Abstract
Background
Drugs are a major source of greenhouse gas (GHG) emissions from healthcare systems. Pressurized metered‐dose inhalers (pMDIs) have raised concerns over their environmental impact due to GHG emissions. Evaluations and reduction strategies for GHGs have been primarily studied in Europe, but not in other regions, including Japan. Therefore, our objective was to calculate the carbon footprint of inhalers in Japan and evaluate their reduction scenarios.
Methods
Using the National Database of Health Insurance Claims, our analysis was conducted on inhaler prescriptions in Japan for the fiscal year of 2019. We calculated the number of inhalers used, GHG emissions, and total costs. Next, we simulated the environmental and economic impacts of three reduction scenarios: the first scenario replaced pMDI with dry power inhalers, followed by age‐based replacements. In the last scenario, we replaced pMDI with a propellant with a lower global warming potential.
Results
All inhaler‐related GHG emissions were 202 ktCO2e, of which 90.9% were attributed to pMDI use. Scenario analysis demonstrated that replacing 10% pMDI with DPI would reduce emissions by 6.7%, with a relatively modest increase in cost; substituting 10% of pMDI used by adults (excluding children and older adults) with alternative inhalers would reduce emissions by 6.1%, with a 0.7% increase in cost; and, replacing 10% of pMDI propellants with lower global warming potential would reduce emissions by 9.3%.
Conclusions
Selecting appropriate inhalers can mitigate GHG emissions in Japan, but its impact will be less than in other countries. Nevertheless, collaborative efforts between physicians, patients, and pharmaceutical companies are necessary to reduce GHG emissions.
Keywords: carbon footprint, global warming, greenhouse gas emission, inhaler, Japan, National Database of Health Insurance Claims
All inhaler‐related GHG emissions in Japan were 202 ktCO2e, of which 90.9% were attributed to pMDI use. Scenario analysis demonstrated that substituting 10% of pMDI used by adults (excluding children and older adults) with alternative inhalers would reduce emissions by 6.1%, with a 0.7% increase in cost.

1. INTRODUCTION
Global warming is a serious and urgent environmental problem. 1 Greenhouse gases (GHGs), such as carbon dioxide (CO2), methane, and chlorofluorocarbons (CFCs), which increase because of human activities, mainly contribute to global warming. In response to this challenge, the United Nations Framework Convention on Climate Change (UNFCCC) serves as the overarching global framework for addressing climate change. 2 At COP21 in 2015, the Paris Agreement was adopted as a successor to the Kyoto Protocol, setting the goal of limiting the global temperature increase to 1.5°C or less, well below the 2°C threshold established in relation to preindustrial levels. To achieve this objective, a number of countries, as well as Japan, have announced plans to achieve virtually zero CO2 emissions by 2050. 3 Although the reduction of fossil fuels and introduction of renewable energy are major policies in Japan, low‐carbon strategies in all industries are essential for achieving this goal.
In recent years, the relationship between healthcare and global warming has attracted significant attention. Global warming not only causes direct health hazards through an increase in heat‐related illnesses, but also has indirect adverse effects on the human body through an increase in heart disease, epidemics of tropical infectious diseases, and deteriorating mental health. 4 , 5 Healthcare's environmental impact is also significant. Nansai et al. calculated healthcare‐related carbon footprint in Japan to be 62 MtCO2e in 2011, which is equivalent to 4.6% of Japan's total carbon footprint. 6 In other developed countries, healthcare‐related GHG emissions are approximately 5%–10% of the national GHG emissions. 7 , 8 , 9 Although global warming must be addressed to promote human health, the healthcare system itself is a major source of GHG emissions.
Greenhouse gas emissions from healthcare stem from various sources and can be mitigated through various reduction strategies. In 2011, the carbon footprint of the Japanese healthcare industry was primarily attributed to healthcare services, such as inpatient and outpatient care, and pharmacy services, accounting for 66.4% of emissions. 5 Among healthcare services, the largest contributor was pharmaceutical procurement (27%). Other contributors included electricity consumption, transportation, and waste disposal. To achieve net zero healthcare‐related emissions in 2050, the US Agency for Healthcare Research and Quality has published a guide containing recommended measures and interventions to reduce the carbon footprint of healthcare. 10 These measures include enhancing energy efficiency, implementing sustainable transportation systems, managing the supply chain, and managing anesthetics. Among these, reducing the percentage of pressurized metered‐dose inhalers (pMDI) prescriptions among all inhalers was identified as the highest priority measure for reducing GHG emissions associated with medications.
