Abstract
Vision plays an important role in an athletes’ success. In sports, nearly 80% of perceptual input is visual, and eye health and sports medicine are closely intertwined fields of utmost importance to athletes. The physical nature of sports activities renders individuals more prone to various eye injuries than the general population. Ocular trauma can lead to lifelong sequelae, and impaired vision requires careful follow-up and management. Apart from injuries, athletes may also experience vision problems that can hamper their performance, including blurred vision, double vision, and light sensitivity.
The interdisciplinary nature of sports medicine necessitates collaboration between sports medicine professionals and ophthalmologists. Through such collaborations, athletes can receive appropriate eye care, education on proper eye protection and guidance on adopting good eye health practices. If any inconspicuous symptoms are not detected and treated promptly, athletes may acquire systemic injuries because of defective vision, preventing them from achieving high level athletic performance in competitions.
The protection of the elite athlete is the responsibility of all of us in sports medicine. To advance a more unified, evidence-informed approach to ophthalmic health assessment and management in athletes and as relevant for sports medicine physicians, the International Olympic Committee Consensus Group aims for a critical evaluation of the current state of the science and practice of ophthalmologic issues and illness in high-level sports, and present recommendations for a unified approach to this important issue.
Keywords: Knowledge translation, Injuries, Eye
Introduction
Vision plays an important role in an athlete’s success.1 In sports, nearly 80% of perceptual input is visual,2and eye health and sports medicine are closely intertwined fields of utmost importance to athletes. The physical nature of sports activities renders individuals more prone to various eye injuries than the general population. Ocular trauma can lead to lifelong sequelae, and impaired vision requires careful follow-up and management. Apart from injuries, athletes may also experience vision problems that can hamper their performance, including blurred vision, double vision and light sensitivity.
The interdisciplinary nature of sports medicine necessitates collaboration between sports medicine professionals and ophthalmologists. Through such collaborations, athletes can receive appropriate eye care, education on proper eye protection and guidance on adopting good eye health practices. If inconspicuous symptoms are not detected and treated promptly, athletes may acquire systemic injuries because of defective vision, preventing them from achieving high-level athletic performance in competitions.
Protecting the athlete is the responsibility of all of us in sports medicine.3 To advance a more unified, evidence-informed approach to ophthalmic health assessment and management in athletes and as relevant for sports medicine physicians, the International Olympic Committee (IOC) Consensus Group aims for a critical evaluation of the current state of the science and practice of ophthalmologic issues and illness in high-level sports.
Methods
This ophthalmology narrative statement used a diverse expert panel of authors: sports medicine physicians, ophthalmologists, sports scientists, former elite athletes and a mental performance consultant. Authors were invited based on their expertise, as demonstrated by previous research and clinical experiences with ophthalmology and sports medicine. In total, 3 females and 12 males from 4 continents participated.
From the entire group of authors, smaller working groups of content experts were tasked with preparing specific subtopics before the in-person consensus in the form of a referenced summary of the existing scientific literature. KS and LE compiled these literature summaries and then circulated them for online reviews. The summaries were discussed at the subsequent meeting in Lausanne, Switzerland, 28 November 2022–30 November 2022. Authors were encouraged to write a minority opinion in the event of disagreement.
Epidemiology of sports-related ophthalmology issues
Sports-related ocular/orbital injuries have generated considerable interest and research. Identifying common ophthalmology health problems in sport, their severity, risk factors and mechanisms, ideally through well-designed prospective cohort studies, are forming the basis for developing targeted preventive strategies—see the four-step model of van Mechelen et al,4 often applied in health epidemiology.
Sports-related ocular injuries are present across individual and team sports. Most of the literature on epidemiology has collected data retrospectively through medical databases in hospitals and emergency departments.
Eye trauma is typically a result of traumatic accidents following crashes or (un)intentional contact with an opponent or equipment. Although most sports-related eye injuries from blunt trauma have relatively good visual outcomes, several blunt traumas result in more severe orbital/intraocular sequelae. These will require follow-up and management.5
We must distinguish between penetrating and perforating injuries. Penetrating injuries occur when there is a single laceration to the eye, causing an open globe. Perforating injuries are when two full-thickness lacerations are present,6 usually resulting from sharp objects.
Sports may be classified as high, moderate and low risk for eye injuries7 (table 1). Another more mechanical definition classifies sports into high energy and low energy with respect to the projectile hitting the eye, injuries and penetration.
Table 1.
Classification of sports into high, moderate and low risk with respect to eye injuries
| Classification | High risk | Moderate risk | Low risk |
| Definition | Small, high speed, dense projectiles close to athletes, air rifle; paintball, hard, dense projectiles, fingers close to athletes or use of bat or stick | High-speed ball, use of bat or stick, aggressive body contact | Not involve a thrown or hit ball, a stick or bat, or aggressive play |
| Examples | Badminton, baseball/softball, basketball, cricket, fencing, field hockey, ice hockey, lacrosse, squash, tennis, boxing, wrestling, judo | American football, archery/darts, Australian football, rugby, football (soccer), volleyball, water polo | Athletics, cycling, rowing, canoeing, skiing, swimming, diving, waterskiing |
Due to the varying popularity of sports worldwide, there are also geographical variations in ophthalmology health issues. While some of the available research focused on single sports,8 9 other research investigated multiple sports,10 11 but with no or limited long-term follow-up of eye injuries.
Prospective studies systematically quantifying and characterising the incidence and type of injuries seen with sports-related ocular trauma are scarce.12–17
A limitation of the current research is that datasets often rely on emergency department data, which may only collect the most severe injuries (eg, National Electronic Injury Surveillance System).18 In addition, many studies reported on the most commonly presented eye issues as absolute numbers rather than as relative proportions, meaning that when a sport is popular in a specific country, it is not surprising that those sports stand for the most injuries.
Sports-related ophthalmology issues in Olympic Games: Anecdotally, following 10 years of data collection across three Summer and three Winter Olympic Games and three Youth Olympic Games, few severe eye injuries have been documented.13 Eye injuries thus seem infrequent during the Olympic Games, though we lack reliable data. Currently, the IOC research methodology does not allow sports medicine physicians to report eye injuries,19 as ‘Face reliably’ is the broad injury location category for National Olympic Committee physicians to capture eye injuries. However, a new category to record ophthalmology-related illness issues has been added to the reporting sheet/database.20
Anatomy for sports medicine physicians
Proper clinical care of sports-related ophthalmology issues requires a good understanding of anatomy and common ocular conditions associated with high-level sports, including proper examination techniques by the sports medicine physician.
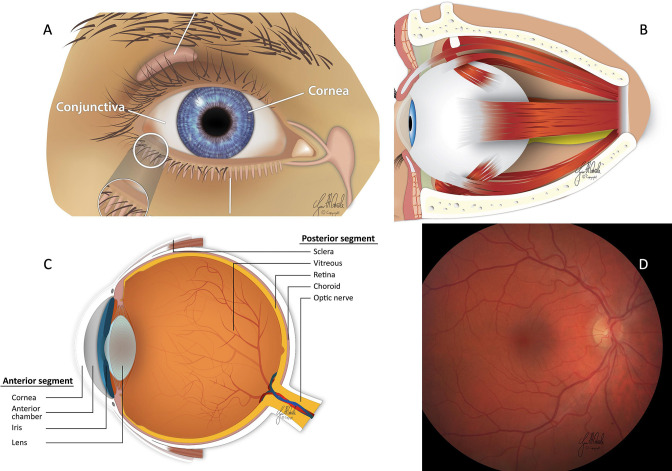
Externally, the upper and lower eyelids cover the eye. In addition, tear fluid produced in the lacrimal gland under the outer part of the frontal bone protects the ocular surface.21 The tear fluid is then drained from the upper and lower puncta medially on the eyelids into the lacrimal canaliculi, the lacrimal sac and further into the inferior nasal meatus of the nasal cavity (figure 1A).
Figure 1.
(A) Eye anatomy: ocular surface; (B) eye anatomy: orbital content; (C) eye anatomy: division of the eye; (D) eye anatomy: retina.
The orbital bones consist of the frontal, zygomatic, maxillary, sphenoid, lacrimal and ethmoid bones forming a four-sided eye protection (figure 1B). Together with the orbital septum (palpebral fascia) anteriorly, this forms a closed compartment with orbital fat providing structural support to orbital structures.21 The medial orbital wall also contains a fragile part, lamina papyrica, vulnerable to trauma and the spread of infections from the sinuses and into the postseptal orbital compartment.
