Abstract
Introduction
At the end of their residency program, urology trainees should reach the minimum skills required to be able to work by themselves and within a team. To achieve this objective, it is fundamental that the training involves not only surgical activities, but also theoretical, academic, and relational ones. What is the perfect balance between these activities within the ideal urological training? This study aims to evaluate the concordance in different concepts of good urological training between different perspectives (trainees vs professors).
Material and methods
Between January and December 2020 the same survey was distributed via email to 967 urology trainees and urology tutors. The survey investigated 5 educational fields: theoretical, clinical, surgical, relational, and simulation. For each field, specific questions investigated the importance of different activities and the training outcomes considered fundamental to be reached by a resident. The questions were evaluated by responders through a Likert 10-point scale.
Results
The survey was completed by 155 trainees (58.9%, Group A) and 108 tutors (41.1%, Group B) from 26 different countries. Relative to the tutors, residents assigned statistically significantly lower scores to prostate biopsy (median score 9.11 vs 9.24), robotic simulator training (5.66 vs 5.93), on-call duties with consultants (6.85 vs 7.99), as well as all aspects of relational training (e.g., proper dialogue with colleagues: 7.95 vs 8.88). Conversely, residents assigned statistically significantly higher scores, albeit below sufficiency, to the performance of robotic prostatectomy as a first operator (4.45 vs 4.26). Finally, no discrepancies between residents’ and tutors’ scores were recorded regarding the remaining items of clinical training (e.g., urodynamics, outpatient clinic, ward duties) and surgical training (e.g., major open, laparoscopic and endoscopic surgical training; all p values >0.05).
Conclusions
There was partial concordance between trainees and tutors regarding the activities that should be implemented and the skills that should be achieved during a urological residency. The residents aimed for more surgical involvement, while the tutors and professors, although giving importance to surgical and theoretical training, considered clinical practice as the fundamental basis on which to train future urologists.
Keywords: urology, training, trainees, education, simulation
INTRODUCTION
The quality of the urology resident training is incredibly important both for trainees and for the country training them [1]. At the end of their training program, urology trainees should reach the minimum skills required to be able to work by themselves and within a team. To achieve this objective, it is fundamental that the training involves not only surgical activities, but also theoretical, academic, and relational ones [2, 3]. What is the perfect balance between these activities within ideal urological training? What do urology residents consider fundamental during their training in order to consider themselves able to work properly as junior consultants? And what is considered important by the academics (professors and tutors) who are responsible for the training? In recent years, training has become a topic under the spotlight, with growing importance day after day, also in urology. Although there are articles evaluating the quality of teaching in some countries, as well as the work conditions, the residents’ laparoscopic and robotics skills, and the use of social media for learning purposes [4–12], a global comprehensive and objective evaluation of ideal urological teaching is still lacking.
This study aims to evaluate the concordance in different concepts of good urological training between different perspectives (trainees vs professors) to provide information that might allow better planning of future national education programs.
MATERIAL AND METHODS
A 57-item survey (supplementary material) including specific questions about urological training during residency was drafted by 2 registrars in urology (GM and DCM) and edited by 3 consultants/professors (JGR, AB, and CT) at tertiary care academic hospitals in Europe.
The authors edited the questions according to the most authoritative text sources, updated literature, and most referenced articles regarding academic and surgical training in urology.
The survey was designed following the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines [13], was uploaded onto Survey-Monkey, and was distributed via e-mail, WhatsApp, and Messenger in 23 European countries among urology residents and urologists (consultants, assistant professors, associate professors, full professors).
The survey was distributed between January and December 2020. Before distribution, we tested the survey for usability and technical functionality. This test was done by distributing the survey link through the urology department of the university of the first affiliated author and verifying the functionality of the web link before distributing it among European residents and consultants. The survey was distributed through national societies’ mailing lists and personal emails sent by European Society of Residents in Urology (ESRU) NCOs to their own countries’ residents and consultants.
The survey consisted of 2 parts: Part 1: General information about the respondents, including age, gender, trainee versus specialist, country of current practice, and length of urological training. Part 2: The survey investigated 5 educational fields: theoretical, clinical, surgical, relational, and simulation. For each field, specific questions investigated the importance of different activities and the training outcomes considered fundamental to be reached by a resident. The questions were evaluated by responders through a Likert 10-point scale.
Responders were divided into 2 groups: Group A (residents in urology) and Group B (consultants, assistants, associates, and full professors in urology). The same survey was administered to both groups.
The mean ± standard deviation (SD) was reported for all variables of interest (continuously coded). The Wilcoxon rank sum test examined the statistical significance of differences in means. In all statistical analyses, R software environment for statistical computing and graphics (R version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria) was used. All tests were 2 sided with a level of significance set at p <0.05.
