Abstract
Purpose of Review
Traumatic and atraumatic shoulder instability is common in pediatric and adolescent patients. It is well-established that young patients with anterior shoulder dislocation are at high risk of recurrent instability. This review assesses the current literature pertaining to management of both anterior instability and MDI in the pediatric and adolescent populations.
Recent Findings
Current research suggests that pediatric and adolescent patients with shoulder instability have excellent outcomes following arthroscopic Bankart repair; however, higher rates of recurrent instability requiring revision surgical management have been identified in patients with more than one dislocation episode pre-operatively, those with Hill-Sachs lesions and those under age 16. The addition of the remplissage procedure to an arthroscopic Bankart repair may be useful in preventing recurrent instability for patients with large Hill-Sachs lesions. Open procedures with bony glenoid augmentation may be indicated in patients with significant glenoid bone loss, or those who have failed primary surgical management, with promising outcomes reported following the Latarjet coracoid process transfer procedure in the adolescent population. Pediatric and adolescent patients with hyperlaxity, and those participating in swimming or gymnastics are more likely to have multidirectional instability (MDI). Non-surgical management with physical therapy is the mainstay of treatment for MDI with positive outcomes reported overall. In young patients with MDI who continue to have symptoms of instability and pain that effects daily activities or sports despite an adequate and appropriate course of rehabilitation, surgical management with capsulorrhaphy may be considered, with promising outcomes reported for both open and arthroscopic techniques.
Summary
Attentive selection of timing and surgical procedure for pediatric and adolescent patients with anterior shoulder instability may help to prevent recurrent instability following shoulder stabilization. Although most pediatric and adolescent patients with MDI do well following non-surgical management alone, those that fail conservative management have good outcomes following arthroscopic or open capsulorrhaphy.
Keywords: Pediatric, Adolescent, Shoulder, Glenohumeral, Instability, Bankart
Introduction
Traumatic and atraumatic shoulder instability is common in pediatric and adolescent patients [19]. The incidence of anterior shoulder dislocations in patients between the ages of 10 and 16 has been estimated as high as 164 per 100,000 person years [49, 85], and may be even higher in recent years in concordance with athletic participation in overhead and collision sports in this age group [29, 74]. For adolescents that participate in contact sports, the incidence of anterior shoulder instability may approach 15% [39]. The incidence of MDI is more difficult to estimate given the spectrum of disease that occurs in individuals with hyperlaxity. In a study of asymptomatic children, Emery and Millaji identified clinical signs of MDI in over 20% of subjects [26]. The incidence of MDI is known to be highest in overhead athletes such as gymnasts and swimmers [1, 34, 53].
Anterior Instability
The immediate management for a pediatric and adolescent patient with a suspected anterior shoulder dislocation consists of a closed reduction, either on the sideline, if possible, or with sedation in the emergency department. However, in patients with open physes, providers may wish to consider radiographs prior to reduction to assess for a proximal humeral physeal fracture [54]. It is known that younger patients are at higher risk of re-dislocation, particularly those 19 years of age and younger [27]. It is unclear based on the evidence to date whether prepubescent children are at similar, or lower risk of recurrent instability compared to younger adolescents following an anterior shoulder dislocation episode [52, 54, 63]. Marans et al. followed 21 skeletally immature patients who had sustained a traumatic anterior shoulder dislocation initially managed non-operatively and found recurrent instability in 100% of the included patients [52]. Hovelius et al. studied patients who were initially managed nonoperatively after a primary anterior shoulder dislocation episode and reported that the youngest group (12–16 years) had the highest rate of recurrent instability followed by those aged 17–19 [35]. Others have found that children aged 13 years and less are less likely to experience recurrent instability than those aged 14–18 [59, 63].
Management After First-Time Dislocation
Historically, the management for a first-time dislocation has been non-operative management consisting of a period of immobilization in a sling following by appropriate physical therapy and rehabilitation. However, even with appropriate nonsurgical treatment, children and adolescents have been shown to have considerable higher risk of developing recurrent instability after a first-time dislocation episode, particularly those 14–18 years of age [2, 38, 66, 81]. Roberts et al. studied 133 children and adolescents between the ages of 13–18 who sustained a primary anterior shoulder dislocation episode and found a 75% rate of recurrent instability [65]. Previously published, smaller studies have reported rates of recurrent instability between 56 and 96% after first-time dislocations in pediatric and adolescent populations [21, 40, 46, 63]. There has been concern that recurrent instability can lead to higher degrees of attritional bone loss to the humerus and glenoid [4, 22], resulting in higher failure rates after surgical stabilization [15, 18•, 43]. Lau et al. compared adolescent and adult patients with a history of anterior shoulder dislocation and found that 24.4% of the adolescent group had “off-track” bone loss compared to only 3.3% in the adult group [47]. The two independent risk factors of glenoid “off-track” lesions were multiple dislocation episodes, and adolescent age group [47]. Yamamoto et al. proposed the glenoid track concept in 2007 [84], which has since gained widespread clinical relevance as a key metric to identify patients at risk for recurrent instability and failure following soft-tissue stabilization alone [70]. The glenoid track concept calculates the size and location of the Hill-Sachs lesion in relation to the glenoid bone loss and classifies bipolar bone loss as either “off-track” if the margin of the Hill-Sachs lesion falls outside of the glenoid track and is likely to engage, or “on-track” if the margin of the Hill-Sachs lesion falls within the glenoid track and is unlikely to engage [84]. Moreover, there is concern that recurrent instability could hasten the progression of glenohumeral osteoarthritis and lead to future glenohumeral arthropathy [10, 14, 36]. Given the concerns of recurrent instability and possible sequelae, some have advocated for surgical stabilization for most adolescent patients with first-time shoulder dislocations [9, 11, 61]. However, others argue that because the rate of recurrent instability after arthroscopic Bankart repair remains high in the pediatric and adolescent populations [18•, 43, 76], and not all patients with recurrent glenohumeral instability would request surgical management [68], routine surgical stabilization for all first-time adolescent shoulder dislocations may not be justified. One non-randomized study of 65 adolescent patients with first-time anterior shoulder dislocations compared outcomes after arthroscopic versus conservative management, and found a 13% rate of recurrent instability in the arthroscopic stabilization group compared to more than 70% in the conservative treatment group [28]. Currently, there is data to support consideration for surgical intervention following a first-time anterior shoulder dislocation in the adolescent population. However, given the high risk of confounding factors affecting outcomes in the literature published to date, further research with randomized study design, large sample size, and long-term follow-up is needed to help determine the optimal management of adolescent patients with first-time shoulder dislocations.