The extraocular muscles arise from the orbit and insert into the eyeball, allowing ocular mobility. These muscles are innervated by the cranial nerves n. abducens (abduction of the eye), n. trochlearis (downward gaze from adducted position) and n. oculomotorius (controlling most other eye movements, constricting the pupil and the levator palpebrae muscle). The optic nerve and the ophthalmic artery also pass through the orbit through the foramen ovale, and the periorbital fat protects the orbital structures.21
The eye globe is divided into three separate layers (figure 1C); the outer layer (tunica fibrosa) consists of the viscoelastic white sclera and the cornea, uvea (tunica vasculosa) consists of the iris, ciliary body and choroid and the innermost layer (tunica interna) consists of the retina and the retinal pigmented epithelium (RPE). The eye can also be divided into an anterior and posterior segment. The anterior segment includes the clear cornea, anterior chamber, iris/pupil and lens. In addition, aqueous humour is produced by the epithelium lining the ciliary body and flows into the anterior chamber, where it is drained from the eye into the trabecular meshwork. The posterior segment includes the vitreous, choroid, retina and optic nerve head.21
When light enters the eye (figure 1D), specialised photoreceptors in the retina generate an electrical signal. Rods are mainly found in the peripheral areas of the retina and are responsible for night and peripheral vision. In contrast, cones are mainly clustered in the macula, providing sharp central and colour vision. The generation of electrical signals and processing by the neural network in the retina has the highest oxygen consumption per weight of all tissues in the body, indicating a high metabolic rate. Thus, the retina also has a dual blood supply through the central retina artery (inner retinal layers) and the choroid (outer retinal layers).22 In addition, the RPE has important supporting functions essential to photoreceptor maintenance, including the transport of nutrients from the choroid to the retina and phagocytosis and removal of the outer segments of the photoreceptors.23
The electrical signal from the retina is then transferred into action potentials by the retinal ganglion cells and travels along the optic nerve to the brain. The optical fibres nasally cross at the optic chiasm so that all signals from the right visual field end up in the left visual cortex and from the left visual field into the right visual cortex.21
Trauma to the orbit, adnexa and eye globe
Eye globe injuries are classified according to The Birmingham Eye Trauma Terminology system24 and there are several classifications for facial and orbital fractures,25 but there is no single classification combining orbital fractures, periorbital and eyeball injuries.
Depending on the energy and area of impact of the trauma, the following can be encountered:
Periorbital tissues: swelling and lacerations of the eyelids.
Eyeball: conjunctival bleedings, corneal abrasions, perforation, hyphema (accumulation of blood in the anterior chamber), iridodialysis (separation of the iris from the ciliary lens subluxation/luxation), lens luxation or traumatic cataract, choroidal and vitreous haemorrhages, commotio retinae, retinal tear/detachment.
Orbit: fracture of orbital bones, traumatic optic neuropathy, optic nerve avulsion, compartment syndrome due to intraorbital haemorrhage.26 The zygomaticomaxillary complex fracture is the most commonly encountered sports-related orbital fracture.27 The roof of the infraorbital canal located in the orbital floor and lamina papyracea in the medial wall are the thinnest and weakest parts of the orbit, and most of the fractures pass through these sites.27
The sideline evaluation of the eye should include visual acuity, pupillary shape, size and light reflex, always comparing to the fellow eye, meaning the other eye. Absent red reflex (reddish-orange reflection of light from the retina) mandates a specialist examination. Diplopia, exophthalmia/enophthalmia, orbital rim step-off and numbness over the cheek can indicate a bone fracture.26 27 It is generally agreed that entrapment of an extraocular muscle, particularly trapdoor fractures in children accompanied with bradycardia, syncope or vomiting (oculocardiac reflex), cosmetically significant exophthalmos or hypoglobus and large orbital floor fractures (more than 50% of the surface area) requires early surgical attention.26 28
Special attention should be paid to the following particular conditions:
The lacrimal drainage system will likely be damaged if a laceration involves the medial eyelid margins. A specialist, for example, oculoplastic, must handle these cases.
Open globe injuries are susceptible to infections, and an intraocular foreign body must be ruled out using a CT-only. MRI cannot be used because of possible magnetic intraocular material risk. Ocular ultrasound must also not be used due to the increased risk of pressure-induced damage from the probe.
Loss of vision and lack of ocular motility can be a sign of orbital compartment syndrome, which should be treated immediately.
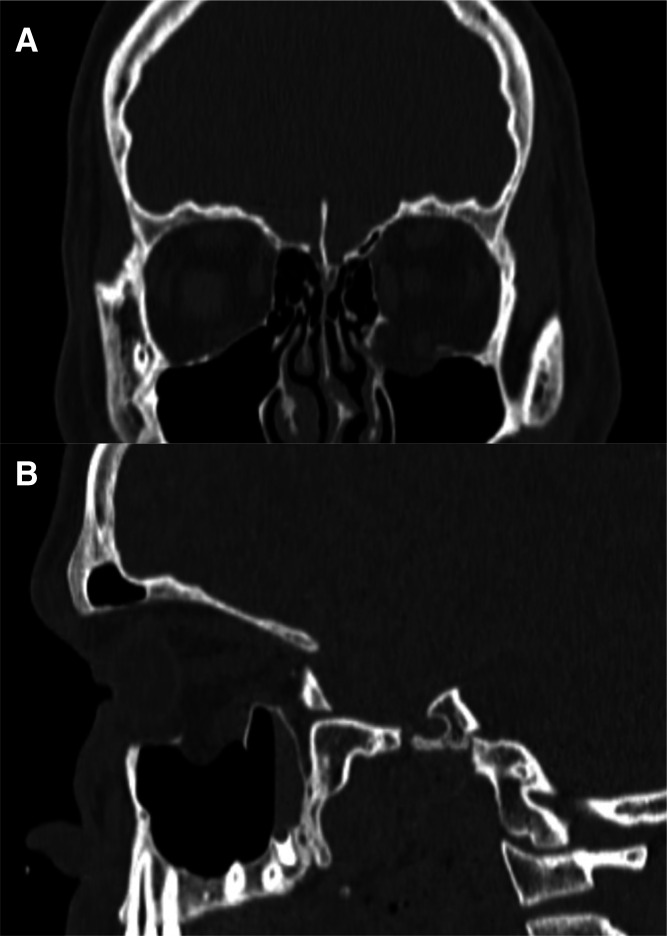
A special type of relatively common injury deserving close attention is the blow-out fracture, which occurs secondary to a sudden explosive increase of the intraorbital pressure transmitted to orbital bones, most often due to high-velocity ball-related injuries. The floor is the most vulnerable part of the orbit, but the orbital rim usually remains intact.29 Blow-out fracture must be considered in the presence of typical signs and symptoms, which include diplopia (on upward gaze), limited upward gaze, tenderness at the infraorbital rim, decreased sensation over the inferior orbital rim, extending to the edge of the nose and ipsilateral upper lip (indicates infraorbital nerve injury).29 30 Subcutaneous or orbital emphysema and crepitation may suggest a fracture of the maxillary sinus or breach in the lamina papyracea. Decreased visual acuity and an absent pupillary light reflex may indicate orbital haemorrhage or optic nerve injury.29 30 In these instances, CT of the orbit is mandatory and may show the fracture lines, air-fluid level or haemorrhage in the maxillary sinus, and herniated orbital contents into the maxillary sinus (figure 2).29 30
Figure 2.
CT scan of a tennis player who received a direct hit of the ball to the left eye. (A) Coronal view: there is a large bony defect in the medial part of the left orbital floor with herniation of the inferior rectus muscle and orbital fat into the maxillary sinus (arrow). (B) CT scan of a tennis player who received a direct hit of the ball to the left eye, sagittal view.
