Abstract
Purpose of Review
The concept of meniscal extrusion has recently been recognized as a hallmark of meniscus dysfunction. This review examines contemporary literature regarding the pathophysiology, classification, diagnosis, treatment, and future directions for investigation regarding meniscus extrusion.
Recent Findings
Meniscus extrusion, defined as >3 mm of radial displacement of the meniscus, leads to altered knee biomechanics and accelerated knee joint degeneration. Meniscus extrusion has been associated with degenerative joint disease, posterior root and radial meniscal tears, and acute trauma. Meniscus centralization and meniscotibial ligament repair have been proposed as techniques to address meniscal extrusion with promising biomechanical, animal model, and early clinical reports.
Summary
Further studies on the epidemiology of meniscus extrusion and associated long-term nonoperative outcomes will help to elucidate its role in meniscus dysfunction and resultant arthritic development. Understanding and appreciation for the anatomic attachments of the meniscus will help to inform future repair techniques. Long-term reporting on the clinical outcomes of meniscus centralization techniques will yield insights into the clinical significance of meniscus extrusion correction.
Keywords: Meniscus tear, Meniscus extrusion, Centralization, Root repair
Introduction
Menisci are crescent-shaped fibrocartilage discs located between the femur and tibia in the knee and are vital structures for the normal functioning of the knee [1]. Menisci are responsible for transmitting the axial load from the femur to the tibia, and play a crucial role in absorbing shock, maintaining stability, and providing lubrication [2–6]. Injury to the menisci can occur in many different locations and be devastating with many complications including but not limited to pain, instability, osteoarthritis, and osteonecrosis [7, 8]. The concept of meniscus extrusion has recently been recognized as an important pathologic state associated with meniscus dysfunction. Meniscus extrusion is the displacement of the meniscus, medially or laterally, outside the margins of the tibial plateau. Some meniscal extrusion is physiologic in nature, with greater degrees thought to be pathologic in nature [9, 10]. Importantly, pathologic degrees of extrusion are known to be associated with development and progression of degenerative joint disease (DJD) [11–13]. However, meniscal extrusion remains incompletely understood. Here we review the related anatomy, pathophysiology, classifications, and treatment techniques.
Anatomy
Histologically, the menisci are highly hydrated (72% water) [14] and composed of circumferential collagen fibers that are bundled via tie fibers with a surface lamellar layer that extends between the fiber bundles and is proteoglycan rich [15]. In addition to capsular attachments, the menisci have posterior and anterior root attachments to the tibial plateau that histologically resemble fibrocartilaginous entheses [16]. This organization facilitates the load dissipating function of the menisci [15].
The medial meniscus covers 50–75% of the medial tibial plateau and is attached circumferentially to the capsule [17]. The medial meniscus anterior root travels over the front of the tibial plateau and attaches 29.8 ± 2.7 mm proximal to the medial aspect of the tibial tuberosity [18]. The medial meniscus posterior root attaches 9.6 ± 0.8 mm posterior and 0.7 ± 0.4 mm lateral to the medial tibial eminence apex [19].
The lateral meniscus covers 75–93% of the lateral tibial plateau and has twice the mobility of the medial meniscus [20]. Due to the popliteal hiatus, the lateral meniscus is not circumferentially attached to the capsule like the medial meniscus. The lateral meniscus posterior horn can have medial condyle femoral attachments that include the Ligament of Humphrey (anterior meniscofemoral ligament) and the Ligament of Wrisberg (posterior meniscofemoral ligament) [17]. The lateral meniscus anterior root attaches 5.0 ± 1.8 mm anterior to the center of the ACL tibia insertion with approximately 40% overlap with the ACL insertion [18]. The lateral meniscus posterior root attaches 4.2 ± 0.4 mm medial and 1.5 ± 0.7 mm posterior to the lateral tibial eminence apex [19].
Recent focus on extrusion has led to a re-examination of the anatomy of the tibio-meniscal attachments. There is a thickening of the deep layer of the MCL known as the meniscotibial ligament, and disruption or abnormality of this complex has been correlated with the degree of meniscus extrusion [21•]. Similarly, on the lateral side of the knee, a recent study by Masferrer-Pino et al. examined peripheral attachments of the lateral meniscus and coined the term “menisco-tibio-popliteus-fibular complex” [22]. The main structures identified in this study include the lateral meniscotibial ligament, popliteofibular ligament, and popliteomeniscal ligament. The authors hypothesize that this complex of structures plays an important role in limiting lateral meniscal extrusion and that reconstruction or repair of these structures may represent a tenable strategy to addressing lateral meniscus extrusion.
Pathophysiology
The menisci are fibrocartilaginous in nature with circumferentially oriented fibers. When a load is applied across the knee joint, a portion of these forces are radially directed. The menisci orientation provides resistance to this outward force, aptly named hoop stress [23, 24]. The loss of this hoop stress leads to altered load distribution with greater forces on the articular cartilage [25, 26]. Thus, insult or frank injury to the meniscus may result in meniscus extrusion [27]. Meniscus extrusion can be observed after tears of the meniscus including radial and root tears and after meniscal allograft transplant. Contributory risk factors for meniscal extrusion include increasing age, knee malalignment, degenerative joint changes, high body mass index, and female sex [10, 27–29].
The most commonly associated finding with meniscal extrusion is a posterior meniscal root tear [30]. Historically, it has been thought that posterior meniscal root tears pre-empt extrusion [28, 31], but this has recently come into question. First, isolated meniscal extrusion can also be observed, though the consequences are unclear [21]. Second, there is acceptance that root repair alone does not eliminate meniscus extrusion [31, 32]. Third, Krych et al. have demonstrated the presence of meniscotibial (MT) ligament disruption (Fig. 1) and meniscal extrusion on MRI in 27 patients prior to medial meniscus posterior root tears [33•]. This suggests that extrusion and MT disruption may lead to increased hoop stress and subsequent medial meniscus posterior root tear (Fig. 2). Consequently, meniscus centralization is being increasingly explored [34•] and will be discussed in the techniques section.
Fig. 1.
Meniscotibial disruption on coronal MRI. Coronal preoperative MRI demonstrating medial meniscotibial ligament intact (left, arrow) and disrupted (right, red arrow), with meniscus extrusion (right, yellow arrow)
Fig. 2.
