Abstract
Cardiovascular disease (CVD) is the leading cause of mortality worldwide. Addressing social determinants of health (SDoH) may be the next forefront of reducing the enormous burden of CVD. SDoH can be defined as any social, economic, or environmental factor that influences a health outcome. Comprehensive evidence of the role of SDoH in CVD is lacking, nevertheless. This umbrella review aims to give a comprehensive overview of the role of SDoH in CVD. We searched systematic reviews (with or without meta‐analyses) using 8 databases and included review reference lists. Four themes (economic circumstances, social/community context, early childhood development, and neighbourhood/built environment) and health literacy in the health/health care theme were considered. Seventy reviews were eligible. Despite the quality of the included reviews being low or critically low, there was consistent evidence that factors relating to economic circumstances and early childhood development themes were associated with an increased risk of CVD and CVD mortality. We also found evidence that factors in the social/community context and neighbourhood/built environment themes, such as social isolation, fewer social roles, loneliness, discrimination, ethnicity, neighborhood socioeconomic status, violence, and environmental attributes, had a role in CVD. SDoH factors without (or with minimal) evidence synthesis for CVD were also identified. In sum, this umbrella review offers evidence that SDoH, especially economic circumstance and early childhood development, play a significant role in CVD. This calls for the strengthening of nonmedical interventions that address multiple factors simultaneously and the inclusion of SDoH in future CVD risk prediction models.
Registration
URL: https://www.crd.york.ac.uk/prospero/; Unique identifier: CRD42022346994.
Keywords: social context cardiovascular disease, social determinants of health, socioeconomic status, umbrella review
Subject Categories: Cardiovascular Disease, Chronic Ischemic Heart Disease, Cerebrovascular Disease/Stroke, Myocardial Infarction, Heart Failure
Nonstandard Abbreviations and Acronyms
- AMSTAR
Assessing the Methodological Quality of Systematic Review
- SDoH
social determinants of health
Cardiovascular disease (CVD) causes 17.9 million deaths worldwide annually. 1 Between 1990 and 2019, there was an alarming increase in total CVD morbidity and mortality. 2 CVD cases increased from 271 million in 1990 to 523 million in 2019, and CVD mortality increased from 12.1 million to 18.6 million. 2 CVD is a highly fatal condition; for instance, one person in the United States dies because of CVD every 34 seconds. 3
There has been increasing recognition that social determinants of health (SDoH) significantly contribute to morbidity, mortality, and health inequality. 4 , 5 , 6 , 7 According to the World Health Organization, SDoH are any situation or circumstance in which individuals are born, grow, live, work, and age. 8 , 9 SDoH can also be described as any environmental factor that affects a person's health, quality of life, or the progression of a disease in a complex and interconnected manner. 10 There are multiple theoretical frameworks for SDoH, such as the World Health Organization conceptual SDoH framework, 11 the social‐ecological framework, 12 and the Healthy People 2020 and 2030 frameworks. 13 , 14 According to Healthy People 2020 and 2030 frameworks, 13 , 14 SDoH are a broad concept and can be classified into 5 main domains/themes: economic stability, education access and quality, social and community context, neighbourhood and built environment, and health and health care domains. Economic stability includes employment/occupation, income, food insecurity, and housing instability. The education access and quality theme include early childhood development and enrollment in higher education. Social support, social capital, social isolation, loneliness, discrimination, and race and ethnicity all fall under the social and community context theme. The neighborhood and built environment theme contains neighborhood socioeconomic status (SES) and environmental attributes, such as food environment, conflict, and violence, whereas the health and health care theme is defined by access to health services, access to primary care, quality of care, health insurance coverage, and health literacy. 13 , 14
There are disparities in CVD occurrence and outcomes as a result of the complex and entangled relationships between SDoH and CVD. 15 , 16 SDoH do not necessarily have a 1‐way causal relationship with health; they can be considered as upstream factors (the causes of the causes). 17 For instance, during the course of a person's life, poor social health influences a variety of health behaviours, including substance abuse, being overweight, and eating poorly. 15 , 18 , 19 They are linked to well‐known traditional CVD risk factors as well. For example, there is evidence that SDoH are related to high blood pressure, inflammation, chronic stress, and excess cholesterol. 7 , 19 , 20 In addition, a lack of health literacy and difficulty in accessing medical services means that diseases are diagnosed late, which can lead to life‐threatening consequences, like mortality attributable to CVD. 7 , 21
Numerous systematic reviews and meta‐analyses have been conducted, focusing on the roles of specific SDoH characteristics in CVD, 22 , 23 , 24 , 25 , 26 and none of these has compared the evidence for different domains of SDoH and thus indicated which areas could best be targeted for the interventions. Besides, an umbrella review, also called an overview of reviews or a systematic review of systematic reviews, gathers data from earlier reviews to provide user‐friendly summaries for decision makers and, therefore, it is incredibly helpful to put the evidence into action. 27 , 28 Therefore, we aimed to provide the first comprehensive overview of the current evidence in the role of SDoH in CVD by undertaking an umbrella review.
METHODS
The Preferred Reporting Items for Overviews of Reviews, 29 a guideline for overviews of reviews of health care interventions, is used for reporting (Table S1). The protocol was registered in International Prospective Register of Systematic Reviews (registration number CRD42022346994).
Eligibility Criteria
Participants from the general population, at‐risk population groups, or both were included. There were no restrictions based on the demographic characteristics of participants, such as age and sex.
The exposure of interest for our review was SDoH. We first considered the SDoH factors and categorizations described in the Healthy People 2020 and 2030 frameworks, 13 , 14 as well as other literature. 7 , 19 , 30 , 31 , 32 As CVD occurs later in life, SDoH factors can be conceptualized as occurring before and directly contributing to CVD. The causal pathway is likely most clear for the SDoH in early childhood (specific to early childhood SES and adverse events related to abuse, neglect, and violence), and for this reason we considered it to be a stand‐alone theme. 30 There is evidence that economic stability and economic development of an individual or a society as a whole is correlated with education. 32 Furthermore, according to the American Psychological Association, 33 education is a measure of the SES along with income, social class, and financial security. We also followed the guidance of other literature 30 , 31 that has incorporated education into the economic stability theme, which we retitled economic circumstance. Hence, in this review we assessed SDoH under 4 themes: (1) economic circumstance; (2) social and community context; (3) early childhood development; and (4) neighbourhood and built environment. In addition, health literacy, which is considered part of the health and health care domain, was considered in this review (Figure 1).
Figure 1. Conceptual framework indicating the domains of the social determinants of health and their association with cardiovascular disease.
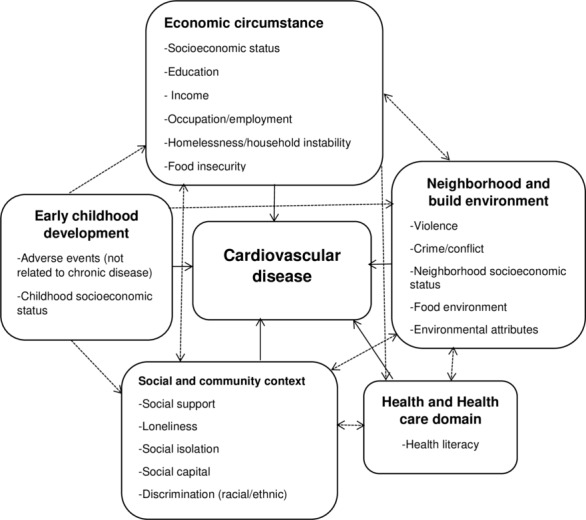
Adapted from Healthy People 2020 and 2030 frameworks. 13 , 14
The outcome of interest was composite CVD incidence or prevalence and mortality, as well as subtypes: coronary artery/heart diseases; ischemic heart disease; heart failure; myocardial infarction; atrial fibrillation; angina; peripheral arterial disease; cardiomyopathy; and stroke (Figure 1).
Systematic reviews with or without meta‐analyses that examined the association between SDoH and CVD or CVD‐specific mortality were included. For our study, we define systematic review as a systematic review if the article identifies itself as a systematic review or meta‐analysis and at least the eligibility criteria, information sources (implementing systematic search using at least one database), selection process, and data collection process from the Preferred Reporting Items for Systematic reviews and Meta‐Analyses checklist 34 had to be stated. There were no restrictions based on setting/country and study design (systematic reviews of both observational and interventional studies were eligible). Narrative and literature reviews and abstract‐only reviews were excluded. The latter was excluded only after having first conducted a hand search and contacting authors twice (when emails were available) to get the published full‐text review.
Search Strategy
Seven databases (Medline, Embase, CINAHL, Scopus, PsycINFO, the Joanna Briggs Institute Database of Systematic Reviews and Implementation Reports, and the Cochrane Database of Systematic Reviews) were searched from their inception to August 2, 2022. Keywords and medical subject headings related to SDoH and CVD were searched and used, with the support from a specialist librarian. The detailed search terms for the Medline database are found in Table S2. In addition, to ensure that all relevant studies were not overlooked, a hand search was conducted using Epistemonikos (a systematic review repository), 35 and reference lists of retrieved articles were checked. We did not restrict our search based on the year of publication and publication language (articles published in non‐English languages were translated using DeepL translator, https://www.deepl.com/translator).
Study Selection and Data Extraction
The identified articles were exported into EndNote X9.3 and deduplicated before importing into Covidence 36 (a web‐based software for screening and data extraction) to screen for eligible articles. Two reviewers (A.B.T. and H.L.H.) independently screened articles, and disagreements were resolved by discussion. As calculated by Covidence, our proportionate agreement was as follows: title/abstract, 0.91 (Cohen κ, 0.82); and full text, 0.79 (Cohen κ, 0.47). After securing the final number of studies to be included in our umbrella review, data were extracted by 2 reviewers (A.B.T. and H.L.H.). The Joanna Briggs Institute data extraction tool for umbrella review was used, and data related to study details, search details, appraisal instruments, and analysis were extracted. 23
Methodological Quality
The quality of the included systematic reviews was assessed using Assessing the Methodological Quality of Systematic Review (AMSTAR) version 2 tool, 37 a modified version of the AMSTAR tool. 38 The AMSTAR tool was established to evaluate systematic reviews of randomized trials. However, AMSTAR 2 is designed to evaluate “systematic reviews that include randomised or non‐randomised studies of healthcare interventions, or both.” 37 AMSTAR 2 has 16 items in total, with 7 critical and 9 noncritical domains. The overall confidence was rated as high quality (if the review had no weakness or had only 1 noncritical weakness), moderate quality (if there were ≥2 noncritical weaknesses), low quality (if the review had only 1 critical weakness without considering noncritical weaknesses), or critically low quality (if there were ≥2 critical weaknesses with or without noncritical weaknesses). Further information about the critical and noncritical domains and the rating of the overall confidence is available elsewhere. 37 Two reviewers (A.B.T. and H.L.H.) assessed independently, and disagreements were resolved through discussion.
Data Synthesis and Statistical Analysis
The general characteristics of the included systematic reviews with or without meta‐analyses were presented descriptively. We narrated our findings qualitatively based on themes of SDoH. For systematic reviews without meta‐analysis, association between a SDoH characteristic and CVD was presented graphically with distinct highlighting for the presence, absence, or inconsistent associations (Figure S1). For systematic reviews with meta‐analysis, the exposure of interest, author and year, number of primary studies that contributed to the meta‐analysis, pooled effect size, and heterogeneity (I2) were presented using forest plots (Figures S2 through S8).