Most specialists agree that surgery must be undertaken within 14 days to prevent fibrosis if indicated.31 In the acute phase, corticosteroids may help dissipating oedema, and the patient must be warned against forceful nose-blowing and refrain from any Valsalva manoeuvres requiring action. Prophylactic oral antibiotics are recommended.29–31 The outcome of blow-out fractures is variable. The recovery is slow; many patients may experience persistent neuralgia, diplopia and enophthalmos. Ocular motility exercises must be instituted early to stimulate the regeneration of orbital septa connecting the extraocular muscle.30
Targeted history and assessment of the athlete’s eye
Regular assessment of the athlete’s eyes
Eye screening—preferably conducted off-season—is essential to maximise visual capacity, protect eye health, and provide an educational opportunity to reduce traumatic eye injury. At the same time, a full ophthalmic examination of the eye examination ought to include history-taking, physical examination, intraocular pressure measurement, slit lamp biomicroscopy of the anterior segment, dilated fundus examination and ocular imaging. The sports medicine physician is expected to take the history, conduct a physical examination of the eye, perform a red reflex, and perform a funduscopy.
Office or off-field assessment
When managing an ocular injury on the field, the primary priorities are to protect the eye from further harm. In the following, decide which injury may require immediate referral to an ophthalmologist. As a sports medicine physician, you should update yourself on the guidelines for returning an athlete to competition.
History taking
If the athlete is anxious, put the athlete at ease. Note the sport, discipline and injury mechanism, and whether the athlete has symptoms only in one or both eyes. In addition, question the athlete about prior eye diseases, whether protective eyewear was used and whether the athlete has any pain. Following this, assess for blunt, penetrating or perforating injuries; the force and direction of the impact; the possibility of a foreign body/s; pre-existing eye conditions (eg, contact lens use, eye-drops, whether undergone cataract surgery, glaucoma and retinal surgery, refractive surgery, cataract surgery and relevant history (eg, head injury)).
In the dressing room, establish the date of the last tetanus immunisation (for tetanus prophylaxis) and underlying medical conditions (eg, autoimmune disease, allergy).
Physical examination and the conditions requiring referral to an ophthalmologist
Triage for associated serious injuries to the head, neck and spine in a well-lit room. In severe bleeding, carefully remove the blood using gauze or tissue and a physiologic/balanced irrigating solution to facilitate inspection without exerting any pressure on the globe. Physical examination of the globe may be difficult in acute eye region injury due to eyelid swelling and severe pain. Be aware of that patient cooperation may be limited by severe pain, unresponsiveness, or altered mental states. Compare both eyes to determine injured eye/s by:
Functional examination encompassing visual acuity (using a visual acuity chart or finger counting distance, hand movement, light perception).
Visual field testing (simple test:any visual field defect suggests an important pathology affecting the retina, optic nerve, or central nervous system).
Ocularmovement (9 cardinal and pursuit and saccadic movement to rule out brain injury and extraocular muscle entrapment caused by orbital wall fractures).
Inspection for facial fractures, hematoma, bleeding and foreign bodies.
Inspection of the eye region, including the eyelids, with smartphone illumination, head LED (Light Emitting Diode) lamp, or a penlight.
Palpate the orbital margins and zygoma to assess for a step or tenderness. If a blowout fracture is suspected, assess the sensation below the orbit. While palpating, avoid direct pressure on the globe if there is a perforation. Ask the patient to open their eyes voluntarily. If unable to do so, gently lift the eyebrow without exerting any pressure on the globe. Compare both sides, inspect for proptosis (abnormal protrusion or displacement of eye), enophthalmos (posterior displacement of eye “sunken” eye) and eyelid asymmetry.
Perform pupillary tests with a penlight, including the swing test in low ambient light. Also, evaluate pupil asymmetry and irregularity. Inspect the anterior segment of the eye with the torch illuminating from the side for foreign bodies, conjunctival bleedings and corneal abrasion/lacerations. Fluorescein strips are very helpful for detecting corneal abrasions and perforations (Siedel Test with Cobalt blue filter). In the anterior chamber, look for hyphema and shallowing of the anterior chamber as well as iridodialyis and traumatic cataracts.
Confirm the red reflex with the ophthalmoscope in all gaze directions–a clear red reflex indicates the transparency of the optical media from the cornea to the retina. In contrast, a reduced or absent red reflex can indicate hyphema, traumatic cataract, vitreous haemorrhage or retinal detachment.
Athletes’ eye conditions requiring referral to an ophthalmologist are shown in online supplemental appendix 3. Table B in online supplemental appendix 5, provides practical recommendations for a sports medicine physician on how to deal with ophthalmology issues onsite.
bmjsem-2023-001644supp003.pdf (226.1KB, pdf)
bmjsem-2023-001644supp005.pdf (55KB, pdf)
Photo/video documentation
Well-taken photos or videos of the injured eye region can provide much more information than written descriptions, conveying useful information when referring to the ophthalmologist. Ensure that the entire face is in the frame so that related facial injuries (eg, Le Fort fracture) can also be captured. The patient should look straight ahead, and both eyes should be captured simultaneously and in isolation for greater detail. Photo images are useful for eyelid, corneal and conjunctival injuries, while video images of eye movements are especially useful for capturing diplopia. Pupillary reflex and the relative apparent pupillary defect can be captured with light in a darkened room. Proptosis and enophthalmos are best captured with a tangential bottom-up shot (online supplemental appendix 1—Kellogg).
bmjsem-2023-001644supp001.pdf (112.3KB, pdf)
Radiologic imaging
In situations with suspected high-impact trauma, orbital fractures, central nervous system symptoms such as diplopia and visual field defects, and suspected penetration or perforation with foreign bodies, radiologic imaging of the head and orbit are necessary to assess the extent of injuries. CT is the imaging modality of choice when intraorbital or intraocular foreign bodies are suspected. Detecting wood with CT may be difficult because it appears hypoattenuating in the acute phase, an appearance that mimics that of air. MRI is contraindicated as a suspicious metallic foreign body would aggravate the eye injury. When an open globe injury is suspected, ophthalmic ultrasonography is not recommended as the probe pressure risks the prolapse of ocular contents.32
Immediate or on-field examination
At the pitch side, observe and take note of the injury mechanism. On reaching the athlete, ensure that the athlete is in a safe area, and then assess the airway, breathing and circulation. Where necessary, initiate cardiopulmonary resuscitation in accordance with Advanced Trauma Life Support guidelines. Palpate the orbital margin for fractures (bony step-offs of the orbital rim) and crepitation due to subcutaneous emphysema. Ask the athlete to open their eye voluntarily and assess their visual acuity (finger counting/hand movement/light perception). Assess for diplopia (monocular or binocular), and look for pupillary symmetry, foreign bodies, open globe injury and anterior segment involvement. In the presence of a suspected globe rupture, avoid further manipulations (no pressure, no digital intraocular pressure, no ophthalmic ultrasound scan), and avoid using eye-drops, including mydriatics and eye ointment. Do not attempt to remove foreign bodies from the field. In cases of globe trauma or suspected globe trauma, pads or wet gauze with pressure patches should be avoided. Instead, put on a transparent hard shell eye shield before transporting the patient, and place on nil-by-mouth (in general case anaesthesia is needed later) (table A in online supplemental appendix 5).
Field bag for a sports medicine physician
The recommended ophthalmological items to carry in the field bag include a penlight with blue cobalt light filter cap, direct ophthalmoscope, transparent hard shell eye shield with micropore tape, fluorescein strip, irrigating physiological/balanced solutions and some eye-drops like lubricating, anaesthetic and antibiotic drops (table 2).
Table 2.
Minimum equipment for a sports medicine physician to examine and manage an eye injury on-field
| Item | Purpose |
| Ocular trauma form | Detailed documentation of the type, severity and initial findings of the ocular trauma (online supplemental appendix 3) |
| Fluorescein paper | Evaluation of ocular surface abrasions or penetrating injuries |
| Penlight | More detailed evaluation of tissues under a light Direct/indirect light reflex |
| Pocket visual acuity chart | Assessment of visual acuity |
| Direct ophthalmoscope | Assessment of the presence of media opacity that prevents visualisation of the retina (eg, vitreous haemorrhage) Evaluation of main fundus structures such as optic nerve and macula |
| Eye shield and tape | Prevention of further damage |
| Red bottle caps of mydriatic drops | Confrontational visual field exam |
| Balanced salt solution | Irrigation of ocular surface |
With smartphones’ ubiquitous availability and capabilities, the smartphone can serve as a light source and a camera for photo and video documentation. Further, a commercially available attachable 20D condensing lens turns the smartphone into a convenient funduscopy camera.
