Abstract
Tooth root resorption is multifactorial, leading to progressive destruction and eventual loss of tooth root dentin and cement. There are internal and external types of root resorption, each having its variety. The etiology and pathogenesis of tooth root resorption are poorly understood, and the most significant etiological factors are trauma, pulpal infection, tooth bleaching, and orthodontic treatment. Tooth root resorption is primarily asymptomatic; thus, it is revealed accidentally by radiographic examination. Progressive clinical manifestations are pain, tooth discoloration, tooth mobility, and other conditions. Awareness of the causes and risk factors allowing tooth root resorption, and regular radiographic examination, in case of necessity, make it possible to reveal resorption at an early stage and to prevent its further development. Thus, the aim of this study is to present etiopathogenesis, a clinical course, and diagnostic peculiarities of internal and external types of tooth root resorption, enabling practicing dentists to timely diagnose root resorption and take appropriate measures to avoid further complications. Within the limitation of this review, even though the etiopathogenesis of tooth root resorption is yet not fully understood, it is suggested that the etiological factors fall into two groups (endogenic and exogenic) to enhance further understanding of the possible causes and mechanisms of root resorption and allow practitioners to monitor high-risk patients and make timely diagnoses. Moreover, radiographic examination and CBCT are indispensable for the diagnosis of root resorption.
Keywords: Root resorption, internal resorption, external resorption, orthodontic force, dental trauma, resorption etiology, resorption classification, resorption pathogenesis, resorption diagnosis
Introduction
A thin anti-resorptive barrier protects the internal and external walls of the tooth roots. The pre-cementum layer protects the external walls, while predentin and odontoblasts protect the inner walls of the tooth dentin.1,2 Resorption is associated with physiological and pathological factors and results in the loss of dentin, cement, or bone tissues. 3 Resorptive cells cannot colonize nonmineralized surfaces.1,2 Multiple mechanical, chemical, and thermal factors have been established that encourage early mineralization of defensive barriers and initiate root resorption.3–6
Various etiological factors of tooth root resorption are mentioned in the literature, among which trauma and iatrogenic factors, such as bleaching and orthodontic treatment, are especially noteworthy.7–10 Regardless of various causative factors, the etiology of some types of resorptions is still unclear, which necessitates further research.11–13
Conditioned by etiological factors and location, the type of resorption is characterized by pathogenetic peculiarities of its development. The cytokines, prostaglandins, and increase in the tooth root canal inner pressure stand out in the pathogenesis of internal root resorption (IRR).14–17 In external inflammatory resorption (EIR), the periodontal tissue lesion and necrotic changes in the tooth root canal play a critical role, since exposed dentinal canals contribute to the accumulation of bacteria, and destroyed tissue remnants.7,18 In contrast, in external replacement resorption (ERR), the decay process is accompanied by reconstructive changes. Thus, decayed areas of tooth dentin and cement are replaced with alveolar bone.7,11
The diagnosis can be made based on clinical and radiographic presentation. The patient should thoroughly be examined since tooth root resorption commonly has relatively mild clinical manifestations or none. However, the final diagnosis is ultimately confirmed by radiographic data.19–21 In this regard, cone beam computed tomography (CBCT) can be informative. 22
Thus, this article aimed to present the etiology, pathogenesis, clinical course, and diagnostic peculiarities of internal and external types of tooth root resorption, focusing on orthodontic etiology, enabling practical dentists to timely diagnose root resorption and take appropriate measures to avoid further complications.
Description of different types of root resorption
External surface resorption (ESR)
ESR is a sterile, transitory, pressure-initiated resorption that involves small tooth root areas. 11 With the elimination of the etiological factor, this type of resorption is reversible, and it is possible to restore the cement of the tooth surface under favorable conditions when the pulp is not infected.11,23 ESR starts with the root surface and mainly involves the cementum and occasionally the dentin. Resorptive lesions rarely extend beyond the cement-dentin limit. ESR is revealed radiographically only with atypically extensive lesions. In practice, however, it is impossible to detect resorptive lesions of the vestibular and oral surfaces of the root. It is, therefore mainly diagnosed through histological examination after a tooth is extracted.24,25
External inflammatory resorption (EIR)
EIR is the most aggressive and destructive type of traumatic resorptions.26,27 EIR is associated with the infected pulp and periodontium.11,19,28 It more often develops after severe trauma and commonly starts with a vestibular surface of the root. The development of the lesion mainly depends on pulp vitality.18,19,28 Consequently, if the blood supply of the affected tooth is not impaired, the activity of osteoclasts only focuses on the transformation of the affected external root surface, and the resorption is self-limiting, similar to that observed in a transitory apical breakdown. However, when the root canal gets infected, microbial toxins can move to the resorption area through dentinal tubules, leading to the progression of inflammatory resorption. Resorptive lesions can be superficial or involve deeper dentin layers. Odontoclasts and areas of granulation tissue are observed at the site of resorption. The pathological process is observed not only in the oral cavity but also with the disorders of cardiovascular, endocrine, and other body systems, conditioned by the changes in general health status.19,26–28
Dental pulp necrotic changes, the presence of microbes, periodontal lesions, exposed and wide dentin tubules are of great significance in the pathogenesis of EIR, since they contribute to the accumulation of bacteria and destroyed tissue remnants. Another contributing factor is undeveloped tooth root (wide dentin tubules, larger pulp tissue). Therefore, EIR is observed in children more often than in adults.18,19,28
EIR is primarily asymptomatic, while rarely observed clinical manifestations can be similar to the signs of the pulpal lesion, so the diagnosis must not be based merely on the clinical manifestations and patient's complaints. When resorption results in further pulpal necrosis, the tooth crown is discolored and patients present esthetic concerns, 29 and clinical picture can be comparable to those of periapical periodontitis, such as lack of tooth response to sensitivity testing and tenderness to palpation and/or percussion.
The roots can be shorter than typically estimated and/or have torn root edges. EIR related to trauma frequently appears as radiolucent crateriform depressions on the root surface with neighboring periradicular radiolucency. The root canal space is noticeable, representing an external resorption lesion to the root canal. Because of 2D nature of conventional radiographs, EIR is identified when it is in the interproximal sides of the root. Resorption over the vestibular/oral surface of the root is not noticeable. CBCT of the tooth is needed to clarify the character of the resorptive area, i.e., the accurate amount and dimension of the resorptive area, the extent of resorptive lesions alongside the root, and the presence of a root wall perforation.19,28,29
The treatment is accomplished considering the severity of root resorption. The prognosis of a positive outcome in the treatment of EIR is more often observed in adults. A more successful outcome prognosis for the treatment of EIR is found to be in adults. The wider the dentinal tubules, the more likely it is that destroyed remnants of the necrotic pulp and bacteria that activate odontoclasts are retained in tubules and destroy cement and dentin.8,22,30
External replacement resorption (ERR)
ERR is caused by severe trauma to the periodontal ligament, resulting in a loss of cell vitality and significant injury to cement. 11 Consequently, the cells of the periodontal ligament undergo necrosis followed by the loss of periodontal tissue. The dentin and cement of the tooth root are destroyed under the influence of osteoclastic activity. The destructive areas are soon replaced by alveolar bone, which is deposited by osteoblasts during the recovery process. Therefore, areas of resorption are not radiolucent, as in the case of EIR. The periodontal ligament between the tooth and alveolar bone is absent. Bone converges to the cement and dentine. ERR may be self-limiting and/or localized.11,19
Where resorption involves more than 20% of the root surface, the root loses its physiological mobility, which can cause a high-pitched metallic sound during percussion. Generally, if there is tertiary dentin formation, the tooth is susceptible to sensitivity testing, albeit with a delay. 11 The final diagnosis requires CBCT to define the degree of vestibular and oral ERR lesion and make a tooth prognosis.
ERR is observed in adults and sometimes in children31,32 and might cause tooth loss over time. In developing dentition, teeth that undergo ERR, the eruption is impaired, precluding further growth of the neighboring alveolus. This leads to the affected tooth becoming infra-occluded. Under these conditions, the immature alveolar ridge associated with the ankylosed tooth can lead to undesirable changes in appearance, phonetics, and function, which will cause complications in any future restorative treatment.33–35
External cervical resorption (ECR)
Certain types of resorptions cannot be classified as superficial, inflammatory, or replacement. These are grouped in the fourth category called either idiopathic, primarily, or cervical resorption. The etiology of this external resorption of the root surface is unclear,11–13 though it is observed mostly after dental treatment.12,13,18,36,37 It commonly starts from the cemento-enamel junction (CEJ) and develops due to damage to the subepithelial cement. The frontal teeth as well as first molars are mainly affected.38,39
ECR takes place in three steps: initiation, resorption (destruction), and repair. 40 Osteoclastic cells of periodontium occupy the root surface through the gaps in the cement, forming a fibrovascular lesion (resorption phase), which can eventually calcify and develop into fibro-osseous tissue (reparative phase).41,42 Minor lesions may resolve.39,43 However, most lesions of ECR are not self-limiting and commonly present with a continued resorption period. 19
ECR lesions are not infected; only secondary invasion of bacteria is observed. 41 Some authors still believe that ECR is caused and maintained by bacteria in the dentinal tubules and/or gingival crevices suggesting their inflammatory nature.19,44
ECR is rather challenging in terms of diagnosis since it is asymptomatic at the early stages, and the pulp and periodontium involvement takes place at the late stages of the development.12,45 Moreover, ECR is often misdiagnosed as caries. A pink spot on the tooth cervix is considered a pathognomonic clinical symptom.19,41 There may be clinical manifestations of pulpitis and apical periodontitis at more advanced stages with pulpal involvement.
Clinically, ECR is determined when the probe's tip meets the lesion and grasps the edges of the resorptive defect. ECR lesions are firm and scratchy during probing and can be distinguished from subgingival caries, which give a tactile sense of stickiness when probing. 46 Moreover, cervical resorption lesions frequently bleed profusely on probing due to their vascularity. Early ECR may not be clinically diagnosed, so a radiographic examination is needed.11,41,42
There is no typical picture present. Lesions may have well-demarcated or uneven borders in the cervical region. However, resorption of the dental hard tissue makes the early lesions radiolucent, while profound (fibrosseous) ECR defects can present with a spotted appearance which reflects the attempt to repair the resorbed root area. 46 The root canal outline is noticeable through the resorption lesion, demonstrating that the lesion is out of the root canal, considered ECR pathognomonic sign.
