Abstract
Purpose
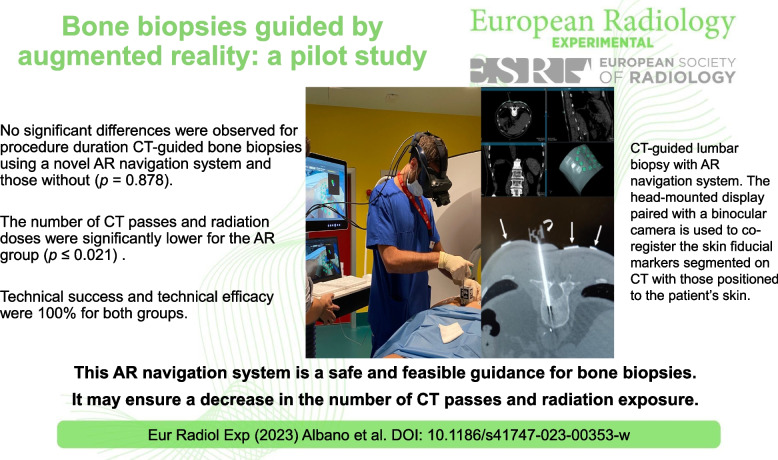
To test the technical feasibility of an augmented reality (AR) navigation system to guide bone biopsies.
Methods
We enrolled patients subjected to percutaneous computed tomography (CT)-guided bone biopsy using a novel AR navigation system. Data from prospectively enrolled patients (AR group) were compared with data obtained retrospectively from previous standard CT-guided bone biopsies (control group). We evaluated the following: procedure duration, number of CT passes, patient’s radiation dose (dose-length product), complications, and specimen adequacy. Technical success was defined as the ability to complete the procedure as planned, reaching the target center. Technical efficacy was assessed evaluating specimen adequacy.
Results
Eight patients (4 males) aged 58 ± 24 years (mean ± standard deviation) were enrolled in the AR group and compared with 8 controls (4 males) aged 60 ± 15 years. No complications were observed. Procedure duration, number of CT passes, and radiation dose were 22 ± 5 min, 4 (median) [4, 6 interquartile range] and 1,034 ± 672 mGy*cm for the AR group and 23 ± 5 min, 9 [7.75, 11.25], and 1,954 ± 993 mGy*cm for controls, respectively. No significant differences were observed for procedure duration (p = 0.878). Conversely, number of CT passes and radiation doses were significantly lower for the AR group (p < 0.001 and p = 0.021, respectively). Technical success and technical efficacy were 100% for both groups.
Conclusions
This AR navigation system is safe, feasible, and effective; it can decrease radiation exposure and number of CT passes during bone biopsies without increasing duration time.
Relevance statement
This augmented reality (AR) navigation system is a safe and feasible guidance for bone biopsies; it may ensure a decrease in the number of CT passes and patient’s radiation dose.
Key points
• This AR navigation system is a safe guidance for bone biopsies.
• It ensures decrease of number of CT passes and patient’s radiation exposure.
• Procedure duration was similar to that of standard CT-guided biopsy.
• Technical success was 100% as in all patients the target was reached.
• Technical efficacy was 100% as the specimen was adequate in all patients.
Graphical Abstract
Keywords: Augmented reality, Bone, Image-guided biopsy, Radiology (interventional), Tomography (x-ray computed)
Background
Imaging is essential in the diagnostic work-up of bone disorders, being also necessary as a guidance for biopsies of focal and diffuse bone lesions to obtain the final diagnosis [1–3]. Computed tomography (CT) is the best guidance when the cortical bone is intact or the lesion is particularly deep. It allows monitoring the needle path to reach the target lesion, avoiding nearby structures [4]. Nevertheless, CT guidance has non-negligible limitations: (i) the needle trajectory cannot be visualized real time unless CT fluoroscopy is used, which exposes both patient and operator to high radiation dose, (ii) its low contrast resolution in the soft tissues limits the visualization of vessels and nerves, and (iii) radiation exposure may be substantial, mostly being dependent on the number of scans performed during the procedure. Magnetic resonance imaging (MRI) has the advantages of avoiding radiation exposure also presenting higher contrast resolution in the soft tissues, but high costs, long procedural times, and the need for specific equipment have limited its application as a guidance for bone interventions [5]. Even ultrasound avoids radiation exposure and ensures real-time monitoring of needle trajectory [6–9] but cannot be used when the bone cortex is intact [10].