Other relevant eye conditions affecting sports activity and performance
Visual symptoms following concussion
Traumatic brain injury (TBI) is the primary cause of trauma-related long-term or permanent disability worldwide. It is categorised as mild, moderate and severe, with 90% of all TBIs being mild to moderate.33 In a mild TBI (mTBI), the most acute symptoms are headache, nausea, dizziness and double vision. Approximately one-half of the brain is devoted to visual processing, and deficits in eye movement and affect recognition are among the impairments reported to arise from mTBI.33 With mTBI, both the afferent and efferent visual pathways can be damaged, disrupting vision.
Sport-related concussion (SRC) is a subset of mTBI and accounts for 20% of all TBIs.32 SRC is an evolving injury in the acute phase, with rapidly changing clinical signs and symptoms, which may reflect the underlying physiological injury in the brain and is among the most complex injuries in sports medicine to diagnose, assess and manage.34 These symptoms can be cognitive, physical, emotional and sleep disturbances. Overall, 80%–90% of SRCs typically resolve within 7–10 days.34 35 However, symptoms can persist for weeks to months in a small subset of athletes. Nearly 30% of concussed athletes report visual problems during the first week after the injury36 and the visual impairments can be caused by accommodative, oculomotor and binocular dysfunction. Visual processing can be disrupted and create issues with balance and hand-eye coordination. Vision can be compromised because of injury to one or both optic nerves, impaired visual processing in diffuse brain injury, or limitation in eye movements because of dysfunction of cranial nerves.37 Ocular motor impairments and symptoms may manifest as blurred vision, diplopia, impaired eye movements, dizziness, photophobia, headaches, ocular pain, difficulty in reading and poor visual-based concentration. Among the most common of these are photophobia and its migraine-like symptoms. Dizziness, which may represent an underlying impairment of the vestibular or ocular motor systems, is reported by 50% of concussed athletes36 and is associated with a 6.4- times greater risk in predicting protracted (>21 days) recovery.38 Prolonged recovery can also be seen when fogginess and blurred vision are present.
Sports medicine physicians are uniquely positioned to diagnose, manage and treat SRC. The need for a multidisciplinary team is widely accepted and viewed as a critical approach to treating SRC’s multifactorial signs and symptoms (online supplemental appendix 2—Vestibular/Ocular-Motor Screening).
bmjsem-2023-001644supp002.pdf (677.8KB, pdf)
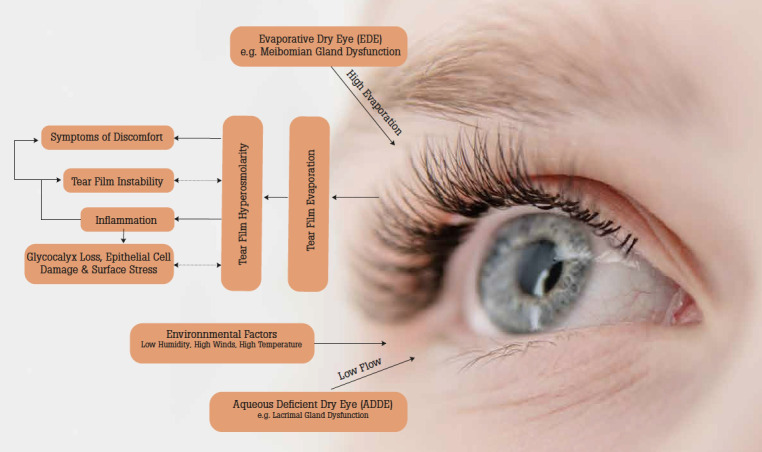
The ocular surface of the eye
Ocular surface diseases (OSDs) encompass a range of pathologies involving the structures and tissues dedicated to the interface between the environment and the highly sensitive external ocular tissues. These protective tissues are of paramount importance, and sight-threatening manifestations may occur in case of loss of both local and extraocular homeostasis and impaired protection sensors (figure 3).
Figure 3.
Ocular surface diseases encompass a range of pathologies involving the structures and tissues.
Adverse environments play a major role in inducing or aggravating dry eye symptoms and OSDs. Dry, windy or dirty environments, air conditioning, blue light and ultraviolet (UV) exposures, pollution, and high altitude, may cause various effects on the ocular surface through oxidative stress, inflammatory, allergic or toxic mechanisms. Video display terminals play a particular role in associating adverse environments, blue light exposure, ocular fatigue and reduced blinking rate.39 40 Other interventions such as chronic use of eye-drops, especially if containing preservatives,41 contact lens wear or refractive surgery are important risk factors of OSD.
Dry eye disease (DED) concerns up to 15% of the general population and approximately 50% of people working or gaming in front of a VDT,42 43 which potentially concerns all electronic sports (Esports) athletes to a level that is still not fully recognised (see paragraph on Esports).
The main consequence of DED is a significant decrease in quality of life (QoL). The symptoms of dry eye, such as sensations of discomfort, foreign body, burning, fluctuating visual disturbances, or tearing, initially intermittent, can become permanent and deeply alter the patient’s QoL and performance.44 DED has thus been shown to impact the QoL at levels comparable to angina pectoris grade III/IV.45
Studies on large cohorts of patients have shown that dry eye significantly negatively impacts many daily activities, such as reading, using a computer, watching television or driving day or night.45 Beyond this impairment of QoL, dry eye is associated with psychological disorders such as anxiety and depression.46
All these elements, symptoms of discomfort or pain, fluctuating vision, glare or even photophobia, are directly influenced by the environment. Athletes can, therefore, be particularly sensitive to the environment they are exposed to. Even more at risk are those individuals who suffer from pre-existing ocular surface pathology: dryness, contact lens wear, skin diseases (eg, seborrheic or atopic dermatitis, rosacea) or allergies. Refractive surgery is of particular significance among the specific risk factors potentially encountered in the sports population. The athlete can, thanks to these procedures, participate in sport without glasses or contact lenses with an undeniable benefit, but dry eye induced in particular by the transection of the corneal nerves can affect up to 30% of individuals with sometimes persistent severe symptoms, and even neuropathic pain that is very difficult to relieve.47 Several cases of suicide have been reported and publicised in the USA, precisely for chronic post-LASIK pain.47
Regarding dry eye and ocular pain therapies, preservative-containing tear substitutes, largely available in OTC, should be avoided as preservatives may aggravate tear instability and cause toxic side effects. Care should be taken to avoid potentially forbidden treatments, like steroids or hormone therapy, cannabinoids or other pain-relievers.
Ultraviolet light exposure and the athlete’s eyes
Besides acute trauma, sports medicine physicians should also be mindful of injuries from excessive exposure to UV light. Sports at increased risk include sailing, surfing and snow sports, where UV rays are reflected off the sea surface and snow, amplifying the exposure.48 49 Excessive UV exposure to the eyes increases the risk of photokeratosis (snow blindness), pinguecula (protein and fat deposits over the sclera, causing eye irritation and disrupting the tear film), pterygium (surfer’s eye, a soft tissue growth that extends from the sclera to the cornea, creeping into the visual axis in severe cases), cataract, basal cell carcinoma and squamous cell carcinoma of the eyelids, and to some degree also the risk for age-related macular degeneration.50–52 However, in adulthood, exposure of the retina to UV radiation is reduced due to decreasing transmission properties of the natural lens.53 These risks can also be effectively reduced using UV-blocking sunglasses and hats.48 49
Sports-related ophthalmology issues in electronic sports
Esports is a developing area in medicine; however, half the world’s population (3+ billion) are estimated to play games regularly. Esports is organised, competitive video gaming and is a worldwide phenomenon. To remain competitive in this popular and sometimes lucrative field, gamers often practice 12 hours daily, performing anywhere from 400 to 600 actions per minute.54 For an esports athlete to perform at an elite level for extended periods, it requires advanced motor skills, mental agility, processing speed, executive function, motivation, and, to a lesser extent, physical exertion. Esports can be played on a personal computer, gaming console (Xbox/PlayStation/Nintendo), mobile device or a head-mounted display. Attention to the needs of gamers and esports athletes has become more prevalent over the past few years with the growth of the industry and the number of professional leagues being established. These needs include optimising visual, mental and physical health and performance, whether casual or professional gaming.
Ophthalmologists and sport medicine practitioners are well positioned to expand their scope of practice into Esports, given the visual, mental and physical demands of gaming.