Arthroscopic Bankart Repair
Given the increased incidence of anterior shoulder instability in the young, active population along with recognition of the potential need for surgical intervention following a primary dislocation, the number of arthroscopic stabilization procedures has increased almost twofold over the past decade [73]. In general, good outcomes have been reported following arthroscopic anterior inferior (Bankart) repair and capsullorhaphy in the pediatric and adolescent populations [16, 44, 60]. Furthermore, rates of return to sport after arthroscopic Bankart repair in pediatric and adolescent populations have been reported between 88 and 100% in recent studies, with 75–90% able to return at the same or higher level [16, 20, 33, 69]. However, high rates of recurrent instability between 20 and 50% have been reported [18•, 60, 71, 76, 78]. Given the relatively high rate of recurrent instability after arthroscopic Bankart repair, recent studies examined the risk factors that might lead to recurrent instability in children and adolescents. Torrance et al. published a case series of 67 adolescent patients < 18 years of age who had undergone arthroscopic Bankart repair, all of whom participated in contact sports, and identified that 34 (51%) developed recurrent instability at a mean 3 months post-operatively [76]. Amongst the risk factors studied, age was the most important predictor of recurrent instability after arthroscopic Bankart repair, with those < 16 years of age 2.2 times more likely to develop recurrence than the older adolescent patients in the cohort [76]. The youngest patient included in the aforementioned study was 14 years of age and, therefore, the impact of age less than 14 years was not clear. Similarly, Cheng et al. assessed 171 adolescents who had undergone arthroscopic Bankart repair and identified 35 (20.5%) who developed recurrent instability. Adolescents with more than one dislocation episode before surgery, those skeletally immature, and those with glenoid retroversion less than 6° had a higher risk of recurrent instability post-operatively [18•]. Kramer et al. assessed 39 adolescent patients (mean age, 16 years) patients who had undergone arthroscopic Bankart repair for traumatic anterior instability and found that 9 (25%) had developed recurrent instability at a mean of 20.7 months follow-up. There was a higher incidence of Hill-Sachs lesions on MRI in those who developed recurrent instability (89%) compared to those that did not develop recurrent instability (52%, p = 0048) [43]. Egger et al. recently studied 59 adolescent patients 12–18 years of age and reported that 10 (17%) required revision stabilization with another 8 (14%) reporting subjective post-operative instability. While “off-track” bone loss was not associated with surgical failure, those requiring revision stabilization surgery were found to have larger Hill-Sachs lesions [25•] (Table 1).
Table 1.
Studies assessing the rate of recurrent instability following arthroscopic Bankart repair in pediatric and adolescent patients as well as factors that predict recurrent instability
| Study | Population | Recurrent instability | Predictors of recurrent instability |
|---|---|---|---|
| Torrance et al. 2018 [76] | 67 patients < 18 years of age participating in collision sports |
At mean 33 months post-operatively Recurrent instability: 34/67 (51%) Revision stabilization: 30/67 (45%) |
Age < 16 (vs. those 16–18 years): Relative risk = 2.2 (p < 0.0001) |
| Cheng et al. 2021 [18•] | 171 patients < 18 years |
At mean 5.4 years post-operatively Recurrent instability: 35/171 (20.5%) |
More than one dislocation: Odds ratio (OR) = 7.7 (p = 0.01) Open physis: OR = 3.9 (p = 0.04) Glenoid retroversion < 6°: OR = 9.1 (p < 0.001) |
| Kramer et al. 2019 [43] | 36 patients 13–18 years |
At a mean of 35.6 months post-operatively Recurrent instability: 9/36 (25%) Revision stabilization: 2/36 (6%) |
Presence of Hill-Sachs lesion on MRI: (p = 0.048) |
| Egger et al. 2023 [25•] | 59 adolescents 12–18 years |
At a mean of 49 months post-operatively Recurrent instability: 18/59 (31%) Revision stabilization: 10/59 (17%) |
Larger Hill-Sachs lesions on MRI associated with revision surgery (p = 0.04) |
| Hughes et al. 2018 [37] | 41 adolescents with Hill Sachs lesions and recurrent instability |
At a mean follow-up of 2.6 years Remplissage group Recurrent instability: 2/15 (13%) Isolated Bankart group Recurrent instability: 8/17 (47%) |
Isolated Bankart repair (vs. Bankart and remplissage): (p = 0.04) |
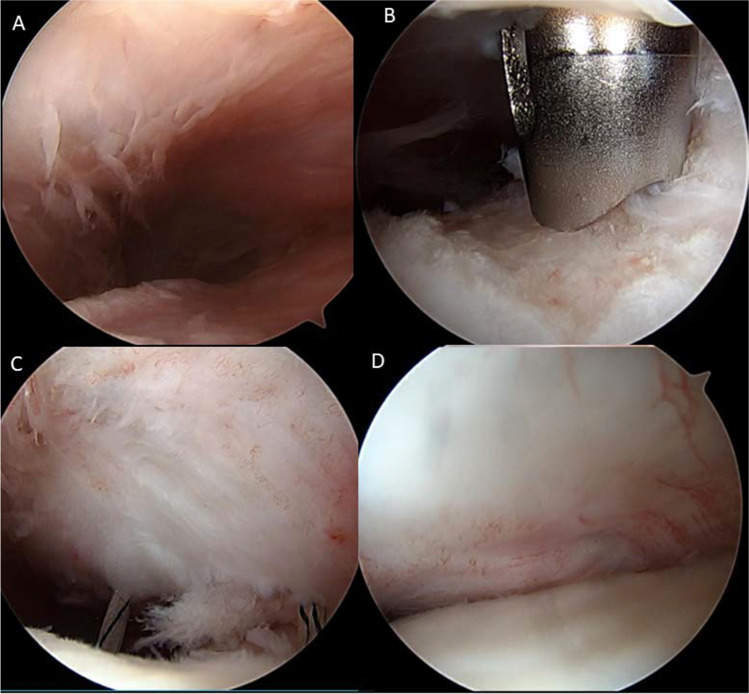
One method of arthroscopically addressing the Hill-Sachs lesion involves filling the humeral head defect with the posterior capsule and infraspinatus tendon, known as the remplissage procedure [64]. The indications for adding a remplissage procedure to a Bankart repair are evolving, but most authors support its use when a Hill-Sachs lesion is found to be engaging, with subcritical glenoid bone loss [48]. An engaging Hill-Sachs lesion is one that the size and orientation of the lesion is such that during arthroscopic evaluation it engages the anterior glenoid when the shoulder is in 90 degrees of abduction and external rotation [12]. Promising results have been reported in the adult literature including a recent randomized-controlled trial (RCT) by MacDonald et al. who randomized patients 14 years of age or older with recurrent instability, engaging Hill-Sachs lesions, and minimal glenoid bone loss to either arthroscopic Bankart repair alone or arthroscopic Bankart repair with remplissage [51]. The study reported significantly higher rates of recurrent instability in the isolated arthroscopic Bankart group (18%) compared to the remplissage group (4%; p = 0.027). While patients with remplissage had decreased external rotation at 12 months, there was no difference in range of motion, complications, patient-reported outcomes or shoulder function between the two groups at 2 years post-operative [51]. Hughes et al. assessed 21 adolescent patients who had undergone an arthroscopic remplissage and Bankart repair and compared these retrospectively to 20 matched controls who had underdone arthroscopic Bankart repair alone [37]. The group of adolescents who had undergone remplissage had a significantly lower rate of recurrence (13%) compared to those with arthroscopic Bankart alone (47%) [37]. There was no significant difference in patient-reported outcomes scores between the two groups [37]. The authors of this study recommend addition of remplissage to an arthroscopic Bankart repair in young, active, non-thrower patients with large, engaging Hill-Sachs lesions. While the potential to decrease the rates of recurrent instability in this high-risk population is promising, the potential of limiting shoulder external rotation, particularly in young throwers, is something that must be considered as part of the clinical decision making. While these studies present encouraging data on the use of remplissage, it must be kept in mind that these reports are limited by low sample size and further well-designed research is necessary to determine the benefits, and drawbacks and broader indications for the remplissage procedure in adolescents (Fig. 1).
