Abstract
The prognosis of advanced adrenocortical carcinoma (ACC) is dismal but heterogeneous. In 2011, mitotane is the only drug approved in Europe and US for the treatment of advanced ACC. Mitotane exerts both antisecretory and antiproliferative effects, which are delayed over time, and requires careful biological and morphological evaluations coupled with mitotane plasma measurement monitoring. In the absence of demonstration of any superior activity of combined polychemotherapy, the least toxic regimen should be considered in routine care. Locoregional therapies, including surgery of the primary tumor and metastases, should be considered part of the therapeutic arsenal. A prolonged survival can be observed in the case of tumor objective response and/or high plasma mitotane levels. New protocols are urgently needed, coupled with ancillary studies dedicated to progress in the findings of predictors or surrogates. International networks and comprehensive databases gathering clinical and biological data constitute the prerequisites for progress.
Keywords: Adrenocortical carcinoma, Prognosis, Treatment, Predictive markers surrogates
Introduction
This review provides a state of the art for the clinical management of advanced adrenocortical carcinoma (ACC) in 2011. Taking into account the recent ENSAT classification, advanced ACC is best defined by stage III (defined by locoregional spread) or stage IV (defined by the presence of distant metastases) and represents 18–26% and 21–46% of ACC patients at diagnosis, respectively [1–3]. Due to the scarcity of data on stage III ACC patients, this review will mainly focus on the management of stage IV ACC patients. However, strategies in unresectable stage III patients benefit from the results derived from studies on stage IV ACC patients. Only results obtained in adult patients are commented in this review. Several recommendations are made based on these data and on our experience in this field. The absence of randomized study makes the level of recommendations still low.
Prognosis of Advanced ACC
The prognosis of stage IV ACC patients is dismal and a vast majority of deaths are due to tumor-related progression [4]. The 5-year survival rate ranges between 0% and 13% in three multicentric studies [1–3]. At the time of first-line cytotoxic chemotherapy initiation, median survivals of 10–15 months have been reported [4–9]. Finally, two studies analyzing a mixed population of unresectable stage III–IV ACC patients reported a median survival of 16–24 months [10, 11]. These figures rank stage IV ACC among the most aggressive solid tumors in adults.
However, several reports suggest a greater heterogeneity of advanced ACC prognosis than initially thought. In 2007, the first prognostic study dedicated to stage IV ACC patients reported a median survival of 20 months from the time of metastasis diagnosis [4]. The number of tumor organs and the mitotic count in the primary tumor were identified as the most powerful prognostic parameters: median survival was 25 months in the case of favorable prognostic parameters (57% of the population under study), but only 9 months when both parameters were found unfavorable. Interestingly, this heterogeneous prognosis is also retrieved in studies analyzing ACC survival at the time of mitotane initiation with a survival ranging from 2 to 190 months [5, 7, 8, 12–18]. In addition, recent studies suggest that stage III ACC prognosis may overlap with stage IV [19–21].
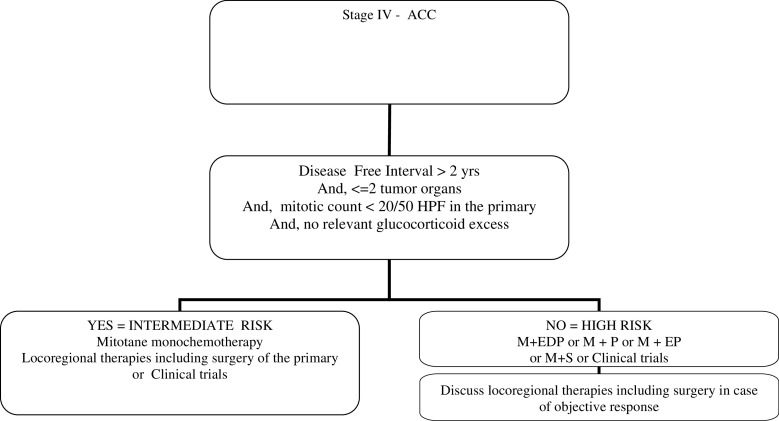
Previous prognostic series, which included ACC of various TNM stages, have confirmed the prognostic value of the mitotic count [19–21] but also identified additional prognostic parameters including history of a previous surgery of the primary tumor [2, 22–25] and the presence of cortisol secretion [26]. At the time of chemotherapy initiation, other studies [5, 7, 11, 27] confirmed the prognostic value of proliferative index [27], previous history of surgery of the primary tumor at the time of chemotherapy [5], or the hormonal status [5, 7, 11]. Finally, prognostic parameters like the performance status [5], the disease-free interval between diagnosis of the primary and stage III–IV ACC [11], or the anatomical location of metastases [8] were also identified and will deserve further attention in the future to refine the prognostic classification. Table 1 provides a list of parameters which should be determined in stage III–IV ACC patients to refine future prognostic analyses and interpretation of therapeutic trials. Figure 1 provides an example of a tailored approach of advanced stage IV ACC patients based on prognostic stratification used at Institut Gustave Roussy.
Table 1.
Minimum data set to be included in reports of advanced ACC at the time of treatment initiation
| Age and comorbidity, performance status |
| Interval of time since first diagnosis of ACC |
| Interval of time since diagnosis of stage III–IV ACC |
| Items of the Weiss score |
| Proliferative index per 50 HPF: mitotic count (count 10 HPF in the area of greatest numbers or mitotic figures) and Ki67 (in the most active regions, count multiple regions) |
| Secretory status |
| pTNM UICC and ENSAT staging |
| FDG-PET status at diagnosis |
| Number of abnormal lymph nodes at imaging or positive at pathology |
| Presence of venous invasion or adjacent organ invasion |
| Number and type of tumor organs |
| Resection of the primary; R status if surgery was performed |
| Mitotane plasma levels at the time of polychemotherapy initiation |
| Signed informed consent for bioresource use when available |
| Planned modality of follow-up |
Fig. 1.