Internal root resorption (IRR)
IRR is also called internal granuloma.9,10 IRR is increasing the destruction of intraradical dentine and dental tubules in 1/3 of the middle or apical tooth root canal. 47 Resorption can involve one or multiple teeth. It is more common in incisors, however, can also be observed in the lateral group of teeth, especially in lower molars. A combination of internal and external resorptions is also possible.
IRR can be slow (years), fast (several months) or proceed with no marked pathological activity. 48 Inflammatory and replacement IRR are differentiated. Internal resorption is mainly caused by pulp infection, orthodontic treatment, and trauma.49,50 At the same time, some clinical cases show the presence of IRR in healthy unerupted teeth.
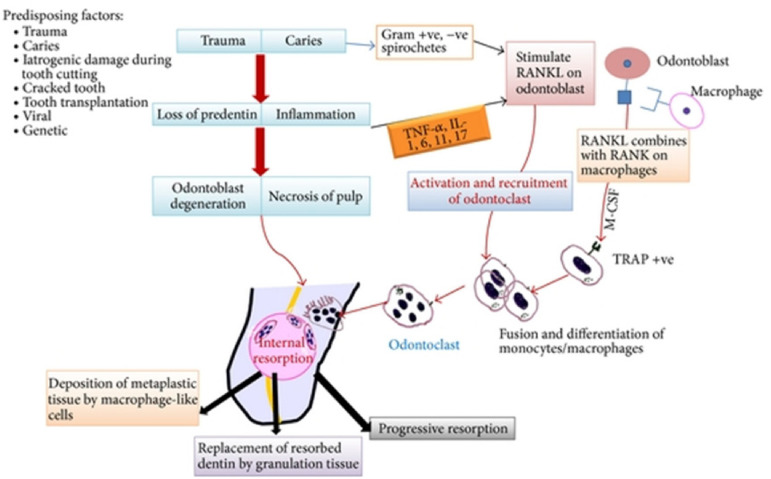
Many aspects of IRR have been studied, however, the true mechanism of its development is still unclear. IRR is a destructive process that occurs only in root canals and/or pulpal cavities. The pathological process can be different, conditioned by etiological factors. Nevertheless, a trauma (mechanical and chemical) to the protective tissues and stimulation by infection or pressure occurs.51,52 A schematic illustration of etiopathogenesis of internal root resorption is presented in Figure 1.
Figure 1.
Schematic demonstration of the etiopathogenesis of internal root resorption development. 52
IRR due to trauma is believed to develop in the following pattern. Sudden trauma to the tooth causes intrapulpal bleeding with further hematoma formation, which is replaced by granulation tissue. Proliferating granulation tissue exerts pressure on the dentin wall, the formation of predentin is discontinued, odontoclasts differentiate from non-differentiated storage cells of the connective tissue and resorption starts.51,52 Resorption proceeds in two phases – degradation of inorganic tissue structure followed by disintegration of organic substance.53,54
Three factors are crucial in the pathogenesis of IRR.14–17
cytokines, such as interleukin 1 (IL-1) and Tumor Necrosis Factor (TNF)
prostaglandins (for example, PGE2)
increase in internal tissue pressure is also possible.
In the case of internal inflammatory root resorption, the coronal pulp in the lesion is necrotic, while the pulp in the apical portion is viable, providing nutrients to the odontoclasts and permitting the development of the resorptive process. Moreover, complete pulp necrosis leads to the termination of resorption, as resorption of the hard tissues requires the presence of living cells.11,19,48 Internal inflammatory resorption, in its turn, can be complicated by root canal wall perforation. 55
Histologically, lesions of replacement resorption reveal the existence of metaplastic hard tissue transforming the resorbed dentin at the boundary of the lesion, which suggests both resorption and replacement: this metaplastic hard tissue is alike cement or osteoid tissues. 28 According to Stanley's data, tooth root resorption is accompanied by an accumulation of minerals in the tissues, similar to bone or cement. The resulting tissue does not look normal, so it is called "metaplastic" tissue.44,51 Thus, internal inflammatory resorption increases dentin loss, while replacement resorption of root canal is a successive accumulation of hard tissue, resembling bone or cement, but not dentin.51,56
Root resorption is known to occur mainly near the blood vessels. Heithersay et al. 43 assume that IRR can be caused by lateral blood flow through large collaterals. Blood supply peculiarities mentioned can create sufficient conditions for resorption to develop. It has been proved that active hyperemia supports and promotes odontoclastic activity due to the high partial pressure of oxygen. The resorptive process can be supported by electrical activity, such as piezoelectric potentials and blood flow potentials (an electrical charge which occurs when the blood flows through the blood vessels).
Multinuclear cells revealed in the lacunae formed due to IRR (Howship lacunae) resemble the structure of the cells occurring in bone resorption.57,58 In addition, waste products produced by bacterial cells can reach the parts of the root canal through the dentin tubes, where the pulp is still viable. In this case, IRR requires a strictly random arrangement of dentin tubules. At one end, they must open into the area where the tissue necrosis occurred so that microorganisms can penetrate the tubules. The other end of the tubules must be in the area of the root canal where the pulp tissue is still viable. The condition is rarely observed, which might explain that progressive IRR in permanent teeth is relatively infrequent.51,57,58
However, progressive IRR with the formation of lacunae (as big as 2 mm, that are manifested radiologically) is accompanied by infection and hard tissue necrosis in the coronal part of the tooth root. Necrosis can develop when, because of progressive IRR, the destruction becomes extensive, with the root surface or crown perforation and communication between the mouth and the pulp cavities. 51
Pulpitis and resorption in people with general health problems proceed in a different way. Notably, all the factors which affect the mineralization of the hard tissue of a tooth can influence the resorptive process as well. These include, for example, low levels of vitamins A, C, and D, which can affect the formation of extracellular material, dentin formation, and mineralization. Excessive vitamin D in the body leads to impaired dentinogenesis, calcification of the pulp, and stimulation of the resorptive process.3–6 A high level of parathyroid hormone was found to contribute to the hypomineralization of newly formed dentin. There is evidence of a possible metastasis of a malignant tumor in the pulp, followed by an increase in root canal pressure and stimulation of the resorptive process.14–17
IRR is clinically asymptomatic, so the presence of resorption can be randomly revealed by radiographic examination. In complete coronary resorption, a formation of a pink spot on the coronary surface might be observed (pink spot disease), a granulation tissue visible from the resorption area9,49,59 (Figure 2). With an asymptomatic process, pathology can develop if the lesion does not affect the periodontal tissues. 60 IRR, complicated with perforation, differs from IRR by the large size of the lesion, which leads to the perforation of the root cement towards the periodontal ligaments. Patient complaints usually accompany root perforation, which results in pathological changes in the periodontium.
Figure 2.
‘Pink spot’ on the crown`s vestibular (A) and palatal (B) surfaces of the right central incisor. 49
In general, during the development of the resorption process, the teeth are partially viable, so pain typical of pulpitis may initially occur. Signs of periodontal diseases, such as the presence of fistula, and tenderness on percussion and palpation, are expected at the later stages of development. Pain may occur due to coronal perforation when metaplastic tissue grows from the periodontal tissue to the oral cavity and is exposed to aggressive stimuli.9,59,60
On visual examination, IRR can be revealed by discoloration of the tooth crown, by conventional radiographic examination, CBCT, and light- and electron microscopy.21,59–61 Radiographic examination is mandatory for IRR diagnostics, revealing the presence of round or oval-shaped radiolucent areas in the pulp chamber. The edges are smooth with clear borders, distorting the natural shape of the root canal.7,62 Several radiographic films of different projections are required to determine the degree of dental tissue loss and draw up a treatment plan.