Fig. 1.
Arthroscopic images of a remplissage procedure for a large Hill-Sachs lesion in an adolescent athlete. A Large Hill-Sachs lesion. B Placement of suture anchor. C Sutures from two suture anchors through the posterior capsule and infraspinatus tendon prior to tensioning. D Tensioned sutures filling the Hill-Sachs defect with the posterior capsule and infraspinatus tendon
Open Bankart Repair and Capsulorrhaphy
Although open stabilization procedures had been the mainstay of surgical management for anterior glenohumeral instability for many years [67, 75], advances in arthroscopic techniques have led to substantially more arthroscopic stabilization procedures than open procedures in the pediatric and adolescent populations in recent years [73]. However, the relatively high rates of recurrent instability following arthroscopic Bankart repair in young, active patients have led some to revisit primary open Bankart repair in these populations [31, 33]. A previous randomized-controlled trial in adults by Mohtadi et al. found that open soft-tissue stabilization resulted in a significantly lower risk of recurrence compared to arthroscopic stabilization, and recommended consideration of open stabilization for those at highest risk of recurrent instability [56]. Hickey et al. assessed 34 male adolescents (aged 15 to 18) participating in collision sports who had undergone open Bankart repair. While 8 (23.5%) had a re-dislocation with 4 (12%) requiring revision stabilization, the study found excellent functional outcomes and high rates of patient satisfaction [33]. Overall, 90% were able to return to sport at a mean of 5.8 months post-operative [33]. Hatch et al. assessed 21 adolescent patients aged 14 to 18 years who had undergone open Bankart repair and reported excellent functional outcomes in 100% of patients with no cases of recurrent instability [31]. However, 34% of patients lost a mean of 11° of external rotation [31]. Monk et al. reported retrospective outcomes for 60 adolescent (15 to 20 years) collision athletes who had undergone open Bankart repair. Eight (13%) had a re-dislocation, with 4 (7%) requiring revision stabilization [57]. Furthermore, strong functional outcomes were reported with 92% returning to sport with 62% able to return to their previous level of sport at a mean of 14 months [57]. Given the long-term track record of open stabilization, the authors of this review consider open Bankart repair and capsulorrhaphy in patients at highest risk of re-dislocation particularly in the revision setting without significant bone loss.
Open Glenoid Augmentation
Although soft tissue Bankart repair for anterior instability is the most common procedure utilized in the pediatric and adolescent populations, some patients including those with significant glenoid bone loss or failed prior arthroscopic stabilization may warrant osseous glenoid reconstruction using coracoid bone grafts, also known as the Latarjet procedure [50, 79••]. In patients found to have any degree of glenoid bone loss on radiographs or MRI, it is helpful to obtain CT scans with 3D reconstruction and humeral head subtraction to accurately measure the degree of glenoid bone loss pre-operatively. In older patients, several studies have demonstrated good outcomes and lower rates of recurrent instability following the Latarjet procedure in the setting of significant bone loss, particularly compared to arthroscopic Bankart repair [6, 7, 17, 45, 62]. However, until recently, there had been limited literature evaluating the safety and efficacy of the Latarjet procedure in the pediatric and adolescent populations. A study published in 2022 by Waltenspül et al. has demonstrated good to excellent functional outcomes, range of motion and satisfaction as well as significantly lower rates of recurrent instability (6%) following the Latarjet procedure in 30 adolescent patients compared to adolescents that had undergone arthroscopic Bankart repair (57%) [79••]. In terms of complications in the Latarjet group, 4 (13%) required screw removal, 1 (3%) had a coracoid block fracture and 1 (3%) had an axillary nerve palsy that resolved spontaneously [79••]. In an unpublished study from the current institution, 18 adolescent patients who had undergone the open Latarjet procedure were compared to a control group of patients with similar presenting features who had undergone alternative procedures. Despite the patients in the Latarjet group having more severe bone loss, including a higher proportion with “off-track” bony instability, the rate of recurrent instability was not significantly different between the Latarjet group (17%) and the control group (23%). Furthermore, adolescents in the Latarjet group reported excellent functional outcomes, patient satisfaction and a 94% rate of return to sport, similar to that in the control group. In terms of complications, there were no instances of coracoid graft fracture, non-union or nerve palsy/deficit in those who underwent the Latarjet, compared to one non-union following bony Bankart ORIF in the control group [32]. An example of a post-operative radiograph following a Latarjet procedure for a 15-year-old adolescent athlete with recurrent instability and glenoid bone loss in the setting of prior arthroscopic Bankart repair is shown in Fig. 2. Given the increased use of the Latarjet procedure in adolescents in recent years, some may question how young can patients be, and whether or not the Latarjet can be done in skeletally immature patients. Domos et al. retrospectively assessed 45 skeletally immature patients between 13 and 17 years of age who had undergone an open Latarjet procedure [24]. The authors reported a low rate of recurrent instability (4%), with no evidence of glenoid growth disturbance or deformity at a median follow-up of 6.6 years [24]. Despite these promising results, some have cautioned for careful selection of adolescent patients for Latarjet procedures based on the amount of glenoid and humeral bone loss, failure of previous stabilization procedures and nature of sports participation given the paucity of long-term literature available in the adolescent population. Higher activity levels and smaller coracoid graft sizes have been postulated as factors that may lead to a greater risk for coracoid graft-related complications [30]. Furthermore, the consequences of a long-term nerve injury are particularly important in this population [30]. In addition, revision of a failed Laterjet procedure may be more complicated, potentially requiring the use of distal tibial allograft or iliac crest bone graft. Therefore, the Latarjet procedure is an option that needs more research, however, should be considered for adolescent patients with significant glenoid bone loss and those that have failed prior stabilization. Larger studies with longer-term outcomes are warranted before broadening the indications to a larger group of patients.