Therapeutic management as a function of prognostic stratification in stage IV ACC patients. ACC adrenocortical carcinoma, HPF high-power field, M mitotane, E etoposide, P cisplatin, S streptozocin
Molecular stratification is expected to make the future of prognostic classifications and to provide a bridge towards new therapeutic options. Preliminary results [28–31] have demonstrated a prognostic impact together with the TNM stage. Additional markers like GLUT1 expression or the results of FDG-PET may also play a prognostic role [32, 33]
Treatment of Advanced ACC
Control of Hormonal Secretions
Due to tumor aggressiveness of most ACC, therapeutic management focuses on tumor burden control. Indeed, control of hormonal secretion mirrors tumor burden control in the vast majority of patients. Finally, a mitotane prescription, which remains the most active antitumor option in 2011, also displays antisecretory activity [13]. However, it should be kept in mind that a deleterious prognostic role of cortisol secretion has been reported in some studies. In keeping with this, control of hypokalemia and early management of sepsis, psychiatric disorders, increased glucose level, and blood pressure remain critical before mitotane or other systemic options become active. In that setting, drugs like ketoconazole, metyrapone, or etomidate may be helpful, but all drug interactions should be cautiously monitored [34–36]. Furthermore, liver chemoembolization may decrease hormone secretions and should be performed in selected cases [37].
Control of Tumor Burden
Monochemotherapy with Mitotane
Mitotane is by far the most studied agent in ACC and the only validated monochemotherapy in advanced ACC. After the demonstration of its cytotoxic properties on the adrenals of dogs and humans, it was first used in 1959 as a palliative therapy of advanced ACC [38, 39]. More than 50 years later, five retrospective and three prospective studies analyzing the antitumor role of this drug used as single agent have been published [5, 12–18] (Table 2). Various dosages of the drug were used, ranging from 3 to 20 g/day, as first-line therapy in most cases in 11–72 patients. Most patients were stage IV and a few had unresectable stage III ACC. Objective responses were reported in 13–33% of cases with duration of 2–190 months. Median progression-free survival was not reported in these studies. In addition, mitotane impact on overall survival is suggested by several recent retrospective studies [9, 15, 40, 41], but not all [7]. Mitotane has been claimed to reverse the P-glycoprotein protein expression which may influence the cell clearance of drugs like doxorubicin and etoposide [42]. However, the relevance of such activity has not been fully demonstrated in ACC patients [7]. Mitotane is approved in Europe and US for the treatment of advanced ACC.
Table 2.
Results of mitotane monochemotherapy
| Author, year; study type (n) | Dosage, g/day | Standardized CT | WHO criteria | Tumor response, n (%) | Duration, months |
|---|---|---|---|---|---|
| Venkatesh, 1989; retrospective (72) | NA | No | No | 21 (29) | NA |
| Luton, 1990; retrospective (37) | 3–20 | No | No | 5 (13) | 5–25 |
| Decker, 1991; prospective (36) | 6 | No | Yes | 8 (22) | 3–82 |
| Pommier, 1992; retrospective (29) | NA | No | No | 7 (24) | NA |
| Haak, 1994; retrospective (55) | 4–8 | No | Yes | 15 (27) | 2–190 |
| Barzon, 1997; retrospective (11) | 4–8 | Yes | Yes | 2 (18) | 12–21 |
| Williamson, 1999; prospective (16) | 4–10 | No | Yes | 2 (13) | NA |
| Baudin, 2001; prospective (13) | 6–12 | Yes | Yes | 4 (33) | 10–48 |
NA not available
Side effects of mitotane are diverse and target mainly the digestive (nausea, vomiting, or diarrhea) and neurological systems (vertigo, dizziness, somnolence, blurred vision, poor verbalization, slow ideation…) [5, 12–18, 34, 35]. Awareness of these side effects is critical and requires a dedicated education of patients. Digestive side effects occur early and are thought to be related to a direct effect of the drug on the digestive mucosa. Due to its cytotoxic role on the adrenals, adrenal insufficiency is a logical consequence of mitotane therapy which requires a corticosteroid and mineralosteroid substitution. As a rule, the appearance of digestive side effects requires an increase of cortisol supplementation dose not only to control the stress but also as a diagnostic test to diagnose an insufficient replacement of cortisol. Mitotane is also a strong inducer of liver enzyme activity including the CYP3A4 with major relevance regarding not only concomitant therapy like cortisol replacement, vitamin K antagonist, and oral contraception but also combined antitumor therapies [35, 36]. As practical consequences, routine cortisol replacement dose is twofold or threefold compared to patients treated for adrenal insufficiency, and heparin treatment and mechanic contraception methods are favored. Blood monitoring of mitotane treatment should include electrolyte measurements, liver tests, and blood cell counts, of which respective alterations constitute rare but potentially severe side effects of the drug. The relevance of monitoring gonad steroids or thyroid function tests is still debatable in the absence of related symptoms [43]. Dyslipidemia should be treated with drugs which do not interfere with CYP3A4 liver enzyme activity
Monochemotherapy or Polychemotherapy Without Mitotane
Apart from mitotane, only doxorubicin and irinotecan have been tested as single agents in first-line or post first-line stage IV ACC patients, respectively. Doxorubicin used as first-line treatment provides a 19% objective response rate in one study [5], but no confirmatory study is yet available and no objective response to doxorubicin used as second-line post mitotane therapy was observed in the same study. Irinotecan used as a second-line therapy or more, provided no objective response [44].
The results of the combination of etoposide and cisplatin without mitotane have been studied in two phase II studies [17, 45]. Objective response rates of 11–46% have been reported.
Polychemotherapy with Mitotane
As a general statement, not only the absence of randomized trial but also of mitotane plasma level monitoring in these studies make unknown the respective role of mitotane and other cytotoxic agents regarding tumor control.