Diagnosis is usually confirmed radiographically. Radiographically, IRR lesions are defined as a radiolucent defect with symmetrical round or oval borders. However, sometimes the radiographic appearance of root resorption may differ from the abovementioned images.28,63 Although the parallax method can be used to identify the location and character of the resorptive lesion, IRR may still be misdiagnosed in teeth with multiple roots as ECR since the root canal of an intact tooth may be superimposed over the affected root, thus providing the appearance of ECR. 63 High-resolution CBCT is optional to confirm the exact nature, position, and amount of the IRR and the existence of a perforation.59,64
Endodontic treatment is considered to be the treatment of choice for IRR. Root canal treatment removes the granulation tissue and stops the blood supply of the clastic cells. IRR is a clinical challenge for clinicians due to the difficulties of instrumentation and filling of the root canal. In the case of root canal perforation, the working length determination cannot be accomplished with an apex locator. 9
One of the most important factors is the application of sodium hypochlorite for the chemical dissolution of pulp tissue. The application of EndoActivator helps to activate sodium hypochlorite and facilitates the penetration of the solution to all the areas of the root canal. This ensures a complete chemomechanical debridement of the root canal system.49,65
The application of calcium hydroxide as a temporary dressing material increases disinfection effectiveness. 29 As a permanent root canal filling, the material should be flowable to seal the root canal system as well as the resorptive defect. Thermoplastic gutta-percha techniques are the methods of choice which provide the best results when the root canal walls are intact. In the case of root canal perforation, MTA is considered to be the material of choice to seal the perforation as it is biocompatible, bioactive, and well tolerated by periradicular tissues.3,9 Currently, Biodentine is widely used as a new calcium silicate-based material for filling resorptive defects. In addition to biocompatibility, Biodentine has some supplementary and desired properties over MTA, such as better antibacterial characteristics, bioactivity-inducing hard tissue formation, better handling, self-adhesion to dentine, less shrinkage, and a shorter setting time. 3
Treatment approaches of IRR using endodontic regenerative treatment protocols
In the 1960s, the terms "regenerative endodontic treatment" (RET) and "revascularization" were founded. Pulp revascularization is a technique that aims to replace previously vital tissue that has been lost due to pulp necrosis with new vital tissue. Revascularization techniques may have an advantage over traditional root canal therapy in the treatment of IRR because they allow for the replacement of missing dental tissues. As a result, the possibility of a better prognosis is a realistic possibility. 66 This is particularly the case of immature permanent teeth, as the possibility of further maturation lowers the risk of root fracture and successive tooth loss later in life. 67 RET promotes root development and thus prevents root fracture by restoring the flow of blood to the tooth in situations of pulp necrosis with an open apex in permanent teeth, not only eradicating and/or preventing apical periodontitis but also eradicating and preventing root fracture. 68 Only three clinical reports are available to date on the use of revascularization in the treatment of IRR.66,69,70 Due to a lack of research, the efficiency cannot be determined conclusively until more research is conducted. Furthermore, because these treatments were only performed in the last five years, there is no information on the long-term results and durability of the revascularization procedure. 71
However, the most recent advancement in the treatment of IRR is RET, which allows for the repair of damaged structures caused by resorption, thus providing a good long-term prognosis for those teeth involved. 69 The major consideration in RET is to decontaminate the root canal system as thoroughly as possible using intracanal medicaments. In RET procedures, the most commonly used intracanal antibiotic combinations are triple (metronidazole, ciprofloxacin, and minocycline) or double (metronidazole, ciprofloxacin). Although antibiotic combinations have been linked to positive outcomes in RET procedures.66,72,73 After a delayed replantation procedure of a mature permanent maxillary central incisor, Tambakad and Naidu 70 described an unusual RET protocol in an internal and external root resorption case. In that case, unlike previous RET reports, platelet-rich plasma (PRP) was used instead of MTA during the replantation procedure, and glass ionomer cement was applied to the PRP. Furthermore, regenerated vital or vascular tissues were injected with a double antibiotic paste (minocycline, metronidazole). The tooth was asymptomatic at the 12-month follow-up, but there was no evidence of hard tissue deposition in the IRR area.70,74 The previous case reports’ findings were significant, and they should be used as a starting point for revascularization treatment in IRR teeth. Nonetheless, the outcomes of all of these cases show that revascularization is effective when treating teeth with IRR. Revascularization was successful in all of the treatments. All previous symptoms vanished, existing root resorption was stopped, and the root canal walls thickened after treatment, reducing the risk of a root fracture. As a result, revascularization should be considered as an alternative to traditional root canal treatment for IRR cases. It has been shown to be effective in the treatment of IRR. 71
Surgical approach as a second intention should be considered when it is not possible to get access to the defect through the canal. Surgical approach provides an opportunity to get direct access to the lesion and to accomplish a mechanical cleaning of the resorption area. 65
Transient apical breakdown (TAB)
Andreasen et al. 75 first described the process of TAB, which is an uninfected transitory resorption of the root apex and the adjacent bone. There is belief that the TAB resolves within one year and is associated with moderate trauma. It may relate to the healing process and elimination of necrotic and damaged tissue11,76:
Examination of the patient clinically may disclose temporary tooth discoloration and postponed or no response to sensibility testing. Sensibility alteration to testing remains particularly if root canal obliteration occurs by tertiary dentin. Preliminary radiographic examination may reveal enlargement of the periodontal ligament space and blurry appearance or loss of apical lamina dura may occur. The radiographic picture of the periodontal ligament and lamina dura returns to a healthy state within 12 months. This occurrence is an EIR with a short resorption period followed by reparation. 11
Classification
Based on several parameters such as resorption location, lesion size, histological picture, etiopathogenetic peculiarities, radiographic observations, various classifications of tooth root resorption have been suggested. Andreasen et al. proposed a classification which distinguishes resorptions between two types: internal (inflammatory and replacement) and external (superficial, inflammatory, and replacement).65,77 Although tooth root resorption can be classified based on the various approaches, however one of the most common classifications is based on the pathogenetic process shown in Table 1.59,78
Table 1.
Types of tooth root resorption.
| Types of resorptions | |
|---|---|
| Internal | External |
|
|
The severity of root resorption can be classified on a scale of 0–4.79,80 Brezniak and Wasserstein 81 described three degrees of root resorption induced by orthodontic force (Table 2).
Table 2.
Root resorption conditioned by orthodontic force. 81
| Degree of root resorption | Root layers included in resorption process | Description |
|---|---|---|
| 1 | Cement or superficial resorption with further remodeling. | Here only outer layers of cement are resorbed with further regeneration or remodeling. |
| 2 | Dentin resorption with further restoration. | Outer layers of cement and dentin are resorbed and mostly reconstructed by cementoid substance. The shape of the root after such resorption can be similar or different from the original shape. |
| 3 | Apex circumferential resorption. | Here, the hard tissues of the root apex are entirely resorbed, and the root radiographically appears to be shortened. No regeneration is observed. |
Levander et al. 82 categorized four levels of apical resorption, while Heithersay 43 suggested four levels of cervical resorption (Table 3).
Table 3.
Levels of a lesion in apical and cervical root resorption.
| Root Resorption Levels | ||
|---|---|---|
| Level | Apical resorption 82 | Cervical resorption 43 |
| 1 | Root resorption is insignificant and gives root apex irregular contour. | Root resorption is a small invasive cervical lesion presenting superficial dentinal erosion. |
| 2 | Root resorption lesion on the hard tissues is up to 2 mm. It is called minor resorption. | Root resorption lesion is restricted and involves the dentin near the pulpal chamber. However, it does not spread further. |
| 3 | Root resorption affects up to the level of the first third of the root. Therefore, the resorption is assessed as severe. | Root resorption lesion penetrates profoundly into the dentin up to the first third of the root. |
| 4 | Root resorption involves spread further than the first third of the root length and, at this stage, is defined as extreme. | The root resorption process is extensively aggressive and extends towards the apex further than the first third of the coronal root. |
More recent, another classification was proposed by Patel et al. (Table 4), which involves external cervical resorption.
Table 4.
Three-dimensional classification of ECR.
| Height | Circumferential spread | Proximity to the root canal |
|---|---|---|
| 1: At cemento-enamel junction level or coronal to the bone crest (supracrestal) 2: Extends into coronal third of the root and apical to the bone crest (subcrestal) 3: Extends into mid-third of the root 4: Extends into apical third of the root |
A: ≤90° B: >90° to ≤180° C: >180° to ≤270° D: >270° |
d: Lesion confined to dentine p: Probable pulpal involvement |
Etiopathogenesis
Though the etiology of tooth root resorption is still not well understood, there are numerous etiological and risk factors noted, which can initiate or trigger resorption. We suggest dividing these factors into two groups, i.e., endogen (host-related) and exogen factors. Endogen factors include body peculiarities, such as gender, age, race, characteristics of occlusion, genetic predisposition, and others.9,14–16,83–89 These factors are outside of any control, however, should be considered particularly when planning orthodontic treatment, after which unwanted changes in the tooth root are often observed. Mechanical factors occurring in orthodontic treatment (detailed description in the section of Orthodontic Treatment Mechanics Factors) can be a precondition to the development of root resorption, but these can be controlled and regulated to prevent complications.83,90 Exogen factors include trauma, pulp infection, orthodontic treatment, tooth bleaching, etc..7–10,19,91–93 Thus, etiological and risk factors which can initiate or stimulate the development of resorption can be summed up as presented in Table 5.
Table 5.
Endogenic (host-related) and exogen factors of tooth root resorption.
| Exogenic factors | Endogenic (host-rated) factors |
|---|---|
|
|
The teeth which previously suffered trauma or might have already been resorbed are more susceptible to the force they undergo in orthodontic treatment. Therefore, it is preferable to wait for at least three months for a re-implanted or transplanted tooth. The risk of resorption in the teeth which have experienced internal bleaching is defined distinctly from orthodontic treatment. Like traumas, the risk of resorption in orthodontic treatment is higher in a tooth with internal bleaching. However, catalytic impact of high temperature can initiate root resorption after whitening non-vital teeth. The sodium perborate with water is less harmful which unlikely to cause resorption.94–96
Resorption can occur because of an injury, such as preparation or trauma to a tooth crown. Injuries to the teeth can damage the gum, alveolar bone, periodontal fibers, tooth root cement, the nerves and blood vessels in the pulp, which leads to difficult healing and possible complications, such as pulp necrosis, root resorption, root canal obliteration, and destructions of alveolar bone. 97 Facial traumas mainly involve anterior teeth with further development of complications. 91 Therefore, radiographic changes and pulp vitality should be assessed over time. There is evidence that in 2% of cases, resorption develops after the tooth root dislocation. It can be caused by vital root resection and following calcium hydroxide pulpotomy. Experimentally, it can be induced by diathermy. Anachoresis is also mentioned as a causative factor.7–9,19,91 Orthodontic treatment is also considered to be an etiologic factor of resorption.10,92
The primary role of dental pulp inflammation and bacterial factor in the pathogenesis of these conditions is confirmed by some studies. 93 Resorption occurs with caries progression as well, as an alternating process with active and passive stages. At the remission stage, stratification of hard tissue in the form of irregular dentin can occur.3,49,55,59,78
Some authors have reported that those who underwent orthodontic treatment at or before the age of 11 have a lower rate of tooth root resorption due to the preventive effect of the pre-dentin layer of underdeveloped roots. This resorption can be avoided if orthodontic tooth movement is carried out before the final formation of the tooth root. 83 Orthodontic movement of the teeth with underdeveloped roots does not interfere with the tooth development, but these roots tend to be shorter. Vieira-Andrade et al. 98 concluded in their study that age is associated with a higher incidence of inflammatory root resorption in permanent molars. Age is supposed to have substantial relation to root resorption since it is commonly observed in people over 20 years. However, no constant association between chronological age and root resorption has been established. 99
Gender is also considered a risk factor for tooth root resorption, with males being at a higher possibility of root resorption than females. 9 However, some authors reported that gender is not associated with the root resorption of the neighboring impacted teeth. 100 Some ethnic groups, namely Hispanics, are more prone to resorption than Asians.84,85 The stimulation of the osteoclast formation (resorption cells) may be genetically linked. Genetic differences related to the interleukine-1ß (IL-1ß) gene, which is associated with the inflammatory process due to orthodontic treatment, may clarify the development of certain external apical resorptions. Interleukin IL-1 (IL-1ß) allele 1 has 5.6-fold increased risk of external apical root resorption (EARR). IL-1ß (13954) gene proposes a role for this cytokine in the pathogenesis of EARR and the defensive mechanism of the cement against root resorption. Qualitative and quantitative measurement estimation of the external root resorption was 44.9% and 42.9% for monozygotic twins and 24.7% and 28.3% for dizygotic twins, respectively. The overall heritability estimation was 0.34.14–16,83,86,87
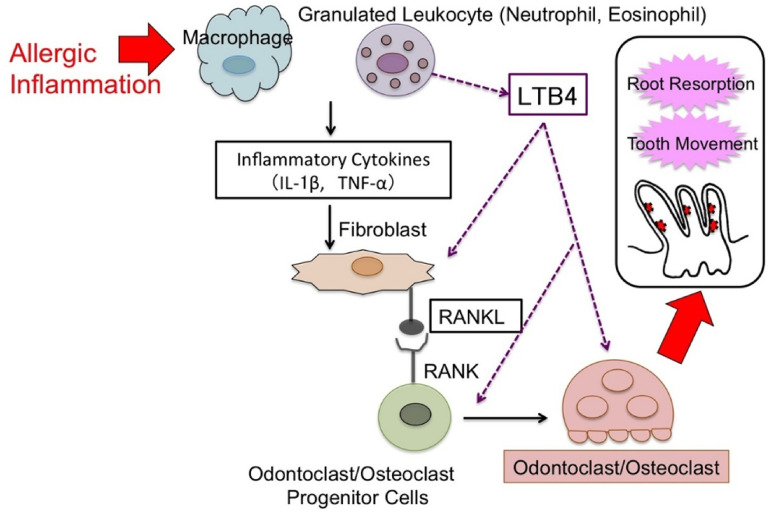
Chronic asthma and allergies increase the risk of inflammatory root resorption during orthodontic treatment101,102 (Figure 3). Patients with chronic asthma have a greater susceptibility to apical root resorption of the maxillary molars. This is due to the fact that asthma permits the inflammation of the maxillary sinuses to be closely related with the apex of the upper molars and bicuspids. Other researchers consider systemic disorders and hormonal deficiencies as risk factors; however, the assumption is not conclusive.103–105
Figure 3.
