Abstract
Purpose of Review
The use of hip arthroscopy has expanded substantially over the last decade, including in pediatric and adolescent populations. Indications for hip arthroscopy in the pediatric population continue to be refined and research of outcomes following hip arthroscopy has increased. The purpose of this review is to provide an overview of current indications for hip arthroscopy in the pediatric population and the outcomes for each indication.
Recent Findings
Hip arthroscopy is used in the treatment of a range of pediatric hip conditions, spanning from the infant to young adult. In femoroacetabular impingement, hip arthroscopy in young adolescents has shown improvement in patient-reported outcome measures, high return to sport rates, and low complications. Intra-articular hip pathology secondary to Legg-Calve-Perthes and the persistent deformities following slipped capital femoral epiphysis can be managed with primary hip arthroscopy, and outcomes show significant improvements in patient-reported outcomes. Arthroscopy can be used safely as a reduction aid in developmental hip dysplasia, and as a primary treatment for borderline hip dysplasia in adolescents. In septic hip arthritis, arthroscopic drainage is a safe and effective treatment.
Summary
Hip arthroscopy is used in the pediatric and adolescent population in the management of femoroacetabular impingement, Legg-Calve-Perthes disease, the sequelae of slipped capital femoral epiphysies, developmental hip dysplasia, and septic arthritis. Research for each of these conditions shows that arthroscopy is a safe and effective treatment when performed for the correct indications, and results are comparable to open surgical options.
Keywords: Hip arthroscopy, Pediatric, Adolescent, Femoroacetabular impingement
Introduction
The indications for hip arthroscopy continue to be refined and the use of the procedure continues to grow [83]. Potential benefits over open procedures include less invasiveness, shorter operative times, shorter hospital stays, and better visualization of intra-articular anatomy [65••, 84].
Conditions of the hip in pediatrics are common and include the spectrum of developmental dysplasia, septic arthritis, Legg-Calve-Perthes disease (LCPD), slipped capital femoral epiphysis (SCFE), femoroacetabular impingement (FAI), juvenile arthritis, and trauma. Early use of hip arthroscopy in pediatric patients was reported by Gross for developmental dysplasia, septic arthritis, LCPD, and SCFE [85]. Other early uses of arthroscopy included the treatment of osteochondral lesions resulting from SCFE and juvenile arthritis [86, 87]. Although the literature is not as robust as in the adult population, there has been increased interest in the use of arthroscopy as the primary treatment of multiple pediatric hip conditions and as an adjunct to address intra-articular pathology. Outcome reporting has increased, with good short to mid-term results for a range of indications. This review provides an overview of hip arthroscopy in the pediatric and adolescent population with a focus on indications and outcomes.
Patient Evaluation
Clinical evaluation starts with taking a thorough history. Identifying the chief complaint, the duration, and onset of symptoms, and evaluating for any history of trauma are important starting points. A history of any known previous pediatric hip conditions should be elicited. Evaluation of whether the pain is from intra-articular or extra-articular pathology aids diagnosis. Intra-articular pathology typically presents with anterior hip or groin pain and may radiate to the knee [78]. Mechanical symptoms, such as snapping or catching, can suggest either an intra-articular or extra-articular pathology [78]. Precipitating factors, sports history, overall medical history, and any attempted treatments should be included.
Physical examination is similar to adults in patients over 12 years of age [78]. Assess the gait (Trendelenburg or ataxic) and weight bearing status. Observe the position of the leg and evaluate for leg length discrepancy. Record hip range of motion, starting with the normal limb, in flexion, extension, abduction, adduction, and internal and external rotation. Obligate external rotation with flexion of the hip may be seen in FAI and SCFE [78]. Decreased internal rotation may indicate intra-articular pathology. FADDIR (flexion, adduction, internal rotation) is a provocative test for impingement. FABER (flexion, abduction, external rotation), Thomas, Scour, and posterior impingement tests should be performed. Examination of the spine and knee, plus a detailed neurologic exam, helps identify other potential causes of hip pain or gait disturbance.
Imaging
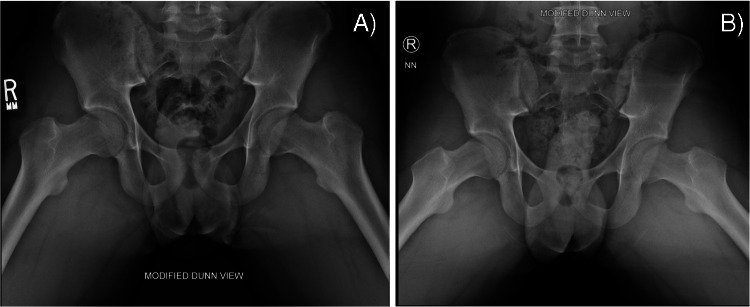
Radiographs including anterior–posterior (AP) and frog leg lateral views are a starting point for many diagnoses and no further imaging may be required. Specific views when assessing for femoroacetabular impingement (FAI) include the modified Dunn lateral [45 degrees flexion] (Fig. 1) and false-profile view of Lequesne and de Seze (78). In very young patients, ultrasound for developmental hip dysplasia is the primary modality. Ultrasound is also useful in the diagnosis of septic arthritis for evaluation of joint effusion and potential aspiration. The benefits of computed tomography (CT) scan should be balanced with risk of radiation. CT provides more details on bony anatomy than radiographs and is frequently used in FAI and DDH evaluation. Magnetic resonance imaging (MRI) provides the most detail about soft tissue and intra-articular anatomy. In young patients where cumulative radiation dosing is a concern, it is especially important. Recent evidence suggests three dimensional (3D) MRI can be used to evaluate osseous morphology in FAI and could replace the need for 3D CT scans, which would be especially beneficial in young patients [79].
Fig. 1.
Modified Dunn views of an adolescent male with femoroacetabular impingement. A Pre-operative images demonstrating cam morphology and B post-operative images after femoral osteochondroplasty with resection of cam morphology
Technique
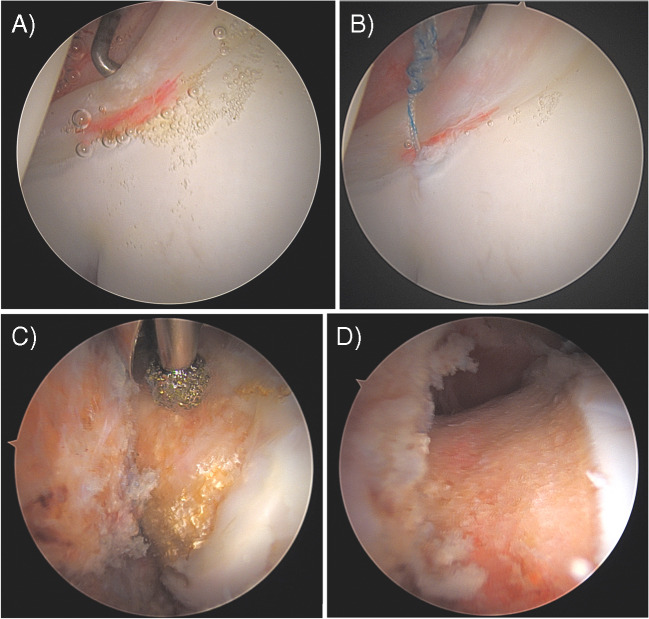
Hip arthroscopy can be performed in the supine or lateral position. Supine positioning on a fracture table without a perineal post is the preferred technique of the authors [89]. In very young children, they may be positioned on a radiolucent table without a post and the surgical assistant can provide gentle traction on the leg as needed [81, 82•]. Portals are established under fluoroscopic guidance, starting with the anterolateral portal [80]. The mid-anterior portal is established under direct visualization. Standard hip arthroscopy equipment can be used in adolescents and older children. In younger and small children, a specific 2.7-mm mini-hip arthroscope may be required [81]. After an interportal capsulotomy is performed with an arthroscopic blade or radiofrequency wand, a diagnostic arthroscopy is performed evaluating the labrum, status of ligamentum teres, articular cartilage, and the presence of cam or pincer morphology (Fig. 2). Further management depends on the indication for which the arthroscopy is being performed. Post-operative care will be dictated by the procedure performed and may involve spica casting in the case of reduction of a dislocated hip in dysplasia, use of a drain in septic arthritis, or a period of non-weight bearing and crutches for treatment of impingement. Early hip range of motion and physiotherapy is an important part of recovery.
