Abstract
Background.
Black Americans face significant discrimination associated with mental health disorder, which may be exacerbated among sexually victimized people. Social support may buffer that relationship.
Methods.
Cross-sectional data from a retrospective cohort study were analyzed to examine if discrimination and sexual victimization overlap to exacerbate symptoms of depression and post-traumatic stress disorder (PTSD) and to determine the extent to which social support moderated that association among Black women living in Baltimore, Maryland [138 non-abused (no physical/sexual victimization) and 98 abused (sexually victimized) since age 18].
Results.
Symptoms of depression and PTSD were independently associated with discrimination. Multilinear regression showed social support from friends moderated the association between discrimination and depressive symptoms among sexually abused participants only.
Conclusion.
Discrimination may exacerbate symptoms of depression and PTSD more for sexually victimized Black women, but sources of informal social support may attenuate adverse effects of discrimination on depressive symptoms among members of that group.
Keywords: Depression, post-traumatic stress disorder, discrimination, social support, sexual violence, victimization, Black women, women’s health, racism
Black Americans are the second largest racial group in the United States (U.S.), making up 14.5% of the population.1 Black Americans experience significant stigma (e.g., discrimination and victimization),2–4 contributing to symptoms of psychological distress.5,6 Discrimination refers to the act of treating a person differently because of their appearance, identities, or attributes. Perceived discrimination is a common measure of discrimination, and refers to one’s self-rated, day-to-day experiences of discrimination (e.g., treated as inferior, called names, presumed of wrongdoing because of their attributes), whereas victimization refers to acts of physical, sexual, or psychological violence perpetrated by one person on another.7,8 Kessler and colleagues’ seminal national survey (N=3,032) found that nearly half of Black participants reported at least one major act of discrimination in their lifetime (e.g., not hired for a job, harassed by police, denied a bank loan). Additionally, higher rates of sexual violence and intimate partner violence (IPV) are experienced by Black women compared with White and Latina women, suggesting racial disparities in stigma exposure.9,10 Exposure to stigma is an established determinant of mental health outcomes, especially for Black Americans in the U.S. Thus, it is imperative that possible protective factors be identified to reduce the harmful effects of stigma on psychological distress symptoms.
Guiding theoretical model.
We apply the Minority Stress Model to understand the association between stigma and mental health among Black women in the U.S. Based on the seminal work of Virginia Rae Brooks,6 Meyer’s Minority Stress Model is an expansion of the concept of psychological stress.5 Psychological stress is defined by Folkman and Lazarus as a state occurring when a person appraises the demands of their environment to exceed their available coping resources.11 Meyers defined minority stress as the excess stress experienced by individuals as a direct result of belonging to a stigmatized social group (whether defined by minority race, sexuality, income status).5 Distal stressors (rejection, racism, and victimization) and proximal stressors (individual perceptions and appraisals, anticipation of rejection, internalized negative feelings about one’s own minority group) can affect the mental health of people with minority identities.5,6 The Minority Stress Model was originally devised to explain stress-related health disparities among sexual minority men and is most commonly used among sexual and gender minority populations.12,13 However, this model may help examine the relationships between persistent social and economic inequity, as well as other structural discrimination that may negatively affect the health of Black Americans.14
The Minority Stress Model posits mechanisms through which discrimination can affect health and well-being, incorporating the concept of social stress, following the analyses in which inequitable social structures and conditions are also acknowledged as sources of stress.5,6 The impact of minority stress is evident in numerous studies linking perceived discrimination and/or victimization to health disparities.6,8,15–18 A longitudinal study of Black women found that perceived discrimination contributed to greater depressive symptomology and worse physical health compared with women with similar demographics with no perceived discrimination.18 In the seminal work by Brooks, economic contributions to minority stress were acknowledged, given that being part of a stigmatized group often results in restricted access to economic opportunities.6 This is an especially relevant consideration for Black U.S. women given the ongoing racial wage gap.19 One significant contribution of this study is the application of the Minority Stress Model to Black women, who are particularly vulnerable to minority stress. The chronic, cumulative nature of minority stress is associated with adverse physical and mental health outcomes including psychological distress, depression, anxiety, and substance use, which contributes to health disparities among minority groups.5,6,17
Compounding effects of stigma on the health of Black women.
Intersectionality, or having multiple minoritized identities (e.g., being a Black woman), likely increases experiences of discrimination and may amplify the negative effects of stigma on health.20,21 Studies suggest that sexism and genderism may compound the detrimental health effects of perceived discrimination and victimization.22 Additionally, several studies show Black women who experience stigma are more likely to experience depression, anxiety, and post-traumatic stress disorder (PTSD) than Black males who experience stigma.2,7,23
Traditional gender norms and inequities are drivers of violence against women.24 Exposure to sexual violence and IPV, considered distal minority stressors, are associated with health and mental health consequences.5,6 According to the National Intimate Partner and Sexual Violence Survey, women who experience physical and sexual violence are more likely to report physical symptoms of stress such as asthma, irritable bowel syndrome, and diabetes than women who did not experience violence.25 In addition to physical symptoms, nearly 30% of abused women experience long-lasting psychological distress due to violence.25 Evidence suggests Black women’s subjective reports of IPV are associated with higher levels of depressive and PTSD symptoms, which worsens with more frequent and severe IPV and stress from IPV.26 These experiences of victimization in addition to perceived discrimination have a greater impact on Black woman’s mental health7,27 and stress symptoms related to life traumas, life events, and chronic strain28 than solely race-based discrimination. However, there is a paucity of research examining the intersectional impact of perceived discrimination on the mental health of Black women who have experienced sexual violence.
Social support as a protective factor.
Social support, posited as a protective factor by the Minority Stress Model, can attenuate the deleterious effects of stigma on health.29,30 In general, mechanisms by which social support may buffer stress include informal support from friends and loved ones who may mobilize to support the distressed individual.31,32 High levels of social support have been found to minimize the effect of perceived racism on poor health, measured by systolic blood pressure.33 Social support reduced the effect of discrimination on health outcomes among low-income Black women who experienced moderate and very frequent discrimination.34 Additionally, several studies have found that social support mediated the relationship between victimization and psychological distress symptoms including symptoms of depression and PTSD.30,35,36 However, prolonged IPV can be associated with lower levels of perceived social support and greater psychological abuse, suggesting those offering social support (e.g., friends, family) are fatigued or otherwise unable to give support for extended periods of time.37
Purpose of the study.
Despite growing attention to the role of discrimination and sexual abuse in mental health among Black women, a paucity of studies examine how discrimination and abuse may overlap to exacerbate depressive and PTSD symptoms. To our knowledge, only one study has examined the combined effects of perceived discrimination and IPV on the mental health (specifically anxiety) of Black women;38 however, the study did not examine the mental health outcomes of depressive and PTSD symptoms or specifically examine sexual violence. We will address this gap in the literature by using the Minority Stress Model: (Aim 1) to determine the associations between sexual violence status, discrimination, social support, and mental health, and (Aim 2) to investigate whether social support moderates the association between discrimination and mental health. We hypothesize that discrimination will be positively associated with poor mental health, with worse outcomes among sexually abused participants, and that social support will moderate the association between discrimination and mental health.
Methods
The current study uses data collected in the ESSENCE Project (the parent study), a retrospective cohort study examining the impact of physiological and environmental factors on sexual violence and HIV risk among Black women living in Baltimore, Maryland, U.S. Data were collected between November 2015 and May 2018. The ethical review boards of Johns Hopkins University and the University of California, San Diego approved all study procedures.
Procedure.
Black women (N=312) were recruited from two public STD clinics in Baltimore City, Maryland by trained research staff. After providing informed consent, participants were screened for eligibility and surveyed using web-based audio computer-assisted self-interview (ACASI), which took approximately 60 to 90 minutes to complete. To be eligible, participants had to test HIV-negative at enrollment and self-report being: 1) female, 2) between ages 18–44 years, 3) Black or African American, 4) have had sex with a male in the past six months, and 5) have had two or more sexual partners in the past year or a high HIV risk sexual partner (i.e., used injection/non-injection drugs; been to prison; was HIV-positive; had sex with men, had a concurrent sex partner, or had an STI). Potential participants were compensated $10 for screening and, if eligible, $25 for completing the full survey.
