PHOTO QUIZ
An 85-year-old woman presented to the emergency department for severe keratitis in the right eye associated with corneal melting. Slit lamp examination revealed conjunctival hyperemia, mucous secretion at the inferior fornix, a subtotal corneal epithelial defect, corneal edema, and 3 mm of hypopyon. The clinical characteristics were compatible with infectious keratitis and with ocular cicatricial pemphigoid, an autoimmune condition that causes conjunctival scarring, aqueous and mucous tear deficiency, and ocular keratinization, which often leads to blindness if left untreated. Corneal scraping was performed to exclude bacterial pathogens and fungi. Molecular detection of herpes simplex virus 1 (HSV-1), varicella zoster virus (VZV), and Acanthamoeba sp. was also requested. Empirical therapy with topical voriconazole, topical moxifloxacin, and ofloxacin ointment was started. Systemic valacyclovir was also initiated. The patient did not show any sign of improvement. Culture and molecular results were negative. Since the patient was not responding to therapy, amniotic membrane transplantation was performed and a therapeutic contact lens was applied to promote epithelial healing. Moreover, the patient was invited to continue the antibiotic and antifungal treatment cited above. Inflammation reduced dramatically, the epithelial defect decreased, and hypopyon resolved.
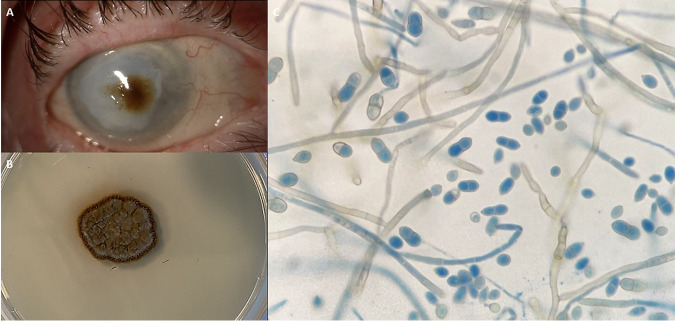
At follow-up, 3 months after the procedure, a brownish corneal infiltrate approximately 2 mm in size appeared on the central cornea (Fig. 1A). The therapeutic contact lens was removed and sent to the microbiology laboratory. Corneal scraping was performed directly on chocolate blood agar and on Sabouraud dextrose agar (SDA). All media were incubated at 30°C. In 5 days, a dark-brown dry colony surrounded by a brownish-maroon halo grew both from the corneal sample and the therapeutic lens (Fig. 1B). An adhesive tape preparation with lactophenol cotton blue staining (LCBS) on the grown mycelium evidenced the structures depicted in Fig. 1C.
FIG 1.
(A) Right eye with therapeutic contact lens showing a brownish corneal infiltrate upon slit lamp examination. (B) Macroscopic view of the colony grown on SDA after 5 days of incubation at 30°C. (C) Microscopic view of lactophenol cotton blue mount, showing smooth, flexuous, pigmented, septate hyphae producing two-celled conidia with a small denticle.
Footnotes
For answer and discussion, see https://doi.org/10.1128/JCM.00075-23 in this issue.
Contributor Information
N. Mancini, Email: nicasio.mancini@uninsubria.it.
Erik Munson, Marquette University.