The overall effects of a specific SDoH characteristic on CVD and CVD mortality were summarized and reported. Although we retained the terminology used by the authors of the included systematic reviews, we grouped CVD outcomes according to the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD‐10‐CM), codes 39 to increase interpretability. Finally, because of the high heterogeneity of the included meta‐analyses, insufficient data, limited number of meta‐analyses per subtypes of CVD, different effect size measures used, and the necessity of considering overlapping articles that was not feasible in this review, we did not conduct statistical pooling and assess credibility of evidence using the preexisting criteria. 40
Amendments Since the Protocol
Initially, we aimed to assess all domains of SDoH and their effect on CVD and CVD mortality. However, the health and health care domain was removed, with the exception of health literacy, because health care quality and accessibility is a broad concept that varied between different countries and conditions. Also, the theme of education access and quality was amended to merge education into the economic circumstance theme because it is highly related to economic status and to create early childhood development as a stand‐alone theme.
In the protocol, we stated whether to include systematic reviews with or without meta‐analysis. However, because there was not enough information to address our objective and assess the methodological quality, abstract‐only systematic reviews were excluded.
We had the plan to use ASRreview software (a machine learning tool) for article screening, 41 which is helpful for screening eligible articles at the title and abstract stage only. However, we found Covidence to be better for screening eligible studies at the title and abstract screening as well as full‐text screening stages. We also planned to stratify our findings based on sex and age. Unfortunately, there were no reviews specific to children/youths (almost all were among adults, and some did not report the age group), and almost all reviews did not report the findings based on sex. It was also difficult to report our findings based on countries, such as low‐, middle‐, and high‐income countries (as initially planned), because reviews have no clear demarcation.
RESULTS
Screening Result
A total of 17 132 studies were identified using the 7 databases (Figure 2). After the removal of duplicates (n=5867), 11 265 studies underwent title and abstract screening, and 286 studies proceeded to full‐text review. Of these, 5 studies 42 , 43 , 44 , 45 , 46 were translated into English because they were published in other languages. Finally, from database searching, 63 studies were identified as eligible. The excluded articles (and the reasons for exclusion) at the full‐text screening stage are provided in Table S3. From references of the retrieved articles and through conducting a hand search using Epistemonikos, we identified an additional 7 eligible studies. 47 , 48 , 49 , 50 , 51 , 52 , 53 Therefore, a total of 70 studies were included.
Figure 2. Flow diagram for selection of studies adapted from the Preferred Reporting Items for Overviews of Reviews flow diagram.
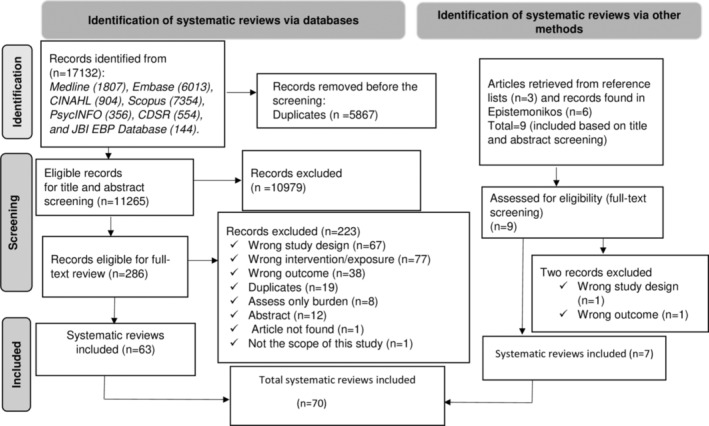
CDSR indicates Cochrane Database of Systematic Reviews; and JBI, Joanna Briggs Institute.
General Characteristics of the Included Reviews
Of the 70 reviews, 30 (43%) included a meta‐analysis. Ten reviews did not report information about the country of the included studies. Of those that did report, most of the reviews included studies from at least 2 countries. However, 11 reviews included studies from a single country: 9 reviews from the United States, 49 , 50 , 54 , 55 , 56 , 57 , 58 , 59 , 60 1 review from South Korea, 61 and 1 review from Australia. 47 Most (n=39; 56%) of the reviews were published in the past 5 years, with 24 (24%) published in the past 2 years. There were 1, 62 3, 62 , 63 , 64 and 7 53 , 62 , 63 , 64 , 65 , 66 , 67 reviews published before 2000, 2005, and 2011, respectively. Nine (13%) of the review authors implemented 1 database search, whereas most authors used ≥2. Cohort study design was the most frequently used in the primary studies included in each review. The general characteristics of the included reviews are found in Table S4.
Description of the Identified Reviews per Themes of SDoH
Of the 70 reviews identified, the greatest proportion included components of social and community context (33%) and economic circumstance (32%), followed by early childhood development (18%) and neighborhood and built environment (17%). Few reviews assessed >1 theme; for instance, 4 reviews assessed both economic circumstance and social and community context themes (Figure 3). The number of reviews per each SDoH characteristic is presented in Table 1.
Figure 3. Graphical presentation of the identified reviews per themes/domains of social determinants of health.
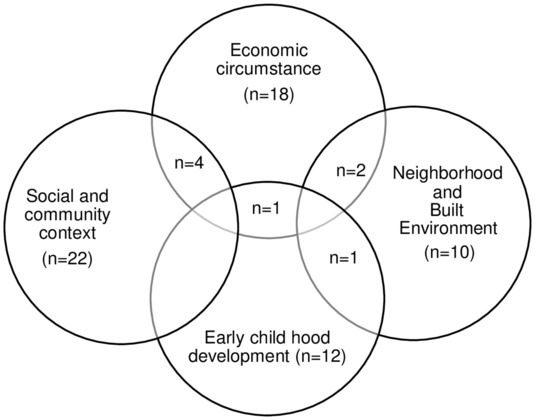
Table 1.
Number of Systematic Reviews by SDoH Characteristic
| SDoH characteristic | Total (reference) | Without meta‐analysis (reference) | With meta‐analysis (reference) |
|---|---|---|---|
| 1. Economic circumstance | 25 24 , 42 , 43 , 57 , 61 , 62 , 66 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 | ||
| Composite socioeconomic status | 9 | 6 24 , 42 , 43 , 61 , 74 , 75 | 3 71 , 72 , 73 |
| Education | 11 | 4 61 , 62 , 82 , 83 | 7 71 , 76 , 77 , 78 , 79 , 80 , 81 |
| Occupation | 10 | 5 61 , 62 , 82 , 83 , 84 | 5 71 , 76 , 77 , 79 , 81 |
| Income | 9 | 3 42 , 61 , 82 | 6 71 , 76 , 77 , 79 , 80 , 81 |
| Job insecurity | 4 | 3 66 , 86 , 87 | 1 85 |
| Homelessness or household instability | 2 | 1 57 | 1 88 |
| Food insecurity | 1 | 1 57 | … |
| 2. Social and community context | 26 25 , 42 , 47 , 50 , 51 , 55 , 56 , 58 , 60 , 63 , 66 , 67 , 68 , 69 , 75 , 87 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 | ||
| Poor/lack of social support | 7 | 3 63 , 66 , 67 | 4 67 , 68 , 89 , 90 |
| Loneliness, social isolation, or both | 3 | 2 60 , 91 | 1 25 |
| Social capital | 4 | 3 92 , 93 , 94 | 1 58 |
| Discrimination | 1 | 1 56 | … |
| Ethnicity and race | 11 | 4 42 , 50 , 75 , 98 | 7 47 , 51 , 55 , 69 , 95 , 96 , 97 |
| 3. Early childhood development | 14 48 , 52 , 53 , 64 , 65 , 78 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 | ||
| Early childhood socioeconomic status | 7 | 6 64 , 65 , 99 , 100 , 101 , 102 | 1 78 |
| Early childhood adverse events | 8 | 3 48 , 102 , 106 | 5 52 , 53 , 103 , 104 , 105 |
| 4. Neighborhood and built environment | 13 26 , 49 , 54 , 59 , 70 , 77 , 81 , 106 , 107 , 108 , 109 , 110 , 111 | ||
| Violence during adulthood | 6 | 5 54 , 59 , 106 , 108 , 109 | 1 107 |
| Conflict | 1 | 1 70 | … |
| Environmental attributes | 2 | 2 49 , 110 | … |
| Neighborhood socioeconomic status | 4 | 1 26 | 3 77 , 81 , 111 |
SDoH indicates social determinants of health.
Measurement of Variables Under SDoH: Evidence From the Included Reviews
The methods used to measure the variables under each SDoH are summarized in Table S5. In most of the reviews, there was no information about the cut points that were used to categorize variables under SDoH as high, low, good, or poor, and they likely differed across primary studies and reviews. Despite the different cut points that may exist, for our review, we used the categories/terms, such as high and low, made by the author of the included reviews.
Outcome Measures
Different reviews reported different CVD outcomes. Even a single review could report many CVD subtypes. For this umbrella review, we used the definition CVD, or subtype, given by the authors. In addition, we included all CVD measurements, including self‐report, record (such as from hospital and death registries), imaging, or diagnosis based on clinical examination. If the included review reported CVD (either by including at least 2 CVD subtypes or without mentioning the subtype), we considered it as composite CVD.
Assessment of Quality
According to the AMSTAR 2 tool, 77% (n=54) of the reviews were identified as critically low quality and 20% (n=14) of the reviews were identified as low quality (Table S6). Only one review 68 was graded as medium quality, and one review 69 was graded as high quality.
As for the critical domains of the AMSTAR 2 tool, only 4 reviews (6%) reported a list of excluded studies. Sixteen reviews (23%) had a registered protocol. A third of review authors (33%) incorporated the risk of bias while interpreting or discussing the results of their review. Most review authors used a comprehensive literature search strategy (59%; n=41), and used a satisfactory technique to assess the risk of bias in individual studies (56%; n=39).
For the noncritical domains of the AMSTAR 2 tool, only one review 70 reported the funding source for the included primary studies. In most (84%; n=59) of the reviews, the reason for the selection of study designs was not explained. Study selection and data extraction were conducted in duplicate in only 44% (n=31) and 25% (n=18) of reviews, respectively. Three‐fourths (76%; n=53) of the reviews provide satisfactory explanations and discussion about the heterogeneity observed in the results of the study.
Summary Findings
A thorough narration of the findings is found in Data S1 with additional display of reviews without meta‐analyses (Figure S1) and with meta‐analyses (Figures S2 through S8) separately. Here, we compiled and condensed the findings from reviews with and without meta‐analysis (Table 2).
Table 2.