Visual demands of gaming are inherent and obvious, as one needs to interact with screens at near distances for extended periods constantly. Gamers are experiencing symptoms of blue light toxicity, digital eye strain (asthenopia), also referred to as computer vision syndrome (CVS), including blurred vision, dry eye, photophobia, double vision and uncontrolled blinking (blepharospasm).55 Non-ocular symptoms associated with eye strain include a stiff neck, general fatigue, headache and backache. The opportunity to educate gamers on proper digital hygiene (20/20/20 rule), identify technologies to monitor vision performance, including the vision performance index (VPI), and treatment options for digital eyestrain as an Esports eye care practitioner are becoming practical and necessary.
Ninety per cent of computer users, who spend more than 3 hours a day in front of the computer screen, suffer from CVS.57 Its multifactorial pathophysiology includes ocular-surface abnormalities, accommodative spasms and ergonomics. A general rule of visual ergonomics that can be effective for gamers to help reduce eye strain is the 20-20-20 rule, which instructs them to briefly look away from the screen for at least 20 s to a distant scene at least 20 feet (6 m) away after every 20 min of continuous screen time. Treatment for CVS can include preservative-free lubricating drops, correction of accommodation issues and astigmatism with optical lenses with different coatings or prisms, improving ergonomics with proper positioning of the gaming set-up and chair, optimising ambient lighting and reduction of blue light with filters, screens and lenses.
The VPI is a holistic assessment tool for measuring, analysing and monitoring vision, cognition and motor function while engaging in interactive media. The VPI is readily accessible through games and other interactive software applications. The VPI comprises over 100 psychometrics generated from user response to stimuli during gameplay,58 and measures 5 dimensions across vision, cognition and motor function. These dimensions include:
Field of view—Identifying stimuli in the central and peripheral field of view.
Accuracy—Decision-making between targets and distractors, along with intentional movements and reaction time to those targets.
Multitracking—Attention and multitasking, involving focused and divided task execution.
Endurance—Ability to perform over time with measures of fatiguability and recoverability.
Detection—Distinguishing features between stimuli, including size discrimination, colour and contrast.
The VPI dimensions allow esports athletes, coaches and trainers to identify strengths and weaknesses, monitor the therapeutic effects of interventions to improve performance and personalise training programmes to game/role-specific skill sets.
With the evolution of the esports industry, Esports medicine will continue to grow. The need for education and awareness of CVS, implementation of preventative eye health strategies and promotion of healthy digital lifestyles for gamers, healthcare practitioners and other key stakeholders are paramount for this emerging field. Additionally, damage to the retina with extended screen time, blue light exposure and increased rates of myopia are areas of concern for esports athletes and gamers. Along with advancements in research on the effects of screen time on the visual system, there will be a significant opportunity for exploring and understanding the intimate relationship between the eye-brain-body.
Subclinical ocular pathologies affecting sports performance
Subclinical ocular pathologies and ambiguous complaints may go unnoticed and undiagnosed in the acute phase of sports injury/illness or are easily overlooked during the routine ophthalmic examination. For example, athletes may be at increased risk of intractable chronic central serous chorioretinopathy development due to the heavy physical and mental stress associated with competitive sports. The use of prohibited drugs can also increase the risk.59 Athletes may also be at increased risk of visual symptoms brought on by repeated concussion events. Hence, improved screening methods must be developed to help identify and manage visual symptoms and guide treatment and the required time for the athlete to return to sport.60–62 If accompanying pathologies such as subclinical retinal, optic nerve and mild brain abnormalities are not detected and treated properly, these pathologies affecting visual quality may also impact performance or predispose further injury.63 For example, even if the best corrected visual acuity is normal or restored postinjury, accompanying retina, retinal ganglion cells, optic nerve injuries and other brain abnormalities may impact visual performance. New and more specific technologies and examination protocols must be developed to detect better and diagnose ambiguous subclinical eye pathologies that will undoubtedly impact vision and, therefore, sporting performance. Multimodal imaging techniques such as optical coherence tomography angiography,64–66 digital vision screener and electrophysiologic tests (eg, retinal function analyzer)67 68 are some of the approaches being trialled and tested to comprehensively evaluate the structural and functional components of the visual pathways for more appropriate diagnosis and treatment of visual impairments. Such developments with particular relevance to identifying visual impairments and ambiguous subclinical eye pathologies in sports must be accelerated.
Prevention
Ninety per cent of all sport-related ocular injuries are preventable with suitable eye protection.69 70 The World Squash Federation (WSF) World Championship regulations require juniors (under 9 years) playing any WSF Team Championship or any WSF Junior Individual Championship to wear appropriate eyewear. No reports of significant ocular injuries have been published subsequently.70 Visors have decreased the incidence of eye injuries in ice hockey.6 71–73 Protective eyewear (goggles) significantly reduced eye injuries in high school hockey and squash.74 75 76
Several Nordic and central European countries have a special interest in floorball eye trauma due to its high prevalence.8 74 77 For example, in a Finnish study, 17% of all eye injuries were sports related, and 45% were caused by floorball.8 Due to these findings, the Finnish Floorball Federation made protective eyewear mandatory in junior floorball. Educational interventions can be beneficial by spreading information about the importance of using safety equipment. By modifying the sport’s rules and promoting safety measures, sports‐related eye injuries and consequent visual impairments and blindness can be prevented.
The American Academy of Pediatrics and Academy of Ophthalmology strongly advocate using eye protection in sports, which carries the risk of an eye injury.26 78 79 Eye protection in sports should be mandatory in functionally one-eyed athletes and after eye surgery.
Overall recommendations published by Dain7 include all International, National and regional standards of eye protection in sports and reveal a high heterogeneity between regions and sports in relation to eye protection.
Recommended eye protection for sports will be provided by either faceguards/visors (attached to helmets) or sports eye guards (goggles or spectacles). Polycarbonate lenses must be used with protectors that meet or exceed the requirements of the current sport-specific ASTM (American Society for Testing and Materials).
Vision and performance
Vision, just like speed and strength, is a critical component in elite sports performance. Vision generates stimuli that can enhance eye-hand coordination making it essential for successful sports performance. However, athletes, in general, rarely consider or train vision. There is also very limited research regarding performance benefits for elite competitors. Nevertheless, the theoretical role of the visual system, areas of the brain that employ vision to make decisions, and how decisions are integrated to generate an intended motor response potentially leading to improved performance can be illustrated by the sports vision pyramid (goal, visual integration, monocular sensory processes, binocular sensory processes, neural processing).2 80
All five levels of the pyramid depend on appropriate input from other levels. It is proposed that correcting or training any one level without optimal information from a level below will impact performance negatively.80 The lowest level of the pyramid begins with the basic visual abilities of each eye, termed ‘monocular sensory processes’, which include visual acuity and contrast sensitivity. Visual acuity is the commonly known score (eg, 20/20 or 20/30), while contrast sensitivity describes the ability to pick out a target from a similar low-contrast background.80 Also relevant to elite sports performance is presentation time, that is, seeing a target for a fraction of a second (eg, shooting). The input of basic visual information from both eyes is integrated and processed to appreciate the depth, which is critical to many sports. According to the sports vision pyramid, the neural processing level concerns how the basic visual information is used and processed to make a decision heavily influenced by an athlete’s prior experience. Once a decision is made, the visual information must be coordinated with hand, foot and body movements to carry out a task. Interventions range from excimer eye laser treatment, glasses or contact lenses to correct problems with visual acuity at the base of the pyramid, to the training of hand/eye/foot coordination, or the ability to track multiple targets at the upper levels. Understanding and evaluating the visual ability needed at each level for each sport (and position within a sport) and then correcting deficits will be necessary for sustained high-level performance. The main testing methods that can be applied to elite sports are described in Table 1 in online supplemental appendix 4.
bmjsem-2023-001644supp004.pdf (158.6KB, pdf)
There are anecdotal accounts that some athletes possess a kind of enhanced visual perception that allows them to eliminate any distractions as they plan their next move, especially during times of stress—a phenomenon known as ‘quiet eye’.81 The quiet eye represents one of the most well-studied visual strategies in sports. It is defined as a gaze behaviour that differentiates expert-novice performance from successful and unsuccessful performance in experts.81 Inevitably, differences in vision and visual-motor coordination skills between athletes and non-athletes exist, and it remains to be determined whether perceptual-cognitive differences between athletes and non-athletes can be explained fully by the quiet eye idea alone.