Scheme of possible explanation of the orthodontically induced root resorption due to the risk factor of allergy. 102
Root resorption may initiate as a result of a neighboring unerupted tooth. A typical problem with unerupted canines is the resorption of the adjacent lateral incisors or bicuspids roots. The 3D evaluation of unerupted canines and root resorption of lateral incisors revealed no root resorption in 40.4% of cases, minor root resorption in 35.7%, 14.2% moderate and sever root resorption in 14.2% and 4.0% cases respectively. 106 Eruptive process or migration of the unerupted canines during the root growth probably can increase the risk of root resorption. One of the most significant predictors for root resorption of the incisors and first bicuspids is up to 1 mm physical proximity between unerupted canine and neighboring roots. The resorption which happens at the neighboring roots can be triggered by direct physical injury, increased force at local root cement, and dentin or focused resorptive molecules from the canine follicle. 107
Development of severe root resorption is considerably less likely in patients with an adequate overjet and Class I occlusion at the start of orthodontic treatment. Probably, this reproduces the less movement of the teeth, mainly of the maxillary incisors. A mean of approximately 1 mm of apical root shortening occurs in patients with Class I. However, patients with Class II division 1 showed a mean root shortening of more than 2 mm. Root resorption depends on the degree of incisor root displacement and the quantity of movement required. Class III cases are overrepresented with severe root resorption, possibly due to an increased chance that compensatory proclination of upper incisors for Class III skeletal relationships have their roots forced against the palatal cortical plate. Some malocclusions lead to undesirable ‘jiggling’ of the teeth once the teeth are in occlusion.88,89 Such patients may have shortened roots before treatment and are consequently at a higher risk of root resorption during treatment, maybe due to uneven loading of the periodontium. Habits may also contribute to the degree of root resorption. Increased root resorption is observed in nail-biters before and after orthodontic treatment. This could be attributed to increased force on the periodontium for sustained periods and actual digit habits. 101 Anterior open bite is also an essential factor in root resorption, as a reciprocating movement was assumed to be caused by the orthodontic force and the force of the tongue pushing the teeth in the opposite direction. Patients who have open bite occlusal relationships had 26.1% of inflammatory root resorption. 83
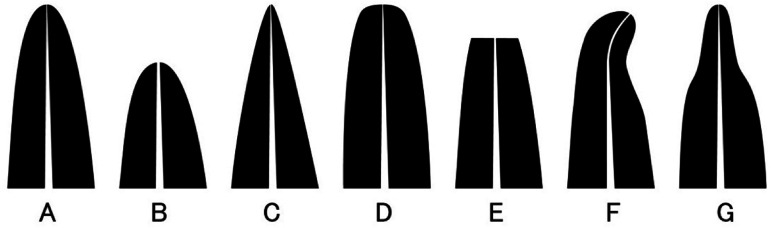
Atypical root shape can be a resorption risk factor.83,108 Root shapes are typically defined as normal, shortened, pointed, blunt, eroded, bent, bottle shaped 102 (Figure 4). Blunt or dropper-shaped apices demonstrate increased resorption compared to apices with regular shapes. An unusual root shape was assumed to cause root resorption due to reduced resistance to mechanical stimuli. The occurrence of root resorption in hypofunctional teeth with atypical root shapes is higher than in functional teeth. The reason is probably that absence of occlusion contacts in hypofunctional teeth did not cause physiological root transformation after teeth eruption; thus, root resorption occurs. Endodontic treatment can be another risk factor for progressive severe inflammatory root resorption during orthodontic treatment. 109 Various types of root resorption are presented in Figure 4. Figure 5
Figure 4.
Morphology classification of the root (A) Normal, (B) Shortened, (C) Pointed, (D) Blunt, (E) Eroded, (F) Bent, (G) Bottle shaped. 102
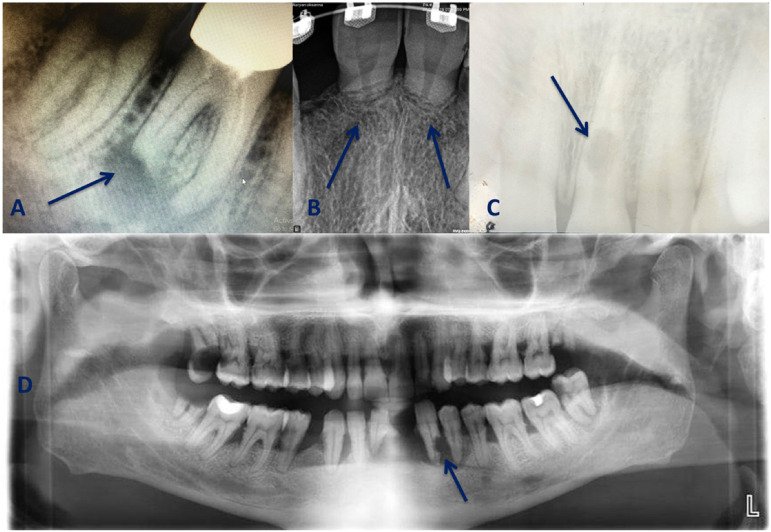
Figure 5.
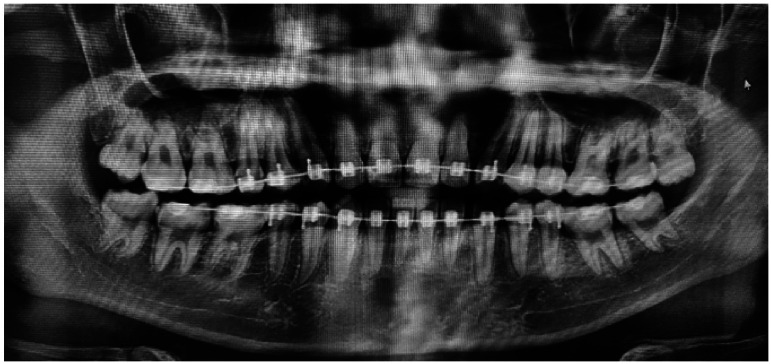
A. Apical root resorption. The tooth has previously undergone endodontic treatment, but the root canals are insufficiently filled, which leads to periapical inflammation followed by root resorption. B. Apical replacement resorption following orthodontic treatment. In this case, resorption was caused by the incorrect application of orthodontic force. 90 C. Tooth root internal resorption. CBCT is preferable to confirm root perforation. 9 D. External root resorption in the lower left canine. The patient reports a jaw trauma he experienced many years ago, which caused the loss of the lower-left lateral incisor. OPG reveals the presence of generalized periodontitis.
Orthodontically induced root resorption
The concept of inflammatory root resorption due to orthodontic treatment is used to distinguish it from other causes of root resorption in permanent teeth. 1 The force applied in orthodontic treatment inevitably leads to the development of the inflammatory process necessary to move the tooth while being the leading cause of root resorption. Therapeutic measures involve the bone, periodontal ligament, and cement. 4
Resorption prevalence in different teeth varies. In particular, the incisors of the upper jaw are more susceptible to resorption; they often resorb after orthodontic treatment. 110 Lower incisors and the distal root of the first permanent molars come next. Root resorption rate in orthodontic treatment ranges from 4 to 91%.111–113 It was also revealed that root shortening of varying degrees was observed in almost all patients and in up to 91% of the teeth. In few cases, it exceeded 4 mm, however. It has been reported that external apical resorption occurs in upper canines and lateral incisors, making 8.5% and 2.6% of cases, respectively. 4% of patients experienced root resorption 6 months after the fixed orthodontic appliances were placed. 114 Figure 6 demonstrate root resorption conditioned by orthodontic treatment.
Figure 6.
Orthodontic treatment has often been found to result in external apical root resorption across the mandibular anterior teeth and the first molars. The extent of root resorption is dependent on the duration, the type of movements carried out, and the magnitude of forces involved.
Destruction of the protective cement layer occurs due to EIR conditioned by orthodontic treatment. 5 The cement layer can regenerate and protect the underlying dentin layer from resorption. 19 Provided that the dentin is not involved, the process is controlled during the orthodontic treatment. When the stimulus destroys the cement and inhibits the repair process, the dentin is exposed. When exposed to destructive cells formed in the periapical ligament, dentin is the beginning of a pathological process. 47 The cement can be regenerated if the dentin is intact. When the dentin decays, the cement cannot be repaired. Such resorption can affect the root and neck of the tooth. The newly formed cement covers the resorption site. 50 Resorption leads to root shortening, while ECR provides favorable conditions for the growth of microorganisms in the lesion.
Reduction of root resorption rate requires using an optimal force of 20–150g to move the tooth. Periodontal ischemia is conditioned by excessive force, especially in adults, in whom more significant apical load occurs, conditioned by the thicker cement layer in comparison with those in adolescents. 56 The root apex is more vulnerable to resorption than the cervix because it is softer, hypomineralized, and contains less Sharpey's fibers. The area of compression of the periodontal ligament created by tooth movement increases the likelihood of root resorption. The resorption is a side effect of orthodontic treatment, but it can be reduced or restored after the orthodontic force is removed. Even though resorption is inevitable in orthodontic treatment, it is insignificant, presenting radiologically up to 2.5mm. 62 In severe root resorption, the tooth becomes mobile, endangering the entire course of treatment. Thus, assessing the risk factors for root resorption before orthodontic treatment is crucial to avoid further adverse outcomes.21,73,115 In fact, some patients tend to root resorption and should be informed of this before the treatment. Many risk factors for resorption are mainly related to genetic predisposition or general health status.116,117 Risk factors can be of a local character, i.e., associated with the patient's past dental history, especially orthodontic treatment. Reducing the advancement of the resorption in orthodontic treatment is provided by changing the applied force. Root resorption caused by orthodontic treatment is an uninfected inflammatory process, which is not fully understood. Considering the numerous predisposing factors for orthodontic root resorption in orthodontic treatment, it is necessary to analyze the risk factors associated with orthodontic treatment to eliminate them, avoid complications, and achieve a successful result.