Two phase II trials have analyzed the antitumor effect of mitotane combined with one cytotoxic drug. With cisplatin in 35 patients, Bukowski et al. reported a 30% objective response rate and a 7.9-month duration [6]. With streptozocin in 22 patients, Khan et al. reported a 36% objective response rate and a 7-month duration [10].
Nine studies analyzed the antitumor effect of mitotane combined with cytotoxic polychemotherapy. Cisplatin and doxorubicin were the most frequently used drugs. In three first-line studies, mitotane, cisplatin, and doxorubicin were combined either with cyclophosphamide, 5-fluorouracile, or etoposide and objective response rates of 18%, 23%, and 55% were reported in 11, 14, and 72 patients, respectively [11, 46, 47]. The rationale of the FIRMACT trial, which is currently under analysis, is based on the results of Berruti et al. and Khan et al. who reported the highest objective response rates of 36% and 55%, respectively [10, 11]. Together with mitotane, cisplatin and etoposide provided a 31% objective response in 18 patients [48] and doxorubicin, etoposide, and vincristine provided a 14% objective response [7]. As second-line treatment with mitotane combined with cisplatin, teniposide, and cyclophosphamide, one objective response was reported among 9 patients [49] and, with gemcitabine and 5-fluorouracile, two objective responses were reported among 28 patients (7%) with a 46% progression-free survival at 4 months [50].
In 2003, a conference consensus recommended, as first-line therapy, to use mitotane combined or not with etoposide–cisplatin, etoposide–cisplatin–doxorubicin, or streptozocin [51]. In 2011, the benefit of combining mitotane to other cytotoxic drugs remains to be demonstrated as well as the antitumor effect of agents like streptozocin or doxorubicin. In addition, only two studies have analyzed the antitumor effect of cisplatin combined with etoposide. In parallel, it is well known that combining mitotane with other cytotoxic agents increases the rate of side effects [6]. In such a context, in the absence of protocol, the least toxic approach should be favored. Therefore, other forms of treatments like locoregional therapies deserve attention and new trials are urgently needed. The forthcoming results of the FIRMACT trial, which aimed to compare the overall survival of ACC patients randomized first line for mitotane plus etoposide–cisplatin–doxorubicin or mitotane plus streptozocin regimen, will provide the first head-to-head comparison of two polychemotherapy regimens in the field of ACC. With a 7% objective response rate in second or third lines, gemcitabine and 5-fluorouracile are new agents also to be considered in the future.
Locoregional Therapies
Although rarely studied in ACC patients, locoregional therapies should be considered as part of the therapeutic arsenal. Locoregional therapeutic tools not only include surgery, embolization combined or not with chemotherapy, and radiofrequency but also other tools including radiotherapy. In one study using liver chemoembolization as second-line treatment, 83% of liver tumor control was reported at 3 months, and this was observed especially in patients with small-sized metastases, below or equal to 3 cm [37]. It can be used together with mitotane alone at the time of initiation to cover the period of mitotane inefficiency or with polychemotherapy in case of more aggressive tumors. For each locoregional tool, the best indication should be discussed, case by case, in the setting of multidisciplinary meetings.
The role of surgery, in the setting of advanced stage III–IV ACC, should be cautiously discussed, since it is associated with a higher risk of morbidity and mortality. Surgery of the primary tumor can be considered in stage IV ACC patients, considering the fact that its prognostic value has been highlighted in several prognostic studies [15, 22–25]. However, caution should be exercised and clinicians should ascertain that the prognostic evaluation is favorable (life expectancy above 6 months) and that the primary represents a significant proportion of the tumor burden and that complete resection of the primary is feasible without major additional risk of mortality. Surgery can also be applied to metastases. Due to the aggressiveness of most stage IV ACC, we recommend its use at the time of tumor response to medical treatment or at tumor stabilization for at least 6 months (Fig. 1). In addition, complete resection of the tumor should be feasible. Such a strategy resulted in complete response in some cases [7, 9, 11]. Surgery, at the time of diagnosis of metastases, can also be an option in case of favorable prognostic presentation and when a complete resection is expected (Fig. 1).
Predictors and Surrogate Markers
Predictors and surrogate markers are best defined in randomized studies. In the absence of any randomized study currently published, the parameters discussed below have to be validated.
Predictors of Response in ACC Patients
Plasma mitotane levels between 14 and 20 mg/L have been suggested to carry an acceptable risk over benefit ratio regarding the prediction of objective response [15]. This result was prospectively confirmed in another study [18]. Objective response rates of 55% and 66% were reported, and significant neurological toxicity was observed when plasma levels were above 20 or 30 mg/L [15, 18, 52]. These two studies yielded to the recommendation that plasma mitotane levels between 14 and 20 mg/L should be reached and maintained in ACC patients treated with mitotane [51]. In addition, four retrospective studies demonstrated a correlation between plasma levels of mitotane above 14 mg/L and improved survival [9, 15, 40, 41]. Recently, a retrospective study of the ENSAT group analyzed the correlation between tumor response and plasma mitotane levels in 97 ACC patients treated with mitotane combined or not with polychemotherapy [41]. A significantly higher objective response rate was observed when plasma mitotane levels exceeded 14 mg/L: 35% of patients with plasma mitotane levels above 14 mg/L experienced an objective response compared to 15% when plasma mitotane levels remained below the 14 mg/L cutoff. In the same study, a specificity of 90% was observed, regarding the prediction of objective response, when mitotane plasma levels above 20 mg/L were reached. In addition, a sensitivity of 89% was observed when mitotane plasma levels above 10 mg/L were reached. These results suggest that new recommendations could be made: to maintain plasma mitotane levels between 10 and 20 mg/L and, in selected patients with good tolerance and absence of objective response, to target a plasma mitotane level above 20 mg/L but below 30 mg/L.