Summary of Findings: Systematic Reviews Assessing the Association Between SDoH and CVD Outcomes (n=70)
| SDoH | CVD outcomes (based on ICD‐10: I00–I99)* | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CVD (composite or unspecified) | Cerebrovascular disease | Ischemic heart disease | Other forms of heart disease | Diseases of arteries | ||||||||||||||
| Composite cardiovascular disease | Composite cardiovascular disease mortality | Stroke | Stroke mortality | Coronary artery/heart disease | Coronary artery/heart disease mortality | ischemic heart disease | Ischemic heart disease mortality | Myocardial infarction | Mortality due to myocardial infarction | Angina | Heart Failure | Heart disease | Heart disease mortality | Atrial fibrillation | Cardiomyopathy | Mortality due to cardiomyopathy | Peripheral arterial disease | |
| Theme 1: economic stability | ||||||||||||||||||
| Low composite socioeconomic status 24 , 42 , 43 , 61 , 71 , 72 , 73 , 74 , 75 | +(1) | +(1) | +(2) | +(2) | +(1), ±(1) | +(1) | +(1) | +(1) | ±(1) | +(1) | ||||||||
| Low education 61 , 62 , 71 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 | +(3), ±(1) | +(2) | +(4) | +(1) | +(3) | +(2) | +(1) | ±(1) | ||||||||||
| Low income 42 , 61 , 71 , 76 , 77 , 79 , 80 , 81 , 82 | n(1) | +(1), n(1), +(1) | +(1) | +(1) | +(1) | +(2) | +(1) | ±(1) | +(1) | |||||||||
| Lower occupation level 61 , 62 , 71 , 76 , 77 , 79 , 81 , 82 , 83 , 84 | +(4), ±(1) | +(2), n(1) | +(2), n(2) | +(1) | n(2) | +(1) | +(2) | +(2) | +(2) | +(2) | ||||||||
| Job insecurity 66 , 85 , 86 , 87 | +(1), n(1) | ±(1), n(1) | ||||||||||||||||
| Homelessness 57 , 88 | +(2) | +(1) | ±(1) | n(1) | n(1) | n(1) | ||||||||||||
| Food insecurity 57 | +(1) | +(1) | +(1) | +(1) | +(1) | |||||||||||||
| Theme 2: social and community context | ||||||||||||||||||
| Low/poor social support 63 , 66 , 67 , 68 , 87 , 89 , 90 | n(1) | n(1) | +(1), n(1) | +(1), n(1) | +(2), n(2) | +(1) | ||||||||||||
| Loneliness and social isolation 25 , 60 , 91 | +(3) | +(2) | n(1) | +(1) | ||||||||||||||
| Low social capital index 93 , 94 | n(2) | n(1) | +(1) | +(1) | ||||||||||||||
| Social capital (few social roles) 92 | +(1) | +(1) | ||||||||||||||||
| Social capital index (low social network) 58 | +(1) | n(1) | n(1) | |||||||||||||||
| Social capital index (low social cohesion) 58 | n(1) | n(1) | ||||||||||||||||
| Discrimination 56 | +(1) | +(1) | +(1) | n(1) | +(1) | +(1) | ||||||||||||
| Disparities in ethnicity and race 42 , 47 , 50 , 51 , 55 , 69 , 75 , 95 , 96 , 97 , 98 | +(1), ±(1), n(1) | +(1) | ±(1), n(1) | +(3), n(1) | +(1), ±(1) | ±(1) | ±(1) | n(1) | +(2) | +(1) | +(1), ±(1) | |||||||
| Theme 3: early childhood development | ||||||||||||||||||
| Childhood socioeconomic disadvantage 64 , 65 , 78 , 99 , 100 , 101 , 102 | +(1) | +(1) | +(3) | +(2) | +(1), ±(1) | +(1) | n(1) | n(1) | ||||||||||
| Adverse childhood events 48 , 52 , 53 , 102 , 103 , 104 , 105 , 106 , † | +(5) | +(2), n(1) | + | +(4) | +(4) | +(1) | ||||||||||||
| Theme 4: neighborhood and built environment | ||||||||||||||||||
| Violence during adulthood 54 , 59 , 106 , 107 , 108 , 109 | +(3), n(1) | ±(1), n(1) | ±(1) | +(1), ±(1) | ±(1) | |||||||||||||
| Conflict 70 | ±(1) | n(1) | n(1) | +(1) | n(1) | n(1) | ±(1) | +(1) | ||||||||||
| Adverse environment 49 , 110 , ‡ | +(2) | +(1), n(1) | +(1) | +(1) | +(1) | |||||||||||||
| Neighborhood socioeconomic disadvantage 26 , 77 , 81 , 111 | +(2) | +(2) | +(2), n(1) | +(2) | +(2) | |||||||||||||
The numbers in the parentheses indicate the number of reviews. + Indicates poorer/worse social determinant associated with an increased risk of CVD outcome (poorer SDoH→worse CVD outcome); ±, an approximately equal number of null and increased risk findings. CVD indicates cardiovascular disease; ICD‐10, International Classification of Diseases, Tenth Revision; n, null/no association; and SDoH, social determinants of health.
World Health Organization. ICD‐10. 2019. I00 to I99 indicate diseases of the circulatory system.
Childhood adverse events, such as lower childhood cumulative adverse events and adverse events specific to abuse, neglect, and violence.
Inaccessibility of health care facilities, environmental noise, proximity to a major road/high traffic density, high crime rate, reduced access to food stores and parks/recreation, and increased access to fast‐food restaurants.
Factors Relating to Economic Circumstance and CVD
Composite SES 24 , 42 , 43 , 61 , 71 , 72 , 73 , 74 , 75 : Lower composite SES was associated with a higher risk of composite CVD 61 and CVD mortality. 24 Besides, it was associated with an increased risk of CVD subtypes, like stroke 24 , 73 and mortality attributable to stroke, 71 coronary heart disease, 24 heart failure, 74 heart disease, 43 myocardial infarction, 24 and cardiomyopathy. 42 However, the association between composite SES with atrial fibrillation was inconsistent. 75 Subjective social status (adjusted for objective statuses) was not associated with coronary heart disease. 72
Education 61 , 62 , 71 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 : In almost all reviews, lower education level was associated with a higher risk of CVDs (composite CVD, 80 , 81 stroke, coronary heart disease, 80 , 81 myocardial infarction, 79 and ischemic heart disease 61 , 62 ) and CVD mortality (mortality attributable to composite CVD 76 , 80 and stroke 71 ). However, in 2 reviews, 82 , 83 education was not consistently associated with composite CVD 83 and atrial fibrillation. 82
Income 42 , 61 , 71 , 76 , 77 , 79 , 80 , 81 , 82 : In most of the reviews, lower level of income was associated with CVD. 42 , 61 , 71 , 77 , 79 , 80 It was associated with higher risk of coronary heart disease, 80 heart failure, 77 myocardial infarction, 61 , 79 cardiomyopathy, 42 stroke (borderline significant), 80 and stroke mortality. 71 Of the 3 reviews that assessed the association between income and composite CVD mortality, 2 reported existence of association, 61 , 80 and the other one 76 found no association. A low income level was not constantly linked to atrial fibrillation. 82
Occupation 61 , 62 , 71 , 76 , 77 , 79 , 81 , 82 , 83 , 84 : Low occupation level was associated with a higher risk of composite CVD 61 , 81 , 84 and CVD mortality. 61 , 84 Specific to CVD subtypes, occupation was associated with a higher risk of heart failure, 77 myocardial infarction, 61 , 79 ischemic heart disease, 62 , 84 angina, 61 atrial fibrillation, 82 stroke, 61 , 84 and stroke mortality. 71 There was no association between lower occupation and stroke and coronary heart disease in one review that assessed the effect in men and women separately. 81 In addition, in one review, 83 occupation was not consistently associated with composite CVD.
Job insecurity 66 , 85 , 86 , 87 : There were only a few systematic reviews assessing job insecurity with CVD, and these fell within the ICD‐10‐CM code of ischemic heart disease. In general, the association between job insecurity and coronary/ischemic heart disease was not consistent. 66 , 86 , 87 Only one review reported a modest association between perceived job insecurity and incident coronary heart disease. 85
Homelessness, household instability, or both 57 , 88 was associated with a higher risk of composite CVD 57 , 88 and composite CVD mortality. 57 However, household instability was inconsistently associated with stroke 57 and was not associated with heart disease, 57 ischemic heart disease, 57 and mortality attributable to cardiomyopathy. 57
Food insecurity 57 was associated with an increased risk of CVD (composite CVD, coronary heart disease, myocardial infarction, and heart failure) and composite CVD mortality.
Factors Relating to Social and Community Context and CVD
Poor/lack of social support 63 , 66 , 67 , 68 , 87 , 89 , 90 was associated with a higher risk of myocardial infarction, 66 but there was no association with composite CVD 68 or CVD mortality. 67 Furthermore, there were inconsistent relationships with stroke 68 , 89 and ischemic 66 , 87 , 90 /coronary heart disease. 63 , 68 In the one review that conducted a separate analysis for men and women, 90 social support was not associated with ischemic heart disease.
Loneliness, social isolation, or both 25 , 60 , 91 : High loneliness and social isolation were associated with an increased risk of stroke. 25 , 60 , 91 However, there was an inconsistent relationship between loneliness and heart disease subtypes. 25 , 60 , 91
Social capital 58 , 92 , 93 , 94 : Low social capital index, measured by both social network and social cohesion, was associated with higher mortality attributable to ischemic heart disease 94 and coronary heart disease, 94 but not stroke 94 and mortality attributable to composite CVD. 93 , 94 Low social network was associated with a higher risk of composite CVD mortality. 58 Considering CVD subtypes, social network had no association with stroke 58 and coronary heart disease. 58 As for social cohesion, perceived social cohesion was not associated with stroke and coronary heart disease. 58 Moreover, fewer social roles were linked to higher composite CVD and composite CVD mortality. 92
Discrimination 56 : Lifetime perceived racial discrimination was associated with a higher risk of composite CVD, myocardial infarction, stroke, and angina. It was also associated with a higher risk of mortality attributable to composite CVD.
Ethnicity and race 42 , 47 , 50 , 51 , 55 , 69 , 75 , 95 , 96 , 97 , 98 : There were racial and ethnic differences in CVD and CVD mortality. For instance, mortality attributable to ischemic heart disease was lower among Afro‐Caribbean compared with White individuals, 98 Hispanic Americans had reduced risks of composite CVD, coronary heart disease, stroke, and heart failure than White people, 69 and Chinese individuals had a lower risk of coronary artery disease compared with White and South Asian individuals. 97 Furthermore, compared with White and White European individuals, Asians had a lower risk of peripheral arterial diseases. 47 , 96
Factors Relating to Early Childhood Development and CVD
Lower childhood SES 64 , 65 , 78 , 99 , 100 , 101 , 102 : Lower childhood SES was associated with a higher risk of composite CVD 65 , 102 , 103 , 104 and stroke 78 , 101 , 102 in later life. However, childhood SES had a less consistent association with coronary heart disease, 100 , 102 heart failure, 101 and heart disease. 99 As for mortality, lower childhood SES was associated with a higher risk of mortality attributable to composite CVD, 64 stroke, 64 and coronary heart disease. 64
Adverse childhood events 48 , 52 , 53 , 102 , 103 , 104 , 105 , 106 : Adverse childhood events were associated with a higher risk of later‐life composite CVD, 53 , 102 , 103 , 104 , 106 coronary heart disease, 102 heart failure, 102 myocardial infarction, 105 and ischemic heart disease. 48 , 52 , 53 , 106 However, they had an inconsistent association with stroke. 102 , 103
Factors Relating to Neighborhood and Built Environment and CVD
Violence during adulthood 54 , 59 , 106 , 107 , 108 , 109 : Violence was associated with a higher risk of composite CVD, 54 , 107 , 108 , 109 but had inconsistent association with CVD subtypes: stroke, 59 , 106 coronary heart disease, 106 heart failure, 106 and myocardial infarction. 59 , 106
Conflict 70 : There was an association between conflict and an increased risk of mortality from ischemic heart disease and heart disease. However, it had an inconsistent association with the occurrence of stroke and heart disease. In addition, there was no association between conflict and myocardial infarction, ischemic heart disease, angina pectoris, and mortality attributable to stroke.
