Abstract
Background/aims
Quantity of cataract surgery has long been an important public health indicator to assess health accessibility, however the quality of care has been less investigated. We aimed to summarise the up-to-date evidences to assess the real-world visual outcomes after cataract surgery in different settings.
Methods
A systematic review was undertaken in October 2021. Population-based cross-sectional and longitudinal studies reporting vision-related outcomes after cataract surgery published from 2006 onward were included. A meta-analysis was not planned.
Results
Twenty-six cross-sectional studies from low-income and middle-income countries (LMICs) and five cross-sectional studies from high-income countries (HICs) were included. The proportions of participants with postoperative presenting visual acuity (VA) ≥0.32 (20/60) were all over 70% in all HICS studies, but mostly below 70% in LMICS studies, ranging from 29.9% to 80.5%. Significant difference in postoperative VA was also observed within countries. The leading causes for postoperative visual impairment (defined mostly as presenting VA <20/60) mainly included refractive error, ocular comorbidities and surgical complications including posterior capsule opacification, except for one study in Nigeria wherein the leading cause was aphakia. Only four population-based cohort studies were included with 5–20 years of follow-up time, generally demonstrating no significant changes in postoperative visual outcomes during the follow-up.
Conclusions
We observed large inequality in the visual outcomes and principal causes of visual impairment after cataract surgery among different countries and regions. Structured quality control and enhancement programmes are needed to improve the outcomes of cataract surgery and reduce inequality.
Keywords: lens and zonules
Key questions.
What is already known on this topic?
Cataract remains the leading cause of global blindness. The quantity of cataract surgery keeps increasing in recent decades, but the quality of cataract surgery could vary remarkably.
What this study adds?
Based on a systematic review of all population-based studies reporting vision-related outcomes after cataract surgery published in the past 15 years, we identified substantial differences in the type of cataract surgery, postoperative vision as well as causes for postoperative visual impairment within and among different countries and regions. The reported postoperative visual outcomes were generally less ideal compared with the WHO recommendation, especially in low-income and middle-income countries. There is a paucity of population-based data from many countries worldwide, and also scarce data from long-term cohorts.
How this study might affect research, practice or policy?
More attention should be paid to understand and improve the quality of cataract surgery and minimise global inequality in the contemporary era.
Introduction
Cataract surgery is the most commonly performed elective surgery worldwide, with more than 20 million surgeries performed annually.1 2 According to the latest Global Burden of Disease study, cataract remains the leading cause of global blindness, meanwhile increasing numbers of cataract surgery are being performed to reduce the ‘backlog’ of cataract blindness in the ageing society.3–5 The cataract surgical rate, which represents the number of surgeries performed per million population in a given year, is the most important public health parameter to assess accessibility to cataract service.6 In parallel with several important advances that have taken place during the last decades, including the micro-incision cataract surgical technique, newer generations of intraocular lens (IOL) and IOL calculation formulas, more attention is being paid to maximise the benefit that patient could achieve through cataract surgery.7
In addition to accessibility, the quality of care plays a critical role towards universal health coverage.8 Despite being proved as one of the most cost-effective health interventions, cataract surgery can be associated with poor visual outcomes due to surgical complications, ocular comorbidities or inadequate optical correction despite the use of an IOL.9 10 The postoperative visual acuity (VA) is a simple direct parameter which could reflect the quality of cataract surgery and postsurgical care to a large extent. The Global Initiative for the Elimination of Avoidable Blindness indicates that cataract surgical services should have a high success rate in terms of VA and improved quality of life.11 Therefore, understanding the nowaday visual outcomes of cataract surgery in the real world is crucial in formulating future strategies on the cataract management, providing important reference for both ophthalmologists and decision-makers.
Both the quantity and quality of cataract surgery vary markedly among different countries and even within countries due to differences in socioeconomic status, availability of medical resources and clinical practice patterns.12 13 The purpose of this review was to summarise the visual status of participants after cataract surgery based on representative population-based studies in both high-income countries (HICs) and low-income and middle-income countries (LMICs), as well as the main cause for visual impairment (VI) after cataract surgery.
Methods
The protocol of this systematic review was prospectively registered at PROSPERO (CRD42021292087). The reporting of this systematic review is based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 checklist.
Eligibility criteria for considering studies for this review
We included population-based studies reporting vision-related outcomes after cataract surgery. Only full-text original studies published in English were included. Unpublished studies and meeting abstracts were not included due to uncertainty of methodological quality. Studies evaluating cataract surgical outcomes other than VA were further excluded.
Search methods for identifying studies
Two researchers (XH and JZ) independently searched PubMed, Embase and Google Scholar from 1 January 2006 to 15 November 2021. The keywords included ‘cataract surgery’, ‘cataract extraction’, ‘population-based’, ‘outcome’, ‘visual acuity’ and ‘vision’. Detailed search terms could be found in the online supplemental appendix 1. Reference lists in published articles were also reviewed.
bjophthalmol-2021-320997supp001.pdf (30.7KB, pdf)
Study selection
To identify relevant studies, retrieved articles were exported to Endnote (V.X9, Clarivate Analytics). After removing duplicates from the initial search, the titles and abstracts of the articles were screened by JZ and XH, independently. Full-text screening was performed subsequently to further exclude articles that did not meet the inclusion criteria. In case of discrepancies, the results were conferred with a third investigator (ZL). For periodical cross-sectional studies, such as the China Nine-Province Survey, the report with larger sample size and published more recently was selected.
Data collection and risk of bias assessment
Data were extracted and entered into an Excel spreadsheet (Microsoft, Redmond, Washington, USA) with predetermined headings including first author, year of publication, study design, country, number of participants, age, gender, examination time, type of cataract surgery, postoperative presenting VA (PVA), postoperative best-corrected VA (BCVA), causes of postoperative VI and so on. For cohort studies which included multiple follow-up visits, the examination time, number of participants, type of cataract surgery, postoperative PVA and BCVA and causes of postoperative VI were recorded separately for each study visit.
We assessed the quality of evidence using the Newcastle-Ottawa Scale (NOS) and adapted NOS for cohort and cross-sectional studies, respectively.14 This tool evaluated three bias domains, including selection, comparability and outcome. Two investigators (JZ and XH) independently assessed the risk of bias, and discrepancies were resolved through discussion (tables 1–3; online supplemental table 1).
Table 1.