Fig. 2.
Arthroscopic intra-operative images of an adolescent male left hip with femoroacetabular impingement showing A a labral tear pre and B post repair in addition to C cam morphology and D post femoroplasty of cam morphology
Specific Indications
Femoroacetabular Impingement
Assessment and Diagnosis
Femoroacetabular impingement (FAI) is a common cause of hip pain and limited sports participation in adolescents. Multiple studies have shown that cam morphology is a risk factor for development of hip osteoarthritis [88]. Diagnosis is based on symptoms, clinical findings, and imaging demonstrating early contact between the femoral head and acetabulum during hip motion [2]. Asymmetric hip pain, decreased hip range of motion, activity-related pain, and mechanical symptoms are all suggestive of FAI. On examination, there may be obligate external rotation with hip flexion and positive impingement signs. Imaging includes standard AP and lateral radiographs with additional Dunn and false-profile views. MRI arthrogram is helpful for evaluating intra-articular pathology such as labral tears and osteochondral defects.
Development of FAI
FAI may develop in adolescents secondary to SCFE, or iatrogenically after periacetabular osteotomy for developmental hip dysplasia [5–7]. Overgrowth of the femoral capital epiphysis not related to other hip pathology likely contributes to the majority of FAI and there is growing evidence to suggest that young athletes are at risk for development of cam-type deformities [8•, 9, 10]. Adolescent male basketball players compared to age-matched controls had higher alpha angles during and after closure of the proximal femur physis on MRI [11]. A systematic review and meta-analysis found male adolescent athletes to be at 1.9–8 times increased risk of developing cam morphology by skeletal maturity [12]. The sports at highest risk of developing cam morphology were basketball and hockey [12]. Adolescent soccer players also appear to have higher prevalence of cam morphology compared to non-athlete controls [9, 13, 14]. In adolescent male athletes, cam morphology appears to develop prior to closure of the proximal femoral physis particularly at the time of peak growth velocity, with evidence supporting a dose–response relationship with involvement in sports activity [8•, 15, 19]. Repetitive mechanical loading on an open physis during growth leading to epiphyseal hypertrophy has been proposed as an explanation for cam development [16, 17]. Prospective and cohort studies of adolescent athletes show that cam morphology primarily develops during growth starting at 12–14 years of age [17, 18]. Despite evidence that male athletes participating in specific sports are at higher risk of developing cam morphology, there is no clear understanding as to who will go on to become symptomatic and therefore it is difficult to recommend activity modifications or specific physical therapy as preventative measures [17]. Despite numerous studies of male adolescent athletes, there is minimal research investigating the development of FAI in females. In a study of the prevalence of cam-type deformity in professional women hockey players, there was a positive correlation between age of menarche and alpha angle [20]. In a retrospective review of female adolescent single sport athletes with a diagnosis of FAI, athletes participating in running, soccer, and hockey had significantly higher alpha angle than dancers [21]. Further research is needed to clarify the development and risk factors of FAI in female adolescent athletes. Pincer morphology on the acetabulum was not associated with sport participation during adolescence in a cohort of male and female athletes [19].
Treatment and Outcomes
Treatment of FAI in adults with hip arthroscopy has shown good mid- to long-term results and the use in pediatric FAI is increasing [3, 4]. Physiotherapy continues to be first-line treatment, with those failing non-operative management being considered for hip arthroscopy. Surgical management is based on individual pathology with femoroplasty for cam morphology, acetabuloplasty for pincer morphology, and repair or debridement of labral tears. Timing of surgery is controversial, although is usually delayed until closure of the proximal femoral physis to avoid damaging the growth plate. In adolescent patients with open physes undergoing hip arthroscopy for FAI, there is a theoretical risk of recurrence and growth restriction [23]. In patients with an open physis and communication of the cam morphology with the physis, it has been suggested to stage the procedure and address the cam morphology after growth plate closure [22]. In adolescents undergoing arthroscopy for FAI with a physis-sparing approach, there were significant sustained improvements in mHHS, HOS-ADL, and HOS-SSS 8.9 years post-operatively and the improvements were greater than in a matched adult cohort [39•]. In non-physeal-sparing femoral osteochondroplasty, ablation of the anterolateral physis during cam resection was utilized by Larson et al. to avoid recurrence, with good radiographic measurements and functional outcome scores and no deformity recurrence at 1 year post-op [23]. Although evidence is limited, other studies of hip arthroscopy for FAI in skeletally immature patients have not shown any avascular necrosis, growth restriction, or high levels of deformity recurrence [24, 25]. Outcomes after hip arthroscopy for FAI in adolescents have shown improved post-operative patient-reported outcome measures (PROMs), low revision rates (2–5%), low complication rates, and high rates of return to sport (84.9%) [26, 27]. In addition to PROMs, minimal clinically important differences (MCID) and patient acceptable symptom states (PASS) are met with high rates in the pediatric population up to 5-year follow-up [28••, 29, 30••]. As FAI is seen at higher rates in the athletic population, return to sport is an important indication of surgical success. Numerous studies have found high rates of return to sport after hip arthroscopy in the adolescent population (78.1–93%) [25, 31•]. Long-term studies are needed to investigate the rates of osteoarthritis and conversion to total hip arthroplasty in the adolescent population undergoing hip arthroscopy for FAI.
Legg-Calve-Perthes Disease
Assessment and Diagnosis
Legg-Calve-Perthes disease (LCPD) is a self-limiting process that develops as a result of ischemia in the capital femoral epiphysis of pediatric patients [35]. Initial diagnosis is made by clinical presentation and hip radiographs. As the fragmentation stage resolves, and re-ossification and remodeling occur, mechanical hip pain may develop secondary to loose bodies, labral tears, or impingement from a misshapen femoral head. MRI is useful in identifying intra-articular hip pathology and should be performed in those with persistent hip pain after a trial of conservative treatment, although it may not identify the full extent of the pathology that can be seen on arthroscopy [35].