Environmental attributes 49 , 110 : Environmental attributes (proximity to a major road, reduced access to food stores, no recreational areas, increased access to fast‐food restaurants, far from a health care facility, and high traffic density) were associated with a higher risk of coronary heart disease, 110 myocardial infarction, 110 heart failure, 110 stroke, 49 , 110 and angina. 110 However, food environments, assessed among adults with low SES, such as access to grocery stores and fast‐food restaurants, were not associated with coronary heart disease. 49
Neighborhood SES 26 , 77 , 81 , 111 : Lower neighborhood SES was associated with a higher risk of composite CVD, 81 stroke, 81 coronary heart disease, 81 heart failure, 77 and composite CVD mortality. 111 However, in one review, 26 neighborhood SES was not associated with stroke.
DISCUSSION
This umbrella review provides a comprehensive overview of the current evidence of the role of SDoH in CVD, including mortality attributable to CVD. We identified 70 eligible systematic reviews, of which 30 undertook meta‐analyses. Overall, there was evidence that lower or worse SDoH characteristics in the 4 themes of SDoH (economic circumstance, social and community context, early childhood development, and neighborhood and built environment) were associated with CVD and CVD mortality.
However, our review also identified areas within the 4 SDoH themes that were understudied and warranted further study. In particular, we only identified 2 systematic reviews assessing homelessness or household instability as well as environmental attributes and their association with CVD. In addition, we only identified single systematic reviews that assessed the role of food insecurity, conflict, or discrimination in regard to CVD. We did not also identify any systematic reviews that examined the association between health literacy and CVD.
Economic Circumstance
This umbrella review provided evidence that economic instability is linked with a higher likelihood of CVD and CVD mortality. Most reviews reported the detrimental influence of composite SES, education, income, occupation, and homelessness on CVD. Food insecurity was also associated with CVD, despite the fact that the finding was from a single systematic review. Our findings are in line with the Health Evidence Network Synthesis Report, 112 which revealed that SDoH is a contributor to health and health disparities, and identified the 4 overarching policy themes: enhancing early child development, promoting fair employment and decent work, providing social protection, and improving living environment.
Several pathways are possible for the association between economic instability and CVD. 7 Economic instability can lead to chronic stress, which, in turn, stimulates the sympathetic nervous system and the adrenal cortex and then results in an increased level of stress hormones, such as catecholamines, independent predictors for the development of CVD. 7 , 113 , 114 People with economic instability could have more trouble getting medical care in a timely manner and paying for their prescription medications, especially if they have to pay out of pocket. 115 , 116 , 117 , 118 It may also be attributable to the mediating role of conventional CVD risk factors, such as high blood pressure and diabetes, because they are unlikely to be treated efficiently and promptly among economically instable individuals. 119 The limited dietary alternatives and basic necessities (food, shelter, and clothing), inadequate sleep quality and quantity, heavy drinking and excessive alcohol intake, and illegal drug use are also more prevalent in people with economic instability, such as homeless people and people with food insecurity, and these might contribute to the high occurrence of CVD. 120 Economically instable people are also forced to eat less‐nutritious and high‐energy items,121 with a higher intake of sugar‐sweetened beverages and processed meats, and this might result in CVD. 122 , 123 , 124 However, in this theme, we identified inconsistent evidence for the association between job insecurity and CVD. Notably, the reviews were different in scope. For instance, 2 reviews were interested in people working in the formal economy or people at work and observed no association with ischemic heart disease. 86 , 87 However, the other review was interested in self‐reported job insecurity in the general population and observed an association with coronary heart disease. 85 This is in contrast to the notion that job insecurity can induce stress 125 and jeopardize the ability to meet crucial demands, including economic safety and social status, which, in turn, has an impact on CVD. 125 , 126 , 127 We also noted that there was no consistent evidence of an association between composite SES, education, and income with the specific CVD subtype, atrial fibrillation. This is somewhat unexpected and could be because atrial fibrillation is difficult to diagnose and socioeconomically privileged individuals may have the time and financial resources to visit a physician and obtain expensive heart rate monitoring. 128
Social and Community Context
This umbrella review found evidence that social role, social isolation, loneliness, ethnicity, and discrimination were associated with a higher risk of CVD. However, there were also reviews in this theme that reported an inconsistent or null association. For example, social support was not associated with CVD in most reviews, and social capital was not associated with CVD subtypes.
A report from the National Academies of Sciences, Engineering, and Medicine identifies poor social health (particularly social isolation and loneliness) as a CVD risk factor, accounting for a one‐third increase in CVD, a 4 times increase in risk of death, and an increased risk of hospitalization and emergency department visits. 129 Preclinical studies also reported a link between a higher level of blood pressure, heart rate, and cortisol levels with social support and social isolation. 130 , 131 Poor social health also increases the risk of developing CVD through a variety of psychological, physiological, and emotional mechanisms. 19 It is hypothesized that poor social health, such as loneliness, is related to depression, anger, and hostility, as well as reduced buffering of external stressors. 132 The negative psychological exposures can amplify harmful physiological reactions, like activated hypothalamic‐pituitary‐adrenal axis and elevated levels of inflammatory markers. 7 These inflammatory markers and the cardiometabolic changes in response to stressors that happened because of poor social health, particularly loneliness, could increase blood pressure and result in variability in heart rate. 132 , 133 People with poor social or community engagement are also more likely to have elevated behavioral CVD risk factors, such as smoking, substance abuse, and low physical activity. 19 Furthermore, poor social health affects people's ability to receive medical support, 134 and this can result in an advanced stage of any disease condition, such as CVD.
The ethnic and racial disparity in CVD has been attributed to population differences in societal factors (including discrimination), which impact substantially on people's health. 135 Notably, our umbrella review is limited as we were unable to make generalizations based on the terminology of ethnic and racial groups described by the review authors. For example, individuals who identified as Black in terms of race may also identify as Hispanic in terms of ethnicity, and many studies did not define specific racial or ethnic groupings in this way.
Early Childhood Development
In this umbrella review, adverse childhood experiences, including cumulative adverse events, adverse events specific to abuse and neglect, and lower SES, were associated with an increased risk of later‐life CVD.
This is in line with a report by Child Welfare Information Gateway 136 explaining that the disruption of neurodevelopment attributable to early childhood adverse experiences increases the risk for the following: (1) physical health consequences, such as diabetes, stroke, health attack, malnutrition, and high blood pressure; (2) psychological consequences, such as diminished cognitive skills, poor mental and emotional health, posttraumatic stress, and social difficulties; and (3) behavioral consequences, like engaging in aversive and self‐destructive behaviors, like smoking and substance abuse. Our finding also agrees with the aforementioned health evidence network synthesis report 112 and with a guideline that urges early access to supporting services for children to help them reach their full potential later in life and avoid serious conditions, like CVD. 137 Unfavorable early childhood experiences may also hinder regular emotional and psychosocial development and increase susceptibility to a range of behavioral, mental, and physical health difficulties in later life, which, in turn, raises the risk of CVD. For instance, it has been demonstrated that exposure to extremely stressful events during childhood can result in engaging in aversive and self‐destructive behaviors, like substance abuse, physical inactivity, sleep disorder, and early‐onset obesity and type 2 diabetes. 138 , 139 , 140 , 141 It can also be rationalized by the possibility that negative childhood experiences led to an increased carotid intima‐media thickness, one of the most prevalent CVD biomarkers, 142 as well as alterations in nervous, neuroendocrine, and immune systems that undergo age‐dependent maturation. 141 , 143 , 144 These systems are important for stress regulation. However, adverse experiences could result in chronic stress and, in turn, result in activation of the hypothalamic‐pituitary‐adrenal axis and then dysregulation and excessive release of glucocorticoid hormones, such as cortisol. 145 Through the above mechanisms, unfavourable childhood experiences could harm several physiological systems, including the cardiovascular system, in later life. 141
Neighborhood and Built Environment
There was evidence that poor neighborhood SES, violence (for composite CVD), and environmental attributes were associated with an increased risk of CVD. Notably, the evidence for environmental attributes was for CVD subtypes, except stroke mortality, in which the finding was inconsistent, highlighting the opportunity for a composite CVD systematic review. However, there was inconsistent evidence for the role of violence and conflict in CVD subtypes.
Our finding of neighborhood socioeconomic disadvantage being associated with CVD is aligned with a study by Gary‐Webb et al 146 that identified living in neighborhoods with socioeconomic disadvantage is associated with poorer health status (physical health, mental health, and global health composite scores). Similarly, the aforementioned health evidence network synthesis report revealed that living environment is an important factor for health and health inequality. 112 Living in a socially deprived neighborhood is associated with increased stress and poorer lifestyle factors (smoking, physical inactivity, and unhealthy diet), which all increase the of risk of CVD. 147 This is aligned with our finding for environmental attributes, especially food environments, and CVD. It has been commonly claimed that the accessibility of affordable, culturally appropriate, healthful foods close to people's places of residence and workplaces influences food choices, which, in turn, affects CVD risk factors and outcomes. 148 Hence, a study on food environment policy implementation recommends an urgent need of tackling the burden of obesity and diet‐related noncommunicable diseases through prioritizing actions toward healthy food environments. 149
Strengths and Limitations
This is the first umbrella review to assess the role of SDoH in CVD. We comprehensively reviewed the evidence by incorporating 4 themes of SDoH, including health literacy in the health and health care domain. All CVD outcomes, including subtypes and mortality, were assessed. Furthermore, our findings are based on systematic reviews, which rank first in the hierarchy of evidence.
All interpretations should be used with caution, however, as this umbrella review does have some limitations. First, except for 2 reviews (1 medium quality 68 and 1 high quality 69 ), all reviews were graded as low and critically low quality based on the AMSTAR 2 quality assessment tool. Reviews with inadequate methods are difficult to understand, tend to overestimate the overall treatment effect, and may draw the wrong conclusions. Second, the terminology and measurement of SDoH factors within and between reviews varied greatly. As social determinants can be context specific (relating to a time or place), measurement recommendations similar to biological factors, such as blood pressure, cannot necessarily be created. However, research translation could be improved by SDoH factors being clearly defined and tested in sensitivity analyses. Third, we identified several SDoH factors; however, SDoH is abroad concept, and there are likely other SDoH factors that should be considered. It is also unlikely that one systematic review (eg, there was only one systematic review for conflict) would provide strong and enough evidence to saturate SDoH areas, as researchers bring a different lens to research that is reflected in eligibility criteria, outcomes, and interpretation of findings. Also, the lack of or few systematic reviews likely demonstrate a lack of primary studies and the need for further research. Fourth, primary studies may have been included in >1 review, and it was not feasible to assess this. Fifth, although most reviews in the economic circumstance theme report the absence of publication bias, most reviews in other themes report that there was a publication bias or did not report any information about publication bias, which limits the interpretation of our findings. Sixth, given the nature of the topic, the systematic reviews predominantly included observational studies with few randomized controlled trials, and observational studies are more prone to bias and confounding. For example, in our review, economic circumstance may influence the neighborhood that the person lives in. Therefore, it is difficult to distinguish the contribution of each factor, or SDoH in this case, even if analyses have controlled for potential confounders. We acknowledge that the individual studies had differences in populations and comparison groups as well, and these differences could help explain the somewhat inconsistent findings. Despite these differences, overall, we found evidence that SDoH are important contributors to CVD and CVD mortality. These differences between included reviews also increase the generalization of our findings and could be considered a strength of this umbrella review. Last, because studies in the included systematic review are observational, there may be survival bias. That is, those in the most impoverished or worse SDoH may have died at an early age because of these impoverished conditions and were not considered in the study. In addition, there might be healthy volunteer bias; people with existing medical conditions are less likely to volunteer and participate in epidemiological studies. Therefore, our results may be influenced by survival bias and the healthy volunteer effect; the first is especially relevant for the early childhood development theme.