Visual outcomes of cataract surgery in population-based cross-sectional studies in low-income and middle-income countries
| First author | Year | Region | Participants | Age (years) | Gender (F/M) | Patients/eyes* | Examination time | Type of cataract surgery | Duration since cataract surgery | Postoperative PVA | Postoperative BCVA | Causes of visual impairment |
| Bourne et al 16 | 2007 | Pakistan | 16 507 | ≥30 | 8766/7741 | 1317/1788 | 2002–2003 | ICCE: 61.0% ECCE: 34.0% |
≤3 years:49.1% 4–8 years: 31.3% ≥9 years: 19.6% |
≤6/12: 15.4% <6/12–6/18: 14.1% <6/18–6/60: 35.3% <6/60–3/60: 4.80% <3/60: 29.5% |
≤6/12: 31.5% <6/12–6/18: 18.6% <6/18–6/60: 27.5% <6/60–3/60: 3.40% <3/60: 18.7% |
Def: PVA ≤6/12 RE: 53.4% Comorbidities: 23.5% Complications: 21.4% |
| Lindfield et al 17 | 2008 | Satkhira District, Bangladesh |
3503 | ≥50 | 1834/1669 | 170/213 | 2005 | – | >5 years: 42.3% <5 years: 57.7% |
≥6/18: 60.1% <6/18–6/60: 16.4% <6/60: 23.5% |
≥6/18: 67.6% <6/18-6/60: 12.2% <6/60: 20.2% |
Def: VA <6/18 Comorbidities: 33.8% Complications: 30.6% RE: 25.8% PCO: 9.70% |
| Salomão et al 19 | 2009 | São Paulo, Brazil | 3642 | ≥50 | 2115/1527 | 231/357 | 2004–2005 | Phaco: 45.4% ECCE: 50.4% ICCE: 3.90% |
>10 years: 22.1% 5–10 years: 25.5% ≤5 years: 52.4% |
>20/40: 41.2% ≤20/40–20/63: 28.1% <20/63–20/200: 14.2% <20/200–20/400: 6.30% <20/400: 10.2% |
>20/40: 61.9% ≤20/40–20/63: 17.6% <20/63–20/200: 8.20% <20/200–20/400: 5.10% <20/400: 7.10% |
Def: PVA <20/63 Comorbidities: 68.8% RE: 16.5% PCO: 4.60% |
| Murthy et al 18 | 2009 | Gujarat, India | 4738 | ≥50 | 2585/2153 | 834/1299 | 2007 | ICCE: 6.60% ECCE: 8.60% ECCE+IOL: 16.8% Phaco+IOL: 12.2% MSICS+IOL: 55.1% |
≥10 years: 17.5% 6–10 years: 15.7% 3–5 years: 35.3% ≤2 years: 30.8% |
≥20/32: 18.7% 20/40–20/63: 32.0% <20/63–20/200: 31.3% <20/200–20/400: 2.50% <20/400: 15.5% |
≥20/32: 55.7% <20/40–20/63: 18.8% <20/63–20/200: 14.5% <20/200–20/400: 1.20% <20/400: 9.80% |
Def: PVA <20/40 RE: 45.5% Comorbidities: 26.9% PCO: 16.5% |
| Kandel et al 21 | 2010 | Nepal | 5138 | ≥50 | 2701/2437 | 359/485 | 2006 | ICCE/ECCE | ≥3 years: 59.0% | ≥6/18: 61.4% | ≥6/18: 84.7% | Def: PVA <6/18 RE: 54.2% Comorbidities: 22.0% PCO: 8.00% |
| Vijaya et al 20 | 2010 | South India | 9600 | ≥40 | – | 934/1385 | 2003 | – | >3 years: 41.8% <3 years: 57.8% |
20/20: 6.20% 20/25–20/60: 47.5% <20/60: 45.3% <20/200: 21.1% <20/400: 16.8% |
20/20: 19.7% 20/25–20/60: 57.9% <20/60: 21.4% <20/200: 12.4% <20/400: 9.70% |
Def: PVA <20/60 RE: 52.5% Comorbidities: 30.2% PCO: 7.90% |
| Imam et al 25 | 2011 | Nigeria | 13 591 | ≥40 | 6560/7031 | 217/288 | 2005–2007 | – | – | ≥6/18: 29.9% <6/18–6/60: 26% <6/60: 44.1% |
≥6/18: 55.9% <6/18–6/60: 20.8% <6/60: 23.3% |
Def: PVA <6/18 Aphakia: 38.6% Comorbidities: 24.4% Complications: 18.8% RE: 10.9% PCO: 3.00% |
| Nangia et al 24 | 2011 | Rural Central India | 4711 | ≥30 | – | 234/318 | 2006 | – | – | ≥6/12: 25.0% <6/12–6/18: 12.0% <6/18–6/60: 52.0% <6/60: 11.0% |
≥6/12: 53.0% <6/12–6/18: 10.0% <6/18–6/60: 26.0% <6/60: 10.0% |
Def: PVA <6/18 RE: 41.8% Comorbidities:14.9% PCO: 13.9% Complications: 12.4% |
| Thapa et al 23 | 2011 | Bhaktapur District, Nepal | 4003 | ≥40 | – | 151/226 | 2001 | – | ≥5 years: 58.9% <5 years: 41.1% |
≥6/18: 54.4% <6/18–6/6: 34.5% <6/60: 11.1% |
≥6/18: 72.6% <6/18–6/60: 19.0% <6/60: 8.40% |
Def: BCVA <6/18 Comorbidities: 54.8% Complications: 27.4% PCO: 14.5% |
| Brian et al 22 | 2011 | Fiji | 1381 | ≥40 | – | 88/113 | 2009 | ICCE: 14.3% ECCE: 85.7% |
– | *ECCE eyes ≥6/18: 56.6% <6/60: 19.7% NLP: 2.60% |
– | – |
| Khanna et al 27 | 2012 | Andhra Pradesh, India | 7281 | ≥50 | – | 1124/1548 | 2009 | – | >10 years: 6.30% 5–10 years: 30.1% <5 years: 63.6% |
<6/18: 31.8% | <6/18: 19.3% | Def: PVA <6/18 RE: 38.8% Comorbidities: 30.3% Complications: 15.9% Aphakia: 15.0% |
| Odugbo et al 26 | 2012 | Plateau State, Nigeria |
4115 | ≥50 | 2176/1939 | 119/180 | 2007 | – | >5 years: 45.0% <5 years: 55.0% |
≥6/18: 25.6% <6/18–6/60: 16.1% <6/60: 58.3% |
– | Def: PVA <6/60 Aphakia: 65.1% Comorbidities: 20.9% Complications: 14.0% |
| Li et al 28 | 2013 | Hainan, South China | 6482 | ≥50 | 3471/3011 | -/524 | 2010 | – | – | >6/18: 59.4% <6/18–6/60: 20.0% <6/60: 20.6% |
– | Def: PVA <6/18 Comorbidities: 35.4% RE: 32.5% Complications: 32.0% |
| Li et al 30 | 2014 | Heilongjiang, North China | 10 384 | 1–94 | – | 21/21 | 2008–2009 | ICCE/ECCE | <5 years: 66.0% <10 years: 81.0% |
≥20/60: 57.1% <20/400–20/60: 19.1% <20/400: 23.8% |
≥20/60: 81.0% | Def: PVA <20/60 RE: 33.0% Complications: 25.0% Comorbidities: 17.0% PCO: 8.00% |
| Katibeh et al 29 | 2014 | Varamin Iran | 2819 | ≥50 | – | 341/526 | 2009 | – | – | ≥6/18: 71.9% <6/18-6/60: 13.5% <6/60: 14.6% |
– | Def: PVA <6/18 Comorbidities: 42.6% Complications: 33.8% RE: 25.0% |
| Mörchen et al 31 | 2015 | Takeo Province, Cambodia | 4471 | ≥50 | 2933/1538 | -/372 | 2011–2012 | – | ≤5 years: 33.3% >5 years: 66.7% |