Time to reach the therapeutic plasma level of mitotane has been shown to last from 1 to 6 months after mitotane initiation and sometimes is never obtained. Indeed, 60% to 100% of patients experience therapeutic plasma levels during the course of the disease, but no robust correlation with the cumulative dose of mitotane was found [15, 18, 53, 54]. As a consequence, the best strategy regarding mitotane daily dose at drug initiation remains debated [50, 54]. In addition, maintenance of plasma therapeutic levels, during the course of the disease, remains a challenge [15]. In daily practice, the delayed action of mitotane forces clinicians to engage polychemotherapy early in the course of ACC together with mitotane therapy. As a consequence, a significant number of ACC patients received a polychemotherapy at the time of first tumor evaluation and the role attributable to each therapeutic option, i.e., mitotane or polychemotherapy, remains undefined. This situation, quite unique in oncology, has notable consequences in the field of ACC management. Indeed, an early progression during mitotane therapy cannot be considered a definitive proof of resistance to the drug and, therefore, the definition of mitotane resistance should be clarified. In a recent study, we suggested that at least two mitotane levels above 14 mg/L, 3 months apart, should be obtained to declare a patient as resistant to mitotane therapy [8]. This proposal was based on the observation that progression of ACC during mitotane monotherapy and a single mitotane plasma level measurement above 14 mg/L was compatible with the further demonstration of an objective response after initiation of polychemotherapy. In other words, demonstration of tumor progression in patients with low or even one mitotane plasma level above 14 mg/L should trigger the start of additional therapeutic options but not the systematic withdrawal of mitotane. Taking into account the recent study of Hermsen et al. [41], mitotane resistance could also be defined by taking into account when the cutoff of 20 mg/L can be reached or the highest plasma mitotane level can be reached at the highest tolerated dose.
In addition to the predictive value of plasma mitotane levels, one study has suggested a link between survival of patients treated with mitotane therapy and cortisol secretion, suggesting similar biological background between the mechanism of cortisol secretion and antitumor activity of mitotane [26]. No confirmatory study is available and the recommendation is to treat secretory and nonsecretory ACC patients with the same strategy. It should be mentioned also that the unfavorable prognostic impact of cortisol secretion has been reported by some studies [7, 11, 26], but not all [4, 6, 10].
Recently, low ERCC1 expression, a marker of active DNA repair complex within tumor cells, was shown to be associated with efficacy of cisplatinum therapy in ACC patients [27]. Ronchi et al. first reported that ERCC1 staining was the strongest predictor of survival after the initiation of cisplatin treatment in 45 ACC patients. In that study, low staining for ERCC1 was indicative of a higher response rate observed in 29% of ACC patients versus 14% when ERCC1 staining was high. A statistically significant impact on survival was also found. Using the same methodology, another study found a similar trend regarding the response rate (26.7% versus 16.7% in ERCC1-low and ERCC1-high patients, respectively), but ERCC1 staining did not influence overall survival after platinum-based chemotherapy [8].
Surrogates of Survival in ACC Patients
Up to now, four retrospective studies have reported a relationship between complete or objective response at 2 or 4 months and improved survival [7, 8, 11, 55], but this was not confirmed in another study [6]. The prolonged median survival of responders, above 34 months in these studies, is remarkable and suggests that this subgroup of patients should be reconsidered for locoregional options including surgery (Fig. 1). In one of these studies, plasma mitotane levels above 14 mg/L and presence of an objective response were found to be the two most significant independent prognostic parameters at the time of therapeutic intervention [8]. Therefore, the results of the plasma mitotane levels may also help to refine the strategy. An example of a therapeutic strategy used at the Institut Gustave Roussy, based on the results of imaging, plasma mitotane levels, and prognostic stratification, as defined above, is provided in Table 3.
Table 3.
Therapeutic management strategy of advanced ACC, used at the Institut Gustave Roussy, as a function of tumor response, plasma mitotane levels, and prognostic parameters
| Plasma mitotane | RECIST: objective response | RECIST: stabilization | RECIST: progression |
|---|---|---|---|
| <14 or >14 mg/La at only one measurement | Increase mitotaneb | Increase mitotaneb | Increase mitotaneb |
| Locoregional optionsc | Combined chemotherapy (high-risk group) and or locoregional therapies (intermediate-risk group) | Combined chemotherapy or clinical trials | |
| >14 mg/L at two measurements 3 months apart | Maintain mitotaneb | Maintain mitotaneb | Discuss withdrawal of mitotane therapy |
| Locoregional optionsc | Combined chemotherapy or trials (high-risk group) and or locoregional therapies (intermediate-risk group) | Chemotherapy or clinical trials |
aConsider results of plasma mitotane within the three previous months
bIn case of good tolerance
cLocoregional options include liver embolization, radiofrequency ablation, external radiotherapy, and surgery of the primary tumor and metastases to be discussed case by case
Future Directions
Obviously, the results discussed above cannot be considered as satisfactory and new therapeutic options are needed. However, the efforts to fight this rare and severe cancer should not be underestimated. We must admit that conditions of progress have been implemented in the last few years including a better characterization of ACC prognosis and preliminary identification of predictors of response and surrogate (see above). The recent creation of networks, including the ENSAT network, dedicated to malignant adrenal tumors allows several expert centers around the world to gather their results and discuss new protocols in the field of ACC. The implementation and achievement of the first international randomized study in the field of ACC, the FIRMACT study, is a direct result of these advances. Ongoing creation of large clinical databases which trace available tumor tissues and fluids for research is another key step of progress together with the increase of available preclinical models.
To speed up the process of drug development in the area of ACC, the following recommendations could be applied in future trials:
Characterization of ACC patients before treatment should be standardized. This includes an appropriate evaluation of the parameters listed in Table 1. Interval of time between major ACC events, pathological analysis with proliferative index measurements (mitotic count and Ki67 index), hormonal tests, and lung, abdomen, and pelvic computerized tomography together with FDG-PET constitute the basis of this approach.