Several navigational system tools have been introduced to improve the accuracy, reliability, and safety of conventional imaging guidance [11, 12]. Image fusion platforms are based on electromagnetic or optical devices [13, 14], CT with laser marker systems [15], CT fluoroscopy [16], cone-beam CT [17], CT with electromagnetic tracking [18], and robotic systems [19] have been introduced in routine daily activity of several institutions. Nevertheless, these systems still present non-negligible drawbacks, including the inability to ensure a real-time (three-dimensional) 3D visualization of the needle, target, and nearby structures, together with the need to move the operator’s gaze from the interventional field and the screen [20]. Recently, technology advancements have led to the development of augmented reality (AR) navigation systems, which allows for real-time interaction by the operator, overlaying digital content onto the visualized real setting through a specific optical device [21, 22]. AR has been used to augment anatomical and pathological structures by creating 3D anatomic volumes from cross-sectional images and overlapping them over patients using advanced tracking systems (like electromagnetic or optical). Previous studies have tested AR on phantoms to guide percutaneous interventions [23, 24], but recently, this technology has been shown to be accurate and safe for guiding percutaneous thermal ablation of liver tumors in humans [25]. However, none of these studies has specifically dealt with bone biopsies.
Routinely, percutaneous CT-guided biopsies are performed as standard procedures for guideline-based diagnosis and subsequent therapy in the care of patients with bone tumors. Nevertheless, some drawback of these interventions should be pointed out. CT scans must be done repeatedly during a CT-guided percutaneous biopsy, to monitor the advancement of the needle, with a non-negligible amount of ionizing radiations. Furthermore, needle tracking and real-time image acquisition cannot be done, so that CT guided requires imaging interruption every time the patient is moved away from the gantry. AR navigation systems to guide bone biopsies have the potential of decreasing the number of CT passes to track the needle (thereby reducing radiation exposure) and procedure duration and also increasing the safety and efficacy of the procedure. Since a feasibility study on this relatively novel navigation system is needed before proceeding with a prospective randomized controlled study, the aim of this pilot study was to test the technical feasibility of Endosight, an advanced AR navigation system, in guiding a biopsy needle to bone lesions of the axial skeletal system.
Methods
Study design
This single-center cross-sectional prospective study was approved by our ethical committee (Protocol: ESBB1, Code number: NCT05732558, approved in 12 October 2022 by Ospedale San Raffaele, Milano, Italy), and all participants provided written informed consent for collection of data to be used for scientific purposes. After matching imaging and clinical data, our database was anonymized to remove any connections between data and patients’ identity according to the General Data Protection Regulation for Research Hospitals.
We prospectively enrolled consecutive patients admitted to the Radiology Department of IRCCS Ospedale Galeazzi-Sant’Ambrogio, Milan, Italy, to be subjected to percutaneous CT-guided bone biopsy in December 2022 and January 2023. Included patients were affected by bone lesion of the axial skeletal system and provided written informed consent to participate in the study. Exclusions criteria were as follows: (i) age < 18 years, (ii) pregnancy, (iii) breast feeding, and (iv) coagulation impairment. Data from prospectively enrolled patients (AR group) were compared with data obtained retrospectively from previous CT-guided bone biopsies performed at our institution between September 2021 and July 2022 (control group). In August 2022, our institution moved to another hospital. After that, there was a long period in which, due to internal rearrangement of our activities, CT-guided biopsies were performed only by orthopedic surgeons up to the start of this study. So, we preferred to include in the control group the last CT-guided biopsies done by the same radiologist that performed the biopsies of the AR group. To do that, our institutional database was searched for lesions with similar features of those included in AR group, i.e., patient of similar age and sex, similar anatomical location, similar size, and similar appearance (sclerotic/lytic, intact/disrupted cortical bone), subjected to conventional CT-guided biopsy. Patients from control group were considered as controls in this study.