Fig. 2.
Post-operative radiographs following a Latarjet procedure for a 15-year-old adolescent athlete with recurrent glenohumeral instability and glenoid bone loss following prior arthroscopic Bankart repair
Multidirectional Instability
MDI can be a debilitating condition that involves a spectrum from subluxation to frank dislocation of the glenohumeral joint in more than one direction [8]. The majority of pediatric and adolescent patients with MDI do not typically require a reduction maneuver for their shoulder dislocations/subluxations. A careful history and examination is important in these patients to assess for family histories of connective tissue disorders such as Ehlers Danlos syndrome which may change the management and prognosis for the patient who has recurrent shoulder instability. The physical exam should include an assessment of Beighton’s criteria [5], which has a maximum score of 9 points, with scores greater than or equal to 4 points indicative of hyperlaxity. Those with hyperlaxity should be further assessed with examination of the skin for dystrophic scars, brown discolouration, striae and subcutaneous spheroids. Furthermore, a cardiac examination should be performed to assess for vessel or valve abnormalities [72]. MR arthrography findings including a patulous capsule typically without labral abnormalities can be indicative of MDI [23]; however, imaging findings in patients with MDI may be difficult to interpret, and it is therefore important to interpret findings in the context of the clinical history and physical examination [54]. In a recent ultrasound study comparing patients with MDI secondary to hypermobile type Ehlers Danlos syndrome to healthy controls, those with MDI were found to have greater subacromial distances with inferior subluxation of the humeral head. The findings of the study could be helpful for targeted rehabilitation programs as they suggest symptoms in patients with MDI may be related more to the inferior subluxation resulting in decreased range of motion rather than from impingement of the shoulder [42]. Patients with MDI typically report instability episodes in mid-range of motion which implies a deficit in the concavity compression role of the rotator cuff in pulling the humerus into the glenoid. This is in contrast to traumatic shoulder dislocations which typically occur at end range of motion and result in torn soft tissues including the labrum, glenohumeral ligaments, and/or capsule.
Most sports medicine providers consider rehabilitation and physical therapy to be the mainstay of initial treatment for patients with MDI. These programs typically focus on periscapular strengthening, postural work, biofeedback and rotator cuff strengthening. Published rehabilitation programs for patients with MDI with enough detail to replicate clinically include the Watson MDI program [83], the Rockwood instability program [13] and the Derby shoulder instability program [3]. Watson et al. assessed 43 adolescents and young adults (mean age 19.8 years) with MDI who had undergone conservative management with a directed exercise program and reported strong outcomes with significant improvements in mean functional outcomes, scapular positioning, and muscle strength [82]. A randomized trial of adolescents and young adults with MDI comparing the Watson and Rockwood programs found that the Watson program was significantly more effective than the Rockwood program in terms of functional instability-specific outcomes, and pain [80]. It is generally recommended that conservative treatment be utilized for a minimum of 6 months for young patients with MDI. Although physical therapy and rehabilitation provides good to excellent results for many young patients, there are those for which non-operative treatment fails to restore adequate stability and function.
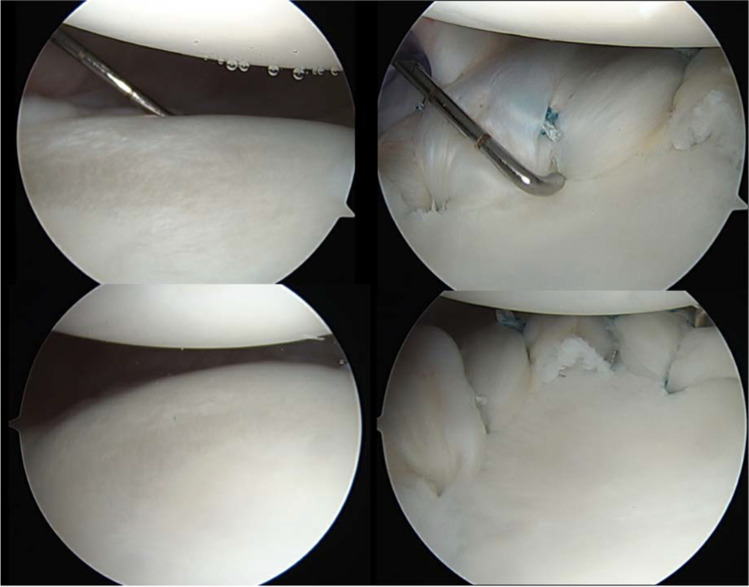
In young patients who fail the above and continue to have symptoms of instability and pain that affects daily activities or sports, surgical management may be considered. Traditionally, surgical management for patients with MDI included open inferior capsular shift [58]. Vavken et al. examined 15 adolescent patients (18 shoulders) who had failed nonsurgical management and had undergone open stabilization with inferior capsular shift [77]. At a mean of 7.5 years post-operative, 87% had improved pain and stability, with mean American Shoulder and Elbow Surgeons scores of 88, and 11-item QuickDASH scores of 14 points [77]. Overall, 60% of patients were able to return to sport, with only 36% returning to prior level of sport participation. While no revision stabilization surgery was required, 47% of patients reported residual subluxation post-operatively [77]. Although an open inferior capsular shift allows for direct capsulorrhaphy which obliterates the inferior pouch and reduces capsular redundancy anteriorly and inferiorly, there are advantages to an arthroscopic approach as well. Patients with MDI should be evaluated preoperatively to determine their primary direction of symptomatic instability. Often, these patients are globally unstable; however, their symptoms can be defined by the primary direction of instability for these patients preoperatively, such as MDI with predominant anterior inferior or MDI with predominant posterior inferior instability. Patients with MDI often have loss of containment of the chondrolabral portion of the glenoid which is associated with reduced labral height in the direction of primary instability [41]. Arthroscopic capsulorrhaphy allows for identification and treatment of any identified intra-articular pathology and allows the surgeon to tailor the capsulorrhaphy to the predominant direction of instability. In addition, an arthroscopic capsulorrhaphy may allow the surgeon to simultaneously tighten the posterior, inferior and anterior capsule to balance the capsular shift better than a direct open anterior approach. Mitchell et al. studied 42 adolescents (50 shoulders) who were refractory to nonsurgical management and had undergone arthroscopic stabilization for MDI at a mean of 6.3 years post-operative [55•]. The reported clinical outcomes were promising with mean SANE scores of 83, PASS scores of 85 and QuickDASH scores of 6.8. Overall, 56% of patients were able to return to their previous level of sport and recurrent instability requiring revision surgical stabilization was reported in 26% of patients [55•]. Further research is necessary to determine the role and benefits for arthroscopic versus open capsulorrhaphy in the various different patient populations and MDI presentation including those with connective tissue disorders, athletes, those with primary posterior inferior instability and those globally and equally unstable in multiple directions. Figure 3 depicts arthroscopic images of an anterior and posterior capsulorrhaphy performed in an adolescent patient with MDI who had failed an extensive course of non-operative management.
