This analysis comprising a cohort study and cross-sectional study estimates the incidence and prevalence of diagnosed vitiligo overall and by sex, age, and race and ethnicity in the US from 2015 to 2019.
Key Points
Question
What were the incidence and prevalence of diagnosed vitiligo overall and by race and ethnicity, age, and sex in the US from 2015 to 2019?
Findings
In this cohort study of 2 980 778 patients with vitiligo (incidence analysis) and cross-sectional study of 1 057 534 patients (prevalence analysis), the highest adjusted incidence rates were found among Asian American patients and patients aged 60 to 69 years. The highest adjusted prevalence estimates were found among Hispanic/Latino patients and patients aged 70 years or older.
Meaning
The findings suggest that Asian American, Hispanic/Latino, and older individuals have the greatest burden of vitiligo in the US.
Abstract
Importance
Vitiligo has substantial psychosocial consequences. Yet its burden is poorly established.
Objective
To estimate incidence and prevalence of diagnosed vitiligo across age, sex, and racial and ethnic subgroups in the US.
Design, Setting, and Participants
This analysis comprising a cohort study and cross-sectional study included electronic health records for health care–seeking children, adolescents, and adults across 4 US census regions. Data for the incidence analysis were obtained from January 1, 2015, through December 31, 2019, and data for the prevalence analysis were obtained from January 1 through December 31, 2019. Data were analyzed from December 13, 2022, to June 8, 2023.
Main Outcomes and Measures
The main outcomes were incidence (per 100 000 person-years [PY]) and prevalence of diagnosed vitiligo overall and by age, race and ethnicity, and sex.
Results
A total of 2 980 778 patients with vitiligo were included in the incidence analysis (mean [SD] age, 41.5 [24.0] years; 57.0% female; 1.4% Asian American; 12.9% Black; 1.5% Hispanic/Latino; 77.3% White; 6.9% other or multiracial) and 1 057 534 in the prevalence analysis (mean [SD] age, 43.4 [24.7] years; 57.5% female; 1.7% Asian American, 14.7% Black, 1.4% Hispanic/Latino; 75.7% White; 6.6% other or multiracial). Age- and sex-adjusted overall incidence rate (IR) of diagnosed vitiligo was 22.6 per 100 000 PY (95% CI, 21.5-23.8 per 100 000 PY), and prevalence was 0.16% (95% CI, 0.15%-0.17%). Sex-adjusted IR was highest among patients aged 60 to 69 years (25.3 per 100 000 PY; 95% CI, 22.2-28.6 per 100 000 PY), and prevalence was highest among patients aged 70 years or older (0.21%; 95% CI, 0.19%-0.23%). The highest age-adjusted IR was observed among Asian American patients (41.2 per 100 000 PY; 95% CI, 28.2-58.2 per 100 000 PY), followed by Hispanic/Latino patients (37.3 per 100 000 PY; 95% CI, 25.7-52.4 per 100 000 PY), patients reporting other or multiple races (31.1 per 100 000 PY; 95% CI, 25.9-37.1 per 100 000 PY), Black patients (29.6 per 100 000 PY; 95% CI, 26.0-33.6 per 100 000 PY), and White patients (18.7 per 100 000 PY; 95% CI, 17.5-20.0 per 100 000 PY). The highest age-adjusted prevalence was observed among Hispanic/Latino patients (0.29%; 95% CI, 0.20%-0.39%), followed by Asian American patients (0.27%; 95% CI, 0.19%-0.35%), patients reporting other or multiple races (0.24%; 95% CI, 0.20%-0.28%), Black patients (0.22%; 95% CI, 0.19%-0.24%), and White patients (0.13%; 95% CI, 0.12%-0.14%).
Conclusions and Relevance
This cross-sectional study found that vitiligo diagnosis was more common in older patients, Hispanic/Latino patients, and Asian American patients.
Introduction
Vitiligo is an immune-mediated disease characterized by selective loss of melanocytes, resulting in depigmented patches commonly affecting visible areas of the body, including the face and hands.1,2 Vitiligo has profound consequences for quality of life and psychosocial well-being3,4 and is associated with comorbid conditions that may influence overall health.5,6
Information on incidence and prevalence, particularly among demographic subgroups, is limited. Vitiligo incidence in the US was assessed in a previous study.7 Population-based prevalence estimates vary considerably due to differences in study design and data collection methods (ie, patient-reported vs health record vs claims).8,9,10,11,12 Moreover, prevalence estimates among children are largely unknown, as previous estimates were from the 1970s.12 To help address these gaps, we estimated incidence and prevalence of diagnosed vitiligo in the US health care–seeking population and in demographic subgroups by age, sex, and race and ethnicity.