Biopsy guided by the AR system
All biopsies of AR group were performed in the same CT suite (Revolution Ascend, GE Medical, Milwaukee, MI, USA) by a radiologist with 7 years of experience in CT-guided bone biopsies. The patients were placed on the CT bed based on the location of the bone lesion. After skin disinfection, the first CT scan was acquired after placing 20 specific fiducial Endosight markers on patient’s skin around the entry point of percutaneous biopsy (Fig. 1a and e, arrows). Then, preprocedural CT images were acquired ensuring to include all 20 Endosight markers and uploaded in the Endosight software. The Endosight AR navigation system (Endosight, R.A.W. Srl, Milan, Italy) is a CE marked system composed by a 27″ medical liquid crystal display (ACL, Leipzig, Germany), a high-performance laptop (Schenker DTR17 Schenker Technologies GmbH, Leipzig, Germany) equipped with Endosight software (Fig. 1b), and a commercially available head-mounted display (HMD) (HTC Vive Pro 2, HTC Corporation, Taoyuan C, Taiwan) paired with a binocular camera Basler Dart, Basler AG, Ahrensburg, Germany) (Fig. 1c, arrows). After uploading the pre-operation CT images in Endosight software, the volume of all anatomical structures is created allowing to recognize and highlight the target lesion, and to plan the needle path, together with its length and diameter (Fig. 1d). Then, the portion of patient’s skin is captured by the binocular cameras allowing the software to co-register all the fiducial Endosight markers applied to the patient’s skin with those previously segmented on the CT images (Fig. 1b). Endosight software is designed for two modes, liver and quick intervention. While liver mode is specifically designed for ablation procedures on the liver, the quick-intervention mode can be adapted to any percutaneous procedures involving a guided needle insertion. In the quick-intervention mode, used within this study, the software provided 3D reconstruction and automatic segmentation (from CT scans to 3D volumes) of the skin and of Endosight markers, and a semiautomatic segmentation of the target lesions. To monitor the correct position and angle of the needle during the procedure, an Endosight sensor was attached, thanks to a dedicated clamp, to the 8-G needle (15 cm in length, Jamshidi 8 G, HS Hospital Service, Italy), which was used to biopsy the bone lesion (Fig. 1c and e, curved arrow). The same radiologist performed all standard CT-guided bone biopsies of controls in a different CT suite, a 64-section CT system (Somatom Emotion, Siemens Medical Solutions, Erlangen, Germany).
Fig. 1.
A representative case with lumbar bone lesion from our study population. The fiducial markers are placed on patient’s skin around the entry point of percutaneous biopsy (arrows in a and e). The AR system (Endosight, R.A.W. Srl, Milan, Italy) consists of a 27″ medical display (ACL, Leipzig, Germany), a laptop (Dell Technologies, Round Rock, TX, USA) with AR software (b), and a commercially available head-mounted display (HMD) (Oculus Rift-S, Facebook Technologies, Menlo Park, CA, USA) paired with a binocular camera (Zed Mini, Stereolabs, San Francisco, CA, USA) (arrows in c) that is used to coregister the fiducial markers segmented on CT images with those positioned to the patient’s skin (b). The best needle trajectory to reach the target is built (d). A specific marker attached to the needle to monitor its position and angle during the procedure (curved arrows in c and e)
Data collection, sample size calculation, and statistical analysis
For each biopsy, we collected the following data:
elapsed time from local anesthesia to specimen withdrawal;
number of CT passes;
radiation dose administered to the patient measured by dose-length product (DLP, mGy*cm);
complications;
specimen adequacy;
height, weight, and body mass index (BMI) of AR group patients.
Concerning the retrospective evaluation of procedure duration, as per our routine during CT-guided bone biopsies, we use to acquire a first CT scan to show the correct position of the needle inserted for injecting local anesthesia and a last CT scan to show the final position of the needle that is used to biopsy the bone lesion. Hence, we can easily calculate the elapsed time from local anesthesia to specimen withdrawal just looking at the time of acquisition of the first and last CT images. Furthermore, we use to report the time of local anesthesia and the time of end of the procedure in a specific form.
Technical success was defined as the ability to complete the procedure as initially planned [11, 26] to reach the target lesion and to obtain a bioptic sample. Technical efficacy was assessed on the basis of specimen adequacy, as determined by the pathology report. Differences in terms of demographics, lesion characteristics, and procedure details were investigated between AR group and control group.