Proposed pathoanatomy of medial meniscus extrusion. A Loading of meniscus increases hoop stresses. B Peripheral displacement of the meniscus alters contact pressures and tibial plateau cartilage coverage with injury to posterior meniscal root. C Posterior meniscal root integrity is lost with increased peripheral displacement of the meniscus. D Accelerated tibial plateau cartilage wear and bone overload secondary to a nonfunctional meniscus
The lateral meniscus has a greater degree of physiologic extrusion, with lateral meniscus extrusion reported in untorn menisci. In one study, the rate of pathologic meniscus extrusion was found to be greater in medial meniscal root tears (7/8) than lateral root tears (6/26) [35]. Nonetheless, lateral meniscus extrusion was noted as a risk factor for progression to arthroplasty [36]. However, an ultrasound study found no association with Kellgren–Lawrence grade and lateral meniscus extrusion [37]. Additionally, ACL tears with concomitant lateral meniscus posterior root tears also have been associated with lateral meniscus extrusion. In these cases, transtibial pullout repair of lateral meniscal root in ACLR was associated with lower lateral meniscus extrusion 6 months postoperatively [38].
Biomechanical studies have suggested that the detrimental effect of lateral meniscus posterior root tears is at least partially mitigated by presence of an intact meniscofemoral ligament [3, 39]. However, one study of patients with isolated ACL injury versus ACL injury with posterolateral meniscus root tear and intact meniscofemoral ligament showed a trend toward increased extrusion despite the presence of an intact meniscofemoral ligament [40].
Knee malalignment is thought to have a causal relationship with meniscus extrusion secondary to compartment overload. Crema et al. identified varus malalignment (≥ 2.0°) as a risk factor for medial meniscus extrusion [27]. More recently, Goto et al. reported that medial meniscus extrusion is independently related to medial meniscus extrusion greater than 3 mm and with progression of osteoarthritis [41]. Willinger et al. found that varus malalignment increased medial meniscus extrusion and peak contact pressures [42]. However, it should be noted that Erquicia et al. did not find an association between mild varus malalignment (2.6°) and meniscal extrusion [43], suggesting that a small degree of malalignment is tolerated up to a critical threshold. Chung et al. found that the main long-term predictors of meniscal root repair failure were preoperative varus alignment (≥ 5.0°) and meniscus extrusion [44•].
Meniscal allograft transplantation is another topic of investigation regarding extrusion. Unique factors such as donor/patient size mismatch and surgical technique may contribute in this setting. Previous studies have demonstrated that graft oversizing as well as improper matching can be related to extrusion of the graft. Additionally, other aspects such as loss of fixation, incorrect positioning, and improper repair of ligaments such as the aforementioned MT ligament may lead to extrusion [45, 46]. Factors associated with extrusion in these cohorts include suture only fixation as compared to osseous fixation [47]. Unsurprisingly, central fixation as compared to medial fixation was associated with less extrusion, though clinical outcomes were not significantly different in these cohorts [48].
Regardless of the cause of extrusion, it is well understood that meniscal extrusion negatively impacts the weight-bearing surface and predisposes patients to damage of the knee. This can take form of osteoarthritis, osteophytosis, chondral lesions, further meniscal tearing, and loss of cartilage [13, 49–51]. However, the natural history of knee degeneration in respect to meniscal extrusion is complex and incompletely understood. As shown by Bennet et al., joint space narrowing may be initiated by meniscal and cartilage degeneration [52]. Foreman et al. suggest that meniscal extrusion and root tears play a significant role in accelerated knee degeneration [53]. Ding et al., in a 2-year longitudinal study with 294 patients, suggest that meniscal extrusion happens subsequent to increased medial tibial bone and osteophyte generation. Thus, in this nonarthritic cohort, subchondral bone expansion may initiate meniscal extrusion which then further mediates knee degeneration [54]. Krych et al. examined 63 serial MRIs in patients presenting with medial knee pain and noted extruded menisci with intact roots progressed with development of a posterior root tear [33]. Therefore, the extruded meniscus may increase the biomechanical forces on the root attachment, leading to a complete root tear with minimal trauma.
Diagnosis and Classification
Meniscus extrusion exists on a spectrum of minimal physiologic extrusion extending to greater than 10 mm of extrusion [55]. Within this range, thresholds have been developed. Costa et al. divided extrusion into two groups: those with meniscal extrusion of less than 3 mm and those with greater than 3 mm, which were described as minor and major, respectively [56]. More recently, a separate study with 718 healthy volunteers found that mean meniscal extrusion was 2.7 mm medially and 1.8 mm laterally [57•]. This has classically led to 3 mm being the cut off for pathologic extrusion; however, extrusion under 3 mm does not rule out meniscus injury. Indeed, Choi et al. in a 248-patient series found mean extrusion of patients with medial meniscal tears that were not posterior root tears was 2.7 ± 1.3 mm, while patients in this study with posterior root tears had mean medial extrusion of 3.8 ± 1.4 mm [58]. This may suggest the 3 mm extrusion threshold as suggestive of medial meniscus root tears; however, the study found low positive predictive value (39%) and specificity (58%).
Similarly, greater meniscal extrusion can been observed in the case of osteoarthritis (OA) with mean meniscal extrusion of 5.1 mm in OA patients versus 2.8 mm in controls [12]. Recently, Liu et al., in 235 participants with 328 knees, found 2.5 mm to be the threshold that maximized the sensitivity and specificity of the progression of knee pain, medial cartilage damage, and medial tibial cartilage damage [59]. In contrast, Svensson et al., in 958 patients, describe 4 mm as the optimal sensitivity and specificity for similar markers of OA [57]. Thus, the literature concerning extrusion as it relates to OA and progression of OA is heterogeneous and does not imply a precise cut off. It is the opinion of the authors that 3.0 mm of medial meniscus extrusion (on a standard MRI coronal image) may be used as a screening tool, with greater extrusion potentially being a marker of frank pathology. It remains that meniscus extrusion should augment clinical findings and judgement. Additionally, further studies on lateral meniscus extrusion are warranted.
In addition to meniscal extrusion varying based on pathologic state, extrusion is also appreciated to be dynamic, with differing extrusion based on position and load bearing status. Achtnich et al., in 75 healthy volunteers, determined a mean supine (1.1 mm) to weight-bearing (1.9 mm) extrusion difference of 0.8 mm ± 0.6 mm seen on ultrasound. Karpinski et al. compared 25 patients with medial root lesions vs 25 healthy controls with dynamic ultrasound. In this study, they demonstrate that patients with a root tear have greater supine (3.6 mm vs 1.3 mm) and load bearing (3.7 mm vs 2.3 mm) extrusion on US, as well as significantly lower extrusion difference (0.1 mm vs 1.0 mm). This is described as the “dead meniscus sign,” or the failure to have dynamic extrusion in the pathologic state [60]. Given this finding, future studies on weight-bearing and dynamic imaging modalities are warranted. Increasing extrusion and extrusion difference could also be observed with elevated BMI [9].