Methods
This analysis comprising a cohort study (incidence) and cross-sectional study (prevalence) was conducted using a 15% random sample of the IBM Explorys database, a multi–health system research platform containing electronic medical record data from over 40 integrated health care systems and approximately 53 million patients in the US.13 Incidence and prevalence of diagnosed vitiligo were studied separately in 2 cohorts of patients with an encounter in the database between January 1, 2015, and December 31, 2019 (incidence), and between January 1 and December 31, 2019 (prevalence). A 1-year baseline period of observable person-time was required prior to study follow-up to ensure adequate time for prevalent cases to be recorded. This study was deemed exempt from institutional review board approval by the Northwell Health Institutional Review Board due to the use of deidentified data. Therefore, informed consent was not required. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
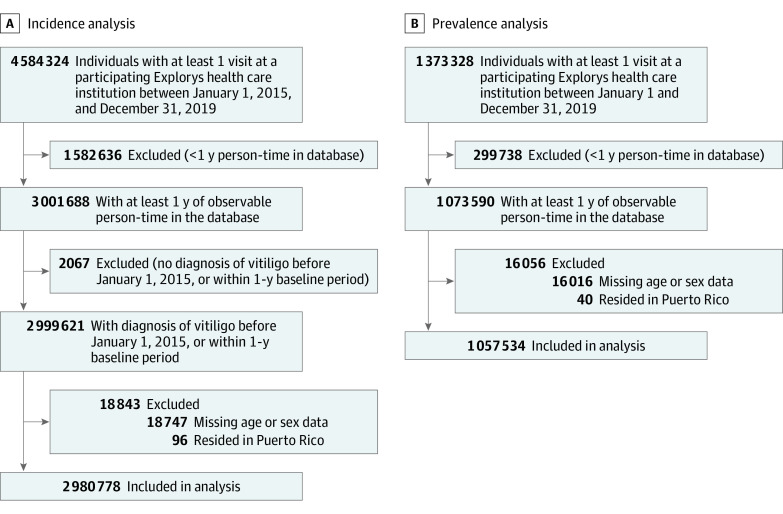
Vitiligo cases were identified based on 1 or more recorded International Classification of Diseases, Ninth Revision or International Statistical Classification of Diseases and Related Health Problems, Tenth Revision code (709.01 or L80). For incidence analysis, patients diagnosed with vitiligo before January 1, 2015, or within their first year of documented encounters in the database were excluded. Individuals with missing sex or age information were excluded (Figure).
Figure. Flowchart of Patients in the Incidence and Prevalence Analyses.
Incidence rate (IR) was calculated as the number of patients newly diagnosed with vitiligo divided by the total observable person-years (PY) of follow-up during the study period. Prevalence was calculated as the number of eligible patients ever diagnosed divided by total number of eligible patients during the study period. Crude and standardized incidence rates and prevalence were calculated for the overall sample and subgroups stratified by age, sex, and race and ethnicity. Race and ethnicity were based on patient self-report and included Asian American, Black, Hispanic/Latino, White, and other or multiracial; other included Asian/Pacific Islander, Native American or Alaska Native, Native Hawaiian, or other (not specified). Direct standardization, based on population estimates from the 2019 American Community Survey,14 was used to adjust incidence and prevalence estimates for age and sex to facilitate subgroup comparisons. Data were analyzed from December 13, 2022, to June 8, 2023. R, version 3.6.3 (R Foundation for Statistical Computing) was used for analysis.