In order to compute the sample size for this pilot study, the following formula was used [27]:
Parameters Δ and represent, respectively, the difference between the means of the two groups and their standard deviation. This study targets a minimum difference of Δ = 3 scans, with = = 2. A significance level of α = 0.05 and a power of the test of 1-β = 0.8 are considered. The number m of patients belonging to the historical control group is set as m = 7 patients. The formula gives a number n of prospective patients to be included in the study as n = 7. Considering a possible dropout rate of 10%, the final total number of patients included in the study is found to be 16, with n = 8 and m = 8.
Anonymous data were analyzed using MATLAB 2016b (the MathWorks, Natick, MA, USA). Differences among variables were evaluated by Fisher’s exact test for categorical variables, and by nonparametric Mann-Whitney U-test for continuous variables. A p-value < 0.05 was considered to indicate statistical significance. Categorical variables were reported as absolute value and percentage; continuous variables were reported as either mean ± standard deviation or median and interquartile (25th–75th) range.
Results
According to our criteria, 8 patients (4 males, 4 females; aged 58 ± 24 years; range 19–83) were prospectively enrolled in AR group, and 8 patients (4 males, 4 females; aged 60 ± 15 years; range 35−74) were retrospectively included in control group. The mean height, weight, and BMI were 173 ± 9 cm, 74 ± 8 kg, and 25 ± 1, respectively. No significant differences in age (p = 0.959), gender (p > 0.999), or lesion characteristics (p > 0.999) were observed among the patients and controls. No complications were observed in both groups. Procedure duration, number of CT passes, and radiation dose were 22 ± 5 min, 4 (4, 6), and 1,034 ± 672 mGy*cm for the AR group and 23 ± 5 min, 9 [7.75, 11.25], and 1,954 ± 993 mGy*cm for the control group, respectively. No significant differences between the two groups were observed in terms of procedure duration (p = 0.878). Conversely, number of CT passes and radiation dose were significantly lower for the AR group than for controls (p < 0.001 and p = 0.021, respectively). Patient demographics, lesion characteristics, and procedure details are reported in Table 1.
Table 1.
Full data of all patients (AR group) and controls (control group)
| Gender | Age (y) | Location | CT passes | Dose (mGy*cm) | Duration (min) | Pathology report |
|---|---|---|---|---|---|---|
| AR group | ||||||
| F | 52 | Pelvis | 4 | 605.43 | 33 | Negative for cancer |
| F | 56 | L3 | 4 | 946.00 | 19 | Spondylodiscitis |
| M | 80 | Pelvis | 6 | 773.43 | 22 | Metastasis |
| M | 67 | L1 | 6 | 326.35 | 21 | Metastasis |
| F | 75 | Scapula | 4 | 775.00 | 22 | Multiple myeloma |
| F | 83 | Pelvis | 4 | 1427.50 | 23 | Metastasis |
| M | 19 | Pelvis | 4 | 912.46 | 17 | Chordoma |
| M | 28 | Pelvis | 7 | 2504.00 | 21 | Hemangioma |
| Control group | ||||||
| M | 61 | Pelvis | 8 | 1927.00 | 18 | Metastasis |
| F | 39 | L1 | 8 | 1089.00 | 20 | Hemangioma |
| F | 74 | Pelvis | 7 | 1531.00 | 20 | Osteoblastoma |
| M | 35 | L2 | 7 | 919.00 | 17 | Spondylodiscitis |
| F | 63 | Scapula | 11 | 2287.00 | 25 | Chondrosarcoma |
| M | 64 | Pelvis | 12 | 2068.00 | 27 | Multiple myeloma |
| F | 69 | Pelvis | 10 | 1686.00 | 26 | Metastasis |
| M | 74 | Pelvis | 14 | 4125.00 | 32 | ARMD |
M Male, F Female, y Years, Dose Radiation dose in DLP, Duration Procedure duration time in minutes, ARMD Adverse reaction to metal debris in a patient with total hip arthroplasty
Technical success was 100% in both groups, as in all patients the center of the target lesion was reached and the sample was obtained. Technical efficacy was 100% in both groups, as the specimen was adequate in all patients according to the pathology report. Pathological analysis reported: one osteoblastoma, one chordoma, one chondrosarcoma, two myelomas, five metastases (from breast, colon, prostate, lung, and ureteral carcinoma), two hemangiomas, two spondylodiscitis, one negative for cancer, one adverse reaction to metal debris in a patient with total hip arthroplasty.