To date, the gold standard for meniscal extrusion measurement is MRI with T2-weighted MRI [46]. MRI provides good sensitivity and specificity along with the ability to identify other meniscal or knee pathology, thus is valuable. Visualization is best appreciated on 3-T MRI in the coronal plane [61]. Fluid sensitive sequences can help to identify joint overload bone edema secondary to extrusion. However, to date, MRI is limited by being non-weight bearing, static, and expensive in nature. Ultrasound can be a viable imaging modality that allows for multiplanar and dynamic imaging of the meniscus and other knee structures. Additionally, ultrasound has been found to have excellent sensitivity and specificity in detecting extrusion along with reliability of quantitative extrusion assessment [62]. However, ultrasound may not provide the fidelity necessary to identify anterior or posterior horn root tears which are key steps on the progression of extrusion. Computed tomography (CT) is uncommonly used; however, could be considered when MRI is unavailable or unusable.
In a clinical setting, multimodal diagnosis of extrusion with ultrasound and MRI is ideal. Both non-weight-bearing and weight-bearing ultrasound could be utilized as screening and primary diagnostics, followed by MRI to both confirm extrusion diagnosis and important associated pathology such as bone edema and articular cartilage status as well as meniscus integrity. Given the increasing interest in extrusion and extrusion repair, there continues to be a need for a viable reliable modality to quantify extrusion intraoperatively.
Treatment
Management of meniscal extrusion and underlying pathology is crucial given the progression of knee pathology including but not limited to OA progression. Nonoperative management, including NSAIDS, weight loss, activity modification, and use of unloader bracing, may be an option in those with advanced DJD or poor surgical candidates. Additionally, relative contraindications to surgery include high BMI, malalignment greater than 10°, any grade 4 or bipolar grade 3 articular cartilage (OARSI), and degenerative meniscus changes [63]. Treatment is reserved for symptomatic (painful) extrusion only. However, surgery remains the mainstay of management in younger, symptomatic cohorts and those with acute injury. Treatment is dependent on a multitude of factors but should be tailored to the underlying cause of extrusion.
Osteotomy
Several studies have demonstrated that offloading osteotomy can decrease extrusion if malalignment is present and causing the extrusion. Choi et al. found that opening-wedge high tibial osteotomy significantly decreased medial meniscus extrusion on MRI [64]. Additionally, it was found by Lee et al. that patient-reported clinical outcome improvement after medial opening wedge HTO was correlated with improvement in medial meniscus extrusion to < 3 mm [65•]. Though studies support worse root repair outcomes in patients with knee varus ≥ 5.0° [66], an exact threshold to employ offloading osteotomy is unclear as a recent matched cohort study by Moon et al. described non-inferiority of root repair alone in those with < 5.0° of varus compared to those with between 5 and 10° of varus [67].
Root Repair
Root tears are an established cause of meniscus extrusion [63]. Partial or total meniscectomy used to be the mainstay of treatment for root tears; however, it is now appreciated that root repair results in superior biomechanics, better patient-reported outcomes, less OA, less total knee replacements, and lower costs [68]. Repair of root tears with both a transtibial tunnel and direct fixation with suture anchors are efficacious with comparable healing and outcomes [69]. Despite the documented similarities, the suture anchor technique is challenging, requires a posterior portal, and utilizes specialized passing devices, thus it is the opinion of the authors and others that the transtibial method is currently preferred with the present technology [63, 70, 71].
Radial Tear
Biomechanically, radial tears are similar to root tears and complete meniscectomy, and, thus, can result in extrusion [56, 72]. Both all-inside and inside out repairs have been well described with newer techniques being developed [73]. To date, there is no consensus on preferred method; however, it remains that anatomic repair without partial or total meniscectomy provides superior outcomes [74, 75].
Centralization/Anatomic Repair
Postoperative meniscus extrusion continues to be a clinical problem even after meniscal repair [28, 76]. Thus, centralization is being increasingly explored as a treatment for extrusion, both in the setting of root repairs and in isolated extrusion (Fig. 3). Biomechanical studies suggest that root repair with centralization is effective at reducing extrusion and the mechanical sequelae that accompany it [32, 77]. The development of minimal footprint, all-suture anchors has spurred the development of a variety of techniques for centralization (Table 1).
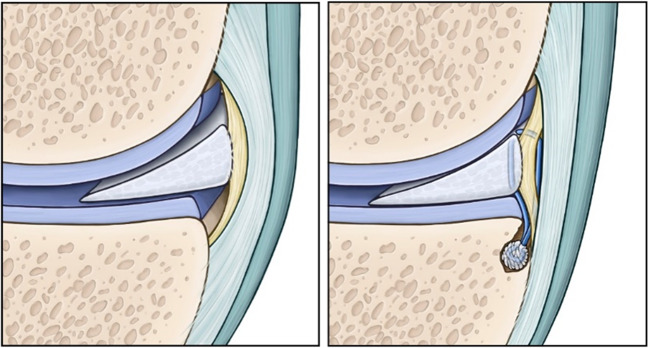
Fig. 3.
Diagram of meniscus centralization. Peripherally displaced meniscus in left picture is restored to its central position with an all-suture anchor placed at the periphery of the tibial plateau with the suture placed in a vertical mattress fashion through the peripheral rim of the meniscus in the right picture
Table 1.
