Abstract
Purpose
Asthma is a common chronic inflammatory respiratory tract disease with high morbidity and mortality. The global trends in asthma burden remain poorly understood, and asthma incidence has increased during the worldwide coronavirus disease 2019 (COVID-19) pandemic. This study aimed to provide a comprehensive view of the global distribution of asthma burden and its attributable risk factors from 1990 to 2019.
Methods
Based on the Global Burden of Disease Study 2019 Database, asthma incidence, deaths, disability-adjusted life years (DALYs), the corresponding age-standardized incidence rate (ASIR), age-standardized death rate (ASDR), age-standardized DALY rate, and estimated annual percentage change were analyzed according to age, sex, sociodemographic index (SDI) quintiles, and locations. Risk factors contributing to asthma deaths and DALYs were also investigated.
Results
Globally, the asthma incidence increased by 15%, but deaths and DALYs decreased. The corresponding ASIR, ASDR, and age-standardized DALY rate also decreased. The high SDI region had the highest ASIR, and the low SDI region had the highest ASDR. The ASDR and age-standardized DALY rate were negatively correlated with the SDI. The low-middle SDI region, particularly South Asia, showed the highest asthma-related deaths and DALYs. The incidence peak was under 9 years old, and more than 70% of all deaths occurred in the population over 60 years old. Smoking, occupational asthmagens, and a high body mass index were the main risk factors for asthma-related mortality and DALYs, and their distributions varied between sexes.
Conclusions
Globally, the asthma incidence has increased since 1990. The greatest asthma burden is borne by the low-middle SDI region. The 2 groups that need special attention are those under 9 years old and those over 60 years old. Targeted strategies are needed to reduce the asthma burden based on geographic and sex-age characteristics. Our findings also provide a platform for further investigation into the asthma burden in the era of COVID-19.
Keywords: Asthma, global burden of disease, risk factors, incidence, death, disability-adjusted life years
INTRODUCTION
Asthma is a common chronic airway disease which is characterized by variable airflow obstriction, airway hypersensitivity, airway wall thickening, and increased mucus hypersecretion. It is a heterogeneous disease with several different clinical manifestations, which varies in the exacerbation rate, response to treatment, and remission rate.1 Asthma attack is characterized by an acute exacerbation of asthma symptoms due to exposure to allergens, viral infections, environmental irritants (including pollution and cigarette smoke), or a combination of these factors. Asthma is a major worldwide public health problem with high morbidity and mortality,2 affecting an estimated 339 million people worldwide. The asthma prevalence varies widely across countries at different levels of development, up to 21-fold among 70 countries.3 The asthma prevalence in the United States (US) is higher than the world average: an estimated 8.4% of the US population has asthma, while 4.3% of the world’s population is affected.4 However, the asthma prevalence continues to rise both in the US and worldwide.5
As the number of asthma cases increases each year, so do the economic costs as confirmed by data from studies of asthma in the US.6 Asthma brought an obvious economic burden, costing 81.9 billion dollars in 2013 including costs caused by absenteeism and death. This figure likely undervalues the current financial cost of asthma treatment, as the number of prescriptions for novel and expensive medications targeting biological pathways is rising.7 From 2008 to 2018, the cost of asthma continued to rise, and this trend indicated that the economic burden of asthma continued to increase. The prevention and treatment of asthma are not perfect,8,9,10 and the burden of asthma deserves our attention.
In the current worldwide pandemic of coronavirus disease 2019 (COVID-19), some studies have shown that COVID-19 does not induce severe asthma exacerbations or increase the risk of worse clinical outcomes of COVID-1911,12; however, a study showed that asthmatic patients infected with COVID-19 were likely to have worse outcomes.13 Therefore, fundamental data on the burden of asthma before the COVID-19 pandemic are valuable to investigate the impact of COVID-19 on the prospective asthma burden.
A few previous studies have reported the burden of asthma. Achakulwisut et al.14 reported on the burden of asthma incidence attributable to ambient NO2 pollution and described that reducing NO2 exposure could help prevent a substantial portion of new pediatric asthma cases. Liu et al.15 reported that the global asthma burden associated with obesity increased in absolute value, but the standardized burden decreased slightly. Zhang et al.16 focused on the burden of childhood asthma and showed that a high body mass index was a stronger risk factor than occupational asthmagens for childhood asthma. However, to date, no studies have examined changes in the burden of asthma in all age groups and provided a detailed analysis of asthma associated with risk factors over the past 30 years for the entire world. Therefore, synthetically analyzing the burden of asthma from different levels and dimensions is necessary.
According to the Global Burden of Disease (GBD) Study 2019 dataset, we analyzed the burden of asthma: incidence, mortality, disability-adjusted life year (DALY: its classic definition refers to all healthy life years lost from onset to death, estimated as the sum of years of life lost and years lived with disability) by region, age, and sex to assess change trends globally from 1990 to 2019. Moreover, the asthma burden distribution based on the sociodemographic index (SDI) quintile was calculated. Furthermore, the influence of multiple risk factors on asthma-related mortality and DALY was analyzed. This study provides a scientific basis for the global healthcare system to establish asthma prevention and treatment strategies by providing a multi-index and multilevel detailed understanding of the global burden of asthma.
MATERIALS AND METHODS
Data sources
In this study, detailed data on all asthma studies from 1990 to 2019 were obtained through the Global Health Data Exchange query tool (http://ghdx.healthdata.org/gbd-results-tool). The GBD 2019 dataset provides the burden of 364 diseases and injuries, 87 risk factors, and 18 causes in 204 countries and territories. Our study followed the Guidelines for Accurate and Transparent Health Estimates Reporting statement.17 First, considering the impact of age and sex on the global disease burden of asthma, data for different age ranges and sexes were extracted for analysis. Previous studies have shown that different sociodemographic characteristics considerably impact the GBD.18,19 Therefore, to understand the burden of asthma in different developing regions, all detailed data extraction referenced 4 dimensions: global, SDI quintiles, 21 GBD regions, and 204 countries and territories. This study used the SDI as a covariate and conducted correlation analysis. The SDI is a comprehensive index combining 3 components—the total fertility rate for those younger than 25 years of age, per capita income, and average educational attainment for those older than 15 years of age. The SDI is divided into 5 grades: high, high-middle, middle, low-middle, and low levels.20 Finally, the age-standardized incidence rate (ASIR), age-standardized death rate (ASDR), and age-standardized DALY rate in 204 countries and territories were used to reflect the asthma burden in the form of tables and world maps.
Statistical analysis
To objectively compare the asthma burden of different population structures or age changes at different time points in the same population, we used the following indicators: ASIR, ASDR, and age-standardized DALY rate. The age-standardized rate (ASR) is calculated based on the age structure of the standard population. ASR (per 100,000 population) is a crucial and representative indicator when there are differences in the age structure of multiple populations. We used the estimated annual percentage change (EAPC) based on ASRs, including ASIR, ASDR, and age-standardized DALY rate, to reflect the change trends of the asthma burden. EAPC is a recognized method to describe the changing trend of ASR with a regression model,21 which quantitatively calculates the average annual rate of change in ASR in all specific intervals. Consequently, a regression line is fit to the natural logarithm of the rates: y = α + βx + ε, where y means ln(ASR), and x means the calendar year. The EAPC value calculation formula is EAPC = 100 × (exp(β) −1). If the EAPC value and its 95% confidence interval (CI) are more than zero, the corresponding ASR is defined as a rising trend. In contrast, when the EAPC value and its 95% CI are less than 0, the ASR indicates a downward trend. Others represent a relatively stable ASR over time. To explore the correlation between ASR change trends and social development degrees, Pearson correlation analysis was used to evaluate the correlation between the EAPCs and SDI values in 2019. Finally, risk factors for asthma death and DALY were retrieved from the GBD database and visualized. P values less than 0.05 were defined as statistically significant differences.
Data visualization
We used R software (version 3.6.3; R Core Team, R Foundation, Vienna, Austria) to analyze all the data and perform data visualization using packages such as world maps and ggplot2. World heatmaps were used to visualize the asthma burden in 204 countries and territories. Histograms were used to demonstrate the global asthma burden with different sexes and age groups in 1990 and 2019. Scatter diagrams were used to show the distribution of the asthma burden in different SDI regions.