Follow-up of ACC patients at the time of medical therapy should be standardized. Plasma mitotane measurement is mandatory at least every month during the first 6 months, at the time of best morphological response, and then every 2–3 months during the follow-up period. A standardized methodology for mitotane measurement should be used to allow comparisons and early implementation of the results. Response to therapy should be evaluated with standardized methodology (RECIST criteria). Tumor response evaluation should be performed, at least every 2 months, for first-line or second-line therapies but at shorter intervals of time, every 4–6 weeks, at the time of third or fourth lines if active therapy is still ongoing or in case of parameters which indicate a poor prognosis. Monitoring of hormonal secretions is also recommended at each imaging evaluation.
All efforts should be made to include ancillary studies focusing on the discovery of predictors of response in new trials. Towards that end, not only archival materials but also fresh tumor tissue analyses, obtained at the time of medical treatment, should be implemented. Indeed, this strategy may allow translating all objective responses into meaningful biological predictors that will help the future selection of patients for each given therapy.
All efforts should be made to validate a surrogate marker of ACC overall survival in new randomized trials. Classical methodology to validate new options involves randomized trials against a standard or a placebo. Although overall survival is a meaningful endpoint in aggressive cancer like ACC, methodological recommendations of such trials may omit crossover in order to avoid the use of the same lines of treatments in both arms. This strategy raises ethical concerns in a cancer like ACC with a limited number of options available and a poor prognosis. One way to overcome this problem is to urgently validate a surrogate of ACC overall survival to be used as a primary endpoint in future studies.
Mitotane action is delayed. In that context, new protocols should be implemented either before the use of mitotane or after mitotane withdrawal. In addition, a consensual definition of mitotane resistance should be provided. In Table 2, we suggest to discuss mitotane withdrawal in case of two mitotane measurements above 14 mg/L, 3 months apart, associated with tumor progression. Alternative options are proposed in this manuscript.
Mitotane is a liver enzyme inducer. In that setting, pharmacokinetic studies are recommended in ACC patients treated with mitotane
Phase II trials testing new agents, worldwide, are urgently needed. ACC patients should be enrolled in phase I trials in the absence of dedicated protocols for ACC. At the time of validation, randomized phase II trials prolonged in phase III trials in the case of attractive interim analysis may constitute the best option in this rare and severe cancer.
Acknowledgments
Conflict of Interest
None.
References
- 1.Fassnacht M, Johanssen S, Quinkler M, Bucsky P, Willenberg HS, Beuschlein F, Terzolo M, Mueller HH, Hahner S, Allolio B. 2009 Limited prognostic value of the 2004 International Union Against Cancer staging classification for adrenocortical carcinoma: proposal for a Revised TNM Classification. Cancer. 2009;115:243–250. doi: 10.1002/cncr.24030. [DOI] [PubMed] [Google Scholar]
- 2.Icard P, Goudet P, Charpenay C, Andreassian B, Carnaille B, Chapuis Y, Cougard P, Henry JF, Proye C. Adrenocortical carcinomas: surgical trends and results of a 253-patient series from the French Association of Endocrine Surgeons study group. World J Surg. 2001;25:891–897. doi: 10.1007/s00268-001-0047-y. [DOI] [PubMed] [Google Scholar]
- 3.Lughezzani G, Sun M, Perrot P, Jeldres C, Alasker A, Isbarn H, Budaus L, Shariat SF, Guazzoni G, Montorsi F, Karakiewicz PI. The European Network for the Study of Adrenal Tumors staging system is prognostically superior to the International Union Against Cancer-staging system. Eur J Cancer. 2010;46:713–719. doi: 10.1016/j.ejca.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Assie G, Antoni G, Tissier F, Caillou B, Abiven G, Gicquel C, Leboulleux S, Travagli JP, Dromain C, Bertagna X, Bertherat J, Schlumberger M, Baudin E. Prognostic parameters of metastatic adrenocortical carcinoma. J Clin Endocrinol Metab. 2007;92:148–154. doi: 10.1210/jc.2006-0706. [DOI] [PubMed] [Google Scholar]
- 5.Decker RA, Elson P, Hogan TF, Citrin DL, Westring DW, Banerjee TK, Gilchrist KW, Horton J. Eastern Cooperative Oncology Group study 1879: mitotane and adriamycin in patients with advanced adrenocortical carcinoma. Surgery. 1991;110:1006–1013. [PubMed] [Google Scholar]
- 6.Bukowski RM, Wolfe M, Levine HS, Crawford DE, Stephens RL, Gaynor E, Harker WG. Phase II trial of mitotane and cisplatin in patients with adrenal carcinoma: a Southwest Oncology Group study. J Clin Oncol. 1993;11:161–165. doi: 10.1200/JCO.1993.11.1.161. [DOI] [PubMed] [Google Scholar]