Measures.
Abuse status.
By study design, two groups of women were recruited into the parent study, including: those who were: (1) unexposed to physical/sexual violence after age 18 (n=138 of 236) and (2) abused or exposed to forced sex by a male since age 18 by physical force (e.g., hit, held down, use of a weapon) or threats thereof (n=98 of 236; Table 1).
Table 1.
DEMOGRAPHIC CHARACTERISTICS OF BLACK WOMEN, BALTIMORE, MD, 2015–2018
| Full Sample (N=236) | Non-abused (N=138) | Abused (N=98) | ||
|---|---|---|---|---|
| Variables | n(%); M(SD) | n(%); M(SD) | n(%); M(SD) | Test Statistic |
| M(SD) | ||||
| Agea | 26.31(6.31) | 24.94(5.2) | 28.23(7.07) | 4.08*** |
| Raceb | .35 | |||
| Black or African American | 218(92.37) | 130(94.20) | 88(89.80) | |
| Black or African Born | 5(2.12) | 3(2.17) | 2(2.04) | |
| Black or African Caribbean | 6(2.54) | 2(1.45) | 4(4.08) | |
| Other mixed race to include Black | 7(2.97) | 3(2.17) | 4(4.08) | |
| Sexual Identityb | 9.63** | |||
| Heterosexual or straight | 201(85.17) | 125(90.58) | 76(77.55) | |
| Gay or lesbian | 1(0.42) | 1(0.72) | 0(0) | |
| Bisexual | 34(14.41) | 12(8.70) | 22(22.45) | |
| Employmentc | 21.24** | |||
| Employed | 142(60.17) | 92(66.67) | 50(51.02) | |
| Disabled | 12(5.08) | 3(2.17) | 9(9.18) | |
| Homemaker | 8(3.39) | 2(1.45) | 6(6.12) | |
| Seasonal/temp worker | 4(1.69) | 0(0) | 4(4.08) | |
| Student | 17(7.20) | 12(8.70) | 5(5.10) | |
| Unemployed | 52(22.03) | 28(20.29) | 24(24.49) | |
| Other | 1(0.42) | 1(0.72) | 0(0) | |
| Educationb | 15.41* | |||
| 8th grade or less | 7(2.97) | 0(0) | 7(7.14) | |
| 9th grade or more but did not complete high school or GED | 30(12.71) | 16(11.59) | 14(14.29) | |
| Completed high school or GED | 78(33.05) | 48(34.78) | 30(30.61) | |
| Some trade or vocational school, or college | 61(25.85) | 38(27.54) | 23(23.47) | |
| Completed trade school or vocational school | 21(8.90) | 10(7.25) | 11(11.22) | |
| Completed college (2-year or 4-year program) | 27(11.44) | 18(13.0) | 9(9.18) | |
| Graduate school | 12(5.08) | 8(5.80) | 4(4.08) | |
| Household Incomec | 8.20 | |||
| Less than $10,000 | 110(46.61) | 58(42.0) | 52(53.06) | |
| $10,000-$19,999 | 35(14.83) | 24(17.3) | 11(11.22) | |
| $20,000-$29,999 | 37(15.68) | 21(15.2) | 16(16.33) | |
| $30,000-$39,999 | 23(9.75) | 16(11.5) | 7(7.14) | |
| $40,000-$49,999 | 12(5.08) | 10(7.25) | 2(2.04) | |
| $50,000 or more | 19(8.05) | 9(6.52) | 10(10.20) | |
| Current Housingb | 8.55* | |||
| Homeless, live in a hotel/motel or transitional housing facility | 15(6.36) | 4(2.90) | 11(11.22) | |
| Live in a house, apartment, or condo | 209(88.56) | 129(93.4) | 80(81.63) | |
| Other | 12(5.08) | 5(3.62) | 7(7.14) |
Notes
independent t-test
Likelihood Ratio
χ2(Pearson’s Chi-square)
p< .05
p< .01
p< .001; 2-tailed
Perceived discrimination.
The Everyday Discrimination Scale (EDS) was used to assess past-year routine and less overt experiences of interpersonal discrimination (Table 2).39 The EDS was developed using qualitative interviews of Black women who described their experiences with everyday racism in the U.S. and the Netherlands.40,41 The EDS was designed to assess a range of day-to-day discriminatory treatment so commonplace as to appear trivial or normal,39 and consisted of nine items, such as You are treated with less courtesy than other people are and You receive poorer service than other people at restaurants or stores. Responses are on a six-point Likert-type scale, ranging from almost every day to never. Scores were summed and ranged from 1 to 54 with higher sores indicating higher levels of perceived discrimination (Cronbach’s alpha = .90). Anyone answering a few times a year or more to one or more items is asked a follow-up question, What do you think is the main reason for these experiences?, with response options such as one’s ancestry, gender, race, age, and religion.
Table 2.
PERCEIVED DISCRIMINATION, MENTAL HEALTH, AND SOCIAL SUPPORT SCORES BASED ON SEXUAL ABUSE HISTORY SINCE AGE 18
| Full Sample (N=236) | Non-abused (N=138) | Abused (N=98) | ||
|---|---|---|---|---|
| Variables | n(%); M(SD) | n(%); M(SD) | n(%); M(SD) | Test Statistic |
| Perceived Reason for Discrimination (N=146)a | ||||
| Race | 87(36.86) | 44(31.88) | 43(43.88) | 0.7 |
| Gender | 66(27.97) | 36(26.09) | 30(30.61) | 0.06 |
| Age | 52(22.03) | 27(19.57) | 25(25.51) | 0.07 |
| Skin Color | 49(20.76) | 24(17.39) | 25(25.51) | 0.59 |
| Physical Appearance | 47(19.92) | 22(15.94) | 25(25.51) | 1.22 |
| Height | 25(10.59) | 14(10.14) | 11(11.22) | 0.08 |
| Weight | 24(10.17) | 16(11.59) | 8(8.16) | 2.02 |
| Education Level | 20(8.47) | 7(5.07) | 13(13.27) | 3.16 |
| Ancestry | 18(7.63) | 6(4.35) | 12(12.24) | 3.33 |
| Sexual Orientation | 15(6.36) | 8(5.80) | 7(7.14) | 0 |
| Other | 15(6.36) | 6(4.35) | 9(9.18) | 1.21 |
| Religion | 13(5.51) | 7(5.07) | 6(6.12) | 0 |
| Physical Disability | 7(2.97) | 1(0.72) | 6(6.12) | 4.53 |
| Tribe | 1(0.42) | 0(0) | 1(1.02) | 1.16 |
| Perceived Discriminationb | 12.61(11.87) | 10.43(10.37) | 15.66(13.16) | −3.41** |
| Depressionb | 9.89(6.35) | 8.01(5.17) | 12.53(6.91) | −5.74*** |
| PTSDb | 1.63(1.14) | 1.22(.99) | 2.20(1.08) | −7.10*** |
| Comorbid Depression and PTSDa | 12(5.1) | 2(1.45) | 10(10.20) | 9.10** |
| Social Supportb | 2.76(.98) | 3.01(.84) | 2.41(1.06) | 4.82*** |
| Social Support from Friendsb | 2.81(1.12) | 3.10(.92) | 2.40(1.24) | 4.96*** |
| Social Support from Familyb | 25.58(1.22) | 2.81(1.13) | 2.26(1.28) | 3.43** |
| Social Support from Significant Other | 29.0(1.04) | 3.13(.87) | 2.59(1.18) | 4.04*** |
Notes
Fisher’s Exact Test
independent t-test
p< .05; 2-tailed
p< .01; 2-tailed
p< .001; 2-tailed
Depressive symptoms.
