Abstract
Introduction
The objective of this study is to compare the safety and efficacy, through the stone-free rate (SFR), as well as the costs, between retrograde intrarenal surgery (RIRS) and percutaneous nephrolithotomy (PCNL), for 2–4 cm kidney stones.
Material and methods
We analysed the data relating to RIRS and PCNL performed in 3 reference centres for kidney stones, in the period between 1/2019 and 12/2021. The total number of procedures was 130 (63 RIRS and 67 PCNL). We defined SFR as the absence of lithiasic fragments or stones <3 mm. Results were compared between 2 groups depending on the stone size: 2–3 cm stones (group 1) and >3 cm stones (group 2).
Results
The duration of RIRS was 90 minutes for group 1 and 115 minutes for group 2, and for PCNL it was 135 minutes for group 1 and 145 minutes for group 2. RIRS had shorter duration with a significant difference in group 1 (p = 0.000014). SFR for RIRS was 78% for group 1 and 21% for group 2, and for PCNL it was 92% for group 1 and 81% for group 2. Therefore, there is a statistically significant difference, which is more evident for 3 cm and multiple stones (p = 0.0057 for group 1, p = 0.000146 for group 2). The difference in costs was estimated by calculating the expected costs for a single surgical procedure and the estimated cost per day for ordinary hospitalization.
Conclusions
2–4 cm stones can be safely treated with both RIRS and PCNL, but RIRS should not be chosen as an option for stones >3 cm, except in selected cases. PCNL remains the gold standard for the treatment of complex stones, especially for stones >3 cm. Risk of postoperative complications is higher in PCNL, even if this difference is not great. The costs associated with RIRS, even when recalculating with the need for new treatments, remain cheaper.
Keywords: percutaneous nephrolithotomy, retrograde intrarenal surgery, kidney stones, endourology, costs in urology, stone-free rate
INTRODUCTION
Urolithiasis is the third pathology influencing the urinary system after urinary tract infections and prostate pathologies [1]. Despite the development of alternatives, definitive treatment of stones is performed with extracorporeal shock wave lithotripsy (ESWL) and minimally invasive surgery. For larger stones (>2 cm) possibly requiring additional interventions, other minimally invasive surgical alternatives like percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) could be recommended as the first choice instead of ESWL treatment [2]. PCNL was first practiced around 40 years ago, and since then it has undergone many modifications and innovations, and minimization. The modifications have been focused on achieving greater stone clearance and reducing morbidity, surgical time, and the duration of hospital stay [3]. The complications include haemorrhage and organ trauma, which occur as a result of the creation of the tract and dilation in the standard PCNL. Minimizing the size of the instruments as well as the introduction of laser technology and improvement of the optical systems have resulted in a reduction in the rate of the complications and the invention of new techniques [4]. RIRS is performed through natural orifices. It can decrease the duration of the hospital stay and the risk of haemorrhage. Studies indicate that although the safety is greater, RIRS may not be very effective in the management of stones larger than 2 cm [5]. RIRS with a holmium laser is an effective technique for the treatment of renal lithiasis, but the largest stone size is related with the need for retreatments, so it must be taken into consideration, especially for stones larger than 2 cm [6].
However, the choice of surgical intervention depends on the stone characteristics, patient anatomy, comorbidities, and choice. For ureteroscopy (URS), a postoperative stent is not needed in uncomplicated cases. RIRS is an alternative if PCNL or ESWL is contraindicated, even for stones >2 cm. For PCNL, prone and supine approaches are equally safe. For uncomplicated PCNL cases, a nephrostomy tube after PCNL is not necessary [7].
The objective of this study is to compare the safety and efficacy, through the stone-free rate (SFR), as well as the costs, between RIRS and PCNL for kidney stones >2 cm and multiple kidney stones.
MATERIAL AND METHODS
In our study we retrospectively analysed the data relating to RIRS and PCNL performed in 3 reference centres for kidney stones in the period between 1/2019 and 12/2021. A total of 130 cases (63 RIRS and 67 PCNL), encompassing 2–4 cm or multiple (for example 2/3 stones of 15 mm each) stones, were treated after obtaining informed consent.
Age, performance status according to the Charlson kidney score, number of stones, duration of procedures, intra- and postoperative complications, side treated, and location of the stone (upper, middle, lower calyx or renal pelvis) were recorded.
