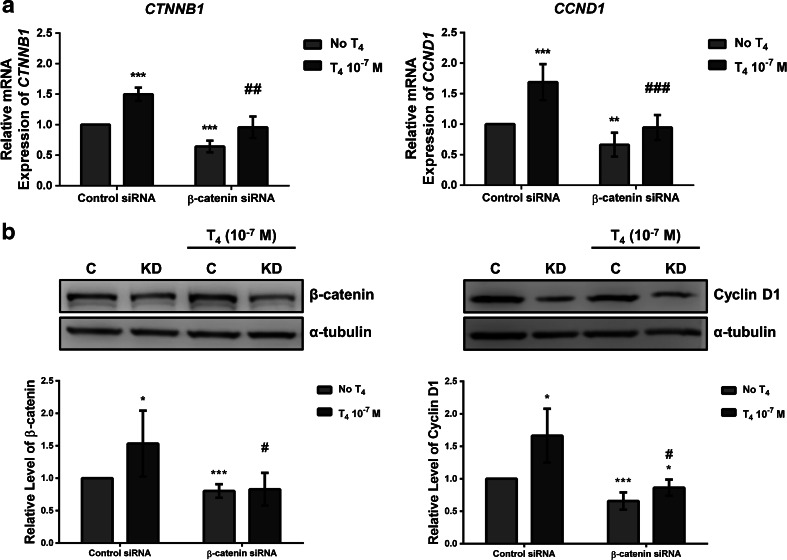
Knockdown of β-Catenin Suppresses Thyroid Hormone T4-Stimulated β-Catenin Activation in Colorectal Cancer Cell Line HCT 116
To verify β-catenin contribution to cell proliferation and β-catenin activation elevated by T4 in the colorectal cancer cells, we blocked β-catenin gene expression using β-catenin siRNA in colorectal cancer cell line HCT 116 and determined whether the knockdown was able to deplete T4 effects (Fig. 6). In the β-catenin siRNA transfected cells, the mRNA expression of CTNNB1 and CCND1 was significantly reduced to 0.64- and 0.66-fold compared to the control cells (Fig. 6a), while the protein levels of β-catenin and cyclin D1 were significantly lowered to 0.80- and 0.66-fold compared to the control cells (Fig. 6b). As 10−7 M of T4 significantly raised the mRNA expression of CTNNB1 and CCND1 in the control cells, T4 gave rise to the significantly lessened CTNNB1 and CCND1 transcription in the knockdown cells, compared to the T4-treated control cells (Fig. 6a). Similar patterns were also observed for the protein levels of β-catenin and cyclin D1 (Fig. 6b).
Fig. 6.
Knockdown of β-catenin suppresses thyroid hormone T4-stimulated β-catenin activation in colorectal cancer cell line HCT 116. Cells were transfected with control/β-catenin siRNA for 48 h and treated with/without 10−7 M T4 for another 24 h before collected. a The mRNA expression of CTNNB1 and CCND1 was examined using qPCR. Data are normalized to the internal control 18S rRNA and presented as mean ± sd from at least three independent experiments performed in replicates (CTNNB1 n = 9; CCND1 n = 7). **P ≤ 0.01 and ***P ≤ 0.001 compared to the untreated control group. ##P ≤ 0.01 and ###P ≤ 0.001 compared to the T4-treated control group. b The protein levels of β-catenin and cyclin D1 in the whole cell lysates were examined using western blotting. Images are representative, with statistics from at least three independent experiments shown below (β-catenin n = 9; cyclin D1 n = 5). Data are normalized to the internal control α-tubulin and presented as mean ± sd. *P ≤ 0.05 and ***P ≤ 0.001 compared to the untreated control group. #P ≤ 0.01 compared to the T4-treated control group. C control siRNA, KD β-catenin siRNA
Discussion
In order to elucidate the role of thyroid hormones (specifically, T4) in colorectal cancer, we aimed to look at its effect on cell proliferation and β-catenin activation, a key event involved in colorectal cancer progression. The study included two colorectal cancer cell lines HCT 116 and HT-29, as well as the primary cells derived from two different colorectal cancer patients. Notably, HCT 116 cells harbor wild-type APC while HT-29 cells bear mutant APC that results in a disruption of β-catenin degradation and the hyper-activation of Wnt/β-catenin cascade [8].
