Abstract
Aim
To highlight potential benefits of using Reichert's ocular response analyzer (ORA) for intraocular pressure (IOP) measurement following glaucoma filtering surgery (GFS), especially in cases of low IOP.
Background
Goldmann applanation tonometry (GAT) is widely regarded as the gold standard of IOP measurement in clinical practice. The ORA also calculates corneal biomechanics, which is used in the calculation of the cornea-compensated IOP (IOPcc).1 This useful, previously unknown information can be used to guide management in challenging clinical cases.
Case description
A 78-year-old lady underwent right trabeculectomy with mitomycin C. During the first 9 months postoperatively, IOP's when measured with GAT, were found to be low (ranging between 2 mm Hg and 5 mm Hg). The patient displayed no clinical features of hypotony and visual acuity remained stable throughout. IOP was also measured with Reichert's ORA, which gives readings for corneal hysteresis (CH), corneal resistance factor and corneal corrected IOP. IOPcc measurements obtained with ORA were consistently higher, ranging from 6.7 mm Hg to 9.3 mm Hg and were more in keeping with the clinical features of the case.
Conclusion
This case highlights the possibility that GAT can underestimate the true IOP in eyes with low IOP following GFS, as it does not account for corneal biomechanical properties.
Clinical significance
Ocular response analyzer (ORA)—measured IOPcc may be a useful adjunct in reassuring surgeons to manage postoperative numerical hypotony conservatively in the absence of any clinical signs of hypotony.
How to cite this article
Dawson S, Mohite A. Use of Ocular Response Analyzer Output Data in the Management of Low Intraocular Pressure after Glaucoma Filtration Surgery. J Curr Glaucoma Pract 2023;17(2):104-105.
Keywords: Glaucoma, Glaucoma surgery, Intraocular pressure measurement, Trabeculectomy
Background
Goldmann applanation tonometry (GAT) is widely regarded as the gold standard of intraocular pressure (IOP) measurement in clinical practice. In addition to measuring IOP, the ocular response analyzer (ORA) also calculates corneal biomechanics such as CH, which are used in the calculation of the IOPcc.1 This useful, previously unknown information can be used to guide management in challenging clinical cases such as in the example described below, where the patient was found to have postoperative hypotony following GFS using values obtained by GAT, with no clinical signs of hypotony.
Case Description
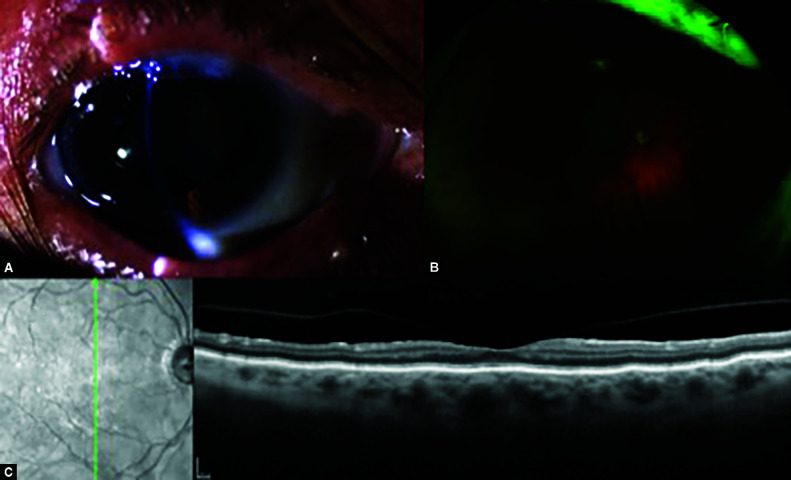
A 78-year-old lady with normal tension glaucoma underwent right trabeculectomy with mitomycin C. The postoperative course over the 1st month was routine, with IOP measuring 12–24 mm Hg. The temporal releasable suture was removed at postoperative week 3, following which the IOP measured 18 mm Hg. One week later, the nasal releasable suture was also removed, reducing the IOP to 2 mm Hg, albeit with no anterior chamber (AC) shallowing or clinical signs of hypotony. A 0.2 mL bolus of Healon® was injected intracamerally, increasing the IOP to 13 mm Hg. After 2 days, the IOP was measured as 1 mm Hg and a further 0.25 mL of intracameral Healon® was injected, increasing the IOP to 36 mm Hg. The IOP was then gradually reduced, measuring 5 mm Hg after 1 week. Best-corrected visual acuity (BCVA) remained 6/9 with no clinical signs of hypotony (shallow AC, macular folds or choroidal detachment). And, 7 weeks postoperatively, the IOP was also measured with the ORA. The IOPcc was found to be higher, 8.7 mm Hg, with a CH of 9.3 mm Hg. The IOPcc of the contralateral eye at this appointment was 23.9 mm Hg, and the CH was found to be lower than the operated eye at 7.1 mm Hg. There were no clinical features of hypotony and the patient was therefore managed conservatively. At 5 months, the GAT-measured IOP was 4 mm Hg, whilst ORA-measured IOPcc again was found to be higher (7.4 mm Hg) with a CH of 7.7 mm Hg. At 9 months, GAT-measured IOP was 3 mm Hg, whilst ORA-measured IOPcc was 6.8 mm Hg with a CH of 7.2 mm Hg. There were no signs of clinical hypotony observed at any time point and BCVA remained stable throughout. Figure 1 shows images taken at twelve months postoperatively, when GAT-measured IOP was 2 mm Hg, whilst ORA-measured IOPcc was 7.7 mm Hg.