Fig. 3.
Arthroscopic images before and after anterior and posterior capsulorraphy using suture anchors in an adolescent patient with multidirectional instability (MDI)
Conclusion
Shoulder instability, including traumatic anterior dislocations and MDI, is common in pediatric and adolescent patients. It is well-established that young patients with anterior shoulder dislocation are at high risk of recurrent instability. Pediatric and adolescent patients have excellent outcomes and high rates of return to sport following arthroscopic Bankart repair; however, higher rates of recurrent instability requiring revision surgical management have been identified in patients with more than one dislocation episode pre-operatively, those with Hill-Sachs lesions, and those under age 16. Recent literature suggests that the arthroscopic remplissage and Latarjet procedures have promising results in the pediatric and adolescent populations with large Hill-Sachs lesions, glenoid bone loss, and those failing primary surgical management. Attentive selection of timing and type of surgical management for pediatric and adolescent patients with anterior shoulder instability may help to prevent recurrent instability following shoulder stabilization. Although most pediatric and adolescent patients with MDI do well following non-surgical management alone, those that fail conservative management have good outcomes following arthroscopic or open capsulorrhaphy.
Declarations
Conflict of Interest
Jeffrey Kay M.D., M.Sc., F.R.C.S.C.: No conflict of interest to disclose. Benton E. Heyworth, M.D.: Imagen Technologies, Inc.—Dr. Heyworth is a consultant and stock owner; Arthrex, Inc. and Kairos Surgical—Educational Consultant, educational fees (2019); Springer Science & Business Media—Royalties (textbook-related); Pediatric Research in Sports Medicine (PRISM)—Dr. Heyworth was a Board of Directors member (Director-At-Large); Pediatric Orthopaedic Society of North America (POSNA)—Dr. Heyworth was a committee member (QSVI Trauma—2021) and committee chair (Mentorship, 2021–22). Matthew D. Milewski, M.D.: Editorial royalties, Elsevier, Inc. Board of Directors, Pediatric Research in Sports Medicine Society. Dennis E. Kramer, M.D.: Kairos surgical—educational support.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jeffrey Kay, Email: jeffrey.kay@medportal.ca.
Benton E. Heyworth, Email: benton.heyworth@childrens.harvard.edu
Matthew D. Milewski, Email: matthew.milewski@childrens.harvard.edu
Dennis E. Kramer, Email: dennis.kramer@childrens.harvard.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Bak K. Nontraumatic glenohumeral instability and coracoacromial impingement in swimmers. Scand J Med Sci Sports. 2007;6(3):132–144. doi: 10.1111/j.1600-0838.1996.tb00081.x. [DOI] [PubMed] [Google Scholar]
- 2.Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Jt Surg Br. 2007;89(11):1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 3.Bateman M, Smith BE, Osborne SE, Wilkes SR. Physiotherapy treatment for atraumatic recurrent shoulder instability: early results of a specific exercise protocol using pathology-specific outcome measures. Shoulder Elb. 2015;7(4):282–288. doi: 10.1177/1758573215592266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beeson MS. Complications of shoulder dislocation. Am J Emerg Med. Published online 1999.10.1016/S0735-6757(99)90127-4. [DOI] [PubMed]
- 5.Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969;51(3):444–453. doi: 10.1302/0301-620X.51B3.444. [DOI] [PubMed] [Google Scholar]
- 6.Bessière C, Trojani C, Carles M, Mehta SS, Boileau P. The open Latarjet procedure is more reliable in terms of shoulder stability than arthroscopic Bankart repair. Clin Orthop Relat Res. 2014;472:2345–2351. doi: 10.1007/s11999-014-3550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bessiere C, Trojani C, Pélégri C, Carles M, Boileau P. Coracoid bone block versus arthroscopic Bankart repair: a comparative paired study with 5-year follow-up. Orthop Traumatol Surg Res. 2013;99(2):123–130. doi: 10.1016/j.otsr.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Best MJ, Tanaka MJ. Multidirectional instability of the shoulder: treatment options and considerations. Sports Med Arthrosc. 2018;26(3):113–119. doi: 10.1097/JSA.0000000000000199. [DOI] [PubMed] [Google Scholar]
- 9.Boone JL, Arciero RA. First-time anterior shoulder dislocations: has the standard changed? Br J Sports Med. 2010;44(5):355–360. doi: 10.1136/bjsm.2009.062596. [DOI] [PubMed] [Google Scholar]
- 10.Brunner UH. Arthropathy of instability. Causes, treatment options and results. Orthopade. Published online 2009. 10.1007/s00132-008-1359-5. [DOI] [PubMed]
- 11.Burkhart SS. Editorial Commentary: Off-Track Hill-Sachs lesions in adolescents with multiple anterior dislocations: the case for stabilizing adolescent first-time dislocators. Arthrosc J Arthrosc Relat Surg. 2017;33(10):1762–1763. doi: 10.1016/j.arthro.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs. Arthrosc J Arthrosc Relat Surg. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 13.Burkhead WZ, Rockwood CA. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74(6):890–896. http://www.ncbi.nlm.nih.gov/pubmed/1634579. [PubMed]
- 14.Carli A De, Vadalà AP, Lanzetti R, et al. Early surgical treatment of first-time anterior glenohumeral dislocation in a young, active population is superior to conservative management at long-term follow-up. IntOrthop. Published online 2019. 10.1007/s00264-019-04382-2. [DOI] [PubMed]
- 15.Cartucho A, Moura N, Sarmento M. Evaluation and management of failed shoulder instability surgery. Open Orthop J. Published online 2017. 10.2174/1874325001711010897. [DOI] [PMC free article] [PubMed]