Key steps in meniscus centralization
| 1. | Patient positioned supine with a lateral post and heels at end of table |
| 2. | Identification of meniscus extrusion by identifying pathologic mobility and/or under coverage of tibial articular surface |
| 3. | Creation of a high accessory portal with optimal trajector for centralization anchor(s) |
| 4. | For medial meniscus, use tissue elevator to release meniscotibial ligament and fully to mobilize meniscus |
| 5. | Rasp edge of plateau for healing |
| 6. | Placement of all-suture anchor with double loaded sutures under the medial meniscus at the edge of plateau in the region normally covered by meniscus |
| 7. | Vertical mattress suture step 1: passage of sutures in full-thickness bottom to top in meniscocapsular junction |
| 8. | Vertical mattress suture step 2: passage of a passing suture in vertical mattress fashion adjacent to first suture, loading initial suture into passing suture and bringing from top to bottom of meniscus |
| 9. | Loading vertical mattress (suture strands exiting on bottom of meniscus) back into the anchor with passage stitch |
| 10. | Repeat for second loaded suture |
| 11. | Sequential reduction of the meniscus with sutures onto the tibial plateau in native footprint, cut sutures tails flush with articular surface after reduction |
| 12. | Verification of fixation with cycling and loading of compartment |
The authors’ preferred technique is outlined in Tables 1 and 2. Briefly, identification of meniscus extrusion is made arthroscopically by examining tibial plateau coverage by the meniscus. The meniscotibial ligament is then released to maximize meniscal mobilization. Next, an area at the periphery of the tibial plateau for an all-suture anchor is identified and prepared before placement of the anchor through an accessory portal with optimal vertical trajectory to the tibial plateau (Fig. 4). The suture anchor sutures are then passed through the periphery of the meniscus in a vertical mattress fashion (Fig. 5). The sutures are then tensioned and secured to eliminate the meniscus extrusion and centralize the meniscus on the plateau (Fig. 6). If a concomitant root repair is done, root fixation is done last. Postoperatively, patients are kept toe touch weight bearing for 4 weeks and flexion is limited to 90° for the first 4 weeks (Fig. 7).
Table 2.
Pearls and pitfalls for arthroscopic meniscus centralization
| Pearls | |
| - Localize trajectory for accessory portal with 18-gauge spinal need prior to making portal | |
| - Viewing through ipsilateral portal and bringing suture passage device from contralateral anterior portal is simplest working strategy | |
| - Parking the sutures not currently being passed in the viewing portal can prevent suture tangle | |
| - Suture passage device can be more easily put into correct location inverted, and then rolled into position | |
| - If using multiple anchors for centralization, work posterior to anterior for visualization | |
| - Consider a medial collateral ligament pie-crusting release to allow better access to meniscus with suture passage device. This also serves to offload the medial compartment if medial collateral ligament is tight. | |
| - With torn root, consider performing root repair fixation after centralization | |
| - With radial tear, incorporate centralization sutures into repair, consider using centralization sutures to aide initial reduction | |
| - Consider use of cannula to avoid suture bridges | |
| Pitfalls | |
| - Consider fixation failure if a patient is not able to follow established rehab protocol | |
| - Inadequate exposure | |
| - Iatrogenic cartilage injury |
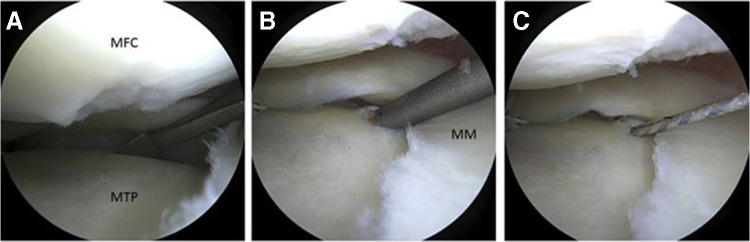
Fig. 4.
Suture anchor placement for medial meniscus centralization. A Elevation/release of the MT ligament with elevator (right knee, viewing from AM portal). B Anchor drill guide placed at the periphery of the MTP. C Deployed anchor with sutures exiting the accessory (acc) AM portal
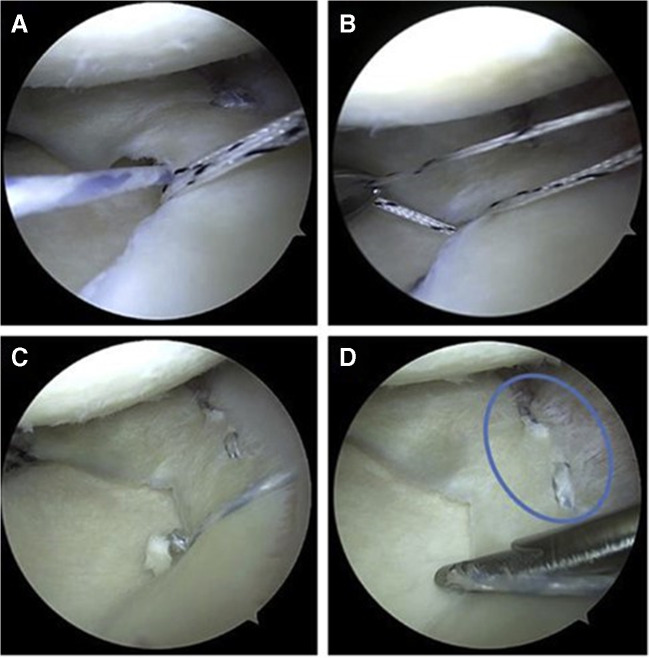
Fig. 5.
Suture passage through the meniscus. A Self-retrieving device from the anterolateral (AL) portal piercing the meniscocapsular junction to pass the repair suture. B Suture retrieved through AL portal. C Passing the shuttle suture
Fig. 6.
Tightening of mattress sutures eliminates meniscus extrusion. A Suture shuttled under the medial meniscus (MM) by the shuttle suture, and retrieved through the anterolateral (AL) portal. B Remaining shuttle suture retrieved through AL portal. C Tensioning is performed. D Final construct
Fig. 7.
Physical therapy and rehabilitation guidelines for meniscus centralization. Initial weight bearing is toe touch for 4 weeks with progression to WBAT starting at 4 weeks. Initial ROM is 0–90 in a brace for 4 weeks to protect centralization
Data on the outcomes of the procedure is sparse (Table 3), but suggests good patient-reported outcomes along with reduction of meniscal extrusion in the lateral compartment [78, 79]. A recent report of 2-year outcomes for medial meniscus centralization with transtibial root repair similarly suggests improvement in extrusion and patient-reported outcomes [80].
Table 3.