≥6/18: 69.9% <6/18–6/60: 16.9% <6/60: 13.2% |
– | Def: PVA <6/60 Comorbidities: 62.5% Complications: 12.5% RE: 6.30% |
| Pawiroredjo et al 32 | 2016 | Suriname | 2998 | ≥50 | – | 1003/1003 | 2013–2014 | – | 3 years: 51.3% 4–6 years: 20.7% >7 years: 27.9% |
≥6/18: 80.5% <6/18–6/60: 9.80% <6/60: 9.80% |
– | Def: PVA <6/60 Comorbidities: 52.0% RE: 30.0% Complications: 11.0% |
| Marmamula et al 34 | 2016 | South Indian State of Andhra Pradesh |
7378 | ≥40 | 3957/3421 | 870/1228 | 2011–2012 | – | <5 years: 65% 6–10 years: 23.3% >10 years: 11.7% |
≥6/18: 74.6% <6/18–6/60: 12.5% <6/60: 13.0% |
– | Def: PVA <6/18 Comorbidities: 30.5% RE: 28.7% Complications: 21.1% Aphakia: 18.4% |
| Paul et al 33 | 2016 | South India | 5530 | ≥50 | – | 749/1112 | 2010 | MICS: 74.7% ECCE: 12.5% ICCE: 8.50% Phaco: 2.90% |
1–2 years: 26.5% 3 years: 18.0% 4–10 years: 44.3% >10 years: 11.1% |
≥6/18: 53.1% <6/18–6/60: 38.1% <6/60: 8.80% |
– | Def: PVA <6/18 RE: 44.6% Comorbidities: 27.2% PCO: 14.2% Complications: 3.64% |
| Zhang et al 35 | 2017 | Chaonan, Guangdong, Southern China | 3484 | ≥50 | 2087/1397 | 155/211 | 2012 | – | – | ≥6/18: 67.2% <6/18–6/60: 16.1% <6/60–3/60: 4.30% <3/60: 12.3% |
– | Def: PVA <6/18 Comorbidities: 42.0% Complications: 33.3% RE: 24.6% |
| Zhang et al 37 | 2018 | Hohhot, North China | 3985 | ≥50 | 2281/1704 | 131/189 | 2014 | – | – | ≥6/12: 58.7% <6/12–6/18: 14.8% <6/18–6/60: 11.1% <6/60: 15.4% |
– | – |
| Thoufeeq et al 36 | 2018 | Maldives | 3020 | ≥50 | 1787/1233 | 850/850 | 2014 | – | – | ≥6/18: 67.9% <6/18–6/60: 17.3% <6/60: 14.8% |
≥6/18: 76.6% <6/18–6/60: 10.0% <6/60: 13.4% |
– |
| Zhao et al 40 | 2018 | China | 51 310 | ≥50 | 29065/22245 | 2100/2877 | 2014 | – | – | ≥20/32: 32.4% <20/40–20/63: 29.9% <20/63–20/200: 20.6% <20/200: 17.2% |
≥20/32: 54.7% <20/40–20/63: 20.5% <20/63–20/200: 11.7% <20/200: 13.1% |
– |
| Jiachu et al 39 | 2019 | Tibetan, China | 4764 | ≥50 | 2677/2087 | 364/364 | 2017 | – | ≤3 years: 42.3% 4–6 years: 28.3% ≥7 years: 29.4% |
– | ≥6/12: 47.5% <6/18–6/12: 11.8% <6/10–6/18: 14.6% <6/60: 26.1% |
Def: PVA <6/18 Comorbidities: 51.3% Complications: 34.8% RE: 6.10% |
| Watanabe et al 38 | 2019 | Parintins, Brazil | 2041 | ≥45 | 1041/1000 | 176/275 | 2014–2015 | Phaco: 62.9% ECCE: 35.3% Unclear: 1.80% |
– | ≥20/32: 44.4% <20/40–20/63: 20.8% <20/63–20/200:14.4% <20/200–20/400: 2.60% <20/400: 17.8% |
≥20/32: 59.2% <20/40–20/63: 13.0% <20/63–20/200:10.4% <20/200–20/400: 1.50% <20/400: 15.9% |
Def: PVA <20/32 Comorbidities: 34.8% Complications: 33.3% RE: 26.6% |
| Shen et al 41 | 2020 | Southwestern (Yunan), China | 6546 | ≥50 | 3943/2603 | 395/525 | 2010 | – | ≤10 years: 84.0% >10 years: 14.3% |
≥20/32: 15.2% <20/40–20/63: 29.3% <20/63–20/200: 30.9% <20/200: 24.6% |
≥20/32: 24.6% <20/40–20/63: 37.3% <20/63–20/200: 29.9% <20/200: 14.9% |
Def: PVA/BCVA<20/63 Comorbidities: 50.8% PCO: 25.1% RE: 22.7% |
*Participants or eyes that received cataract surgery.
BCVA, best-corrected visual acuity; Def, definition of visual impairment; ECCE, extracapsular cataract extraction; ICCE, intracapsular cataract extraction; IOL, intraocular lens; MSICS, manual small incision cataract surgery; PCO, posterior capsule opacification; Phaco, phacoemulsification; PVA, presenting visual acuity; RE, refractive error.
Table 2.
Outcomes of cataract surgery in population-based cross-sectional studies in high-income countries
| First author | Year | Region | Participants | Age (years) |
Gender (F/M) |
Patients/eyes* | Examination time | Duration since cataract surgery | Postoperative PVA | Postoperative BCVA | Causes of visual impairment |
| Barañano et al 42 | 2008 | California | 6357 | ≥40 | 3687/2670 | 261/422 | 2000–2003 | – | >20/40:51.9% ≤20/40–20/63:22.8% ≤20/80–20/160: 9.00% ≤20/200: 16.4% |
>20/40: 67.8% ≤20/40–20/63: 13.5% ≤20/80–20/160: 6.20% ≤20/200: 12.6% |
Def: PVA <20/40 comorbidities: 50.7% RE: 33.0% PCO: 7.40% |
| Lavanya et al 45 | 2009 | Singapore | 3266 | 40–80 | 1657/1568 | 438/592 | 2004–2006 | – | ≤20/60: 26.8% | ≤20/60: 10.8% | Def: PVA ≤20/60 RE: 59.5% Comorbidities: 33.6% PCO: 6.00% |
| Gupta et al 43 | 2013 | Singapore | 3388 | ≥40 | – | 486/795 | 2007–2009 | – | ≤20/60: 25.5% | ≤20/60: 10.9% | Def: PVA ≤20/60 RE: 57.1% Comorbidities: 31.6% PCO: 7.90% |
| Keel et al 44 | 2018 | Australia | 4836 | ≥40 | – | 773/1333 | 2015–2016 | 47.6%: ≤3 years 43.7%: >3 years |
≥6/12: 77.6% <6/12–6/60: 19.7% <6/60: 2.63% |
– | Def: PVA <6/12 Comorbidities: 50.0% RE: 37.6% surgery Complications: 0.30% |
| Owen et al 46 | 2021 | USA | 68 526 828 | – | – | 1 824 196/3 648 392 | 2019–2020 | Within 90 days | ≥20/20: 28.8% | ≥20/20: 83.0% | – |
*Participants or eyes received cataract surgery.
BCVA, best-corrected visual acuity; Def, definition of visual impairment; IOL, intraocular lens; PCO, posterior capsule opacification; PVA, presenting visual acuity; RE, refractive error.
Table 3.