Implications for Practice
There is an urgent need to focus on implementing cost‐effective policies and interventions to reduce premature mortality attributable to noncommunicable disease. 1 The World Health Organization has a sustainable development goal (number 3, target 4) of reducing premature mortality attributable to noncommunicable diseases by a third by 2030. 150 CVD is by far the most common noncommunicable disease 151 ; therefore, efforts to reduce CVD will likely have the greatest impact.
This umbrella review provides simple yet comprehensive evidence about the roles of SDoH in CVD outcomes and demonstrates that the massive burden of CVD could be lessened by recognizing and addressing unfavorable SDoH. Our evidence suggests the importance of taking a system view of risk factors for CVD. The breadth of SDoH factors linked with CVD identified in this umbrella review along with the interconnections that are known to exist between these SDoH factors (and other CVD risk factors) imply that addressing one factor in isolation is unlikely to make much difference. There is a need for policies and interventions to take a holistic and integrated approach, tackling SDoH at macro and meso levels, and considering the knock‐on consequences that changes in one factor will have in others. A complex adaptive systems approach with interconnected policies across each of the 4 theme areas we identified, as well as the health and health care theme, would greatly benefit health and well‐being across many domains.
More immediately, this evidence can be used to inform the development of CVD prevention interventions, as well as selection of targeted subpopulations to increase the impact of such interventions. The evidence found could be used by policy makers and health care professionals to set appropriate guidelines and policies and to improve patient outcomes through nonmedical interventions, such as social prescribing. 152 Because SDoH are currently overlooked in predicting health outcomes, including CVD, 153 , 154 , 155 , 156 and because our review identified that SDoH factors have a role in CVD and CVD mortality, we recommend that future clinical CVD prediction models should include the SDoH.
CONCLUSIONS
This comprehensive umbrella review provides overwhelming evidence that SDoH are important contributors to CVD and CVD mortality. We identified consistent evidence that economic circumstance and early childhood development themes play a role in CVD and CVD mortality. Specifically, we identified evidence that childhood adverse events, childhood abuse or neglect, childhood SES, neighborhood SES, violence, environmental attributes, education, income, occupation, food insecurity, homelessness, composite SES, social role, social isolation, loneliness, ethnicity, and discrimination play roles in CVD and CVD mortality. However, as we only identified 1 or 2 systematic reviews assessing homelessness or household instability, food insecurity, neighborhood conflict, environmental attributes, or discrimination with CVD, further studies and synthesis are required. In addition, we identified a complete lack of evidence synthesis for health literacy with CVD or CVD mortality.
Although our findings are constrained by the included reviews' low methodological quality, the implications of our findings are clear; we provide evidence that detecting and addressing SDoH will likely benefit CVD risk factors and outcomes. This evidence should be used to inform CVD prevention policies and interventions through each stage of development, including selection of targeted subpopulations. Given that the identified SDoH factors are interconnected with each other and other CVD risk factors, our evidence suggests the importance of taking a system view with a holistic and integrated approach. Furthermore, incorporating SDoH into CVD risk prediction models could be helpful to set nonmedical interventions and to lower the social inequities in health.
Sources of Funding
A. B. Teshale and H. L. Htun are supported by Monash International Tuition Scholarship and Monash Graduate Scholarship. The funder was not involved in design, data collection, interpretation of data, and writing of the manuscript.
Disclosures
None.
Supporting information
Data S1
Tables S1–S6
Figures S1–S8
Acknowledgments
For her support in developing the search strategy, we are grateful to Lorena Romero, the senior librarian from the Ian Potter Library at the Alfred Hospital in Melbourne, Victoria, Australia. We are also grateful for Miranda Cumpston for her technical guidance during the review process.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.123.029765
This article was sent to Tiffany M. Powell‐Wiley, MD, MPH, Associate Editor, for review by expert referees, editorial decision, and final disposition.
For Sources of Funding and Disclosures, see page 13.
References
- 1. Non communicable diseases. World Health Organization; 2022. Available at: https://www.who.int/news‐room/fact‐sheets/detail/noncommunicable‐diseases. Accessed September 26, 2022. [Google Scholar]
- 2. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Multiple cause of death 1999–2020. Centers for Disease Control and Prevention. Available at: https://wonder.cdc.gov/wonder/help/mcd.html. Accessed September 10, 2022.
- 4. Watkins DA, Yamey G, Schäferhoff M, Adeyi O, Alleyne G, Alwan A, Berkley S, Feachem R, Frenk J, Ghosh G. Alma‐Ata at 40 years: reflections from the Lancet Commission on Investing in Health. Lancet. 2018;392:1434–1460. doi: 10.1016/S0140-6736(18)32389-0.1007/s4064 [DOI] [PubMed] [Google Scholar]
- 5. Dean CA, Zhang D, Kulchycki KT, Ventline B, Jagirdar R, Milan RA. Social determinants of cardiovascular disease among Michigan residents: a call to action for population health initiatives. J Racial Ethn Health Disparities. 2020;7:144–161. doi: 10.1007/s40615-019-00644-2 [DOI] [PubMed] [Google Scholar]
- 6. Cockerham WC, Hamby BW, Oates GR. The social determinants of chronic disease. Am J Prev Med. 2017;52:S5–S12. doi: 10.1016/j.amepre.2016.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Powell‐Wiley TM, Baumer Y, Baah FO, Baez AS, Farmer N, Mahlobo CT, Pita MA, Potharaju KA, Tamura K, Wallen GR. Social determinants of cardiovascular disease. Circ Res. 2022;130:782–799. doi: 10.1161/CIRCRESAHA.121.31981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reutter L, Kushner KE. ‘Health equity through action on the social determinants of health’: taking up the challenge in nursing. Nurs Inq. 2010;17:269–280. doi: 10.1111/j.1440-1800.2010.00500.x [DOI] [PubMed] [Google Scholar]
- 9. Closing the gap in a generation: Health equity through action on the social determinants of health: Final report of the commission on social determinants of health. World Health Organization; 2008. Available at: https://www.who.int/publications/i/item/WHO‐IER‐CSDH‐08.1. Accessed June 16, 2023. [DOI] [PubMed] [Google Scholar]
- 10. Marmot M, Friel S, Bell R, Houweling TA, Taylor S; Commission on Social Determinants of Health . Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–1669. doi: 10.1016/S0140-6736(08)61690-6 [DOI] [PubMed] [Google Scholar]
- 11. Solar O, Irwin A. A conceptual framework for action on the social determinants of health. In: Social Determinants of Health Discussion Paper 2 (Policy and Practice). WHO Document Production Services; 2010. Available at: https://apps.who.int/iris/handle/10665/44489. Accessed June 16, 2023. [Google Scholar]
- 12. Max J, Sedivy V, Garrido M. Increasing Our Impact by Using a Social‐Ecological Approach. Administration on Children, Youth and Families, Family and Youth Services Bureau; 2015. [Google Scholar]
- 13. Social Determinants of Health . Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Available at: https://health.gov/healthypeople/objectives‐and‐data/social‐determinants‐health. Accessed November 8, 2022.
- 14. National Center for Health Statistics . Chapter 39: Social determinants of health. In: Healthy People 2020 Midcourse Review. Hyattsville, MD; 2016. Available at: https://www.cdc.gov/nchs/data/hpdata2020/HP2020MCR‐C39‐SDOH.pdf. Accessed June 16, 2023. [Google Scholar]
- 15. Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz‐Flores S, Davey‐Smith G, Dennison‐Himmelfarb CR, Lauer MS, Lockwood DW. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 16. Coke LA, Himmelfarb CD. Guideline on the primary prevention of cardiovascular disease: let's get it into practice! J Cardiovasc Nurs. 2019;34:285–288. doi: 10.1097/JCN.0000000000000586 [DOI] [PubMed] [Google Scholar]
- 17. Bharmal N, Derose KP, Felician M, Weden MM. Understanding the Upstream Social Determinants of Health. RAND; 2015:1–18. [Google Scholar]
- 18. Singu S, Acharya A, Challagundla K, Byrareddy SN. Impact of social determinants of health on the emerging COVID‐19 pandemic in the United States. Front Public Health. 2020;406. doi: 10.3389/fpubh.2020.00406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Singh R, Javed Z, Yahya T, Valero‐Elizondo J, Acquah I, Hyder AA, Maqsood MH, Amin Z, Al‐Kindi S, Cainzos‐Achirica M. Community and social context: an important social determinant of cardiovascular disease. Methodist Debakey Cardiovasc J. 2021;17:15–27. doi: 10.14797/mdcvj.846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Knox SS, Adelman A, Ellison RC, Arnett DK, Siegmund K, Weidner G, Province MA. Hostility, social support, and carotid artery atherosclerosis in the National Heart, Lung, and Blood Institute Family Heart Study. Am J Cardiol. 2000;86:1086–1089. doi: 10.1016/s0002-9149(00)01164-4 [DOI] [PubMed] [Google Scholar]
- 21. Magnani JW, Mujahid MS, Aronow HD, Cené CW, Dickson VV, Havranek E, Morgenstern LB, Paasche‐Orlow MK, Pollak A, Willey JZ. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation. 2018;138:e48–e74. doi: 10.1161/CIR.0000000000000579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aromataris E, Fernandez R, Godfrey C, Holly C, Kahlil H, Tungpunkom P. Methodology for JBI umbrella reviews. Joanna Briggs Institute reviewer's manual 2014. Adelaide: The Joanna Briggs Institute; 2014. [Google Scholar]
- 24. Williams J, Allen L, Wickramasinghe K, Mikkelsen B, Roberts N, Townsend N. A systematic review of associations between non‐communicable diseases and socioeconomic status within low‐and lower‐middle‐income countries. J Glob Health. 2018;8. doi: 10.7189/jogh.08.020409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta‐analysis of longitudinal observational studies. Heart. 2016;102:1009–1016. doi: 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim Y, Twardzik E, Judd SE, Colabianchi N. Neighborhood socioeconomic status and stroke incidence: a systematic review. Neurology. 2021;96:897–907. doi: 10.1212/WNL.0000000000011892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. JBI Evid Implement. 2015;13:132–140. doi: 10.1097/XEB.0000000000000055 [DOI] [PubMed] [Google Scholar]
- 28. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 29. Gates M, Gates A, Pieper D, Fernandes RM, Tricco AC, Moher D, Brennan SE, Li T, Pollock M, Lunny C, et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ. 2022;378:e070849. doi: 10.1136/bmj-2022-070849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mannoh I, Hussien M, Commodore‐Mensah Y, Michos ED. Impact of social determinants of health on cardiovascular disease prevention. Curr Opin Cardiol. 2021;36:572–579. doi: 10.1097/HCO.0000000000000893 [DOI] [PubMed] [Google Scholar]
- 31. Barr DA, Blair IV, Cohen MS, Cruz‐Flores S, Davey‐Smith G, Dennison‐Himmelfarb C, Havranek E, Lauer M, Lockwood D, Mujahid M. Social determinants of risk and outcomes for cardiovascular disease. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 32. Ozturk I. The role of education in economic development: a theoretical perspective. Available at SSRN 11375412008.