Summary of published studies of meniscus centralization
| Xue et al. Int Orthop 2022 | 16 pts | Posterior anchor MM, +MMRR (transtibial) |
| Katagiri et al. J Knee Surg 2021 | 21 pts | Centralization MM, +OWHTO |
| Mochizuki et al. EJOST 2021 | 26 pts | Centralization MM, +MMRR (transtibial) |
| Koga et al. AJSM 2020 | 27 pts | Centralization LM, +capsuloplasty |
| Ohnishi et al. Knee 2018 | 52 pts | Centralization LM (discoid), saucerization |
| Koga et al. Arthroscopy 2016 | 21 pts | Centralization LM |
| Wu et al. Arth Tech 2022 | Technique | Centralization MM (knotless anchor), +MMRR (transtibial) |
| Koga et al. Arth Tech 2021 | Technique | Centralization MM (knotless anchor) |
| Leafblad et al. Arth Tech 2020 | Technique | Centralization MM |
| Nakagawa et al. JOS 2020 | Case report | Centralization LM |
| Nakamura et al. Arth Tech 2018 | Technique | Centralization MM, +MMRR (transtibial), OWHTO |
| Chernchujit et al. EJOST 2018 | Technique | Centralization MM, +MMRR (transtibial) |
| An et al. Asia Pac J SMART 2017 | Case report | Centralization LM, +OATS LTP |
| Koga et al. Arth Tech 2017 | Technique | Centralization MM, +MMRR (transtibial) |
| Koga et al. Arth Tech 2012 | Technique | Centralization LM |
| Kohno et al. JOR 2022 | Animal | Centralization LM in pigs, biomechanics |
| Park et al. AJSM 2022 | Animal | Circumferential rim suture MM in rabbits |
| Kubota et al. BMC Musc Dis 2020 | Animal | Centralization LM in pigs w/LMRT restores contact pressure |
| Ozeki et al. JOS 2020 | Animal | Centralization lateral meniscus in pig |
| Nakamura et al. KSSTA 2019 | Animal | Centralization LM in pigs w/ACLR |
| Ozeki et al. JOS 2017 | Animal | Centralization in rat limits cartilage degradation |
| Ueki et al. KSSTA 2022 | Biomechanic | 14 cadaver knees ALCR ± centralization MM |
| Nakamura et al. AJSM 2021 | Biomechanic | 14 cadaver knees ACLR + centralization reduced knee laxity with centralization |
| Debieux et al. KSSTA 2020 | Biomechanic | 10 cadaver knees centralization MM significant changes contact are w/>3 mm |
| Daney et al. AJSM 2019 | Biomechanic | 10 cadaver knees MMRR with centralization |
While coronal meniscus extrusion has been the primary focus of most research in this area, recent studies have suggested that sagittal extrusion is just as important [81]. Xue et al. compared patients with medial meniscus posterior root tears repair with transtibial root repair against those with transtibial root repair with an additional posteromedial corner anchor, and found improved posterior medial meniscus extrusion and remaining medial meniscal volume with the latter approach [82•].
Conclusions
Restoring native meniscus anatomy and biomechanical function is key to successful repair for meniscus extrusion either isolated or with an associated root tear. Proper repair of the meniscotibial ligaments and other attachments may help prevent postoperative extrusion and associated meniscus dysfunction. When pathologic meniscus extrusion is present, assessment for background factors and potential surgical correction of the extrusion with centralization may more optimally restore the anatomy and function of the meniscus. While early clinical outcomes are encouraging, future comparative outcome studies with clearly defined indications are needed to affirm the efficacy of the centralization procedure.
Funding
This study was partially funded by the following: National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Compliance with Ethical Standards
Conflict of Interest
Mark Langhans, Abhinav Lamba, Daniel Saris, Patrick Smith, and Aaron Krych declare they have no conflict of interest.
Aaron Krych voluntarily discloses: Aesculap/B.Braun: research support; American Journal of Sports Medicine: editorial or governing board; Arthrex, Inc: IP royalties; paid consultant; research support; International Cartilage Repair Society: board or committee member; International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine: board or committee member. Daniel Saris voluntarily discloses: Cartilage: editorial or governing board; JRF: research support; NewClip: paid consultant. Patrick Smith voluntarily discloses: American Orthopaedic Society for Sports Medicine: board or committee member; Arthrex, Inc: IP royalties; paid consultant; paid presenter or speaker; research support; Associate Editor-Journal of Knee Surgery: editorial or governing board; Spinal Simplicity: stock or stock options.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mark T. Langhans, Email: langhans.mark@mayo.edu
Abhinav Lamba, Email: lamba.abhinav@mayo.edu.
Daniel B. F. Saris, Email: saris.daniel@mayo.edu
Patrick Smith, Email: psmithmudoc@aol.com.
Aaron J. Krych, Email: krych.aaron@mayo.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30(4):664–670. doi: 10.1302/0301-620X.30B4.664. [DOI] [PubMed] [Google Scholar]
- 2.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 3.Forkel P, Herbort M, Schulze M, Rosenbaum D, Kirstein L, Raschke M, et al. Biomechanical consequences of a posterior root tear of the lateral meniscus: stabilizing effect of the meniscofemoral ligament. Arch Orthop Trauma Surg. 2013;133(5):621–626. doi: 10.1007/s00402-013-1716-7. [DOI] [PubMed] [Google Scholar]
- 4.Harner CD, Mauro CS, Lesniak BP, Romanowski JR. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2):257–270. doi: 10.2106/JBJS.I.00500. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 6.Walker PS, Arno S, Bell C, Salvadore G, Borukhov I, Oh C. Function of the medial meniscus in force transmission and stability. J Biomech. 2015;48(8):1383–1388. doi: 10.1016/j.jbiomech.2015.02.055. [DOI] [PubMed] [Google Scholar]
- 7.Smoak JB, Matthews JR, Vinod AV, Kluczynski MA, Bisson LJ. An up-to-date review of the meniscus literature: a systematic summary of systematic reviews and meta-analyses. Orthop J Sports Med. 2020;8(9):2325967120950306. doi: 10.1177/2325967120950306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fox AJ, Wanivenhaus F, Burge AJ, Warren RF, Rodeo SA. The human meniscus: a review of anatomy, function, injury, and advances in treatment. Clin Anat. 2015;28(2):269–287. doi: 10.1002/ca.22456. [DOI] [PubMed] [Google Scholar]
- 9.Achtnich A, Petersen W, Willinger L, Sauter A, Rasper M, Wörtler K, et al. Medial meniscus extrusion increases with age and BMI and is depending on different loading conditions. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2282–2288. doi: 10.1007/s00167-018-4885-7. [DOI] [PubMed] [Google Scholar]