PCNL was performed in a supine position with Valdivia modification or in a prone position. Both modalities have advantages and disadvantages. Both procedures require placement of an occluding ureteral catheter (usually 5 F). The supine position has the advantage of maintaining a single position throughout the operation, allowing better management by the anaesthetist and the possibility to integrate with a retrograde procedure. The main disadvantage is the lack of expertise of some urologists in puncture through the supine position. The prone position has the advantage of being better known by urologists, but the management is more difficult for the anaesthetists, a change of position is required after the placement of an occluding catheter, and the duration of surgery is longer. We analysed the puncture mode for renal access (radio- or ultrasound-guided), the diameter of the nephroscopy sheath, and the energy used for lithotripsy (laser, usually from 550 μm to 1000 μm fibres, ballistic and ultrasonic).
For all RIRS a holmium laser was the source of energy used in lithotripsy, with 220 μm and 365 μm fibres. Six distinct power settings were tested, including 0.2–2.0 J and 10–40 Hz. The duration was measured for all surgical procedures. The intra- and postoperative complications were recorded and classified according to the Clavien-Dindo scale. The number of days of hospitalization was also recorded. We defined the SFR, in our work, as the absence of lithiasic fragments or stones <3 mm. We compared all these parameters, looking for similarities and differences between PCNL and RIRS, considering that the surgeons were experienced in the procedures (>50 procedures each). We looked for statistically significant differences using Student's t-test. We also included an important discussion regarding data in the literature comparing RIRS and PCNL, and then drew conclusions. All the results were compared between 2 groups depending on stone size: 2–3 cm stones (group 1) and >3 cm stones (group 2).
RESULTS
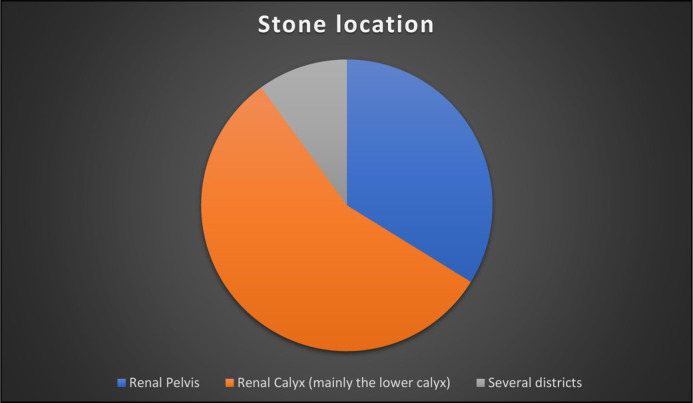
We treated 130 patients, 63 with RIRS and 67 with PCNL. The median age was 56 years (σ = 12.81). Ninety-eight per cent of the procedures were unilateral. Only 3 procedures were bilateral with RIRS, and all of these were partial with duration >2 h. In 72 procedures (55%) the kidney stones were multiple or staghorn calculi. The median value of the maximum diameter of single stones, thus also including multiple stones, was 20 mm (σ = 7.00). Forty-four patients (33.8%) had stones exclusively in the renal pelvis, 73 patients (56.2%) had stones exclusively in a renal calyx (mainly the lower calyx), and 13 patients (10%) had stones with the involvement of several locations (Figure 1). In over 85% of PCNL procedures the sheath diameter was 22–24 F. In a few selected cases, with complex staghorn stones, a 30 F sheath was used. In all RIRS, except for 2 procedures, we used an access sheath, and the diameter used for the ureteral sheath was 11–13 F. We created 2 groups to analyse the results: 2–3 cm stones and >3 cm stones (group 1 and group 2, respectively). The distribution of stone sizes is presented in Figure 2.
Figure 1.
The most frequent locations with relative percentages: 33.8% in the renal pelvis, 56.2% exclusively within a renal calyx (mainly the lower calyx), 10% with the involvement of several locations.
Figure 2.
Distribution of stone sizes.
The median duration of RIRS was 90 minutes for group 1 and 115 minutes for group 2. The median duration of PCNL was 135 for group 1 and 145 minutes for group 2 (Table 1, Table 2). The difference in duration between RIRS and PCNL was statistically significant in group 1 (p = 0.000014).
Table 1.