RESULTS
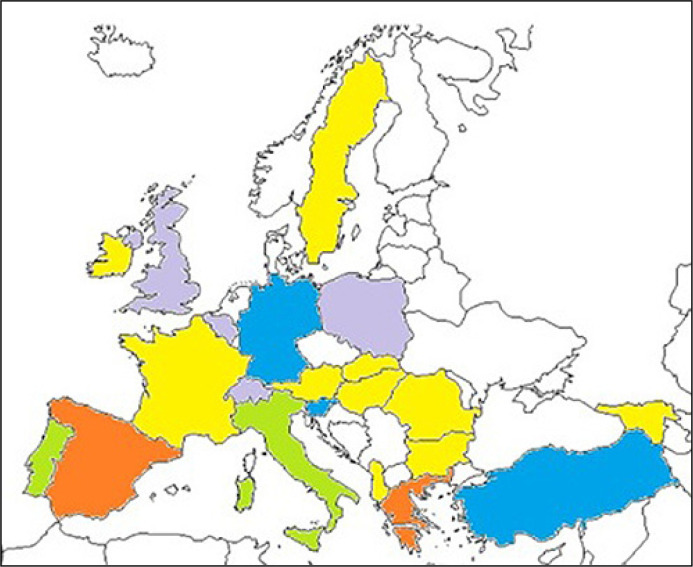
The survey was given to 1024 urologists and residents, and completed by 155 trainees (58.9%, Group A) and 108 tutors (41.1%, Group B). The completion rate was 25.7%. Group A consisted of 42 postgraduate year 2 (PGY2) or below and 113 postgraduate year 3 (PGY3) or above residents, while Group B comprised 75 tutor consultants, 15 associates, 14 assistants, and 4 full professors. The median age of Group A was 30 (28–33) years, and in Group B it was 42.5 (38–48) years. Only 4 (4.32%) responders were female in Group B vs 41 (24.7%) in Group A. Most of the responders were from Greece (n = 114; 43%), Spain (n = 41; 15%), and Italy (n = 24; 9%), followed by Turkey (n = 11; 4%), Germany (n = 9; 3%), and Slovenia (n = 8; 3%) (Figure 1).
Figure 1.
Distribution of responders.
red: countries providing more than 10% of total sample/replies; green: more than 5%; blue: more than 2.5%; purple: more than 1%; yellow: less than 1%
Table 1 displays the mean score assigned by trainees and tutors to each item of the 5 key educational fields of interest. In terms of relevance in the context of an ideal residency program, the theoretical training received stackable scores by the 2 groups, all over 6/10 points. In general, clinical practice was considered more relevant by tutors, from the preoperatory assessment to the post-operative revaluation. Of note, the urodynamics training did not achieve sufficiency among the residents. Both groups rated achieving proper skills in the operating theatre to be of utmost importance, especially in performing prostate biopsies, prostate and bladder endoscopic resections, and ureteroscopies as a first operator. Significant differences, with higher scores assigned by residents, were registered when considering major open surgery as a first operator or table assistant and a trend towards a significative difference regarding laparoscopic nephrectomy as a first operator; for these 3 items the tutors did not assign scores ≥6. The tutors and residents did not confer much importance to the execution of a radical prostatectomy, a urethroplasty, or a kidney transplantation as a first operator; performing a kidney transplantation received the lowest scores in both groups overall. Networking was meant as a fundamental aspect of a proper educational program by the tutors, particularly emphasizing the active attendance at congresses and mutual interplay between colleagues. Residents and tutors agreed that an ideal residency program should include more practice with a laparoscopic simulator rather than a robotic console simulator.
Table 1.