Outcomes of cataract surgery in population-based cohort studies
| Cohort | Study location | Baseline year | Participants | Age (years) | Gender (F/M) |
Examination time | Patients/eyes* | Type of cataract surgery | Duration since cataract surgery | Postoperative PVA | Postoperative BCVA | Causes of visual impairment |
| The Beijing Eye Study47 | Beijing, China | 2001 | 4378 | ≥40 | 2458/1920 | 2006 (5 years) |
92/133 | – | ≤3 years: 42.1% >3 years: 57.9% |
≥6/12: 72.9% <6/12–6/18: 6.80% <6/18–6/60: 13.5% <6/60: 6.80% |
≥6/12: 88.0% <6/12–6/18: 1.50% <6/18–6/60: 8.30% <6/60: 2.30% |
Def: PVA <6/18 RE: 50.0% Comorbidities: 38.3% PCO: 7.70% |
| The Blue Mountains Eye Study49 |
Sydney, Australia | 1992–1994 | 3654 | ≥49 | 2072/1582 | 1997–1999 (5 years) |
– | – | – | <6/12: 26.0% | <6/12: 8.60% | Def: PVA <6/12 RE: 66.7% Comorbidities: 9.10% |
| 2002–2004 (10 years) |
90/130 | – | – | <6/12: 23.0% | <6/12: 9.20% | Def: PVA <6/12 RE: 59.3% PCO: 18.5% Comorbidities: 14.8% |
||||||
| The Liwan Eye study48 | Guangzhou, China | 2003–2004 | 1405 | ≥50 | – | 2003–2004 | 62/90 | Phaco: 54.4% ECCE: 44.4% ICCE: 1.2% |
>10 years: 16.7% ≤10 years: 83.3% |
*PVA with pinhole ≥6/18: 62.2% <6/18–6/60:22.2% <6/60–3/60: 3.3% <3/60: 12.2% |
≥6/18: 75.6% <6/18–6/60:13.3% <6/60–3/60: 2.20% <3/60: 8.90% |
Def: PVA <6/18 Comorbidities: 50.0% Uncorrected aphakia: 20.6% RE: 14.7% PCO: 14.7% |
| 2009 (5 years) |
44/62 | Phaco: 100% | – | ≥6/18: 59.7% <6/18–6/60: 17.7% <6/60–3/60: 14.5% <3/60: 8.06% |
≥6/18: 80.6% <6/18–6/60: 9.68% <6/60–3/60: 8.06% <3/60: 1.61% |
Def: PVA ≤6/18 RE: 42.8% Comorbidities: 35.7% PCO: 7.10% |
||||||
| Sweden cohort50–53 | Sweden | 1997–1998 | 863 | ≥30 | 578/312 | 2002–2003 (5 years) |
810/810 | Phaco: 97.9 | – | – | ≤20/40: 16.4% | – |
| 2007–2008 (10 years) |
289/- | Phaco: 100% | – | – | ≥20/30: 65.0% 20/40–20/32: 11.0% 20/42–20/80: 9.0% 20/100–20/200: 5.00% <20/200: 9.00% |
– | ||||||
| 2012–2013 (15 years) |
168/168 | Phaco: 100% | – | – | ≥20/30: 71.0% 20/40–20/32: 10.0% 20/42–20/80: 6.00% 20/100–20/200: 5.00% <20/200: 8.00% |
– | ||||||
| 2017–2018 (20 years) |
114/- | Phaco: 100% | – | – | Median: 20/63 | – |
*Participants or eyes received cataract surgery.
BCVA, best-corrected visual acuity; Def, definition of visual impairment; ECCE, extracapsular cataract extraction; ICCE, intracapsular cataract extraction; PCO, posterior capsule opacification; Phaco, phacoemulsification; PVA, presenting visual acuity; RE, refractive error.;
bjophthalmol-2021-320997supp002.pdf (73.1KB, pdf)
Data synthesis and analysis
Categorising each study site into LMICs or HICs was based on the World Bank list of economies.15 The VA representation format varied among the included studies, and equivalent Snellen decimal VA was presented to facilitate direct comparison and understanding.
Given the aim of this review was to present and compare visual outcomes of cataract surgery, findings were reported narratively and meta-analysis was not planned. Ethical approval was not required for this study.
Results
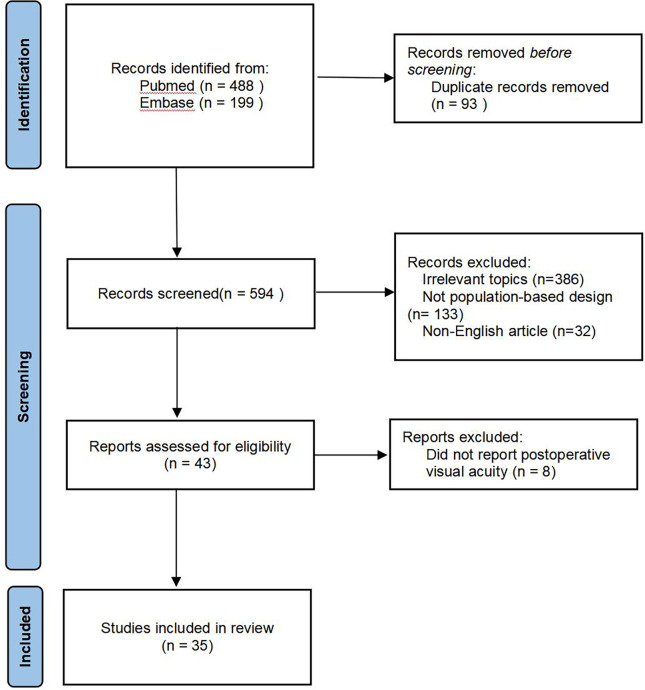
We identified 687 studies after a systematic literature review. After checking for duplicates and eligibility criteria, 652 studies were further excluded, including 93 duplicates, 386 studies due to irrelevant topics, 133 studies without population-based design and 32 studies written in language other than English. Forty-three full-text articles were screened, and eight studies were further excluded due to a lack of data on postoperative VA status. No study was excluded based on further quality appraisal. As a result, this review included 35 population-based studies which reported the visual outcome of cataract surgery (figure 1).
Figure 1.
Flow diagram.
The included studies differed with respect to the study type, country, year as well as the definition and categorisation of postoperative VA and VI. A total of 31 population-based cross-sectional studies were included, among which 26 (83.87%) were conducted in LMICs,16–41 and only 5 (16.13%) were conducted in HICs (tables 1 and 2).42–46 An additional four population-based cohort studies were identified, including two from China,47 48 one from Australia49 and one from Sweden50–53 (table 3). Notably, the American Academy of Ophthalmology Intelligent Research In Sight (IRIS) study46 was classified as a cross-sectional study in this review, given that it only reported the VA at one visit within 90 days after cataract surgery. All included studies displayed no significant bias.
In assessing the postoperative VA outcomes, most available studies included middle-aged and elderly population and reported the proportion of participants with PVA and BCVA in different VA subgroups (mostly including the ≥0.32 group). Table 1 demonstrates the detailed visual outcomes of cataract surgery for each study in time sequence. Of the 26 population-based cross-sectional studies in LMICs, half were from China (n=7)28 30 35 37 39–41 and India (n=6).18 20 24 27 33 34 Six studies in China included subjects aged ≥50 years with sample size ranging from 3484 to 51 310, and the proportions of participants with postoperative PVA ≥0.32 (recorded as 6/18 or 20/60 or 20/63) ranged from 44.5% (Shen et al 2020 Southwestern China)41 to 73.5% (Zhang et al 2018 Northern China).37 The proportions of participants with postoperative BCVA ≥0.32 ranged from 59.3% (Jiachu et al 2019 Tibetan China)39 to 81.0% (Li et al 2014 Northern China).30 Postoperative VI was mostly defined as PVA <0.32, ocular comorbidities were the leading cause of postoperative VI. The other study in Heilongjiang, Northern China (2014)30 included 10 384 participants aged 1–94 years and only 21 received cataract surgery (intracapsular cataract extraction [ICCE]/extracapsular cataract extraction [ECCE]). In this study, 57.1% participants achieved postoperative PVA ≥20/60 (0.32) and 81.0% with BCVA ≥20/60 (0.32), the main cause for postoperative VI was refractive error (RE) (33.0%). All the six studies in India included adult subjects (≥30 years) with sample size ranging from 4711 to 9600. Two studies18 33 reported the distribution of cataract surgery types, with manual small-incision cataract surgery as the most commonly performed (55.1% and 74.7%), followed by ECCE and phacoemulsification. The proportions of participants with postoperative PVA ≥0.32 (recorded as 6/18 or 20/60 or 20/63) ranged from 37.0% (Nangia et al 2011, Rural Central India)24 to 74.6% (Marmamula et al 2016, Southern India)34 and the proportions with postoperative BCVA ≥0.32 ranged from 63.0% (Nangia et al 2011, Rural Central India)24 to 80.7% (Khanna et al 2012, Southeast India).27 RE is the leading cause of postoperative VI (PVA <0.32), one exception is that ocular comorbidities was the leading cause in the study by Marmamula et al (2016).34