RESULTS
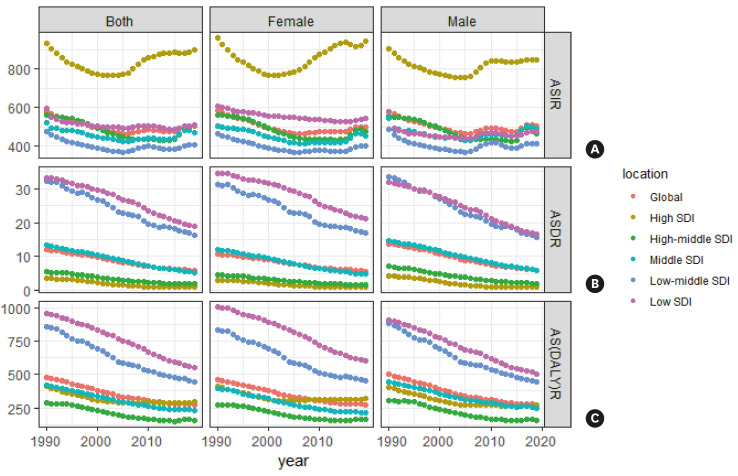
The incidence rate of asthma
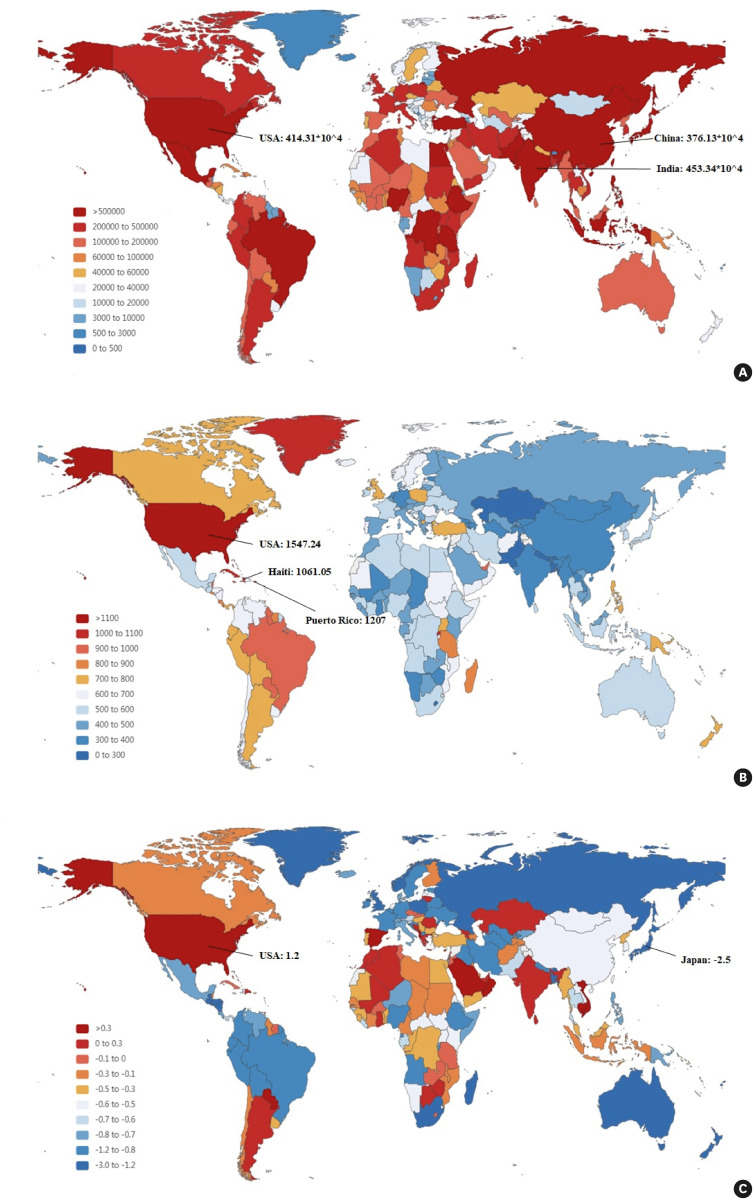
Globally, the incidence of asthma was 3,697.9 × 104 in 2019, with an insignificant increase of 15.0% from 3,216.32 × 104 in 1990. The incidence of asthma was slightly higher in males than in females. However, the ASIR decreased globally from 580.09/100,000 persons (95% urinary incontinence [UI] = 378.49, 579.59) in 1990 to 504.28/100,000 persons (95% UI = 216.71, 343.38) in 2019, EAPC = −0.47 (95% UI = −0.67, −0.27) (Table 1). Concerning all 5 SDI regions, except for the high-middle region, the incidence of asthma increased in the other 4 SDI regions. The middle SDI region had the highest number of asthma cases (952.99 × 104 in 1990 and 1,010.92 × 104 in 2019) (Fig. 1A). The ASIRs of the 5 SDI regions all showed downward trends, and the ASIR in the high SDI region maintained the highest level (Fig. 2A). At the 21 GBD region level, the highest number of asthma cases were observed in South Asia, high-income North America, and East Asia (South Asia: 543.80 × 104 in 2019; high-income North America: 436.64 × 104 in 2019; East Asia: 397.99 × 104 in 2019). The ASIR in high-income North America showed the most mushrooming rise during the past 30 years, with an EAPC = 1.12 (95% UI = 0.68, 1.56). We found that the ASIR of 21 GBD regions increased with increasing SDI values (Fig. 3A). At the country and territory levels, India, the USA, China, and Brazil had the highest number of asthma cases (453.34 × 104, 414.31 × 104, 376.13 × 104, and 162.32 × 104 in 2019, respectively) (Fig. 4A). The USA had the highest age-standardized ASIR, 1,547.24/100,000 persons in 2019 (Fig. 4B). In the past 30 years, the ASIR in Japan had the fastest decrease (EAPC = −2.5; 95% UI = −2.89, −2.10) and that in the USA had the promptest increase (EAPC = 1.20; 95% UI = 0.73, 1.69) (Fig. 4C).
Table 1. The incident cases and age-standardized incidence rate of asthma between 1990 and 2019 and its temporal trends from 1990 to 2019.