We have demonstrated here that cell proliferation in both colorectal cancer cell lines and primary cultures of cancer cells was enhanced in response to T4 within physiological range (10−8 and 10−7 M) (Figs. 1 and 4). Additionally, T4 increased cell viability in HCT 116 and HT-29 cells in a dose-dependent manner according to an alternative method MTT assay (Supplementary Fig. 1). As noted in a previous paper on the colorectal cancer cell lines [7], the physiological concentration of T4 elevated the mRNA abundance of PCNA, CCND1, and c-Myc in the primary cells derived from both colorectal cancer patients (Fig. 5a). The raised protein levels of cyclin D1 and c-Myc stimulated by T4 were also detected in one of the patients (Fig. 5c). Together with our previous findings, these results regarding cell number, cell viability, and proliferative marker expressions substantiated that T4 supports the proliferation of colorectal cancer cells.
Evidence has shown that thyroid hormone acts as a growth factor in cancers of various origins [2, 3]. These non-genomic actions of T4 occur via the binding between T4 and integrin αvβ3, a plasma membrane protein that contains the cell surface receptor for thyroid hormones. Consequently, the thyroid hormone-induced signaling transduction and oncogenic properties can be blocked by tetraiodothyroacetic acid (tetrac) and its nano-particulate derivative, the deaminated analogues of T4 that compete with T4 for integrin αvβ3 thyroid hormone binding site. In the colorectal cancer cell lines, combination treatment with tetrac and cetuximab potentiated the anticancer actions of cetuximab in terms of downregulated proliferative genes, upregulated apoptotic genes, and inhibited cell growth [7].
In colorectal cancer patients, nuclear β-catenin distribution—a hallmark of Wnt/β-catenin signaling—predicted progress disease and unfavorable survival [16]. The depletion of β-catenin nuclear translocation thus decelerated cancer progression and sensitized the cancer cells to PI3K/AKT inhibitors as well as radiation therapy [17, 18]. We have demonstrated in the current study that T4 positively mediated the nuclear localization of β-catenin, indicating the activation of β-catenin pathway, in both colorectal cancer cell lines and primary cell cultures (Figs. 2a and 5b). In agreement with β-catenin activation, the raised cyclin D1 and c-Myc levels in response to T4 application were displayed in these colorectal cancer cells (Figs. 2b and 5c). The physiological concentration of T4, as Wnt signaling ligand WNT3A, enhanced the transactivation of both CCND1 and c-Myc promoters directed by β-catenin in APC wild-type HCT 116 cells (Fig. 2c). One of the downstream targets of Wnt/β-catenin pathway, CTNNB1, underwent transcription induced by T4 in APC wild-type HCT 116 cells with dose-dependent manner, but not in APC mutant HT-29 cells that have the high background level of β-catenin (Fig. 3a). Nonetheless, the accumulation of β-catenin within cells that resulted from T4 exposure was observed in both established cell lines and was concentration-dependent (Fig. 3b). These data indicated that in the colorectal cancer cells with different APC status, the T4-mediated β-catenin activation involved different mechanisms. Last of all, the knockdown of β-catenin suppressed the T4-enhanced β-catenin and cyclin D1 expression at both mRNA and protein levels in colorectal cancer cell line HCT 116 (Fig. 6), pointing to the direct involvement of β-catenin pathway in the above described T4 effects.