- 7.Abraham J, Bakke S, Rutt A, Meadows B, Merino M, Alexander R, Schrump D, Bartlett D, Choyke P, Robey R, Hung E, Steinberg SM, Bates S, Fojo T. A phase II trial of combination chemotherapy and surgical resection for the treatment of metastatic adrenocortical carcinoma: continuous infusion doxorubicin, vincristine, and etoposide with daily mitotane as a P-glycoprotein antagonist. Cancer. 2002;94:2333–2343. doi: 10.1002/cncr.10487. [DOI] [PubMed] [Google Scholar]
- 8.Malandrino P, Al Ghuzlan A, Castaing M, Young J, Caillou B, Travagli JP, Elias D, de Baere T, Dromain C, Paci A, Chanson P, Schlumberger M, Leboulleux S, Baudin E. Prognostic markers of survival after combined mitotane- and platinum-based chemotherapy in metastatic adrenocortical carcinoma. Endocr Relat Cancer. 2010;17:797–807. doi: 10.1677/ERC-09-0341. [DOI] [PubMed] [Google Scholar]
- 9.Fareau GG, Lopez A, Stava C, Vassilopoulou-Sellin R. Systemic chemotherapy for adrenocortical carcinoma: comparative responses to conventional first-line therapies. Anticancer Drugs. 2008;19:637–644. doi: 10.1097/CAD.0b013e328300542a. [DOI] [PubMed] [Google Scholar]
- 10.Khan TS, Imam H, Juhlin C, Skogseid B, Grondal S, Tibblin S, Wilander E, Oberg K, Eriksson B. Streptozocin and o,p’DDD in the treatment of adrenocortical cancer patients: long-term survival in its adjuvant use. Ann Oncol. 2000;11:1281–1287. doi: 10.1023/A:1008377915129. [DOI] [PubMed] [Google Scholar]
- 11.Berruti A, Terzolo M, Sperone P, Pia A, Casa SD, Gross DJ, Carnaghi C, Casali P, Porpiglia F, Mantero F, Reimondo G, Angeli A, Dogliotti L. Etoposide, doxorubicin and cisplatin plus mitotane in the treatment of advanced adrenocortical carcinoma: a large prospective phase II trial. Endocr Relat Cancer. 2005;12:657–666. doi: 10.1677/erc.1.01025. [DOI] [PubMed] [Google Scholar]
- 12.Venkatesh S, Hickey RC, Sellin RV, Fernandez JF, Samaan NA. Adrenal cortical carcinoma. Cancer. 1989;64:765–769. doi: 10.1002/1097-0142(19890801)64:3<765::AID-CNCR2820640333>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 13.Luton JP, Cerdas S, Billaud L, Thomas G, Guilhaume B, Bertagna X, Laudat MH, Louvel A, Chapuis Y, Blondeau P, Bonnin A, Bricaire H. Clinical features of adrenocortical carcinoma, prognostic factors, and the effect of mitotane therapy. N Engl J Med. 1990;322:1195–1201. doi: 10.1056/NEJM199004263221705. [DOI] [PubMed] [Google Scholar]
- 14.Pommier RF, Brennan MF. An eleven-year experience with adrenocortical carcinoma. Surgery. 1992;112:963–970. [PubMed] [Google Scholar]
- 15.Haak HR, Hermans J, van de Velde CJ, Lentjes EG, Goslings BM, Fleuren GJ, Krans HM. Optimal treatment of adrenocortical carcinoma with mitotane: results in a consecutive series of 96 patients. Br J Cancer. 1994;69:947–951. doi: 10.1038/bjc.1994.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barzon L, Fallo F, Sonino N, Daniele O, Boscaro M. Adrenocortical carcinoma: experience in 45 patients. Oncology. 1997;54:490–496. doi: 10.1159/000227608. [DOI] [PubMed] [Google Scholar]
- 17.Williamson SK, Lew D, Miller GJ, Balcerzak SP, Baker LH, Crawford ED. Phase II evaluation of cisplatin and etoposide followed by mitotane at disease progression in patients with locally advanced or metastatic adrenocortical carcinoma: a Southwest Oncology Group study. Cancer. 2000;88(5):1159–1165. doi: 10.1002/(SICI)1097-0142(20000301)88:5<1159::AID-CNCR28>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 18.Baudin E, Pellegriti G, Bonnay M, Penfornis A, Laplanche A, Vassal G, Schlumberger M. Impact of monitoring plasma 1,1-dichlorodiphenildichloroethane (o,p’DDD) levels on the treatment of patients with adrenocortical carcinoma. Cancer. 2001;92:1385–1392. doi: 10.1002/1097-0142(20010915)92:6<1385::AID-CNCR1461>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 19.Volante M, Bollito E, Sperone P, Tavaglione V, Daffara F, Porpiglia F, Terzolo M, Berruti A, Papotti M. Histopathol. 2009;55:53–54. doi: 10.1111/j.1365-2559.2009.03423.x. [DOI] [PubMed] [Google Scholar]
- 20.Stojadinovic A, Ghossein RA, Hoos A, Nissan A, Marshall D, Dudas M, Cordon-Cardo C, Jaques DP, Brennan MF. Adrenocortical carcinoma: clinical, morphologic, and molecular characterization. J Clin Oncol. 2002;20:941–950. doi: 10.1200/JCO.20.4.941. [DOI] [PubMed] [Google Scholar]
- 21.Miller BS, Gauger PG, Hammer G, Giordano T, Doherty GM. Proposal for modification of the ENSAT staging system for adrenocortical carcinoma using tumor grade. Langenbecks Arch Surg. 2010;34:1380–1387. doi: 10.1007/s00423-010-0698-y. [DOI] [PubMed] [Google Scholar]
- 22.Soreide JA, Brabrand K, Thoresen SO. Adrenal cortical carcinoma in Norway, 1970–1984. World J Surg. 1992;16:663–667. doi: 10.1007/BF02067349. [DOI] [PubMed] [Google Scholar]
- 23.Lee JE, Berger DH, el-Naggar AK, Hickey RC, Vassilopoulou-Sellin, Gagel RF, Burgess A, Evans DB. Surgical management, DNA content, and patient survival in adrenal cortical carcinoma. Surgery. 1995;118:1090–1098. doi: 10.1016/S0039-6060(05)80119-9. [DOI] [PubMed] [Google Scholar]