Discussion
The main finding of this pilot study was that this novel AR navigation system can be used as a feasible and safe guidance for bone biopsies in the axial skeletal system presenting 100% technical success and efficacy. AR allowed for a significant reduction of radiation dose and number of CT passes required to monitor the needle trajectory, without significant changes in procedural duration time, when compared with standard percutaneous CT-guided biopsy.
Imaging guidance is essential for diagnostic and therapeutic musculoskeletal interventions to improve reliability and safety of the procedure itself [28–30], but CT cannot provide a real-time monitoring of needle advancement without the need of interrupting the procedure to check the needle position. On the other hand, the Endosight AR navigation system, by overlapping 3D anatomic volumes over patients in the real interventional field, ensures a sort of real-time monitoring of needle trajectory, thereby decreasing the need of acquiring several CT passes generally performed to check needle trajectory and to reach the target safely avoiding neurovascular structures. This makes the method safe, as proven by the absence of complications seen in our study. The most important results of this pilot study, in addition to the safety of this AR system, are the feasibility of this tool demonstrated by the complete technical success and technical feasibility observed in all procedures. Indeed, all biopsies performed in the AR group were completed as initially planned to obtain a bioptic sample, and all specimens were adequate, as reported by the pathologist. It means that this navigation system might be used in future randomized studies to be compared with the standard CT-guided percutaneous procedure.
As a matter of fact, the most crucial point for the application of an AR navigation system is the reliability of superimposition of images that can be achieved only with a perfect coregistration. Previous studies have investigated the registration accuracy on phantoms and humans reporting interesting results. Hecht et al. [31] used an AR navigation system to guide needle advancement on phantoms reporting about 2.7-mm mean error of the needle positioning, which resulted 78% lower than the standard CT-guided intervention. Similar improvements were reached also by Long et al. [32] in an abdominal phantom using cone-beam CT-guided fluoroscopy and AR navigation systems. Notably, both studies also reported a substantial decrease of procedure duration.
The need of reliable navigation systems for bone procedures has been already highlighted by other studies recently published, involving spine surgical interventions [33] and CT-guided bone procedures [34]. Solbiati et al. [25] used the same Endosight AR system employed in our study to guide thermal ablation of liver tumors. This system consists of skin fiducial markers attached to the patient before the first CT acquisition, a specific Endosight sensor attached to the needle and a software that allows for segmentation of markers, organs, and target lesion, to coregister virtual and real images to build the best trajectory of the needle that can be followed through a display, HMD, or screen. The authors reported very high accuracy of the antenna tip positioning, with technical success of the ablation obtained in all patients. Furthermore, the procedure time was similar to that of conventional CT-guided interventions performed by expert radiologists.
This AR navigation system has never been tested for bone procedures. In our study, we have shown how it might be applied to decrease patient’s radiation exposure and number of CT passes. The procedure duration time was not different from standard percutaneous CT-guided bone biopsies. These results were achieved despite the time required to place all skin fiducial markers and the need to acquire an additional preprocedural CT scan with large field of view to include all the skin markers. Such preparatory procedures will arguably be streamlined with already planned Endosight upgrades, such as the switch from optical to infrared tracking, which should make the whole setup easier and more straightforward. In spite of this limitation, the procedure time remained low, as well as patient’s radiation dose and number of CT passes were significantly decreased, suggesting that, with some moderate adaptation of the technology to the novel scope of use, the timeframe could be further reduced.
The phenomenon of motion sickness (signs and symptoms related to AR experience using the HMD) is still a potential drawback of immersive AR systems due to possible discrepancies between the visual and vestibular senses [35]. However, it was just a mild issue for the radiologist during the first procedures. Indeed, motion sickness has been recently limited by commercially available HMDs. The patient’s respiratory movement and motion are still one of the most important technical issues, with the risk of shifting of the target relative to the expected site. In our study, we decided to focus on bone lesions located in the axial skeleton reducing the risk of shifting related to the motion of patient’s limbs. Further studies should investigate technical feasibility of this AR system to guide bone biopsies in the appendicular skeleton.