Results
Incidence
There were 1605 patients newly diagnosed with vitiligo among 2 980 778 patients over a total follow-up of 7 081 566 PYs. Mean (SD) age of the total sample was 41.5 (24.0) years; 57.0% were female, 43.0% male, 1.4% Asian American, 12.9% Black, 1.5% Hispanic/Latino, 77.3% White, and 6.9% other or multiracial. The crude overall IR was 22.7 per 100 000 PY (95% CI, 21.6-23.8 per 100 000 PY). Age- and sex-adjusted overall IR was 22.6 per 100 000 PY (95% CI, 21.5-23.8 per 100 000 PY). Sex-adjusted IR generally increased with advancing age groups up to ages 60 to 69 years (25.3 per 100 000 PY; 95% CI, 22.2-28.6 per 100 000 PY). Crude and standardized IRs according to race and ethnicity are provided in Table 1. The highest age-adjusted IR was observed among Asian American patients (41.2 per 100 000 PY; 95% CI, 28.2-58.2 per 100 000 PY), followed by Hispanic/Latino patients (37.3 per 100 000 PY; 95% CI, 25.7-52.4 per 100 000 PY), patients reporting other or multiple races (31.1 per 100 000 PY; 95% CI, 25.9-37.1 per 100 000 PY), Black patients (29.6 per 100 000 PY; 95% CI, 26.0-33.6 per 100 000 PY), and White patients (18.7 per 100 000 PY; 95% CI, 17.5-20.0 per 100 000 PY).
Table 1. Incidence of Diagnosed Vitiligo Overall and by Sex, Age, and Race and Ethnicity From 2015 to 2019.
| Group | Vitiligo cases, No. | Patients, No. | Follow-up time, PY | Crude incidence rate, per 100 000 PY (95% CI) | Standardized incidence rate, per 100 000 PY (95% CI)a | Standardized incidence rate ratio, (95% CI)a |
|---|---|---|---|---|---|---|
| Overall | 1605 | 2 980 778 | 7 081 566 | 22.7 (21.6-23.8) | 22.6 (21.5-23.8) | NA |
| Sex | ||||||
| Female | 905 | 1 697 610 | 4 093 581 | 22.1 (20.7-23.6) | 21.9 (20.5-23.4) | 0.94 (0.85-1.03) |
| Male | 700 | 1 283 168 | 2 987 985 | 23.4 (21.7-25.2) | 23.4 (21.7-25.3) | 1 [Reference] |
| Age group, y | ||||||
| 0-17 (Pediatric) | 293 | 626 539 | 1 408 038 | 20.8 (18.5-23.3) | 20.8 (18.5-23.4) | 0.89 (0.79-1.01) |
| 0-9 | 162 | 373 329 | 808 543 | 20.0 (17.1-23.4) | 20.2 (17.2-23.5) | NA |
| 10-17 | 131 | 253 210 | 599 496 | 21.9 (18.3-25.9) | 21.9 (18.3-26.0) | NA |
| ≥18 (Adult) | 1312 | 2 354 239 | 5 673 527 | 23.1 (21.9-24.4) | 23.3 (22.1-24.6) | 1 [Reference] |
| 18-29 | 167 | 403 457 | 884 482 | 18.9 (16.1-22.0) | 19.3 (16.4-22.6) | NA |
| 30-39 | 195 | 352 656 | 812 244 | 24.0 (50.8-27.6) | 24.8 (20.8-27.6) | NA |
| 40-49 | 218 | 358 629 | 872 007 | 25.0 (21.8-28.5) | 24.7 (21.4-28.2) | NA |
| 50-59 | 272 | 432 337 | 1 090 563 | 24.9 (22.1-28.1) | 24.9 (22.0-28.1) | NA |
| 60-69 | 256 | 398 390 | 1 023 230 | 25.0 (22.0-28.3) | 25.3 (22.2-28.6) | NA |
| ≥70 | 204 | 408 770 | 991 001 | 20.6 (17.9-23.6) | 20.9 (18.1-24.0) | NA |
| Race and ethnicityb | ||||||
| Asian American | 33 | 36 886 | 77 686 | 42.5 (29.2-59.7) | 41.2 (28.2-58.2) | 2.20 (1.89-2.57) |
| Black | 252 | 333 794 | 851 482 | 30.0 (26.1-33.5) | 29.6 (26.0-33.6) | 1.58 (1.48-1.69) |
| Hispanic/Latino | 34 | 40 086 | 92 491 | 36.8 (25.5-51.4) | 37.3 (25.7-52.4) | 2.00 (1.71-2.32) |
| White | 916 | 2 002 447 | 4 827 627 | 19.0 (17.8-20.2) | 18.7 (17.5-20.0) | 1 [Reference] |
| Other or multiracialc | 126 | 177 964 | 405 268 | 31.1 (25.9-37.0) | 31.1 (25.9-37.1) | 1.66 (1.53-1.81) |
Abbreviations: NA, not applicable; PY, person-years.