The use of portable inhalers in patients with asthma and chronic obstructive pulmonary disease (COPD) has one of the greatest impacts on global warming. 11 , 12 There are two main types of inhalers: dry powder inhalers (DPI) and pMDI. Of these, pMDIs contain CFC substitutes as propellants, which are harmful to the environment, whereas DPI is propellant‐free. Currently prescribed pMDIs include 1,1,1,2‐tetrafluoroethane (HFA‐134a) or 1,1,1,2,3,3‐heptafluoropropane (HFA‐227ea). The percentage of pMDI and DPI use varies by country. In 2019, the United Kingdom used more pMDI at 69.6%, but the average was approximately 30%–40%. 13 It is estimated that 3.9% of the UK health service's carbon footprint is due to the use of pMDIs. 14 In the United States, the reported usage of pMDI in 2018 was approximately 75%. 10 One advantage of pMDIs over DPIs is that they require less inspiration force. Thus, pMDIs may be more desirable for children and older adults with decreased inspiratory flow. 15 , 16 Elderly individuals, particularly those over 70, have a marked decrease in inhaler technique and knowledge. 17 Despite the relatively small contribution of pMDI usage to GHG emissions (0.03%), the substantial proportion of emissions within the healthcare sector highlights the potential for reduction. 18 For instance, in 2019, the National Health Service in the United Kingdom proposed a target to decrease inhaler‐related GHG emissions by 50% within the next decade. 19
Several studies have examined strategies to reduce the GHG emissions associated with pMDIs and evaluated their environmental and economic impacts. The first strategy is to replace pMDI with a nonpMDI (NPI). Wilkinson et al. estimated that for every 10% replacement, 58 ktCO2e could be saved. 20 Forced replacement of inhalers throughout a country could lead to up to 76%–84% reduction in pMDI‐related GHG emissions. 13 , 20 , 21 The second strategy is to replace pMDI propellant with an eco‐friendly one. HFA134a and HFA227ea, currently in use, have high global warming potentials (GWP) of 1300 and 3350, respectively. Recently, a pMDI device that uses HFA152a (GWP of 138), has been developed. 11 Pernigotti et al. estimated that this replacement would result in a 65%–71% reduction. 13 The third strategy is to optimize the use of SABAs. Their overuse is associated with worse asthma outcomes. 22 These devices are often pMDIs; therefore, reducing the use of SABAs may improve patient outcomes and reduce GHG emissions.
This study aims to examine GHG emissions associated with inhaler use in Japan and assess potential reduction strategies. Despite the limited studies in Japan, we aim to fill this gap using data from The National Database of Health Insurance Claims and Specific Health Checkups of Japan (NDB) Open Data. This study will calculate inhaler usage and associated GHG emissions in Japan and evaluate the environmental and economic implications of various reduction scenarios, including the replacement of pMDI with DPI, selective replacement of DPI only for adults who can use them appropriately, and implementation of the most eco‐friendly pMDI. This study is novel in its utilization of age‐specific usage data, which has not been evaluated in prior research. These results will provide valuable insights for the Japanese and worldwide government and medical professionals to understand the potential impact and the most efficient methods of reducing GHG emissions from inhalers.
2. METHOD
2.1. Study design and data source
This was a nationwide, cross‐sectional study. The NDB, developed by the Ministry of Health, Labour and Welfare (MHLW), provides reliable data on drug prescriptions in Japan. MHLW also published NDB Open Data Japan, which contains fundamental spreadsheets and are easily accessible to the public. In this study, all inhaler use data were obtained from the 6th NDB Open Data Japan. 23 This database included medical claims for almost all populations in Japan for fiscal year (FY) 2019. Data on medications included drug names, codes, prices, and the number of prescriptions. The database also provided prescription numbers by age group and prefecture. No data were provided for prescriptions below 1000. Data on the top 100 drugs by class were published. We excluded data on topical and nebulizer medications to collect only portable inhaler data.
Additional information on inhalers was obtained from the online published package inserts. All inhalers were separated into the following classes: SABAs, short‐acting muscarinic antagonists (SAMAs), inhaled corticosteroids (ICS), long‐acting beta2‐agonists (LABAs), long‐acting muscarinic antagonists (LAMAs), ICS + LABAs, ICS + LAMAs, LABAs + LAMAs, and ICS + LABAs + LAMAs. The device types were divided into pMDIs, DPIs, and soft mist inhalers (SMIs). Because GHG is used only for pMDIs, DPIs and SMIs were placed in the same category as NPIs in this study. We further identified the propellants used in pMDIs (only HFA‐134a and HFA‐227ea were used in Japan).