| Characteristics | 1990 | 1990 | 2019 | 2019 | 1990–2019 | |
|---|---|---|---|---|---|---|
| Incident cases, No. ×104 (95% UI) | ASR per 100,000, No. (95% UI) | Incident cases, No. ×104 (95% UI) | ASR per 100,000, No. (95% UI) | EAPC, No. (95% UI) | ||
| Overall | 3,216.32 (2,575.28, 4,051.31) | 580.09 (474.68, 715.04) | 3,697.93 (2,960.2, 4,592.81) | 504.28 (400.64, 633.26) | −0.47 (−0.67, −0.27) | |
| Sex | ||||||
| Male | 1,628.01 (1,282.9, 2,100.9) | 577.74 (466.39, 721.91) | 1,862.72 (1,469.48, 2,364.98) | 505.76 (394.92, 649.36) | −0.40 (−0.60, −0.19) | |
| Female | 1,588.31 (1,295.51, 1,970.68) | 582.27 (480.29, 709.48) | 1,835.21 (1,495.63, 2,237.83) | 501.55 (402.41, 621.43) | −0.55 (−0.75, −0.34) | |
| Sociodemographic index | ||||||
| Low | 376.30 (296.68, 482.53) | 594.50 (491.39, 718.57) | 655.77 (506.74, 848.56) | 511.23 (415.12, 624.63) | −0.31 (−0.44, −0.19) | |
| Low-middle | 568.25 (452.33, 722.52) | 475.36 (395.35, 574.04) | 697.63 (563.06, 863.36) | 409.29 (335.58, 505.67) | −0.39 (−0.62, −0.17) | |
| Middle | 952.99 (735.79, 1,246.65) | 523.33 (417.01, 662.57) | 1,010.92 (796.43, 1,275.85) | 471.75 (366.17, 607.69) | −0.28 (−0.49, −0.07) | |
| High-middle | 624.27 (502.08, 787.63) | 559.79 (446.64, 704.44) | 537.36 (432.19, 667.92) | 470.70 (356.3, 609.99) | −0.83 (−1.08, −0.58) | |
| High | 692.00 (572.97, 841.07) | 933.66 (749.54, 1,169.89) | 705.61 (590.01, 840.68) | 897.36 (711.33, 1,111.67) | 0.18 (−0.08, 0.44) | |
| Region | ||||||
| Central Asia | 29.96 (23.21, 38.95) | 406.44 (328.07, 503.31) | 35.37 (27.27, 45.98) | 379.29 (293.17, 489.20) | −0.43 (−0.54, −0.32) | |
| Central Europe | 86.05 (72.31, 103.42) | 714.15 (592.85, 873.9) | 58.70 (48.67, 70.48) | 616.99 (483.35, 789.96) | −0.69 (−0.77, −0.61) | |
| Eastern Europe | 143.34 (115.97, 177.06) | 655.11 (519.74, 826.37) | 75.53 (58.61, 96.63) | 461.89 (338.65, 613.63) | −1.63 (−1.82, −1.44) | |
| Australasia | 13.79 (11.08, 16.63) | 784.22 (622.41, 957.42) | 13.99 (11.16, 17.51) | 615.20 (473.25, 790.74) | −1.35 (−1.56, −1.14) | |
| High-income Asia Pacific | 137.13 (115.24, 164.67) | 852.87 (707.47, 1,042.26) | 79.59 (66.40, 95.14) | 554.49 (421.06, 724.34) | −2.02 (−2.31, −1.72) | |
| High-income North America | 336.88 (267.85, 431.51) | 1,351.69 (1,038.96, 1,769.35) | 436.64 (365.33, 520.76) | 1,474.11 (1,188.89, 1,810.73) | 1.12 (0.68, 1.56) | |
| Southern Latin America | 36.84 (30.77, 45.12) | 729.20 (612.38, 887.35) | 45.37 (37.03, 55.97) | 742.26 (592.41, 935.55) | −0.02 (−0.05, 0.02) | |
| Western Europe | 225.13 (192.29, 262.84) | 627.59 (526.75, 750.60) | 178.55 (147.21, 213.06) | 512.21 (397.33, 640.62) | −0.79 (−0.89, −0.68) | |
| Andean Latin America | 47.28 (35.09, 61.26) | 928.50 (698.16, 1,197.35) | 48.42 (36.07, 65.22) | 760.27 (565.28, 1,022.67) | −1.06 (−1.27, −0.85) | |
| Caribbean | 39.62 (31.46, 49.38) | 1,008.24 (804.93, 1,253.61) | 40.33 (32.15, 50.23) | 938.42 (741.65, 1,178.96) | −0.30 (−0.35, −0.25) | |
| Central Latin America | 143.56 (108.92, 185.18) | 717.59 (561.67, 909.60) | 137.26 (101.59, 182.39) | 583.29 (427.80, 775.69) | −0.95 (−1.19, −0.70) | |
| Tropical Latin America | 184.17 (133.85, 248.40) | 1,045.37 (769.77, 1,384.46) | 168.65 (121.47, 221.02) | 916.11 (645.54, 1,218.08) | −0.97 (−1.15, −0.80) | |
| North Africa and Middle East | 239.78 (187.36, 305) | 613.97 (502.26, 748.23) | 348.81 (276.77, 435.43) | 589.78 (473.10, 728.85) | −0.28 (−0.36, −0.21) | |
| South Asia | 390.16 (318.51, 491.99) | 388.17 (325.47, 459.44) | 543.80 (452.54, 658.72) | 329.58 (274.87, 394.58) | 0.08 (−0.32, 0.48) | |
| East Asia | 471.88 (354.47, 636.12) | 400.46 (301.23, 534.05) | 397.99 (308.29, 517.98) | 361.24 (264.84, 499.83) | −0.58 (−1.20, 0.03) | |
| Oceania | 5.33 (4.33, 6.51) | 781.11 (662.50, 910.50) | 9.15 (7.61, 11.00) | 665.36 (567.70, 777.32) | −0.70 (−0.78, −0.62) | |
| Southeast Asia | 289.48 (230.62, 367.68) | 576.89 (474.49, 709.35) | 345.10 (281.03, 427.10) | 553.39 (445.75, 698.10) | −0.20 (−0.25, −0.15) | |
| Central Sub-Saharan Africa | 41.52 (31.83, 53.02) | 585.13 (480.34, 707.87) | 81.81 (62.91, 105.37) | 518.71 (420.69, 641.53) | −0.52 (−0.56, −0.48) | |
| Eastern Sub-Saharan Africa | 186.66 (143.70, 242.65) | 744.14 (605.15, 919.93) | 331.91 (250.72, 434.45) | 651.85 (518.29, 817.23) | −0.55 (−0.61, −0.49) | |
| Southern Sub-Saharan Africa | 32.39 (23.75, 42.49) | 563.12 (429.98, 713.65) | 38.54 (28.92, 50.46) | 496.95 (376.47, 641.51) | −1.16 (−1.80, −0.51) | |
| Western Sub-Saharan Africa | 135.38 (102.55, 178.19) | 581.54 (469.32, 726.04) | 282.42 (210.29, 378.17) | 514.29 (408.95, 658.46) | −0.59 (−0.67, −0.51) | |
UI, urinary incontinence; ASR, age-standardized rate; EAPC, estimated annual percentage change.
Fig. 1. Changes in (A) asthma incidence, (B) deaths, and (C) DALYs from 1990 to 2019. Blue bars represent males, and red bars represent females.
DALY, disability-adjusted life year; SDI, sociodemographic index.
Fig. 2. The trends of (A) ASIR change, (B) ASDR, and (C) age-standardized DALY rate (per 100,000 persons) globally and among different SDI quintiles between 1990 and 2019.
ASIR, age-standardized incidence rate; ASDR, age-standardized death rate; DALY, disability-adjusted life year; SDI, sociodemographic index.
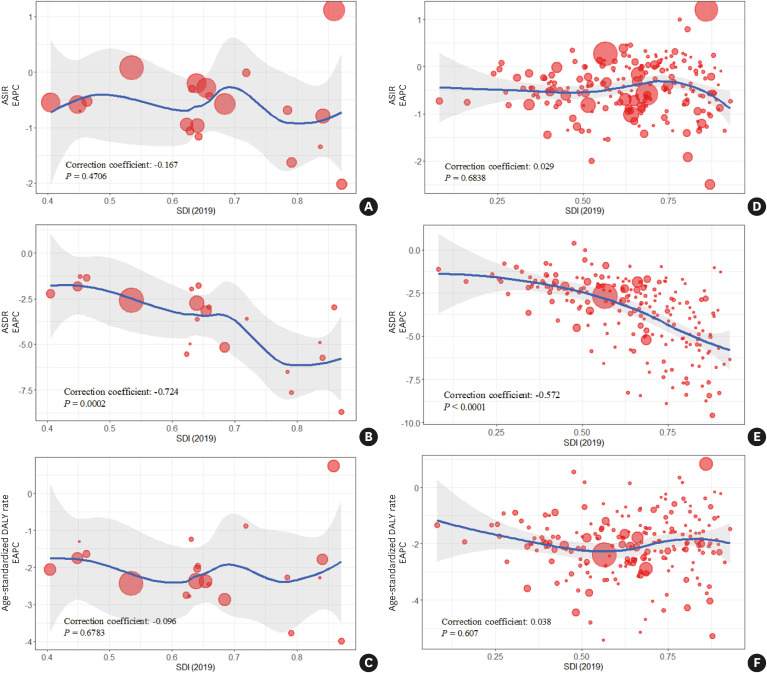
Fig. 3. The change trends and correlation analyses of age-standardized rates and SDI (2019) from 1990 to 2019 in 21 Global Burden of Disease regions. (A) ASIRs-SDI (2019). (B) ASDRs-SDI (2019). (C) Age-standardized DALY rates-SDI (2019).
ASIR, age-standardized incidence rate; ASDR, age-standardized death rate; DALY, disability-adjusted life year; SDI, sociodemographic index.
Fig. 4. The global disease burden of asthma in 204 countries or territories. (A) The absolute number of asthma cases in 2019. (B) The ASIR (per 100,000 persons) of asthma in 2019. (C) The EAPCs in asthma ASIRs between 1990 and 2019.
ASIR, age-standardized incidence rate; EAPC, estimated annual percentage change.