- 24.Schulick RD, Brennan MF. Long-term survival after complete resection and repeat resection in patients with adrenocortical carcinoma. Ann Surg Oncol. 1999;6:719–726. doi: 10.1007/s10434-999-0719-7. [DOI] [PubMed] [Google Scholar]
- 25.Bilimoria KY, Shen WT, Elaraj D, Bentrem DJ, Winchester DJ, Kebebew E, Sturgeon C. Cancer. 2008;13:3130–3136. doi: 10.1002/cncr.23886. [DOI] [PubMed] [Google Scholar]
- 26.Abiven G, Coste J, Groussin L, Anract P, Tissier F, Legmann P, Dousset B, Bertagna X, Bertherat J. Clinical and biological features in the prognosis of adrenocortical cancer: poor outcome of cortisol-secreting tumors in a series of 202 consecutive patients. J Clin Endocrinol Metab. 2006;91:2650–2655. doi: 10.1210/jc.2005-2730. [DOI] [PubMed] [Google Scholar]
- 27.Ronchi C, Sbiera S, Kraus L, Wortmann S, Johanssen S, Adam P, Willenberg H, Hahner S, Allolio B, Fassnacht M. Expression of excision repair cross complementing group 1 and prognosis in adrenocortical carcinoma patients treated with platinum-based chemotherapy. Endocr Relat Cancer. 2009;16:907–918. doi: 10.1677/ERC-08-0224. [DOI] [PubMed] [Google Scholar]
- 28.Giordano TJ, Kuick R, Else T, Gauger PG, Vinco M, Bauersfeld J, Sanders D, Thomas DG, Doherty G, Hammmer G. Molecular classification and prognostication of adrenocortical tumors by transcriptome profiling. Clin Cancer Res. 2009;15:668–676. doi: 10.1158/1078-0432.CCR-08-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Reynies A, Assié G, Rickman DS, Tissier F, Groussin L, Rné-Corail F, Dousset B, Bertagna X, Clauser E, Bertherat Gene expression profiling reveals a new classification of adrenocortical tumors and identified molecular predictors of malignancy and survival. J Clin Oncol. 2009;27:1108–1115. doi: 10.1200/JCO.2008.18.5678. [DOI] [PubMed] [Google Scholar]
- 30.Sbiera S, Schmull S, Assie G, Voelker HU, Kraus L, Beyer M, Ragazzon B, Beuschlein, Willenberg HS, Hahner S, Saeger W, Bertherat J, Allolio B, Fassnacht M. High diagnostic and prognostic value of steroidogenic factor-1 expression in adrenal tumors. J Clin Endocrinol Metab. 2010;95:161–171. doi: 10.1210/jc.2010-0653. [DOI] [PubMed] [Google Scholar]
- 31.Gaujoux S, Grabar S, Fassnacht M, Ragazzon B, Launay P, Libe R, Chokri I, Audbourg A, Royer B, Sbiera S, Vacher-Lavenu MC, Dousset B, Bertagna X, Allolio B, Bertherat J. β-Catenin activation is associated with specific clinical and pathologic characteristics and a poor outcome in adrenocortical carcinoma. Clin Cacer Res. 2010;17:328–336. doi: 10.1158/1078-0432.CCR-10-2006. [DOI] [PubMed] [Google Scholar]
- 32.Fenske W, Volker HU, Adam P, Hahner S, Johanssen S, Wortmann S, Schmidt M, Morcos M, Muller-Hermelink, Allolio B, Fassnacht M. Glucose transporter GLUT 1 expression is an stage-independent predictor of clinical outcome in adrenocortical carcinoma. Endocr Relat Cancer. 2009;16(3):919–928. doi: 10.1677/ERC-08-0211. [DOI] [PubMed] [Google Scholar]
- 33.Leboulleux S, Dromain C, Bonniaud G, Auperin A, Caillou B, Lumbroso J, Sigal R, Baudin E, Schlumberger M. Diagnostic and prognostic value of 18-fluorodeoxyglucose positron emission tomography in adrenocortical carcinoma: a prospective comparison with computed tomography. J Clin Endocrinol Metab. 2006;91:920–925. doi: 10.1210/jc.2005-1540. [DOI] [PubMed] [Google Scholar]
- 34.Kamenicky P, Droumaguet C, Salenave S, Blanchard A, Jublanc C, Gautier JF, Brailly-Tabard S, Leboulleux S, Schlumberger M, Baudin E, Chanson P, Young J. Mitotane, metyrapone, and ketoconazole combination therapy as an alternative to rescue adrenalectomy for severe ACTH-dependent Cushing’s syndrome. J Clin Endocrinol Metab. 2011;96:2796–2804. doi: 10.1210/jc.2011-0536. [DOI] [PubMed] [Google Scholar]
- 35.Veytsman I, Nieman L, Fojo T. Management of endocrine manifestations and the use of mitotane as a chemotherapeutic agent for adrenocortical carcinoma. J Clin Oncol. 2009;27:1–14. doi: 10.1200/JCO.2008.17.2775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kroiss M, Quinkler M, Lutz WK, Allolio B, Fassnacht M. Drug interactions with mitotane by induction of CYP3A4 metabolism in the clinical management of adrenocortical carcinoma. Clinical Endoc. 2011;75:585–591. doi: 10.1111/j.1365-2265.2011.04214.x. [DOI] [PubMed] [Google Scholar]
- 37.Cazejust J, De Baere T, Auperin A, Deschamps F, Hechelhammer, Abdel-rehim M, Schlumberger M, Leboulleux S, Baudin E. Transcatheter arterial chemoembolization for liver metastases in patients with adrenocortical carcinoma. Int Vasc Radiol. 2010;94:204–210. doi: 10.1016/j.jvir.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 38.Nelson AA, Woodard G. Severe adrenal cortical atrophy (cytotoxic) and hepatic damage produced in dogs by feeding 2,2-bis(parachlorophenyl)-1,1-dichloroethane (DDD or TDE) Arch Pathol (Chic) 1949;48:387–394. [PubMed] [Google Scholar]
- 39.Hutter AM, Jr, Kayhoe DE. Adrenal cortical carcinoma. Results of treatment with o,p’DDD in 138 patients. Am J Med. 1966;41(4):581–592. doi: 10.1016/0002-9343(66)90220-8. [DOI] [PubMed] [Google Scholar]