2.2. Inhaler use
The 6th NDB Open database provided data on the total number of prescriptions for all inhalers. However, for DPIs that use two devices (Breezhaler® and Handihaler®), the number of capsules prescribed were provided. In addition, the use of Rotadisk® inhalers was defined as the number of blisters prescribed. Most inhalers are designed to be consumed as one device per month. Therefore, considering the percentage of inhaler use, the total number of capsules or blisters divided by the standard number of puffs for 28 days was used as the equivalent number of inhaler prescriptions for these DPIs. In addition, SABAs were considered a separate category to examine the percentage of use.
2.3. Carbon footprint analysis
The carbon footprint of an inhaler is the amount of CO2 equivalent (CO2e) of all GHG emissions associated with its manufacture, distribution, use, and disposal. 18 Data on the carbon footprint per inhaler or per inhalation for all inhalers were obtained from previous studies and nonprofit public information. 13 , 20 , 24 Although we requested that pharmaceutical companies provide missing information, some data were unavailable. Missing data were estimated by referring to data on similar drugs. In the estimation of the missing pMDI data, we referred to their carbon footprint using the same HFA. The carbon footprint data of inhalers are presented in Appendix S1.
More than 95% of pMDI carbon footprint was attributable to the HFA propellant in during use. 18 By contrast, the carbon footprint of NPIs was largely unrelated to the use. Considering these characteristics, we mainly used the carbon footprint per inhaler for NPIs and the carbon footprint per puff for pMDIs when calculating total GHG emissions. The exception was NPIs that use capsules and blisters, for which the carbon footprint per puff was used in the calculation.
2.4. Economic analysis
Drug prices per inhaler were included in the dataset, and inhaler‐related costs were calculated by multiplying them by the total number of prescriptions. In DPIs with capsules or blisters, drug prices were calculated by multiplying the drug price per capsule or blister by the total prescribed number.
2.5. Scenario analysis
We simulated the environmental and economic impacts of three possible scenarios to reduce the carbon footprint of inhalers.
2.5.1. Scenario 1: Forced replacement
This scenario examined the impact of replacing pMDIs with DPIs for inhaler types. In Japan, pMDIs are commonly used in six drug classes: ICS, SABAs, SAMA, ICS + LABA, LABA+LAMA, and ICS + LABA+LAMA. Of the NPIs, SMI is used primarily for LABAs and LABA+LAMA and is a limited candidate to replace pMDI. Therefore, we replaced pMDI with DPI in this scenario. In addition, SAMA was removed from this replacement analysis because only pMDI is commercially available.
To assess the environmental impact, we calculated the total GHG emissions assuming 10% of pMDIs were replaced by DPIs. In the replacement, the carbon footprint per DPI inhaler was calculated to be 0.8 kg CO2e. Because the carbon footprint of DPI is almost the same regardless of drug class, this value was applied consistently to all pMDI replacements.
We then evaluate the economic impact of replacement. As noted above, pMDIs were used in six drug classes. Cost calculations were performed using the price of the most prescribed DPI for each drug class. The details of these drugs are provided in Appendix S1
2.5.2. Scenario 2: Age‐adjustment replacement
In scenario 1, we replaced pMDIs with DPIs, but preferred agents also depend on patient age. Children generally prefer pMDIs; existing data show a high rate of pMDI use in the pediatric group. 17 Among older adults, the preferred device was determined by their disability. 15 For example, DPIs are not preferred by patients with reduced maximal inspiratory volume, whereas pMDIs are not preferred by those with reduced manual dexterity. Therefore, in Scenario 2 we only replaced 10% of pMDIs with DPIs for adults aged between 15 to 74 years while retaining the original inhalation devices for children and older adults. The same calculation methods were used as in Scenario 1.
2.5.3. Scenario 3: Replacement with low‐GWP pMDI
The newly developed HFA propellant, HFA‐152a, has a significantly reduced GWP of 138, which is 11% of the GWP of HFA‐134a and 4% of that of HFA‐227ea. 11 , 13 This scenario assumed that 10% of pMDIs using propellants currently used were replaced with pMDIs using HFA‐152a. Calculations were made assuming that GHG emissions from inhalers using HFA‐134a were reduced by up to 11%, and GHG emissions from inhalers using HFA‐227ea were reduced by up to 4%. As inhalers utilizing this propellant are not currently commercially available, an economic analysis was not performed for this scenario.
2.6. Statistical analysis
This study was mainly descriptive and, therefore, did not contain any statistical hypotheses to analyze. First, we described the percentage of inhaler use and total costs. We then calculated the inhaler‐related GHG emissions and summarized them by drug class. The calculations were repeated for each age group and prefecture. The scenarios were calculated as described above. A graphical summary of the calculation methodology is presented in the Appendix S1.