Factors of Orthodontic Treatment Mechanics
There is an ongoing debate about whether root resorption can be caused by orthodontic force alone and whether a small amount of force can cause it. As a solution, some authors have suggested using force ranging from 7 to 26 g/cm2. The amount of force used is a determining factor, and the intermittent use of force can cause less damage. The incidence of root resorption may be induced by using greater orthodontic force and hyalinization of the periodontal tissue caused by the high activity of cementoclasts and osteoclasts.118,119
Long-lasting orthodontic treatment had been established to be a causative factor of resorption. One month of additional treatment causes extra root resorption of 0.1 and 0.2 mm of the most severely resorbed central and lateral incisor, respectively. Typically root resorption is absent when treatment duration does not last more than 1.5 years. Complete treatment longer than 30 months has been confirmed to increase the risk of severe resorption, as measured by the number of patients and the number of teeth. Figure 7 demonstrates root resorption development after orthodontic treatment.
Figure 7.
Prolonged orthodontic treatment usually demonstrates external root resorption. As can be seen in the figure, the apical region of the root tends to resorb under the influence of orthodontic forces and shows a more bulbous end after an extended duration of treatment.
Although continuous force has been proven to produce quicker tooth movement than intermittent force, it is associated with a greater risk of root resorption. Intermittent force is applied to avoid more significant root resorption, which allows the reparative mechanism to be initiated. The application of intermittent force was obtained with a 4-day force application period followed by a 3-day resting period, and considerably less overall root resorption was found. This eventually has led to using light continuous forces for carrying out all types of tooth movements. Reparative cement formation occurs over-dependent and tooth movement when a load is applied intermittently for a long time. Arc activation is preferable once every 2-3 months, rather than once a month.83,120
Conditioned by the root morphology and force direction, the root surface compression area is more vulnerable to resorption than the tension area. Periodontal ligament compression in tipping movement was more significant in the apex and cervix of the tooth, whereas in vestibular root torque, the root resorption occurs more on the apex. The extent of tooth movement in the bodily tooth movement was less than half that in the tipping tooth movement. The most significant amount of tooth movement took place when 10gm tipping and 50gm bodily force was applied. The resorption from the extrusive force was restricted and not considerably different from the control group. Intrusive force considerably increased root resorption by 4-fold and is considered the most harmful tooth movement since the forces are focused and compressed on the apical tooth part.121,122 A new approach to reducing root resorption during intrusion has been suggested by applying a lighter and more constant force and controlling the force direction and the vestibulo-oral position of the tooth. Application of substantial force beyond its acceptable limits for tooth movement will increase the likelihood of root resorption. Tooth vertical movements apically and proclination of incisor are critical indicators of external apical root resorption. Tooth rotation leads to the formation of many resorptive lacunae on the root surface revealed by scanning electron microscopic examination. The resorption zones were located primarily at the middle root third, in regions that corresponded to the major sites of the roots. CBCT showed statistically significant volume loss in root resorption after quick maxillary expansion. Expansion with passive self-ligating brackets showed clinically significant expansion (approximately 3.5 mm in 8 weeks) with no apical root resorption.123,124
Diagnosis and radiological image
External and internal types of resorptions have common features, so the clinical and radiological manifestations of both conditions are often quite similar. In addition, the presence of carious lesions and other conditions present in the form of radiolucency can be confusing in the differential diagnosis of internal and external resorption.9,21,22,110
Clinical diagnosis of IRR is rather challenging. Although this condition has its characteristic symptoms, it is still complicated to reveal.29,59,60,110 The diagnosis of IRR is primarily based on two aspects. The algorithm of the complex diagnosis is figured out with the help of these two aspects:
resorption signs in a radiographic image
clinical manifestations
Root resorption is nearly always clinically asymptomatic, especially at an early stage of development. ECR can clinically present discomfort and manifest as pink discoloration of the neck region, while apical resorption may be completely asymptomatic. Considering all this, the diagnosis of root resorption can indeed be considered very difficult, especially at the early stages. 7
Histological and radiological methods can assess tooth root resorption. The benefit of the histological technique is that it permits to directly observe the root's surface, and even the most minor lesions are visible. Several radiological methods are used to diagnose and differentiate various types of root resorptions. However, many dentists prefer three-dimensional imaging, such as CBCT and micro-CT.125,126 Absence of the overlapping structure providing better visibility and simplifies root resorption diagnosis. 127 In orthodontics, radiological examination is carried out 3–6 months after installing the orthodontic appliances and then repeated once a year.
Current approaches to detecting biological markers of root resorption are considered sensitive, safe and predictable. 128 Specific biomarkers such as aspartate aminotransferase, salivary sIgA and serum IgG are also informative for this purpose. Biomarkers generated by orthodontic tooth displacement indicate biological changes.129,130 The presence of organic matrix proteins and cytokines, released from the adjacent bone and dentin into the gingival crevice confirms the initial diagnosis. 131 In tooth root resorption, as well as in periodontal pathology gingival crevicular fluid volume increase and pH changes are observed.86,132–134 Over 2000 new biomarkers associated with root resorption have been identified by several studies.135,136 A large amount of dentin sialoprotein and dentin phosphoprotein were found in physiological root resorption.137,138 Detection of these biomarkers can be helpful in diagnosing root resorption.
Thus, radiographic interpretation of the resorptive process is essential for the differential diagnosis and prediction of treatment outcomes. 61 Three-dimensional imaging makes it possible to precisely assess the required area without overlapping the surrounding structures.47,137 In contrast to conventional computed tomography, CBCT at lower radiation doses provides reliable information. 139 Daily use of CBCT for endodontic purposes is not suggested, but it is justified to assess dental-alveolar injury when conventional radiographic examination methods provide insufficient information. 140 Only high-resolution small-field scans are acceptable for the diagnosis and treatment of resorption lesions. Radiation dose reduction is essential to optimize patient affection. 77 This will guarantee agreement with as low as reasonably achievable (ALARA) principle, depending on the quantity of affected teeth and the areas involved.
Several radiographic images with different projections need to be made to accurately distinguish between internal and external resorption. If a radiolucent area in the radiographic image does not change its position, IRR is diagnosed (Table 6).
Table 6.
Radiological study of root resorption.
| Internal resorption | External resorption |
|---|---|
| 1. Roentgenographically presents as round, symmetrical lesion | 1. Pathological lesion has rough, isolated, asymmetrical edges |
| 2. The position of the lesion is inside the root canal, regardless of the X-ray projection | 2. The location of the lesion changes with different projection of the image |
| 3. Resembles an enlarged pulp cavity or root canal margin | 3. Presents as an isolated area, demarcated from the root surface |
CBCT is considered as an assistant and not a replacement for conventional radiography. CBCT examination is accomplished after detailed clinical and conventional radiographic evaluation has been carried out.
Discussion
Resorption of tooth and periodontal apparatus is represented by loss of dentin, cement, or bone conditioned by certain physiological or pathological processes. 3 Tooth root inner and outer walls are secured by a thin antiresorptive barrier,1,2 but various chemical, mechanical, and thermal factors can cause structural changes in the barrier, promoting the resorption process.3–6
Several root resorption classifications have been suggested,19,20,43,59,78–82,140 each having its own characteristics and advantages, but none of them is complete. Histological classifications are mainly performed after tooth extraction and are therefore clinically ineffective. Regarding Heithersay classification13,41,43 is only two-dimensional i.e., it is valid only if the resorption of the cervix is limited only to the interproximal sides of the tooth. In fact, this is uncommon, as ECR often involves the vestibular surface of the teeth and are therefore underestimated. A three-dimensional classification proposed by some researchers allows overcoming these limitations and accurately documenting the true nature of the ECR. 141
Various etiological factors in the development of the resorption, such as trauma, pulpal infection, orthodontic treatment, bleaching, etc. are described in the literature.7–10,19,91–93 Risk factors include patient's gender, 9 age, 99 ethnicity,84,85 root form,83,106 occlusal peculiarities,83,88,89 genetic predisposition,14–16,83,86,87 underlying diseases.101,103,105 The study of the above literature showed that there is no clear definition of etiological risk factors, all these factors either contribute or provoke the development of resorption.
Though each type of resorption has its characteristic pathophysiologic peculiarities, there are two factors mandatory for the development of the condition, i.e., trauma (mechanical, surgical, chemical, among others) and stimulation (infection, pressure etc.).7,140 Trauma is associated with unmineralized tissues covering the root surface, precement or predentin. The resorption process is initiated by multinucleated cells that colonize exposed mineralized tissues. In the absence of stimulation of resorption cells, a spontaneous termination of the process and recovery within 2-3 weeks is observed if injured tissue does not cover a wide surface area. However, bone cells sometimes attach to tooth roots before cement production resulting in ankylosis.1,2
Root resorption is generally asymptomatic, but clinical signs of pulpitis or apical periodontitis may be observed. Crown discoloration is sometimes the only clinical manifestation.9,59,60 Consequently, the diagnosis cannot be based solely on clinical findings and a radiographic examination is required.28,63 In this case, the most informative radiological study is CBCT, which reveals the site of resorption, the size of the lesion, and allows drawing an appropriate treatment plan. 64
Conclusion
Although the etiopathogenesis of tooth root resorption is not fully understood, the article presents the currently adopted approaches to the issue. Division of etiological factors into two groups (endogenic and exogenic) may enhance further understanding of the possible causes and mechanisms of root resorption and allow practitioners to monitor high-risk patients and make timely diagnoses, thereby preventing further complications. Moreover, radiographic examination and CBCT are indispensable for the diagnosis of root resorption.