We identified two studies in Brazil. Salomão et al (2009)19 included 3642 participants aged ≥50 years, 231 (357 eyes) patients had received cataract surgery, including 50.4% ECCE, 45.4% phacoemulsification and 3.9% ICCE. Watanabe et al (2019)38 included 2041 participants aged ≥45 years, 176 (275 eyes) patients had received cataract surgery, including 35.3% ECCE, 62.9% phacoemulsification and 1.8% unclear. Proportions of participants with postoperative PVA of ≥20/32 (0.625), <20/40 (0.5) to 20/63 (0.32), <20/63 (0.32) to 20/200 (0.1), <20/200 (0.1) to 20/400 (0.05) and <20/400 (0.05) were 41.2%, 28.1%, 14.2%, 6.3%, 10.2% and 44.4%, 20.8%, 14.4%, 2.6%, 17.8%, respectively. The corresponding numbers for postoperative BCVA were 61.9%, 17.6%, 8.2%, 5.10%, 7.10% and 59.2%, 13.0%, 10.4%, 1.50%, 15.9%, respectively. Postoperative VI was defined as PVA <0.32 and ocular comorbidities was the leading cause of VI in both studies. Two studies were identified in Nepal. Kandel et al (2010)21 included 5138 subjects aged ≥50 years, among whom 359 (485 eyes) participants had received ICCE or ECCE. They reported that 61.4% and 84.7% study participants achieved a postoperative PVA and BCVA ≥6/18 (0.32), respectively. Thapa et al 23 included 4003 subjects aged ≥40 years, among whom 151 (226 eyes) participants had received cataract surgery (type not reported). The corresponding proportions of participants with postoperative PVA and BCVA ≥6/18 (0.32) were 54.4% and 72.6%, respectively. Postoperative VI was also defined as PVA <6/18 (0.32) and RE was the leading cause in Kandel et al 21, and ocular comorbidities was the main cause in Thapa et al.23 Of the two studies conducted in Nigeria, Imam et al 25 included 13 591 subjects aged ≥40 years and only 217 (288 eyes) participants had received cataract surgery. The proportions of participants with postoperative PVA of ≥6/18 (0.32), <6/18 (0.32) to 6/60 (0.1) and <6/60 (0.1) were 29.9%, 26% and 44.1%, the corresponding numbers for postoperative BCVA were 55.9%, 20.8% and 23.3%, respectively. In contrast to other studies, the leading cause of postoperative VI (PVA <0.32) was uncorrected aphakia (38.6%), followed by comorbidities (24.4%) and complications (18.8%). Odugbo et al 26 included 4115 subjects aged ≥50 years in Nigeria, they also identified a low rate of cataract surgery (119/4115) and poor surgical outcomes (postoperative PVA ≥0.32: 25.6%). Aphakia (65.1%) and comorbidities (20.9%) were also the first two causes for postoperative VI.
Only one population-based cross-sectional study was identified for the following regions. Bourne et al 16 included 16 507 subjects aged ≥30 years in Pakistan, 1317 (1788 eyes) participants had received cataract surgery (61.0% ICCE, 34.0% ECCE). The proportion of participants with postoperative PVA and BCVA of ≥6/18 (0.32), <6/18 (0.32) to 6/60 (0.1) and <6/60 (0.1) was 29.5%, 35.3%, 34.3% and 50.1%, 27.5%, 22.1%, respectively. The top three leading causes of postoperative VI included RE (53.4%), ocular comorbidities (23.5%) and complications (21.4%). Lindfield et al 17 included 3503 subjects aged ≥50 years in Bangladesh, 170 (213 eyes) participants had received cataract surgery. The proportion of participants with postoperative PVA and BCVA of ≥6/18 (0.32), <6/18 (0.32) to 6/60 (0.1) and <6/60 (0.1) was 60.1%, 16.4%, 23.5% and 67.6%, 12.2%, 20.2%, respectively. The top three leading cause of postoperative VI in this study were comorbidities (33.8%), complications (30.6%) and RE (25.8%). Brian et al 22 included 1381 subjects aged ≥40 year in Fiji, 88 (113 eyes) participants had received cataract surgery and among the ECCE eyes, 56.6% achieved postoperative PVA ≥6/18 (0.32) and 19.7% were <6/60 (0.1). Katibeh et al 29 included 2819 subjects aged ≥50 years in Iran, 341 (526 eyes) participants had received cataract surgery. About 71.9% of the study participants achieved postoperative PVA ≥6/18 (0.32), and the major reasons for not achieving this VA criteria included comorbidities (42.6%), complications (33.8%) and RE (25.0%). Morchen et al 31 included 4471 subjects aged ≥50 years in Cambodia, cataract surgery was performed in 372 eyes. The proportion of participants with postoperative PVA of ≥6/18 (0.32), <6/18 (0.32) to 6/60 (0.1) and <6/60 (0.1) was 69.9%, 16.9%, 13.2%, respectively. Postoperative VI was defined as PVA <6/60 (0.1) in this study, and the three leading causes were comorbidities (62.5%), complications (12.5%) and RE (6.3%). Pawiroredjo et al (2016)32 included 2998 participants aged ≥50 years in Suriname, and reported a relatively high cataract surgical coverage (1003/2998) and good surgical outcome (postoperative PVA ≥0.32: 80.5%). Postoperative VI was also defined as PVA <6/60 (0.1) in this study, and the three leading causes were comorbidities (52.0%), RE (30.0%) and complications (11.0%). Thoufeeq et al 36 included 3020 subjects aged ≥50 years in Maldives, 850 (850 eyes) participants had received cataract surgery. The proportion of participants with postoperative PVA and BCVA of ≥6/18 (0.32), <6/18 (0.32) to 6/60 (0.1) and <6/60 (0.1) was 67.9%, 17.3%, 14.8% and 76.6%, 10%, 13.4%, respectively. Causes for postoperative VI were not reported.
Only five population-based cross-sectional studies in HICs were identified. Barañano et al 42 included 6357 participants aged ≥40 years during 2000–2003 in California, 261 (422 eyes) participants had received cataract surgery and the proportion of participants with postoperative PVA and BCVA of >20/40 (0.5), <20/40 (0.5) to 20/63 (0.32), <20/80 (0.25) to 20/160 (0.125) and <20/200 (0.1) was 51.9%, 22.8%, 9.00%, 16.4% and 67.8%, 13.5%, 6.20%, 12.6%, respectively (table 2). Postoperative VI was defined as PVA <20/40 (0.5), and the top three reasons for VI included ocular comorbidities (50.7%), RE (33.0%) and posterior capsule opacification (PCO) (7.40%). Two studies were conducted in Singapore which included participants aged 40 years and above. The study by Lavanya et al 45 was conducted during 2004 and 2006, 438 (592 eyes) patients of 3266 participants received cataract surgery, and there were 26.8% of participants with postoperative PVA ≤6/18 (0.32) and 10.8% with BCVA ≤6/18 (0.32). The study by Gupta et al 43 was conducted during 2007–2009, 486 (795 eyes) patients of 3388 participants received cataract surgery, and there were 25.5% of participants with postoperative PVA ≤20/60 (0.32) and 10.9% with BCVA ≤20/60 (0.32). The study by Keel et al 44 was from the Australian National Eye Health Survey which included 4836 participants during 2015–2016. Of the 773 (1333 eyes) patients who received cataract surgery, 77.6% achieved postoperative PVA ≥6/12 (0.5), 19.7% with PVA between 6/60 (0.1) and 6/12 (0.5) and 2.63% were <6/60 (0.1). In the two Singapore studies, postoperative VI was defined as PVA <0.32, nearly 60% of VI was due to RE, followed by comorbidities and PCO. In the other two studies, PVA was defined as PVA <0.5, and the leading cause was comorbidities (50% in Australia), followed by RE and surgical complications. The most recent study by Owen et al 46 was from the IRIS study which included over 1.8 million patients who underwent bilateral cataract surgery. There were 28.8% of eyes achieved postoperative PVA ≥20/20 (1.0) with no information regarding other status of PVA nor the cause of VI.