The Center for Epidemiologic Studies Depression Short Scale (CESD-10) is a 10-item, self-reported measure used to assess depressive feelings and behaviors over the last week.42 Items include feeling depressed and having restless sleep. Responses use a four-point Likert-type scale ranging from 0 = rarely or none of the time (less than 1 day) to 3 = all of the time (5–7 days). Two items were reverse-coded. Items were summed and scores range from 0 to 30 with higher scores indicating greater depressive symptoms (Cronbach’s alpha = .81). A score of 10 or more was considered depressed.
PTSD symptoms.
The National Stressful Events Survey PTSD Short Scale (NSESSS) was used to assess symptoms of traumatic stress over the past month.41,43 The NSESSS is a nine-item self-report tool assessing the severity of PTSD symptoms in the past month in adults following a traumatic event or experience. On a five-point Likert scale (0 = not at all to 4 = extremely), participants are asked to rank the degree to which they have been bothered by various symptoms such as feeling very emotionally upset when something reminded you of a stressful experience. The average of each sum score was used for analysis. Scores range from 0 to 4 with scores indicating severity of the individual’s PTSD this way: none (0), mild (1), moderate (2), severe (3), or extreme (4) (Cronbach’s alpha = .93). For participants who left one or two items unanswered, a prorated score was used. For participants who did not answer three or more items, scores were not included and were removed via listwise deletion.
Social support.
Multidimensional Scale of Perceived Social Support (MSPSS) was used to assess the perceived adequacy of social support in this study.44 The MSPSS consists of 12 items such as: There is a special person around when I am in need and My friends really try to help me. Response options are on a five-point Likert-type scale ranging from (0) strongly disagree to (4) strongly agree. All items were averaged to obtain a total score and were further divided into three subscales measuring the source of social support: (a) friends, (b) family, and (c) significant other. Higher scores correspond with greater perceived social support. Mean scores of the complete scale ranging from 1 to 2.9 are considered low support; scores of 3 to 5 are considered moderate support; and scores from 5.1 to 7 are considered high support (Cronbach’s alpha = .92 full scale; .93 friends subscale; .93 family subscale; .85 significant other subscale).45
Analyses.
All statistical analyses were conducted using SPSS, Version 25.46 First, variables of interest were examined for outliers and normality. Next, a Pearson’s correlation matrix was produced to identify statistically significant bivariate associations for inclusion in the main statistical model (Table 3). Age was controlled for in all MLR models. For Aim 1, multiple linear regression (MLR) models estimated the association between perceived discrimination and depressive and PTSD symptoms (separate models). For Aim 2, hierarchical forward entry MLR models included a mean-centered interaction term between perceived discrimination and social support (Model 1, Table 4) and interaction terms for each of the social support subscales (i.e., friends—Model 2, Table 4; family—Model 3, Table 4; significant other—Model 4, Table 4) were used to examine the moderating effect of social support. Abuse status was controlled for in models with the full sample and additional analyses were stratified by abuse status. Standardized and unstandardized regression coefficients were then compared, and significance testing was conducted at alpha level 0.05 (two-sided to account for unknown associations with demographic variables). Overall model fit was examined via the R2 (the coefficient of determination) and F-ratio/change in F-ratio at alpha level 0.05.
Table 3.
PEARSON’S CORRELATIONS OF VARIABLES OF INTEREST AND DESCRIPTIVE STATISTICS (N=236)
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | |||||||||||
| 2. Sexual Minority Identity | .03 | ||||||||||
| 3. Abused | .26*** | .18** | |||||||||
| 4. Perceived Discrimination | −.05 | .14* | .22** | ||||||||
| 5. Depression | −.003 | .15* | .35*** | 40*** | |||||||
| 6. PTSD | −.02 | .10 | .43*** | .45*** | .67*** | ||||||
| 7. Comorbid Depression/PTSD | .02 | .23*** | .20** | .31*** | .48*** | .42*** | |||||
| 8. Social Support (Full scale) | −.06 | −.02 | −.30*** | −.10 | −.19** | −.28*** | −0.11 | ||||
| 9. Social Support—Friends | −.06 | −.09 | −.31*** | −.08 | −.20** | −.28*** | −.16* | 90*** | |||
| 10. Social Support—Family | −.04 | .02 | −.22** | −.16* | −.22** | −.28*** | −.12 | .87*** | .67*** | ||
| 11. Social Support—Significant Other | −.04 | .01 | −.26*** | −.02 | −.06 | −.16* | .003 | .84*** | .67*** | .55*** | |
| Cronbach’s alphaa | — | — | — | .91 | .83 | .93^ | — | .94 | .94 | .94 | .89 |
Notes
the PTSD Cronbach’s alpha was run with only people who answered all items; N=229.
p<.05
p<.01
p<.001
PTSD= Post-Traumatic Stress Disorder
Table 4.
RESULTS OF HIERARCHICAL REGRESSION ANALYSES FOR SYMPTOMS OF DEPRESSION AND POST-TRAUMATIC STRESS DISORDERa
| Model 1—Social Support (Full Scale) | Model 2—Social Support from Friends | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Independent Variables | Depressive Symptoms | PTSD Symptoms | Depressive Symptoms | PTSD Symptoms | |||||||||||
| Sample | Full Sample | Non- Abused | Abused | Full Sample | Non- Abused | Abused | Full Sample | Non- abused | Abused | Full Sample | Non- abused | Abused | |||
| Step 1: Demographics | |||||||||||||||
| Age | −.06 | 0 | −.13 | −.1 | −.05 | −.14 | −.06 | 0 | −.14 | −.1 | −.06 | −.15 | |||
| Sexual Identity | .06 | .06 | .03 | −.01 | .03 | −.1 | .06 | .06 | .04 | −.02 | .04 | −.12 | |||
| Abuse Status | .26*** | .33*** | .26*** | .33*** | |||||||||||
| R2 | .14 | 0 | .05 | .2 | .01 | .05 | .14 | 0 | .05 | .2 | .01 | .05 | |||
| F | 12.66*** | .09 | 2.45 | 19.50*** | .52 | 2.47 | 12.66*** | .09 | 2.45 | 19.50*** | .52 | 2.47 | |||
| Step 2: Main Predictor | |||||||||||||||
| Discrimination | .33*** | .22* | .50*** | 37*** | .28** | .58*** | .33*** | .24** | .51*** | 37*** | .28** | .59*** | |||
| R2 | .24 | .06 | .21 | .33 | .09 | .3 | .24 | .06 | .21 | .33 | .09 | .3 | |||
| ΔR2 | .1 | .06 | .16 | .13 | .08 | .25 | .1 | .06 | .16 | .13 | .08 | .25 | |||
| ΔF | 29.41*** | 8.76** | 19.03*** | 42.72*** | 12.33** | 33.69*** | 29.41*** | 8.76** | 19.03*** | 42.72*** | 12.33** | 33.69*** | |||
| Step 3: Protective Factors | |||||||||||||||
| Social Support (full scale) | −.08 | −.14 | −.01 | −.14* | −.04 | −.28** | |||||||||
| Social support (subscales) | |||||||||||||||
| Friends | −.09 | −.16 | −.02 | −.15** | −.1 | −.24** | |||||||||
| R2 | .24 | .08 | .21 | .35 | .09 | .39 | .25 | .09 | .21 | .35 | .1 | .36 | |||
| ΔR2 | .01 | .02 | 0 | .02 | 0 | .09 | .01 | .03 | 0 | .02 | .01 | .06 | |||
| ΔF | 1.74 | 2.54 | .28 | 6.97** | .22 | 13.56*** | 2.35 | 3.72 | .27 | 7.51** | 1.32 | 9.20** | |||
| Step 4: Moderator | |||||||||||||||
| Social support (subscales) | |||||||||||||||
| Discrimination * Friends | .22* | ||||||||||||||
| R2 | .25 | ||||||||||||||
| ΔR2 | .04 | ||||||||||||||
| ΔF | 4.63* | ||||||||||||||
| Model 3—Social Support from Family | Model 4—Social Support from Significant Other | ||||||||||||||
| Independent Variables | Depressive Symptoms | PTSD Symptoms | Depressive Symptoms | PTSD Symptoms | |||||||||||
| Sample | Full Sample | Non− Abused | Abused | Full Sample | Non− Abused | Abused | Full Sample | Nonabused | Abused | Full Sample | Nonabused | Abused | |||
| Step 1: Demographic Variables | |||||||||||||||
| Age | −.06 | .01 | −.12 | −.1 | −.05 | −.14 | −.06 | .01 | −.13 | −.1 | −.05 | −.14 | |||
| Sexual Identity | .07 | .06 | .04 | 0 | .03 | −.08 | .06 | .05 | .03 | −.01 | .02 | −.09 | |||
| Abuse Status | .26*** | .34*** | 29*** | .35*** | |||||||||||
| R2 | .14 | 0 | .05 | .2 | .01 | .05 | .14 | 0 | .05 | .2 | .01 | .05 | |||
| F | 12.66*** | .09 | 2.45 | 19.50*** | .52 | 2.47 | 12.66*** | .09 | 2.45 | 19.50*** | .52 | 2.47 | |||