Another potential drawback of this AR system is needle bending due to corrections to the trajectory done during needle advancement within the bone. This might create an iatrogenic shift of few millimeters from the intended trajectory. Furthermore, the Endosight sensor attached to the needle is still quite large and may hamper the advancement of the needle itself in deep lesions in addition to potentially hide the view of some skin markers by the HMD, but this technical issue will be solved soon.
Some other limitations of this system and of our study need to be pointed out. The main limitation of our pilot study was the relatively small sample size, although it was enough according to sample size calculation allowing us to reach statistically significant results. Furthermore, this study is valid only as a pilot study indicating safety and efficacy and not as a controlled study. Notably, the CT protocol for guiding percutaneous bone biopsies installed in the two CT units was the same, so the required radiation dose can be just slightly affected by the different machine, while the different device manufacturers cannot impact on the required time of the whole procedure, which is totally dependent on the work of the radiologist. Last, given that it was not a prospective randomized controlled study, we tried to select similar biopsies to be included in the control group based on age, sex, lesion location, size, and appearance (lytic/sclerotic, intact/disrupted cortical bone), precisely to reduce the bias related to different conditions due to patients’ characteristics. We acknowledge that it might be considered a selection bias, but it was the only way to try to make homogeneous the two groups of patients.
In conclusion, this AR navigation system is a safe and feasible tool that can be helpful to decrease patient’s radiation dose and number of CT passes during bone biopsies without increasing the procedural duration time. Although further technological advancements could improve the adoption in the clinical practice, these results encourage further investigation of applications in the musculoskeletal system. Future prospective randomized controlled trials will aim to better understand the real advantages and disadvantages of AR-guided bone biopsies over standard percutaneous CT-guided procedures.
Abbreviations
- 3D
Three-dimensional
- AR
Augmented reality
- BMI
Body mass index
- CT
Computed tomography
- HMD
Head-mounted display
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by DA. and CM. Statistical analysis was performed by SG. and LMS. The first draft of the manuscript was written by D. A. and V. C. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The work was supported by R.A.W. Srl, Milan, Italy, which provided funding to authors’ institution (IRCCS Istituto Ortopedico Galeazzi, Milano, Italy). Authors did not receive any direct compensation for this work. Authors' work was also supported by the Italian Ministry of Health (MOH). Authors declare that the funding body contributed to study design but did not have any role in the analysis and interpretation of data.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This prospective study was approved by our ethical committee (Protocol: ESBB1, approved on 12 October 2022 by Ospedale San Raffaele, Milano, Italy) and certified by an external study monitor, and all participants provided written informed consent for being involved in this study. Study protocol was registered on ClinicalTrials.gov with number NCT05732558.
Consent for publication
All participants provided written informed consent for study participation, collection of data to be used for publication, and to the publication of their images and data.