Overall incidence was standardized by age and sex using the direct method and population estimates from the 2019 US Community Survey.14 Sex-specific and race-specific incidences were standardized by age. Age-specific incidences were standardized by sex.
Data were missing for 389 601 patients. Missing data were included in the estimates of vitiligo incidence for the overall group and sex and age subgroups.
Other included Asian/Pacific Islander, Native American or Alaska Native, Native Hawaiian, or other (not specified).
Prevalence
A total of 1 057 534 patients met inclusion criteria. Mean (SD) age was 43.4 (24.7) years; 57.5% were female, 42.5% male, 1.7% Asian American, 14.7% Black, 1.4% Hispanic/Latino, 75.7% White, and 6.6% other or multiracial. Of these patients, 1730 (0.16%; 95% CI, 0.16%-0.17%) had at least 1 code for vitiligo. Age- and sex-adjusted overall prevalence was 0.16% (95% CI, 0.15%-0.17%). Sex-adjusted prevalence increased with increasing age groups up to ages 40 to 49 years (0.19%; 95% CI, 0.16%-0.21%) and slightly increased thereafter in the group aged 70 years or older (0.21%; 95% CI, 0.19%-0.23%). Crude and standardized prevalence estimates according to race and ethnicity are provided in Table 2. The highest age-adjusted prevalence was observed among Hispanic/Latino patients (0.29%; 95% CI, 0.20%-0.39%), followed by Asian American patients (0.27%; 95% CI, 0.19%-0.35%), patients reporting other or multiple races (0.24%; 95% CI, 0.20%-0.28%), Black patients (0.22%; 95% CI, 0.19%-0.24%), and White patients (0.13%; 95% CI, 0.12%-0.14%).
Table 2. Prevalence of Diagnosed Vitiligo Overall and by Sex, Age, and Race and Ethnicity in 2019.
| Group | Vitiligo cases, No. | Patients, No. | Prevalence, % (95% CI) | Standardized prevalence ratio (95% CI)a | |
|---|---|---|---|---|---|
| Crude | Standardizeda | ||||
| Overall | 1730 | 1 057 534 | 0.16 (0.16-0.17) | 0.16 (0.15-0.17) | NA |
| Sex | |||||
| Female | 997 | 607 633 | 0.16 (0.15-0.17) | 0.16 (0.15-0.17) | 0.97 (0.88-1.07) |
| Male | 733 | 449 901 | 0.16 (0.15-0.18) | 0.16 (0.15-0.17) | 1 [Reference] |
| Age group, y | |||||
| 0-17 (Pediatric) | 233 | 226 306 | 0.10 (0.09-0.12) | 0.10 (0.09-0.12) | 0.57 (0.50-0.66) |
| 0-9 | 98 | 125 331 | 0.08 (0.06-0.10) | 0.08 (0.06-0.09) | NA |
| 10-17 | 135 | 100 975 | 0.13 (0.11-0.16) | 0.13 (0.11-0.16) | NA |
| ≥18 (Adult) | 1497 | 831 228 | 0.18 (0.17-0.19) | 0.18 (0.17-0.19) | 1 [Reference] |
| 18-29 | 161 | 121 955 | 0.13 (0.11-0.15) | 0.13 (0.11-0.15) | NA |
| 30-39 | 162 | 112 538 | 0.14 (0.12-0.17) | 0.15 (0.13-0.17) | NA |
| 40-49 | 212 | 115 873 | 0.18 (0.16-0.21) | 0.19 (0.16-0.21) | NA |
| 50-59 | 281 | 144 521 | 0.19 (0.17-0.22) | 0.19 (0.17-0.22) | NA |
| 60-69 | 301 | 156 531 | 0.19 (0.17-0.22) | 0.19 (0.17-0.21) | NA |
| ≥70 | 380 | 179 810 | 0.21 (0.19-0.23) | 0.21 (0.19-0.23) | NA |
| Race and ethnicityb | |||||
| Asian American | 45 | 15 422 | 0.29 (0.22-0.39) | 0.27 (0.19-0.35) | 2.01 (1.76-2.30) |
| Black | 294 | 130 173 | 0.23 (0.20-0.25) | 0.22 (0.19-0.24) | 1.62 (1.53-1.72) |
| Hispanic/Latino | 36 | 12 368 | 0.29 (0.21-0.40) | 0.29 (0.20-0.39) | 2.19 (1.89-2.54) |
| White | 956 | 672 092 | 0.14 (0.13-0.15) | 0.13 (0.12-0.14) | 1 [Reference] |
| Other or multiracialc | 142 | 58 293 | 0.24 (0.21-0.29) | 0.24 (0.20-0.28) | 1.81 (1.67-1.96) |
Abbreviation: NA, not applicable.