| Step 2: Main Predictor | |||||||||||||||
| Discrimination | .31*** | .21* | .44*** | .36*** | .29** | .55*** | .33*** | .24** | .48*** | .38*** | .29** | .62*** | |||
| R2 | .24 | .06 | .21 | .33 | .09 | .3 | .24 | .06 | .21 | .33 | .09 | .3 | |||
| ΔR2 | .1 | .06 | .16 | .13 | .08 | .25 | .1 | .06 | .16 | .13 | .08 | .25 | |||
| ΔF | 29.41*** | 8.76** | 19.03*** | 42.72*** | 12.33** | 33.69*** | 29.41*** | 8.76** | 19.03*** | 42.72*** | 12.33** | 33.69*** | |||
| Step 3: Protective Factors | |||||||||||||||
| Social support (subscales) | |||||||||||||||
| Family | −.12 | −.15 | −.12 | −.15** | −.03 | −.35*** | |||||||||
| Significant Other | .02 | −.03 | .07 | −.06 | .01 | −.15 | |||||||||
| R2 | .25 | .08 | .22 | .35 | .09 | .42 | .24 | .06 | .21 | .33 | .09 | .33 | |||
| ΔR2 | .01 | .02 | .01 | .02 | 0 | .12 | 0 | 0 | 0 | 0 | 0 | .03 | |||
| ΔF | 3.8 | 2.76 | 1.68 | 7.64** | .04 | 19.71*** | .05 | .15 | .25 | 1.45 | .02 | 3.79 | |||
Notes
Full sample N=236; Non- abused participants N=138; Abused participants only N=98; All standardized regression coefficients are from the final step in the analyses.
p< .05
p< .01
p< .001(2-tailed)
Power analysis.
A post hoc sensitivity analysis revealed that given the smaller sample of 98 participants who were stratified by abuse status (full sample N = 236, abused = 98, non-abused = 138) could detect effect sizes as small as f2 = 0.15 with power set at 80%, an alpha level of 0.05, and six predictors, which is considered a medium effect size.47–49
Results
Participants.
Our analytic sample size was 236 after excluding 69 participants who lacked complete data. All participants identified as female gender and reported their race as either Black or African American (92%), Black or African Born (2%), Black or African Caribbean (3%), or other mixed race including Black (3%) (Table 1). Few identified as Hispanic/Latinx (< 2%), born outside of the U.S. (< 2%), or as gay/lesbian or bisexual (15%). Nearly half of the sample reported a household income of less than $10,000 a year (47%), most were employed (> 60%), had a high school education or more (> 50%), and reported living in a house, apartment, or condominium (89%).
Aim 1. Determine the associations between sexual abuse status, discrimination, social support, and symptoms of (a) depression and (b) PTSD.
Discrimination.
Overall, 83% of participants reported experiencing some perceived discrimination (mean [M] = 12.61, standard deviation [SD] = 11.87). Perceived discrimination scores were significantly higher among abused participants (M = 15.66, SD = 13.16) compared with non-abused participants (M = 10.43, SD = 10.37); t(234) = −3.41, mean difference [Mdiff] = 5.23, standard error of difference[SEdiff] = 1.53, p < .01). Only 146 of the 236 participants reported the reason they believed they were discriminated against. The most common reasons for perceived discrimination were race (37%), gender (28%), age (22%), skin color (21%), and physical appearance (20%); no statistical differences were noted by abuse status (Table 2).
Social support.
Overall, the average score for social support was 2.76 (SD = .98), indicating a low level of support. Social support scores were significantly lower among abused participants (M = 2.41, SD = 1.06) compared with non-abused participants (M = 3.01, SD = .84, t(234) = 4.82, Mdiff = .60, SEdiff = .12, p < .001). By subscale, abused women reported significantly less social support from friends, family, and significant others compared with non-abused women (see Table 2).
Depressive symptoms.
The average score for symptoms of depression was 9.89 (SD = 6.35; range = 0–29) indicating low to moderate levels of depressive symptoms, just below the threshold of depression diagnosis (a score ≥10 was considered depressed). Severity of depression symptoms was significantly higher among abused participants (Median (Mn) = 12, inter quartile range (IQR) = 11.5; M(SD) = 12.53(6.91)) than non-abused participants (Mn = 7, IQR = 7; M(SD) = 8.01(5.17), t(234) = −5.74; Mdiff = 4.52, SEdiff = .79, p<.001).
Perceived discrimination scores were significantly positively associated with depressive symptoms, accounting for abuse status, sexual minority status, and age; a regression model that explained 24% of the variance in depressive symptoms reported (F(4, 231) = 18.01, p < .001). A one unit increase in perceived discrimination was associated with a .33 increase in symptoms of depression (p < .001) (Table 4). Stratified analysis by abuse group revealed that the full model explained more of the variance in depressive symptoms among abused women (21% of the variance; F(3, 94) = 8.28, p < 001) than non-abused women (6% of the variance; F(3, 134) = 2.98, p < .05). Similarly, among abused women, a one-unit increase in perceived discrimination was associated with a small to moderate increase in depressive symptoms (standardized beta [β] = .50, p < .001), whereas among non-abused women it was associated with only a small increase in depressive symptoms (β = .22 p < .05) (Table 4)
PTSD symptoms.
The average score for symptoms of PTSD was 1.63 (SD = 1.14; range = 0–4) indicating a low to moderate severity of symptoms. Severity of PTSD symptoms was statistically significantly higher among abused participants (M(SD) = 2.20(1.08)) compared with non-abused participants (M(SD) = 1.22(.99), t(197.18) = −7.10, Mdiff(SE) = −.98(.14), p < .001).
Perceived discrimination scores were significantly positively associated with increased severe/extreme PTSD symptoms, accounting for abuse status, sexual minority status, and age. The regression model including perceived discrimination, abuse status, sexual minority status, and age, explained 33% of the variance in PTSD symptoms reported (F(4, 231) = 27.94, p < .001). A one-unit increase in perceived discrimination was associated with increased symptoms of PTSD (β = .37, p < .001) (Table 4).
Stratified analysis by abuse group revealed that the full model explained more of the variance in PTSD symptoms among abused women (30% of the variance; (F(3, 94) = 13.44, p < .001) than non-abused women (9% of the variance; (F(3, 135) = 4.49, p < .01). Similarly, among abused women, a one-unit increase in perceived discrimination was associated with increased PTSD symptoms (β = .58, p < .001), whereas among non-abused women it was associated with a smaller increase in PTSD symptoms (β = .28, p < .01) (Table 4)
Aim 2. Investigate whether social support moderates the association between perceived discrimination and symptoms of (a) depression and (b) PTSD.
Depressive symptoms.
Statistical modeling yielded in a non-significant interaction between perceived discrimination scores and social support (and the three social support subscales [friends, family, and significant other]). Social support did not significantly moderate the association between perceived discrimination and depressive symptoms among the full sample (Table 4). However, stratified analysis by abuse status revealed there was a statistically significant interaction between perceived discrimination score and social support from friends among abused participants only—suggesting the association between perceived discrimination scores and symptoms of depression among abused participants depends on the amount of social support one receives from friends. Specifically, Figure 1 shows that people with high social support from friends (scores above 3) demonstrated the greatest moderating effect on the association between perceived discrimination and symptoms of depression. The regression model including perceived discrimination, social support from friends, an interaction between perceived discrimination and social support from friends, sexual minority status, and age, explained 25% of the variance in depression symptoms reported among abused participants (F(5, 92) = 6.11, p < .001). Among abused participants, a one unit increase in perceived discrimination and a one unit increase in social support from friends was associated with a very small increase in symptoms of depression (β = .22, p < .05) (Table 4).