Shooting is one example of a sport where vision plays a paramount role in performance. Shooting requires intense focus, concentration and precision, further compounded by the pressure of competition, spectators and the allotted time to make the shot. It is not surprising, therefore, that improving key visual skills such as the ones described in online supplemental appendix 4, table 2 can lead to significant increases in performance.
There is much anecdotal support for the idea that strong visual skills are just as important to an athlete’s success as conditioned skeletal muscles. As with this link between vision and performance, there is a good theoretical underpinning for visual training to improve sports performance. However, whether vision training has a direct transfer to the sport-field setting remains unclear according to the field of science, but several performance metrics following visual training, both sport-specific and non-sport-specific tests, exist. For example, a group of hockey players who participated in a 6-week sports vision training programme improved the visual tasks used in training. At the same time, no improvements were found on a separate transfer task82 The finding that non-sport-specific vision training period could induce significant performance improvements, was also confirmed in another study involving a tennis field-based test.83 Generalised vision training improved some measures of visual skills, but not all studies did find vision training to improve performance.84 These studies that find a positive effect of generic vision training on sport-specific metrics attribute this finding to the ability of visual training to inhibit attention to task-irrelevant or distracting stimuli.82 83 85 86 Further studies involving vision training, both sport-specific and non-sport-specific, conducted in elite athletes and examining performance in real competition is needed to more definitively resolve the question of the impact of visual training on performance before vision training becomes a mainstay of training and preparation of the elite athlete. This advance will also require larger, better-designed, powered studies with consistent and precise outcome measures.1 Table 3 in online supplemetal appendix 4 describes some of the most commonly used training modalities elite athletes use.
Given the good theoretical underpinning and some evidence linking superior vision and vision training and performance, research on components that help improve vision in sports but also minimise the associated risk of injuries should be encouraged. This collective knowledge, when made available for the athletes, coaches, medical professionals and the larger sports ecosystem to build on further, would help safeguard athletes’ physical health and promote high-level performance.
Conclusion
In the event of an eye injury, sports medicine physicians must assess whether the athlete can return to the field of play, be substituted with another athlete, be referred to an ophthalmologist or be immediately transported to the nearest hospital. This decision requires a good understanding of anatomy, common ocular conditions associated with high-level sports, and knowledge of proper examination techniques by the sports medicine physician. In addition, good eye health is crucial to prevent visual problems in athletes, while regular eye examinations using specialised techniques and equipment allow the early detection and management of visual impairments.
Equity, diversity and inclusion statement
A diverse expert panel of authors consisted of sports medicine physicians, former Olympic athletes as athlete representatives, sports physiologists, sports scientists and mental performance consultants. Authors were invited based on their expertise, as demonstrated by previous research and clinical experiences with Ophthalmology. In total, 3 females and 12 males from 4 continents participated.
Acknowledgments
The authors would like to thank the International Olympic Committee for prioritising and supporting athlete health and well-being. We would also like to thank Geir A. Qvale, Department of Ophthalmology, Oslo University Hospital, for creating the illustrations in figure 1.
Footnotes
Contributors: All authors were involved in the final manuscript’s conception, revising and approval before submission. LE was responsible for leading the consensus project and KS for coordinating the consensus statement manuscript. AB represented the athlete’s voice. RB, UE and LE represented the International Olympic Committee’s Medical and Scientific department.
Funding: No external funding was obtained for this publication. The International Olympic Committee supported the logistics for the related in-person consensus meeting in Lausanne, Switzerland.
Competing interests: RB is the IOC Medical and Scientific Director. LE is the IOC Head of Science Activities and an Editor of BJSM IPHP. UE is an IOC member and the Chair of the IOC Medical and Scientific Commission. KS is coeditor of the British Journal of Sports Medicine—Injury Prevention & Health Protection. BT is a member of the IOC Medical and Scientific Commission, and Vice President of the Singapore National Olympic Council. YPP is a member of the IOC Medical and Scientific Commission, a member of the Executive Committee and Chair of the Scientific Commission of the International Sports Medicine Federation (FIMS), a member of the Scientific and Education Commission of the European Federation of Sports Medicine Associations (EFSMA), a member of WADA’s Health Medical Research Committee (HMRC).
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Laby DM, Appelbaum LG. Review: vision and on-field performance: A critical review of visual assessment and training studies with athletes. Optom Vis Sci 2021;98:723–31. 10.1097/OPX.0000000000001729 [DOI] [PubMed] [Google Scholar]
- 2.Arie B. Sports vision: how enhancing your vision can give you that extra edge in competition. Peak Performance 2003;22:6–8. [Google Scholar]
- 3.Engebretsen L, Steffen K. Protection of the elite athlete is the responsibility of all of us in sports medicine. Br J Sports Med 2015;49:1089–90. 10.1136/bjsports-2015-095221 [DOI] [PubMed] [Google Scholar]
- 4.van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, Aetiology and prevention of sports injuries. A review of concepts. Sports Med 1992;14:82–99. 10.2165/00007256-199214020-00002 [DOI] [PubMed] [Google Scholar]
- 5.Ashraf G, Arslan J, Crock C, et al. Sports-related ocular injuries at a tertiary eye hospital in Australia: A 5-year retrospective descriptive study. Emerg Med Australas 2022;34:794–800. 10.1111/1742-6723.13982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Micieli JA, Easterbrook M. Eye and orbital injuries in sports. Clin Sports Med 2017;36:299–314. 10.1016/j.csm.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 7.Dain SJ. Sports Eyewear protective standards. Clin Exp Optom 2016;99:4–23. 10.1111/cxo.12349 [DOI] [PubMed] [Google Scholar]
- 8.Leivo T, Haavisto AK, Sahraravand A. Sports-related eye injuries: the current picture. Acta Ophthalmol 2015;93:224–31. 10.1111/aos.12633 [DOI] [PubMed] [Google Scholar]
- 9.Gardner EC. Head, face, and eye injuries in collegiate women’s field hockey. Am J Sports Med 2015;43:2027–34. 10.1177/0363546515588175 [DOI] [PubMed] [Google Scholar]
- 10.Haring RS, Sheffield ID, Canner JK, et al. Epidemiology of sports-related eye injuries in the United States. JAMA Ophthalmol 2016;134:1382. 10.1001/jamaophthalmol.2016.4253 [DOI] [PubMed] [Google Scholar]
- 11.Zhang J, Zhu X, Sun Z, et al. Epidemiology of sports-related eye injuries among athletes in Tianjin, China. Front Med (Lausanne) 2021;8. 10.3389/fmed.2021.690528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soligard T, Palmer D, Steffen K, et al. Sports injury and illness incidence in the Pyeongchang 2018 Olympic winter games: a prospective study of 2914 athletes from 92 countries. Br J Sports Med 2019;53:1085–92. 10.1136/bjsports-2018-100236 [DOI] [PubMed] [Google Scholar]