A few contradicting results concerning proliferation and proliferation signaling in cancers derived from gastrointestinal tract have been noted previously and appear to be T3-depentdent in the contexts of receptors activated [9–13]. Instead of classical genomic actions directed by the T3-bound thyroid hormone receptors (TRα and TRβ), the cancer-promoting effects of thyroid hormones are mostly related to their cell surface receptor integrin αvβ3 and the function of circulating T4 [2, 3]. Being the major product secreted by thyroid gland, the amount of circulating T4 is far more than the amount of T3 and the integrin αvβ3 affinity for T4 is higher than the affinity for T3 [19]. It is therefore considered that the importance of T4 as a growth factor in cancer exceeds T3 [3]. These previous reports point out that T4 and T3 may possess distinct functions in colorectal cancer and the complex networks of thyroid hormones require further exploration. To sum up, we have provided evidence that in colorectal cancer, β-catenin pathway and cell proliferation are stimulated by thyroid hormone T4. Patients’ thyroid hormone status might hence be playing a part in the therapeutic strategies of colorectal cancer.
Electronic Supplementary Material
(PDF 342 kb)
Acknowledgements
We appreciate excellent research techniques and endless efforts of Dr. Meng-Ti Hsieh and Ms. Hsuan-Yu Lai (Taipei Medical University, Taipei, Taiwan).
Funding Information
This work was supported in part by the grants from Ministry of Science and Technology, Taiwan (http://www.most.gov.tw) (Grant Numbers: MOST-103-2632-B-038-001, MOST-104-2314-B-038-046-MY3, and MOST-105-2320-B-038-006).
Compliance with Ethical Standards
The enrolled patients received no chemotherapy or radiation therapy prior to surgeries and provided the written informed consents to protocol approved by Taipei Medical University-Joint Institutional Review Board (TMU-JIRB) (TMU-JIRB number: N201603078) (Supplementary Material-JIRB Approval, with original certificate in Chinese on page 1 and the translated certificate in English on page 2). All experiments were performed in accordance with relevant guidelines and regulations.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Moeller LC, Fuhrer D. Thyroid hormone, thyroid hormone receptors, and cancer: a clinical perspective. Endocr Relat Cancer. 2013;20(2):R19–R29. doi: 10.1530/ERC-12-0219. [DOI] [PubMed] [Google Scholar]
- 3.Lin HY, Chin YT, Yang YC, Lai HY, Wang-Peng J, Liu LF, Tang HY, Davis PJ. Thyroid hormone, cancer, and apoptosis. Compr Physiol. 2016;6(3):1221–1237. doi: 10.1002/cphy.c150035. [DOI] [PubMed] [Google Scholar]
- 4.Hellevik AI, Asvold BO, Bjoro T, Romundstad PR, Nilsen TIL, Vatten LJ. Thyroid function and cancer risk: a prospective population study. Cancer Epidemiol Biomark Prev. 2009;18(2):570–574. doi: 10.1158/1055-9965.EPI-08-0911. [DOI] [PubMed] [Google Scholar]
- 5.Boursi B, Haynes K, Mamtani R, Yang YX. Thyroid dysfunction, thyroid hormone replacement and colorectal cancer risk. J Natl Cancer Inst. 2015;107(6):djv084. doi: 10.1093/jnci/djv084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iishi H, Tatsuta M, Baba M, Okuda S, Taniguchi H (1992) Enhancement by thyroxine of experimental carcinogenesis induced in rat colon by azoxymethane. Int J Cancer 50(6):974–976. 10.1002/ijc.2910500625 [DOI] [PubMed]