Competing interests
L. M. Sconfienza is a member of the European Radiology Experimental Editorial Board. He has not taken part in the review or selection process of this article. The other authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Albano D, Messina C, Gitto S, et al. Differential diagnosis of spine tumors: my favorite mistake. Semin Musculoskelet Radiol. 2019;23:26–35. doi: 10.1055/s-0038-1675551. [DOI] [PubMed] [Google Scholar]
- 2.Pozzi G, Albano D, Messina C, et al. Solid bone tumors of the spine: diagnostic performance of apparent diffusion coefficient measured using diffusion-weighted MRI using histology as a reference standard. J Magn Reson Imaging. 2017;47:1034–1042. doi: 10.1002/jmri.25826. [DOI] [PubMed] [Google Scholar]
- 3.Chianca V, Albano D, Messina C, et al. An update in musculoskeletal tumors: from quantitative imaging to radiomics. Radiol Med. 2021;126:1095–1105. doi: 10.1007/S11547-021-01368-2. [DOI] [PubMed] [Google Scholar]
- 4.Filippiadis DK, Charalampopoulos G, Mazioti A, et al. Bone and soft-tissue biopsies: what you need to know. Semin Intervent Radiol. 2018;35:215–220. doi: 10.1055/S-0038-1669467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bucknor MD, Baal JD, McGill KC, et al. Musculoskeletal applications of magnetic resonance-guided focused ultrasound. Semin Musculoskelet Radiol. 2021;25:725–734. doi: 10.1055/S-0041-1735472. [DOI] [PubMed] [Google Scholar]
- 6.Sconfienza LM, Adriaensen M, Albano D, et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part VI, foot and ankle. Eur Radiol. 2022;32:1384–1394. doi: 10.1007/S00330-021-08125-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sconfienza LM, Adriaensen M, Alcala-Galiano A, et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part IV, hip. Eur Radiol. 2022;32:551–560. doi: 10.1007/S00330-021-07997-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sconfienza LM, Adriaensen M, Albano D, et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part VII, nerves of the lower limb. Eur Radiol. 2022;32:1456–1464. doi: 10.1007/S00330-021-08283-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sconfienza LM, Adriaensen M, Albano D, et al. Clinical indications for image guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part III, nerves of the upper limb. Eur Radiol. 2020;30:1498–1506. doi: 10.1007/s00330-019-06479-z. [DOI] [PubMed] [Google Scholar]
- 10.Saifuddin A, Mitchell R, Burnett SJD, et al. Ultrasound-guided needle biopsy of primary bone tumours. J Bone Joint Surg Br. 2000;82:50–54. doi: 10.1302/0301-620X.82B1.10141. [DOI] [PubMed] [Google Scholar]
- 11.Mauri G, Gitto S, Pescatori LC, et al. Technical feasibility of electromagnetic US/CT fusion imaging and virtual navigation in the guidance of spine biopsies. Ultraschall Med. 2022;43:387–392. doi: 10.1055/A-1194-4225. [DOI] [PubMed] [Google Scholar]
- 12.Johnston EW, Fotiadis N, Cummings C, et al. Developing and testing a robotic MRI/CT fusion biopsy technique using a purpose-built interventional phantom. Eur Radiol Exp. 2022;6:55. doi: 10.1186/S41747-022-00308-7/FIGURES/6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chehab MA, Brinjikji W, Copelan A, Venkatesan AM. Navigational tools for interventional radiology and interventional oncology applications. Semin Intervent Radiol. 2015;32:416–427. doi: 10.1055/S-0035-1564705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rajagopal M, Venkatesan AM. Image fusion and navigation platforms for percutaneous image-guided interventions. Abdom Radiol (New York) 2016;41:620–628. doi: 10.1007/S00261-016-0645-7. [DOI] [PubMed] [Google Scholar]
- 15.Kloeppel R, Weisse T, Deckert F, et al. CT-guided intervention using a patient laser marker system. Eur Radiol. 2000;10:1010–1014. doi: 10.1007/S003300051054. [DOI] [PubMed] [Google Scholar]
- 16.Schweiger GD, Brown BP, Pelsang RE, et al. CT fluoroscopy: technique and utility in guiding biopsies of transiently enhancing hepatic masses. Abdom Imaging. 2000;25:81–85. doi: 10.1007/S002619910016. [DOI] [PubMed] [Google Scholar]
- 17.Braak SJ, Van Strijen MJL, Van Leersum M, et al. Real-time 3D fluoroscopy guidance during needle interventions: technique, accuracy, and feasibility. AJR Am J Roentgenol. 2010;194:W445–451. doi: 10.2214/AJR.09.3647. [DOI] [PubMed] [Google Scholar]
- 18.Kim E, Ward TJ, Patel RS, et al. CT-guided liver biopsy with electromagnetic tracking: results from a single-center prospective randomized controlled trial. AJR Am J Roentgenol. 2014;203:W715–W723. doi: 10.2214/AJR.13.12061. [DOI] [PubMed] [Google Scholar]