Footnotes
Consent statement: Not applicable
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical statement: Not applicable
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Artak Heboyan https://orcid.org/0000-0001-8329-3205
Mohmed Isaqali Karobari https://orcid.org/0000-0002-0313-9695
Anand Marya https://orcid.org/0000-0003-2009-4393
Zohaib Khurshid https://orcid.org/0000-0001-7998-7335
Dinesh Rokaya https://orcid.org/0000-0002-3854-667X
Gustavo Vicentis de Oliveira Fernandes https://orcid.org/0000-0003-3022-4390
References
- 1.Brezniak N, Wasserstein A. Orthodontitis: “the inflammation behind tooth movement and orthodontic root resorption. In: Shroff B. (ed) Biology of orthodontic tooth movement: current concepts and applications in orthodontic practice. Switzerland: Springer International Publishing, 2016, pp.67–101. [Google Scholar]
- 2.Al-Qawasmi RA, Hartsfield JK, Jr., et al. Genetic predisposition to external apical root resorption. American Journal of Orthodontics & Dentofacial Orthopedics 2003; 123: 242–252. [DOI] [PubMed] [Google Scholar]
- 3.Umashetty G, Hoshing U, Patil S, Ajgaonkar N. Management of Inflammatory Internal Root Resorption with Biodentine and Thermoplasticised Gutta-Percha. Case Rep Dent. 2015;2015:452609. doi: 10.1155/2015/452609. Epub 2015 Oct 22. PMID: 26579316; PMCID: PMC4633547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abuara A. Biomechanical aspects of external root resorption in orthodontic therapy. Med Oral Patol Oral Cir Bucal 2007; 12: E610–E613. [PubMed] [Google Scholar]
- 5.Olivieri JG, Duran Sindreu F, Mercade Met al. et al. Treatment of a perforating inflammatory external root resorption with mineral trioxide aggregate and histologic examination after extraction. J Endod 2012; 38: 1007–1011. [DOI] [PubMed] [Google Scholar]
- 6.Ne RF, Witherspoon DE, Gutmann JL. Tooth resorption. Quintessence Int 1999; 30: 9–25. [PubMed] [Google Scholar]
- 7.Tronstad L. Root resorption-etiology, terminology and clinical manifestations. Endod Dent Traumatol 1988; 4: 241–252. [DOI] [PubMed] [Google Scholar]
- 8.Al-Badri S, Kinirons M, Cole Bet al. et al. Factors affecting resorption in traumatically intruded permanent incisors in children. Dent Traumatol 2002; 18: 73–76. [DOI] [PubMed] [Google Scholar]
- 9.Heboyan AG, Avetisyan AA, Margaryan MM. Clinical case of a rarely diagnosed tooth root internal resorption. The New Armenian Medical Journal 2018; 12: 87–92. [Google Scholar]
- 10.Consolaro A. Extreme root resorption in orthodontic practice: teeth do not have to be replaced with implants. Dental Press J Orthod 2019; 24: 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel S, Pitt Ford T. Is the resorption external or internal? Dent Update 2007; 34: 218–229. [DOI] [PubMed] [Google Scholar]
- 12.Mavridou AM, Bergmans L, Barendregt Det al. et al. Descriptive analysis of factors associated with external cervical resorption. J Endod 2017; 43: 1602–1610. [DOI] [PubMed] [Google Scholar]
- 13.Heithersay GS. Invasive cervical resorption: an analysis of potential predisposing factors. Quintessence Int 1999; 30: 83–95. [PubMed] [Google Scholar]
- 14.Bastos JV, Silva TA, Colosimo EAet al. Expression of inflammatory cytokines and chemokines in replanted permanent teeth with external root resorption. J Endod 2017; 43: 203–209. [DOI] [PubMed] [Google Scholar]
- 15.Ahuja R, Almuzian M, Khan Aet al. et al. A preliminary investigation of short-term cytokine expression in gingival crevicular fluid secondary to high-level orthodontic forces and the associated root resorption: case series analytical study. Prog Orthod 2017; 18: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hakami Z, Kitaura H, Kimura Ket al. Effect of interleukin-4 on orthodontic tooth movement and associated root resorption. Eur J Orthod 2015; 37: 87–94. [DOI] [PubMed] [Google Scholar]
- 17.Iglesias-Linares A, Hartsfield JK. Cellular and molecular pathways leading to external root resorption. J Dent Res 2017; 96: 145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trope M. Root resorption due to dental trauma. Endod Topics 2002; 1: 79–100. [Google Scholar]
- 19.Makedonas D, Lund H, Grondahl Ket al. et al. Root resorption diagnosed with cone beam computed tomography after 6 months of orthodontic treatment with fixed appliance and the relation to risk factors. Angle Orthodontist 2012; 82: 196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andreasen JO. Luxation of permanent teeth due to trauma. A clinical and radiographic follow-up study of 189 injured teeth. Scand J Dent Res 1970; 78: 273–286. [DOI] [PubMed] [Google Scholar]
- 21.Cohenca N, Simon JH, Mathur Aet al. et al. Clinical indications for digital imaging in dento-alveolar trauma. Part 2: root resorption. Dent Traumatol 2007; 23: 105–113. [DOI] [PubMed] [Google Scholar]
- 22.Patel S, Durack C, Abella Fet al. et al. European society of endodontology position statement: the use of CBCT in endodontics. Int Endod J 2014; 47: 502–504. [DOI] [PubMed] [Google Scholar]
- 23.Andreasen JO. External root resorption: its implications in dental traumatology, paedodontics, periodontics, orthodontics and endodontics. Int Endod J 1985; 18: 109–118. [DOI] [PubMed] [Google Scholar]
- 24.Gunraj MN. Dental root resorption. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 88: 647–653. [DOI] [PubMed] [Google Scholar]
- 25.Abbott P. Prevention and management of external inflammatory resorption following trauma to teeth. Aust Dent J 2016; 61: 82–94. [DOI] [PubMed] [Google Scholar]
- 26.Nayak MT, Nayak A. External inflammatory root resorption in mandibular first molar: a case report. Malays J Med Sci 2015; 22: 63–66. [PMC free article] [PubMed] [Google Scholar]
- 27.Patel S, Durack C, Ricucci D. Root resorption. In: Hargreaves KM, Berman LH. (eds) Pathways of the pulp. 11th edition. St Louis: Elsevier, 2016, pp. 660–683. [Google Scholar]
- 28.Santos JBD, Castillo JFM, Nishiyama CK, et al. External root resorption: diagnosis and treatment. Clinical case report. J Dent Health Oral Disord Ther 2018; 9: 160–164. [Google Scholar]
- 29.Trope M, Moshonov J, Nissan Ret al. et al. Short vs. Long-term calcium hydroxide treatment of established inflammatory root resorption in replanted dog teeth. Endod Dent Traumatol 1995; 11: 124–128. [DOI] [PubMed] [Google Scholar]
- 30.Trope M. Luxation injuries and external root resorption—etiology, treatment, and prognosis. J Calif Dent Assoc 2000; 28: 860–866. [PubMed] [Google Scholar]
- 31.Öktem ZB, Çetinbaş T, Özer Let al. et al. Treatment of aggressive external root resorption with calcium hydroxide medicaments: a case report. Dent Traumatol 2009; 25: 527–531. [DOI] [PubMed] [Google Scholar]
- 32.Malmgren B, Malmgren O, Andreasen JO. Alveolar bone development after decoronation of ankylosed teeth. Endod Topics 2006; 14: 35–40. [Google Scholar]
- 33.Cohenca N, Stabholz A. Decoronation – a conservative method to treat ankylosed teeth for preservation of alveolar ridge before permanent prosthetic reconstruction: literature review and case presentation. Dent Traumatol 2007; 23: 87–94. [DOI] [PubMed] [Google Scholar]
- 34.Malmgren B. Ridge preservation/decoronation. J Endod 2013; 39: S67–S72. [DOI] [PubMed] [Google Scholar]
- 35.Gunst V, Huybrechts B, De Almeida Neves Aet al. et al. Playing wind instruments as a potential aetiologic cofactor in external cervical resorption: two case reports. Int Endod J 2011; 44: 268–282. [DOI] [PubMed] [Google Scholar]
- 36.Patel S, Saberi N. External cervical resorption associated with the use of bisphosphonates: a case series. J Endod 2015; 41: 472–478. [DOI] [PubMed] [Google Scholar]
- 37.Jiang YH, Lin Y, Ge Jet al. et al. Multiple idiopathic cervical root resorptions: report of one case with 8 teeth involved successively. Int J Clin Exp Med 2014; 7: 1155–1159. [PMC free article] [PubMed] [Google Scholar]
- 38.Neely AL, Thumbigere-Math V, Somerman MJet al. et al. A familial pattern of multiple idiopathic cervical root resorption with a 30-year follow-up. J Periodontol 2016; 87: 426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mavridou AM, Hauben E, Wevers Met al. et al. Understanding external cervical resorption in vital teeth. J Endod 2016; 42: 1737–1751. [DOI] [PubMed] [Google Scholar]
- 40.Heithersay GS. Invasive cervical resorption. Endod Topics 2004; 7: 73–92. [Google Scholar]
- 41.Gunst V, Mavridou A, Huybrechts Bet al. et al. External cervical resorption: an analysis using cone beam and microfocus computed tomography and scanning electron microscopy. Int Endod J 2013; 46: 877–887. [DOI] [PubMed] [Google Scholar]
- 42.Lin YP, Love RM, Friedlander LTet al. et al. Expression of toll-like receptors 2 and 4 and the OPGRANKLRANK system in inflammatory external root resorption and external cervical resorption. Int Endod J 2013; 46: 971–981. [DOI] [PubMed] [Google Scholar]
- 43.Heithersay GS. Invasive cervical resorption following trauma. Aust Endod J 1999; 25: 79–85. [DOI] [PubMed] [Google Scholar]
- 44.Mavridou AM, Hauben E, Wevers Met al. et al. Understanding external cervical resorption patterns in endodontically treated teeth. Int Endod J 2017; 50: 1116–1133. [DOI] [PubMed] [Google Scholar]
- 45.Patel S, Kanagasingam S, Pitt Ford T. External cervical resorption: a review. J Endod 2009; 35: 616–625. [DOI] [PubMed] [Google Scholar]
- 46.Hartsfield JK., Jr.Pathway in external apical root resorption associated with orthodontia. Orthod Craniofac Res 2009; 12: 236–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nilsson E, Bonte E, Bayet Fet al. et al. Management of internal root resorption on permanent teeth. Int J Dent 2013Article ID 929486; 2013: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lopatiene K, Dumbravaite A. “Risk factors of root resorption after orthodontic treatment”. Stomatologija, Baltic Dental Maxillofacial J 2008; 10: 89–95. [PubMed] [Google Scholar]