Four cohort studies were identified with a follow-up period ranging from 5 years to 20 years (table 3). The Beijing Eye Study47 is a population-based cohort study which included 4378 participants aged ≥40 years at baseline in 2001. The cataract surgical outcome was not assessed at baseline, while at the 5-year follow-up, 92 (133 eyes) participants had received cataract surgery among whom 42.1% received cataract surgery in the last 3 years. The proportion of participants with postoperative PVA and BCVA of >6/12 (0.5), <6/12 (0.5) to 6/18 (0.32), <6/18 (0.32) to 6/60 (0.1) and <6/60 (0.1) was 72.9%, 6.80%, 13.5%, 6.80% and 88%, 1.50%, 8.30%, 2.30%, respectively. Fifty percent of postoperative VI (PVA <6/18) was attributed to RE, 38.3% to comorbidities and 7.7% to PCO. The Blue Mountain Eye Study,49 which included 3654 participants aged ≥49 years during 1992–1994, reported the cataract surgical outcomes at 5-year and 10-year follow-up. The proportion of participants with postoperative PVA and BCVA <6/12 (0.5) were similar at 5 (26% and 8.6%) and 10 (23% and 9.2%) years. Sixty percent of the postoperative VI was due to RE at both follow-ups. The Liwan Eye Study48 included 1405 participants aged ≥50 years at baseline during 2003–2004, 62 (90 eyes) participants had received cataract surgery including 54.4% with phacoemulsification, 44.4% with ECCE and 1.2% with ICCE. Postoperative PVA (measured with pin-hole) was ≥6/18 (0.32) in 62.2% and BCVA was ≥6/18 (0.32) in 75.6% of the study population. During the 5-year follow-up, 44 of 62 participants received phacoemulsification, the proportion of participants with pin-hole PVA and BCVA of ≥6/18 (0.32) was 59.7% and 80.6%, respectively. The leading cause of postoperative VI was ocular comorbidities at baseline and RE at 5-year follow-up in the Liwan Eye Study. Eva Monestam included 890 participants during 1997–1998 in Sweden and followed up for 20 years.50–53 Phacoemulsification was the dominate type of cataract surgery (97.9% at 5-year follow-up and 100% afterwards). The proportion of participants with postoperative BCVA >20/40 (0.5) at 5-year, 10-year and 15-year follow-up was 83.6%, 76% and 81%, respectively. At the 20-year follow-up, only a median postoperative BCVA of 20/63 was reported.
Discussion
With the continuous global effort leading to increasing cataract surgical volume in recent decades, equal attention must be paid to ensure the cataract surgical quality and adequate postoperative care.5 6 Based on this systematic review, we found that there was a lack of population-based data on the post-cataract surgery VA outcomes in many countries, and existing evidence demonstrated substantial difference in the cataract surgery type, postoperative VA status as well as principle causes for postoperative VI among different countries and regions.
The majority of the identified population-based studies in this review were cross-sectional studies from LMICs, especially China and India. Cohort studies were scarce, as well as studies from HICs and many other LMICs. Understanding the long-term VA outcome after cataract surgery is of great value considering 20–40 years of life ahead after the surgery for most patients.54 In addition, the VA prognosis for different types of IOLs was not addressed in existing population-based studies, perhaps due to a paucity of cases. With the increasing popularity in the use of newer IOLs, including the toric IOL and presbyopia-correcting IOL,55 56 more data and prolonged observations from across the world are needed to better understand the visual outcomes of cataract surgery in the modern society for global strategic planning.
We observed significant difference in the postoperative VA between LMICs and HICs. The proportions of patients with postsurgical VA ≥0.32 were mostly below 70%, varying significantly among different LMICs (29.9% in Nigeria to 80.5% in Suriname) and even within the same LMIC country (37%–74.6% in India). In contrast, the proportions of patients with postsurgical VA ≥0.32 were all above 70% in HICs. The fact that only half of the cataract surgeries resulted in a PVA of 6/18 or better in many LMICs is of great concern. Referring to the WHO recommendation of an uncorrected VA of ≥20/60 (0.32) in at least 80% of operated eyes,57 we still have a long way to go in achieving this goal in the real world, especially for LMICs.
Postoperative VI was mostly defined as a PVA <0.32 (<0.5 in some studies) and with varying principal causes in different studies. In the four studies from HICs, ocular comorbidities (California and Australia) and RE (both Singapore studies) were the leading causes of postoperative VI. In most LMICs, the most common causes of postoperative VI included ocular comorbidities, RE and surgical complications including the development of PCO. Sight-threatening ocular comorbidities, including glaucoma, age-related macular degeneration, diabetic retinopathy, can cause inadequate visual outcomes after the cataract surgery. A thorough preoperative examination could differentiate VI due to cataract from other causes, helping better informed surgical decision and more reasonable surgical outcome expectations.58 RE is found to be another leading cause of postoperative VI, suggesting the lack of appropriate refractive spectacles for a large proportion of patients after cataract surgery. To address this issue, greater attention should also be paid to ensure that the IOL implant is of appropriate power. The newer generations of the IOL formulas, including the Kane and Barrett Universal II formula, have been reported to be able to predict the postoperative RE with high accuracy and stability.59 Adequate postoperative follow-up and timely prescription of spectacles in need are important to ensure the fulfilment of VA potential for each patient. It should also be noted that in the two studies from Nigeria, the leading cause for postoperative VI was aphakia, suggesting a high unmet need for IOL implantation in this region. Despite being easily treatable with a yttrium-aluminum-garnet-laser capsulotomy, PCO caused 3%–25% of the postoperative VI in existing studies, which suggested poor adherence to necessary postoperative follow-ups. For the vision-restoring potential of cataract surgery to be fully realised, the importance of regular postoperative follow-up care must be emphasised to all patients.
Apparently, quality control and enhancement are needed to improve the outcomes of cataract surgeries. This is important not only in better patient prognosis but also in further increasing the receipt of cataract surgeries in the population. Standard cataract surgical training for young ophthalmologists and strict quality-control system would be helpful in ensuring the quality of the surgery itself. More evidence-based studies or guidelines regarding the choice of IOL and structured postoperative follow-up management will also help in minimising the risk of correctable VI after the surgery. Previously reported barriers to cataract service were mostly related to poor accessibility, including lack of transport, low awareness, high cost and less family support.60 61 Numerous global and regional action plans and campaigns have been taken to reduce these barriers, while factors that contribute to unideal VA outcomes, including inadequate preoperative examination for surgical plan, poor postoperative VA monitoring and lost to follow-up, are often neglected in the real world. Actions to integrate and coordinate the continuous medical care for postoperative patients, development of standardised follow-up process and financial support for the patients and health institutions should be implemented. The significant inequality in cataract surgical outcome between HICs and LMICs also warrants global attention and audit, as the worse VA outcomes can further lead to lower productivity and higher socioeconomic burden.2 13
Conclusion
We provided a comprehensive and systematic review of visual outcomes after cataract surgery based on population-based studies worldwide during the previous 15 years. The reported visual outcomes were less ideal based on the WHO recommendation criteria, especially in LMICs. Significant inequalities in cataract surgery quality were observed within and among different countries and regions, which call for regional and global actions to tackle this problem.
Footnotes
Contributors: XH, JZ and LL had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. XH and JZ were responsible for the concept and design. Acquisition, analysis and interpretation of data were done by all authors. Drafting of the manuscript was done by XH and JZ. Critical revision of the manuscript for important intellectual content was done by all the authors. LL was responsible for securing of funding. Administrative, technical or material support was provided by ZL and LL. Supervision was done by LL. All authors approved the final version. The cooresponding author LL is responsible for the overall content as the guarantor.