- 10.Gajjar SM, Solanki KP, Shanmugasundaram S, Kambhampati SBS. Meniscal extrusion: a narrative review. Orthop J Sports Med. 2021;9(11):23259671211043797. doi: 10.1177/23259671211043797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonté F, Beaudoin G, Bloch DA, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64(4):556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D. Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthr Cartil. 1999;7(6):526–532. doi: 10.1053/joca.1999.0256. [DOI] [PubMed] [Google Scholar]
- 13.Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol. 1999;54(8):502–506. doi: 10.1016/S0009-9260(99)90846-2. [DOI] [PubMed] [Google Scholar]
- 14.Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011;32(30):7411–7431. doi: 10.1016/j.biomaterials.2011.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andrews SH, Rattner JB, Abusara Z, Adesida A, Shrive NG, Ronsky JL. Tie-fibre structure and organization in the knee menisci. J Anat. 2014;224(5):531–537. doi: 10.1111/joa.12170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacob G, Shimomura K, Krych AJ, Nakamura N. The meniscus tear: a review of stem cell therapies. Cells. 2019;9(1) [DOI] [PMC free article] [PubMed]
- 17.Mameri ES, Dasari SP, Fortier LM, Verdejo FG, Gursoy S, Yanke AB, et al. Review of meniscus anatomy and biomechanics. Curr Rev Musculoskelet Med. 2022;15(5):323–335. doi: 10.1007/s12178-022-09768-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.LaPrade CM, Ellman MB, Rasmussen MT, James EW, Wijdicks CA, Engebretsen L, et al. Anatomy of the anterior root attachments of the medial and lateral menisci: a quantitative analysis. Am J Sports Med. 2014;42(10):2386–2392. doi: 10.1177/0363546514544678. [DOI] [PubMed] [Google Scholar]
- 19.Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40(10):2342–2347. doi: 10.1177/0363546512457642. [DOI] [PubMed] [Google Scholar]
- 20.Nakamura T, Marshall BD, Price TM, Mao Y, Linde MA, Koga H, et al. Arthroscopic centralization for lateral meniscal injuries reduces laxity in the anterior cruciate ligament-reconstructed knee. Am J Sports Med. 2021;49(13):3528–3533. doi: 10.1177/03635465211041747. [DOI] [PubMed] [Google Scholar]
- 21•.Krych AJ, Bernard CD, Leland DP, Camp CL, Johnson AC, Finnoff JT, et al. Isolated meniscus extrusion associated with meniscotibial ligament abnormality. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3599–3605. doi: 10.1007/s00167-019-05612-1. [DOI] [PubMed] [Google Scholar]
- 22.Masferrer-Pino A, Saenz-Navarro I, Rojas G, Perelli S, Erquicia J, Gelber PE, et al. The menisco-tibio-popliteus-fibular complex: anatomic description of the structures that could avoid lateral meniscal extrusion. Arthroscopy. 2020;36(7):1917–1925. doi: 10.1016/j.arthro.2020.03.010. [DOI] [PubMed] [Google Scholar]
- 23.Fox AJ, Bedi A, Rodeo SA. The basic science of human knee menisci: structure, composition, and function. Sports Health. 2012;4(4):340–351. doi: 10.1177/1941738111429419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones RS, Keene GC, Learmonth DJ, Bickerstaff D, Nawana NS, Costi JJ, et al. Direct measurement of hoop strains in the intact and torn human medial meniscus. Clin Biomech (Bristol, Avon). 1996;11(5):295–300. doi: 10.1016/0268-0033(96)00003-4. [DOI] [PubMed] [Google Scholar]
- 25.Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 26.Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51(6):871–879. doi: 10.3109/17453678008990887. [DOI] [PubMed] [Google Scholar]
- 27.Crema MD, Roemer FW, Felson DT, Englund M, Wang K, Jarraya M, et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the Multicenter Osteoarthritis study. Radiology. 2012;264(2):494–503. doi: 10.1148/radiol.12110986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Furumatsu T, Kodama Y, Kamatsuki Y, Hino T, Okazaki Y, Ozaki T. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29(4):295–301. doi: 10.5792/ksrr.17.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606–1610. doi: 10.1177/0363546512447792. [DOI] [PubMed] [Google Scholar]
- 30.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33(10):569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 31.Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG. Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45(1):42–49. doi: 10.1177/0363546516662445. [DOI] [PubMed] [Google Scholar]
- 32.Daney BT, Aman ZS, Krob JJ, Storaci HW, Brady AW, Nakama G, et al. Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med. 2019;47(7):1591–1600. doi: 10.1177/0363546519844250. [DOI] [PubMed] [Google Scholar]
- 33•.Krych AJ, LaPrade MD, Hevesi M, Rhodes NG, Johnson AC, Camp CL, et al. Investigating the chronology of meniscus root tears: do medial meniscus posterior root tears cause extrusion or the other way around? Orthop. J Sports Med. 2020;8(11):2325967120961368. Manuscript describing the presense of meniscotibial disruption and meniscus extrusion on MRI prior to diagnosis of medial meniscus posterior root tear. [DOI] [PMC free article] [PubMed]
- 34•.Leafblad ND, Smith PA, Stuart MJ, Krych AJ. Arthroscopic centralization of the extruded medial meniscus. Arthrosc Tech., Manuscript describing the techniques for transtibial medial meniscus posterior root repair with concomittant meniscus centralization for limit meniscus extrusion. 2021;10(1):e43–e8. [DOI] [PMC free article] [PubMed]
- 35.Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239(3):805–810. doi: 10.1148/radiol.2393050559. [DOI] [PubMed] [Google Scholar]
- 36.Pareek A, Parkes CW, Bernard CD, Abdel MP, Saris DBF, Krych AJ. The SIFK score: a validated predictive model for arthroplasty progression after subchondral insufficiency fractures of the knee. Knee Surg Sports Traumatol Arthrosc. 2020;28(10):3149–3155. doi: 10.1007/s00167-019-05792-w. [DOI] [PubMed] [Google Scholar]
- 37.Singh AP, Saran S, Thukral BB, Kaushik R. Ultrasonographic evaluation of osteoarthritis-affected knee joints: comparison with Kellgren-Lawrence grading and pain scores. J Med Ultrasound. 2021;29(1):39–45. doi: 10.4103/JMU.JMU_45_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Okazaki Y, Furumatsu T, Kamatsuki Y, Okazaki Y, Masuda S, Hiranaka T, et al. Transtibial pullout repair of the lateral meniscus posterior root tear combined with anterior cruciate ligament reconstruction reduces lateral meniscus extrusion: a retrospective study. Orthop Traumatol Surg Res. 2020;106(3):469–473. doi: 10.1016/j.otsr.2019.10.022. [DOI] [PubMed] [Google Scholar]