- 33. Education and Socioeconomic Status . American Psychological Association. 2017. Available at: https://www.apa.org/pi/ses/resources/publications/education. Accessed April 21, 2022.
- 34. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:1–11. doi: 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rada G, Pérez D, Araya‐Quintanilla F, Ávila C, Bravo‐Soto G, Bravo‐Jeria R, Cánepa A, Capurro D, Castro‐Gutiérrez V, Contreras V. Epistemonikos: a comprehensive database of systematic reviews for health decision‐making. BMC Med Res Methodol. 2020;20:1–7. doi: 10.1186/s12874-020-01157-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Babineau J. Product review: covidence (systematic review software). J Can Health Lib Assoc. 2014;35:68–71. [Google Scholar]
- 37. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non‐randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:1–7. doi: 10.1186/1471-2288-7-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. WHO . International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD‐10)‐WHO Version for; 2019‐covid‐expanded. Chapter IX: Diseases of the circulatory system (I00–I99). 2019. Available at: https://icd.who.int/browse10/2019/en#/IX. Accessed June 16, 2023.
- 40. Gosling CJ, Solanes A, Fusar‐Poli P, Radua J. Metaumbrella: the first comprehensive suite to perform data analysis in umbrella reviews with stratification of the evidence. BMJ Ment Health. 2023;26:e300534. doi: 10.1136/bmjment-2022-300534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. ASReview LAB developers . ASReview LAB ‐ A tool for AI‐assisted systematic reviews. Zenodo. 2022. Available at: https://zenodo.org/record/6625304. Accessed June 20, 2022.
- 42. Agisilaou K, Lambrinou E. Risk factors for peripartum cardiomyopathy. Cyprus Nursing Chronicles. 2020;20:24–37. [Google Scholar]
- 43. Salgado‐Barreira Á, Estany‐Gestal A, Figueiras A. Effect of socioeconomic status on mortality in urban areas: a systematic critical review. Cadernos de Saúde Pública. 2014;30:1609–1621. doi: 10.1590/0102-311x00152513 [DOI] [PubMed] [Google Scholar]
- 44. Mezzoiuso AG, Gola M, Rebecchi A, Riccò M, Capolongo S, Buffoli M, Tirani M, Odone A, Signorelli C. Indoors and health: results of a systematic literature review assessing the potential health effects of living in basements. Acta Biomed. 2017;88:375–382. doi: 10.23750/abm.v88i3.6741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Oliveira G, Schimith MD, Silveira VDN. Fatores de risco cardiovascular em mulheres: revisão integrativa da literatura. Enfermagem Brasil. 2019;18:799–815. [Google Scholar]
- 46. Foguet‐Boreu Q. Psychosocial stress, high blood pressure and cardiovascular risk. Hipertens Riesgo Vasc. 2021;38:83–90. doi: 10.1016/j.hipert.2020.09.001 [DOI] [PubMed] [Google Scholar]
- 47. Ho CL, Chih HJ, Garimella PS, Matsushita K, Jansen S, Reid CM. Prevalence and risk factors of peripheral artery disease in a population with chronic kidney disease in Australia: a systematic review and meta‐analysis. Nephrology. 2021;26:798–808. doi: 10.1111/nep.13914 [DOI] [PubMed] [Google Scholar]
- 48. Kalmakis KA, Chandler GE. Health consequences of adverse childhood experiences: a systematic review. J Am Assoc Nurse Pract. 2015;27:457–465. doi: 10.1002/2327-6924.12215 [DOI] [PubMed] [Google Scholar]
- 49. Kraft AN, Thatcher EJ, Zenk SN. Neighborhood food environment and health outcomes in us low‐socioeconomic status, racial/ethnic minority, and rural populations: a systematic review. J Health Care Poor Underserved. 2020;31:1078–1114. doi: 10.1353/hpu.2020.0083 [DOI] [PubMed] [Google Scholar]
- 50. Oramasionwu CU, Hunter JM, Brown CM, Morse GD, Lawson KA, Koeller JM, Frei CR. Cardiovascular disease in Blacks with HIV/AIDS in the United States: a systematic review of the literature. Open AIDS J. 2012;6:29–35. doi: 10.2174/1874613601206010029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Park DY, An S, Romero ME, Kaur A, Ravi V, Huang HD, Vij A. Incidence and risk factors of atrial fibrillation and atrial arrhythmias in people living with HIV: a systematic review and meta‐analysis. J Interv Card Electrophysiol. 2022;1–9. doi: 10.1007/s10840-022-01233-w [DOI] [PubMed] [Google Scholar]
- 52. Petruccelli K, Davis J, Berman T. Adverse childhood experiences and associated health outcomes: a systematic review and meta‐analysis. Child Abuse Negl. 2019;97:104127. doi: 10.1016/j.chiabu.2019.104127 [DOI] [PubMed] [Google Scholar]
- 53. Wegman HL, Stetler C. A meta‐analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosomatic Med. 2009;71:805–812. doi: 10.1097/PSY.0b013e3181bb2b46 [DOI] [PubMed] [Google Scholar]
- 54. Burnette CE, Ka'apu K, Scarnato JM, Liddell J. Cardiovascular health among US indigenous peoples: a holistic and sex‐specific systematic review. J Evid Based Soc Work. 2020;17:24–48. doi: 10.1080/26408066.2019.1617817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cortes‐Bergoderi M, Goel K, Murad MH, Allison T, Somers VK, Erwin PJ, Sochor O, Lopez‐Jimenez F. Cardiovascular mortality in Hispanics compared to non‐Hispanic whites: a systematic review and meta‐analysis of the Hispanic paradox. Eur J Intern Med. 2013;24:791–799. doi: 10.1016/j.ejim.2013.09.003 [DOI] [PubMed] [Google Scholar]
- 56. Panza GA, Puhl RM, Taylor BA, Zaleski AL, Livingston J, Pescatello LS. Links between discrimination and cardiovascular health among socially stigmatized groups: a systematic review. PLoS ONE. 2019;14:e0217623. doi: 10.1371/journal.pone.0217623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Parekh T, Xue H, Cheskin LJ, Cuellar AE. Food insecurity and housing instability as determinants of cardiovascular health outcomes: a systematic review. Nutr Metab Cardiovasc Dis. 2022;32:1590–1608. doi: 10.1016/j.numecd.2022.03.025 [DOI] [PubMed] [Google Scholar]
- 58. Park JW, Mealy R, Saldanha IJ, Loucks EB, Needham BL, Sims M, Fava JL, Dulin AJ, Howe CJ. Multilevel resilience resources and cardiovascular disease in the United States: a systematic review and meta‐analysis. Health Psychol. 2022;41:278–290. doi: 10.1037/hea0001069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Peer N, Abrahams N, Kengne A‐P. A systematic review of the associations of adult sexual abuse in women with cardiovascular diseases and selected risk factors. Global Heart. 2020;15:65. doi: 10.5334/gh.760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tibiriçá L, Jester DJ, Jeste DV. A systematic review of loneliness and social isolation among Hispanic/Latinx older adults in the United States. Psychiatry Research. 2022;313:114568. doi: 10.1016/j.psychres.2022.114568 [DOI] [PubMed] [Google Scholar]
- 61. Lee C‐Y, Im E‐O. Socioeconomic disparities in cardiovascular health in South Korea: a systematic review. J Cardiovasc Nurs. 2021;36:8–22. doi: 10.1097/JCN.0000000000000624 [DOI] [PubMed] [Google Scholar]
- 62. Gonzalez MA, Artalejo FR, Calero JR. Relationship between socioeconomic status and ischaemic heart disease in cohort and case‐control studies: 1960–1993. Int J Epidemiol. 1998;27:350–358. doi: 10.1093/ije/27.3.350 [DOI] [PubMed] [Google Scholar]
- 63. Kuper H, Marmot M, Hemingway H. Systematic review of prospective cohort studies of psychosocial factors in the etiology and prognosis of coronary heart disease. Semin Vasc Med. 2002;2:267–314. doi: 10.1055/s-2002-35401 [DOI] [PubMed] [Google Scholar]
- 64. Galobardes B, Lynch JW, Davey SG. Childhood socioeconomic circumstances and cause‐specific mortality in adulthood: systematic review and interpretation. Epidemiol Rev. 2004;26:7–21. doi: 10.1093/epirev/mxh008 [DOI] [PubMed] [Google Scholar]
- 65. Galobardes B, Smith GD, Lynch JW. Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Ann Epidemiol. 2006;16:91–104. doi: 10.1016/j.annepidem.2005.06.053 [DOI] [PubMed] [Google Scholar]
- 66. Eller NH, Netterstrøm B, Gyntelberg F, Kristensen TS, Nielsen F, Steptoe A, Theorell T. Work‐related psychosocial factors and the development of ischemic heart disease: a systematic review. Cardiol Rev. 2009;17:83–97. doi: 10.1097/CRD.0b013e318198c8e9 [DOI] [PubMed] [Google Scholar]
- 67. Barth J, Schneider S, Von Känel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta‐analysis. Psychosom Med. 2010;72:229–238. doi: 10.1097/PSY.0b013e3181d01611 [DOI] [PubMed] [Google Scholar]
- 68. Freak‐Poli R, Phyo AZZ, Hu J, Barker SF. Are social isolation, lack of social support or loneliness risk factors for cardiovascular disease in Australia and New Zealand? A systematic review and meta‐analysis. Health Promot J Austr. 2022;33:278–315. doi: 10.1002/hpja.592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ezzatvar Y, Ramírez‐Vélez R, Izquierdo M, García‐Hermoso A. Racial differences in all‐cause mortality and future complications among people with diabetes: a systematic review and meta‐analysis of data from more than 2.4 million individuals. Diabetologia. 2021;64:2389–2401. doi: 10.1007/s00125-021-05554-9 [DOI] [PubMed] [Google Scholar]
- 70. Jawad M, Vamos EP, Najim M, Roberts B, Millett C. Impact of armed conflict on cardiovascular disease risk: a systematic review. Heart. 2019;105:1388–1394. doi: 10.1136/heartjnl-2018-314459 [DOI] [PubMed] [Google Scholar]
- 71. Wang S, Zhai H, Wei L, Shen B, Wang J. Socioeconomic status predicts the risk of stroke death: a systematic review and meta‐analysis. Prev Med Rep. 2020;19:101124. doi: 10.1016/j.pmedr.2020.101124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Tang KL, Rashid R, Godley J, Ghali WA. Association between subjective social status and cardiovascular disease and cardiovascular risk factors: a systematic review and meta‐analysis. BMJ Open. 2016;6:e010137. doi: 10.1136/bmjopen-2015-010137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Kerr GD, Slavin H, Clark D, Coupar F, Langhorne P, Stott DJ. Do vascular risk factors explain the association between socioeconomic status and stroke incidence: a meta‐analysis. Cerebrovasc Dis. 2011;31:57–63. doi: 10.1159/000320855 [DOI] [PubMed] [Google Scholar]
- 74. Hawkins NM, Jhund PS, McMurray JJ, Capewell S. Heart failure and socioeconomic status: accumulating evidence of inequality. Eur J Heart Fail. 2012;14:138–146. doi: 10.1093/eurjhf/hfr168 [DOI] [PubMed] [Google Scholar]