The mortality rate of asthma
Globally, the number of deaths slightly increased during the past 30 years (460.01 × 103 in 1990 and 461.07 × 103 in 2019), whereas the ASDR decreased (Table 2). Given the sociodemographic factors, more than half of the total asthma death cases occurred in the low-middle and middle SDI regions. The low-middle SDI region had the most deaths until 2019 (Fig. 1B). The ASDRs of 5 SDI regions exhibited a downward trend, with the high SDI region showing the most obvious decline (EAPC = −5.35; 95% UI = −5.76, −4.93) (Fig. 2B). For 21 GBD regions, South Asia and Southeast Asia were the top 2 countries with the highest death cases (South Asia: 232.19 × 104 in 2019; Southeast Asia: 72.06 × 104 in 2019). From 1990 to 2019, asthma death cases increased in 5 of the 21 GBD regions and decreased to varying degrees in other regions. ASDR showed a downward trend with increasing SDI value. The ASDR declined in all 21 GBD regions, with the most remarkable decline in high-income Asia Pacific (EAPC = −8.69; 95% UI = −9.24, −8.14), followed by Eastern Europe and Central Europe (Fig. 3B). Subgroup analysis by 204 countries and territories revealed that India, Indonesia, and China accounted for the highest number of deaths (Supplementary Fig. S1A). Kiribati was the country with the highest ASDR, 80.50/100,000 persons (95% UI = 59.22, 104.19) in 2019 (Supplementary Fig. S1B). The ASDR in the Republic of Korea showed the sharpest decrease (EAPC = −9.59; 95% UI = −10.30, −8.87), and that in Zimbabwe showed the most rapid increase (EAPC = 0.39; 95% UI = 0.12, 0.67) (Supplementary Fig. S1C).
Table 2. The death cases and age-standardized incidence rate of asthma between 1990 and 2019 and its temporal trends from 1990 to 2019.
| Characteristics | 1990 | 1990 | 2019 | 2019 | 1990–2019 | |
|---|---|---|---|---|---|---|
| Death cases, No. ×103 (95% UI) | ASR per 100,000, No. (95% UI) | Death cases, No. ×103 (95% UI) | ASR per 100,000, No. (95% UI) | EAPC, No. (95% UI) | ||
| Overall | 460.01 (342.62, 599.60) | 11.91 (8.80, 15.86) | 461.07 (366.58, 559.01) | 5.80 (4.62, 7.03) | −2.65 (−2.73, −2.57) | |
| Sex | ||||||
| Male | 232.93 (168.39, 323.36) | 13.76 (9.82, 19.51) | 213.67 (174.06, 260.24) | 5.93 (4.84, 7.21) | −3.06 (−3.14, −2.98) | |
| Female | 227.08 (152.95, 313.98) | 10.67 (7.15, 14.80) | 247.40 (179.85, 320.09) | 5.72 (4.16, 7.39) | −2.32 (−2.41, −2.24) | |
| Sociodemographic index | ||||||
| Low | 75.92 (52.69, 102.49) | 33.26 (22.16, 49.06) | 90.18 (65.75, 127.84) | 18.94 (13.35, 28.66) | −2.03 (−2.16, −1.90) | |
| Low-middle | 175.69 (118.67, 247.70) | 32.29 (21.25, 48.01) | 200.06 (143.31, 257.38) | 16.29 (11.60, 21.33) | −2.46 (−2.55, −2.36) | |
| Middle | 118.02 (92.35, 150.27) | 13.26 (10.19, 17.46) | 116.85 (100.29, 131.92) | 5.33 (4.55, 6.02) | −3.25 (−3.34, −3.15) | |
| High-middle | 53.39 (45.39, 64.00) | 5.50 (4.64, 6.65) | 35.68 (30.69, 40.38) | 1.83 (1.57, 2.07) | −4.16 (−4.32, −4.00) | |
| High | 36.67 (32.6, 39.1) | 3.57 (3.17, 3.81) | 17.96 (15.62, 20.18) | 0.96 (0.86, 1.07) | −5.35 (−5.76, −4.93) | |
| Region | ||||||
| Central Asia | 4.47 (3.68, 5.32) | 10.26 (8.30, 12.43) | 3.34 (2.87, 4.05) | 5.42 (4.69, 6.54) | −2.96 (−3.34, −2.59) | |
| Central Europe | 6.36 (5.78, 6.82) | 4.63 (4.20, 5.00) | 1.78 (1.51, 2.14) | 0.81 (0.69, 0.98) | −6.52 (−6.87, −6.17) | |
| Eastern Europe | 11.36 (9.33, 12.43) | 4.20 (3.43, 4.62) | 2.33 (1.96, 3.41) | 0.70 (0.59, 1.02) | −7.62 (−8.16, −7.09) | |
| Australasia | 0.98 (0.88, 1.06) | 4.33 (3.88, 4.67) | 0.54 (0.45, 0.64) | 1.14 (0.96, 1.31) | −4.93 (−5.61, −4.26) | |
| High-income Asia Pacific | 12.38 (9.71, 13.50) | 7.03 (5.44, 7.69) | 4.95 (3.76, 6.27) | 0.83 (0.66, 1.04) | −8.69 (−9.24, −8.14) | |
| High-income North America | 5.53 (5.10, 6.36) | 1.65 (1.53, 1.88) | 4.37 (3.59, 4.70) | 0.83 (0.70, 0.88) | −2.96 (−3.26, −2.67) | |
| Southern Latin America | 1.26 (1.10, 1.41) | 2.79 (2.45, 3.12) | 0.88 (0.73, 1.01) | 1.07 (0.89, 1.21) | −3.61 (−3.80, −3.42) | |
| Western Europe | 17.56 (15.99, 19.07) | 3.11 (2.83, 3.36) | 6.90 (5.73, 7.83) | 0.70 (0.61, 0.79) | −5.74 (−6.17, −5.30) | |
| Andean Latin America | 1.29 (0.91, 1.61) | 4.13 (3.09, 5.01) | 0.52 (0.40, 0.66) | 0.95 (0.73, 1.19) | −4.97 (−5.17, −4.77) | |
| Caribbean | 2.39 (1.88, 2.91) | 8.06 (6.35, 10.09) | 2.23 (1.69, 2.83) | 4.54 (3.43, 5.83) | −1.96 (−2.09, −1.84) | |
| Central Latin America | 5.75 (4.90, 6.17) | 6.52 (5.64, 7.02) | 3.42 (2.81, 4.05) | 1.49 (1.23, 1.76) | −5.55 (−5.83, −5.27) | |
| Tropical Latin America | 3.28 (2.88, 3.59) | 3.45 (3.01, 3.79) | 2.94 (2.61, 3.45) | 1.28 (1.14, 1.50) | −3.64 (−3.84, −3.44) | |
| North Africa and Middle East | 32.42 (26.00, 42.14) | 20.45 (15.90, 28.03) | 32.08 (26.20, 38.35) | 8.39 (6.86, 9.92) | −3.16 (−3.23, −3.09) | |
| South Asia | 185.11 (118.30, 278.67) | 38.82 (24.26, 61.63) | 232.19 (160.83, 316.30) | 18.95 (12.92, 26.43) | −2.61 (−2.75, −2.47) | |
| East Asia | 43.49 (33.08, 61.96) | 6.60 (4.92, 9.65) | 27.21 (22.73, 33.03) | 1.59 (1.33, 1.93) | −5.18 (−5.40, −4.96) | |
| Oceania | 1.60 (1.26, 2.12) | 67.94 (51.62, 94.50) | 2.56 (1.89, 3.45) | 46.76 (34.38, 63.61) | −1.29 (−1.37, −1.20) | |
| Southeast Asia | 72.71 (55.59, 86.99) | 30.93 (22.89, 38.63) | 72.06 (61.16, 81.55) | 13.79 (11.64, 15.64) | −2.74 (−2.81, −2.67) | |
| Central Sub-Saharan Africa | 7.10 (4.64, 10.33) | 31.20 (18.83, 55.74) | 9.79 (6.18, 17.11) | 20.63 (12.04, 41.64) | −1.38 (−1.60, −1.16) | |
| Eastern Sub-Saharan Africa | 18.63 (14.01, 22.32) | 20.73 (15.29, 28.44) | 19.76 (15.36, 28.24) | 11.29 (8.54, 17.52) | −2.23 (−2.30, −2.15) | |
| Southern Sub-Saharan Africa | 6.39 (5.50, 7.60) | 22.72 (19.10, 27.97) | 7.11 (6.30, 8.29) | 13.78 (12.14, 16.11) | −1.80 (−2.40, −1.19) | |
| Western Sub-Saharan Africa | 19.95 (15.91, 23.96) | 23.04 (18.35, 28.45) | 24.11 (19.91, 29.11) | 13.13 (10.95, 15.72) | −1.83 (−1.87, −1.79) | |
UI, urinary incontinence; ASR, age-standardized rate; EAPC, estimated annual percentage change.