Survey for the assessment of good urological training: scores assigned by residents and tutors within 5 key educational fields
| Group A,n = 155 (58.9%) | Group B,n = 108 (41.1%) | p value | |
|---|---|---|---|
| Theoretical training | |||
| In-clinic exams | 6.43 (±2.48) | 6.59 (±3.02) | 0.028 |
| Lectures from professors to residents | 6.01 (±2.57) | 6.56 (±2.57) | 0.8 |
| Lectures from residents to residents | 6.19 (±2.47) | 6.11 (±2.36) | 0.9 |
| Clinical training | |||
| Ward duties | 7.21 (±2.13) | 7.92 (±1.80) | 0.086 |
| On-call with a consultant | 6.85 (±2.55) | 7.99 (±2.11) | 0.015 |
| Outpatient clinic | 7.33 (±2.22) | 7.99 (±1.76) | 0.2 |
| Urodynamics | 5.89 (±2.48) | 6.40 (±2.39) | 0.5 |
| Ultrasound training | 7.07 (±2.81) | 7.24 (±2.48) | 0.2 |
| Surgical training | |||
| Prostate biopsy, 1st operator | 9.11 (±1.55) | 9.24 (±1.52) | 0.028 |
| TURP, 1st operator | 8.72 (±1.90) | 8.59 (±1.75) | 0.1 |
| TURBT, 1st operator | 8.80 (±1.92) | 8.93 (±1.59) | 0.4 |
| Nephrostomy, 1st operator | 7.65 (±2.82) | 7.27 (±2.81) | 0.3 |
| URS/RIRS, 1st operator | 8.14 (±2.27) | 7.85 (±2.41) | 0.3 |
| Major open surgery, 1st operator | 6.44 (±2.63) | 5.72 (±2.61) | 0.5 |
| Major open surgery, 1st assistant | 6.44 (±2.63) | 5.72 (±2.61) | 0.091 |
| Laparoscopic nephrectomy, 1st operator | 6.29 (±2.92) | 5.69 (±2.58) | 0.1 |
| Laparoscopic nephrectomy, 1st assistant | 7.56 (±2.86) | 7.99 (±2.53) | 0.7 |
| RARP, 1st operator | 4.45 (±2.89) | 4.26 (±2.61) | 0.034 |
| RARP, 1st assistant | 5.84 (±3.36) | 6.72 (±3.11) | 0.3 |
| Urethroplasty, 1st operator | 4.63 (±2.59) | 4.00 (±2.37) | 0.2 |
| Kidney transplantation, 1st operator | 3.94 (±2.84) | 3.25 (±2.37) | 0.1 |
| Relational/social media training | |||
| Participation in congresses | 7.47 (±2.35) | 8.19 (±1.55) | 0.046 |
| Poster presentations at congresses | 6.94 (±2.45) | 7.77 (±1.77) | 0.020 |
| Involvement in urology associations | 7.30 (±2.50) | 7.99 (±1.95) | 0.011 |
| Proper dialogue with colleagues | 7.95 (±2.03) | 8.88 (±1.37) | 0.020 |
| Hands-on / simulator training | |||
| Robotic simulator console | 5.66 (±3.30) | 5.93 (±3.24) | 0.009 |
RARP – robot-assisted radical prostatectomy; URS/RIRS – rigid and flexible ureteroscopy; TURP – transurethral resection of the prostate; TURBT – trans urethral removal of bladder tumour; n – numbers of patients
DISCUSSION
The slow adoption of a surgical training system based on the acquisition of clinical competences [14] and of assessment tools is slowly changing how proctoring is carried out during residency. The acquisition of clinical and surgical skills requires time, and procedures must be repeated several times before proficiency is achieved [15, 16, 17]. Furthermore, current times require the doctor to possess not only surgical and clinical qualities, but also relational and academic ones. However, although these concepts have been repeatedly reaffirmed by the scientific literature in recent years, including in the urological field, it has not yet been determined how ideal training should be structured so that it leads to the formation of competent urologists as required by current times.
This study represents the first report in the European urological field aimed at comparing the opinions of the trainees with those of the tutors, to evaluate any differences in the perception of ideal urological training. Interestingly, the study shows that both trainees and their tutors agreed on a similar optimal value for most of the items. However, differences were found for 13 (28.3%) out of the 46 rating scale items, thus indicating a moderate mismatch between teachers’ and students’ perceptions of training needs. Although the opinions of the 2 groups are quite uniform as regards the theoretical and clinical fields, major differences are found in the surgical and relational/social media fields. Young trainees, understandably, aspire to do more surgery, especially more traditional and robotic major surgery. The tutors, on the other hand, believe that although surgical training is fundamental, the postgraduates must also be more involved in the relational part of the job. Participation in congresses and presentation of scientific works, involvement in urological associations, networking, and a real dialogue with patients and colleagues are considered fundamental parts of ideal training.
These differences of opinion are understandable: trainees enter urology specialization schools because they are attracted by the most active part of the work, i.e., the operating room, which represents a relative novelty for them and for which they are excited. However, tutors and professors know that learning major surgical procedures requires time, experience, and maturity, which often cannot be fully acquired by residents during their specialty, so they cannot be considered completely autonomous during major procedures.
Taken together, the current study takes a step forward on the path of updating and refining the urological training program. Sharing perspectives between residents and tutors is key in the process, as well as among practitioners of countries that may rely on consistently different health care systems (notably, 26 different countries were involved in this study). The process is still far from completion. Active involvement in everyday practice (e.g., clinical and surgical tutoring) will invariably remain the mainstay of a solid and reliable residency program. Nevertheless, investments in technology (e.g., simulator consoles, theorical and hands-on training programs), education and networking (e.g., national and international meetings, research and clinical fellowship programs), and time will continue to play important roles in the development and standardization of the optimal urological training program.