Funding: This study was supported by the Construction Project of High-Level Hospitals in Guangdong Province (303020102); National Natural Science Foundation of China (81770905). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. Richard L. Thoughts on cataract surgery. Review of ophthalmology, 2015. Available: https://www.reviewofophthalmology.com/article/thoughts-on-cataract-surgery-2015
- 2. Wang W, Yan W, Müller A, et al. A global view on output and outcomes of cataract surgery with national indices of socioeconomic development. Invest Ophthalmol Vis Sci 2017;58:3669–76. 10.1167/iovs.17-21489 [DOI] [PubMed] [Google Scholar]
- 3. Aggarwal S, Jain P, Jain A. COVID-19 and cataract surgery backlog in Medicare beneficiaries. J Cataract Refract Surg 2020;46:1530–3. 10.1097/j.jcrs.0000000000000337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. GBD 2019 Blindness and Vision Impairment Collaborators, Vision Loss Expert Group of the Global Burden of Disease Study . Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to vision 2020: the right to sight: an analysis for the global burden of disease study. Lancet Glob Health 2021;9:e144–60. 10.1016/S2214-109X(20)30489-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Blindness GBD, Vision Impairment C. Vision loss expert group of the global burden of disease S. trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the global burden of disease study. Lancet Glob Health 2021;9:e130–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang W, Yan W, Fotis K, et al. Cataract surgical rate and socioeconomics: a global study. Invest Ophthalmol Vis Sci 2016;57:5872–81. 10.1167/iovs.16-19894 [DOI] [PubMed] [Google Scholar]
- 7. Limburg H, Ramke J. Cataract indicators: their development and use over the last 30 years. Community Eye Health 2017;30:82–4. [PMC free article] [PubMed] [Google Scholar]
- 8. Greer SL, Méndez CA. Universal health coverage: a political struggle and governance challenge. Am J Public Health 2015;105 Suppl 5:S637–9. 10.2105/AJPH.2015.302733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology 2007;114:1670–8. 10.1016/j.ophtha.2006.12.013 [DOI] [PubMed] [Google Scholar]
- 10. Pershing S, Henderson VW, Goldstein MK, et al. Cataract surgery complexity and surgical complication rates among Medicare beneficiaries with and without dementia. Am J Ophthalmol 2021;221:27–38. 10.1016/j.ajo.2020.08.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ackland P. The accomplishments of the global initiative vision 2020: the right to sight and the focus for the next 8 years of the campaign. Indian J Ophthalmol 2012;60:380–6. 10.4103/0301-4738.100531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zijlmans BL, van Zijderveld R, Manzulli M, et al. Global multi-site, prospective analysis of cataract surgery outcomes following ICHOM standards: the European CAT-Community. Graefes Arch Clin Exp Ophthalmol 2021;259:1897–905. 10.1007/s00417-021-05181-5 [DOI] [PubMed] [Google Scholar]
- 13. Yan W, Wang W, van Wijngaarden P, et al. Longitudinal changes in global cataract surgery rate inequality and associations with socioeconomic indices. Clin Exp Ophthalmol 2019;47:453–60. 10.1111/ceo.13430 [DOI] [PubMed] [Google Scholar]
- 14. Wells G, Shea B, O’Connell D. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Accessed 10 Mar 2022].
- 15. The World Bank . World bank list of economies, 2020. Available: https://databank.worldbank.org/data/download/site-content/CLASS.xls [Accessed 10 Mar 2022].
- 16. Bourne R, Dineen B, Jadoon Z, et al. Outcomes of cataract surgery in Pakistan: results from the Pakistan national blindness and visual impairment survey. Br J Ophthalmol 2007;91:420–6. 10.1136/bjo.2006.106724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lindfield R, Polack S, Wadud Z, et al. Causes of poor outcome after cataract surgery in Satkhira district, Bangladesh. Eye 2008;22:1054–6. 10.1038/sj.eye.6702836 [DOI] [PubMed] [Google Scholar]
- 18. Murthy GVS, Vashist P, John N, et al. Prevalence and vision-related outcomes of cataract surgery in Gujarat, India. Ophthalmic Epidemiol 2009;16:400–9. 10.3109/09286580903315809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Salomão SR, Soares FS, Berezovsky A, et al. Prevalence and outcomes of cataract surgery in Brazil: the São Paulo eye study. Am J Ophthalmol 2009;148:199–206. 10.1016/j.ajo.2009.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vijaya L, George R, Rashima A, et al. Outcomes of cataract surgery in a rural and urban South Indian population. Indian J Ophthalmol 2010;58:223–8. 10.4103/0301-4738.62648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kandel RP, Sapkota YD, Sherchan A, et al. Cataract surgical outcome and predictors of outcome in Lumbini zone and Chitwan district of Nepal. Ophthalmic Epidemiol 2010;17:276–81. 10.3109/09286586.2010.508355 [DOI] [PubMed] [Google Scholar]
- 22. Brian G, Ramke J, Szetu J, et al. Cataract and its surgery in Fiji. Clin Exp Ophthalmol 2011;39:449–55. 10.1111/j.1442-9071.2010.02477.x [DOI] [PubMed] [Google Scholar]
- 23. Thapa SS, Khanal S, Paudyal I, et al. Outcomes of cataract surgery: a population-based developing world study in the Bhaktapur district, Nepal. Clin Exp Ophthalmol 2011;39:851–7. 10.1111/j.1442-9071.2011.02576.x [DOI] [PubMed] [Google Scholar]
- 24. Nangia V, Jonas JB, Gupta R, et al. Prevalence of cataract surgery and postoperative visual outcome in rural central India central India eye and medical study. J Cataract Refract Surg 2011;37:1932–8. 10.1016/j.jcrs.2011.08.020 [DOI] [PubMed] [Google Scholar]
- 25. Imam AU, Gilbert CE, Sivasubramaniam S, et al. Outcome of cataract surgery in Nigeria: visual acuity, autorefraction, and optimal intraocular lens powers--results from the Nigeria national survey. Ophthalmology 2011;118:719–24. 10.1016/j.ophtha.2010.08.025 [DOI] [PubMed] [Google Scholar]
- 26. Odugbo OP, Mpyet CD, Chiroma MR, et al. Cataract blindness, surgical coverage, outcome, and barriers to uptake of cataract services in plateau state, Nigeria. Middle East Afr J Ophthalmol 2012;19:282–8. 10.4103/0974-9233.97925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Khanna RC, Pallerla SR, Eeda SS, et al. Population based outcomes of cataract surgery in three tribal areas of Andhra Pradesh, India: risk factors for poor outcomes. PLoS One 2012;7:e35701. 10.1371/journal.pone.0035701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Li EY, Liu Y, Zhan X, et al. Prevalence of blindness and outcomes of cataract surgery in Hainan Province in South China. Ophthalmology 2013;120:2176–83. 10.1016/j.ophtha.2013.04.003 [DOI] [PubMed] [Google Scholar]
- 29. Katibeh M, Ziaei H, Rajavi Z, et al. Profile of cataract surgery in Varamin Iran: a population-based study. Clin Exp Ophthalmol 2014;42:354–9. 10.1111/ceo.12185 [DOI] [PubMed] [Google Scholar]
- 30. Li Z, Song Z, Wu S, et al. Outcomes and barriers to uptake of cataract surgery in rural Northern China: the Heilongjiang eye study. Ophthalmic Epidemiol 2014;21:161–8. 10.3109/09286586.2014.903499 [DOI] [PubMed] [Google Scholar]
- 31. Mörchen M, Langdon T, Ormsby GM, et al. Prevalence of blindness and cataract surgical outcomes in Takeo Province, Cambodia. Asia Pac J Ophthalmol 2015;4:25–31. 10.1097/APO.0000000000000061 [DOI] [PubMed] [Google Scholar]