The DALY rate of asthma
At the global level, the DALY number decreased from 2,232.11 × 104 in 1990 to 2,155.10 × 104 in 2019, and the age-standardized DALY rate decreased from 476.28/100,000 persons (95% UI = 378.49, 579.59) in 1990 to 273.63/100,000 to persons (95% UI = 216.71, 343.38) in 2019, EAPC = −2.05 (95% UI = −2.16, −1.94) (Table 3). Subgroup analysis by sociodemographic factor showed that only the DALY numbers in the low SDI and low-middle SDI regions increased from 1990 to 2019 (Fig. 1C). The age-standardized DALY rates in the 5 SDI regions all decreased and were most serious in the high-middle SDI region, with an EAPC of −2.52 (95% UI = −2.76, −2.27) (Fig. 2C). In the subgroup analysis of 21 GBD regions, the top 2 highest DALY numbers were observed in South Asia and Southeast Asia (South Asia: 690.76 × 104 in 2019; Southeast Asia: 267.87 × 104 in 2019). The age-standardized DALY rate in high-income North America was the only one showing an upward trend with an EAPC = 0.74 (95% UI = 0.34, 1.15), and that in high-income Asia Pacific displayed the greatest decrease with an EAPC = −3.99 (95% UI = −4.38, −3.59). Similar to the ASDR, the age-standardized DALY rate tended to decrease with increasing SDI values (Fig. 3C). At the level of 204 countries and territories, India, the USA, China, and Indonesia had the most DALY numbers (583.88 × 104, 141.32 × 104, 141.46 × 104, and 104.50 × 104 in 2019, respectively) (Supplementary Fig. S2A). Kiribati had the highest age-standardized DALY rate, 2,630.86/100,000 persons (95% UI = 2,187.96, 3,178.83) in 1990 and 1,795.09/100,000 persons (95% UI = 1,411.44, 2,242.16) in 2019 (Supplementary Fig. S2B). In the past 30 years, the age-standardized DALY rate in the Maldives showed the fastest decrease (EAPC = −5.42; 95% UI= −5.81, −5.04), and that in the USA showed the most pronounced increase (EAPC = 0.83; 95% UI = 0.40, 1.26) (Supplementary Fig. S2C).
Table 3. The DALYs and age-standardized DALY rate of asthma between 1990 and 2019 and its temporal trends from 1990 to 2019.
| Characteristics | 1990 | 1990 | 2019 | 2019 | 1990–2019 | |
|---|---|---|---|---|---|---|
| DALY cases, No. ×104 (95% UI) | Age-standardized DALY rate per 100,000, No. (95% UI) | DALY cases, No. ×104 (95% UI) | Age-standardized DALY rate per 100,000, No. (95% UI) | EAPC, No. (95% UI) | ||
| Overall | 2,232.11 (1,790.95, 2,734.42) | 476.28 (378.49, 579.59) | 2,155.10 (1,714.16, 2,697.2) | 273.63 (216.71, 343.38) | −2.05 (−2.16, −1.94) | |
| Sex | ||||||
| Male | 1,118.99 (896.42, 1,392.93) | 498.88 (392.53, 620.97) | 1,043.47 (831.89, 1,305.02) | 272.16 (216.88, 340.92) | −2.22 (−2.33, −2.10) | |
| Female | 1,113.12 (854.82, 1,393.92) | 461.30 (353.71, 579.02) | 1,111.63 (867.46, 1,407.52) | 275.24 (214.89, 349.63) | −1.94 (−2.05, −1.84) | |
| Sociodemographic index | ||||||
| Low | 342.34 (264.04, 407.69) | 958.70 (705.09, 1,243.84) | 418.87 (332.02, 525.88) | 553.90 (434.74, 726.78) | −1.99 (−2.07, −1.91) | |
| Low-middle | 647.86 (486.57, 802.91) | 859.43 (615.47, 1,143.21) | 655.82 (519.11, 797.41) | 445.90 (348.53, 546.29) | −2.36 (−2.44, −2.28) | |
| Middle | 566.51 (463.59, 691.22) | 419.94 (341.9, 508.8) | 542.95 (436.30, 675.84) | 230.64 (183.79, 290.27) | −2.20 (−2.29, −2.11) | |
| High-middle | 316.31 (245.87, 410.70) | 286.79 (224.27, 369.40) | 235.39 (176.17, 316.81) | 158.33 (114.00, 220.25) | −2.52 (−2.76, −2.27) | |
| High | 357.27 (263.10, 483.65) | 409.25 (295.92, 561.89) | 300.22 (209.17, 420.21) | 293.69 (200.72, 419.44) | −1.10 (−1.36, −0.85) | |
| Region | ||||||
| Central Asia | 17.48 (14.36, 21.24) | 324.22 (270.15, 387.10) | 16.07 (12.66, 20.47) | 197.95 (160.01, 246.02) | −2.45 (−2.76, −2.15) | |
| Central Europe | 42.59 (32.15, 56.97) | 317.67 (236.94, 429.27) | 22.63 (15.72, 31.84) | 180.45 (119.9, 263.92) | −2.27 (−2.48, −2.07) | |
| Eastern Europe | 72.43 (56.56, 92.70) | 288.54 (221.46, 374.87) | 26.08 (18.44, 36.39) | 124.09 (84.15, 182.59) | −3.78 (−4.09, −3.47) | |
| Australasia | 12.08 (8.90, 16.22) | 593.53 (433.65, 802.06) | 10.11 (6.92, 14.49) | 359.99 (239.04, 527.64) | −2.28 (−2.52, −2.03) | |
| High-income Asia Pacific | 74.19 (55.81, 98.14) | 409.49 (306.25, 543.25) | 33.58 (23.72, 46.49) | 160.29 (105.89, 237.58) | −3.99 (−4.38, −3.59) | |
| High-income North America | 112.01 (78.38, 157.65) | 401.62 (276.72, 570.29) | 148.46 (102.18, 205.73) | 412.95 (282.52, 584.39) | 0.74 (0.34, 1.15) | |
| Southern Latin America | 16.24 (11.72, 22.12) | 333.79 (242.27, 454.37) | 19.06 (13.04, 27.12) | 275.77 (188.18, 399.41) | −0.88 (−0.95, −0.81) | |
| Western Europe | 176.88 (129.03, 241.52) | 396.41 (284.2, 551.61) | 115.01 (78.58, 164.12) | 245.62 (162.85, 361.91) | −1.79 (−1.95, −1.63) | |
| Andean Latin America | 18.37 (13.12, 24.63) | 396.37 (290.64, 521.9) | 12.16 (7.86, 18.56) | 192.28 (124.91, 291.95) | −2.78 (−3.13, −2.42) | |
| Caribbean | 21.74 (16.29, 27.56) | 608.76 (462.11, 763.86) | 19.30 (14.62, 24.99) | 422.79 (315.68, 553.54) | −1.25 (−1.37, −1.14) | |
| Central Latin America | 52.91 (40.52, 69.98) | 337.68 (271.21, 429.32) | 40.39 (28.31, 57.46) | 166.15 (116.28, 237.45) | −2.75 (−3.05, −2.45) | |
| Tropical Latin America | 53.57 (37.98, 76.89) | 340.11 (250.73, 473.47) | 46.60 (32.18, 68.55) | 227.28 (154.5, 339.89) | −2.03 (−2.22, −1.84) | |
| North Africa and Middle East | 152.44 (124.45, 182.69) | 618.12 (513.67, 757.56) | 167.78 (131.81, 212.26) | 324.16 (259.23, 397.53) | −2.38 (−2.45, −2.31) | |
| South Asia | 610.59 (428.46, 820.81) | 935.82 (632.71, 1,352.04) | 690.76 (520.56, 869.53) | 472.00 (350.52, 601.23) | −2.44 (−2.51, −2.36) | |
| East Asia | 213.84 (160.83, 280.15) | 215.90 (165.88, 279.90) | 152.81 (114.20, 206.25) | 106.42 (75.33, 152.05) | −2.87 (−3.30, −2.43) | |
| Oceania | 6.23 (5.11, 7.79) | 1,610.92 (1,286.27, 2,090.81) | 9.50 (7.41, 12.22) | 1,102.21 (863.7, 1,431.32) | −1.30 (−1.38, −1.23) | |
| Southeast Asia | 296.37 (245.48, 341.1) | 860.93 (699.29, 995.38) | 267.87 (225.29, 316.45) | 433.23 (365.45, 509.73) | −2.37 (−2.40, −2.34) | |
| Central Sub-Saharan Africa | 36.53 (25.88, 45.29) | 920.05 (640.15, 1,325.52) | 47.95 (34.14, 65.87) | 572.95 (389.25, 907.95) | −1.64 (−1.82, −1.46) | |
| Eastern Sub-Saharan Africa | 122.82 (96.13, 149.56) | 790.39 (622.07, 947.47) | 145.06 (112.06, 185.67) | 450.86 (356.42, 582.77) | −2.07 (−2.12, −2.02) | |
| Southern Sub-Saharan Africa | 29.37 (25.01, 34.92) | 744.87 (640.15, 871.84) | 29.90 (24.90, 36.62) | 446.49 (378.51, 530.69) | −1.97 (−2.45, −1.49) | |
| Western Sub-Saharan Africa | 93.44 (77.18, 110.39) | 704.15 (582.61, 830.73) | 134.01 (108.09, 167.04) | 425.22 (354.05, 508.79) | −1.75 (−1.80, −1.70) | |
DALY, disability-adjusted life year; UI, urinary incontinence; EAPC, estimated annual percentage change.