- 40.Wangberg B, Khorram-Manesh A, Jansson S, Nilsson B, Nilsson O, Jakobsson CE, Lindstedt S, Oden A, Ahlman H. The long-term survival in adrenocortical carcinoma with active surgical management and use of monitored mitotane. Endocr Relat Cancer. 2010;17:265–272. doi: 10.1677/ERC-09-0190. [DOI] [PubMed] [Google Scholar]
- 41.Hermsen IG, Fassnacht M, Terzolo M, et al. Plasma concentrations of o,p’DDD, o,p’DDA, and o,p’DDE as predictors of tumor response to mitotane in adrenocortical carcinoma: results of a retrospective ENS@T multicenter study. J Clin Endocrinol Metab. 2011;96:1844–1851. doi: 10.1210/jc.2010-2676. [DOI] [PubMed] [Google Scholar]
- 42.Bates SE, Shieh CY, Mickley LA, et al. Mitotane enhances cytotoxicity of chemotherapy in cell lines expressing a multidrug resistance gene (mdr-1/P-glycoprotein) which is also expressed by adrenocortical carcinomas. J Clin Endocrinol Metab. 1991;73(1):18–29. doi: 10.1210/jcem-73-1-18. [DOI] [PubMed] [Google Scholar]
- 43.Daffara F, De Francia S, Reimondo G, Zaggia B, Aroasio E, Porpiglia F, Volante M, Termine A, Di Carlo F, Dogliotti L, Angeli A, Berruti A, Terzolo M. Prospective evaluation of mitotane toxicity in adrenocortical cancer patients treated adjuvantly. Endocr Relat Cancer. 2008;15:1043–1053. doi: 10.1677/ERC-08-0103. [DOI] [PubMed] [Google Scholar]
- 44.Baudin E, Docao C, Gicquel C, Vassal G, Bachelot A, Penfornis A, Schlumberger M. Use of a topoisomerase I inhibitor (irinotecan, CPT-11) in metastatic adrenocortical carcinoma. Ann Oncol. 2002;13:1806–1809. doi: 10.1093/annonc/mdf291. [DOI] [PubMed] [Google Scholar]
- 45.Burgess MA, Legha SS, Sellin RV (1983) Chemotherapy with cisplatinum and etoposide (VP16) for patients with advanced adrenal cortical carcinoma. ASCO proceedings: A5
- 46.van Slooten HMA, van Seters AP, Smeenk D. The treatment of adrenocortical carcinoma with o,p’-DDD: prognostic implications of serum level monitoring. Eur J Cancer Clin Oncol. 1984;20(1):47–52. doi: 10.1016/0277-5379(84)90033-6. [DOI] [PubMed] [Google Scholar]
- 47.Schlumberger M, Brugieres L, Gicquel C, Travagli JP, Droz JP, Parmentier C. 5-Fluorouracil, doxorubicin, and cisplatin as treatment for adrenal cortical carcinoma. Cancer. 1991;67:2997–3000. doi: 10.1002/1097-0142(19910615)67:12<2997::AID-CNCR2820671211>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 48.Bonacci R, Gigliotti A, Baudin E, Wion-Barbot N, Emy P, Bonnay M, Cailleux AF, Nakib I, Schlumberger M, Reseau Comete INSERM Cytotoxic therapy with etoposide and cisplatin in advanced adrenocortical carcinoma. Br J Cancer. 1998;78:546–549. doi: 10.1038/bjc.1998.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khan TS, Sundin A, Juhlin C, Wilander E, Oberg K, Eriksson E. Vincristine, cisplatin, teniposide, and cyclophosphamide combination in the treatment of recurrent or metastatic adrenocortical carcinoma. Medical Oncol. 2004;21:167–177. doi: 10.1385/MO:21:2:167. [DOI] [PubMed] [Google Scholar]
- 50.Sperone P, Ferrero A, Daffara F, Priola A, Zaggia B, Volante M, Santini D, Vincenzi B, Badalamenti G, Intrivici C, del Buono S, De Francia S, Kalomirakis E, Ratti R, Angeli A, Dogliotti L, Papotti M, Terzolo M, Berruti A. Gemcitabine plus metronomic 5-fluorouracil or capecitabine as a second-/third-line chemotherapy in advanced adrenocortical carcinoma: a multicenter phase II study. Endocr Relat Cancer. 2010;17:445–453. doi: 10.1677/ERC-09-0281. [DOI] [PubMed] [Google Scholar]
- 51.Schteingart DE, Doherty GM, Gauger PG, Giordano TJ, Hammerr GD, Korobkin M, Worden FP. Management of patients with adrenal cancer: recommendations of an international consensus conference. Endocr Relat Cancer. 2005;12:667–680. doi: 10.1677/erc.1.01029. [DOI] [PubMed] [Google Scholar]
- 52.van Slooten H, Moolenaar AJ, van Seters AP, Smeenk D. The treatment of adrenocortical carcinoma with o,p’-DDD: prognostic implications of serum level monitoring. Eur J Cancer Clin Oncol. 1984;20:47–53. doi: 10.1016/0277-5379(84)90033-6. [DOI] [PubMed] [Google Scholar]
- 53.Terzolo M, Pia A, Berruti A, Osella G, Ali A, Carbone V, Testa E, Dogliotti L, Angeli A. Low-dose monitored mitotane treatment achieves the therapeutic range with manageable side effects in patients with adrenocortical cancer. J Clin Endocrinol Metab. 2000;85:2234–2238. doi: 10.1210/jc.85.6.2234. [DOI] [PubMed] [Google Scholar]
- 54.Faggiano A, Leboulleux S, Young J, Schlumberger M, Baudin E. Rapidly progressing high o,p’DDD doses shorten the time required to reach the therapeutic threshold with an acceptable tolerance: preliminary results. Clin Endocrinol. 2006;64:110–113. doi: 10.1111/j.1365-2265.2005.02403.x. [DOI] [PubMed] [Google Scholar]
- 55.Gonzales RJ, Tamm EP, Chaan Ng, Phan AT, Vassilopoulou-Sellin R, Perrier ND, Evans DB, Lee JE. Response to mitotane therapy predicts outcome in patients with recurrent adrenal cortical carcinoma. Sugery. 2007;142:867–875. doi: 10.1016/j.surg.2007.09.006. [DOI] [PubMed] [Google Scholar]