- 75. Allan V, Honarbakhsh S, Casas J‐P, Wallace J, Hunter R, Schilling R, Perel P, Morley K, Banerjee A, Hemingway H. Are cardiovascular risk factors also associated with the incidence of atrial fibrillation? Thromb Haemost. 2017;117:837–850. doi: 10.1160/TH16-11-0825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Vathesatogkit P, Batty GD, Woodward M. Socioeconomic disadvantage and disease‐specific mortality in Asia: systematic review with meta‐analysis of population‐based cohort studies. J Epidemiol Community Health. 2014;68:375–383. doi: 10.1136/jech-2013-203053 [DOI] [PubMed] [Google Scholar]
- 77. Potter EL, Hopper I, Sen J, Salim A, Marwick TH. Impact of socioeconomic status on incident heart failure and left ventricular dysfunction: systematic review and meta‐analysis. Eur Heart J Qual Care Clin Outcomes. 2019;5:169–179. doi: 10.1093/ehjqcco/qcy047 [DOI] [PubMed] [Google Scholar]
- 78. McHutchison CA, Backhouse EV, Cvoro V, Shenkin SD, Wardlaw JM. Education, socioeconomic status, and intelligence in childhood and stroke risk in later life. Epidemiology. 2017;28:608–618. doi: 10.1097/EDE.0000000000000675 [DOI] [PubMed] [Google Scholar]
- 79. Manrique‐Garcia E, Sidorchuk A, Hallqvist J, Moradi T. Socioeconomic position and incidence of acute myocardial infarction: a meta‐analysis. J Epidemiol Community Health. 2011;65:301–309. doi: 10.1136/jech.2009.104075 [DOI] [PubMed] [Google Scholar]
- 80. Khaing W, Vallibhakara SA, Attia J, McEvoy M, Thakkinstian A. Effects of education and income on cardiovascular outcomes: a systematic review and meta‐analysis. Eur J Prev Cardiol. 2017;24:1032–1042. doi: 10.1177/2047487317705916 [DOI] [PubMed] [Google Scholar]
- 81. Backholer K, Peters SA, Bots SH, Peeters A, Huxley RR, Woodward M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: a systematic review and meta‐analysis. J Epidemiol Community Health. 2017;71:550–557. doi: 10.1136/jech-2016-207890 [DOI] [PubMed] [Google Scholar]
- 82. Lunde ED, Nielsen PB, Riahi S, Larsen TB, Lip GY, Fonager K, Larsen ML, Joensen AM. Associations between socioeconomic status, atrial fibrillation, and outcomes: a systematic review. Expert Rev Cardiovasc Ther. 2018;16:857–873. doi: 10.1080/14779072.2018.1533118 [DOI] [PubMed] [Google Scholar]
- 83. Birhanu MM, Zaman SB, Thrift AG, Evans RG, Zengin A. Risk factors for incident cardiovascular events among adults in low‐and middle‐income countries: a systematic review and meta‐analysis of prospective cohort studies. Prev Med. 2022;158:107036. doi: 10.1016/j.ypmed.2022.107036 [DOI] [PubMed] [Google Scholar]
- 84. Saif‐Ur‐Rahman KM, Mamun R, Li Y, Matsunaga M, Ota A, Yatsuya H. Work‐related factors among people with diabetes and the risk of cardiovascular diseases: a systematic review. J Occup Health. 2021;63:e12278. doi: 10.1002/1348-9585.12278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Virtanen M, Nyberg ST, Batty GD, Jokela M, Heikkilä K, Fransson EI, Alfredsson L, Bjorner JB, Borritz M, Burr H. Perceived job insecurity as a risk factor for incident coronary heart disease: systematic review and meta‐analysis. BMJ. 2013;347:f4746. doi: 10.1136/bmj.f4746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Anfossi CM, Muñoz MA, Fredes CT, Rojas FP, Ross J, Head J, Britton A. Work exposures and development of cardiovascular diseases: a systematic review. Ann Work Expo Health. 2022;66:698. doi: 10.1093/annweh/wxac004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Theorell T, Jood K, Järvholm LS, Vingård E, Perk J, Östergren PO, Hall C. A systematic review of studies in the contributions of the work environment to ischaemic heart disease development. Eur J Public Health. 2016;26:470–477. doi: 10.1093/eurpub/ckw025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Al‐Shakarchi NJ, Evans H, Luchenski SA, Story A, Banerjee A. Cardiovascular disease in homeless versus housed individuals: a systematic review of observational and interventional studies. Heart. 2020;106:1483–1488. doi: 10.1136/heartjnl-2020-316706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Lightbody CE, Clegg A, Patel K, Lucas JC, Storey H, Hackett ML, Watkins DCL. Systematic review and meta‐analysis of psychosocial risk factors for stroke. Semin Neurol. 2017;37:294–306. doi: 10.1055/s-0037-1603758 [DOI] [PubMed] [Google Scholar]
- 90. Smaardijk VR, Lodder P, Kop WJ, van Gennep B, Maas AH, Mommersteeg PM. Sex‐and gender‐stratified risks of psychological factors for incident ischemic heart disease: systematic review and meta‐analysis. J Am Heart Assoc. 2019;8:e010859. doi: 10.1161/JAHA.118.010859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Petitte T, Mallow J, Barnes E, Petrone A, Barr T, Theeke L. A systematic review of loneliness and common chronic physical conditions in adults. Open Psychol J. 2015;8:113. doi: 10.2174/1874350101508010113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Chin B, Cohen S. Review of the association between number of social roles and cardiovascular disease: graded or threshold effect? Psychosom Med. 2020;82:471–486. doi: 10.1097/PSY.0000000000000809 [DOI] [PubMed] [Google Scholar]
- 93. Choi M, Mesa‐Frias M, Nüesch E, Hargreaves J, Prieto‐Merino D, Bowling A, Smith GD, Ebrahim S, Dale CE, Casas JP. Social capital, mortality, cardiovascular events and cancer: a systematic review of prospective studies. Int J Epidemiol. 2014;43:1895–1920. doi: 10.1093/ije/dyu212 [DOI] [PubMed] [Google Scholar]
- 94. Rodgers J, Valuev AV, Hswen Y, Subramanian S. Social capital and physical health: an updated review of the literature for 2007–2018. Soc Sci Med. 2019;236:112360. doi: 10.1016/j.socscimed.2019.112360 [DOI] [PubMed] [Google Scholar]
- 95. Zaman MJS, Philipson P, Chen R, Farag A, Shipley M, Marmot MG, Timmis AD, Hemingway H. South Asians and coronary disease: is there discordance between effects on incidence and prognosis? Heart. 2013;99:729–736. doi: 10.1136/heartjnl-2012-302925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Sebastianski M, Makowsky MJ, Dorgan M, Tsuyuki RT. Paradoxically lower prevalence of peripheral arterial disease in South Asians: a systematic review and meta‐analysis. Heart. 2014;100:100–105. doi: 10.1136/heartjnl-2013-303605 [DOI] [PubMed] [Google Scholar]
- 97. Jin K, Ding D, Gullick J, Koo F, Neubeck L. A Chinese immigrant paradox? Low coronary heart disease incidence but higher short‐term mortality in Western‐dwelling Chinese immigrants: a systematic review and meta‐analysis. J Am Heart Assoc. 2015;4:e002568. doi: 10.1161/JAHA.115.002568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Francis DK, Bennett NR, Ferguson TS, Hennis AJ, Wilks RJ, Harris EN, MacLeish MM, Sullivan LW. Disparities in Cardiovascular disease among caribbean populations: a systematic literature review. BMC Public Health. 2015;15:828. doi: 10.1186/s12889-015-2166-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. McEniry M. Early‐life conditions and older adult health in low‐and middle‐income countries: a review. J Dev Orig Health Dis. 2013;4:10–29. doi: 10.1017/S2040174412000499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Mallinson PAC, Lieber J, Kinra S. Childhood socioeconomic position and risk of cardiovascular disease in adulthood: systematic review of evidence from low‐and middle‐income countries. Am J Prev Med. 2021;61:e251–e266. doi: 10.1016/j.amepre.2021.04.027 [DOI] [PubMed] [Google Scholar]
- 101. Bijker R, Agyemang C. The influence of early‐life conditions on cardiovascular disease later in life among ethnic minority populations: a systematic review. Intern Emerg Med. 2016;11:341–353. doi: 10.1007/s11739-015-1272-y [DOI] [PubMed] [Google Scholar]
- 102. Pool LR, Aguayo L, Brzezinski M, Perak AM, Davis MM, Greenland P, Hou L, Marino BS, Van Horn L, Wakschlag L. Childhood risk factors and adulthood cardiovascular disease: a systematic review. J Pediatr. 2021;232:118–126.e23. doi: 10.1016/j.jpeds.2021.01.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long‐term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta‐analysis. PLoS Med. 2012;9:e1001349. doi: 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP. The effect of multiple adverse childhood experiences on health: a systematic review and meta‐analysis. Lancet Public Health. 2017;2:e356–e366. doi: 10.1016/S2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- 105. Jacquet‐Smailovic M, Brennstuhl M‐J, Tarquinio CL, Tarquinio C. Relationship between cumulative adverse childhood experiences and myocardial infarction in adulthood: a systematic review and meta‐analysis. J Child Adolesc Trauma. 2021;15:701–714. doi: 10.1007/s40653-021-00404-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Suglia SF, Sapra KJ, Koenen KC. Violence and cardiovascular health: a systematic review. Am J Prev Med. 2015;48:205–212. doi: 10.1016/j.amepre.2014.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Jakubowski KP, Murray V, Stokes N, Thurston RC. Sexual violence and cardiovascular disease risk: a systematic review and meta‐analysis. Maturitas. 2021;153:48–60. doi: 10.1016/j.maturitas.2021.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Pate T, Simonič B. Intimate partner violence and physical health problems in women. Slov Med J. 2021;90:390–398. [Google Scholar]
- 109. O'Neil A, Scovelle AJ. Intimate partner violence perpetration and cardiovascular risk: a systematic review. Prev Med Rep. 2018;10:15–19. doi: 10.1016/j.pmedr.2018.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Malambo P, Kengne AP, De Villiers A, Lambert EV, Puoane T. Built environment, selected risk factors and major cardiovascular disease outcomes: a systematic review. PLoS One. 2016;11:e0166846. doi: 10.1371/journal.pone.0166846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Sánchez‐Santos MT, Mesa‐Frias M, Choi M, Nüesch E, Asunsolo‐Del Barco A, Amuzu A, Smith GD, Ebrahim S, Prieto‐Merino D, Casas JP. Area‐level deprivation and overall and cause‐specific mortality: 12 years' observation on British women and systematic review of prospective studies. PLoS One. 2013;8:e72656. doi: 10.1371/journal.pone.0072656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Saunders M, Barr B, McHale P, Hamelmann C. WHO Health Evidence Network Synthesis Reports. In: Key policies for addressing the social determinants of health and health inequities. WHO Regional Office for Europe; 2017. [PubMed] [Google Scholar]
- 113. Benedict CR, Shelton B, Johnstone DE, Francis G, Greenberg B, Konstam M, Probstfield JL, Yusuf S. Prognostic significance of plasma norepinephrine in patients with asymptomatic left ventricular dysfunction. Circulation. 1996;94:690–697. doi: 10.1161/01.cir.94.4.690 [DOI] [PubMed] [Google Scholar]