Age and sex distribution of asthmatic patients
Globally, over the past 30 years, although the number of asthma cases was higher in males than in females, deaths and DALYs in females gradually exceeded those in males. The peak incidence of asthma occurred in those aged younger than 5 years, and the asthma incidence aged between 5 and 9 years was also extremely high (Fig. 5A). The ratio of patients aged younger than 24 years to total individuals was approximately 66% in 2019. Before the age of 9 years, the asthma incidence in male individuals was higher, and the reverse was true thereafter. The number of asthma deaths remained at a stable low level between the ages of 5 and 29 years, with a gradual upward trend from the age of 35 years until the peak at 80 plus years. Worryingly, the deaths of children under 5 years were also not low (Fig. 5B). Regarding the number of DALY in 2019, 2 peaks were observed: children (younger than 9 years old) and the elderly (60 to 64 years old). The DALY cases were higher in females than in males aged 20 to 49 years in 1990, and they were higher in females than in males after the age of 25 years in 2019 (Fig. 5C). We analyzed changes in the incidence, death, and DALY rates of asthma in different age groups during the past 30 years and found that compared with older patients, the death and DALY rates of younger patients younger than 50 years were lower than those of ASDR and the age-standardized DALY rate, respectively. In addition, the death and DALY rates of patients older than 50 years decreased more significantly over the year (Supplementary Fig. S3).
Fig. 5. The global burden of asthma in both sexes and different age groups in 1990 and 2019. (A) The absolute number of asthma cases. (B) The absolute number of deaths. (C) The absolute number of DALYs. Blue bars represent male individuals, and red bars represent female individuals; light bars represent 1990, and dark bars represent 2019.
DALY, disability-adjusted life year.
Correlations between the SDI and asthma burden
First, we calculated the correlation coefficients between the SDI in 2019 and EAPC values of the ASIR, ASDR, and age-standardized DALY rate in 204 countries and territories. The correlations between the SDI and EAPCs of ASIR and age-standardized DALY rate were not statistically significant, whereas the EAPC of the ASDR was markedly negatively correlated with the SDI (correlation coefficient of EAPC = −0.572; P < 0.0001) (Fig. 6). To further evaluate the association between the SDI and asthma burden, we investigated the correlation between the SDI and ASIR, ASDR and age-standardized DALY rate in 21 GBD regions worldwide from 1990 to 2019. The ASIR value was positively correlated with the SDI (correlation coefficient of the ASIR = 0.228; P < 0.0001); however, the ASDR and age-standardized DALY rate values were negatively correlated with the SDI (correlation coefficient of the ASDR = −0.653; correlation coefficient of the age-standardized DALY rate = −0.599; P < 0.0001) (Fig. 3).
Fig. 6. Correlation analyses of EAPCs-SDI (2019). EAPCs of (A) ASIR-SDI (2019), (B) ASDR-SDI (2019), and (C) age-standardized DALY rate-SDI (2019) in 21 GBD regions; EAPCs of (D) ASIR-SDI (2019), (E) ASDR-SDI (2019), and (F) age-standardized DALY rate-SDI (2019) in 204 countries or territories. The size of the circle represents the quantity of asthma patients in a single region/country or territory.
ASIR, age-standardized incidence rate; ASDR, age-standardized death rate; DALY, disability-adjusted life year; EAPC, estimated annual percentage change; SDI, sociodemographic index.
Asthma-related death and DALY attributable risk factors from 1990 to 2019
We searched the GBD database for potential asthma-related risk factors for deaths and DALYs. The leading risk factors for deaths and DALYs due to asthma were smoking, occupational asthmagens, and high body mass index. From 1990 to 2019, globally, the proportion of asthma deaths/DALYs attributable to smoking declined, and the proportion of patients with a high body mass index increased. For occupational asthmagens, the proportion of asthma deaths also decreased; however, the proportion of asthma DALYs showed no obvious change law.
Smoking-related asthma deaths/DALYs showed a downward trend in all SDI quintiles, most notably in the high SDI region. The proportions of asthma deaths/DALYs attributable to a high body mass index showed an upward trend in all SDI quintiles, most significantly in the high SDI region. At the same time, we found that the higher the SDI was, the higher the proportion of asthma deaths/DALYs attributed to smoking/high body mass index, but that for occupational asthmagens was almost the opposite (Fig. 7).
Fig. 7. Risk factors for asthma-related deaths and DALYs. (A) The proportions of the 3 risk factors contributing to asthma-related deaths from 1990 to 2019 globally and in different regions. (B) The proportions of the 3 risk factors contributing to asthma-related DALYs from 1990 to 2019 globally and in different regions.
DALY, disability-adjusted life year; SDI, sociodemographic index.
For 21 GBD regions, the percentage of asthma deaths/DALYs attributable to smoking/occupational asthmagens was much higher in males than in females; however, that for high body mass index was reversed. It is important to note that in all GBD regions, the percentage of asthma deaths/DALYs attributable to high body mass index increased in 2019 when compared with 1990 in both sexes (Supplementary Fig. S4). At all ages, the percentage of asthma deaths/DALYs attributable to smoking/occupational asthmagens was significantly higher in males than in females. For high body mass index, the percentage was much higher in females than in males and higher in 2019 than in 1990 (Supplementary Fig. S5).
To determine the relationship between risk factors associated with asthma deaths/DALYs and the SDI, we also calculated the correlation coefficient between the SDI and percentage of asthma-related risk factors in 204 countries and territories. By analyzing the data on risk factors associated with asthma deaths, the proportion of high body mass index/smoking increased as the SDI value increased, showing a positive correlation (correlation coefficient of high body mass index = 0.66; P < 0.0001 in 2019; correlation coefficient of smoking = 0.511; P < 0.0001 in 2019). However, our findings demonstrated a negative correlation between the proportion of asthma-related occupational asthmagens and the SDI (correlation coefficient of occupational asthmagens = −0.692; P < 0.0001 in 2019). The relationship between the proportion of DALYs attributable to high body mass index/smoking and SDI was similar to that between the proportion of high body mass index/smoking attributable to asthma deaths and the SDI; however, the association between the proportion of occupational asthmagens contributing to asthma DALYs and the SDI was not statistically significant (Supplementary Fig. S6).
DISCUSSION
Understanding the temporal trends of the asthma burden facilitates the initiation of more targeted public health strategies. The present study comprehensively reflected the latest global burden of asthma by analyzing data on the incidence, death, DALY, and most relevant risk factors for asthma from 1990 to 2019. Although the incidence and death rate of asthma slightly increased (15% and 0.2%, respectively) during the past 30 years, the overall ASIR, ASDR, and age-standardized DALY rate relatively decreased and showed a declining trend with negative EAPC values. This phenomenon might be attributable to the population size and distribution structure and the changes in diagnostic methods from clinical to laboratory examination—for example, lung function tests. In addition, variabilities in region, sex, and age played important roles in the asthma incidence and mortality. The incidence, death, and DALY of asthma were heterogeneous among people in different age groups and from country to country.