- 13.Soligard T, Palmer D, Steffen K, et al. New sports, COVID-19 and the heat: sports injuries and illnesses in the Tokyo 2020 summer Olympics. Br J Sports Med 2022. 10.1136/bjsports-2022-106155 [DOI] [PubMed] [Google Scholar]
- 14.Soligard T, Steffen K, Palmer D, et al. Sports injury and illness incidence in the Rio de Janeiro 2016 Olympic summer games: A prospective study of 11274 athletes from 207 countries. Br J Sports Med 2017;51:1265–71. 10.1136/bjsports-2017-097956 [DOI] [PubMed] [Google Scholar]
- 15.Soligard T, Steffen K, Palmer-Green D, et al. Sports injuries and illnesses in the Sochi 2014 Olympic winter games. Br J Sports Med 2015;49:441–7. 10.1136/bjsports-2014-094538 [DOI] [PubMed] [Google Scholar]
- 16.Toldi JP, Thomas JL. Evaluation and management of sports-related eye injuries. Curr Sports Med Rep 2020;19:29–34. 10.1249/JSR.0000000000000677 [DOI] [PubMed] [Google Scholar]
- 17.Engebretsen L, Soligard T, Steffen K, et al. Sports injuries and illnesses during the London summer Olympic games 2012. Br J Sports Med 2013;47:407–14. 10.1136/bjsports-2013-092380 [DOI] [PubMed] [Google Scholar]
- 18.Patel PS, Uppuluri A, Oydanich M, et al. Epidemiology of United States tennis-related ocular injuries from 2000 to 2019. Int Ophthalmol 2023;43:997–1003. 10.1007/s10792-022-02502-3 [DOI] [PubMed] [Google Scholar]
- 19.Junge A, Engebretsen L, Alonso JM, et al. Injury surveillance in multi-sport events: the International Olympic committee approach. British Journal of Sports Medicine 2008;42:413–21. 10.1136/bjsm.2008.046631 [DOI] [PubMed] [Google Scholar]
- 20.Bahr R, Clarsen B, Derman W, et al. International Olympic committee consensus statement: methods for recording and reporting of Epidemiological data on injury and illness in sport 2020 (including STROBE extension for sport injury and illness surveillance (STROBE-SIIS)). Br J Sports Med 2020;54:372–89. 10.1136/bjsports-2019-101969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Basic and clinical science course (BCSC) section 02: 2022-2023 fundamentals and principles of Ophth. Available: aao.org
- 22.Spaide RF. CHOROIDAL BLOOD FLOW: review and potential explanation for the Choroidal venous anatomy including the vortex vein system. Retina 2020;40:1851–64. [DOI] [PubMed] [Google Scholar]
- 23.Campbell WG, Pejnovic TM. Treatment of Amelanotic Choroidal Melanoma with Photodynamic therapy. Retina 2012;32:1356–62. 10.1097/IAE.10.1097/IAE.0b013e31822c28ec [DOI] [PubMed] [Google Scholar]
- 24.Kuhn F, Morris R, Witherspoon CD, et al. The Birmingham eye trauma terminology system (BETT). J Fr Ophtalmol 2004;27:206–10. 10.1016/s0181-5512(04)96122-0 [DOI] [PubMed] [Google Scholar]
- 25.Kunz C, Audigé L, Cornelius C-P, et al. The comprehensive AOCMF classification system: orbital fractures - level 3 Tutorial. Craniomaxillofacial Trauma & Reconstruction 2014;7(1_suppl):92–102. 10.1055/s-0034-1389562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petrigliano FA, Williams RJ. 3rd orbital fractures in sport: a review. Sports Med 2003;33:317–22. 10.2165/00007256-200333040-00005 [DOI] [PubMed] [Google Scholar]
- 27.Ohana O, Alabiad C. Ocular related sports injuries. J Craniofac Surg 2021;32:1606–11. 10.1097/SCS.0000000000007618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burnstine MA. Clinical recommendations for repair of isolated orbital floor fractures: an evidence-based analysis. Ophthalmology 2002;109:1207–10. 10.1016/S0161-6420(02)01057-6 [DOI] [PubMed] [Google Scholar]
- 29.Lozada KN, Cleveland PW, Smith JE. Orbital trauma. Semin Plast Surg 2019;33:106–13. 10.1055/s-0039-1685477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scolozzi P. Reflections on a patient-centered approach to treatment of blow-out fractures: why the wisdom of the past must guide our decision-making. J Plast Reconstr Aesthet Surg 2022;75:2268–76.:S1748-6815(22)00229-7. 10.1016/j.bjps.2022.04.034 [DOI] [PubMed] [Google Scholar]
- 31.Kim HS, Jeong EC. Orbital floor fracture. Arch Craniofac Surg 2016;17:111–8. 10.7181/acfs.2016.17.3.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sung EK, Nadgir RN, Fujita A, et al. Injuries of the globe: what can the Radiologist offer Radiographics 2014;34:764–76. 10.1148/rg.343135120 [DOI] [PubMed] [Google Scholar]
- 33.Theadom A, Starkey NJ, Dowell T, et al. Sports-related brain injury in the general population: an Epidemiological study. J Sci Med Sport 2014;17:591–6. 10.1016/j.jsams.2014.02.001 [DOI] [PubMed] [Google Scholar]
- 34.McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport-the 5(Th) international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med 2017;51:838–47. 10.1136/bjsports-2017-097699 [DOI] [PubMed] [Google Scholar]
- 35.Putukian M. The acute symptoms of sport-related concussion: diagnosis and on-field management. Clin Sports Med 2011;30:49–61, 10.1016/j.csm.2010.09.005 [DOI] [PubMed] [Google Scholar]
- 36.Kontos AP, Elbin RJ, Schatz P, et al. A revised factor structure for the post-concussion symptom scale: baseline and Postconcussion factors. Am J Sports Med 2012;40:2375–84. 10.1177/0363546512455400 [DOI] [PubMed] [Google Scholar]
- 37.Cockerham GC, Goodrich GL, Weichel ED, et al. Eye and visual function in traumatic brain injury. J Rehabil Res Dev 2009;46:811–8. 10.1682/jrrd.2008.08.0109 [DOI] [PubMed] [Google Scholar]
- 38.Lau BC, Kontos AP, Collins MW, et al. Which on-field signs/symptoms predict protracted recovery from sport-related concussion among high school football players Am J Sports Med 2011;39:2311–8. 10.1177/0363546511410655 [DOI] [PubMed] [Google Scholar]
- 39.Mehra D, Galor A. Digital screen use and dry eye: A review. Asia Pac J Ophthalmol (Phila 2020;9:491–7. 10.1097/APO.0000000000000328 [DOI] [PubMed] [Google Scholar]
- 40.Fjaervoll H, Fjaervoll K, Magno M, et al. The association between visual display terminal use and dry eye: a review. Acta Ophthalmol 2022;100:357–75. 10.1111/aos.15049 [DOI] [PubMed] [Google Scholar]
- 41.Baudouin C, Labbé A, Liang H, et al. Preservatives in Eyedrops: the good, the bad and the ugly. Prog Retin Eye Res 2010;29:312–34. 10.1016/j.preteyeres.2010.03.001 [DOI] [PubMed] [Google Scholar]
- 42.Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. The Ocular Surface 2017;15:276–83. 10.1016/j.jtos.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 43.Courtin R, Pereira B, Naughton G, et al. Prevalence of dry eye disease in visual display terminal workers: a systematic review and meta-analysis. BMJ Open 2016;6:e009675. 10.1136/bmjopen-2015-009675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Friedman NJ. Impact of dry eye disease and treatment on quality of life. Curr Opin Ophthalmol 2010;21:310–6. 10.1097/ICU.0b013e32833a8c15 [DOI] [PubMed] [Google Scholar]
- 45.Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and validity of the ocular surface disease index. Arch Ophthalmol 2000;118:615–21. 10.1001/archopht.118.5.615 [DOI] [PubMed] [Google Scholar]
- 46.Labbé A, Wang YX, Jie Y, et al. Dry eye disease, dry eye symptoms and depression: the Beijing eye study. Br J Ophthalmol 2013;97:1399–403. 10.1136/bjophthalmol-2013-303838 [DOI] [PubMed] [Google Scholar]
- 47.Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf 2017;15:511–38. 10.1016/j.jtos.2017.05.004 [DOI] [PubMed] [Google Scholar]
- 48.Bulirsch LM, Weber C, Saßmannshausen M, et al. Histological changes in Keratoconus and wound healing after corneal cross-linking [Impact of ultraviolet radiation on the retina]. Ophthalmologe 2022;119:342–9. 10.1007/s00347-021-01537-8 [DOI] [PubMed] [Google Scholar]
- 49.Fonn D. A special issue on ultraviolet radiation and its effects on the eye. Eye Contact Lens 2011;37:167. 10.1097/ICL.0b013e318227a1ef [DOI] [PubMed] [Google Scholar]