- 16.Castagna A, Delle Rose G, Borroni M, et al. Arthroscopic stabilization of the shoulder in adolescent athletes participating in overhead or contact sports. Arthrosc J Arthrosc Relat Surg. 2012;28(3):309–315. doi: 10.1016/j.arthro.2011.08.302. [DOI] [PubMed] [Google Scholar]
- 17.Cerciello S, Edwards TB, Walch G. Chronic anterior glenohumeral instability in soccer players: results for a series of 28 shoulders treated with the Latarjet procedure. J Orthop Traumatol. 2012;13(4):197–202. doi: 10.1007/s10195-012-0201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng TT, Edmonds EW, Bastrom TP, Pennock AT. Glenoid pathology, skeletal immaturity, and multiple preoperative instability events are risk factors for recurrent anterior shoulder instability after arthroscopic stabilization in adolescent athletes. Arthrosc J Arthrosc Relat Surg. 2021;37(5):1427–1433. doi: 10.1016/j.arthro.2020.12.211. [DOI] [PubMed] [Google Scholar]
- 19.Cleeman E, Flatow EL. Shoulder dislocations in the young patient. Orthop Clin North Am. 2000;31(2):217–229. doi: 10.1016/S0030-5898(05)70142-5. [DOI] [PubMed] [Google Scholar]
- 20.Cordasco FA, Lin B, Heller M, Asaro LA, Ling D, Calcei JG. Arthroscopic shoulder stabilization in the young athlete: return to sport and revision stabilization rates. J Shoulder Elb Surg. 2020;29(5):946–953. doi: 10.1016/j.jse.2019.09.033. [DOI] [PubMed] [Google Scholar]
- 21.Deitch J, Mehlman CT, Foad SL, Obbehat A, Mallory M. Traumatic anterior shoulder dislocation in adolescents. Am J Sports Med. Published online 2003. 10.1177/03635465030310052001. [DOI] [PubMed]
- 22.Denard PJ, Dai X, Burkhart SS. Increasing preoperative dislocations and total time of dislocation affect surgical management of anterior shoulder instability. Int J Shoulder Surg. Published online 2015. 10.4103/0973-6042.150215. [DOI] [PMC free article] [PubMed]
- 23.Dewing CB, McCormick F, Bell SJ, et al. An analysis of capsular area in patients with anterior, posterior, and multidirectional shoulder instability. Am J Sports Med. 2008;36(3):515–522. doi: 10.1177/0363546507311603. [DOI] [PubMed] [Google Scholar]
- 24.Domos P, Chelli M, Lunini E, et al. Clinical and radiographic outcomes of the open Latarjet procedure in skeletally immature patients. J Shoulder Elb Surg. 2020;29(6):1206–1213. doi: 10.1016/j.jse.2019.09.039. [DOI] [PubMed] [Google Scholar]
- 25.Egger AC, Willimon SC, Busch MT, Broida S, Perkins CA. Arthroscopic Bankart repair for adolescent anterior shoulder instability: clinical and imaging predictors of revision surgery and recurrent subjective instability. Am J Sports Med. 2023;51(4):877–884. doi: 10.1177/03635465231151250. [DOI] [PubMed] [Google Scholar]
- 26.Emery R, Mullaji A. Glenohumeral joint instability in normal adolescents. Incidence and significance. J Bone Joint Surg Br. 1991;73-B(3):406–408. doi: 10.1302/0301-620X.73B3.1670438. [DOI] [PubMed] [Google Scholar]
- 27.Franklin CC, Weiss JM. The natural history of pediatric and adolescent shoulder dislocation. J Pediatr Orthop. 2019;39(Supplement 1):S50–S52. doi: 10.1097/BPO.0000000000001374. [DOI] [PubMed] [Google Scholar]
- 28.Gigis I, Heikenfeld R, Kapinas A, Listringhaus R, Godolias G. Arthroscopic versus conservative treatment of first anterior dislocation of the shoulder in adolescents. J Pediatr Orthop. Published online 2014. 10.1097/BPO.0000000000000108. [DOI] [PubMed]
- 29.Goldberg AS, Moroz L, Smith A, Ganley T. Injury surveillance in young athletes: a clinician’s guide to sports injury literature. Sport Med. Published online 2007. 10.2165/00007256-200737030-00005. [DOI] [PubMed]
- 30.Hanson JA, Foster MJ, Pearce SS, Millett PJ. Primary Latarjet for anterior shoulder instability in adolescents: an unstable conclusion. J Bone Jt Surg. 2022;104(12):1129–1129. doi: 10.2106/JBJS.22.00370. [DOI] [PubMed] [Google Scholar]
- 31.Hatch MD, Hennrikus WL. The open Bankart repair for traumatic anterior shoulder instability in teenage athletes. J Pediatr Orthop. 2018;38(1):27–31. doi: 10.1097/BPO.0000000000000744. [DOI] [PubMed] [Google Scholar]
- 32.Heyworth BE, Wu M, Kramer DE, Bae DS. The Latarjet procedure for anterior shoulder instability in pediatric and adolescent athletes. Orthop J Sport Med. 2018;6(7_suppl4):2325967118S0012. doi: 10.1177/2325967118S00127. [DOI] [Google Scholar]
- 33.Hickey IPM, Davey MS, Hurley ET, Gaafar M, Delaney RA, Mullett H. Return to play following open Bankart repair in collision athletes aged 18 years or less. J Shoulder Elb Surg. 2022;31(6):S8–S12. doi: 10.1016/j.jse.2021.11.001. [DOI] [PubMed] [Google Scholar]
- 34.Hinds N, Angioi M, Birn-Jeffery A, Twycross-Lewis R. A systematic review of shoulder injury prevalence, proportion, rate, type, onset, severity, mechanism and risk factors in female artistic gymnasts. Phys Ther Sport. 2019;35:106–115. doi: 10.1016/j.ptsp.2018.11.012. [DOI] [PubMed] [Google Scholar]
- 35.Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. J Bone Jt Surgery-American. 2008;90(5):945–952. doi: 10.2106/JBJS.G.00070. [DOI] [PubMed] [Google Scholar]
- 36.Hovelius L, Saeboe M. Neer Award 2008: Arthropathy after primary anterior shoulder dislocation-223 shoulders prospectively followed up for twenty-five years. J Shoulder Elb Surg. Published online 2009. 10.1016/j.jse.2008.11.004. [DOI] [PubMed]
- 37.Hughes JL, Bastrom T, Pennock AT, Edmonds EW. Arthroscopic Bankart repairs with and without remplissage in recurrent adolescent anterior shoulder instability with Hill-Sachs deformity. Orthop J Sport Med. 2018;6(12):232596711881398. doi: 10.1177/2325967118813981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kao JT, Chang CL, Su WR, Chang WL, Tai TW. Incidence of recurrence after shoulder dislocation: a nationwide database study. J Shoulder Elb Surg. Published online 2018. 10.1016/j.jse.2018.02.047. [DOI] [PubMed]