- 49.Silveira FF, Nunes E, Soares JAet al. et al. Double ‘pink tooth’ associated with extensive internal root resorption after orthodontic treatment: a case report. Dent Traumatol 2009; 25: e43–e47. [DOI] [PubMed] [Google Scholar]
- 50.Fernandes M, de Ataide I, Wagle R. Tooth resorption part I-pathogenesis and case series of internal resorption. J Conserv Dent 2013; 16: 4–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thomas P, Krishna Pillai R, Pushparajan Ramakrishnan Bet al. et al. An insight into internal resorption. ISRN Dent 2014; 2014: 759326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Krishnan V, Davidovitch Z. Biological mechanisms of tooth movement. 2nd EdnOxford, UK: John Wiley and Sons, 2015, ISBN-13: 9781118688861, pp.312. [Google Scholar]
- 53.Bhaskar SN. Orban's oral histology and embryology. 10th ed. St Louis: C. V. Mosby, 1986, pp.206–208. [Google Scholar]
- 54.Patel S, Dawood A, Wilson Ret al. et al. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography — an in vivo investigation. Int Endod J 2009; 42: 831–838. [DOI] [PubMed] [Google Scholar]
- 55.Mittal S, Kumar T, Mittal Set al. et al. "Internal root resorption: an endodontic challenge: a case series”. J Conserv Dent 2014; 17: 590–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Koçkapan C, Wetzel WE. SEM Findings in osteoclasts and Howship's lacunae during the resorption of deciduous teeth. Dtsch Zahnarztl Z 1986; 41: 841–846. [PubMed] [Google Scholar]
- 57.Liao SC, Chang HP. The study of root resorption of human deciduous teeth. I. Histological observation by light microscope. Gaoxiong Yi Xue Ke Xue Za Zhi 1990; 6: 88–99. [PubMed] [Google Scholar]
- 58.Fuss Z, Tsesis I, Lin S. Root resorption-diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol 2003; 19: 175–182. [DOI] [PubMed] [Google Scholar]
- 59.Patel S, Ricucci D, Durak Cet al. et al. Internal root resorption: a review. J Endod 2010; 36: 1107–1121. [DOI] [PubMed] [Google Scholar]
- 60.Goske MJ, Applegate KE, Boylan J, et al. The image gently campaign: working together to change practice. The American Journal of Roentgenology 2008; 190: 273–274. [DOI] [PubMed] [Google Scholar]
- 61.Ustus R. Iatrogenic effects of orthodontic treatment. 1st EdnSwitzerland: Springer International Publishing, 2015; pp. 1–35. [Google Scholar]
- 62.Durack C, Patel S. Root resorption. In: Patel S, Harvey S, Shemesh H, Durack C. (eds) Cone beam computed tomography in endodontics. 1st edition. Berlin: Quintessence Publishing Co. Ltd, 2016, pp.119–131. [Google Scholar]
- 63.Bhuva B, Barnes JJ, Patel S. The use of limited cone beam computed tomography in the diagnosis and management of a case of perforating internal root resorption. Int Endod J 2011; 44: 777–786. [DOI] [PubMed] [Google Scholar]
- 64.Andreasen; J FM, Andreasen O. Diagnosis of luxation injuries: the importance of standardized clinical, radiographic and photographic techniques in clinical investigations. Endod Dent Traumatol 1985; 1: 160–169. [DOI] [PubMed] [Google Scholar]
- 65.Elbay ÜŞ, Baysal A, Elbay Met al. et al. Multidisciplinary approach to delayed treatment of traumatic teeth injuries involving extrusive luxation, avulsion and crown fracture. Oper Dent 2014; 39: 566–571. [DOI] [PubMed] [Google Scholar]
- 66.Kaval M, Güneri P, Çalışkan M. Regenerative endodontic treatment of perforated internal root resorption: a case report. Int Endod J 2018; 51: 128–137. [DOI] [PubMed] [Google Scholar]
- 67.Paryani K, Kim SG. Regenerative endodontic treatment of permanent teeth after completion of root development: a report of 2 cases. J Endod 2013; 39: 929–934. [DOI] [PubMed] [Google Scholar]
- 68.Chen MH, et al. Responses of immature permanent teeth with infected necrotic pulp tissue and apical periodontitis/abscess to revascularization procedures. Int Endod J 2012; 45: 294–305. [DOI] [PubMed] [Google Scholar]
- 69.Saoud TMA, et al. Regenerative endodontic procedures for traumatized teeth after horizontal root fracture, avulsion, and perforating root resorption. J Endod 2016; 42: 1476–1482. [DOI] [PubMed] [Google Scholar]
- 70.Tambakad PB, Naidu J. Pulp and periodontal regeneration of an avulsed permanent mature incisor using platelet-rich plasma after delayed replantation: a 12-month clinical case study. J Endod 2016; 42: 66–71. [DOI] [PubMed] [Google Scholar]
- 71.Ashraf A, Pérez Alfayate R. Regenerative endodontic treatment in teeth with internal root resorption: an insight over the available literature. International Journal of Scientific Research in Dental and Medical Sciences 2020; 2: 131–134. [Google Scholar]
- 72.Shetty H, et al. Three-dimensional semi-automated volumetric assessment of the pulp space of teeth following regenerative dental procedures. Sci Rep 2021; 11: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Karobari MI, et al. Root and canal morphology of the anterior permanent dentition in Malaysian population using two classification systems: a CBCT clinical study. Aust Endod J 2021; 47: 202–216. [DOI] [PubMed] [Google Scholar]
- 74.Arshad S, Tehreem F, Rehab Khan M, Ahmed F, Marya A, Karobari MI. Platelet-Rich Fibrin Used in Regenerative Endodontics and Dentistry: Current Uses, Limitations, and Future Recommendations for Application. Int J Dent. 2021 Dec 15;2021:4514598. doi: 10.1155/2021/4514598. PMID: 34956367; PMCID: PMC8695013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Andreasen FM. Transient apical breakdown and its relation to colour and sensibility changes after luxation injuries to teeth. Endod Dent Traumatol 1986; 2: 9–19. [DOI] [PubMed] [Google Scholar]
- 76.Makedonas DT. “Orthodontically induced root resorption: a clinical and radiographic survey”, University of Gothenburg. Sweden, 2012 [Thesis].
- 77.Tronstad L, Andreasen JO, Hasselgren Get al. et al. pH changes in dental tissues after root canal filling with calcium hydroxide. J Endod 1981; 7: 17–21. [DOI] [PubMed] [Google Scholar]
- 78.Lima TF, Neto JV, de Jesus Soares A. Diagnosis and management of root resorption in traumatized teeth: report of two cases. Eur J Gen Dent 2017; 6: 127–130. [Google Scholar]
- 79.Marques LS, Generoso R, Armond MCet al. et al. Short-root anomaly in an orthodontic patient. Am. J. Orthodontics Dentofacial Orthopedics 2010; 138: 346–348. [DOI] [PubMed] [Google Scholar]
- 80.Sharab LY, Morford LA, Dempsey J, et al. Genetic and treatment-related risk factors associated with external apical root resorption (EARR) concurrent with orthodontia. J. Orthodontics Craniofacial Res 2015; 18: 71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part I: the basic science aspects. Angle Orthod 2002; 72: 175–179. [DOI] [PubMed] [Google Scholar]
- 82.Levander E, Malmgren O, Stenback K. Apical root resorption during orthodontic treatment of patients with multiple aplasia: a study of maxillary incisors. Eur J Orthod 1998; 20: 427–434. [DOI] [PubMed] [Google Scholar]
- 83.Heboyan A, Avetisyan A, Markaryan M, et al. Tooth root resorption conditioned by orthodontic treatment. Oral Health Dental Sci 2019; 3: 1–8. [Google Scholar]
- 84.Le Norcy E, Lautrou A, Le Goff C. Facteurs affectant la résorption radiculaire associée aux traitements d’orthodontie. International Orthodontics 2005; 3: 129–140. [Google Scholar]
- 85.Sameshima GT, Sinclair PM. Predicting and preventing root resorption: part I. Diagnostic factors. Am J Orthod Dentofac Orthop 2001; 119: 505–510. [DOI] [PubMed] [Google Scholar]
- 86.Heboyan A, Syed AUY, Rokaya Det al. et al. Cytomorphometric analysis of inflammation dynamics in the periodontium following the use of fixed dental prostheses. Molecules 2020; 25: 4650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Avetisyan A, Markaryan M, Rokaya Det al. Characteristics of periodontal tissues in prosthetic treatment with fixed dental prostheses. Molecules 2021; 26: 1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Proffit WR, Fields HW, Sarver DM. Contemporary orthodontics. Mosby: Elsevier, 2007, pp. 331–358. [Google Scholar]
- 89.Estevez R, Aranguren J, Escorial Aet al. et al. Invasive cervical resorption class III in a maxillary central incisor: diagnosis and follow-up by means of cone-beam computed tomography. J Endod 2010; 36: 2012–2014. [DOI] [PubMed] [Google Scholar]
- 90.Heboyan AG, Avetisyan AA. Clinical case of root resorption due to improper orthodontic treatment. J Res Med Dent Sci 2019; 7: 91–93. [Google Scholar]
- 91.Şermet Elbay Ü, Elbay M, Kaya Eet al. et al. Management of an intruded tooth and adjacent tooth showing external resorption as a late complication of dental injury: three-year follow-up. Case Rep Dent 2015; 2015: 741687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Topkara A, Karaman AI, Kau CH. Apical root resorption caused by orthodontic forces: a brief review and a long-term observation. Eur J Dent 2012; 6: 445–453. [PMC free article] [PubMed] [Google Scholar]
- 93.Gabor C, Tam E, Shen Yet al. et al. Prevalence of internal inflammatory root resorption. J Endod 2012; 38: 24–27. [DOI] [PubMed] [Google Scholar]
- 94.Newton R, Hayes J. The association of external cervical resorption with modern internal bleaching protocols: what is the current evidence? Br Dent J 2020; 228: 333–337. [DOI] [PubMed] [Google Scholar]
- 95.Abbott P, Heah S. Internal bleaching of teeth: an analysis of 255 teeth. Aust Dent J 2009; 54: 326–333. [DOI] [PubMed] [Google Scholar]
- 96.Dahl JE, Pallesen U. Tooth bleaching—a critical review of the biological aspects. Crit Rev Oral Biol Med 2003; 14: 292–304. [DOI] [PubMed] [Google Scholar]