In 2019, the highest incidence was found in children aged younger than 9 years, particularly those aged 0 to 5 years, because they are vulnerable to respiratory infections and other environmental hazards.22 In addition, the age-specific incidence was higher in boys (0–9 years old), almost equal in sex during adolescence (10–14 years old), and higher in females later, indicating a switch during puberty (Fig. 5A). Possibly because of the high diagnosis rate of asthma in that age group, this finding was consistent with those of some large sample studies.23,24 Boys have higher incidences partly because of their smaller airway relative to lung size compared with girls, but this mode reverses during puberty. Additionally, a prospective study confirmed that asthma remission was more likely in boys, but less likely in girls and severe asthma or sensitization to furred animals.25 These factors explain the high incidence of asthma in young boys. The incidence of asthma after puberty was higher in females than in males, particularly in middle-aged women, likely because of their obvious hormonal changes. Menopause, for example, was used as a forceful predictor of asthma in women not using exogenous hormones.26
The number of asthma deaths increased with age, and most asthma deaths occurred in people aged older than 60 years (more than 70% of all deaths) (Fig. 5B). One reason is the increasingly prominent aging social structure; currently, 8.5% of the world’s population is aged older than 60 years.27 Between 1990 and 2019, the number of older persons (those aged 60 years or older) in the world grew by 114%, from 483 million to more than 1.03 billion. The number of children aged younger than 14 years also showed an increasing trend (1990: 1.7 billion; 2019: 2.0 billion).28 Thus, the ratio of elderly and pediatric patients with asthma has increased. A second reason is that some studies have shown that asthma with onset later in life has a poorer prognosis.29,30 The pathophysiology of asthma in elderly individuals is different from that of early-onset asthma. Older individuals experience a decrease in elastic fibers, curvature in the spine, and a stiffening of the thorax because of a decline in particular movements, all of which will decrease the amount of traction on the bronchi of the lungs. For elderly patients, these events may lead to the narrowing of the bronchioles.31 Iwanaga et al.32 found that R5-R20, representing the index for the small airway, was distinctly higher in elderly asthmatic patients aged older than 65 years. Therefore, small airway disease was more severe in elderly asthmatic patients than in younger patients with asthma. Furthermore, the disease burden is mainly focused on 2 groups of people, those aged older than 60 years and children younger than 9 years, which were the focus of our healthcare institutions.
The burden of asthma was the highest in South Asia, Southeast Asia, and East Asia, and it was higher in high-income North America, Western Sub-Saharan Africa, and Tropical Latin America. South Asia, Southeast Asia and East Asia, are the most densely populated regions in the world, home to approximately half of the world's population. The large population also contributed to the higher burden of asthma. Tropical Latin America is usually racially admixed, with heterogeneous proportions of European, Native American, and African ancestry. A study showed that African ancestry has been associated with lower lung function, leading to an increased susceptibility to asthma in these populations.33 Therefore, it makes sense for Western Sub-Saharan Africa and Tropical Latin America to have a higher disease burden of asthma.
At the country level, except for China, India, and Indonesia, different countries faced different asthma burdens. Considering the increasing incidence of asthma in children in China, the National Clinical Research Center for Respiratory Diseases developed the Action Plan for Asthma in Children in China to improve the level of self-management of asthma in children.34 Notably, the asthma incidence in the United States of America (USA) remained in the top 3 all along, and the ASIR not only always maintained the first place but also kept rising the fastest. Because the incidence and outcome of asthma vary widely across geographical regions, such as the greater disease burden in rural areas, rural health has become increasingly crucial in health surveillance and health equity in the US,35 and much work has been performed to measure asthma indicators by demographic characteristics and poverty level.36 Therefore, targeted health policy systems must be specified according to different situations.
During the past 30 years, asthma incidences have increased, particularly in high-income North America and South Asia. Moreover, our study demonstrated that the ASIR of asthma in high-income North America always remained the highest with an upward trend, such as in the USA. The region is one of the most economically developed in the world and rich in medical resources. Therefore, the screening and diagnosis of disease are timelier. Encouragingly, little increase was observed in the number of deaths and DALYs, and the ASDR and age-standardized DALY rate continued to decline, suggesting that health policy designation had a positive effect on the burden of asthma, both fatal and nonfatal. However, concerns persist about the burden of asthma in individual regions.
The difference in asthma burden changes is due to multiple factors. In addition to the health care system, it also includes biological, sociocultural, and built environments. For example, many risk alleles and loci representing almost all chromosomes in the human genome were identified by genome-wide association studies of asthma, such as 6p21, 2q12, 5q22, and 9p24. However, some studies have confirmed that every locus is not equally expressed in all populations. The 17q12-21 locus is verified as the most replicated and most distinct asthma locus and is highly associated with early-onset asthma among European, Asian, and Latino individuals. However, weak and inconsistent associations of 17q are found in Africans.37,38 Therefore, the expression and polymorphism of asthma-related genes vary among ethnic groups, resulting in different disease occurrences and outcomes. A clear understanding of the changes in the burden of asthma and the characteristics of the disease will help policy-makers develop more precise strategies to reduce the burden of asthma.
We demonstrated that the global distribution of asthma burden was heterogeneous and uneven. At the level of sociodemographic factors, the area with the highest disease burden of asthma was the high SDI region—for instance, the USA—likely attributable to better asthma diagnosis and registry systems, as well as increasing population size and obvious aging trends. However, in some low-SDI and middle-SDI regions with low-income countries, health resources are relatively limited, and defining asthma by reported symptoms and a clinician diagnosis could result in an underestimate of asthma incidence in those countries.39 In addition, poverty, air pollution, climate change, exposure to indoor allergens, urbanization, and diet contribute to inadequate control and poor outcomes in developing countries.40 In high-SDI regions with high-income countries, the burden of death and DALY was lower due to greater access to health care and better treatment options based on international asthma guidelines.41 Therefore, the formulation of medical policies must be adjusted according to the actual local disease burden.
Our data showed that smoking, occupational asthmagens, and a high body-mass index were risk factors for asthma-caused death and DALY. A previous study showed that asthmatic patients who smoke have distinctly increased morbidity and mortality compared with nonsmokers.42 Continued smoking is related to aggravated loss of lung function over time in adult-onset asthma.43 Therefore, several initiatives have been implemented to reduce exposure to smoke. Some measures, such as banning advertising, creating tobacco-free spaces, inserting health warnings on the packaging of tobacco products, and increasing cigarette taxation, were advocated by the World Health Organization. The effect of high body mass index on asthma cannot be ignored. A study in the USA showed that genetic predisposition to obesity was a risk factor for asthma, particularly for childhood-onset asthma, in females44 but not in males. Having an obese mother also increases the risk of asthma in children.45 Obese asthma results in worse asthma control and increased healthcare utilization due to asthma.46 We found that the higher the SDI, the higher the proportion of asthma deaths/DALYs attributed to smoking/high body mass index. Although the age-standardized global prevalence of daily smoking was 15.3%, a 29.4% decrease from 1990,47 globally in 2019, most countries with the highest tobacco consumption per person were in the high SDI and high-middle SDI regions, such as Slovenia, Montenegro, and North Macedonia, all having consumption exceeding 2,350 cigarette equivalents per person. However, the low SDI regions, such as sub-Saharan Africa, had the lowest tobacco consumption per person.48 Similarly, obesity is more common in developed countries than in developing countries.49
Occupational asthmagens, including gas, smoke or dust, organic dust, dampness and mold, cold conditions, and other agents, were associated with exacerbation of asthma. The proportion due to occupational asthmagens was much higher in the low and low-middle SDI regions, and no obvious downward trend of asthma deaths/DALYs was attributable to occupational asthmagens in either sex over time. With globalization, many manufacturing factories were relocated to underdeveloped regions; however, strict occupational protection was not fully implemented. Thus, some occupational interventions and policies to reduce work-related asthma were needed according to the SDI.
In summary, globally, the incidence of asthma has prominently increased, and children have a higher risk of developing asthma. The number of deaths slightly increased, and more than 70% of all deaths occurred in patients aged older than 60 years. The low-middle SDI region, particularly South Asia, had the highest asthma-related death and DALY burden. The high SDI region had the highest ASIR, and the low SDI region had the highest ASDR. The ASDR and age-standardized DALY rate of asthma were negatively correlated with SDI values, indicating that the death and DALY rates were significantly higher in the developing regions than in the developed regions. Smoking, occupational asthmagen, and higher body mass index were the main risk factors contributing to asthma-related mortality and DALYs, and the effects of the 3 risk factors on asthma were different between sexes and regions. The asthma burden showed considerable spatiotemporal and sex-age heterogeneity. Globally, considering population growth and accelerated aging trends, the asthma burden might further increase. Systematic efforts must be achieved to reduce the asthma burden through ongoing efforts to identify the contribution of factors within the biological, behavioral, sociocultural, built environment, and healthcare domains to the development of asthma.