Retrograde intrarenal surgery (RIRS) and percutaneous nephrolithotomy (PCNL) are compared in group 1 (2–3 cm stones). The median value is considered in the duration box and for days of hospitalization. The stone-free rate (SFR) is shown in the last box
| Number of procedures | Duration [minutes] | Intraoperative complications | Clavien-Dindo 1 | Clavien-Dindo 2 | Clavien-Dindo 3 | Days of hospitalization | SFR [%] | |
|---|---|---|---|---|---|---|---|---|
| PCNL | 20 | 135 | 2 | 2 | 3 | 1 | 5 | 92 |
| RIRS | 45 | 90 | 0 | 3 | 0 | 0 | 2 | 78 |
Table 2.
Retrograde intrarenal surgery (RIRS) and percutaneous nephrolithotomy (PCNL) are compared in group 2 (stones >3 cm). The median value is considered in the duration box and for days of hospitalization. The stone-free rate (SFR) is shown in the last box
| Number of procedures | Duration [minutes] | Intraoperative complications | Clavien-Dindo 1 | Clavien-Dindo 2 | Clavien-Dindo 3 | Days of hospitalization | SFR [%] | |
|---|---|---|---|---|---|---|---|---|
| PCNL | 47 | 145 | 1 | 2 | 1 | 1 | 5 | 81 |
| RIRS | 18 | 115 | 0 | 2 | 0 | 0 | 2 | 21 |
In PCNLs, ultrasonic energy was used exclusively for 22.2% of the procedures. In the other procedures the energy was used in hybrid mode (e.g. ultrasonic + pneumatic; ultrasonic + holmium laser). In RIRS the lithotripsy of stones was obtained by laser energy, both with dusting and fragmented, depending on the operator's choice, through 200–365 μm fibres.
There were no intraoperative complications in RIRS, although the procedures did not last longer than 2 h, so in some cases the stone lithotripsy was partial. Five patients had fever (Clavien-Dindo 1) that required an extension of the hospital stay. The median value for hospital stay was 2 days for RIRS (σ = 1.66). For PCNL 3 patients had intraoperative bleeding that required discontinuation of procedure. Four patients had fever (Clavien-Dindo 1), 4 patients had post-operative anemization that required blood transfusion (Clavien-Dindo 2), one patient required arterial embolization, and one patient had renal pelvis injury requiring placement of ureteral stenting and retroperitoneal drainage (both Clavien-Dindo 3). The difference in postoperative complications shows a statistically significant difference, but with low relevance (p = 0.011). The median value for hospital stay was 5 days for PCNL (σ = 4.2).
The SFR for RIRS was 78% for group 1 and 21% for group 2 (Table 1, Table 2). The SFR for PCNL was 92% for group 1 and 81% for group 2 (Figure 3). Therefore, there is a statistically significant difference, which is even more evident for stones >3 cm and multiple stones (p = 0.0057 for group 1 and p = 0.000146 for group 2).
Figure 3.
Graph showing the differences in the SFR between the 2 groups. A large difference is evident in group 2. SFR – RIRS group 1: 78%, SFR – RIRS group 2: 21%, SFR – PCNL group 1: 92%, SFR – PCNL group 2: 81% (p = 0.0057 for group 1, p = 0.000146 for group 2).
RIRS – retrograde intrarenal surgery; PCNL – percutaneous nephrolithotomy; SFR – stone-free rate
The difference in costs was estimated by calculating the expected costs for the single surgical procedure (€1700 for RIRS and €4300 for PCNL) and the estimated cost per day for normal hospitalization (€709.23).
The median hospital stay was 2 days for RIRS and 6 for PCNL, so we can estimate a total cost of €3118.46 for RIRS and €8555.38 for PCNL. By calculating the difference in costs over 100 procedures, excluding the costs of prolonged hospitalization due to complications, we can deduce that the estimated costs are €311,846 for 100 RIRS and €855,538 for 100 PCNL.
DISCUSSION
PCNL is the first choice in the management of large stones, but life-threatening complications can occur [8]. PCNL may not be suitable in patients with obesity, bleeding disorders, and anatomic anomalies complicating percutaneous access [9, 10]. However, in a systematic review and network meta-analysis by Doo Yong Chung et al. PCNL showed the highest success and stone-free rate in the surgical treatment of renal stones [11]. In our study we compared PCNL and RIRS by analysing the effectiveness through the stone-free rate, as well as the complication rate and the costs of performing the procedures and hospital stays. It is evident, also from the data in the literature, that for stones >2 cm or multiple stones, PCNL seems to be the most effective treatment. However, RIRS is a safe method and has fewer complications and shorter hospitalization time [12].