- 7.Lee YS, Chin YT, Yang YCSH, Wei PL, Wu HC, Shih A, Lu YT, Pedersen JZ, Incerpi S, Liu LF, Lin HY, Davis PJ. The combination of tetraiodothyroacetic acid and cetuximab inhibits cell proliferation in colorectal cancers with different K-ras status. Steroids. 2016;111:63–70. doi: 10.1016/j.steroids.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Tortelote GG, Reis RR, de Almeida Mendes F, Abreu JG. Complexity of the Wnt/betacatenin pathway: searching for an activation model. Cell Signal. 2017;40:30–43. doi: 10.1016/j.cellsig.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Plateroti M, Kress E, Mori JI, Samarut J. Thyroid hormone receptor alpha1 directly controls transcription of the beta-catenin gene in intestinal epithelial cells. Mol Cell Biol. 2006;26(8):3204–3214. doi: 10.1128/MCB.26.8.3204-3214.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kress E, Rezza A, Nadjar J, Samarut J, Plateroti M. The frizzled-related sFRP2 gene is a target of thyroid hormone receptor alpha1 and activates beta-catenin signaling in mouse intestine. J Biol Chem. 2009;284(2):1234–1241. doi: 10.1074/jbc.M806548200. [DOI] [PubMed] [Google Scholar]
- 11.Natsume H, Sasaki S, Kitagawa M, Kashiwabara Y, Matsushita A, Nakano K, Nishiyama K, Nagayama K, Misawa H, Masuda H, Nakamura H. Beta-catenin/Tcf-1-mediated transactivation of cyclin D1 promoter is negatively regulated by thyroid hormone. Biochem Biophys Res Commun. 2003;309(2):408–413. doi: 10.1016/j.bbrc.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Dentice M, Luongo C, Ambrosio R, Sibilio A, Casillo A, Iaccarino A, Troncone G, Fenzi G, Larsen PR, Salvatore D. Beta-catenin regulates deiodinase levels and thyroid hormone signaling in colon cancer cells. Gastroenterology. 2012;143(4):1037–1047. doi: 10.1053/j.gastro.2012.06.042. [DOI] [PubMed] [Google Scholar]
- 13.Catalano V, Dentice M, Ambrosio R, Luongo C, Carollo R, Benfante A, Todaro M, Stassi G, Salvatore D. Activated thyroid hormone promotes differentiation and chemotherapeutic sensitization of colorectal cancer stem cells by regulating Wnt and BMP4 signaling. Cancer Res. 2016;76(5):1237–1244. doi: 10.1158/0008-5472.CAN-15-1542. [DOI] [PubMed] [Google Scholar]
- 14.Carey, M.F., C.L. Peterson, and S.T. Smale. 2009. Chromatin immunoprecipitation (ChIP). Cold Spring Harb Protoc. 2009(9): p. pdb prot5279 [DOI] [PubMed]
- 15.Lee JM, Kim IS, Kim H, Lee JS, Kim K, Yim HY, Jeong J, Kim JH, Kim JY, Lee H, Seo SB, Kim H, Rosenfeld MG, Kim KI, Baek SH. RORalpha attenuates Wnt/beta-catenin signaling by PKCalpha-dependent phosphorylation in colon cancer. Mol Cell. 2010;37(2):183–195. doi: 10.1016/j.molcel.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Chen Z, et al. Beta-catenin overexpression in the nucleus predicts progress disease and unfavourable survival in colorectal cancer: a meta-analysis. PLoS One. 2013;8(5):e63854. doi: 10.1371/journal.pone.0063854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arques O, Chicote I, Puig I, Tenbaum SP, Argiles G, Dienstmann R, Fernandez N, Caratu G, Matito J, Silberschmidt D, Rodon J, Landolfi S, Prat A, Espin E, Charco R, Nuciforo P, Vivancos A, Shao W, Tabernero J, Palmer HG. Tankyrase inhibition blocks Wnt/beta-catenin pathway and reverts resistance to PI3K and AKT inhibitors in the treatment of colorectal cancer. Clin Cancer Res. 2016;22(3):644–656. doi: 10.1158/1078-0432.CCR-14-3081. [DOI] [PubMed] [Google Scholar]
- 18.Wang W, Wen Q, Luo J, Chu S, Chen L, Xu L, Zang H, Alnemah MM, Li J, Zhou J, Fan S. Suppression of beta-catenin nuclear translocation by CGP57380 decelerates poor progression and potentiates radiation-induced apoptosis in nasopharyngeal carcinoma. Theranostics. 2017;7(7):2134–2149. doi: 10.7150/thno.17665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergh JJ, Lin HY, Lansing L, Mohamed SN, Davis FB, Mousa S, Davis PJ. Integrin alphaVbeta3 contains a cell surface receptor site for thyroid hormone that is linked to activation of mitogen-activated protein kinase and induction of angiogenesis. Endocrinology. 2005;146(7):2864–2871. doi: 10.1210/en.2005-0102. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 342 kb)