- 39.Kawasaki T, Ota C, Urayama S, et al. Incidence of and risk factors for traumatic anterior shoulder dislocation: an epidemiologic study in high-school rugby players. J Shoulder Elb Surg. Published online 2014. 10.1016/j.jse.2014.05.007. [DOI] [PubMed]
- 40.Khan A, Samba A, Pereira B, Canavese F. Anterior dislocation of the shoulder in skeletally immature patients: comparison between non-operative treatment versus open latarjet’s procedure. Bone Jt J. Published online 2014. 10.1302/0301-620X.96B3. [DOI] [PubMed]
- 41.Kim SH, Noh KC, Park JS, Ryu BD, Oh I. Loss of chondrolabral containment of the glenohumeral joint in atraumatic posteroinferior multidirectional instability. J Bone Jt Surg. 2005;87(1):92–98. doi: 10.2106/JBJS.C.01448. [DOI] [PubMed] [Google Scholar]
- 42.Kjær BH, de Wandele I, Spanhove V, Juul-Kristensen B, Cools AM. Subacromial space outlet in female patients with multidirectional instability based on hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorder measured by ultrasound. J Shoulder Elb Surg. 2020;29(3):600–608. doi: 10.1016/j.jse.2019.08.003. [DOI] [PubMed] [Google Scholar]
- 43.Kramer J, Gajudo G, Pandya NK. Risk of recurrent instability after arthroscopic stabilization for shoulder instability in adolescent patients. Orthop J Sport Med. 2019;7(9):232596711986899. doi: 10.1177/2325967119868995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kraus R, Pavlidis T, Heiss C, Kilian O, Schnettler R. Arthroscopic treatment of post-traumatic shoulder instability in children and adolescents. Knee Surgery, Sport Traumatol Arthrosc. 2010;18(12):1738–1741. doi: 10.1007/s00167-010-1092-6. [DOI] [PubMed] [Google Scholar]
- 45.Kukkonen J, Elamo S, Flinkkilä T, et al. Arthroscopic Bankart versus open Latarjet as a primary operative treatment for traumatic anteroinferior instability in young males: a randomised controlled trial with 2-year follow-up. Br J Sports Med. 2022;56(6):327–333. doi: 10.1136/bjsports-2021-104028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lampert C, Baumgartner G, Slongo T, Kohler G, Horst M. Traumatic shoulder dislocation inchildren and adolescents. Eur J Trauma. Published online 2003. 10.1007/s00068-003-1218-3.
- 47.Lau BC, Conway D, Curran PF, Feeley BT, Pandya NK. Bipolar bone loss in patients with anterior shoulder dislocation: a comparison of adolescents versus adult patients. Arthrosc J Arthrosc Relat Surg. 2017;33(10):1755–1761. doi: 10.1016/j.arthro.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 48.Lazarides AL, Duchman KR, Ledbetter L, Riboh JC, Garrigues GE. Arthroscopic remplissage for anterior shoulder instability: a systematic review of clinical and biomechanical studies. Arthrosc J Arthrosc Relat Surg. 2019;35(2):617–628. doi: 10.1016/j.arthro.2018.09.029. [DOI] [PubMed] [Google Scholar]
- 49.Leroux T, Ogilvie-Harris D, Veillette C, et al. The epidemiology of primary anterior shoulder dislocations in patients aged 10 to 16 years. Am J Sports Med. 2015;43(9):2111–2117. doi: 10.1177/0363546515591996. [DOI] [PubMed] [Google Scholar]
- 50.Levy DM, Cole BJ, Bach BR. History of surgical intervention of anterior shoulder instability. J Shoulder Elb Surg. 2016;25(6):e139–e150. doi: 10.1016/j.jse.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 51.MacDonald P, McRae S, Old J, et al. Arthroscopic Bankart repair with and without arthroscopic infraspinatus remplissage in anterior shoulder instability with a Hill-Sachs defect: a randomized controlled trial. J Shoulder Elb Surg. 2021;30(6):1288–1298. doi: 10.1016/j.jse.2020.11.013. [DOI] [PubMed] [Google Scholar]
- 52.Marans HJ, Angel KR, Schemitsch EH, Wedge JH. The fate of traumatic anterior dislocation of the shoulder in children. J Bone Joint Surg Am. 1992;74(8):1242–1244. http://www.ncbi.nlm.nih.gov/pubmed/1400553. [PubMed]
- 53.Meeusen R, Borms J. Gymnastic injuries. Sport Med. 1992;13(5):337–356. doi: 10.2165/00007256-199213050-00004. [DOI] [PubMed] [Google Scholar]
- 54.Milewski MD, Nissen CW. Pediatric and adolescent shoulder instability. Clin Sports Med. 2013;32(4):761–779. doi: 10.1016/j.csm.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 55.Mitchell BC, Siow MY, Carroll AN, Pennock AT, Edmonds EW. Clinical outcomes, survivorship, and return to sport after arthroscopic capsular repair with suture anchors for adolescent multidirectional shoulder instability: results at 6-year follow-up. Orthop J Sport Med. 2021;9(2):232596712199387. doi: 10.1177/2325967121993879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohtadi NGH, Chan DS, Hollinshead RM, et al. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability. J Bone Jt Surg. 2014;96(5):353–360. doi: 10.2106/JBJS.L.01656. [DOI] [PubMed] [Google Scholar]
- 57.Monk AP, Crua E, Gatenby GC, et al. Clinical outcomes following open anterior shoulder stabilization for glenohumeral instability in the young collision athlete. J Shoulder Elb Surg. 2022;31(7):1474–1478. doi: 10.1016/j.jse.2021.12.013. [DOI] [PubMed] [Google Scholar]
- 58.Neer CS, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. J Bone Jt Surgery-American. 2001;83(10):1586. doi: 10.2106/00004623-200110000-00021. [DOI] [PubMed] [Google Scholar]
- 59.Olds M, Donaldson K, Ellis R, Kersten P. In children 18 years and under, what promotes recurrent shoulder instability after traumatic anterior shoulder dislocation? A systematic review and meta-analysis of risk factors. Br J Sports Med. 2016;50(18):1135–1141. doi: 10.1136/bjsports-2015-095149. [DOI] [PubMed] [Google Scholar]
- 60.Owens BD, DeBerardino TM, Nelson BJ, et al. Long-term follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocations in young athletes. Am J Sports Med. 2009;37(4):669–673. doi: 10.1177/0363546508328416. [DOI] [PubMed] [Google Scholar]