Indications and Treatment Outcomes
In many patients, LCPD is well managed non-operatively with restricted weight bearing, analgesics, and physiotherapy, resulting in excellent results and preserved hip range of motion. Hip arthroscopy is indicated in patients who develop painful hips with mechanical symptoms after the resolution of active LCPD. Intra-articular findings seen as a sequelae of LCPD that can be addressed with arthroscopy include labral tears, osteochondritis dissecans, and ligamentum teres tears [32, 33]. Although there is limited published literature on hip arthroscopy for the treatment of sequelae of LCPD, initial results show improvement in hip function. At 2-year follow-up, Lee et al. found improved hip range of motion, VAS, and mHHS scores in a retrospective review of patients with late-stage sequelae of LCPD (p < 0.001) at a mean age of 26.4 years [36]. In six patients with late-stage LCPD and mean age of 15.2 years undergoing arthroscopy, there was improved hip function and symptoms after undergoing debridement, loose body removal, and osteochondroplasty [37]. In a systematic review and meta-analysis of hip arthroscopy for LCPD, there was a significant improvement in post-operative mHHS [38]. Specific technical challenges to arthroscopy with prior LCPD include navigating hypertrophy of the greater trochanter, coxa magna, and acetabular changes [33].
Borderline Developmental Dysplasia of the Hip
Assessment and Diagnosis
Developmental dysplasia of the hip (DDH) is a challenging problem to manage surgically throughout a patient’s life. As adolescents and adults, under coverage of the femoral head by the acetabulum can result in impingement on the labrum and micro-instability, and is a risk factor for developing osteoarthritis [40, 41]. Borderline DDH (BDDH) is defined as a lateral center–edge angle (LCEA) of 20–25 degrees [42]. Patients typically present with hip pain of insidious onset, although acute onset after a traumatic event is possible, and with functional impairment plus mechanical symptoms [43]. The LCEA is measured from the AP hip radiograph. MRI or MR arthrogram is a useful adjunct to evaluate for labral tears and intra-articular pathology [42].
Indications and Treatment Outcomes
Arthroscopy alone in the management of symptomatic borderline DDH has positive results in the adolescent population but is not recommended in patients with an LCEA < 18–20 degrees. Two systematic reviews have evaluated the PROMs of patients treated with arthroscopy for BDDH, all finding significant improvements in the mHHS and high rates of achieving the MCID (79.5%) for the mHHS [44, 45]. Meta-analysis by Krivicich et al. found patients with BDDH had non-inferior outcomes for multiple PROMs compared to control subjects without dysplasia, further supporting arthroscopy as a treatment for patients with symptomatic BDDH [46•]. Many studies included in the systematic reviews include patients less than 18 years old in their cohorts, but there are very few studies specifically looking at arthroscopy for BDDH in adolescents. Evans et al. compared adolescent patients, mean age 15.5 years, undergoing primary arthroscopy with BDDH to a control group and found significant improvements in mHHS, HOS-ADL, HOS-SS, and NAHS at 2 years post-operatively [43]. All patients in this study underwent capsular plication and epiphyseal closure (43). There were no revisions or conversions to total hip arthroplasty (THA) within the 2-year follow-up window [43]. This study supports hip arthroscopy as a viable option for mechanical pain in BDDH patients, with low rates of conversion to THA at least in the short term.
For patients with an LCEA < 20 degrees, periacetabular osteotomy (PAO) is often recommended. The use of arthroscopy as an adjunct to PAO to address intra-articular pathology is increasing and can be done in a combined or staged fashion. These procedures are done once growth has stopped, typically in the late adolescent to young adult ages when symptoms develop prior to the onset of arthritis. Although PAO alone shows good results in terms of functional outcome and PROMs improvements, intra-articular lesions that are a risk factor for progression of osteoarthritis are not addressed without addition of arthroscopy or open arthrotomy [51, 52]. Up to 59% of patients undergoing PAO for dysplasia have chondrolabral injuries [47]. In concomitant arthroscopy and PAO, the arthroscopy is completed first to address any intra-articular pathology or cam morphology with capsular closure. This has shown good results in terms of improvement in PROMs, high return to sport, comparable revision rates, and no increased complications compared to PAO alone [48, 49•, 50•, 54•]. Staging arthroscopy to be done at an earlier surgical date than the PAO is an emerging concept. In a comparison between staged versus combined hip arthroscopy and PAO, Orner et al. found no differences in the outcomes at 12 months post-op and significantly improved PROMs from pre- to post-op for both groups [53]. The authors propose that a benefit of staging would be the arthroscopy could inform operative decision-making for the PAO, including canceling surgery if the chondral defects were sufficiently advanced to be a contraindication for PAO [53].
Arthroscopic-Assisted Reduction in Developmental Dysplasia
Assessment and Diagnosis
Ultrasound screening for DDH has significantly reduced the need for surgical management and the likelihood of late presentation [55]. In infants with developmental hip dysplasia and failure of treatment with a Pavlik harness, there are several potential blocks to a closed reduction. Obstacles to reduction in dislocated hips include a hypertrophied ligamentum teres and transverse ligament, a constricted capsule, or the pulvinar [57].
Indications and Treatment Outcomes
In patients with DDH and failed closed reduction, surgical management is indicated. Traditionally open reduction through a medial or anterior approach has been used. The major concern with open reduction is the risk of avascular necrosis (AVN), with a systematic review finding an overall AVN rate after medial open reduction to be 20% [56]. Arthroscopic-assisted reduction has been used as an alternative to traditional open reduction. The majority of studies are small retrospective case series with 3 to 40 patients [57–61, 63]. All studies showed successful reduction in 80–100% of cases, with capsule constriction, hypertrophied ligamentum teres, and transverse ligament being the most common reason for a block to reduction and requiring release [57–61, 63]. The rate of AVN was reported from 0% at 60-month follow-up, to 38% at 13.2-month follow-up [57, 58]. In a comparison of patients treated with open medial reduction versus arthroscopic reduction, there were no differences in acetabular index 26 degrees in both groups or rate of AVN [62••]. These results are comparable to those reported for open reduction and further studies plus longer term follow-up will help determine if there are any clear differences in the outcome between arthroscopic and open reduction.
Septic Arthritis
Assessment and Diagnosis
Septic arthritis of the hip in pediatrics requires urgent diagnosis and treatment to prevent long-term sequelae. Presenting symptoms include inability to weight bear, dysfunction and pain in the hip, fever, and malaise [64]. Laboratory studies showing an elevated white blood cell count, CRP, ESR and blood cultures aid in the diagnosis [64]. Ultrasound and MRI imaging can identify an effusion and support the diagnosis [64]. Arthrocentesis of synovial fluid with positive cultures and cell count demonstrating a WBC of > 50,000/mm3 and > 75% polymorphonuclear neutrophils is diagnostic [64].
Indications and Treatment
Once septic arthritis of the hip is diagnosed, treatment with arthrocentesis, arthroscopy, or arthrotomy is required to drain and irrigate the joint. Destruction of the articular surface can begin within 8 hours of inoculation and increased intracapsular pressure may lead to ischemia and avascular necrosis [64]. Arthroscopy has emerged as an alternative to open arthrotomy in the treatment of septic hip arthritis in pediatrics. In a prospective controlled study investigating arthrotomy versus arthroscopy for septic hip arthritis, El-Sayed found all infections were successfully treated in each group and there were no difference in the outcomes following surgery [65••]. There were significant differences in the length of hospital stay, with patients treated with arthroscopy having an earlier discharge (3.8 versus 6.4 days) [65••]. In a large retrospective database review, there was no difference in the return to operating room or short-term complications at 30 days between arthrotomy and arthroscopy [65••]. In a systematic review of drainage techniques for pediatric septic hip arthritis, patients treated with arthroscopy without a drain required a repeat drainage in 14% of cases compared to 3% risk of additional drainage with arthrotomy [66]. There were worse clinical outcomes and increased radiological findings at follow-up after arthrotomy than with arthroscopy; however, the authors felt it was difficult to draw conclusions as the quality of studies was low [66]. From the available literature, it appears arthroscopy with the use of a drain is an effective technique for treating pediatric septic hip arthritis, including very young children from 6 months of age [67].