- 114. Lundberg U. Stress hormones in health and illness: the roles of work and gender. Psychoneuroendocrinology. 2005;30:1017–1021. doi: 10.1016/j.psyneuen.2005.03.014 [DOI] [PubMed] [Google Scholar]
- 115. Elwell‐Sutton T, Fok J, Albanese F, Mathie H, Holland R. Factors associated with access to care and healthcare utilization in the homeless population of England. J Public Health. 2017;39:26–33. doi: 10.1093/pubmed/fdw008 [DOI] [PubMed] [Google Scholar]
- 116. Stafford A, Wood L. Tackling health disparities for people who are homeless? Start with social determinants. Int J Environ Res Public Health. 2017;14:1535. doi: 10.3390/ijerph14121535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Havranek EP. The influence of social and economic factors on heart disease. JAMA Cardiol. 2019;4:1212–1213. doi: 10.1001/jamacardio.2019.3802 [DOI] [PubMed] [Google Scholar]
- 118. Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. 2018;39:273–289. doi: 10.1146/annurev-publhealth-031816-044628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Gozdzik A, Salehi R, O'Campo P, Stergiopoulos V, Hwang SW. Cardiovascular risk factors and 30‐year cardiovascular risk in homeless adults with mental illness. BMC Public Health. 2015;15:165. doi: 10.1186/s12889-015-1472-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Baggett TP, Liauw SS, Hwang SW. Cardiovascular disease and homelessness. J Am Coll Cardiol. 2018;71:2585–2597. doi: 10.1016/j.jacc.2018.02.077 [DOI] [PubMed] [Google Scholar]
- 121. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363:6–9. doi: 10.1056/NEJMp1000072 [DOI] [PubMed] [Google Scholar]
- 122. Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower‐income adults. J Acad Nutr Diet. 2014;114:1943–1953.e2. doi: 10.1016/j.jand.2014.06.353 [DOI] [PubMed] [Google Scholar]
- 123. Iqbal R, Dehghan M, Mente A, Rangarajan S, Wielgosz A, Avezum A, Seron P, AlHabib KF, Lopez‐Jaramillo P, Swaminathan S. Associations of unprocessed and processed meat intake with mortality and cardiovascular disease in 21 countries [prospective urban rural epidemiology (pure) study]: a prospective cohort study. Am J Clin Nutr. 2021;114:1049–1058. doi: 10.1093/ajcn/nqaa448 [DOI] [PubMed] [Google Scholar]
- 124. Pacheco LS, Lacey JV Jr, Martinez ME, Lemus H, Araneta MRG, Sears DD, Talavera GA, Anderson CA. Sugar‐sweetened beverage intake and cardiovascular disease risk in the California Teachers Study. J Am Heart Assoc. 2020;9:e014883. doi: 10.1161/JAHA.119.014883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. De Witte H, Pienaar J, De Cuyper N. Review of 30 years of longitudinal studies on the association between job insecurity and health and well‐being: is there causal evidence? Aust Psychol. 2016;51:18–31. [Google Scholar]
- 126. Jahoda M. Employment and Unemployment. Cambridge Books; 1982. [Google Scholar]
- 127. Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9:360–370. doi: 10.1038/nrcardio.2012.45 [DOI] [PubMed] [Google Scholar]
- 128. Harris K, Edwards D, Mant J. How can we best detect atrial fibrillation? J R Coll Physicians Edinb. 2012;42:5–22. doi: 10.4997/JRCPE.2012.S02 [DOI] [PubMed] [Google Scholar]
- 129. National Academies of Sciences Engineering, and Medicine . Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. National Academies Press; 2020. [PubMed] [Google Scholar]
- 130. Shively CA, Clarkson TB, Kaplan JR. Social deprivation and coronary artery atherosclerosis in female cynomolgus monkeys. Atherosclerosis. 1989;77:69–76. doi: 10.1016/0021-9150(89)90011-7 [DOI] [PubMed] [Google Scholar]
- 131. Sapolsky RM, Alberts SC, Altmann J. Hypercortisolism associated with social subordinance or social isolation among wild baboons. Arch Gen psychiatry. 1997;54:1137–1143. doi: 10.1001/archpsyc.1997.01830240097014 [DOI] [PubMed] [Google Scholar]
- 132. Paul E, Bu F, Fancourt D. Loneliness and risk for cardiovascular disease: mechanisms and future directions. Curr Cardiol Rep. 2021;23:68. doi: 10.1007/s11886-021-01495-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Steptoe A, Owen N, Kunz‐Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle‐aged men and women. Psychoneuroendocrinology. 2004;29:593–611. doi: 10.1016/S0306-4530(03)00086-6 [DOI] [PubMed] [Google Scholar]
- 134. Ozbay F, Johnson DC, Dimoulas E, Morgan C III, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont). 2007;4:35. [PMC free article] [PubMed] [Google Scholar]
- 135. Post WS, Watson KE, Hansen S, Folsom AR, Szklo M, Shea S, Barr RG, Burke G, Bertoni AG, Allen N. Racial and ethnic differences in all‐cause and cardiovascular disease mortality: the MESA study. Circulation. 2022;146:229–239. doi: 10.1161/CIRCULATIONAHA.122.059174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Child Welfare Information Gateway . Long‐term consequences of child abuse and neglect. Washington, DC: U.S. Department of Health and Human Services, Administration for Children and Families, Children's Bureau; 2019. [Google Scholar]
- 137. Supporting young children and their families early, to reach their full potential. 2022. The National Disability Insurance Scheme (NDIS). Available at: https://www.ndis.gov.au/community/we‐listened/you‐said‐we‐heard‐post‐consultation‐reports/supporting‐young‐children‐and‐their‐families‐early‐reach‐their‐full‐potential. Accessed January 25, 2023.
- 138. Fink DS, Galea S. Life course epidemiology of trauma and related psychopathology in civilian populations. Current Psychiatry Rep. 2015;17:31. doi: 10.1007/s11920-015-0566-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Naughton AM, Maguire SA, Mann MK, Lumb RC, Tempest V, Gracias S, Kemp AM. Emotional, behavioral, and developmental features indicative of neglect or emotional abuse in preschool children: a systematic review. JAMA Pediatr. 2013;167:769–775. doi: 10.1001/jamapediatrics.2013.192 [DOI] [PubMed] [Google Scholar]
- 140. Maguire S, Williams B, Naughton A, Cowley L, Tempest V, Mann M, Teague M, Kemp A. A systematic review of the emotional, behavioural and cognitive features exhibited by school‐aged children experiencing neglect or emotional abuse. Child Care Health Dev. 2015;41:641–653. doi: 10.1111/cch.12227 [DOI] [PubMed] [Google Scholar]
- 141. Su S, Jimenez MP, Roberts CT, Loucks EB. The role of adverse childhood experiences in cardiovascular disease risk: a review with emphasis on plausible mechanisms. Curr Cardiol Rep. 2015;17:1–10. doi: 10.1007/s11886-015-0645-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Thurston RC, Chang Y, Derby CA, Bromberger JT, Harlow SD, Janssen I, Matthews KA. Abuse and subclinical cardiovascular disease among midlife women: the study of women's health across the nation. Stroke. 2014;45:2246–2251. doi: 10.1161/STROKEAHA.114.005928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Nusslock R, Miller GE. Early‐life adversity and physical and emotional health across the lifespan: a neuroimmune network hypothesis. Biol psychiatry. 2016;80:23–32. doi: 10.1016/j.biopsych.2015.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Buss C, Entringer S, Wadhwa PD. Fetal programming of brain development: intrauterine stress and susceptibility to psychopathology. Sci Signal. 2012;5:pt7. doi: 10.1126/scisignal.2003406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23:185–222. doi: 10.1016/j.chc.2014.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Gary‐Webb TL, Baptiste‐Roberts K, Pham L, Wesche‐Thobaben J, Patricio J, Pi‐Sunyer FX, Brown AF, Jones‐Corneille L, Brancati FL. Neighborhood socioeconomic status, depression, and health status in the Look AHEAD (Action for Health in Diabetes) study. BMC Public Health. 2011;11:349. doi: 10.1186/1471-2458-11-349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Calling S, Li X, Kawakami N, Hamano T, Sundquist K. Impact of neighborhood resources on cardiovascular disease: a nationwide six‐year follow‐up. BMC Public Health. 2016;16:634. doi: 10.1186/s12889-016-3293-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Vadiveloo MK, Sotos‐Prieto M, Parker HW, Yao Q, Thorndike AN. Contributions of food environments to dietary quality and cardiovascular disease risk. Curr Atheroscler Rep. 2021;23:14. doi: 10.1007/s11883-021-00912-9 [DOI] [PubMed] [Google Scholar]
- 149. Pineda E, Poelman MP, Aaspõllu A, Bica M, Bouzas C, Carrano E, De Miguel‐Etayo P, Djojosoeparto S, Blenkuš MG, Graca P. Policy implementation and priorities to create healthy food environments using the Healthy Food Environment Policy Index (Food‐EPI): a pooled level analysis across eleven European countries. Lancet Reg Health Eur. 2022;23:100522. doi: 10.1016/j.lanepe.2022.100522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Katila P, Colfer CJP, De Jong W, Galloway G, Pacheco P, Winkel G. Sustainable Development Goals. Cambridge University Press; 2019. [Google Scholar]
- 151. Noncommunicable diseases (NCDs)—mainly cancer, cardiovascular disease, chronic respiratory diseases, and diabetes—are the #1 cause of death and disability worldwide. NCDAlliance. Available at: https://ncdalliance.org/why‐ncds/NCDs. Accessed January 5, 2022.
- 152. Htun HL, Teshale AB, Cumpston MS, Demos L, Ryan J, Owen A, Freak‐Poli R. Effectiveness of social prescribing for chronic disease prevention in adults: a systematic review and meta‐analysis of randomised controlled trials. J Epidemiol Community Health. 2023;77:265–276. doi: 10.1136/jech-2022-220247 [DOI] [PubMed] [Google Scholar]
- 153. Tan M, Hatef E, Taghipour D, Vyas K, Kharrazi H, Gottlieb L, Weiner J. Including social and behavioral determinants in predictive models: trends, challenges, and opportunities. JMIR Med Inform. 2020;8:e18084. doi: 10.2196/18084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Zhao Y, Wood EP, Mirin N, Cook SH, Chunara R. Social determinants in machine learning cardiovascular disease prediction models: a systematic review. Am J Prev Med. 2021;61:596–605. doi: 10.1016/j.amepre.2021.04.016 [DOI] [PubMed] [Google Scholar]
- 155. Lans A, Kanbier LN, Bernstein DN, Groot OQ, Ogink PT, Tobert DG, Verlaan JJ, Schwab JH. Social determinants of health in prognostic machine learning models for orthopaedic outcomes: a systematic review. J Eval Clin Pract. 2023;29:292–299. [DOI] [PubMed] [Google Scholar]
- 156. Hammond G, Johnston K, Huang K, Joynt Maddox KE. Social determinants of health improve predictive accuracy of clinical risk models for cardiovascular hospitalization, annual cost, and death. Circ Cardiovasc Qual Outcomes. 2020;13:e006752. doi: 10.1161/CIRCOUTCOMES.120.006752 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Tables S1–S6
Figures S1–S8