Figs 1A to C.
The 12-month postoperative images: (A) Anterior segment photograph showing deep AC; (B) Wide-field fundus photograph showing normal appearance of fundus with no choroidal detachment; (C) Spectral-domain optical coherence tomography of the macula confirming normal posterior pole and absence of hypotony-related maculopathy
Using the IOP measurement obtained with GAT, numerically, this patient fulfills the criteria for hypotony (the World Glaucoma Association defines hypotony as pressure ≤5 mm Hg).2 Clinically, this patient had no AC shallowing, maculopathy or choroidal detachment, and vision remained stable throughout. In addition to measuring IOP, the ORA also calculates corneal biomechanics, such as the CH, which are used in the calculation of the IOPcc.1 CH is an indicator of the viscous properties of the cornea and has a normal range of 9.6–12.2 mm Hg.3 Our patient had an average postoperative CH of 8.0 mm Hg, compared to 7.6 mm Hg in the unoperated contralateral eye. A recent study demonstrated that the IOP-lowering effects of GFS cause a postoperative increase in CH.4 The average IOPcc on three postoperative visits, in this case, was 4.3 mm Hg higher than the GAT-measured IOPs and more in keeping with the clinical picture. The IOPcc values, in this case, strengthened the clinician's decision not to intervene surgically unnecessarily.
Conclusion
This case highlights the possibility that GAT can underestimate the true IOP in eyes with low IOP following GFS as it does not account for corneal biomechanical properties. This correlates with previous studies that have found GAT to underestimate IOP measurements by 3–4 mm Hg after trabeculectomy.5 Using the GAT value alone may lead surgeons to manage the case with an unnecessary return to theater for bleb revision when only observation is required, as is demonstrated in this case.
Clinical Significance
ORA-measured IOPcc may be a useful adjunct in reassuring surgeons to manage postoperative numerical hypotony conservatively in the absence of any clinical signs of hypotony.
Patient Consent
Patient consent for publishing information included in this case report, including images, has been obtained.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Konstantinidis A, Panagiotopoulou EK, Panos GD, et al. The effect of antiglaucoma procedures (trabeculectomy vs ex-press glaucoma drainage implant) on the corneal biomechanical properties. J Clin Med. 2021;10(4):802. doi: 10.3390/jcm10040802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaarawy TM, Sherwood MB, Grehn F. World Glaucoma Association Guidelines on Design and Reporting of Glaucoma Surgical Trials. Kugler Publications; 2009. [Google Scholar]
- 3.Shah S, Laiquzzaman M, Cunliffe I, et al. The use of the Reichert ocular response analyzer to establish the relationship between ocular hysteresis, corneal resistance factor and central corneal thickness in normal eyes. Cont Lens Anterior Eye. 2006;29(5):257–262. doi: 10.1016/j.clae.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Pakravan M, Afroozifar M, Yazdani S. Corneal biomechanical changes following trabeculectomy, phaco-trabeculectomy, Ahmed glaucoma valve implantation and phacoemulsification. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4074468/ J Ophthalmic Vis Res. 2014;9(1):7–13. Retrieved from: [PMC free article] [PubMed] [Google Scholar]
- 5.Pillunat K, Spoeri E, Terai N, et al. Corneal biomechanical changes after trabeculectomy and the impact on intraocular pressure measurement. J Glaucoma. 2017;26(3):278–282. doi: 10.1097/IJG.0000000000000595. [DOI] [PubMed] [Google Scholar]