Postoperative complications in our study, in agreement with the data in the literature, were significantly fewer in RIRS, especially the need for blood transfusions; hence, RIRS has a high efficiency for the management of intrarenal stones and with fewer complications [13, 14].
Another parameter to consider is the expertise needed for PCNL. It is a routine procedure for urologists, but hands-on training for PCNL is still not adequate in most institutions during the residency period. Hence, before starting an independent practice, a urologist must spend a further 1-2 years in a high-volume centre to attain expertise in PCNL, to improve and modify their skills in performing the procedure and to reduce the likelihood of adverse outcomes [15]. Even for the most experienced urologist, complications can occur – up to 7% of patients undergoing PCNL suffer a major complication, and minor complications may be encountered in up to 25% of patients [16].
Although RIRS is a safe and effective procedure (less so for large stones), the need for re-treatment is greater than that of PCNL. One of the risks of a new treatment is the development ureteral stricture. It is one of the more serious complications that may occur after ureteroscopy. Approximately 2 decades ago, the reported incidence of ureteral stricture after ureteroscopy was as high as 10%. More recently, however, the incidence of a postoperative stricture is reported to be 3% to 6% [17]. Another possible reason for a second procedure after RIRS is the greater risk of infection because of the stent indwelling time.
The choice between RIRS and PCNL is based on several features, the first of which comprises the anatomical characteristics: the surgeon must perform the procedure while optimizing the effectiveness and reducing the risk of complications. For example, an obese patient and/or an abnormally positioned kidney may cause difficulties in the access of the calyx to perform PCNL. On the other hand, a severe ureteral stenosis, although the stones may seem easily accessible and susceptible to laser lithotripsy, can make retrograde access impossible with RIRS. The patient's comorbidities may also necessitate a shift from PCNL to RIRS, for example in patients with chronic renal insufficiency, anaemia, or solitary kidney. Finally, the choice of the patient must be considered, with awareness of the benefits and risks associated with the procedure. The patient should be informed that, in the case of complex stones (>3 cm), the effectiveness of RIRS is very low and the risk of reoperation is high.
A further analysis was carried out on the costs of the procedures. So-Young Yang et al. performed a study based on the non-retreatment rates (NRRs) and the respective real-world costs for RIRS and ESWL. They were derived through retrospective analysis of health insurance claims data from 2015 to 2017. Decision tree modelling was performed to demonstrate the cost-effectiveness of RIRS. Probabilistic modelling also indicated that the introduction of RIRS as the first line of treatment was less likely to be cost-effective than the other options of introducing RIRS as the second, third, or fourth line of treatment. The conclusion of this study was that performing RIRS as early as possible should be recommended for eligible patients, to reduce the overall failure rate, even if it is not as cost-effective as performing RIRS later [18].
In our study we compared the costs of PCNL and RIRS considering mainly surgery and hospitalization, referring to the median values, as described in 'Results'. This would seem not to favour PCNL with its much higher costs. However, considering that RIRS often requires re-treatment, especially for stones >3 cm, the costs of this would increase.
If we consider the costs of a new single treatment, we can say that to perform 100 RIRS, with satisfactory SFR, the real costs would be €561,322.80, and €1,026,645.60 for PCNL. Therefore, if from first analysis the difference in costs for 100 procedures is €543,692, from second analysis it appears to be reduced, i.e. €465,322.80. We can therefore conclude that, despite the need for new treatments, RIRS remain cheaper than PCNL. However, in our analysis, the difference in SFR in group 2 (stones >3 cm) was very large: 81% (PCNL) vs 21% (RIRS). This suggests that patients undergoing RIRS can also undergo multiple treatments, thus increasing the cost of RIRS, the anaesthetic risk, and iatrogenic ureteral stenosis, making PCNL highly advantageous.