Overall prevalence was standardized by age and sex using the direct method and population estimates from the 2019 US Community Survey.14 Sex-specific and race-specific prevalence was standardized by age. Age-specific prevalence was standardized by sex.
Data were missing for 169 186 patients. Missing data were included in the estimates of vitiligo prevalence for the overall group and sex and age subgroups.
Other included Asian/Pacific Islander, Native American or Alaska Native, Native Hawaiian, or other (not specified).
Discussion
This study represents one of the largest and most robust epidemiologic descriptions of vitiligo in the US. Based on the estimated US population size in 2019,14 this analysis suggests that there are approximately 528 000 prevalent cases and 74 600 new cases per year. Incident and prevalent cases were highest in older individuals. Prevalence rates were nearly double in adults compared with pediatric patients. Observed age-related trends may be associated with increased health care utilization among older individuals. There were no significant differences in incidence and prevalence of diagnosed vitiligo between males and females.
This study found an increased rate of diagnosed vitiligo among racial and ethnic minority populations, who also may experience the greatest disease-related effects on quality of life.4 Among Asian American and Hispanic/Latino patients, rates of diagnosed vitiligo were approximately twice as high as rates for White patients. The greater disease burden in racial and ethnic minority populations may partially be explained by easier detection or increased psychosocial burden leading to clinical evaluation. Rates among racial and ethnic minority patients may also have been underestimated if there was differential access to care.
To our knowledge, the only previous incidence estimate in the US was from the Nurses’ Health Study 2, in which female nurses self-reported diagnosis.7 Incidence between 2009 and 2011 was approximately 51 per 100 000 PY, over twice the present estimate. Increased incidence among nurses may be partially attributable to higher health literacy in this population. Results, however, were subject to selection bias and are not generalizable due to the substantial sample homogeneity.
Vitiligo prevalence estimates in the US range from 0.05% to 1.4% depending on the study population and sampling methods.3,8,9,10,11,12 In 2 cross-sectional studies, prevalence based on self-report was 1.4%.3,8 In 1 of these studies, prevalence was reduced to 0.76% after adjudication of photographs from a subsample by clinicians experienced in vitiligo.8 However, only a small proportion (20.1%) of patients submitted photographs, and vitiligo could not be verified in approximately 45% of these photographs.8 Self-reported prevalence was 1.53 and 1.30 times as high among Black and Asian patients, respectively, compared with White patients.8
The prevalence estimate using health record data from the All of Us Research Program, an initiative with a focus on historically underrepresented groups, was 0.33%.9,15 Hispanic individuals had the highest adjusted odds of diagnosis compared with White patients (odds ratio [OR], 2.25; 95% CI, 1.87-2.71), followed by Black patients (OR, 1.71; 95% CI, 1.40-2.08) and patients reporting other race (OR, 1.60; 95% CI, 1.22-2.08).9 The All of Us Research Program requires participants to self-enroll online, potentially resulting in selection bias.15 Moreover, estimates may not be applicable to the overall US population owing to its focus on underrepresented groups and overrepresentation of older individuals.15
Pediatric-specific prevalence estimates from the first National Health and Nutrition Examination Survey in the early 1970s ranged from 0.02% to 0.67% among patients aged 1 to 17 years.12 Estimate variation was likely due to the small number of included cases.
Strengths and Limitations
Strengths of this study include the large sample size, demographic diversity, patient-reported race and ethnicity data, and standardization of estimates using age- and sex-specific strata, all of which support generalizability. We also report incidence estimates for, to our knowledge, previously unexamined demographic groups, including pediatric patients and racial and ethnic groups.
A limitation of this study is that it only captured patients who sought care in health systems included in the database. Since not all patients with vitiligo seek care, estimates may underreport overall burden and may overrepresent greater disease severity. There is a paucity of evidence regarding validity of coded algorithms to identify cases. Missing race or ethnicity data may bias subgroup estimates if missingness was related to both race and ethnicity and presence of vitiligo. However, comparisons between racial and ethnic groups were similar to those in previous studies.8,9
Conclusions
This study found a vitiligo prevalence of 0.2% and incidence of 22.6 per 100 000 PY. Diagnosis was more common in older patients and racial and ethnic minority patients, particularly Hispanic and Asian American individuals. These observations may support improving awareness of vitiligo disease burden in medical and public sectors, informing research agendas, improving enrollment of racial and ethnic minority populations in trials, and developing health policies.