Sequelae of Slipped Capital Femoral Epiphyses
Assessment and Diagnosis
Slipped capital femoral epiphyses (SCFE) is the most common adolescent hip pathology, with an incidence of up to 10 cases per 100,000 [68]. Patients present with either hip/groin or knee pain and may be unable to weight bear on the affected leg. On physical exam, the leg may be shortened and held in an externally rotated position and there is limited internal rotation, abduction, and flexion of the affected hip [69]. Anteroposterior and frog leg lateral radiographs display the posterior-inferior translation of the capital femoral epiphysis in relation to the metaphysis [69]. Treatment of SCFE is initially with either in situ pinning or open reduction. Even in cases with mild residual deformity, there is an increased risk of osteoarthritis after SCFE treatment [70].
Indications and Treatment
Persistent deformity at the proximal femoral epiphysis leads to FAI secondary to SCFE [71, 72]. The resulting deformity results in loss of sphericity at the anterior femoral neck and results in an increased alpha angle [71]. Arthroscopy post-SCFE fixation has shown chondrolabral pathology, impingement at the anterior acetabular rim, and labral tears, with more advanced pathology the longer out from SCFE fixation [72, 74]. At 5-year follow-up, a retrospective review of SCFE patients treated with in situ pinning and staged arthroscopy showed stable improvement in the alpha angle to within normal range and normal hip internal range of motion [73•]. There were signs of progressive cartilage damage in 4/11 patients at 5-year follow-up MRI [73•]. A systematic review by Saito et al. found that in FAI secondary to SCFE, arthroscopic osteochondroplasty improved PROMs at short-term follow-up, improved hip internal rotation, and restored the alpha angle [74]. In patients with severe slips (> 60 degrees), more complex deformities such as acetabular or femoral retroversion can develop, which are challenging to address with arthroscopy [75]. While there is evidence that FAI after severe SCFE may be treated successfully with arthroscopy, other research has shown poor results in those with severe SCFE [76, 77]. Arthroscopy to address post-SCFE FAI has good results in mild and moderate slips, while further research is needed to determine outcomes in more severe slips. A short interval between initial SCFE management and arthroscopy may reduce the long-term sequelae associated with post-SCFE FAI [74].
Conclusion
Hip arthroscopy is used in pediatric and adolescent patients for a variety of indications including FAI, LCPD, SCFE, septic hip arthritis, and developmental hip dysplasia. Safety of hip arthroscopy in very young children to adolescents has been demonstrated, with some evidence for shorter duration of hospitalization and operative times over open procedures [65••, 84]. Short- to medium-term outcomes show significant improvements in patient-reported outcome measures and return to sport [26, 27, 36, 39•, 44, 45, 62••, 65••, 73•, 74]. Studies reporting long-term follow-up will further help to refine indications for hip arthroscopy in adolescents.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Ethics Approval
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Conflict of Interest
Helen Crofts, Mark McConkey, and Parth Lodhia declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Helen Crofts, Email: h.crofts@alumni.ubc.ca.
Mark McConkey, Email: mark_mcconkey@hotmail.com.
Parth Lodhia, Email: parth.lodhia@ubc.ca.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Grifn DR, Dickenson EJ, O’Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50:1169–1176. doi: 10.1136/bjsports-2016-096743. [DOI] [PubMed] [Google Scholar]
- 2.Kyin C, Maldonado DR, Go CC, Shapira J, Lall AC, Domb BG. Mid- to long-term outcomes of hip arthroscopy: a systematic review. Arthroscopy. 2021;37(3):1011–1025. doi: 10.1016/j.arthro.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Sing David C, Brian T Feeley, Bobby Tay, Thomas P Vail, and Alan L Zhang. “Age-related trends in hip arthroscopy: a large cross-sectional analysis.” Arthroscopy: The Journal of Arthroscopic & Related Surgery: Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2015;31, 12: 2307-2313.e2. 10.1016/j.arthro.2015.06.008. [DOI] [PubMed]
- 4.Myers, S. R. MD; Eijer, H. MD; Ganz, R. MD. Anterior femoroacetabular impingement after periacetabular osteotomy. Clinical Orthopaedics and Related Research 363():p 93–99, June 1999. [PubMed]
- 5.Leunig, Michael, Mark M Casillas, Marc Hamlet, Othmar Hersche, Hubert Nötzli, Theddy Slongo, and Reinhold Ganz. “Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis.” Acta Orthopaedica Scandinavica 71 4 (2000): 370–75. 10.1080/000164700317393367. [DOI] [PubMed]
- 6.Wenger Dennis R, Kishan Shyam, Pring Maya E. Impingement and childhood hip disease. Journal of Pediatric Orthopaedics B. 2006;15(4):233–243. doi: 10.1097/01202412-200607000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Siebenrock KA, Wahab KH, Werlen S, Kalhor M, Leunig M, Ganz R. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;418:54–60. doi: 10.1097/00003086-200401000-00010. [DOI] [PubMed] [Google Scholar]
- 8•.Hanke MS, Schmaranzer F, Steppacher SD, Reichenbach S, Werlen SF, Siebenrock KA. A cam morphology develops in the early phase of the final growth spurt in adolescent ice hockey players: results of a prospective MRI-based study. Clin Orthop Relat Res. 2021;479(5):906–18. 10.1097/CORR.0000000000001603.PMID:33417423;PMCID:PMC8052031.This prospective study of adolescent hockey players used MRI at 1.5 years and 3 years during their growth spurt and showed cam morphology develops in the early phases of the final growth spurt. [DOI] [PMC free article] [PubMed]
- 9.Siebenrock KA, Ferner F, Noble PC, Santore RF, Werlen S, Mamisch TC. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res. 2011;469(11):3229–40. doi: 10.1007/s11999-011-1945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agricola R, Bessems JH, Ginai AZ, Heijboer MP, van der Heijden RA, Verhaar JA, Weinans H, Waarsing JH. The development of cam-type deformity in adolescent and young male soccer players. Am J Sports Med. 2012;40(5):1099–1106. doi: 10.1177/0363546512438381. [DOI] [PubMed] [Google Scholar]