CONCLUSIONS
2–4 cm stones can be safely treated with both RIRS and PCNL, but RIRS should not be chosen as an option for stones >3 cm, except in selected cases. PCNL remains the gold standard for the treatment of complex stones, especially for stones >3 cm. The risk of postoperative complications (especially anaemia) is higher in PCNL, but this difference is not great. The costs of RIRS remain cheaper even when recalculating including the need for more treatments, but for stones >3 cm the need for multiple treatments makes PCNL highly advantageous.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Türk C, Petřík A, Sarica K, et al. EAU Guidelines on diagnosis and conservative management of urolithiasis. Eur Urol. 2016; 69: 468-674. [DOI] [PubMed] [Google Scholar]
- 2.Türk C, Petřík A, Sarica K, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016; 69: 475-482. [DOI] [PubMed] [Google Scholar]
- 3.Jones P, Elmussareh M, Aboumarzouk OM, Mucksavage P, Somani BK. Role of minimally invasive (Micro and Ultra-mini) PCNL for adult urinary stone disease in the modern era: evidence from a systematic review. Curr Urol Rep. 2018; 19: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De S, Autorino R, Kim FJ, et al. Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol. 2015; 67: 125-137. [DOI] [PubMed] [Google Scholar]
- 5.Li Z, Lai C, Shah AK, et al. Comparative analysis of retrograde intrarenal surgery and modified ultra-mini percutaneous nephrolithotomy in management of lower pole renal stones (1.5–3.5 cm). BMC Urol. 2020; 20: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palmero-Martí JL, Panach-Navarrete J, Valls-González L, Ganau-Ituren A, Pastor-Lence JC, Benedicto-Redón A. Renal lithiasis, can we predict the need for retreatment in retrograde intrarenal surgery (RIRS)? Arch Esp Urol. 2017; 70: 534-541. [PubMed] [Google Scholar]
- 7.Geraghty RM, Davis NF, Tzelves L, et al. Best practice in interventional management of urolithiasis: an update from the European Association of Urology guidelines panel for urolithiasis 2022. Eur Urol Focus. 2023; 9: 199-208. [DOI] [PubMed] [Google Scholar]
- 8.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol. 2007; 51: 899-906. [DOI] [PubMed] [Google Scholar]
- 9.Symons S, Biyani CS, Bhargava S, et al. Challenge of percutaneous nephrolithotomy in patients with spinal neuropathy: Percutaneous nephrolithotomy. Int J Urol. 2006; 13: 874-879. [DOI] [PubMed] [Google Scholar]
- 10.Rizvi SA, Naqvi SA, Hussain Z, et al. The management of stone disease. BJU Int. 2002; 89 Suppl 1: 62-68. [DOI] [PubMed] [Google Scholar]
- 11.Chung DY, Kang DH, Cho KS, et al. Comparison of stone-free rates following shock wave lithotripsy, percutaneous nephrolithotomy, and retrograde intrarenal surgery for treatment of renal stones: A systematic review and network meta-analysis. PLoS One. 2019; 14: e0211316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karakoyunlu AN, Cakici MC, Sari S, et al. Comparison of retrograde intrarenal surgery and percutaneous nephrolithotomy methods for management of big-sized kidney stones (? 4 cm): single center retrospective study. Urol J. 2019; 16: 232-235. [DOI] [PubMed] [Google Scholar]
- 13.Galvin DJ; Pearle MS. The contemporary management of renal and ureteric calculi. BJU Int. 2006; 98: 1283-1288. [DOI] [PubMed] [Google Scholar]
- 14.Aboumarzouk OM, Monga M, Kata SG, Traxer O, Somani BK. Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis. J Endourol. 2012; 26: 1257-1263. [DOI] [PubMed] [Google Scholar]
- 15.Chaurasia A. Percutaneous Nephrolithotomy: Challenges for a novice urologist. Minim Invasive Surg. 2020; 2020: 1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Preminger GM, Assimos DG, Lingeman JE, et al. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005; 173: 1991-2000. [DOI] [PubMed] [Google Scholar]
- 17.Assimos D, Krambeck A, Miller NL, et al. Surgical management of stones: American Urological Association/Endourological Society Guideline, PART I. J Urol. 2016; 196: 1153-1160. [DOI] [PubMed] [Google Scholar]
- 18.Yang SY, Jung HD, Kwon SH, Lee EK, Lee JY, Lee SH. Does early retrograde intrarenal surgery improve the cost-effectiveness of renal stone management? Yonsei Med J. 2020; 61: 515-523. [DOI] [PMC free article] [PubMed] [Google Scholar]