Data Sharing Statement
References
- 1.Picardo M, Dell’Anna ML, Ezzedine K, et al. Vitiligo. Nat Rev Dis Primers. 2015;1:15011. doi: 10.1038/nrdp.2015.11 [DOI] [PubMed] [Google Scholar]
- 2.Rodrigues M, Ezzedine K, Hamzavi I, Pandya AG, Harris JE; Vitiligo Working Group . New discoveries in the pathogenesis and classification of vitiligo. J Am Acad Dermatol. 2017;77(1):1-13. doi: 10.1016/j.jaad.2016.10.048 [DOI] [PubMed] [Google Scholar]
- 3.Bibeau K, Pandya AG, Ezzedine K, et al. Vitiligo prevalence and quality of life among adults in Europe, Japan and the USA. J Eur Acad Dermatol Venereol. 2022;36(10):1831-1844. doi: 10.1111/jdv.18257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ezzedine K, Eleftheriadou V, Jones H, et al. Psychosocial effects of vitiligo: a systematic literature review. Am J Clin Dermatol. 2021;22(6):757-774. doi: 10.1007/s40257-021-00631-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadi A, Wang JF, Uppal P, Penn LA, Elbuluk N. Comorbid diseases of vitiligo: a 10-year cross-sectional retrospective study of an urban US population. J Am Acad Dermatol. 2020;82(3):628-633. doi: 10.1016/j.jaad.2019.07.036 [DOI] [PubMed] [Google Scholar]
- 6.Gill L, Zarbo A, Isedeh P, Jacobsen G, Lim HW, Hamzavi I. Comorbid autoimmune diseases in patients with vitiligo: a cross-sectional study. J Am Acad Dermatol. 2016;74(2):295-302. doi: 10.1016/j.jaad.2015.08.063 [DOI] [PubMed] [Google Scholar]
- 7.Drucker AM, Thompson JM, Li WQ, et al. Incident alopecia areata and vitiligo in adult women with atopic dermatitis: Nurses’ Health Study 2. Allergy. 2017;72(5):831-834. doi: 10.1111/all.13128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gandhi K, Ezzedine K, Anastassopoulos KP, et al. Prevalence of vitiligo among adults in the United States. JAMA Dermatol. 2022;158(1):43-50. doi: 10.1001/jamadermatol.2021.4724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmed F, Moseley I, Ragi SD, Ouellette S, Rao B. Vitiligo in underrepresented communities: an All of Us database analysis. J Am Acad Dermatol. 2022;S0190-9622(22)03074-2. doi: 10.1016/j.jaad.2022.11.027 [DOI] [PubMed] [Google Scholar]
- 10.Lim HW, Collins SAB, Resneck JS Jr, et al. The burden of skin disease in the United States. J Am Acad Dermatol. 2017;76(5):958-972.e2. doi: 10.1016/j.jaad.2016.12.043 [DOI] [PubMed] [Google Scholar]
- 11.Bickers DR, Lim HW, Margolis D, et al. ; American Academy of Dermatology Association; Society for Investigative Dermatology . The burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. J Am Acad Dermatol. 2006;55(3):490-500. doi: 10.1016/j.jaad.2006.05.048 [DOI] [PubMed] [Google Scholar]
- 12.Johnson MT, Roberts J. Skin conditions and related need for medical care among persons 1-74 years: United States, 1971-1974. Vital Health Stat 11. 1978;(212):i-v, 1-72. [PubMed] [Google Scholar]
- 13.IBM Watson Health . The IBM Explorys Platform: liberate your healthcare data. Accessed December 22, 2022. https://www.ibm.com/downloads/cas/4P0QB9JN
- 14.US Census Bureau . 2019 American Community Survey 1-year estimates detailed tables: sex by age (B01001). Accessed March 25, 2022. https://data.census.gov/cedsci/table?q=american%20community%20survey%20b01001&tid=ACSDT1Y2019.B01001.
- 15.Denny JC, Rutter JL, Goldstein DB, et al. ; All of Us Research Program Investigators . The “All of Us” Research Program. N Engl J Med. 2019;381(7):668-676. doi: 10.1056/NEJMsr1809937 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement