Abstract
Background
Cardiac involvement is a main determinant of mortality in light chain (AL) amyloidosis but data on survival of patients with cardiac AL amyloidosis proven by endomyocardial biopsy (EMB) are sparse.
Methods
This study analysed clinical, laboratory, electrocardiography and echocardiographic parameters for their prognostic value in the assessment of patients with AL amyloidosis and cardiac involvement. Patients with AL amyloidosis who had their first visit to the amyloidosis centre at the University Hospital Heidelberg between 2006 and 2017 (n=1628) were filtered for cardiac involvement proven by EMB. In the final cohort, mortality-associated markers were analysed by univariate and multivariable Cox regression. Cut-off values for each parameter were calculated using the survival time.
Results
One-hundred and seventy-four patients could be identified. Median overall survival time was 1.5 years and median follow-up time was 5.2 years. At the end of the investigation period, 115 patients had died. In multivariable analysis, New York Heart Association-functional class >II (HR 1.65; 95% CI 1.09 to 2.50; p=0.019), left ventricular global longitudinal strain (HR 1.12; 95% CI 1.03 to 1.22; p=0.007), left ventricular end-systolic volume (HR 1.02; 95% CI 1.01 to 1.03; p=0.001), systolic pulmonary artery pressure (HR 0.98; 95% CI 0.96 to 0.99; p=0.027), N-terminal pro-B-type natriuretic peptide (HR 1.57; 95% CI 1.17 to 2.11; p=0.003) and difference in free light chains (HR 1.30; 95% CI 1.05 to 1.62; p=0.017) were independently predictive.
Conclusion
Among all patients with AL amyloidosis those with cardiac involvement represent a high-risk population with limited therapy options. Therefore, accurate risk stratification is necessary to identify cardiac amyloidosis patients with favourable prognosis. Incorporation of modern imaging techniques into existing or newly developed scoring systems is a promising option that might enable the implementation of risk-adapted therapeutic strategies.
Keywords: Cardiomyopathy, Restrictive; Heart Failure, Systolic; Echocardiography
WHAT IS ALREADY KNOWN ON THIS TOPIC
Among all patients with light chain (AL) amyloidosis those with cardiac involvement represent a high-risk population with limited therapy options. Although current staging systems are powerful prognostic tools for AL amyloidosis in general, the prediction of survival in patients with cardiac involvement is not equally well investigated and patient data for endomyocardial biopsy-proven cardiac AL amyloidosis is sparse.
WHAT THIS STUDY ADDS
This study could demonstrate that a relevant number of patients with cardiac amyloidosis shows long-term survival over many years. To separate patients according to prognosis, we identified different clinical, laboratory and echocardiography parameters that are independent predictors of survival in cardiac AL amyloidosis.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Strain imaging holds great potential to identify cardiac amyloidosis patients with favourable prognosis as it provides direct and objective read-outs on cardiac structure and function. Modern imaging techniques might, therefore, be incorporated into existing or newly developed scoring systems to enable the implementation of risk-adapted therapeutic strategies.
Introduction
Amyloidosis comprises a group of diseases characterised by extracellular deposition of amyloid, a fibrillar aggregation of at least 30 different misfolded precursor proteins.1 Light chain (AL) amyloidosis accounts for more than three-quarters of cases in patients with systemic amyloidosis and among those, another 75% suffer from cardiac involvement.2 With an incidence of 1.2 cases per 100 000 person-years, AL amyloidosis is a rare disease, but a trend towards higher incidence rates with time might reflect an increased awareness of the disease and diagnostic improvements.3 4 Nevertheless, up to 37% of patients are diagnosed more than 1 year after the onset of initial symptoms.5
In the case of AL amyloidosis, cardiac deposition of misfolded immunoglobulin light chain-derived amyloid fibrils disrupts tissue integrity and causes stiffening of the myocardium eventually leading to restrictive cardiomyopathy and congestive heart failure (HF).6 Prefibril oligomers, in addition, have direct toxic effects on cardiomyocytes and thus amplify organ dysfunction even further.7–12
Amyloid deposits and myocardial injury can cause elevation of cardiac biomarkers such as N-terminal pro-brain natriuretic peptide (NT-proBNP) or cardiac troponins.13–15 These biomarkers have accordingly been incorporated into different risk classification scores.16–19 While these staging systems are powerful prognostic tools for AL amyloidosis in general, the prediction of survival in patients with endomyocardial biopsy (EMB) proven cardiac involvement is not equally well investigated.
Cardiac involvement is commonly associated with a poor prognosis of AL amyloidosis. Although new therapy options have improved overall survival (OS) over the last two decades,20 mortality is still high among patients with confirmed or suspected cardiac involvement and after onset of HF, outcome continues to deteriorate.21 However, some high-risk patients survive even for years,22 23 raising the question whether variables not included in the established scoring systems may indicate a potentially superior therapy response and survival. Therefore, we investigated the predictive value of different clinical, laboratory, electrocardiography and echocardiograpic parameters in an initially therapy-naïve cohort of patients with AL amyloidosis and cardiac involvement proven by EMB.
Methods
Study design and population
The present study is a single-centre investigation based on register datasets collected at the amyloidosis centre of the University Hospital Heidelberg, Germany. The records of all patients with AL amyloidosis who had their initial visit from 27 July 2006 to 27 December 2017 were filtered for cardiac involvement that was confirmed by an EMB. In our cardiology department EMB was performed in patients referred for further invasive HF diagnostics when coronary artery disease could be excluded during heart catheterisation or in case of uncertainty of cardiac amyloidosis based on basic diagnostics (eg, imaging, biomarkers) collected in the haematology or cardiology department.
To exclude a potential bias caused by former amyloidosis treatment or by diseases other than amyloidosis that would lead to altered functional imaging parameters and elevated cardiac biomarkers, patients who were already on chemotherapy for AL amyloidosis at the time of presentation and patients with significant cardiovascular or renal comorbidities were excluded from further analysis. To ensure optimal conditions for echocardiographic measurements, in particular strain imaging, only patients in sinus rhythm and with sufficient image quality were included.
Diagnosis of AL amyloidosis and cardiac involvement
Monoclonal gammopathy was confirmed by immunoelectrophoresis and immunofixation of serum and urine. Systemic AL amyloidosis with cardiac involvement was verified by light-microscopy immunohistochemistry and Congo red staining of myocardial biopsies showing green birefringence under polarised light.
Clinical, laboratory, electrocardiography and echocardiography assessment
Data on demographics, medical history, physical examination, blood samples and urine samples were collected on the day of first presentation at the Heidelberg University Hospital. Additionally, a 12-lead ECG and a comprehensive echocardiography examination were performed in every patient.
Electrocardiography was analysed for heart rhythm and heart rate, cardiac axis, time intervals and low-QRS-voltage pattern (QRS complex amplitude <5 mm in any limb lead).
Echocardiography examinations were conducted using commercially available ultrasound machines (Vivid E9 BT 11, GE Vingmed Ultrasound, Horten, Norway and iE33, Philips Medical Systems, Andover, Massachusetts, USA). Three consecutive heart cycles were acquired for each two-dimensional image, with a sampling rate of 55–60 frames/s. Offline analysis was conducted according to the recommendation of the American Society of Echocardiography and the European Association of Cardiovascular Imaging24 using Image Arena including the 2D cardiac performance analysis software (TOMTEC Imaging Systems, Unterschleissheim, Germany).
Follow-up data were retrieved from digital clinical records and/or telephone interviews with the patients, their relatives or their family doctors.
Statistical analysis
The study cohort was described using summary measures of the empirical distribution. Nominal variables are reported as absolute and relative frequencies and continuous variables are given as medians with 25% and 75% quantiles. In the comparison of survivors and nonsurvivors, for nominal variables, the χ2-test was used, and for continuous variables, the t-test for independent groups or the Mann-Whitney-Wilcoxon-test was used, as appropriate.
OS was investigated using the Kaplan-Meier estimator and the median follow-up was calculated with the reverse Kaplan-Meier method. The variables’ association with OS was examined by calculating HRs applying univariate Cox regression models, whereby NT-proBNP, high sensitivity Troponin T (hsTnT) and difference of free light chains (dFLC) were log-transformed due to their highly skewed distributions. For multivariable Cox regression modelling, the missing values (occurring in total in 1.82% of the investigated variables) were multiple (n=50) imputed. On each imputed dataset, forward selection using Cox regression was performed. In each step, the coefficients were pooled using Rubins’s rules and variable selection was done by using a criterion of p<0.1 for the pooled regression coefficients.25
Optimal cut-off values for risk stratification were calculated by optimising the log-rank test statistic and a 95% bootstrap CI was computed as certainty measure.26
Since this was a retrospective data analysis, all p values should be interpreted in a descriptive manner; p values<0.05 were accepted as significant. All statistical analyses were performed using the software R V.≥4.10.2.
Results
From 27 July 2006 to 27 December 2017, 1628 patients with AL amyloidosis had initial contact with the amyloidosis centre at the University Hospital Heidelberg. Figure 1 depicts a flow chart of the inclusion and exclusion criteria for this study. Only patients who were chemotherapy naïve for AL amyloidosis were included. Cardiac involvement was confirmed by EMB in 216 cases. To minimise the impact of confounders, patients with known cardiovascular (atrial fibrillation n=2, cardiac decompensation n=2, complete heart block n=2, pacemaker n=10, former heart surgery n=2, heart transplantation during follow-up n=8) or severe kidney disease (renal artery stenosis n=1, acute kidney failure n=2, dialysis n=2) as well as patients with suboptimal echocardiography image quality (n=11), were excluded. The final study population consisted of 174 patients. At the end of the follow-up period in August 2021, 115 patients had died.
Figure 1.
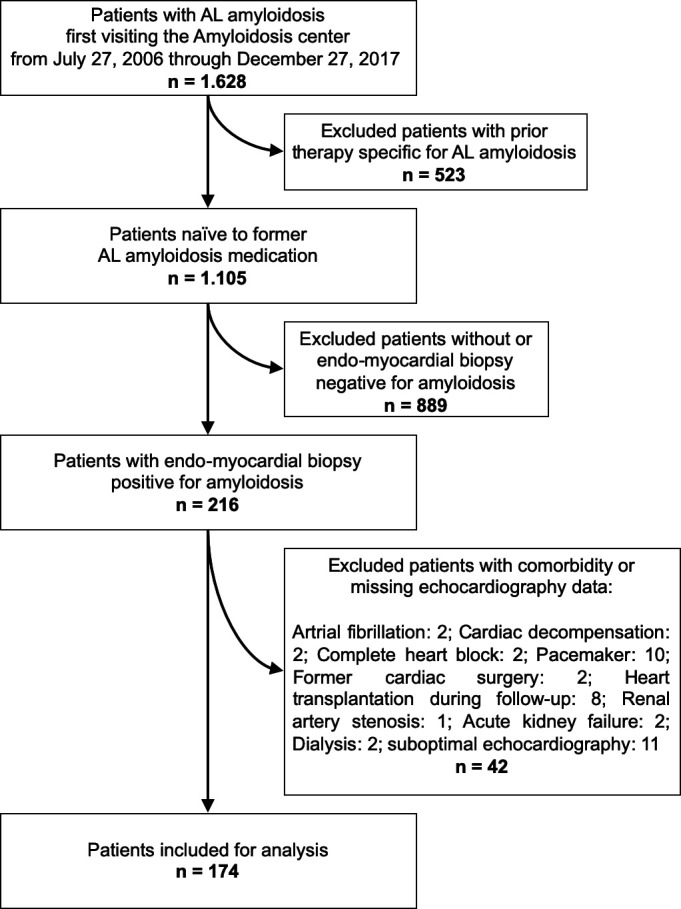
Flow chart of the inclusion and exclusion criteria of the study. AL, amyloid light chain.
Characteristics of the study population
The clinical, laboratory, electrocardiography and echocardiograpic parameters of the entire study cohort, of survivors and non-survivors are summarised in table 1. Male subjects predominated. Survivors had higher systolic blood pressure and estimated glomerular filtration rate (eGFR) whereas New York Heart Association functional class (NYHA-FC), serum levels of dFLC, NT-proBNP, hsTnT, left ventricular (LV) global longitudinal strain and the ratio of E/e’ were lower. Furthermore, pericardial effusion was less often detected in survivors. Online supplemental table 1 compares patients who survived at least 1 year with patients who died within 1 year after initial presentation, excluding censored cases. Cardiac staging according to the MAYO 3b18 score is presented in table 2. Among survivors most patients were in stages II and III and among non-survivors most patients were in stages III and IIIb. None of the patients met the criteria for stage I.
Table 1.
Characteristics of the study population
| Parameter | Survivors (n=59) | Non-survivors (n=115) | Total (n=174) | P value |
| Basic and clinical data | ||||
| Male sex, n (%) | 32 (54) | 81 (70) | 113 (65) | 0.034 |
| Age, years | 62 (53; 68) | 63 (56; 70) | 63 (55; 69) | 0.369 |
| Hight, cm | 171(165; 183) | 176 (168; 181) | 175 (166; 182) | 0.344 |
| Weight, kg | 78 (65; 86) | 77 (66; 84) | 77 (66; 85) | 0.963 |
| Systolic blood pressure, mm Hg | 110 (105; 125) | 110 (110; 120) | 110 (110; 120) | 0.030 |
| Diastolic blood pressure, mm Hg | 75 (70; 80) | 70 (65; 80) | 70 (65; 80) | 0.080 |
| NYHA-FC>II, n (%) | 26 (44) | 76 (66) | 102 (59) | 0.005 |
| Clinical chemistry | ||||
| Light chain type Lambda, n (%) | 53 (90) | 96 (83) | 149 (86) | 0.258 |
| dFLC, mg/L | 274 (141; 415) | 325 (155; 711) | 300 (152; 589) | 0.033 |
| NT-proBNP, ng/L | 4528 (2472; 8482) | 7516 (5046; 13 419) | 6894 (3333; 11 119) | <0.001 |
| hsTnT, pg/mL | 57 (40; 89) | 86 (48; 138) | 71 (43; 126) | 0.010 |
| eGFR, mL/min/1.73 m2 | 81 (72;93) | 74 (62;93) | 77 (64;93) | 0.036 |
| ECG | ||||
| Sinus rhythm, n (%) | 56 (100) | 115 (100) | 174 (100) | – |
| Heart rate, s-1 | 78 (69; 90) | 82 (74; 91) | 81 (71; 90) | 0.452 |
| Heart axis | 0.871 | |||
| Normal heart axis, n (%) | 22 (37) | 39 (34) | 61 (35) | |
| Left axis deviation, n (%) | 26 (44) | 55 (48) | 81 (47) | |
| Right axis deviation, n (%) | 11 (19) | 20 (18) | 31 (18) | |
| PQ interval, ms | 186 (166; 216) | 178 (158; 208) | 180 (160; 210) | 0.348 |
| QRS interval, ms | 96 (88; 112) | 100 (90; 112) | 98 (90; 112) | 0.792 |
| QTc interval, ms | 441 (421; 457) | 437 (419; 456) | 439 (419; 456) | 0.656 |
| Low-QRS-voltage pattern, n (%) | 20 (34) | 53 (47) | 73 (42) | 0.101 |
| Echocardiogram | ||||
| LV-Septum, mm | 17 (15; 20) | 17 (15; 20) | 17 (15; 20) | 0.377 |
| LV-posterior wall, mm | 16 (13; 17) | 15 (13; 18) | 15 (13; 18) | 0.694 |
| LV-EDD, mm | 41 (38; 44) | 41 (38; 46) | 41 (38; 45) | 0.697 |
| LV-ESD, mm | 31 (27; 34) | 31 (28; 37) | 31 (27; 35) | 0.329 |
| LV-mass/BSA, g/m² | 143 (119; 164) | 150 (124; 182) | 147 (124; 180) | 0.388 |
| LV-EDV, mL | 75 (57; 90) | 78 (60; 96) | 77 (60; 94) | 0.146 |
| LV-ESV, mL | 36 (25; 46) | 39 (32; 54) | 38 (29; 50) | 0.075 |
| Ejection fraction, % | 51 (44; 56) | 49 (41; 55) | 49 (43; 55) | 0.120 |
| MAPSE, mm | 9 (7; 11) | 8 (7; 10) | 9 (7; 10) | 0.138 |
| TAPSE, mm | 15(12; 20) | 15 (11; 19) | 15 (11; 19) | 0.419 |
| LV-GLS, % | −9.1 (−12; −7.1) | −8.1(−10; −6.4) | −8.4 (−10; −6.5) | 0.013 |
| RV-GLS, % | −15 (−20; −12) | −15 (−17; −10) | −15 (−19; −11) | 0.201 |
| Relative apical sparing, n (%) | 23 (39) | 52 (45) | 75 (43) | 0.432 |
| LA-volume/BSA, mL/m² | 44 (34; 55) | 45 (32; 53) | 44 (33; 54) | 0.896 |
| E-wave/A-wave | 2.3 (1; 3.2) | 2.6 (1.5; 3.4) | 2.5 (1.4; 3.3) | 0.191 |
| E-wave/e‘-wave | 16 (12; 20) | 18 (13; 22) | 17 (13; 22) | 0.017 |
| E-wave deceleration time, ms | 158 (142; 206) | 167 (135; 196) | 164 (137; 206) | 0.992 |
| sPAP, mm Hg | 40 (32; 46) | 39 (32; 46) | 39 (32; 46) | 0.602 |
| Pericardial effusion, n (%) | 12 (20) | 40 (35) | 52 (30) | 0.049 |
Results are given as number (percentage) or median (25th; 75th percentile).
BSA, body surface area; dFLC, difference of free light chains; EDD, end-diastolic diameter; EDV, end-diastolic volume; eGFR, estimated glomerular filtration rate; ESD, end-systolic diameter; ESV, end-systolic volume; GLS, global longitudinal strain; hsTnT, high sensitivity troponin T; LV, left ventricle; MAPSE, mitral annular plane systolic excursion; NT-proBNP, N-terminal pro-B-type natriuretic peptide; NYHA-FC, New York Heart Association functional class; RV, right ventricle; sPAP, systolic pulmonary artery pressure; TAPSE, tricuspid annular plane systolic excursion.
Table 2.
Cardiac staging according to the MAYO 3b Score18
| MAYO 3b stage | Survivors (n=59) |
Non-survivors (n=115) |
Total (n=174) |
P value |
| I | – | – | – | 0.016 |
| II | 25 (43) | 27 (24) | 52 (30) | |
| III | 22 (37) | 45 (39) | 67 (39) | |
| IIIb | 12 (20) | 43 (37) | 55 (31) |
None of the patients was in MAYO 3b stage I. Results are given as number (percentage).
openhrt-2023-002310supp001.pdf (61.7KB, pdf)
In addition to cardiac involvement, at least one other organ was affected in 41% of the patients, and at least two other organs were affected in 10%. Soft tissue was the second most often involved organ system (24%), followed by gastrointestinal system and kidneys (17% and 6%, respectively). In our study, no difference was observed in the type or number of organs involved between survivors and non-survivors (online supplemental table 2). There was also no difference between both groups with regard to the underlying haematological disease. However, survivors had lower bone marrow plasma cell infiltration (online supplemental table 3).
Throughout the follow-up period, 94% of the patients received specific AL amyloidosis therapy. The therapy regimens are shown in online supplemental table 4. Bortezomib plus dexamethasone was the most frequently used treatment (53%). Other drugs commonly used in various combinations were cyclophosphamide, lenalinomide and melphalan. Bendamustine, doxorubicin and rituximab were ordered less often. One patient received stem cell transplantation (SCT). All others were classified as unsuitable for SCT due to advanced cardiac involvement. Ten patients remained untreated, all of whom belonged to the non-survivor group (five died before the therapy decision, three refused therapy, two were too old and in a significantly reduced general condition).
Survival analysis
The median OS time was 1.47 years (95% CI 1.04 to 2.92) or 17.6 moths (95% CI 12.5 to 35) figure 2. The median follow-up time was 5.16 years (95% CI 4.35 to 7.22) or 61.9 months (95% CI 52.2 to 86.6). The results of univariate Cox regression analysis and the final multivariable Cox regression model resulting from variable selection are presented in table 3. Male sex, blood pressure, NYHA-FC, low-voltage pattern (LVP), LV end-systolic volume (ESV), LV ejection fraction (EF), longitudinal ventricular function, pericardial effusion, NT-proBNP, hsTnT, dFLC and eGFR were associated with poor outcome, but only LV global longitudinal strain (HR 1.12; 95% CI 1.03 to 1.22; p=0.007), LV-ESV (HR 1.02; 95% CI 1.01 to 1.03; p=0.001), systolic pulmonary artery pressure (HR 0.98; 95% CI 0.96 to 0.99; p=0.027), NYHA-FC>II (HR 1.65; 95% CI 1.09 to 2.50; p=0.019), NT-proBNP (HR 1.57; 95% CI 1.17 to 2.11; p=0.003) and dFLC (HR 1.30; 95% CI 1.05 to 1.62; p=0.017) were independently predictive in the final Cox regression model.
Figure 2.

Kaplan-Meier curve displaying overall survival of the complete study cohort. Median survival time was 1.47 years.
Table 3.
Univariate and multivariable Cox regression analysis
| Parameter | Univariate Cox regression | Multivariable Cox regression | ||||
| HR | 95% CI | P value | HR | 95% CI | P value | |
| Male sex | 1.641 | 1.096 to 2.456 | 0.016 | |||
| Age, years | 1.007 | 0.987 to 1.026 | 0.513 | 1.009 | 0.988 to 1.030 | 0.407 |
| Height, cm | 1.014 | 0.996 to 1.032 | 0.137 | |||
| Weight, kg | 1.007 | 0.995 to 1.019 | 0.242 | |||
| Systolic blood pressure, mm Hg | 0.984 | 0.973 to 0.995 | 0.003 | |||
| Diastolic blood pressure, mmHg | 0.977 | 0.960 to 0.995 | 0.011 | |||
| NYHA-FC>II | 1.941 | 1.315 to 2.867 | 0.001 | 1.637 | 1.081 to 2.479 | 0.020 |
| Light chain type lambda | 0.747 | 0.456 to 1.224 | 0.247 | |||
| dFLC-log, mg/L | 1.410 | 1.161 to 1.713 | 0.001 | 1.333 | 1.076 to 1.650 | 0.009 |
| NT-proBNP-log, ng/L | 1.989 | 1.554 to 2.546 | <0.001 | 1.714 | 1.291 to 2.276 | <0.001 |
| hsTnT-log, pg/mL | 1.563 | 1.188 to 2.058 | 0.001 | |||
| eGFR, mL/min/1.73 m2 | 0.985 | 0.977 to 0.994 | 0.001 | |||
| Heart rate/s | 1.011 | 0.998 to 1.025 | 0.095 | |||
| Normal heart axis (reference) | ||||||
| Left axis deviation | 1.227 | 0.814 to 1.851 | 0.329 | |||
| Right axis deviation | 1.117 | 0.651 to 1.916 | 0.687 | |||
| PQ interval, ms | 0.998 | 0.992 to 1.003 | 0.385 | |||
| QRS interval, ms | 1.004 | 0.994 to 1.013 | 0.428 | |||
| QTc interval, ms | 0.998 | 0993 to 1.004 | 0.535 | |||
| Low-QRS-voltage pattern | 1.842 | 1.269 to 2.672 | 0.001 | |||
| LV-septum, mm | 1.053 | 0.995 to 1.115 | 0.074 | |||
| LV-posterior wall, mm | 1.041 | 0.970 to 1.117 | 0.266 | |||
| LV-EDD, mm | 1.000 | 0.972 to 1.029 | 0.993 | |||
| LV-ESD, mm | 1.021 | 0.995 to 1.048 | 0.117 | |||
| LV-mass/BSA, g/m2 | 1.002 | 0.998 to 1.007 | 0.372 | |||
| LV-EDV, mL | 1.004 | 0.997 to 1.011 | 0.240 | |||
| LV-ESV, mL | 1.014 | 1.003 to 1.025 | 0.009 | 1.021 | 1.009 to 1.033 | 0.001 |
| Ejection fraction, % | 0.967 | 0.949 to 0.985 | <0.001 | |||
| MAPSE | 0.904 | 0.841 to 0.973 | 0.007 | |||
| TAPSE | 0.950 | 0.913 to 0.989 | 0.012 | |||
| LV-GLS | 1.151 | 1.073 to 1.235 | <0.001 | 1.117 | 1.032 to 1.210 | 0.007 |
| RV-GLS | 1.036 | 1.002 to 1.072 | 0.040 | |||
| Relative apical sparing | 1.332 | 0.921 to 1.926 | 0.127 | |||
| LA-Volumen/BSA, mL/m2 | 1.002 | 0.991 to 1.014 | 0.688 | |||
| E-wave/A-wave | 1.192 | 1.018 to 1.395 | 0.029 | |||
| E-wave/e‘-wave | 1.022 | 1.000 to 1.044 | 0.055 | |||
| E-wave Deceleration time, ms | 0.999 | 0.995 to 1.002 | 0.462 | |||
| sPAP, mm Hg | 0.995 | 0.978 to 1.013 | 0.582 | 0.975 | 0.955 to 0.995 | 0.016 |
| Pericardial effusion | 1.661 | 1.128 to 2.447 | 0.010 | |||
| Organs involved >1 | 0.913 | 0.629 to 1.326 | 0.632 | |||
| Organs involved >2 | 0.849 | 0.466 to 1.547 | 0.593 | |||
BSA, body surface area; dFLC, difference of free light chains; EDD, end-diastolic diameter; EDV, end-diastolic volume; eGFR, estimated glomerular filtration rate; ESD, end-systolic diameter; ESV, end-systolic volume; GLS, global longitudinal strain; hsTnT, high sensitivity troponin T; LV, left ventricle; MAPSE, mitral annular plane systolic excursion; NT-proBNP, N-terminal pro-B-type natriuretic peptide; NYHA-FC, New York Heart Association functional class; RV, right ventricle; sPAP, systolic pulmonary artery pressure; TAPSE, tricuspid annular plane systolic excursion.
Cut-off calculation and risk stratification
For all continuous parameters that were independent predictors of mortality in the final Cox regression model, their individual optimal cut-off values were computed (table 4). Corresponding Kaplan-Meier curves using the identified thresholds of NT-proBNP (5762 ng/L), global longitudinal strain (−8.9%), LV-ESV (43 mL), systolic pulmonary artery pressure (28 mm Hg) and dFLC (439 mg/L) for stratification are presented in figure 3A–F. Based on the aforementioned cut-off values a staging system incorporating global longitudinal strain and NT-proBNP was developed. The resulting stratification of our study population into three patient cohorts with low (both parameters below the threshold), intermediate (one of the two parameters above the threshold) and high risk (both parameters above the threshold) is shown in figure 4.
Table 4.
Cut-off values for risk stratification with corresponding 95% bootstrap percentile of continuous variables
| Parameter | Optimal cut-off | 2.5% | 97.5% |
| GLS, % | −8.9 | −10.2 | −6.5 |
| LV-ESV, mL | 43 | 22 | 62 |
| sPAP, mm Hg | 28 | 28 | 53 |
| NT-proBNP, ng/L | 5762 | 4337 | 8840 |
| dFLC, mg/L | 439 | 220 | 537 |
dFLC, difference of free light chains; GLS, global longitudinal strain; LV-ESV, left ventricular end-systolic volume; NT-proBNP, N-terminal pro-B-type natriuretic peptide; sPAP, systolic pulmonary artery pressure.
Figure 3.
Kaplan-Meier curves displaying the survival probability according to parameters that were independent predictors in the multivariable Cox regression analysis. Stratification was done using individually calculated thresholds for each parameter. dFLC, difference of free light chains; ESV, end-systolic volume; LV-GLS, left ventricular-global longitudinal strain; NT-proBNP, N-terminal pro-brain natriuretic peptide; NYHA-FC, New York Heart Association functional class; sPAP, systolic pulmonary artery pressure.
Figure 4.
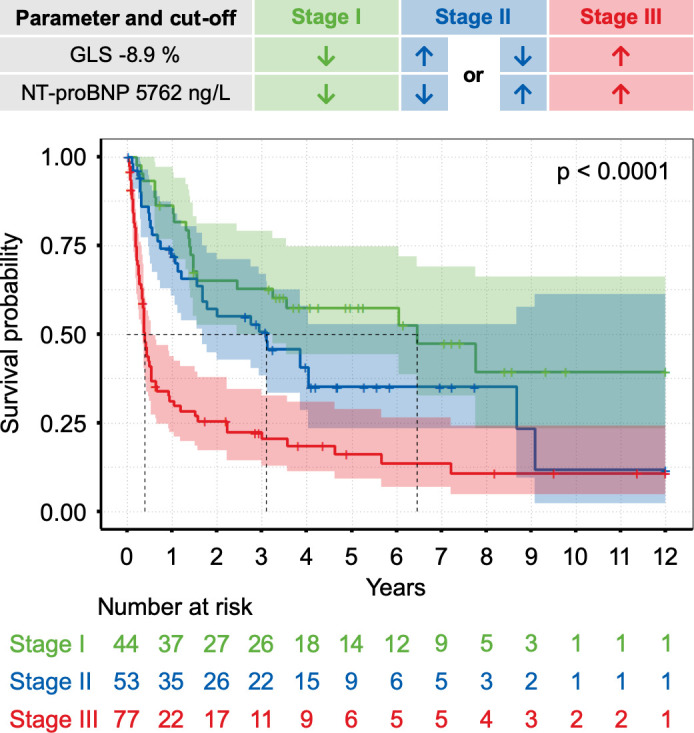
Risk stratification based on a scoring system incorporating N-terminal pro-B-type natriuretic peptide (NT-proBNP) and global longitudinal strain (GLS). The thresholds were 5762 ng/L for NT-proBNP and −8.9% for GLS. A combination of both parameters separated groups with lower (both parameters below the threshold)=stage I, intermediate (one parameter above the threshold)=stage II and higher mortality risk (both parameters above the threshold)=stage III.
Discussion
This study aimed to investigate clinical, laboratory, electrocardiography and echocardiographic parameters for usefulness to predict outcome in AL amyloidosis with cardiac involvement proven by EMB.
Besides response to therapy, cardiac involvement is the main prognostic determinant in AL amyloidosis.27 Patients with cardiac involvement have a shorter survival than those without cardiac involvement, and mortality is even higher when congestive HF occurs.28 29 The search for prognostic markers therefore plays a crucial role, as they might aid in selecting therapeutic strategies, not only targeting the clonal disease but also regarding a timely and appropriate HF management.
Serum levels of NT-proBNP and cardiac troponins have emerged as important prognostic parameters and are therefore commonly used for risk stratification.16 18 In an unselected population of patients with AL amyloidosis the prognostic value of these biomarkers results from separating patients with a low (MAYO stage I) from those with a high probability of cardiac involvement (MAYO stage>I). Furthermore, they subdivide patients with suspected or proven cardiac involvement into a group with milder (MAYO stage II) and more advanced HF (MAYO stage III and IIIb). Beyond serological testing, functional cardiac imaging, particularly strain analysis, plays a fundamental role in risk stratification and prognostication in AL amyloidosis.30 However, the aforementioned parameters must be interpreted with caution because increased levels of biomarkers and pathological imaging findings can also be found in the context of other diseases and do not necessarily confirm or reflect cardiac involvement in AL amyloidosis.
The gold standard for the diagnosis of cardiac involvement is EMB.31 32 Due to its invasiveness, EMB is not common in most studies investigating survival criteria in AL amyloidosis in general23 33 34 and few studies have investigated the prognosis of patients with cardiac involvement proven by EMB in particular. These studies identified sex, Karnofsky index, diastolic blood pressure, NYHA-FC, NT-proBNP, GFR, mineralocorticoid receptor antagonist use, lack of β-blocker use, E-wave deceleration time, LV-EF, LV mass, LV wall thickness, LVP, intraventricular conduction delay, amyloid load, response to chemotherapy and SCT as markers associated with survival.22 35–37 Only LV-EF, LVP,35 NYHA-FC,36 NT-proBNP, GFR, response to chemotherapy and amyloid load37 were independent predictors of mortality in the multivariable model. However, cardiac deformation assessed by strain imaging had not been investigated for its prognostic value in patients with AL amyloidosis and EMB-proven cardiac involvement so far.
To close this knowledge gap, we screened the database of the amyloidosis centre at Heidelberg University Hospital, one of the largest of its kind worldwide. Among 1628 patients who had their initial visit from July 2006 to December 2017, we identified 216 patients with EMB proven cardiac involvement. To eliminate the effect of chemotherapy and to reduce the influence of comorbidities on our analysis, only therapy-naïve patients without a history of significant cardiac or renal disease at the time of EMB were further investigated. At the end of the screening process 174 patients met the criteria for inclusion in this study.
The median OS of the complete cohort was 1.47 years (95% CI 1.04 to 2.92 years) which is comparable with the literature on patients with AL amyloidosis.6 28 29 One hundred and fifteen patients (66%) had died after the 12 years of the investigation. The survival probability at 10 years from the time of first contact with the amyloidosis centre was 0.195 (95% CI 0.120 to 0.316).
Comparing survivors with non-survivors male sex, blood pressure, NYHA-FC, LVP, LV- ESV, LV-EF, longitudinal ventricular function, pericardial effusion, NT-proBNP, hsTNT, dFLC and eGFR were associated with poor outcome but only NYHA-FC >II, LV global longitudinal strain, LV-ESV, systolic pulmonary artery pressure, NT-proBNP and dFLC were independently predictive in multivariable analysis. Interestingly, from the time of EMB proven cardiac involvement, neither the serum level of cardiac hsTNT, as an indicator of myocardial damage and integral component of current amyloidosis staging systems, nor LV-EF, as a standard measure of cardiac systolic function and crucial criterion for HF classification, had independent prognostic significance in our study cohort. However, this does not mean that both parameters have no predictive value at all. Rather our variable selection was subject to some restrictions and the circumstances of missing values might have introduced additional uncertainty. Due to the number of predictors in relation to the effective sample size for multivariable Cox regression, the better approach of backward elimination was not feasible and so forward selection was performed for variable selection.
New treatment options have improved the survival of patients with AL amyloidosis over the past few decades.20 A basic requirement before starting therapy is optimal risk stratification. However, only patients in MAYO stage I had significant survival improvement over time, while the survival improvement in MAYO stage II and III/IIIb was marginal or nil, respectively.38 Risk stratification tools in patients with both, AL amyloidosis and cardiac involvement, should therefore provide a better predictive power. A first step to improve the original MAYO score was to implement a more appropriate cut-off level for NT-proBNP to identify a very poor-prognosis subgroup of patients in MAYO stage III.18 From the cardiologist’s point of view additional options exist, that could supplement a prognostic evaluation based purely on blood tests. In this context, cardiac imaging holds great potential as it provides direct and objective structural and functional read-outs. A focused analysis of myocardial performance may be superior to clinical classification systems like NYHA-FC, the assessment of which may vary substantially, or biomarkers such as dFLC that primarily reflects haematological disease burden.17
Global longitudinal strain could be a promising candidate to optimise the risk stratification of cardiac AL amyloidosis. Compared with other echocardiographic parameters that were independently predictive in our study, global longitudinal strain has lower intraobserver and interobserver variability than LV-ESV39 40 and, unlike systolic pulmonary artery pressure, should be measurable in most patients. Furthermore, recent studies have demonstrated that strain imaging can predict survival and therapy response in AL amyloidosis in general41–45 while our data further suggest that global longitudinal strain in combination with NT-proBNP may offer a useful survival risk stratification for AL amyloidosis patients with cardiac involvement in particular. However, a prognostic benefit for patients with cardiac AL amyloidosis needs to be prospectively validated and tested against other accepted staging systems in the field.
The inclusion criteria of our study resulted in a highly selected patient cohort especially since some comorbidities such as atrial fibrillation might have been directly related to AL amyloidosis. Furthermore, the rates of atrial fibrillation, additional kidney amyloidosis and the use of SCT were very low compared with a general population with AL amyloidosis. Therefore, our findings are not transferable to all AL amyloidosis patients, especially to those without cardiac involvement.
Limitations
Although the amyloidosis centre at Heidelberg University Hospital has a nationwide catchment area, this is a single-centre study. The retrospective nature of our study and the requirement for EMB proven cardiac involvement may contribute to a selection bias. We minimised any bias by including all patients with AL amyloidosis and cardiac involvement during the above-mentioned time interval. Nevertheless, we want to point out that the cohort examined in this study is not representative of the total population of patients diagnosed with AL amyloidosis. This is reflected, among other things, in a low rate of concomitant renal involvement or atrial fibrillation.
The onset and therefore the true duration of AL amyloidosis are difficult to assess because patients often show no clinical signs even at the beginning of cardiac involvement. The fact that all patients in our study underwent EMB indicates a high suspicion for an advanced stage of the disease in our cohort.
While the multivariable Cox regression analysis identified predictors for mortality, other important indicators may have been missed. Additionally, the variable selection might have suffered from the uncertainty due to the multiple imputation.
Conclusion
Among all patients with AL amyloidosis those with cardiac involvement represent a high-risk population with limited therapy options and poor prognosis. However, the present study suggests, that a relevant number of patients with cardiac AL amyloidosis can survive many years after the initial diagnosis. Therefore, accurate risk stratification is necessary to identify cardiac amyloidosis patients with favourable prognosis. Incorporation of modern imaging techniques into existing or newly developed scoring systems is a promising option that might enable the implementation of risk-adapted therapeutic strategies.
Acknowledgments
For the publication fee, we acknowledge financial support by Deutsche Forschungsgemeinschaft within the funding programme 'Open Access Publikationskosten' as well as by Heidelberg University.
Footnotes
Twitter: @echobasics
Contributors: Conception and design of data: MA and DM. Analysis and interpretation: MA, JB, JAV and SG. Drafting of the manuscript: MA. Criticall revision of the manuscript for important intellectual content: FADS, UH and SS. Final approval of the manuscript: HAK, NF and DM. DM is responsible for the overall content, accepts full responsibility for the finished work, had access to the data, and controlled the decision to publish.
Funding: This study was funded by Deutsche Forschungsgemeinschaft, Heidelberg University.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and this study was carried out after approval by the ethics committee of the University of HeidelbergReference number: 123/2006. Participants gave informed consent to participate in the study before taking part.
References
- 1.Benson MD, Buxbaum JN, Eisenberg DS, et al. Amyloid nomenclature 2020: update and recommendations by the International Society of Amyloidosis (ISA) nomenclature committee. Amyloid 2020;27:217–22. 10.1080/13506129.2020.1835263 [DOI] [PubMed] [Google Scholar]
- 2.Palladini G, Merlini G. What is new in diagnosis and management of light chain amyloidosis Blood 2016;128:159–68. 10.1182/blood-2016-01-629790 [DOI] [PubMed] [Google Scholar]
- 3.Kyle RA, Larson DR, Kurtin PJ, et al. Incidence of AL amyloidosis in Olmsted county, Minnesota, 1990 through 2015. Mayo Clin Proc 2019;94:465–71. 10.1016/j.mayocp.2018.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinney JH, Smith CJ, Taube JB, et al. Systemic amyloidosis in England: an epidemiological study. Br J Haematol 2013;161:525–32. 10.1111/bjh.12286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lousada I, Comenzo RL, Landau H, et al. Light chain amyloidosis: patient experience survey from the amyloidosis research consortium. Adv Ther 2015;32:920–8. 10.1007/s12325-015-0250-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mankad AK, Sesay I, Shah KB. Light-chain cardiac amyloidosis. Curr Probl Cancer 2017;41:144–56. 10.1016/j.currproblcancer.2016.11.004 [DOI] [PubMed] [Google Scholar]
- 7.Liao R, Jain M, Teller P, et al. Infusion of light chains from patients with cardiac amyloidosis causes diastolic dysfunction in isolated mouse hearts. Circulation 2001;104:1594–7. [PubMed] [Google Scholar]
- 8.Brenner DA, Jain M, Pimentel DR, et al. Human amyloidogenic light chains directly impair cardiomyocyte function through an increase in cellular oxidant stress. Circ Res 2004;94:1008–10. 10.1161/01.RES.0000126569.75419.74 [DOI] [PubMed] [Google Scholar]
- 9.Shi J, Guan J, Jiang B, et al. Amyloidogenic light chains induce cardiomyocyte contractile dysfunction and apoptosis via a non-canonical P38Α MAPK pathway. Proc Natl Acad Sci U S A 2010;107:4188–93. 10.1073/pnas.0912263107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guan J, Mishra S, Shi J, et al. Stanniocalcin1 is a key mediator of amyloidogenic light chain induced cardiotoxicity. Basic Res Cardiol 2013;108:378. 10.1007/s00395-013-0378-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishra S, Guan J, Plovie E, et al. Human amyloidogenic light chain proteins result in cardiac dysfunction, cell death, and early mortality in Zebrafish. Am J Physiol Heart Circ Physiol 2013;305:H95–103. 10.1152/ajpheart.00186.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lavatelli F, Imperlini E, Orrù S, et al. Novel mitochondrial protein Interactors of immunoglobulin light chains causing heart amyloidosis. FASEB J 2015;29:4614–28. 10.1096/fj.15-272179 [DOI] [PubMed] [Google Scholar]
- 13.Takemura G, Takatsu Y, Doyama K, et al. Expression of atrial and brain natriuretic peptides and their genes in hearts of patients with cardiac amyloidosis. J Am Coll Cardiol 1998;31:754–65. 10.1016/s0735-1097(98)00045-x [DOI] [PubMed] [Google Scholar]
- 14.Palladini G, Campana C, Klersy C, et al. Serum N-terminal pro-brain natriuretic peptide is a sensitive marker of myocardial dysfunction in AL amyloidosis. Circulation 2003;107:2440–5. 10.1161/01.CIR.0000068314.02595.B2 [DOI] [PubMed] [Google Scholar]
- 15.Dispenzieri A, Kyle RA, Gertz MA, et al. Survival in patients with primary systemic amyloidosis and raised serum cardiac troponins. Lancet 2003;361:1787–9. 10.1016/S0140-6736(03)13396-X [DOI] [PubMed] [Google Scholar]
- 16.Dispenzieri A, Gertz MA, Kyle RA, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol 2004;22:3751–7. 10.1200/JCO.2004.03.029 [DOI] [PubMed] [Google Scholar]
- 17.Kumar S, Dispenzieri A, Lacy MQ, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol 2012;30:989–95. 10.1200/JCO.2011.38.5724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wechalekar AD, Schonland SO, Kastritis E, et al. A European collaborative study of treatment outcomes in 346 patients with cardiac stage III AL amyloidosis. Blood 2013;121:3420–7. 10.1182/blood-2012-12-473066 [DOI] [PubMed] [Google Scholar]
- 19.Lilleness B, Ruberg FL, Mussinelli R, et al. Development and validation of a survival staging system incorporating BNP in patients with light chain amyloidosis. Blood 2019;133:215–23. 10.1182/blood-2018-06-858951 [DOI] [PubMed] [Google Scholar]
- 20.Witteles RM, Liedtke M. AL amyloidosis for the cardiologist and oncologist: epidemiology, diagnosis, and management. JACC CardioOncol 2019;1:117–30. 10.1016/j.jaccao.2019.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tahir UA, Doros G, Kim JS, et al. Predictors of mortality in light chain cardiac amyloidosis with heart failure. Sci Rep 2019;9:8552. 10.1038/s41598-019-44912-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grogan M, Gertz MA, Kyle RA, et al. Five or more years of survival in patients with primary systemic amyloidosis and biopsy-proven cardiac involvement. Am J Cardiol 2000;85:664–5, 10.1016/s0002-9149(99)00832-2 [DOI] [PubMed] [Google Scholar]