3. RESULTS
3.1. Current inhaler uses
Among all inhalers prescribed in Japan in FY2019, pMDIs accounted for 22.6% of them, whereas NPIs accounted for 77.4% (69.5% DPIs, 7.9% SMI; Table 1). The total cost of inhaler use was 159 billion yen, of which DPIs, pMDIs, and SMIs were responsible for 73.9%, 15.0%, and 11.1%, respectively.
TABLE 1.
Descriptive summaries of inhaler usage in Japan in fiscal year 2019.
| pMDI | DPI | SMI | Total | |
|---|---|---|---|---|
| Prescribed inhalers | 7.5 million (22.6%) | 23.1 million (69.5%) | 2.6 million (7.9%) | 33.1 million |
| Greenhouse gas emission (ktCO2e) | 184.0 (90.9%) | 18.5 (9.1%) | 0.0 (0.0%) | 202.6 |
| Cost (yen) | 24.0 billion (15.0%) | 117.9 billion (73.9%) | 17.7 billion (11.1%) | 160.0 billion |
Abbreviations: DPI, dry powder inhaler; pMDI, pressurized metered‐dose inhaler; SMI, soft mist inhaler.
3.2. Carbon footprint calculation
GHG emissions from inhalers totaled 202.6 ktCO2e, of which 90.9% (184 ktCO2e) were attributed to the use of pMDIs (Table 1). By drug class, ICS + LABA accounted for 53.5%, SABAs for 37.6%, and ICSs for 7.7%; these drug classes were responsible for most emissions.
3.3. Differences in inhaler use by age and prefecture
The number of inhalers used, costs, and GHG emissions by age group are shown in Figure 1. Children under 15 years of age used 4.5% of all inhalers, of which 44.6% were pMDIs. In other age groups, pMDI use ranged from 14.6%–26%. SMI use was high among older adults (60 years and above), accounting for 88.8% of total SMI use. The age group with the highest GHG emissions from inhaler use was the 44–59 age group (24.4%), followed by the 60–74 (23.8%), and 75–90 (20.5%) age groups.
FIGURE 1.
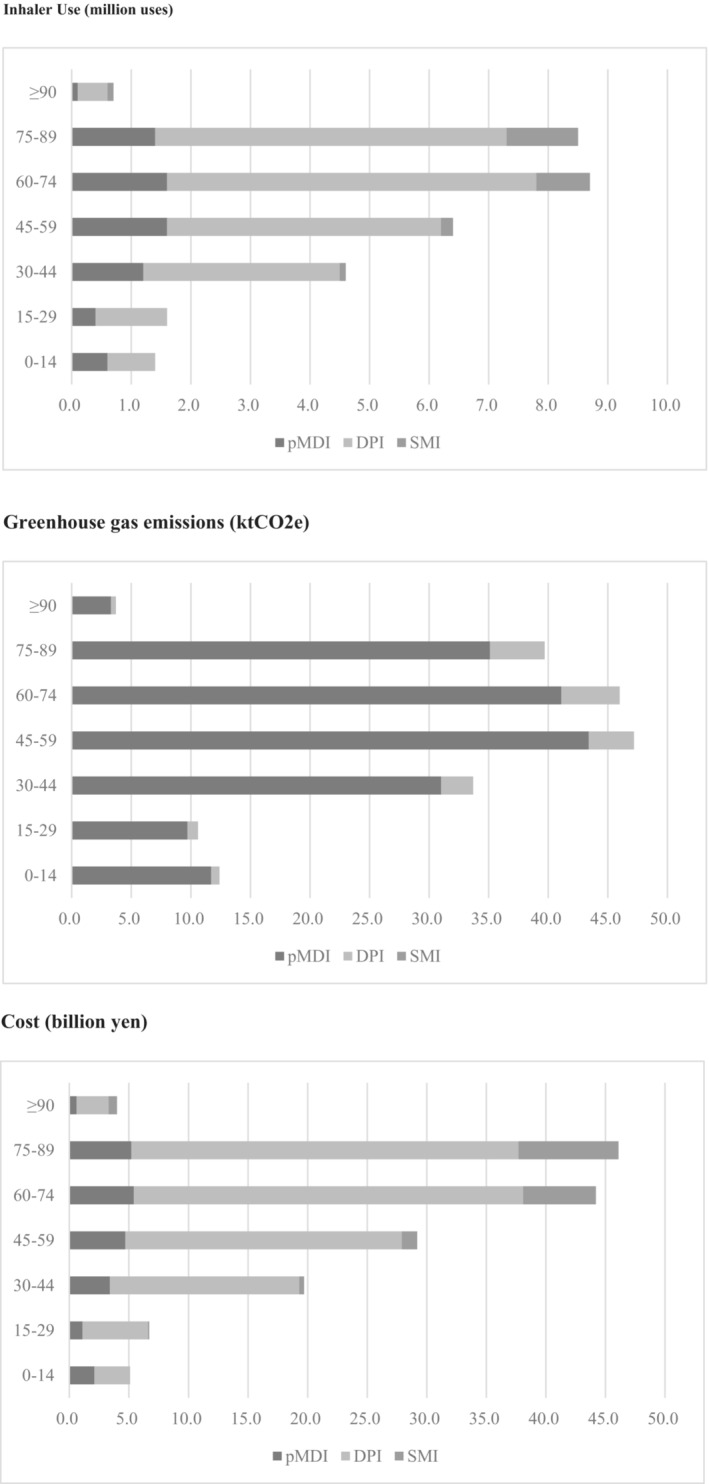
Descriptive summaries of inhaler usage by age group. pMDI, pressurized metered‐dose inhaler; DPI, dry powder inhaler; SMI, soft mist inhaler.