- 39.Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF. Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1469–1477. doi: 10.1007/s00167-015-3742-1. [DOI] [PubMed] [Google Scholar]
- 40.Pula DA, Femia RE, Marzo JM, Bisson LJ. Are root avulsions of the lateral meniscus associated with extrusion at the time of acute anterior cruciate ligament injury?: a case control study. Am J Sports Med. 2014;42(1):173–176. doi: 10.1177/0363546513506551. [DOI] [PubMed] [Google Scholar]
- 41.Goto N, Okazaki K, Akiyama T, Akasaki Y, Mizu-Uchi H, Hamai S, et al. Alignment factors affecting the medial meniscus extrusion increases the risk of osteoarthritis development. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2617–2623. doi: 10.1007/s00167-018-5286-7. [DOI] [PubMed] [Google Scholar]
- 42.Willinger L, Lang JJ, Berthold D, Muench LN, Achtnich A, Forkel P, et al. Varus alignment aggravates tibiofemoral contact pressure rise after sequential medial meniscus resection. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1055–1063. doi: 10.1007/s00167-019-05654-5. [DOI] [PubMed] [Google Scholar]
- 43.Erquicia J, Gelber PE, Cardona-Muñoz JI, Pelfort X, Tey M, Monllau JC. There is no relation between mild malalignment and meniscal extrusion in trauma emergency patients. Injury. 2012;43(Suppl 2):S68–S72. doi: 10.1016/S0020-1383(13)70183-9. [DOI] [PubMed] [Google Scholar]
- 44•.Chung KS, Ha JK, Ra HJ, Kim JG. Preoperative varus alignment and postoperative meniscus extrusion are the main long-term predictive factors of clinical failure of meniscal root repair. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4122–30. Manuscript highlighting the independent risk factors of varus malalignment and meniscus extrusion in predicting clincal failure of posterior root tear repair. [DOI] [PubMed]
- 45.Noyes FR, Barber-Westin SD. A systematic review of the incidence and clinical significance of postoperative meniscus transplant extrusion. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):290–302. doi: 10.1007/s00167-014-3329-2. [DOI] [PubMed] [Google Scholar]
- 46.Lee DH, Kim TH, Lee SH, Kim CW, Kim JM, Bin SI. Evaluation of meniscus allograft transplantation with serial magnetic resonance imaging during the first postoperative year: focus on graft extrusion. Arthroscopy. 2008;24(10):1115–1121. doi: 10.1016/j.arthro.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 47.Abat F, Gelber PE, Erquicia JI, Pelfort X, Gonzalez-Lucena G, Monllau JC. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40(7):1591–1596. doi: 10.1177/0363546512446674. [DOI] [PubMed] [Google Scholar]
- 48.Yoon KH, Lee HW, Park SY, Kim JS, Park JY. Centralized anterior bone plug results in less graft extrusion in patients undergoing medial meniscus allograft transplantation following anterior cruciate ligament reconstruction. Knee. 2020;27(3):884–890. doi: 10.1016/j.knee.2020.02.014. [DOI] [PubMed] [Google Scholar]
- 49.Puig L, Monllau JC, Corrales M, Pelfort X, Melendo E, Cáceres E. Factors affecting meniscal extrusion: correlation with MRI, clinical, and arthroscopic findings. Knee Surg Sports Traumatol Arthrosc. 2006;14(4):394–398. doi: 10.1007/s00167-005-0688-8. [DOI] [PubMed] [Google Scholar]
- 50.Raynauld JP, Martel-Pelletier J, Berthiaume MJ, Beaudoin G, Choquette D, Haraoui B, et al. Long term evaluation of disease progression through the quantitative magnetic resonance imaging of symptomatic knee osteoarthritis patients: correlation with clinical symptoms and radiographic changes. Arthritis Res Ther. 2006;8(1):R21. doi: 10.1186/ar1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Y, Wluka AE, Pelletier JP, Martel-Pelletier J, Abram F, Ding C, et al. Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees. Rheumatology (Oxford). 2010;49(5):997–1004. doi: 10.1093/rheumatology/keq034. [DOI] [PubMed] [Google Scholar]
- 52.Bennett LD, Buckland-Wright JC. Meniscal and articular cartilage changes in knee osteoarthritis: a cross-sectional double-contrast macroradiographic study. Rheumatology (Oxford). 2002;41(8):917–923. doi: 10.1093/rheumatology/41.8.917. [DOI] [PubMed] [Google Scholar]
- 53.Foreman SC, Neumann J, Joseph GB, Nevitt MC, McCulloch CE, Lane NE, et al. Longitudinal MRI structural findings observed in accelerated knee osteoarthritis: data from the Osteoarthritis Initiative. Skeletal Radiol. 2019;48(12):1949–1959. doi: 10.1007/s00256-019-03242-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ding C, Martel-Pelletier J, Pelletier JP, Abram F, Raynauld JP, Cicuttini F, et al. Knee meniscal extrusion in a largely non-osteoarthritic cohort: association with greater loss of cartilage volume. Arthritis Res Ther. 2007;9(2):R21. doi: 10.1186/ar2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Patel R, Eltgroth M, Souza R, Zhang CA, Majumdar S, Link TM, et al. Loaded versus unloaded magnetic resonance imaging (MRI) of the knee: effect on meniscus extrusion in healthy volunteers and patients with osteoarthritis. Eur J Radiol Open. 2016;3:100–107. doi: 10.1016/j.ejro.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. doi: 10.2214/ajr.183.1.1830017. [DOI] [PubMed] [Google Scholar]
- 57•.Svensson F, Felson DT, Zhang F, Guermazi A, Roemer FW, Niu J, et al. Meniscal body extrusion and cartilage coverage in middle-aged and elderly without radiographic knee osteoarthritis. Eur Radiol. 2019;29(4):1848–54. Manuscript describing meniscus extrusion via MRI in over 700 patients validating the commonly used 3 mm cutoff for pathologic extrusion. [DOI] [PMC free article] [PubMed]
- 58.Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602–1606. doi: 10.1016/j.arthro.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 59.Liu Y, Joseph GB, Foreman SC, Li X, Lane NE, Nevitt MC, et al. Determining a threshold of medial meniscal extrusion for prediction of knee pain and cartilage damage progression over 4 years: data from the Osteoarthritis Initiative. AJR Am J Roentgenol. 2021;216(5):1318–1328. doi: 10.2214/AJR.20.23864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Karpinski K, Diermeier T, Willinger L, Imhoff AB, Achtnich A, Petersen W. No dynamic extrusion of the medial meniscus in ultrasound examination in patients with confirmed root tear lesion. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3311–3317. doi: 10.1007/s00167-018-5341-4. [DOI] [PubMed] [Google Scholar]