- 61.Owens BD, Harrast JJ, Hurwitz SR, Thompson TL, Wolf JM. Surgical trends in Bankart repair: an analysis of data from the American board of orthopaedic surgery certification examination. Am J Sports Med. Published online 2011.10.1177/0363546511406869. [DOI] [PubMed]
- 62.Paul RW, Reddy MP, Sonnier JH, et al. Increased rates of subjective shoulder instability after Bankart repair with remplissage compared to Latarjet surgery. J Shoulder Elb Surg. Published online December 2022. 10.1016/j.jse.2022.11.001. [DOI] [PubMed]
- 63.Postacchini F, Gumina S, Cinotti G. Anterior shoulder dislocation in adolescents. J Shoulder Elb Surg. Published online 2000. doi:10.1067/mse.2000.108385. [DOI] [PubMed]
- 64.Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-Sachs “Remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion. Arthrosc J Arthrosc Relat Surg. 2008;24(6):723–726. doi: 10.1016/j.arthro.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 65.Roberts SB, Beattie N, McNiven ND, Robinson CM. The natural history of primary anterior dislocation of the glenohumeral joint in adolescence.Bone Jt J. Published online 2015. 10.1302/0301-620X.97B4.34989. [DOI] [PubMed]
- 66.Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Jt Surg - Ser A. Published online 2006. 10.2106/JBJS.E.01327. [DOI] [PubMed]
- 67.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60(1):1–16. http://www.ncbi.nlm.nih.gov/pubmed/624747. [PubMed]
- 68.Sachs RA, Lin D, Stone M Lou, Paxton E, Kuney M. Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Jt Surg - Ser A. Published online 2007. 10.2106/JBJS.F.00261. [DOI] [PubMed]
- 69.Saper MG, Milchteim C, Zondervan RL, Andrews JR, Ostrander RV. Outcomes after arthroscopic Bankart repair in adolescent athletes participating in collision and contact sports. Orthop J Sport Med. 2017;5(3):232596711769795. doi: 10.1177/2325967117697950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schwihla I, Wieser K, Grubhofer F, Zimmermann SM. Long-term recurrence rate in anterior shoulder instability after Bankart repair based on the on- and off-track concept. J Shoulder Elb Surg. 2023;32(2):269–275. doi: 10.1016/j.jse.2022.07.025. [DOI] [PubMed] [Google Scholar]
- 71.Shanmugaraj A, Chai D, Sarraj M, et al. Surgical stabilization of pediatric anterior shoulder instability yields high recurrence rates: a systematic review. Knee Surgery, Sport Traumatol Arthrosc. Published online 2020. 10.1007/s00167-020-05913-w. [DOI] [PubMed]
- 72.Shirley ED, DeMaio M, Bodurtha J. Ehlers-Danlos syndrome in orthopaedics. Sport Heal A Multidiscip Approach. 2012;4(5):394–403. doi: 10.1177/1941738112452385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Smith HE, Morgan AM, Patel NM. On the rise: the increasing frequency of pediatric shoulder stabilization surgery in children and adolescents. Orthopedics. Published online January 10, 2023:1–6. 10.3928/01477447-20230104-04. [DOI] [PubMed]
- 74.Smucny M, Kolmodin J, Saluan P. Shoulder and elbow injuries in the adolescent athlete. Sports Med Arthrosc. 2016;24(4):188–194. doi: 10.1097/JSA.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 75.Thomas SC, Matsen FA. An approach to the repair of avulsion of the glenohumeral ligaments in the management of traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 1989;71(4):506–513. http://www.ncbi.nlm.nih.gov/pubmed/2703510. [PubMed]
- 76.Torrance E, Clarke CJ, Monga P, Funk L, Walton MJ. Recurrence after arthroscopic labral repair for traumatic anterior instability in adolescent rugby and contact athletes. Am J Sports Med. Published online 2018.doi:10.1177/0363546518794673. [DOI] [PubMed]
- 77.Vavken P, Tepolt FA, Kocher MS. Open inferior capsular shift for multidirectional shoulder instability in adolescents with generalized ligamentous hyperlaxity or Ehlers-Danlos syndrome. J Shoulder Elb Surg. 2016;25(6):907–912. doi: 10.1016/j.jse.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 78.Voos JE, Livermore RW, Feeley BT, et al. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38(2):302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 79.Waltenspül M, Ernstbrunner L, Ackermann J, Thiel K, Galvin JW, Wieser K. Long-term results and failure analysis of the open latarjet procedure and arthroscopic Bankart repair in adolescents. J Bone Jt Surg. 2022;104(12):1046–1054. doi: 10.2106/JBJS.21.01050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Warby SA, Ford JJ, Hahne AJ, et al. Comparison of 2 Exercise rehabilitation programs for multidirectional instability of the glenohumeral joint: a randomized controlled trial. Am J Sports Med. 2018;46(1):87–97. doi: 10.1177/0363546517734508. [DOI] [PubMed] [Google Scholar]
- 81.Wasserstein D, Dwyer T, Veillette C, et al. Predictors of dislocation and revision after shoulder stabilization in Ontario, Canada, From 2003 to 2008. Am J Sports Med. 2013;41(9):2034–2040. doi: 10.1177/0363546513492952. [DOI] [PubMed] [Google Scholar]
- 82.Watson L, Balster S, Lenssen R, Hoy G, Pizzari T. The effects of a conservative rehabilitation program for multidirectional instability of the shoulder. J Shoulder Elb Surg. 2018;27(1):104–111. doi: 10.1016/j.jse.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 83.Watson L, Warby S, Balster S, Lenssen R, Pizzari T. The treatment of multidirectional instability of the shoulder with a rehabilitation program: Part 1. Shoulder Elb. 2016;8(4):271–278. doi: 10.1177/1758573216652086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: A new concept of glenoid track. J Shoulder Elb Surg. 2007;16(5):649–656. doi: 10.1016/j.jse.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 85.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Jt Surg - Ser A. Published online 2010. doi:10.2106/JBJS.I.00450. [DOI] [PubMed]