Appendix S1 presents the utilization of inhalers, associated costs, and GHG emissions by prefecture. The national average percentage of pMDIs among all inhalers was 20.7%. The prefectures with the highest percentage of pMDI utilization were Tokushima (26.5%), Hyogo (25.8%), and Fukuoka (25.4%), while the prefectures with the lowest were Yamanashi (13.0%), Tottori (15.4%), and Iwate (15.8%).
3.4. Scenario analysis
3.4.1. Scenario 1: Forced replacement
This scenario evaluated the impact of replacing the inhaler type from a pMDI to a DPI. In terms of environmental impact, replacing 10% of the pMDIs prescribed in Japan in FY2019 with DPIs would reduce their GHG emissions by 6.7% (12.4 ktCO2e). The economic impact of switching from a 10% pMDI to DPI was small, with a 1.4% increase in total drug cost (2.2 billion yen).
3.4.2. Scenario 2: Age‐adjustment replacement
The environmental impact of switching from pMDIs to DPIs for adult patients aged 15–74 years was evaluated in this scenario. We found that replacing 10% of pMDIs with DPIs in this age group would reduce GHG emissions by 8.7%, reducing all GHG emissions by 6.1%. Considering the fiscal impact, switching to DPIs would increase inhaler costs for adults by 1.1%, resulting in an overall increase of 0.7%.
3.4.3. Scenario 3: Replacement to low‐GWP pMDI
A hypothetical scenario was constructed wherein 10% of pMDIs utilizing current propellants were replaced with pMDIs using newly developed low WGP formulation, HFA‐152a propellants. The results of this scenario indicate a 9.3% reduction in GHG emissions associated with the use of pMDIs. When considering the overall GHG emissions from all inhaler formulations, GHG emissions would be reduced by 8.4%.
4. DISCUSSION
In this study, we assessed nearly all prescribed inhalers in Japan in FY2019 using the 6th NDB Open database. The inhaler‐related GHG emissions were 202 ktCO2e per year. Although used in only 22.6% of inhalers, most of the emissions (90.9%) were derived from pMDIs. An age‐specific analysis revealed that a greater proportion of children were prescribed pMDIs (44.6%); however, there was a slight variation in utilization by prefecture. For each replacement of pMDI with 10% DPI, emissions could be reduced by 6.7%, with limited economic impact. Replacing 10% pMDI among adults would result in an overall emission reduction of 6.1%. If 10% of pMDI propellants were replaced with a novel low‐GWP propellant, the emissions would be markedly reduced by 9.3%. This study provides essential data to promote the environmentally appropriate use of inhalers in Japan and can serve as a starting point for future research.
The study estimated inhaler‐related GHG emissions in Japan in FY2019 to be 202 ktCO2e, which is relatively small compared to European countries, even when accounting for population differences. In 2019, Pernigotti et al. found domestic emissions for the United Kingdom, France, and Germany to be 1300 ktCO2e, 520 ktCO2e, and 450 ktCO2e, respectively. 13 The difference in emissions can be attributed to Japan's low use of pMDI (22.6%); in Europe it is approximately 40%–50%, and in the United Kingdom, it is close to 70%. In addition, while SABAs are the main source of pMDI emissions in Europe, in Japan the share is lower at 37.6%, with ICS + LABAs (53.5%) instead being the largest source. These differences influence strategies for reducing inhaler‐related GHG emissions in Japan.