- 19.Kettenbach J, Kronreif G. Robotic systems for percutaneous needle-guided interventions. Minim Invasive Ther Allied Technol. 2015;24:45–53. doi: 10.3109/13645706.2014.977299. [DOI] [PubMed] [Google Scholar]
- 20.De Ribaupierre S, Eagleson R. Editorial: challenges for the usability of AR and VR for clinical neurosurgical procedures. Healthc Technol Lett. 2017;4:151. doi: 10.1049/HTL.2017.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elsayed M, Kadom N, Ghobadi C, et al. Virtual and augmented reality: potential applications in radiology. Acta Radiol. 2020;61:1258–1265. doi: 10.1177/0284185119897362. [DOI] [PubMed] [Google Scholar]
- 22.Pratt P, Ives M, Lawton G, et al. Through the HoloLens™ looking glass: augmented reality for extremity reconstruction surgery using 3D vascular models with perforating vessels. Eur Radiol Exp. 2018;2:2. doi: 10.1186/S41747-017-0033-2/FIGURES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Racadio JM, Nachabe R, Homan R, et al. Augmented reality on a C-arm system: a preclinical assessment for percutaneous needle localization. Radiology. 2016;281:249–255. doi: 10.1148/RADIOL.2016151040. [DOI] [PubMed] [Google Scholar]
- 24.Solbiati M, Passera KM, Rotilio A, et al. Augmented reality for interventional oncology: proof-of-concept study of a novel high-end guidance system platform. Eur Radiol Exp. 2018;2:18. doi: 10.1186/s41747-018-0054-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solbiati M, Ierace T, Muglia R, et al. Thermal ablation of liver tumors guided by augmented reality: an initial clinical experience. Cancers (Basel) 2022;14:1312. doi: 10.3390/cancers14051312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sconfienza LM, Albano D, Messina C, et al. Ultrasound-guided percutaneous tenotomy of the long head of biceps tendon in patients with symptomatic complete rotator cuff tear: in vivo non-controlled prospective study. J Clin Med. 2020;9:2114. doi: 10.3390/jcm9072114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang S, Cao J, Ahn C. Calculating sample size in trials using historical controls. Clin Trials. 2010;7:343–353. doi: 10.1177/1740774510373629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silvestri E, Barile A, Albano D, et al. Interventional therapeutic procedures in the musculoskeletal system: an Italian survey by the Italian College of Musculoskeletal Radiology. Radiol Med. 2018;123:314–321. doi: 10.1007/s11547-017-0842-7. [DOI] [PubMed] [Google Scholar]
- 29.Sconfienza LM, Adriaensen M, Albano D, et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part V, knee. Eur Radiol. 2022;32:1438–1447. doi: 10.1007/s00330-021-08258-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sconfienza LM, Adriaensen M, Albano D, et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part II, elbow and wrist. Eur Radiol. 2020;30:2220–2230. doi: 10.1007/s00330-019-06545-6. [DOI] [PubMed] [Google Scholar]
- 31.Hecht R, Li M, de Ruiter QMB, et al. Smartphone augmented reality CT-based platform for needle insertion guidance: a phantom study. Cardiovasc Intervent Radiol. 2020;43:756–764. doi: 10.1007/S00270-019-02403-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Long DJ, Li M, De Ruiter QMB, et al. Comparison of smartphone augmented reality, smartglasses augmented reality, and 3D CBCT-guided fluoroscopy navigation for percutaneous needle insertion: a phantom study. Cardiovasc Intervent Radiol. 2021;44:774–781. doi: 10.1007/S00270-020-02760-7. [DOI] [PubMed] [Google Scholar]
- 33.Butler AJ, Colman MW, Lynch J, Phillips FM. Augmented reality in minimally invasive spine surgery: early efficiency and complications of percutaneous pedicle screw instrumentation. Spine J. 2023;23:27–33. doi: 10.1016/J.SPINEE.2022.09.008. [DOI] [PubMed] [Google Scholar]
- 34.Faiella E, Castiello G, Bernetti C, et al. Impact of an augmented reality navigation system (SIRIO) on bone percutaneous procedures: a comparative analysis with standard CT-guided technique. Curr Oncol. 2021;28:1751–1760. doi: 10.3390/CURRONCOL28030163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weech S, Kenny S, Barnett-Cowan M. Presence and cybersickness in virtual reality are negatively related: a review. Front Psychol. 2019;10:158. doi: 10.3389/fpsyg.2019.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.