This study has some limitations. First, the sample examined (both tutors and trainees) was not homogeneous according to the country of origin. Greece, Spain, Italy, Turkey, Portugal, Germany, and Slovenia made up the majority of the examined sample. However, we believe that by having multiple responses from different countries, this study can still offer a basic overview of the European situation. Second, among tutors, very few were full professors in urology, compared to associate professors, assistant professors, and academic consultants. Third, the sample was limited to just under 300 responses. This number is small compared to the total number of European postgraduates and professors/tutors. However, it is a good number if compared to recent surveys published on the subject of European training.
CONCLUSIONS
There is just partial agreement between trainees and tutors on activities that should be implemented and skills that should be achieved during urological residency. Residents aim for more surgical involvement, while tutors and professors, albeit giving importance to surgical and theoretical training, consider clinical practice as the fundamental basis on which to train future urologists.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Mantica G, Fransvea P, Virdis F, et al. Surgical Training in South Africa: An Overview and Attempt to Assess the Training System from the Perspective of Foreign Trainees. World J Surg. 2019; 43: 2137-2142. [DOI] [PubMed] [Google Scholar]
- 2.Carrion DM, Rodríguez-Socarrás ME, Mantica G, et al. Interest and involvement of European urology residents in academic and research activities. An ESRU-ESU-ESUT collaborative study. Minerva Urol Nefrol. 2020; 72: 384-387. [DOI] [PubMed] [Google Scholar]
- 3.Carrion DM, Rodriguez-Socarrás ME, Mantica G, et al. Current status of urology surgical training in Europe: an ESRU-ESU-ESUT collaborative study. World J Urol. 2020; 38: 239-246. [DOI] [PubMed] [Google Scholar]
- 4.González Padilla DA, Subiela JD, Carrion DM, et al. Evidence-based Medicine: Perceptions, Attitudes, and Skills Among European Urology Residents. Eur Urol Open Sci. 2022; 45: 44-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mantica G, Chierigo F, Gallo F, et al. Patients' perceptions of quality of care delivery by urology residents: A nationwide study. BJU Int. 2022; 130: 832-838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cocci A, Patruno G, Gandaglia G, et al. ; Senato degli Specializzandi Study Group . Urology Residency Training in Italy: Results of the First National Survey. Eur Urol Focus. 2018; 4: 280-287. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez-Socarras ME, Gomez Rivas J, Garcia-Sanz M, et al. Medical-surgical activity and the current state of training of urology residents in Spain: Results of a national survey. Actas Urol Esp. 2017; 41: 391-399. [DOI] [PubMed] [Google Scholar]
- 8.Borgmann H, Arnold HK, Meyer CP, et al. Training, Research, and Working Conditions for Urology Residents in Germany: A Contemporary Survey. Eur Urol Focus. 2018; 4: 455-460. [DOI] [PubMed] [Google Scholar]
- 9.Soares DS, Chan L. Stress and wellbeing of junior doctors in Australia: a comparison with American doctors and population norms. BMC Med Educ. 2016; 16: 183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mantica G, Rivas JG, Carrion DM, et al. Simulator Availability Index: a novel easy indicator to track training trends. Is Europe currently at a urological training recession risk? Cent European J Urol. 2020; 73: 231-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pereira-Lourenco M, Ucar T, Nikles S, et al. Annual educational expenses of European urology residents and the role of sponsorship in urology training: a survey-based analysis. Cent European J Urol. 2022; 75: 418-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lagrange F, Fiard G, Larose C, Eschwege P, Hubert J. Role and Training of the Bedside Surgeon in Robotic Surgery: A Survey Among French Urologists-in-Training. Res Rep Urol. 2022; 14: 17-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004; 6: e34. Erratum in: J Med Internet Res. 2012; 14: e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller G. The assessment of clinical skills/competence/performance. Acad Med. 1990; 65: s63-s67. [DOI] [PubMed] [Google Scholar]
- 15.Duvivier RJ, Dalen J, Muijtjens AM, Moulaert V, van der Vleuten C, Scherpbier A. The role of deliberate practice in the acquisition of clinical skills. BMC Med Educ. 2011; 11: 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bosse HM, Mohr J, Buss B, et al. The benefit of repetitive skills training and frequency of expert feedback in the early acquisition of procedural skills. BMC Med Educ. 2015; 15: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santonja-Medina F, García-Sanz MP, Santonja-Renedo S, García-Estañ J. Mismatch between student and tutor evaluation of training needs: a study of traumatology rotations. BMC Res Notes. 2018; 11: 826. [DOI] [PMC free article] [PubMed] [Google Scholar]