In the scenario analysis, changing 10% of pMDIs to DPIs with the highest prescription volume for each drug class resulted in a 6.7% GHG reduction (12.4 ktCO2e), while increasing costs by 1.3% (2.2 billion yen). According to the UK estimates, a 10% replacement would result in a 9.1% GHG reduction. 20 Pernigotti et al. made similar estimates for five EU countries and reported that 80% replacement would result in 68% GHG reduction. 13 In Japan, the reduction effect of replacement is relatively small, probably because the ratio of pMDI prescriptions is lower than that in these countries. The economic impact of replacement has also been investigated in the United Kingdom and the Netherlands, and it appears that a change to lower‐cost DPIs can result in cost reductions, while a conventional change would lead to an increase in cost. 20 , 21 In this study, it appears that a change to a DPI with a higher prescribing volume would lead to only a slight cost increase.
Age‐specific analysis was a unique aspect of this study. The device selection among children and older adults differs from that in adults. In children, the use of pMDIs was relatively high at 44.6%, which is also true in other studies. The use of DPI formulations is more difficult in childhood due to their lower inhalation capacity, and pMDIs are generally preferred. As SMIs are only available in LAMA and LABA+LAMA, they are mostly used in older patients with COPD. The change from pMDI LAMA to SMI LAMA is favorable because SMI is a device with very low GHG emissions. In addition, in older adults with reduced physical function, DPI is difficult to use when inhalation force is reduced, and pMDI is difficult to use when hand dexterity is reduced. 15 Therefore, the simple replacement of pMDIs with DPIs is not a realistic option for both children and older adults, and different methods of reducing GHGs should be encouraged.
This study estimated the inhaler‐related GHG emissions in Japan to be 202 ktCO2e., which correspond to 2.4% of the total GHG emissions from all drug prescriptions. 6 This GHG emission cannot be ignored, and its reduction should be encouraged. Table 2 lists the possible strategies for reducing inhaler use in Japan. For clinicians and patients, the crucial factor is to take into account environmental considerations when selecting an inhaler device. Inhaler device selection is typically based on factors such as efficacy, cost, and personal preference. 25 Physicians should educate patients on the environmental impact of inhaler devices and discuss the potential for choosing environmentally friendly options. In this context, the effect of inhaler replacement on patient outcomes is a critical aspect that requires consideration. Nonetheless, this study could not assess this aspect due to the limitations of the NDB Open Data, which does not include patient‐specific information. A post‐hoc analysis of a randomized controlled trial on adults showed that switching from ICS/LABA pMDIs to DPIs improved asthma control in those who switched compared to those who remained on pMDIs. 26 Considering the substantial GHG emissions from ICS/LABA pMDIs in Japan, it may be both safe and effective to replace ICS/LABA. However, replacing inhalers may be challenging for children and the elderly. Therefore, the simulation in this study focuses on reducing GHG emissions in adult cases, resulting in a 6.1% reduction compared to the 6.7% reduction from replacing all ages. Hence, it may be beneficial to initially focus on reducing GHG emissions in adult cases. Cost is also a concern, but the increase in cost may be minimal depending on the chosen device. Pharmacists can also facilitate the selection of appropriate inhalers. Pharmacists routinely educate patients on the use of inhalers and have sufficient time to provide information to patients regarding eco‐friendly inhaler selection. Pharmaceutical companies play a major role in reducing GHG emissions. Changing the propellant used in pMDIs would make the greatest impact. GHG emissions from pMDIs could be significantly reduced if devices are developed using the new propellant, HFA‐152a. Furthermore, most Japanese pharmaceutical companies do not disclose their carbon footprint data for the inhalers they market. This information should be actively released to enable clinicians and patients to make appropriate choices.
TABLE 2.
Strategies to reduce greenhouse gas emissions from inhaler in Japan.