- 61.Cheng Q, Zhao FC. Comparison of 1.5- and 3.0-T magnetic resonance imaging for evaluating lesions of the knee: a systematic review and meta-analysis (PRISMA-compliant article) Medicine (Baltimore). 2018;97(38):e12401. doi: 10.1097/MD.0000000000012401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nogueira-Barbosa MH, Gregio-Junior E, Lorenzato MM, Guermazi A, Roemer FW, Chagas-Neto FA, et al. Ultrasound assessment of medial meniscal extrusion: a validation study using MRI as reference standard. AJR Am J Roentgenol. 2015;204(3):584–588. doi: 10.2214/AJR.14.12522. [DOI] [PubMed] [Google Scholar]
- 63.Krych AJ, Hevesi M, Leland DP, Stuart MJ. Meniscal root injuries. J Am Acad Orthop Surg. 2020;28(12):491–499. doi: 10.5435/JAAOS-D-19-00102. [DOI] [PubMed] [Google Scholar]
- 64.Choi HG, Kang YS, Kim JS, Lee HS, Lee YS. Meniscal and cartilage changes on serial MRI after medial opening-wedge high tibial osteotomy. Orthop J Sports Med. 2021;9(12):23259671211047904. doi: 10.1177/23259671211047904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65•.Lee CH, Yang HY, Seon JK. Increased medial meniscus extrusion led to worse clinical outcomes after medial opening-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2022:1–9. Manuscript describing the negative impact of >3 mm meniscus extrusion on outcomes of medial opening-wedge high tibial osteotomies. [DOI] [PubMed]
- 66.Jiang EX, Abouljoud MM, Everhart JS, DiBartola AC, Kaeding CC, Magnussen RA, et al. Clinical factors associated with successful meniscal root repairs: a systematic review. Knee. 2019;26(2):285–291. doi: 10.1016/j.knee.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 67.Moon HS, Choi CH, Yoo JH, Jung M, Lee TH, Jeon BH, et al. Mild to moderate varus alignment in relation to surgical repair of a medial meniscus root tear: a matched-cohort controlled study with 2 years of follow-up. Am J Sports Med. 2021;49(4):1005–1016. doi: 10.1177/0363546520988072. [DOI] [PubMed] [Google Scholar]
- 68.Faucett SC, Geisler BP, Chahla J, Krych AJ, Kurzweil PR, Garner AM, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–9. Manuscript describing the nearly half rate of osteoarthritis and lower costs associated with meniscus root repair as compared to meniscectomy and non-operative treatment. [DOI] [PubMed]
- 69.Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 70.Kaiser JT, Damodar D, Udine MJ, Meeker ZD, McCormick JR, Wagner KR, et al. Meniscal extrusion: a critical analysis review. JBJS Rev. 2022;10(7). [DOI] [PubMed]
- 71.Cinque ME, Chahla J, Moatshe G, Faucett SC, Krych AJ, LaPrade RF. Meniscal root tears: a silent epidemic. Br J Sports Med. 2018;52(13):872–876. doi: 10.1136/bjsports-2017-098942. [DOI] [PubMed] [Google Scholar]
- 72.Fithian DC, Kelly MA, Mow VC. Material properties and structure-function relationships in the menisci. Clin Orthop Relat Res. 1990;252:19–31. doi: 10.1097/00003086-199003000-00004. [DOI] [PubMed] [Google Scholar]
- 73.Cinque ME, Geeslin AG, Chahla J, Dornan GJ, LaPrade RF. Two-tunnel transtibial repair of radial meniscus tears produces comparable results to inside-out repair of vertical meniscus tears. Am J Sports Med. 2017;45(10):2253–2259. doi: 10.1177/0363546517704425. [DOI] [PubMed] [Google Scholar]
- 74.Cinque ME, DePhillipo NN, Moatshe G, Chahla J, Kennedy MI, Dornan GJ, et al. Clinical outcomes of inside-out meniscal repair according to anatomic zone of the meniscal tear. Orthop J Sports Med. 2019;7(7):2325967119860806. doi: 10.1177/2325967119860806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee WQ, Gan JZ, Lie DTT. Save the meniscus — clinical outcomes of meniscectomy versus meniscal repair. J Orthop Surg (Hong Kong). 2019;27(2):2309499019849813. doi: 10.1177/2309499019849813. [DOI] [PubMed] [Google Scholar]
- 76.Kaplan DJ, Alaia EF, Dold AP, Meislin RJ, Strauss EJ, Jazrawi LM, et al. Increased extrusion and ICRS grades at 2-year follow-up following transtibial medial meniscal root repair evaluated by MRI. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2826–2834. doi: 10.1007/s00167-017-4755-8. [DOI] [PubMed] [Google Scholar]
- 77.Kohno Y, Koga H, Ozeki N, Matsuda J, Mizuno M, Katano H, et al. Biomechanical analysis of a centralization procedure for extruded lateral meniscus after meniscectomy in porcine knee joints. J Orthop Res. 2022;40(5):1097–1103. doi: 10.1002/jor.25146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Koga H, Muneta T, Watanabe T, Mochizuki T, Horie M, Nakamura T, et al. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32(10):2000–2008. doi: 10.1016/j.arthro.2016.01.052. [DOI] [PubMed] [Google Scholar]
- 79.Koga H, Nakamura T, Katagiri H, Nakagawa Y, Ozeki N, Ohara T, et al. Two-year outcomes after meniscoplasty by capsular advancement with the application of arthroscopic centralization technique for lateral compartment knee osteoarthritis. Am J Sports Med. 2020;48(13):3154–3162. doi: 10.1177/0363546520957367. [DOI] [PubMed] [Google Scholar]
- 80.Mochizuki Y, Kawahara K, Samejima Y, Kaneko T, Ikegami H, Musha Y. Short-term results and surgical technique of arthroscopic centralization as an augmentation for medial meniscus extrusion caused by medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. 2021;31(6):1235–1241. doi: 10.1007/s00590-021-02874-9. [DOI] [PubMed] [Google Scholar]
- 81.Kodama Y, Furumatsu T, Okazaki Y, Takihira S, Hiranaka T, Miyazawa S, et al. Transtibial pullout repair of medial meniscus posterior root tears: effects on the meniscus healing score and ICRS grade among patients with mild osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2021;29(9):3001–3009. doi: 10.1007/s00167-020-06332-7. [DOI] [PubMed] [Google Scholar]
- 82•.Xue H, Furumatsu T, Hiranaka T, Kintaka K, Higashihara N, Tamura M, et al. Concomitant posterior anchoring further reduces posterior meniscal extrusion during pullout repair of medial meniscus posterior root tears: a retrospective study. Int Orthop. 2022:1–10. Manuscript describing the efficacy of adjunct posterior anchoring at limiting meniscus extrusion after posterior root tear repaired with the transtibial method. [DOI] [PubMed]