- 11.Nepple, Jeffrey J., Jonathan M. Vigdorchik, and John C. Clohisy. “What is the association between sports participation and the development of proximal femoral cam deformity?: a systematic review and meta-analysis.” The Am J Sports Med 2015;43, no. 11: 2833–40. 10.1177/0363546514563909. [DOI] [PubMed]
- 12.Yépez, Anthony Kerbes, Marcelo Abreu, Bruno Germani, and Carlos Roberto Galia. “Prevalence of femoroacetabular impingement morphology in asymptomatic youth soccer players: magnetic resonance imaging study with clinical correlation.” Revista Brasileira De Ortopedia 2017;52, Suppl 1: 14–20. 10.1016/j.rboe.2017.06.005. [DOI] [PMC free article] [PubMed]
- 13.Fernquest Scott, Palmer Antony, Gimpel Mo, Birchall Richard, Broomfield John, Wedatilake Thamindu, Dijkstra Hendrik, et al. A longitudinal cohort study of adolescent elite footballers and controls investigating the development of cam morphology. Sci. Rep. 2021;11(1):18567. doi: 10.1038/s41598-021-97957-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tak, Igor, Adam Weir, Rob Langhout, Jan Hendrik Waarsing, Janine Stubbe, Gino Kerkhoffs, and Rintje Agricola. “The relationship between the frequency of football practice during skeletal growth and the presence of a cam deformity in adult elite football playerS.” Br. J. Sports Med 2015; 49, 9: 630–34. 10.1136/bjsports-2014-094130. [DOI] [PubMed]
- 15.Pettit, M, Doran C, Singh Y, Saito M, Sunil Kumar KH, and Khanduja V. “How does the cam morphology develop in athletes? A systematic review and meta-analysis.” Osteoarthritis and Cartilage 2021;29, 8: 1117–29. 10.1016/j.joca.2021.02.572. [DOI] [PubMed]
- 16.Carsen, Sasha, Paul J. Moroz, Kawan Rakhra, Leanne M. Ward, Hal Dunlap, John A. Hay, R. Baxter Willis, and Paul E. Beaulé. “The Otto Aufranc Award. On the etiology of the cam deformity: a cross-sectional pediatric MRI studyClin. Orthop. Relat. Res. 2014; 472, 2: 430–36. 10.1007/s11999-013-2990-y. [DOI] [PMC free article] [PubMed]
- 17.Palmer A, Fernquest S, Gimpel Mo, Birchall R, Judge A, Broomfield J, Newton J, Wotherspoon M, Carr A, Glyn-Jones S. Physical activity during adolescence and the development of cam morphology: a cross-sectional cohort study of 210 individuals. Br J Sports Med. 2018;52(9):601–610. doi: 10.1136/bjsports-2017-097626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Klij, Pim, Marinus P. Heijboer, Abida Z. Ginai, Jan A. N. Verhaar, Jan H. Waarsing, and Rintje Agricola. “Cam morphology in young male football players mostly develops before proximal femoral growth plate closure: a prospective study with 5-yearfollow-up.” Br. J. Sports Med. 2019;53, 9: 532–38. 10.1136/bjsports-2018-099328. [DOI] [PubMed]
- 19.Westermann RW, Scott EJ, Schaver AL, Schneider A, Glass NA, Levy SM, Willey MC. Activity level and sport type in adolescents correlate with the development of cam morphology. JB JS Open Access. 2021 Nov 11;6(4):e21.00059. 10.2106/JBJS.OA.21.00059. PMID: 34841184; PMCID: PMC8613345. [DOI] [PMC free article] [PubMed]
- 20.Carter, Cordelia W, Abigail Campbell, Darryl Whitney, Oren Feder, Matthew Kingery, Samuel Baron, Thomas Youm, and Guillem Gonzalez-Lomas. “Characterizing cam-type hip impingement in professional women’s ice hockey players.” Phys Sportsmed 2021;49, 2: 203–6. 10.1080/00913847.2020.1808434. [DOI] [PubMed]
- 21.Fraser, Joana L., Dai Sugimoto, Yi-Meng Yen, Pierre A. d’Hemecourt, and Andrea Stracciolini. “Bony morphology of femoroacetabular impingement in young female dancers and single-sport athletes.” Orthopaedic J Sports Med. 2017; 5, 8: 2325967117723108. 10.1177/2325967117723108. [DOI] [PMC free article] [PubMed]
- 22.Philippon, Marc J, Leandro Ejnisman, Henry B Ellis, and Karen K Briggs. “Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years.” Arthroscopy: The Journal of Arthroscopic & Related Surgery 2012;28, 9: 1255–61. 10.1016/j.arthro.2012.02.006. [DOI] [PubMed]
- 23.Larson, Christopher M, Rebecca Stone McGaver, Nicole R, Collette M, Russell Giveans, James R. Ross, Asheesh Bedi, and Jeffrey J. Nepple. “Arthroscopic surgery for femoroacetabular impingement in skeletally immature athletes: radiographic and clinical analysis.” Arthroscopy: The Journal of Arthroscopic & Related Surgery 2019; 35, 6: 1819–25. 10.1016/j.arthro.2019.01.029. [DOI] [PubMed]
- 24.Nwachukwu BU, McFeely ED, Nasreddine AY, Krcik JA, Frank J, Kocher MS. Complications of hip arthroscopy in children and adolescents. Journal of Pediatric Orthopaedics. 2011;31(3):227. doi: 10.1097/BPO.0b013e31820cadc5. [DOI] [PubMed] [Google Scholar]
- 25.Tran P, Pritchard M, O’Donnell J. Outcome of arthroscopic treatment for cam type femoroacetabular impingement in adolescents. ANZ J Surg. 2013;83(5):382–386. doi: 10.1111/j.1445-2197.2012.06197.x. [DOI] [PubMed] [Google Scholar]
- 26.Huang H-J, Zhou X, Huang Z-G, Dang H-H, Xue S-L, Zhang Z-y, Zhang X, Wang J-Q. Arthroscopic treatment for femoroacetabular impingement syndrome in adolescents: a systematic review and meta-analysis. Clin J Sport Med. 2022;32(6):608. doi: 10.1097/JSM.0000000000001053. [DOI] [PubMed] [Google Scholar]
- 27.Chen, Sarah L, David R, Maldonado Cammille C Go, Cynthia Kyin, Ajay C, Lall, and Benjamin G. Domb. “Outcomes of hip arthroscopic surgery in adolescents with a subanalysis on return to sport: a systematic review.” Am J Sports Med. 2020;48, 61526–34. 10.1177/0363546519875131. [DOI] [PubMed]
- 28••.Maldonado David R, Allison Y Kufta, Aaron J Krych, Bruce A Levy, Kelechi R Okoroha, Karina Gonzalez-Carta, and Benjamin G Domb. “Primary hip arthroscopy for femoroacetabular impingement syndrome in adolescents improves outcomes and clinical benefit achievement rates at short-term follow-Up. A multicenter analysis.” Arthrosc. - J. Arthrosc. Relat. Surg, December 8, 2022. 10.1016/j.arthro.2022.11.020.This study of adolescent patients with FAI undergoing primary hip arthroscopy showed significant improvement in all PROM’s at 2 year follow-up and high patient satisfaction. [DOI] [PubMed]
- 29.Cvetanovich Gregory L, Alexander E Weber, Benjamin D Kuhns, Charles P Hannon, Dwayne D’Souza, Joshua Harris, Richard C III Mather, and Shane J Nho. “Clinically meaningful improvements after hip arthroscopy for femoroacetabular impingement in adolescent and young adult patients regardless of gender.” J. Pediatr. Orthop. 38, 9 (2018): 465. 10.1097/BPO.0000000000000852. [DOI] [PubMed]
- 30••.Beck Edward C, Nwachuckwu Benedict U, Jan Kyleen, Nho Shane J. “Hip arthroscopy for femoroacetabular impingement syndrome in adolescents provides clinically significant outcome benefit at minimum 5-year follow-up” Arthroscopy. J Arthrosc Relat Surg. 2021;37(5):1467-1473.e2. 10.1016/j.arthro.2020.12.188.This study of adolescent patients undergoing primary hip arthroscopy for FAI showed at 5 year follow-up 89.2% of patients reached the MCID and there was a low (2.4%) revision rate. [DOI] [PubMed]
- 31•.Barastegui, David, Roberto Seijas, Eduard Alentorn-Geli, Alfred Ferré-Aniorte, Patricia Laiz, and Ramon Cugat. “Hip arthroscopy is a successful treatment for femoroacetabular impingement in under-16 competitive football players: a prospective study with minimum 2-year follow-up.” Archives of Orthopaedic and Trauma Surgery, 2022. 10.1007/s00402-022-04584-1.This prospective study of under-16 competitive football players undergoing hip arthroscopy for FAI showed significant improvements in all PROM’s at minimum 2 year follow-up and high return to sport (92.86%) at final follow-up. [DOI] [PubMed]
- 32.Ross JR, Nepple JJ, Baca G, Schoenecker PL, Clohisy JC. Intraarticular abnormalities in residual Perthes and Perthes-like hip deformities. Clin Orthop Relat Res. 2012;470(11):2968–2977. doi: 10.1007/s11999-012-2375-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roy Dennis R. “Arthroscopic findings of the hip in new onset hip pain in adolescents with previous Legg–Calvé–Perthes disease.” J. Pediatr. Orthop. 2005;B 14, 3: 151. [DOI] [PubMed]
- 34.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calvé-Perthes disease. JBJS. 1981;63(7):1095. doi: 10.2106/00004623-198163070-00006. [DOI] [PubMed] [Google Scholar]
- 35.Tiwari V, Gamanagatti S, Mittal R, Nag H, Khan SA. Correlation between MRI and hip arthroscopy in children with Legg-Calve-Perthes disease. Musculoskelet Surg. 2018;102(2):153–157. doi: 10.1007/s12306-017-0513-9. [DOI] [PubMed] [Google Scholar]
- 36.Lee W-Y, Hwang D-S, Ha Y-C, Kim P-S, Zheng L. Outcomes in patients with late sequelae (healed stage) of Legg-Calvé-Perthes disease undergoing arthroscopic treatment: retrospective case series. Hip International: The Journal of Clinical and Experimental Research on Hip Pathology and Therapy. 2018;28(3):302–308. doi: 10.5301/hipint.5000563. [DOI] [PubMed] [Google Scholar]
- 37.Lim, Chaemoon, Tae-Joon Cho, Chang Ho Shin, In Ho Choi, and Won Joon Yoo. “Functional outcomes of hip arthroscopy for pediatric and adolescent hip disorders.” Clin Orthop Surg 2020;12, 1: 94–99. 10.4055/cios.2020.12.1.94. [DOI] [PMC free article] [PubMed]
- 38.Goyal Tarun, Sitanshu Barik, and Tushar Gupta. “Hip arthroscopy for sequelae of Legg-Calve-Perthes disease: a systematic review.” Hip & Pelvis 2021;33, 1: 3–10. 10.5371/hp.2021.33.1.3. [DOI] [PMC free article] [PubMed]
- 39•.Fukase, Naomasa, Yoichi Murata, Lauren A. Pierpoint, Rui W. Soares, Justin W. Arner, Joseph J. Ruzbarsky, Patrick M. Quinn, and Marc J. Philippon. “Outcomes and survivorship at a median of 8.9 years following hip arthroscopy in adolescents with femoroacetabular impingement: a matched comparative study with adults.” J. Bone Jt. Surg. American Volume 2022; 104, 10: 902–9. 10.2106/JBJS.21.00852.In this comparative study between adolescents (<19 years) and adults with FAI undergoing hip arthroscopy, adolescent patients with open physes had significant improvements in PROM’s post-operatively and no difference in revision rates compared to adults. [DOI] [PubMed]
- 40.Klaue, K, Durnin CW, and Ganz R. “The acetabular rim syndrome. A clinical presentation of dysplasia of the hip.” J. Bone Jt. Surg British Volume 1991;73-B, 3: 423–29. 10.1302/0301-620X.73B3.1670443 [DOI] [PubMed]
- 41.Boykin RE, Anz AW, Bushnell BD, Kocher MS, Stubbs AJ, Philippon MJ. Hip instability. JAAOS - Journal of the American Academy of Orthopaedic Surgeons. 2011;19(6):340. doi: 10.5435/00124635-201106000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Evans Peter T, John M Redmond, Jon E Hammarstedt, Yuan Liu, Edwin O Chaharbakhshi, and Benjamin G Domb. “Arthroscopic treatment of hip pain in adolescent patients with borderline dysplasia of the hip: minimum 2-year follow-upArthrosc. - J. Arthrosc. Relat. Surg. 2017; 33, 8: 1530–36. 10.1016/j.arthro.2017.03.008. [DOI] [PubMed]
- 43.Evans Peter T, John M Redmond, Jon E Hammarstedt, Yuan Liu, Edwin O Chaharbakhshi, and Benjamin G Domb. “Arthroscopic treatment of hip pain in adolescent patients with borderline dysplasia of the hip: minimum 2-year follow-up.” Arthroscopy: J. Arthrosc. Relat. Surg. 2017; 33, 8: 1530–36. 10.1016/j.arthro.2017.03.008. [DOI] [PubMed]
- 44.Ding Zheci, Sun Yaying, Liu Shaohua, Chen Jiwu. Hip arthroscopic surgery in borderline developmental dysplastic hips: a systematic review. Am J Sports Med. 2019;47(10):2494–2500. doi: 10.1177/0363546518803367. [DOI] [PubMed] [Google Scholar]
- 45.Kuroda Yuichi, Masayoshi Saito, Karadi Hari Sunil Kumar, Ajay Malviya, and Vikas Khanduja. “Hip arthroscopy and borderline developmental dysplasia of the hip: a systematic review.” Arthrosc. - J. Arthrosc. Relat. Surg. 2020; 36, 9: 2550–2567.e1. 10.1016/j.arthro.2020.05.035. [DOI] [PubMed]
- 46• .Krivicich Laura M, Rice Morgan, Sivasundaram Lakshmanan, Nho Shane J. Borderline dysplastic hips undergoing hip arthroscopy achieve equivalent patient reported outcomes when compared with hips with normal acetabular coverage: a systematic review and meta-analysis. JAAOS - J Am Acad Orthop Surg. 2023;31(6):e336. 10.5435/JAAOS-D-22-00302.This systematic review and meta-analysis of studies reporting post-operative PROM’s for patients with borderline DDH found there were no differences in PROM’s between borderline DDH patients and those with normal acetabular coverage. [DOI] [PubMed]
- 47.Ross James R, Zaltz Ira, Nepple Jeffrey J, Schoenecker Perry L, Clohisy John C. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011;39(1):72–78. doi: 10.1177/0363546511412320. [DOI] [PubMed] [Google Scholar]
- 48.Domb Benjamin G, LaReau Justin M, Hammarstedt Jon E, Gupta Asheesh, Stake Christine E, Redmond John M. Concomitant hip arthroscopy and periacetabular osteotomy. Arthrosc. - J. Arthrosc. Relat. Surg. 2015;31(11):2199–2206. doi: 10.1016/j.arthro.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 49•.Sabbag Casey M, Jeffrey J Nepple, Cecilia Pascual-Garrido, Gopal R Lalchandani, John C Clohisy, and Rafael J Sierra. “The addition of hip arthroscopy to periacetabular osteotomy does not increase complication rates: a prospective case series.” Am J Sports Med. 2019;47, no. 3: 543–51. 10.1177/0363546518820528.This study of patients undergoing combined hip arthroscopy and peri-acetabular osteotomy (PAO) found a complication rate of 3%, which is similar to published complication rates for PAO alone. [DOI] [PubMed]
- 50•.Edelstein Adam I, Jeffrey J Nepple, Wahid Abu-Amer, Cecilia Pascual-Garrido, Charles W Goss, and John C Clohisy. “What mid-term patient-reported outcome measure scores, reoperations, and complications are associated with concurrent hip arthroscopy and periacetabular osteotomy to treat dysplasia with associated intraarticular abnormalities?” Clin. Orthop. Relat. Res. ® 2021; 479, 5: 1068. 10.1097/CORR.0000000000001599.This study showed that in patients with DDH, concurrent hip arthroscopy and PAO provided significant improvements in PROM’s at minimum 4 year follow-up but persistent symptoms in 21% of patients. [DOI] [PMC free article] [PubMed]
- 51.Clohisy John C, Ackerman Jeffrey, Baca Geneva, Baty Jack, Beaulé Paul E, Kim Young-Jo, Millis Michael B, et al. Patient-reported outcomes of periacetabular osteotomy from the prospective ANCHOR cohort study. J. Bone Jt. Surg. American. 2017;99(1):33–41. doi: 10.2106/JBJS.15.00798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fujii M, Nakashima Y, Noguchi Y, Yamamoto T, Mawatari T, Motomura G, and Iwamoto Y. “Effect of intra-articular lesions on the outcome of periacetabular osteotomy in patients with symptomatic hip dysplasia.” J. Bone Jt. Surg.. British Volume 2011;93, 11: 1449–56. 10.1302/0301-620X.93B11.27314. [DOI] [PubMed]
- 53.Orner, Caitlin A, Brittany E Haws, John Reuter, Raymond Kenney, P Christopher Cook, and Brian D Giordano. “Patient-reported outcomes are similar in the first two years after staged versus combined hip arthroscopy and periacetabular osteotomy for hip dysplasia.” Arthrosc. - J. Arthrosc. Relat. Sur 2023. 10.1016/j.arthro.2023.02.017. [DOI] [PubMed]
- 54•.Jimenez Andrew E, Michael S Lee, Jade S Owens, David R Maldonado, Justin M LaReau, and Benjamin G. Domb. “Athletes undergoing concomitant hip arthroscopy and periacetabular osteotomy demonstrate greater than 80% return-to-sport rate at 2-year minimum follow-up.” Arthroscopy: The Journal of Arthroscopic & Related Surgery: Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2022;38, 9: 2649–58. 10.1016/j.arthro.2022.02.017.This study showed that at 2 year follow up patients with acetabular dysplasia who underwent concomitant hip arthroscopy and PAO had significant improvements in PROM’s and high return to sport (81.8%). [DOI] [PubMed]
- 55.Wirth T, Stratmann L, and Hinrichs F. “Evolution of late presenting developmental dysplasia of the hip and associated surgical procedures after 14 years of neonatal ultrasound screening.” J. Bone Jt. Surg. British Volume 2004;86-B, 4: 585–89. 10.1302/0301-620x.86b4.14586. [PubMed]
- 56.Gardner ROE, Bradley CS, Howard A, Narayanan UG, Wedge JH, and Kelley SP. “The incidence of avascular necrosis and the radiographic outcome following medial open reduction in children with developmental dysplasia of the hip: a systematic review.” J. Bone Jt. Surg. 2014;96-B, 2: 279–86. 10.1302/0301-620X.96B2.32361. [DOI] [PubMed]
- 57.Eberhardt O, Fernandez FF, and Wirth T. “Arthroscopic reduction of the dislocated hip in infants.” J. Bone Jt. Surg. British Volume 2012;94-B, 6: 842–47. 10.1302/0301-620X.94B6.28161. [DOI] [PubMed]
- 58.Zhao Liang, Yan Hua, Yang Changsheng, Cai Daozhang, Wang Yijun. Medium-term results following arthroscopic reduction in walking-age children with developmental hip dysplasia after failed closed reduction. J. Orthop. Surg. Res. 2017;12(1):135. doi: 10.1186/s13018-017-0635-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xu Hui-fa, Yan Ya-bo, Chao Xu, Li Tian-qing, Zhao Tian-feng, Liu Ning, Huang Lu-yu, Zhang Chun-li, Lei Wei. Effects of arthroscopic-assisted surgery on irreducible developmental dislocation of hip by mid-term follow-up: an observational study. Medicine. 2016;95(33):e4601. doi: 10.1097/MD.0000000000004601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Öztürk, Hayati, Zekeriya Öztemür, Okay Bulut, Gündüz Tezeren, and Sema Bulut. “Arthroscopic-assisted surgical treatment for developmental dislocation of the hip before the age of 18 months.” Archives of Orthopaedic and Trauma Surgery 2013;133, 9: 1289–94. 10.1007/s00402-013-1781-y. [DOI] [PubMed]
- 61.Kitano, Toshio, Yuuki Imai, Mitsuaki Morita, Keisuke Nakagawa, Mayuko Wada, Toshiyuki Sakai, Yoshitaka Eguchi, and Takaaki Kuroda. “New treatment method for developmental dysplasia of the hips after walking age: arthroscopic reduction with limboplasty based on the findings of preoperative imaging.” J Orthop Sci 2010;15 ,4: 443–51. 10.1007/s00776-010-1497-6. [DOI] [PubMed]
- 62••.Duman S, Camurcu Y, Sofu H, Ucpunar H, Akbulut D, Yildirim T. Arthroscopic versus open, medial approach, surgical reduction for developmental dysplasia of the hip in patients under 18 months of age. Acta Orthop. 2019;90(3):292–6. 10.1080/17453674.2019.1599775.This retrospective case-series compared medial open approach versus arthroscopic assisted reduction of patients with DDH under 18 months and showed no difference in radiologic or clinical outcomes between groups [DOI] [PMC free article] [PubMed]
- 63.Feng, Chao, Xue-Min Lv, Shi-Qi Wan, and Yuan Guo. “A single approach to arthroscopic reduction and debridement for developmental dislocation of the hip in 12 infants.” Medical Science Monitor: International Medical Journal of Experimental and Clinical Research 2019;25: 8807–13. 10.12659/MSM.916434. [DOI] [PMC free article] [PubMed]
- 64.Montgomery Nicole I, and Howard R Epps. “Pediatric septic arthritis.” Orthopedic Clinics of North America, Infection, 2017;48, 2: 209–16. 10.1016/j.ocl.2016.12.008. [DOI] [PubMed]
- 65••.Khazi, Zain M, William T Cates, Qiang An, Kyle R Duchman, Brian R Wolf, and Robert W Westermann. “Arthroscopy versus open arthrotomy for treatment of native hip septic arthritis: an analysis of 30-day complications.” Arthroscopy: The Journal of Arthroscopic & Related Surgery: Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2020; 36, 4 1048–52. 10.1016/j.arthro.2019.10.008.This study of patients with septic hip arthritis compared arthroscopic versus open arthrotomy and found no significant difference in early complications or risk of recurrence between groups. [DOI] [PubMed]
- 66.Donders, Cornelia Maria, Anne J Spaans, Johannes H J M Bessems, and Christiaan J A van Bergen. “A systematic review of the optimal drainage technique for septic hip arthritis in children.” HIP International 2022;32, 5: 685–93. 10.1177/1120700021989666. [DOI] [PubMed]
- 67.Ellis, Henry B, Lawson Copley, Andrew Pennock, Jeffrey J Nepple, Clifton Willimon, Stephanie W Mayer, and Yi-Meng Yen. “Tractionless hip arthroscopy for septic arthritis in children.” Arthrosc. Tech. 2021;10, 3: e659–67. 10.1016/j.eats.2020.10.079. [DOI] [PMC free article] [PubMed]
- 68.Lehmann CL, Arons RR, Loder RT, Vitale MG. The epidemiology of slipped capital femoral epiphysis: an update. J Pediatr Orthop. 2006;26(3):286–290. doi: 10.1097/01.bpo.0000217718.10728.70. [DOI] [PubMed] [Google Scholar]
- 69.Purcell D, Varthi A, Lee MC. Slipped capital femoral epiphysis: current concepts review. Current Orthopaedic Practice. 2011;22(1):81–89. doi: 10.1097/BCO.0b013e3181f49e80. [DOI] [Google Scholar]
- 70.Helgesson Lukas, Peter Kälebo Johansson, Ylva Aurell, Carl-Johan Tiderius, Johan Kärrholm, and Jacques Riad. “Early osteoarthritis after slipped capital femoral epiphysis.” Acta Orthopaedica 2018;89, 2: 222–28. 10.1080/17453674.2017.1407055. [DOI] [PMC free article] [PubMed]
- 71.Ziebarth K, Leunig M, Slongo T, Kim Y-J, Ganz R. Slipped capital femoral epiphysis: relevant pathophysiological findings with open surgery. Clin Orthop Relat Res. 2013;471(7):2156–2162. doi: 10.1007/s11999-013-2818-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Besomi Javier, Escobar Valeria, Alvarez Santiago, Valderrama Juanjose, Lopez Jaime, Mella Claudio, Lara Joaquin, Meneses Claudio. Hip arthroscopy following slipped capital femoral epiphysis fixation: chondral damage and labral tears findings. J Child Orthop. 2021;15(1):24–34. doi: 10.1302/1863-2548.15.200178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73•.Rahm Stefan, Lukas Jud, Anna Jungwirth-Weinberger, Timo Tondelli, Anna L Falkowski, Reto Sutter, and Patrick O Zingg. “Mid-term results after in situ pinning and hip arthroscopy for mild slipped capital femoral epiphysis: a minimum five-year follow-up.” J Child Orthop 2020;14, 6: 521–28. 10.1302/1863-2548.14.200068.This retrospective review of patients with SCFE who underwent in situ pinning and staged hip arthroscopy showed stable improvement in alpha angle at 5 year follow up and near normalized internal rotation. [DOI] [PMC free article] [PubMed]
- 74.Lieberman Elizabeth G, Pascual-Garrido Cecilia, Abu-Amer Wahid, Nepple Jeffrey J, Shoenecker Perry L, Clohisy John C. Patients with symptomatic sequelae of slipped capital femoral epiphysis have advanced cartilage wear at the time of surgical intervention. J. Pediatr. Orthop. 2021;41(6):e398. doi: 10.1097/BPO.0000000000001797. [DOI] [PubMed] [Google Scholar]
- 75.Soni JF, Valenza WR, Uliana CS. Surgical treatment of femoroacetabular impingement after slipped capital femoral epiphysis. Curr Opin Pediatr. 2018;30(1):93. doi: 10.1097/MOP.0000000000000565. [DOI] [PubMed] [Google Scholar]
- 76.Basheer SZ, Cooper AP, Maheshwari R, Balakumar B, and Madan S. “Arthroscopic Treatment of femoroacetabular impingement following slipped capital femoral epiphysis.” Bone Jt. J. 2016;98-B, 1 21–27. 10.1302/0301-620X.98B1.35831. [DOI] [PubMed]
- 77.Chen Austin, Ari Youderian, Summer Watkins, and Prasad Gourineni. “Arthroscopic femoral neck osteoplasty in slipped capital femoral epiphysis.” Arthroscopy: The Journal of Arthroscopic & Related Surgery: Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2014;30, 10: 1229–34. 10.1016/j.arthro.2014.05.024. [DOI] [PubMed]
- 78.Yen Y-M, Kocher MS. Clinical and radiographic diagnosis of femoroacetabular impingement. Journal of Pediatric Orthopaedics. 2013;33:S112. doi: 10.1097/BPO.0b013e318288b450. [DOI] [PubMed] [Google Scholar]
- 79.Samim M, Eftekhary N, Vigdorchik JM, Elbuluk A, Davidovitch R, Youm T, Gyftopoulos S. 3D-MRI versus 3D-CT in the evaluation of osseous anatomy in femoroacetabular impingement using Dixon 3D FLASH sequence. Skeletal Radiol. 2019;48(3):429–436. doi: 10.1007/s00256-018-3049-7. [DOI] [PubMed] [Google Scholar]
- 80.Byrd JW, Thomas. “Hip arthroscopy: the supine position.” Clin Sports Med 2001;20, 4: 703–32. 10.1016/S0278-5919(05)70280-5. [PubMed]
- 81.Eberhardt Oliver, Thomas Wirth, and Francisco F Fernandez. “Arthroscopic anatomy of the dislocated hip in infants and obstacles preventing reduction.” Arthrosc. - J. Arthrosc. Relat. Surg. 2015; 31, 6: 1052–59. 10.1016/j.arthro.2014.12.019. [DOI] [PubMed]
- 82•.Garg R, Ho J, Gourineni PV. Simplified arthroscopic lavage of pediatric septic hip: case series. Journal of Pediatric Orthopaedics B. 2020;29(3):304. 10.1097/BPB.0000000000000717. This retrospective study of patients with septic hip arthritis managed with arthroscopic lavage demonstrated effective treatment in a young age demographic, including patients under 1 year old. [DOI] [PubMed]
- 83.Colvin Alexis Chiang, John Harrast, and Christopher Harner. “Trends in hip arthroscopy.” J. Bone Jt. Surg. American 2012; 94, 4: e23 10.2106/JBJS.J.01886. [DOI] [PubMed]
- 84.DeAngelis Nicola A, and Brian D Busconi. “Hip arthroscopy in the pediatric population.” Clin. Orthop. Relat. Res. ® 2003;406, 1: 60. [DOI] [PubMed]
- 85.Gross RH. “Arthroscopy in hip disorders in children.” Arthroscopy in Hip Disorders in Children. 1977.
- 86.Bowen, J. Richard, V. Prem Kumar, John J. Iii Joyce, and J. Christopher Bowen. “Osteochondritis dissecans following Perthes’ disease arthroscopic-operative treatment.” Clin. Orthop. Relat. Res. ® 209 1986; 49. [PubMed]
- 87.Holgersson S, Brattström H, Mogensen B, Lidgren L. Arthroscopy of the hip in juvenile chronic arthritis. Journal of Pediatric Orthopaedics. 1981;1(3):273. doi: 10.1097/01241398-198111000-00006. [DOI] [PubMed] [Google Scholar]
- 88.Casartelli NC, NA, Maffiuletti PL, Valenzuela A Grassi, E Ferrari, MM A. van Buuren, M. C. Nevitt, M. Leunig, and R. Agricola. “Is hip morphology a risk factor for developing hip osteoarthritis? A systematic review with meta-analysis.” Osteoarthritis and Cartilage 2021;29, 9: 1252–64. 10.1016/j.joca.2021.06.007. [DOI] [PubMed]
- 89.Kraeutler, Matthew J., Sydney M. Fasulo, Iciar M. Dávila Castrodad, Omer Mei-Dan, and Anthony J. Scillia. (2023) “A prospective comparison of groin-related complications after hip arthroscopy with and without a perineal postAm J Sports Med. 51, 1 155–59. 10.1177/03635465221130768. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.