| Strategy | Key stakeholder | Effect | Potential reduction | Feasibility | Additional comment |
|---|---|---|---|---|---|
| Switch from pMDI to NPI (DPI or SMI) | Physician, Patient, Pharmacist | Avoid use of HFA propellants | All age: 6.7% reduction with 10% replacement Adults: 6.1% reduction with 10% replacement | All age: Moderate Adults: High | Difficult for children and the elderly |
| Switch from HFA‐227ea pMDI to HFA‐134a pMDI | Pharmaceutical company | Avoid use of high GWP propellants | 61% reduction per pMDI inhaler | Moderate | HFA‐227ea is used in top share SABA |
| Change propellant of pMDI to HFA‐152a | Pharmaceutical company | Utilize HFAs with significantly lower GWP | 9.1% reduction with 10% replacement | Low | Not commercially available |
| Reduction of SABA use | Physician | Reduce use of SABA pMDI | Unknown | Moderate | SABA overuse worsens asthma outcomes |
| Recycle and Reuse | Physician, Patient, Pharmacist, Pharmaceutical company | Reduce disposal of propellants | Depends on the recycling rate of the inhaler and the quantity of residual propellant (25%–50%) 13 , 20 | Moderate | No recycle program available in Japan |
Note: This table illustrates possible strategies for reducing inhaler‐associated GHG emissions in Japan. The strategies and their effects have been derived from the simulation outcomes of the present investigation and prior studies.
Abbreviations: DPI, dry powder inhaler; HFA, hydrofluoroalkane; pMDI, pressurized metered‐dose inhaler; SABA, short‐acting beta agonist; SMI, soft mist inhaler.
This study had several limitations. First, carbon footprint data for every drug in this study were not available in detail, and some of the calculations were based on assumptions. Furthermore, the carbon footprint data for inhalers was calculated in other countries, and variations in the calculation may occur in different countries. Second, the feasibility of these scenarios has not been verified. We do not know how much of an effort it would require for clinicians and pharmaceutical companies to replace pMDI to DPI in the real world, and this needs to be investigated in the future. Third, there are other strategies to reduce GHGs emissions from inhalers. These strategies include changing HFA‐227ea inhalers to HFA‐134a inhalers, reducing the use of SABAs, and promoting inhaler recycling.
5. CONCLUSION
Although the GHG emissions associated with inhalers in Japan are relatively low compared to those in other European countries, there remains considerable potential for reduction. Collaborative efforts among healthcare providers, patients, and pharmaceutical companies are required to care for patients with asthma and COPD in an environmentally responsible manner.
CONFLICT OF INTEREST STATEMENT
The authors declare that no conflicts of interest exist.
ETHICAL APPROVAL
This study was approved by the Ethics Review Board of Mito Kyodo General Hospital (No 22–14). This study used NDB Open Data, which are anonymized, and so, individual patients could not be identified. Therefore, there was no direct patient involvement in this study and informed consent was not required.
Supporting information
Appendix S1
ACKNOWLEDGMENT
We thank members of the Green Practice Japan (https://greenpractice‐jp.studio.site/0) for their assistance. This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
Nagasaki K, Kaji Y, Wada Y, Sasaki T. The environmental impact of inhaler replacement: A carbon footprint and economic calculation of the National Database of Health Insurance Claims in Japan. J Gen Fam Med. 2023;24:207–214. 10.1002/jgf2.622
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available as the National Database of Health Insurance Claims in Japan at https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177221_00010.html.
REFERENCES
- 1. Atwoli L, Baqui AH, Benfield T, Bosurgi R, Godlee F, Hancocks S, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. N Engl J Med. 2021;385(12):1134–7. 10.1056/nejme2113200 [DOI] [PubMed] [Google Scholar]
- 2. Shigetomi Y, Nansai K, Kagawa S, Tohno S. Changes in the carbon footprint of Japanese households in an aging society. Environ Sci Technol. 2014;48(11):6069–80. [DOI] [PubMed] [Google Scholar]
- 3. METI . Japan's roadmap to “beyond‐zero” carbon. [cited 2022 Sep 14]. Available from: https://www.meti.go.jp/english/policy/energy_environment/global_warming/roadmap/
- 4. Rocque RJ, Beaudoin C, Ndjaboue R, Cameron L, Poirier‐Bergeron L, Poulin‐Rheault RA, et al. Health effects of climate change: an overview of systematic reviews. BMJ Open. 2021;11(6):e046333. 10.1136/bmjopen-2020-046333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rossati A. Global warming and its health impact. Int J Occup Environ Med. 2017;8(1):7–20. 10.15171/ijoem.2017.963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nansai K, Fry J, Malik A, Takayanagi W, Kondo N. Carbon footprint of Japanese health care services from 2011 to 2015. Resour, Conserv Recycl. 2020;152:104525. 10.1016/j.resconrec.2019.104525 [DOI] [Google Scholar]