- 23.Finocchiaro G, Merlo M, Pinamonti B, et al. Long term survival in patients with cardiac amyloidosis: prevalence and characterisation during follow-up. Heart, Lung and Circulation 2013;22:647–54. 10.1016/j.hlc.2013.01.010 [DOI] [PubMed] [Google Scholar]
- 24.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr 2015;28:1–39. 10.1016/j.echo.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 25.Eekhout I, van de Wiel MA, Heymans MW. Methods for significance testing of categorical covariates in logistic regression models after multiple imputation: power and applicability analysis. BMC Med Res Methodol 2017;17:129. 10.1186/s12874-017-0404-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Contal C, O’Quigley J. An application of changepoint methods in studying the effect of age on survival in breast cancer. Comput Stat Data Anal 1999;30:253–70. 10.1016/S0167-9473(98)00096-6 [DOI] [Google Scholar]
- 27.Obici L, Perfetti V, Palladini G, et al. Clinical aspects of systemic amyloid diseases. Biochim Biophys Acta 2005;1753:11–22. 10.1016/j.bbapap.2005.08.014 [DOI] [PubMed] [Google Scholar]
- 28.Dubrey SW. The clinical features of immunoglobulin light-chain (AL) amyloidosis with heart involvement. QJM 1998;91:141–57. 10.1093/qjmed/91.2.141 [DOI] [PubMed] [Google Scholar]
- 29.Kapoor P, Thenappan T, Singh E, et al. Cardiac amyloidosis: a practical approach to diagnosis and management. Am J Med 2011;124:1006–15. 10.1016/j.amjmed.2011.04.013 [DOI] [PubMed] [Google Scholar]
- 30.Buss SJ, Emami M, Mereles D, et al. Longitudinal left ventricular function for prediction of survival in systemic light-chain amyloidosis: incremental value compared with clinical and biochemical markers. J Am Coll Cardiol 2012;60:1067–76. 10.1016/j.jacc.2012.04.043 [DOI] [PubMed] [Google Scholar]
- 31.Kieninger B, Eriksson M, Kandolf R, et al. Amyloid in endomyocardial biopsies. Virchows Arch 2010;456:523–32. 10.1007/s00428-010-0909-5 [DOI] [PubMed] [Google Scholar]
- 32.Banypersad SM, Moon JC, Whelan C, et al. Updates in cardiac amyloidosis: a review. J Am Heart Assoc 2012;1:e000364. 10.1161/JAHA.111.000364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Milani P, Dispenzieri A, Scott CG, et al. Independent prognostic value of stroke volume index in patients with immunoglobulin light chain amyloidosis. Circ Cardiovasc Imaging 2018;11:e006588. 10.1161/CIRCIMAGING.117.006588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee MH, Lee SP, Kim YJ, et al. Incidence, diagnosis and prognosis of cardiac amyloidosis. Korean Circ J 2013;43:752–60. 10.4070/kcj.2013.43.11.752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kristen AV, Perz JB, Schonland SO, et al. Non-invasive predictors of survival in cardiac amyloidosis. Eur J Heart Fail 2007;9:617–24. 10.1016/j.ejheart.2007.01.012 [DOI] [PubMed] [Google Scholar]
- 36.Austin BA, Duffy B, Tan C, et al. Comparison of functional status, electrocardiographic, and echocardiographic parameters to mortality in endomyocardial-biopsy proven cardiac amyloidosis. Am J Cardiol 2009;103:1429–33. 10.1016/j.amjcard.2009.01.361 [DOI] [PubMed] [Google Scholar]
- 37.Kristen AV, Brokbals E, Aus dem Siepen F, et al. Cardiac amyloid load: a prognostic and predictive biomarker in patients with light-chain amyloidosis. J Am Coll Cardiol 2016;68:13–24. 10.1016/j.jacc.2016.04.035 [DOI] [PubMed] [Google Scholar]
- 38.Muchtar E, Gertz MA, Kumar SK, et al. Improved outcomes for newly diagnosed AL amyloidosis between 2000 and 2014: cracking the glass ceiling of early death. Blood 2017;129:2111–9. 10.1182/blood-2016-11-751628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aurich M, André F, Keller M, et al. Assessment of left ventricular volumes with echocardiography and cardiac magnetic resonance imaging: real-life evaluation of standard versus new semiautomatic methods. J Am Soc Echocardiogr 2014;27:1017–24. 10.1016/j.echo.2014.07.006 [DOI] [PubMed] [Google Scholar]
- 40.Aurich M, Keller M, Greiner S, et al. Left ventricular mechanics assessed by two-dimensional echocardiography and cardiac magnetic resonance imaging: comparison of high-resolution speckle tracking and feature tracking. Eur Heart J Cardiovasc Imaging 2016;17:1370–8. 10.1093/ehjci/jew042 [DOI] [PubMed] [Google Scholar]
- 41.Barros-Gomes S, Williams B, Nhola LF, et al. Prognosis of light chain amyloidosis with preserved LVEF: added value of 2d speckle-tracking echocardiography to the current prognostic staging system. JACC Cardiovasc Imaging 2017;10:398–407. 10.1016/j.jcmg.2016.04.008 [DOI] [PubMed] [Google Scholar]
- 42.Pun SC, Landau HJ, Riedel ER, et al. Prognostic and added value of two-dimensional global longitudinal strain for prediction of survival in patients with light chain amyloidosis undergoing autologous hematopoietic cell transplantation. J Am Soc Echocardiogr 2018;31:64–70. 10.1016/j.echo.2017.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee Chuy K, Drill E, Yang JC, et al. Incremental value of global longitudinal strain for predicting survival in patients with advanced AL amyloidosis. JACC CardioOncol 2020;2:223–31. 10.1016/j.jaccao.2020.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cohen OC, Ismael A, Pawarova B, et al. Longitudinal strain is an independent predictor of survival and response to therapy in patients with systemic AL Amyloidosis. Eur Heart J 2022;43:333–41. 10.1093/eurheartj/ehab507 [DOI] [PubMed] [Google Scholar]
- 45.Huntjens PR, Zhang KW, Soyama Y, et al. Prognostic utility of echocardiographic atrial and ventricular strain imaging in patients with cardiac amyloidosis. JACC Cardiovasc Imaging 2021;14:1508–19. 10.1016/j.jcmg.2021.01.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2023-002310supp001.pdf (61.7KB, pdf)
Data Availability Statement
Data are available on reasonable request.