Figure 1.
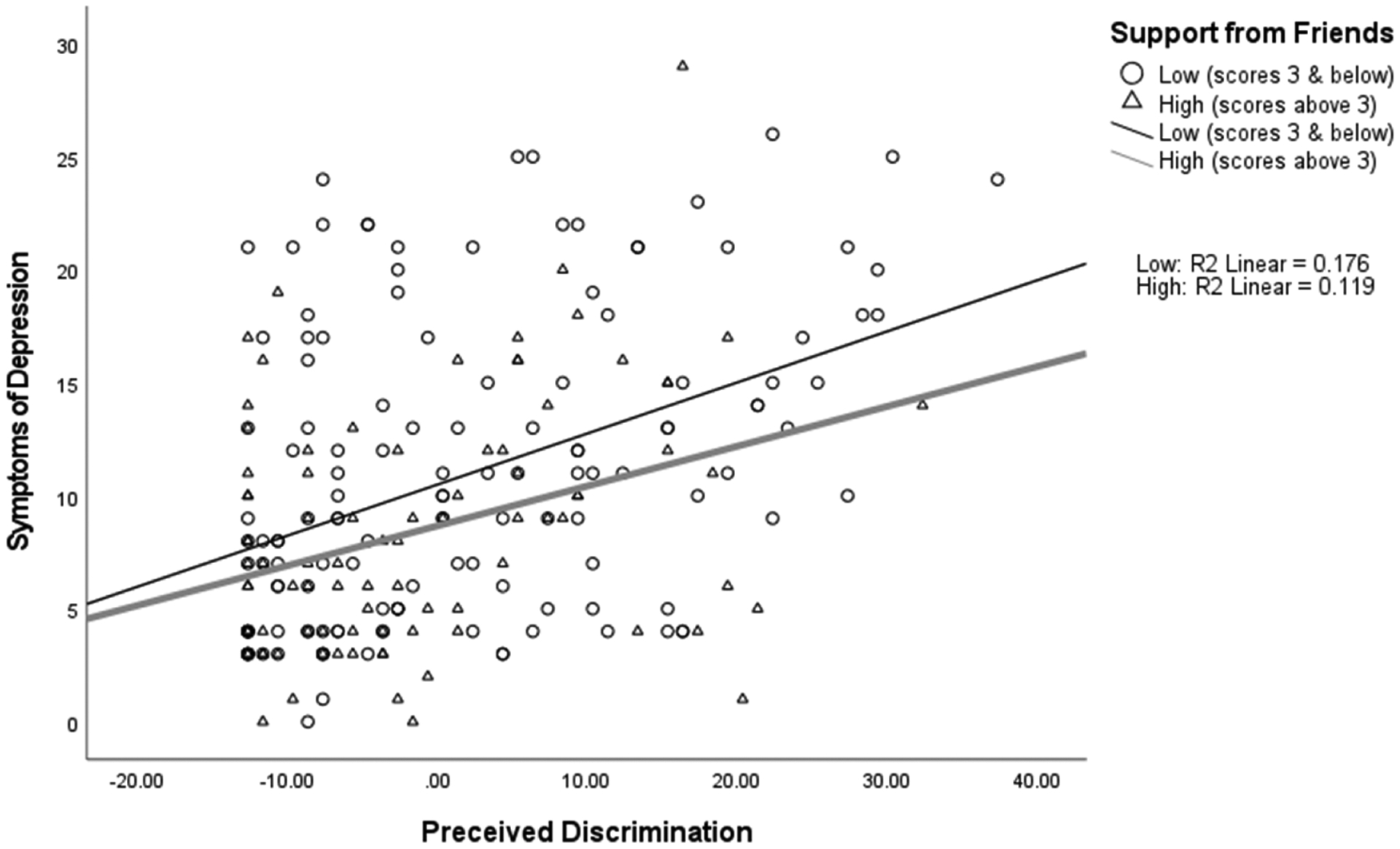
NEED Caption
PTSD symptoms.
Statistical modeling of the interaction between perceived discrimination scores and (a) social support (full scale) and (b) the three social support subscales (friends, family, and significant other) revealed social support did not moderate the association between perceived discrimination and symptoms of PTSD among the full sample or the stratified analysis based on abuse group (Table 4). This suggests the association between perceived discrimination scores and symptoms of PTSD among participants does not vary in effect by the amount of social support one receives.
Discussion
This study examined if discrimination and sexual violence overlap to exacerbate symptoms of depression and PTSD, and to what extent social support attenuated the association, among Black women living in Baltimore, Maryland. We found that perceived discrimination was independently associated with symptoms of depression and PTSD, accounting for abuse status, sexual minority status, and age. Our findings support the association between discrimination and adverse mental health as discussed in the Minority Stress Model.5 We hypothesized that that discrimination would be positively associated with poor mental health, with worse outcomes among sexually abused participants, and that social support would moderate the association between discrimination and mental health. As expected, depressive symptoms and PTSD symptoms were more pronounced in abused women than non-abused women. We found abused women experienced significantly more severe discrimination (Mdiff = 5.23), depressive symptoms (Mdiff = 4.52), PTSD symptoms (Mdiff = 1.22), and lower levels of social support (Mdiff = −.60) when compared to non-abused participants, which is consistent with other research.37,50 Only the abused sample met the cutoff for depression and PTSD, which is unsurprising since 30% of IPV survivors experience long-lasting depression and PTSD.25
Another key finding from our multivariate analyses showed that social support from friends moderated the association between discrimination and depressive symptoms only for abused participants. This finding suggests the association between perceived discrimination and symptoms of depression among abused participants varies in strength and magnitude based on the amount of social support one reports receiving from friends. A number of studies have demonstrated that social support from family, friends, and peers moderates depressive symptoms for Black Americans.51–53 Other research finds similar moderating effects of social support for abused women.50,54–56 No other moderation by social support (i.e., significant other and family member) was noted in our analyses. We can only speculate as to why social support from significant other or family members did not moderate the association between discrimination and depressive symptoms for abused women. Although, it is not surprising that social support from a significant other for abused women did not moderate the association as the significant other may be the source of abuse, although our survey did not ask this specifically. However, another study found that abused women receive little social support from their partners.57 In terms of social support from family members, potential explanations could be an abusive partner’s tactic of isolating women from family members,58 victims’ reluctance to disclose abuse,59 cultural norms,60 or negative interactions with family members.61 In addition to informal social supports, future research should examine religious coping,62 and formal social support (i.e., police, shelter, health care or other service providers), as abused women seek out different types of support as their needs change.63
Our findings must be contextualized within Baltimore’s history with racism and recent events of anti-racist protests. Data collection for this study occurred in neighborhoods fraught with historic redlining that resulted in segregation and community disinvestment that perpetuates systemic bias and inequality.64 This history of racism has contributed to the over-policing of Black neighborhoods, mass incarceration of Black men, destabilization of Black families, and pockets of intense poverty and high crime in Baltimore. This context often leads to Black women being the head of household, having diminished access to family support, and having decreased health and increased mortality.65 It is also important to note data collection began soon after the death of Freddie Gray (April 19, 2015), a 25-year-old Black man killed in police custody in Baltimore. There were mass protests against police brutality (April 27, 2015) following his death and throughout the criminal proceedings against the six officers, which ended in the charges being dropped (July 27, 2016). In addition, participant recruitment occurred in neighborhoods where the protests were most intense.66 Our cross-sectional study design cannot determine to what extent adverse mental health effects were due to these recent and consistent acts of racism or historical trauma from long-standing racism in the U.S. (including through such varied signal periods as slavery, Jim Crow, the War on Drugs). However, parsing out current and past experiences of discrimination may be inappropriate and/or impossible as racial discrimination in the U.S. is pervasive, life long, and intergenerational.67
Limitations.
One limitation of this study is the cross-sectional study design, which cannot order discrimination and mental health symptoms temporally or isolate the effects of gender-based violence and discrimination. Future studies may consider a longitudinal cohort design to capture the health effects of experienced discrimination and victimization over time. Another limitation is the study’s sample represents low-income, urban-dwelling Black women at high risk for HIV and is not generalizable to all Black women living in the U.S. Finally, the EDS is a widely used but unidimensional measure of discrimination first validated in the 1990s, and it may not allow for identification of nuances in experienced discrimination and complex discrimination related to multiple stigmatized identities or social positions. Future studies examining discrimination among Black women should consider measures such as the Giscombe Superwoman Schema Questionnaire, a 35-item measure with five subscales (α = .70 to .87), created to help quantify the lived experiences of Black women in consideration of their gendered and racialized stress and discrimination.68,69 Incorporating this measure, or similar comprehensive measures, in research could enhance our understanding of the effects of discrimination on the mental health of Black women.
Recommendations.
Our findings highlight the need for health and mental health care providers to consider the roles perceived discrimination and structural racism play in the lives of Black Americans, in particular Black women, and take steps to actively change it. Structural racism refers to macro-level racism that is embedded in culture, ideologies, and institutions, and—specifically—the medical system.70 First, providers must recognize that institutionalized racist practices—housing and workplace discrimination, over-policing of people of color, segregation of health care access, and other instances of economic and political exploitation—are determinants of health directly contributing to racial health disparities.71,72 Then, health providers should identify discriminatory beliefs that may influence their own thoughts and behaviors. For example, a 2016 study of medical students and residents found 50% of White participants (N = 418) held false beliefs that Black people feel pain differently, have thicker skin, are more fertile, and have other biological differences compared with White people.73 Adherence to false beliefs and other implicit biases can affect how medical professionals treat minority patients.74 Finally, health professionals can take active steps to provide equitable care by centering at the margins, which means redefining normal care and shifting to the perspectives and needs of marginalized groups.72[p.2114]
To be more responsive, health and mental health care providers can practice person-centered trauma informed care, which emphasizes “knowing the person behind the patient—as a human being with reason, feelings and needs,”75[p.249] assessing and modifying health care provision to address how trauma exposure may affect health and health care engagement, and treating the patient-provider relationship as a partnership.75,76 Inquiring about experiences of discrimination and violence and attempting to understand whether, and how, they are related to a patient’s health concerns supports a person-centered trauma informed care approach.76 Principles of patient-centered trauma-informed care include (a) gathering a patient’s narrative of the illness and trauma history and its perceived impact on life, (b) shared decision-making regarding care best suited to a patient’s lifestyle, and (c) documenting the patient’s beliefs and values.75 Other changes can be made to address health disparities such as increasing the number of minorities in health professions, developing linguistically and culturally-appropriate health and educational materials, and increasing provider education on cultural issues including discrimination and structural racism.77
One of our main findings was the moderating effect of social support from friends, therefore, we recommend mental health and community-based interventions that can activate and promote social support. For example, support groups conducted by mental health providers can address racism and abuse history. Ideally, these groups should be among racially concordant persons (i.e., shared racial identity). One systematic review of race-concordance reported health communication improved among racially-matched Black patients and providers78 and Black youth found that interaction with same race and gender peers helped to validate the culmination of their experiences at the intersection of their race and gender.79 It should also be noted that historically Black communities have been victimized and discriminated against by health care professionals contributing to delayed treatment seeking and medical distrust among the Black community.80–83 Thus, community listening spaces, designed and facilitated by community members, may be an appropriate intervention to activate and promote social support among Black women with exposure to discrimination and violence.84
Conclusion.
Racial and gender discrimination are persistent sources of minority stress among Black women in Baltimore City, Maryland. Perceived discrimination and sexual abuse are interpersonal sources of trauma linked to depression and PTSD. Social support from friends can attenuate the negative effect of perceived discrimination and sexual abuse on symptoms of depression among Black women with histories of sexual abuse.
Acknowledgments
We thank the study participants who generously provided the data for this research. We also thank the Baltimore City Health Department for their support on this project. This research was supported by the Eunice Kennedy Shriver National Institute on Child Health and Human Development (NICHD Grant #R01HD077891). J. K. Stockman and K. Tsuyuki acknowledge support by the San Diego Center for AIDS Research (Grant #P30AI036214). A.D.F. Sherman acknowledges support by National Institute Of Nursing Research of the National Institutes of Health (Grant #K23NR020208). A.N. Cimino and J.C. Campbell acknowledge support by the Johns Hopkins Center for AIDS Research (Grant #P30AI094189). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Contributor Information
Athena D. F. Sherman, Nell Hodgson Woodruff School of Nursing, Emory University..
Andrea N. Cimino, School of Nursing, Johns Hopkins University..
Monique Balthazar, Nell Hodgson Woodruff School of Nursing, Emory University.; Byrdine F. Lewis College of Nursing and Health Professions, Georgia State University.
Kalisha Bonds Johnson, Nell Hodgson Woodruff School of Nursing, Emory University..
Desirée D. Burns, College of Social Work, Florida State University..
Angie Denisse Otiniano Verissimo, Department of Health Science and Human Ecology, California State University, San Bernardino..
Jacquelyn C. Campbell, School of Nursing, Johns Hopkins University..
Kiyomi Tsuyuki, Division of Infectious Diseases and Global Public Health, School of Medicine, University of California, San Diego..
Jamila K. Stockman, Division of Infectious Diseases and Global Public Health, School of Medicine, University of California, San Diego..
References
- 1.United States Census Bureau. American Community Survey: ACS demographic and housing estimates. Washington, DC: United States Census Bureau, 2016. Available at: https://data.census.gov/cedsci/table?d=ACS 5-Year Estimates Data Profiles&tid =ACSDP5Y2016.DP05. [Google Scholar]
- 2.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40(3):208–30. 10.2307/2676349 [DOI] [PubMed] [Google Scholar]
- 3.Kim G, Sellbom M, Ford KL. Race/ethnicity and measurement equivalence of the Everyday Discrimination Scale. Psychol Assess. 2014;26(3):892–900. 10.1037/a0036431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reeve BB, Willis G, Shariff-Marco SN, et al. Comparing cognitive interviewing and psychometric methods to evaluate a racial/ethnic discrimination scale. Field methods. 2011. Nov;23(4):397–419. Epub 2011 Aug 25. 10.1177/1525822X11416564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003. Sep;129(5): 674–97. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brooks V Minority stress and lesbian women. Lexington, MA: Lexington Books, 1981:84. [Google Scholar]
- 7.Fischer AR, Shaw CM. African Americans’ mental health and perceptions of racist discrimination: the moderating effects of racial socialization experiences and self-esteem. J Couns Psychol. 1999;46(3):395–407. 10.1037/0022-0167.46.3.395 [DOI] [Google Scholar]
- 8.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. 10.1007/s10865-008-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.West CM. Black women and intimate partner violence: new directions for research. J Interpers Violence. 2004;19(12):1487–93. 10.1177/0886260504269700 [DOI] [PubMed] [Google Scholar]
- 10.Catalano S, Smith E, Snyder H, et al. Female victims of violence. Washington, DC: U.S. Department of Justice, 2009. Available at: https://bjs.ojp.gov/content/pub/pdf/fvv.pdf. 10.1037/e525992010-001 [DOI] [Google Scholar]
- 11.Folkman S, Lazarus RS, Dunkel-Schetter C, et al. Dynamics of a stressful encounter. Cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol. 1986;50(5): 992–1003. 10.1037/0022-3514.50.5.992 [DOI] [PubMed] [Google Scholar]
- 12.Cox N, Dewaele A, van Houtte M, et al. Stress-related growth, coming out, and internalized homonegativity in lesbian, gay, and bisexual youth. An examination of stress-related growth within the minority stress model. J Homosex. 2010;58(1):117–37. 10.1080/00918369.2011.533631 [DOI] [PubMed] [Google Scholar]
- 13.Plöderl M, Sellmeier M, Fartacek C, et al. Explaining the suicide risk of sexual minority individuals by contrasting the minority stress model with suicide models. Arch Sex Behav. 2014. Nov;43(8):1559–70. Epub 2014 Feb 27. 10.1007/s10508-014-0268-4 [DOI] [PubMed] [Google Scholar]
- 14.Nelson A Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002. Aug;94(8):666–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):1–48. 10.1371/journal.pone.0138511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seng JS, Lopez WD, Sperlich M, et al. Marginalized identities, discrimination burden, and mental health: Empirical exploration of an interpersonal-level approach to modeling intersectionality. Soc Sci Med. 2012;75(12):2437–45. 10.1016/j.socscimed.2012.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93(2):200–8. 10.2105/AJPH.93.2.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schulz AJ, Gravlee CC, Williams DR, et al. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. Am J Public Health. 2006;96(7):1265–70. 10.2105/AJPH.2005.064543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blau FD, Kahn LM. The gender wage gap: extent, trends, & explanations. J Econ Lit. 2017;55(3):789–865. 10.1257/jel.20160995 [DOI] [Google Scholar]
- 20.Crenshaw K Demarginalizing the intersection of race and sex: a Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chic Leg Forum. 1989:139–68. [Google Scholar]
- 21.Bowleg L, Huang J, Brooks K, et al. Triple jeopardy and beyond: multiple minority stress and resilience among Black lesbians. J Lesbian Stud. 2003;7(4):87–108. 10.1300/J155v07n04_06 [DOI] [PubMed] [Google Scholar]
- 22.Moradi B, Subich LM. Examining the moderating role of self-esteem in the link between experiences of perceived sexist events and psychological distress. J Couns Psychol. 2004;51(1):50–6. 10.1037/0022-0167.51.1.50 [DOI] [Google Scholar]
- 23.Kearns MC, D’Inverno AS, Reidy DE. The association between gender inequality and sexual violence in the U.S. Am J Prev Med. 2020;58(1):12–20. 10.1016/j.amepre.2019.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Black MC, Basile KC, Breiding MJ, et al. National Intimate Partner and Sexual Violence Survey: 2010 summary report. Atlanta, GA: CDC, National Center for Injury Prevention and Control, 2011;1–8. Available at: https://www.cdc.gov/violenceprevention/pdf/nisvs_executive_summary-a.pdf. [Google Scholar]
- 25.Martinez-Torteya C, Bogat GA, Von Eye A, et al. Women’s appraisals of intimate partner violence stressfulness and their relationship to depressive and posttraumatic stress disorder symptoms. Violence Vict. 2009;24(6):707–22. 10.1891/0886-6708.24.6.707 [DOI] [PubMed] [Google Scholar]
- 26.Williams CC, Curling D, Steele LS, et al. Depression and discrimination in the lives of women, transgender and gender liminal people in Ontario, Canada. Heal Soc Care Community. 2017;25(3):1139–50. 10.1111/hsc.12414 [DOI] [PubMed] [Google Scholar]
- 27.Taylor J, Truner RJ. Perceived discrimination, social stress, and depression in the transition to adulthood: racial contrasts. Soc Psychol Q. 2002;65(3):213–25. 10.2307/3090120 [DOI] [Google Scholar]
- 28.Prelow HM, Mosher CE, Bowman MA. Perceived racial discrimination, social support, and psychological adjustment among African American college students. J Black Psychol. 2006;32(4):442–54. 10.1177/0095798406292677 [DOI] [Google Scholar]
- 29.Catabay CJ, Stockman JK, Campbell JC, et al. Perceived stress and mental health: the mediating roles of social support and resilience among Black women exposed to sexual violence. J Affect Disord. 2019;259:143–9. Epub 2019 Aug 19. 10.1016/j.jad.2019.08.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barrera MJ. Models of social support and life stress: beyond the buffering hypothesis. In: Cohen LH L(ed.). Life events and psychological functioning: theoretical and methodological issues. Newbury Park, CA: SAGE, 1988:211–36. [Google Scholar]
- 31.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57. 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- 32.Clark R Perceived racism and vascular reactivity in Black college women: moderating effects of seeking social support. Heal Psychol. 2006;25(1):20–5. 10.1037/0278-6133.25.1.20 [DOI] [PubMed] [Google Scholar]
- 33.Ajrouch KJ, Reisine S, Lim S, et al. Perceived everyday discrimination and psychological distress: does social support matter? Ethn Heal. 2010;15(4):417–34. 10.1080/13557858.2010.484050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mitchell MD, Hargrove GL, Collins MH, et al. Coping variables that mediate the relation between intimate partner violence and mental health outcomes among low-income, African American women. J Clin Psychol. 2006;62(12):1503–20. 10.1002/jclp.20305 [DOI] [PubMed] [Google Scholar]
- 35.Fowler DN, Hill HM. Social support and spirituality as culturally relevant factors in coping among African American women survivors of partner abuse. Violence Against Women. 2004;10(11):1267–82. 10.1177/1077801204269001 [DOI] [Google Scholar]
- 36.Thompson MP, Kaslow NJ, Kingree JB, et al. Partner violence, social support, and distress among inner-city African American women. Am J Community Psychol. 2000;28(1):127–43. 10.1023/A:1005198514704 [DOI] [PubMed] [Google Scholar]
- 37.Waltermaurer E, Watson C-A, McNutt L-A. Black women’s health: the effect of perceived racism and intimate partner violence. Violence Against Women. 2006;12(12): 1214–22. 10.1177/1077801206293545 [DOI] [PubMed] [Google Scholar]
- 38.Forman TA, Williams DR, Jackson JS. Race, place, and discrimination. Soc Probl. 1997;9:231–61. [Google Scholar]
- 39.Essed P. Knowledge and resistance: Black women talk about racism in the Netherlands and the USA. Fem Psychol. 1991;1(2):201–19. 10.1177/0959353591012003 [DOI] [Google Scholar]
- 40.Essed P Understanding everyday racism: an interdisciplinary theory and analysis of the experiences of Black women. Amsterdam, Netherlands: University of Amsterdam, 1990. 10.4135/9781483345239 [DOI] [Google Scholar]
- 41.Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well older adults: evaluation if a short form of the CES-D. Am J Prev Med. 1994;10(2):77–84. 10.1016/S0749-3797(18)30622-6 [DOI] [PubMed] [Google Scholar]
- 42.LeBeau R, Mischel E, Resnick H, et al. Dimensional assessment of posttraumatic stress disorder in DSM-5. Psychiatry Res. 2014;218(1–2):143–7. 10.1016/j.psychres.2014.03.032 [DOI] [PubMed] [Google Scholar]
- 43.Zimet GD, Dahlem NW, Zimet SG, et al. The Multidimensional Scale of Perceived Social Support (MSPSS). J Pers Assess. 1988;52(1):30–41. 10.1207/s15327752jpa5201_2 [DOI] [Google Scholar]
- 44.Zimet GD. Multidimensional Scale of Perceived Social Support (MSPSS)—scale items and scoring information. 2016. Available at: https://www.researchgate.net/publication/311534896_Multidimensional_Scale_of_Perceived_Social_Support_MSPSS_-_Scale_Items_and_Scoring_Information.
- 45.IBM Corp. IBM SPSS statistics for windows, (version 25). Armonk, NY: IBM Corp., 2017. [Google Scholar]
- 46.Ferguson CJ. An effect size primer : a guide for clinicians and researchers. Prof Psychol Res Pr. 2009;40(5):532–8. 10.1037/a0015808 [DOI] [Google Scholar]
- 47.Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2–18. 10.1037/a0024338 [DOI] [PubMed] [Google Scholar]
- 48.Cohen J Using effect size—or why the p-value is not enough. J Gr Med Educ. 2012; 4:279–82. 10.4300/JGME-D-12-00156.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barnett OW, Martinez TE, Keyson M. The relationship between violence, social support, and self-blame in battered women. J Interpers Violence. 1996;11(2):221–33. 10.1177/088626096011002006 [DOI] [Google Scholar]
- 50.Lincoln KD, Taylor RJ, Bullard KM, et al. Emotional support, negative interaction and DSM IV lifetime disorders among older African Americans: findings from the National Survey of American Life (NSAL). Int J Geriatr Psychiatry. 2010;25(6):612–21. 10.1002/gps.2383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peirce RS, Frone MR, Russell M, et al. A longitudinal model of social contact, social support, depression, and alcohol use. Heal Psychol. 2000;19(1):28–38. 10.1037/0278-6133.19.1.28 [DOI] [PubMed] [Google Scholar]
- 52.Wethington E, Kessler RC. Perceived support, received support, and adjustment to stressful life events. J Health Soc Behav. 1986;27(1):78–89. 10.2307/2136504 [DOI] [PubMed] [Google Scholar]
- 53.Beeble ML, Bybee D, Sullivan CM, et al. Main, mediating, and moderating effects of social support on the well-being of survivors of intimate partner violence across 2 years. J Consult Clin Psychol. 2009. Aug;77(4):718–29. 10.1037/a0016140 [DOI] [PubMed] [Google Scholar]
- 54.Mburia-Mwalili A, Clements-Nolle K, Lee W, et al. Intimate partner violence and depression in a population-based sample of women: can social support help? J Inter-pers Violence. 2010;25(12):2258–78. 10.1177/0886260509354879 [DOI] [PubMed] [Google Scholar]
- 55.Coker AL, Smith PH, Thompson MP, et al. Social support protects against the negative effects of partner violence on mental health. J Womens Health Gend Based Med. 2002. Jun;11(5):465–76. 10.1089/15246090260137644 [DOI] [PubMed] [Google Scholar]
- 56.Carlson BE, McNutt L-A, Choi DY, et al. Intimate partner abuse and mental health. Violence Against Women. 2002;8(6):720–45. 10.1177/10778010222183251 [DOI] [Google Scholar]
- 57.El-Bassel N, Gelbert L, Foleno A, et al. Social support among women in metha-done treatment who experience partner violence. Violence Against Women. 2001;7(3):246–74. 10.1177/10778010122182433 [DOI] [Google Scholar]
- 58.Dunham K, Senn CY. Memorizing negative experiences: women’s disclosure of partner abuse. J Interpers Violence. 2000;15(3):251–61. 10.1177/088626000015003002 [DOI] [Google Scholar]
- 59.Lee RM, Su J, Yoshida E. Coping with intergenerational family conflict among Asian American college students. J Couns Psychol. 2005;52(3):389–99. 10.1037/0022-0167.52.3.389 [DOI] [Google Scholar]
- 60.Taylor RJ, Chae DH, Lincoln KD, et al. Extended family and friendship support networks are both protective and risk factors for major depressive disorder, and depressive symptoms among African Americans and Black Caribbeans. J Nerv Ment Dis. 2015;203(2):132–40. 10.1097/NMD.0000000000000249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bradley R, Schwartz AC, Kaslow NJ. Posttraumatic stress disorder symptoms among low-income, African American women with a history of intimate partner violence and suicidal behaviors: self-esteem, social support, and religious coping. J Trauma Stress. 2005;18(6):685–96. 10.1002/jts.20077 [DOI] [PubMed] [Google Scholar]
- 62.Liang B, Goodman L, Tummala-Narra P, et al. A theoretical framework for understanding help-seeking processes among survivors of intimate partner violence. Am J Community Psychol. 2005;36(1–2):71–84. 10.1007/s10464-005-6233-6 [DOI] [PubMed] [Google Scholar]
- 63.Grove M, Ogden L, Pickett S, et al. The legacy effect: understanding how segregation and environmental injustice unfold over time in Baltimore. Annals Am Assoc Geogr. 2018;108:524–37. 10.1080/24694452.2017.1365585 [DOI] [Google Scholar]
- 64.Mode NA, Evans MK, Zonderman AB. Race, neighborhood economic status, income inequality and mortality. PLoS One. 2016;11(5):1–14. 10.1371/journal.pone.0154535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pratt-Harris NC, Sinclair MM, Bragg CB, et al. Police-involved homicide of unarmed Black males: observations by Black scholars in the midst of the April 2015 Baltimore uprising. J Hum Behav Soc Environ. 2016;26(3–4):377–89. 10.1080/10911359.2015.1132853 [DOI] [Google Scholar]
- 66.Tolliver WF, Hadden BR, Snowden F, et al. Police killings of unarmed Black people: centering race and racism in human behavior and the social environment content. J Hum Behav Soc Environ. 2016;26(3–4):279–86. 10.1080/10911359.2015.1125207 [DOI] [Google Scholar]
- 67.Woods-Giscombé CL. Superwoman schema: African American womens views on stress, strength, and health. Qual Health Res. 2010;20(5):668–3. 10.1177/1049732310361892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Woods-Giscombe CL, Allen AM, Black AR, et al. The Giscombe Superwoman Schema Questionnaire: psychometric properties and associations with mental health and health behaviors in African American women. Issues Ment Heal Nurs. 2019;40(8):672–81. 10.1080/01612840.2019.1584654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8(1):115–32. 10.1017/S1742058X11000130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.King CJ, Redwood Y. The health care institution, population health and Black lives. J Natl Med Assoc. 2016;108(2):131–6. 10.1016/j.jnma.2016.04.002 [DOI] [PubMed] [Google Scholar]
- 71.Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting Black lives—the role of health professionals. N Engl J Med. 2016;375(22):2113–5. 10.1056/NEJMp1609535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hoffman KM, Trawalter S, Axt JR, et al. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between Blacks and Whites. 2016. Apr 19;113(16):4296–301. Epub 2016 Apr 4. 10.1073/pnas.1516047113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60–76. 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ekman I, Swedberg K, Taft C, et al. Person-centered care—ready for prime time. Eur J Cardiovasc Nurs. 2011;10(4):248–51. 10.1016/j.ejcnurse.2011.06.008 [DOI] [PubMed] [Google Scholar]
- 75.Raja S, Hasnain M, Hoersch M, et al. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Heal. 2015;38(3):216–26. 10.1097/FCH.0000000000000071 [DOI] [PubMed] [Google Scholar]
- 76.Betancourt JR, Green AR, Carrillo JE, et al. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118(4):293–302. 10.1016/S0033-3549(04)50253-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shen MJ, Peterson EB, Costas-Muñiz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Heal Disparities. 2018;5(1):117–40. 10.1007/s40615-017-0350-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Singh AA. Transgender youth of color and resilience: negotiating oppression and finding support. Sex Roles. 2013;68(11–12):690–702. 10.1007/s11199-012-0149-z [DOI] [Google Scholar]
- 79.Sutton AL, He J, Edmonds MC, et al. Acknowledging the roles of the trustor and the trustee. 2020;34(3):600–7. 10.1007/s13187-018-1347-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kolar SK, Wheldon C, Hernandez ND, et al. Human papillomavirus vaccine knowledge and attitudes, preventative health behaviors, and medical mistrust among a racially and ethnically diverse sample of college women. J Racial Ethn Health Disparities. 2015;2(1):77–85. Epub 2014 Sep 11. 10.1007/s40615-014-0050-2 [DOI] [PubMed] [Google Scholar]
- 81.Brenick A, Romano K, Kegler C, et al. Understanding the influence of stigma and medical mistrust on engagement in routine health care among Black women who have sex with women. LGBT Health. 2017. Feb;4(1):4–10. 10.1089/lgbt.2016.0083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tekeste M, Hull S, Dovidio JF, et al. Differences in medical mistrust between Black and White women: implications for patient-provider communication about PrEP. AIDS Behav. 2019;23(7):1737–48. 10.1007/s10461-018-2283-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Swedeen B, Cooney M, Moss C, et al. Launching inclusive efforts through community conversations. Madison, WI: Waisman Center, 2012. Available at: www.waisman.wisc.edu/naturalsupports. [Google Scholar]