- 7. Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PloS One. 2016;11(6):e0157014. 10.1371/journal.pone.0157014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T, et al. Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5(2):e84–92. 10.1016/s2542-5196(20)30271-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Malik A, Lenzen M, McAlister S, McGain F. The carbon footprint of Australian health care. Lancet Planet Health. 2018;2(1):e27–35. 10.1016/s2542-5196(17)30180-8 [DOI] [PubMed] [Google Scholar]
- 10. AHRQ . Reducing Healthcare Carbon Emissions. [cited 2023 Jan 27]. Available from: https://www.ahrq.gov/sites/default/files/wysiwyg/healthsystemsresearch/decarbonization/decarbonization.pdf
- 11. Wilkinson A, Woodcock A. The environmental impact of inhalers for asthma: a green challenge and a golden opportunity. Br J Clin Pharmacol. 2022;88(7):3016–22. 10.1111/bcp.15135 [DOI] [PubMed] [Google Scholar]
- 12. Woodcock A, Beeh KM, Sagara H, Aumônier S, Addo‐Yobo E, Khan J, et al. The environmental impact of inhaled therapy: making informed treatment choices. Eur Respir J. 2022;60(1):2102106. 10.1183/13993003.02106-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pernigotti D, Stonham C, Panigone S, Sandri F, Ferri R, Unal Y, et al. Reducing carbon footprint of inhalers: analysis of climate and clinical implications of different scenarios in five European countries. BMJ Open Respir Res. 2021;8(1):e001071. 10.1136/bmjresp-2021-001071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Unit NSD . Reducing the Use of Natural Resources in Health and Social Care. Available from: https://networks.sustainablehealthcare.org.uk/sites/default/files/resources/20180912_Health_and_Social_Care_NRF_web.pdf
- 15. Gibson PG, McDonald VM, Marks GB. Asthma in older adults. Lancet. 2010;376(9743):803–13. 10.1016/s0140-6736(10)61087-2 [DOI] [PubMed] [Google Scholar]
- 16. Brocklebank D, Wright J, Cates C. Systematic review of clinical effectiveness of pressurised metered dose inhalers versus other handheld inhaler devices for delivering corticosteroids in asthma. BMJ. 2001;323(7318):896–900. 10.1136/bmj.323.7318.896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hira D, Komase Y, Koshiyama S, Oguma T, Hiramatsu T, Shiraki A, et al. Problems of elderly patients on inhalation therapy: difference in problem recognition between patients and medical professionals. Allergol Int. 2016;65(4):444–9. [DOI] [PubMed] [Google Scholar]
- 18. Emeryk AW, Sosnowski T, Kupczyk M, Śliwiński P, Zajdel‐Całkowska J, Zielonka T, et al. Impact of inhalers used in the treatment of respiratory diseases on global warming. Advances. Respir Med. 2021;89(4):427–38. 10.5603/arm.a2021.0092 [DOI] [PubMed] [Google Scholar]
- 19. NHS . NHS Long Term Plan. Available from: https://www.longtermplan.nhs.uk
- 20. Wilkinson AJK, Braggins R, Steinbach I, Smith J. Costs of switching to low global warming potential inhalers. An economic and carbon footprint analysis of NHS prescription data in England. BMJ Open. 2019;9(10):e028763. 10.1136/bmjopen-2018-028763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Have P t, P van H, Wichers I, et al. Turning green: the impact of changing to more eco‐friendly respiratory healthcare – a carbon and cost analysis of Dutch prescription data. BMJ Open. 2022;12(6):e055546. 10.1136/bmjopen-2021-055546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nwaru BI, Ekström M, Hasvold P, Wiklund F, Telg G, Janson C. Overuse of short‐acting β2‐agonists in asthma is associated with increased risk of exacerbation and mortality: a nationwide cohort study of the global SABINA programme. Eur Respir J. 2020;55(4):1901872. 10.1183/13993003.01872-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. MHLW . 6th NDB Open data. [cited 2022 Sep 15]. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177221_00010.html
- 24. PrescQIPP . Inhaler carbon footprint data. [cited 2022 Sep15]. Available from: https://www.prescqipp.info/our‐resources/bulletins/bulletin‐295‐inhaler‐carbon‐footprint/
- 25. Schreiber J, Sonnenburg T, Luecke E. Inhaler devices in asthma and COPD patients—a prospective cross‐sectional study on inhaler preferences and error rates. BMC Pulm Med. 2020;20(1):1–2. 10.1186/s12890-020-01246-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Woodcock A, Janson C, Rees J, Frith L, Löfdahl M, Moore A, et al. Effects of switching from a metered dose inhaler to a dry powder inhaler on climate emissions and asthma control: post‐hoc analysis. Thorax. 2022;77(12):1187–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
The data that support the findings of this study are openly available as the National Database of Health Insurance Claims in Japan at https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177221_00010.html.