- 32. Pawiroredjo JC, Minderhoud J, Mans DRA, et al. The cataract situation in Suriname: an effective intervention programme to increase the cataract surgical rate in a developing country. Br J Ophthalmol 2017;101:89–93. 10.1136/bjophthalmol-2016-308659 [DOI] [PubMed] [Google Scholar]
- 33. Paul P, Kuriakose T, John J, et al. Prevalence and visual outcomes of cataract surgery in rural South India: a cross-sectional study. Ophthalmic Epidemiol 2016;23:309–15. 10.1080/09286586.2016.1212991 [DOI] [PubMed] [Google Scholar]
- 34. Marmamula S, Khanna RC, Shekhar K, et al. Outcomes of cataract surgery in urban and rural population in the South Indian state of Andhra Pradesh: rapid assessment of visual impairment (RAVI) project. PLoS One 2016;11:e0167708. 10.1371/journal.pone.0167708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang X, Li EY, Leung CK-S, et al. Prevalence of visual impairment and outcomes of cataract surgery in Chaonan, South China. PLoS One 2017;12:e0180769. 10.1371/journal.pone.0180769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Thoufeeq U, Das T, Limburg H, et al. First rapid assessment of avoidable blindness survey in the Maldives: prevalence and causes of blindness and cataract surgery. Asia Pac J Ophthalmol 2018;7:316–20. 10.22608/APO.2017332 [DOI] [PubMed] [Google Scholar]
- 37. Zhang G, Tham Y-C, Gong H, et al. Blindness, low vision and cataract surgery outcome among adults in Hohhot of inner Mongolia: a rapid assessment of avoidable blindness (RAAB) study. Br J Ophthalmol 2018;102:1653–7. 10.1136/bjophthalmol-2017-311633 [DOI] [PubMed] [Google Scholar]
- 38. Watanabe SES, Berezovsky A, Furtado JM, et al. Population-Based cataract surgery complications and their impact on visual status in the Brazilian Amazon region. Am J Ophthalmol 2019;208:295–304. 10.1016/j.ajo.2019.07.017 [DOI] [PubMed] [Google Scholar]
- 39. Jiachu D, Jin L, Jiang F, et al. Prevalence and service assessment of cataract in Tibetan areas of Sichuan Province, China: population-based study. BMJ Open 2019;9:e031337. 10.1136/bmjopen-2019-031337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhao J, Xu X, Ellwein LB, et al. Cataract surgical coverage and visual acuity outcomes in rural China in 2014 and comparisons with the 2006 China Nine-Province survey. Am J Ophthalmol 2018;193:62–70. 10.1016/j.ajo.2018.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shen W, Cun Q, Zhong H, et al. Ethnic variation in prevalence, self-reported barriers and outcome of cataract surgery in a rural population in southwestern China: the Yunnan minority eye study. BMC Public Health 2020;20:893. 10.1186/s12889-020-09009-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Barañano AE, Wu J, Mazhar K, et al. Visual acuity outcomes after cataract extraction in adult Latinos. The Los Angeles Latino eye study. Ophthalmology 2008;115:815–21. 10.1016/j.ophtha.2007.05.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gupta P, Zheng Y, Ting TW, et al. Prevalence of cataract surgery and visual outcomes in Indian immigrants in Singapore: the Singapore Indian eye study. PLoS One 2013;8:e75584. 10.1371/journal.pone.0075584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Keel S, Xie J, Foreman J, et al. Population-Based assessment of visual acuity outcomes following cataract surgery in Australia: the National eye health survey. Br J Ophthalmol 2018;102:1419–24. 10.1136/bjophthalmol-2017-311257 [DOI] [PubMed] [Google Scholar]
- 45. Lavanya R, Wong TY, Aung T, et al. Prevalence of cataract surgery and post-surgical visual outcomes in an urban Asian population: the Singapore Malay eye study. Br J Ophthalmol 2009;93:299–304. 10.1136/bjo.2008.148650 [DOI] [PubMed] [Google Scholar]
- 46. Owen JP, Blazes M, Lacy M, et al. Refractive outcomes after immediate sequential vs delayed sequential bilateral cataract surgery. JAMA Ophthalmol 2021;139:876–85. 10.1001/jamaophthalmol.2021.2032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Liu B, Xu L, Wang YX, et al. Prevalence of cataract surgery and postoperative visual outcome in greater Beijing: the Beijing eye study. Ophthalmology 2009;116:1322–31. 10.1016/j.ophtha.2009.01.030 [DOI] [PubMed] [Google Scholar]
- 48. Huang W, Zheng Y, Wang L, et al. Five-Year incidence and postoperative visual outcome of cataract surgery in urban southern China: the Liwan eye study. Invest Ophthalmol Vis Sci 2012;53:7936–42. 10.1167/iovs.12-10903 [DOI] [PubMed] [Google Scholar]
- 49. Kanthan GL, Mitchell P, Burlutsky G, et al. Intermediate- and longer-term visual outcomes after cataract surgery: the blue Mountains eye study. Clin Exp Ophthalmol 2011;39:201–6. 10.1111/j.1442-9071.2010.02440.x [DOI] [PubMed] [Google Scholar]
- 50. Lundqvist B, Mönestam E. Gender-Related differences in cataract surgery outcome: a 5-year follow-up. Acta Ophthalmol 2008;86:543–8. 10.1111/j.1600-0420.2007.01099.x [DOI] [PubMed] [Google Scholar]
- 51. Mönestam EI, Lundqvist B. Extended long-term outcomes of cataract surgery. Acta Ophthalmol 2012;90:651–6. 10.1111/j.1755-3768.2011.02138.x [DOI] [PubMed] [Google Scholar]
- 52. Mönestam E. Long-Term outcomes of cataract surgery: 15-year results of a prospective study. J Cataract Refract Surg 2016;42:19–26. 10.1016/j.jcrs.2015.07.040 [DOI] [PubMed] [Google Scholar]
- 53. Mönestam E. Long-Term outcome of cataract surgery: 20-year results from a population-based prospective study. J Cataract Refract Surg 2019;45:1732–7. 10.1016/j.jcrs.2019.07.026 [DOI] [PubMed] [Google Scholar]
- 54. Fene F, Ríos-Blancas MJ, Lachaud J, et al. Life expectancy, death, and disability in Haiti, 1990-2017: a systematic analysis from the global burden of disease study 2017. Rev Panam Salud Publica 2020;44:e136:1. 10.26633/RPSP.2020.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Negishi K, Hayashi K, Kamiya K, et al. Nationwide prospective cohort study on cataract surgery with multifocal intraocular lens implantation in Japan. Am J Ophthalmol 2019;208:133–44. 10.1016/j.ajo.2019.07.019 [DOI] [PubMed] [Google Scholar]
- 56. Kanclerz P, Toto F, Grzybowski A, et al. Extended Depth-of-Field intraocular lenses: an update. Asia Pac J Ophthalmol 2020;9:194–202. 10.1097/APO.0000000000000296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Cockburn N, Steven D, Lecuona K, et al. Prevalence, causes and socio-economic determinants of vision loss in Cape town, South Africa. PLoS One 2012;7:e30718. 10.1371/journal.pone.0030718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Sudhalkar A, Vasavada V, Bhojwani D, et al. Incorporating optical coherence tomography in the cataract preoperative armamentarium: additional need or additional burden? Am J Ophthalmol 2019;198:209–14. 10.1016/j.ajo.2018.10.025 [DOI] [PubMed] [Google Scholar]
- 59. Connell BJ, Kane JX. Comparison of the Kane formula with existing formulas for intraocular lens power selection. BMJ Open Ophthalmol 2019;4:e000251. 10.1136/bmjophth-2018-000251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Aboobaker S, Courtright P. Barriers to cataract surgery in Africa: a systematic review. Middle East Afr J Ophthalmol 2016;23:145–9. 10.4103/0974-9233.164615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lewallen S, Courtright P. Recognising and reducing barriers to cataract surgery. Community Eye Health 2000;13:20–1. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjophthalmol-2021-320997supp001.pdf (30.7KB, pdf)
bjophthalmol-2021-320997supp002.pdf (73.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.