- 97.Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas of traumatic injuries to the teeth. 4th. Oxford, UK: Blackwell, 2007. [Google Scholar]
- 98.Raquel Gonçalves V-A, Clarissa Lopes D, Laura Pereira Azevedo Aet al. et al. Inflammatory root resorption in primary molars: prevalence and associated factors. Braz Oral Res 2012; 26: 335–340. [DOI] [PubMed] [Google Scholar]
- 99.Motokawa M, Terao A, Kaku Met al. et al. Open bite as a risk factor for orthodontic root resorption. Eur. J. Orthodontics 2013; 35: 790–795. [DOI] [PubMed] [Google Scholar]
- 100.Hussein Ali I, Ali Al-Turaihi B, Khidher Mohammed Let al. et al. Root resorption of teeth adjacent to untreated impacted maxillary canines: a CBCT study. BioMed Res Int 2021Article ID 6635575; 2021: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Owman-Moll P, Kurol J. Root resorption after orthodontic treatment in high- and low-risk patients: analysis of allergy as a possible predisposing factor. Eur J Orthod 2000; 22: 657–663. [DOI] [PubMed] [Google Scholar]
- 102.Ioi H, Kido MA, Murata N, et al. Effect of allergy on root resorption induced by orthodontic tooth movement. In: Bourzgui F. (ed) Issues in contemporary orthodontics. London: IntechOpen Limited, 2015; pp. 113–132. [Google Scholar]
- 103.Haugland L, Dahl Kristensen K, Atle Lie Set al. et al. The effect of biologic factors and adjunctive therapies on orthodontically induced inflammatory root resorption: a systematic review and meta-analysis. Eur J Orthod 2018; 40: 326–336. [DOI] [PubMed] [Google Scholar]
- 104.Consolaro A, Telma Regina Gobbi F, Laurindo Zanco F. Multiple or severe root resorptions are not associated with systemic factors, individual susceptibility, family tendency or individual predisposition. Dental Press J Orthod 2011; 16: 17–21. [Google Scholar]
- 105.Oberoi S, Knueppel S. Three-dimensional assessment of impacted canines and root resorption using cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 260–267. [DOI] [PubMed] [Google Scholar]
- 106.Yan B, Sun Z, Fields Het al. et al. Maxillary canine impaction increases root resorption risk of adjacent teeth: a problem of physical proximity. Am. J. Orthodontics Dentofacial Orthopedics 2012; 142: 750–757. [DOI] [PubMed] [Google Scholar]
- 107.Marques LS, Chaves KC, Rey ACet al. et al. Severe root resorption and orthodontic treatment: clinical implications after 25 years of follow-up. Am. J. Orthodontics Dentofacial Orthopedics 2011; 139: S166–S169. [DOI] [PubMed] [Google Scholar]
- 108.Esteves T, Ramos AL, Pereira CMet al. et al. Orthodontic root resorption of endodontically treated teeth. J Endod 2007; 33: 119–122. [DOI] [PubMed] [Google Scholar]
- 109.Aidos H, Diogo P, Santos JM. Root resorption classifications: a narrative review and a clinical aid proposal for routine assessment. Eur Endod J 2018; 3: 134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lund H, Grondahl K, Hansen Ket al. et al. Apical root resorption during orthodontic treatment. A prospective study using cone beam CT. Angle Orthodontist 2012; 82: 480–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Marques LS, Ramos-Jorge ML, Rey ACet al. et al. Severe root resorption in orthodontic patients treated with the edgewise method: prevalence and predictive factors. Am. J. Orthodontics Dentofacial Orthopedics 2010; 137: 384–388. [DOI] [PubMed] [Google Scholar]
- 112.Motokawa M, Sasamoto T, Kaku Met al. et al. Association between root resorption incident to orthodontic treatment and treatment factors. Eur. J. Orthodontics 2012; 34: 350–356. [DOI] [PubMed] [Google Scholar]
- 113.Pereira SA, Lopez M, Lavado Net al. et al. A clinical risk prediction model of orthodontic-induced external apical root resorption. Revista Portuguesa Estomatologia Medicina Dentaria Cirurgia Maxilofacial 2014; 55: 66–72. [Google Scholar]
- 114.Maues CPR, Nascimento RRD, Vilella ODV. Severe root resorption resulting from orthodontic treatment: prevalence and risk factors”. Dental Press J. Orthodontics 2015; 20: 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sehr K, Bock NC, Serbesis Cet al. et al. Severe external apical root resorption: local cause or genetic predisposition? J Orofac Orthop 2011; 72: 321–331. [DOI] [PubMed] [Google Scholar]
- 116.Al-Qawasmi RA, Hartsfield JK, Jr., Everett ETet al. et al. Genetic predisposition to external apical root resorption in orthodontic patients: linkage of chromosome-18 marker. J Dent Res 2003; 82: 356–360. [DOI] [PubMed] [Google Scholar]
- 117.Travess H. Orthodontics. Part 6: risks in orthodontic treatment. Br Dent J 2004; 196: 1–7. [DOI] [PubMed] [Google Scholar]
- 118.Tripuwabhrut P, Brudvik P, Fristad Iet al. et al. Experimental orthodontic tooth movement and extensive root resorption: periodontal and pulpal changes. Eur J Oral Sci 2010; 118: 596–603. [DOI] [PubMed] [Google Scholar]
- 119.Wahab RMA, Shafiai NAA, Ariffin SHZ. An insight into risk factors for root resorption during orthodontic treatment. J. Med. Sci 2017; 17: 1–9. [Google Scholar]
- 120.Wang Q, Chen W, Smales RJet al. et al. Apical root resorption in maxillary incisors when employing micro-implant and J-hook headgear anchorage: a 4-month radiographic study. J. Huazhong Univ. Sci. Technol. Med. Sci 2012; 32: 767–773. [DOI] [PubMed] [Google Scholar]
- 121.Villa PA, Oberti G, Moncada CAet al. et al. Pulpdentine complex changes and root resorption during intrusive orthodontic tooth movement in patients prescribed nabumetone. J Endod 2005; 31: 61–66. [DOI] [PubMed] [Google Scholar]
- 122.Baysala A, Karadedeb I, Hekimogluc Set al. et al. Evaluation of root resorption following rapid maxillary expansion using cone-beam computed tomography. Angle Orthod 2012; 82: 488–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Walker S. Root resorption during orthodontic treatment. Evid Based Dent 2010; 11: 88. [DOI] [PubMed] [Google Scholar]
- 124.Matsuda Y, Motokawa M, Kaku M, et al. Clinical survey of the association between root resorption incident to orthodontic treatment and host factors. Orthodontic Waves 2012; 71: 40. [DOI] [PubMed] [Google Scholar]
- 125.Yu L, He S, Chen S. Diagnostic accuracy of orthopantomogram and periapical film in evaluating root resorption associated with orthodontic force. Hua Xi Kou Qiang Yi Xue Za Zhi 2012; 30: 169–172. [PubMed] [Google Scholar]
- 126.Heboyan AG, Avetisyan AA, Margaryan MM, et al. Rare clinical case of tooth root external resorption as a delayed post-traumatic complication. The New Armenian Medical Journal 2018; 12: 93–98. [Google Scholar]
- 127.Mah J, Prasad N. Dentine phosphoproteins in gingival crevicular fluid during root resorption. Eur. J. Orthodontics 2004; 26: 25–30. [DOI] [PubMed] [Google Scholar]
- 128.Ramos SP, Ortolan GO, Santos LMDet al. et al. Anti-dentine antibodies with root resorption during orthodontic treatment. Eur. J. Orthodontics 2011; 33: 584–591. [DOI] [PubMed] [Google Scholar]
- 129.Ariffin SHZ, Yamamoto Z, Abidin LZZet al. et al. Cellular and molecular changes in orthodontic tooth movement. Sci. World J 2011; 11: 1788–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.George A, Evans CA. Detection of root resorption using dentin and bone markers. J. Orthodontics Craniofacial Res 2009; 12: 229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Heboyan AG, Avetisyan AA. Comparative assessment of periodontal complex by experimental method and elaboration of new protocols for corresponding treatment of external and perforating internal resorption resulted many years after trauma. Biomed Res 2019; 30: 693–696. [Google Scholar]
- 132.Heboyan AG, Manrikyan ME, Markaryan MMet al. et al. Changes in the parameters of gingival crevicular fluid in masticatory function restoration by various prosthodontic constructions. Int J Pharm Sci Res 2020; 12: 2088–2093. [Google Scholar]
- 133.Heboyan A, Manrikyan M, Zafar MSet al. Bacteriological evaluation of gingival crevicular fluid in teeth restored using fixed dental prostheses: an in vivo study. Int. J. Mol. Sci 2021; 22: 5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Shaa H, Bai Y. Comparison between electrochemical ELISA and spectrophotometric ELISA for the detection of dentine sialophosphoprotein for root resorption. Am J Orthod Dentofacial Orthop 2014; 145: 36–40. [DOI] [PubMed] [Google Scholar]
- 135.Rody WJ, Jr, Shannon Holliday L. Mass spectrometry analysis of gingival crevicular fluid in the presence of external root resorption. Am J Orthod Dentofacial Orthop 2014; 145: 787–798. [DOI] [PubMed] [Google Scholar]
- 136.Kereshanan S, Stephenson P, Waddington R. Identification of dentine sialoprotein in gingival crevicular fluid during physiological root resorption and orthodontic tooth movement. Eur. J. Orthodontics 2008; 30: 307–314. [DOI] [PubMed] [Google Scholar]
- 137.Berkovitz BKB, Moxham BJ, Linden RWAet al. et al. Master dentistry volume 3: oral biology. 3rd EdnLondon, UK: Elsevier, ISBN: 9780702044588, 2011, pp.312. [Google Scholar]
- 138.Loubele M, Bogaerts R, van Dijck E, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol 2009; 71: 461–468. [DOI] [PubMed] [Google Scholar]
- 139.European Commission. Radiation Protection No. 172. “Cone Beam CT for Dental and Maxillofacial Radiology, Evidence Based Guidelines”, Luxembourg: Directorate-General for Energy Directorate D—Nuclear Energy Unit D4—Radiation Protection, 2012.
- 140.Patel S, Foschi F, Mannocci Fet al. et al. External cervical resorption: a three-dimensional classification. Int Endod J 2017; 51: 206–214. [DOI] [PubMed] [Google Scholar]
- 141.Trope M. Root resorption of dental and traumatic origin: classification based on etiology. Pract Periodont Aesthet Dent 1998; 10: 515–522. [PubMed] [Google Scholar]