- 50.Eisenbeisz HC, Kudrna JJ, Greenwood M, et al. Corneal refractive surgery in the right patient at the right time. S D Med 2021;74:358–62. [PubMed] [Google Scholar]
- 51.Willmann G. Ultraviolet Keratitis: from the pathophysiological basis to prevention and clinical management. High Alt Med Biol 2015;16:277–82. 10.1089/ham.2015.0109 [DOI] [PubMed] [Google Scholar]
- 52.Modenese A, Korpinen L, Gobba F. Solar radiation exposure and outdoor work: an underestimated occupational risk. Int J Environ Res Public Health 2018;15. 10.3390/ijerph15102063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Delcourt C, Cougnard-Grégoire A, Boniol M, et al. Lifetime exposure to ambient ultraviolet radiation and the risk for cataract extraction and age-related macular degeneration: the Alienor study. Invest Ophthalmol Vis Sci 2014;55:7619–27. 10.1167/iovs.14-14471 [DOI] [PubMed] [Google Scholar]
- 54.Bányai FMDG, Király O, Demetrovics Z. The psychology of Esports: a systematic literature review. J Gambl Stud 2019;35:351–65. [DOI] [PubMed] [Google Scholar]
- 55.Kaur K, Gurnani B, Nayak S, et al. Digital eye Strain- A comprehensive review. Ophthalmol Ther 2022;11:1655–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaur K, Gurnani B, Nayak S, et al. Digital eye strain-a comprehensive review. Ophthalmol Ther 2022;11:1655–80. 10.1007/s40123-022-00540-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Erdinest N, Berkow D. Computer vision syndrome [COMPUTER VISION SYNDROME]. Harefuah 2021;160:386–92. [PubMed] [Google Scholar]
- 58.Ahmed SF, McDermott KC, Burge WK, et al. Visual function, Digital behavior and the vision performance index. Clin Ophthalmol 2018;12:2553–61. 10.2147/OPTH.S187131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dağ U, Çağlayan M, Öncül H, et al. Central Serous chorioretinopathy associated with high-dose Follistatin-344: a retrospective case series. Int Ophthalmol 2020;40:3155–61. 10.1007/s10792-020-01501-6 [DOI] [PubMed] [Google Scholar]
- 60.Tzekov R, Quezada A, Gautier M, et al. Repetitive mild traumatic brain injury causes optic nerve and retinal damage in a mouse model. J Neuropathol Exp Neurol 2014;73:345–61. 10.1097/NEN.0000000000000059 [DOI] [PubMed] [Google Scholar]
- 61.Chan JW, Hills NK, Bakall B, et al. Indirect traumatic optic neuropathy in mild chronic traumatic brain injury. Invest Ophthalmol Vis Sci 2019;60:2005–11. 10.1167/iovs.18-26094 [DOI] [PubMed] [Google Scholar]
- 62.Ciuffreda KJ, Kapoor N, Rutner D, et al. Occurrence of Oculomotor dysfunctions in acquired brain injury: a retrospective analysis. Optometry 2007;78:155–61. 10.1016/j.optm.2006.11.011 [DOI] [PubMed] [Google Scholar]
- 63.Master CL, Scheiman M, Gallaway M, et al. Vision diagnoses are common after concussion in adolescents. Clin Pediatr (Phila) 2016;55:260–7. 10.1177/0009922815594367 [DOI] [PubMed] [Google Scholar]
- 64.Jiang H, Wei Y, Shi Y, et al. Altered macular Microvasculature in mild cognitive impairment and Alzheimer disease. J Neuroophthalmol 2018;38:292–8. 10.1097/WNO.0000000000000580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lanzillo R, Cennamo G, Criscuolo C, et al. Optical coherence tomography angiography retinal vascular network assessment in multiple sclerosis. Mult Scler 2018;24:1706–14. 10.1177/1352458517729463 [DOI] [PubMed] [Google Scholar]
- 66.Yanik Odabaş Ö, Demirel S, Özmert E, et al. Repeatability of automated vessel density and superficial and deep foveal avascular zone area measurements using optical coherence tomography angiography: diurnal findings. Retina 2018;38:1238–45. 10.1097/IAE.0000000000001671 [DOI] [PubMed] [Google Scholar]
- 67.Wroblewski JJ, McChancy C, Pickel K, et al. Reproducibility of fixed-Luminance and multi-Luminance flicker electroretinography in patients with diabetic retinopathy using an office-based testing paradigm. J Diabetes Sci Technol 2020;14:1095–103. 10.1177/1932296819882719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pescosolido N, Barbato A, Stefanucci A, et al. Role of electrophysiology in the early diagnosis and follow-up of diabetic retinopathy. J Diabetes Res 2015;2015. 10.1155/2015/319692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Goldstein MH, Wee D. Sports injuries: an ounce of prevention and a pound of cure. Eye Contact Lens 2011;37:160–3. 10.1097/ICL.0b013e31821790db [DOI] [PubMed] [Google Scholar]
- 70.Hoskin AK, Mackey DA, Keay L, et al. Eye injuries across history and the evolution of eye protection. Acta Ophthalmol 2019;97:637–43. 10.1111/aos.14086 [DOI] [PubMed] [Google Scholar]
- 71.Micieli JA, Zurakowski D, Ahmed IIK. Impact of Visors on eye and orbital injuries in the National hockey League. Can J Ophthalmol 2014;49:243–8. 10.1016/j.jcjo.2014.03.008 [DOI] [PubMed] [Google Scholar]
- 72.Micieli R, Micieli JA. Visor use among national hockey League players and its relationship to on-ice performance. Inj Prev 2016;22:392–5. 10.1136/injuryprev-2015-041900 [DOI] [PubMed] [Google Scholar]
- 73.Micieli R, Micieli JA. Factors influencing visor use among players in the National hockey league (NHL). Open Access J Sports Med 2014;5:43–6. 10.2147/OAJSM.S61010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Maxén M, Kühl S, Krastl G, et al. Eye injuries and orofacial Traumas in Floorball--a survey in Switzerland and Sweden. Dent Traumatol 2011;27:95–101. 10.1111/j.1600-9657.2010.00960.x [DOI] [PubMed] [Google Scholar]
- 75.Eime R, Finch C, Wolfe R, et al. The effectiveness of a squash Eyewear promotion strategy. Br J Sports Med 2005;39:681–5. 10.1136/bjsm.2005.018366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kriz PK, Zurakowski D, Almquist JL, et al. Eye protection and risk of eye injuries in high school field hockey. Pediatrics 2015;136:521–7. 10.1542/peds.2015-0216 [DOI] [PubMed] [Google Scholar]
- 77.Ghosh F, Bauer B. Sports-related eye injuries. Acta Ophthalmol Scand 1995;73:353–4. 10.1111/j.1600-0420.1995.tb00042.x [DOI] [PubMed] [Google Scholar]
- 78.Drolsum L. Eye injuries in sports. Scand J Med Sci Sports 1999;9:53–6. 10.1111/j.1600-0838.1999.tb00207.x [DOI] [PubMed] [Google Scholar]
- 79.American Academy of Pediatrics, Committee on Sports Medicine and Fitness, American Academy of Ophthalmology, Eye Health and Public Information Task Force . Protective Eyewear for young athletes. Ophthalmology 2004;111:600–3. 10.1016/j.ophtha.2003.12.027 [DOI] [PubMed] [Google Scholar]
- 80.Laby DL, Kirschen DG. A new model for sports and performance vision. Vision Development & Rehabilitation 2018;4. [Google Scholar]
- 81.Dalton K. Review: the quiet eye in sports performance-is the quiet eye the ultimate explanation or only the beginning? Optom Vis Sci 2021;98:732–7. 10.1097/OPX.0000000000001728 [DOI] [PubMed] [Google Scholar]
- 82.Schwab S, Memmert D. The impact of a sports vision training program in youth field hockey players. J Sports Sci Med 2012;11:624–31. [PMC free article] [PubMed] [Google Scholar]
- 83.Maman P, Gaurang S, Sandhu JS. The effect of vision training on performance in tennis players. Serb J Sports Sci 2011;5:11–6. [Google Scholar]
- 84.Abernethy B, Wood JM. Do generalized visual training programmes for sport really work? an experimental investigation. J Sports Sci 2001;19:203–22. 10.1080/026404101750095376 [DOI] [PubMed] [Google Scholar]
- 85.Di Noto P, Uta S, DeSouza JFX. Eye exercises enhance accuracy and letter recognition, but not reaction time, in a modified rapid serial visual presentation task. PloS One 2013;8:e59244. 10.1371/journal.pone.0059244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Clark JF, Ellis JK, Bench J, et al. High-performance vision training improves batting statistics for University of Cincinnati baseball players. PLoS One 2012;7. 10.1371/journal.pone.0029109 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2023-001644supp003.pdf (226.1KB, pdf)
bmjsem-2023-001644supp005.pdf (55KB, pdf)
bmjsem-2023-001644supp001.pdf (112.3KB, pdf)
bmjsem-2023-001644supp002.pdf (677.8KB, pdf)
bmjsem-2023-001644supp004.pdf (158.6KB, pdf)