Although this study analyzed the global burden and attributable risk factors of asthma in 204 countries and territories from 1990 to 2019, it has several limitations. First, the accuracy of the GBD data used for analysis relies on the quality of the existing data in each country, and data collected by different regions and countries may vary substantially in terms of quality, comparability, accuracy, and the degree of data missing. Secondly, the lack of data on other asthma-associated risk factors limits the analysis of overall risk factors. Thirdly, our study is implemented at the regional and national levels and lacks an analysis of differences between urban and rural areas.
ACKNOWLEDGMENTS
This work were supported by The Scientific Research and Sharing Platform Construction Project of Shaanxi Province (Grant Number: 2022PT-07) and Scientific Research Foundation of The First Affiliated Hospital of Xi’an Jiaotong University (Project Number: 2021ZYTS-34).
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
SUPPLEMENTARY MATERIALS
Global death burden of asthma in 204 countries or territories. (A) Absolute number of asthma deaths in 2019. (B) ASDR (per 100,000 persons) of asthma in 2019. (C) Estimated annual percentage change of asthma ASDRs between 1990 and 2019.
Global DALY burden of asthma in 204 countries or territories. (A) Absolute number of asthma DALYs in 2019. (B) Age-standardized DALY rate (per 100,000 persons) of asthma in 2019. (C) Estimated annual percentage change of asthma age-standardized DALY rate between 1990 and 2019.
Trends of the incidence, death, and DALY rates (per 100,000 persons) among different age groups between 1990 and 2019.
Proportion of deaths/DALYs attributable to 3 risk factors in 21 Global Burden of Disease regions in 1990 and 2019. Blue bars represent male individuals, and red bars represent female individuals; light bars represent 1990, and dark bars represent 2019.
Proportions of deaths/DALYs attributable to 3 risk factors in different age groups in 1990 and 2019. Blue bars represent male individuals, and red bars represent female individuals; light bars represent 1990, and dark bars represent 2019.
Correlation analyses of the proportions of 3 risk factors attributable to deaths/DALYs-SDI (2019). (A) Smoking attributable to deaths-SDI (2019) and (D) smoking attributable to DALYs-SDI (2019). (B) High body-mass index attributable to deaths-SDI (2019) and (E) high body-mass index attributable to DALYs-SDI (2019). (C) Occupational asthmagens attributable to deaths-SDI (2019) and (F) occupational asthmagens attributable to DALYs-SDI (2019). The size of the circle represents the quantity of asthmatic patients in a single country or territory.
References
- 1.Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018;391:783–800. doi: 10.1016/S0140-6736(17)33311-1. [DOI] [PubMed] [Google Scholar]
- 2.Global Asthma Network. The global asthma report 2018. Auckland: Global Asthma Network; 2018. [Google Scholar]
- 3.To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12:204. doi: 10.1186/1471-2458-12-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perez MF, Coutinho MT. An overview of health disparities in asthma. Yale J Biol Med. 2021;94:497–507. [PMC free article] [PubMed] [Google Scholar]
- 5.Aaron SD, Boulet LP, Reddel HK, Gershon AS. Underdiagnosis and overdiagnosis of asthma. Am J Respir Crit Care Med. 2018;198:1012–1020. doi: 10.1164/rccm.201804-0682CI. [DOI] [PubMed] [Google Scholar]
- 6.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001-2010. Vital Health Stat. 2012;3 [PubMed] [Google Scholar]
- 7.Inselman JW, Jeffery MM, Maddux JT, Shah ND, Rank MA. Trends and disparities in asthma biologic use in the United States. J Allergy Clin Immunol Pract. 2020;8:549–554.e1. doi: 10.1016/j.jaip.2019.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nurmagambetov T, Kuwahara R, Garbe P. The economic burden of asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018;15:348–356. doi: 10.1513/AnnalsATS.201703-259OC. [DOI] [PubMed] [Google Scholar]
- 9.Perry R, Braileanu G, Palmer T, Stevens P. The economic burden of pediatric asthma in the United States: literature review of current evidence. Pharmacoeconomics. 2019;37:155–167. doi: 10.1007/s40273-018-0726-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan PW, Ghushchyan V, Navaratnam P, Friedman HS, Kavati A, Ortiz B, et al. The national cost of asthma among school-aged children in the United States. Ann Allergy Asthma Immunol. 2017;119:246–252.e1. doi: 10.1016/j.anai.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Grandbastien M, Piotin A, Godet J, Abessolo-Amougou I, Ederlé C, Enache I, et al. SARS-CoV-2 pneumonia in hospitalized asthmatic patients did not induce severe exacerbation. J Allergy Clin Immunol Pract. 2020;8:2600–2607. doi: 10.1016/j.jaip.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sunjaya AP, Allida SM, Di Tanna GL, Jenkins C. Asthma and risk of infection, hospitalization, ICU admission and mortality from COVID-19: systematic review and meta-analysis. J Asthma. 2022;59:866–879. doi: 10.1080/02770903.2021.1888116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karlsson Sundbaum J, Vanfleteren LE, Konradsen JR, Nyberg F, Ekberg-Jansson A, Stridsman C. Severe COVID-19 among patients with asthma and COPD: a report from the Swedish National Airway Register. Ther Adv Respir Dis. 2021;15:17534666211049738. doi: 10.1177/17534666211049738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Achakulwisut P, Brauer M, Hystad P, Anenberg SC. Global, national, and urban burdens of paediatric asthma incidence attributable to ambient NO2 pollution: estimates from global datasets. Lancet Planet Health. 2019;3:e166–e178. doi: 10.1016/S2542-5196(19)30046-4. [DOI] [PubMed] [Google Scholar]
- 15.Liu J, Yuan M, Chen Y, Wang Y, Wang Q, Zhang Q, et al. Global burden of asthma associated with high body mass index from 1990 to 2019. Ann Allergy Asthma Immunol. 2022;129:720–730.e8. doi: 10.1016/j.anai.2022.08.013. [DOI] [PubMed] [Google Scholar]
- 16.Zhang D, Zheng J. The burden of childhood asthma by age group, 1990-2019: a systematic analysis of Global Burden of Disease 2019 data. Front Pediatr. 2022;10:823399. doi: 10.3389/fped.2022.823399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 18.Dong Y, Shi O, Zeng Q, Lu X, Wang W, Li Y, et al. Leukemia incidence trends at the global, regional, and national level between 1990 and 2017. Exp Hematol Oncol. 2020;9:14. doi: 10.1186/s40164-020-00170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ouyang G, Pan G, Liu Q, Wu Y, Liu Z, Lu W, et al. The global, regional, and national burden of pancreatitis in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. BMC Med. 2020;18:388. doi: 10.1186/s12916-020-01859-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Institute for Health Metrics and Evaluation (IHME) Global Burden of Disease Study 2017 (GBD 2017) socio-demographic index (SDI) 1950–2017 [Internet] Seattle (WA): IHME; 2022. [cited 2022 Jun 26]. Available from: https://ghdx.healthdata.org/record/ihme-data/gbd-2017-socio-demographic-index-sdi-1950%E2%80%932017. [Google Scholar]
- 21.Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, et al. The trends in incidence of primary liver cancer caused by specific etiologies: Results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70:674–683. doi: 10.1016/j.jhep.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Environmental Protection Agency. Children are not little adults! [Internet] Washington, D.C.: Environmental Protection Agency; 2014. [cited 2022 Jun 26]. Available from: https://www.epa.gov/children/children-are-not-little-adults. [Google Scholar]
- 23.Honkamäki J, Hisinger-Mölkänen H, Ilmarinen P, Piirilä P, Tuomisto LE, Andersén H, et al. Age- and gender-specific incidence of new asthma diagnosis from childhood to late adulthood. Respir Med. 2019;154:56–62. doi: 10.1016/j.rmed.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Hedman L, Bjerg A, Lundbäck B, Rönmark E. Conventional epidemiology underestimates the incidence of asthma and wheeze-a longitudinal population-based study among teenagers. Clin Transl Allergy. 2012;2:1. doi: 10.1186/2045-7022-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersson M, Hedman L, Bjerg A, Forsberg B, Lundbäck B, Rönmark E. Remission and persistence of asthma followed from 7 to 19 years of age. Pediatrics. 2013;132:e435–e442. doi: 10.1542/peds.2013-0741. [DOI] [PubMed] [Google Scholar]
- 26.Triebner K, Johannessen A, Puggini L, Benediktsdóttir B, Bertelsen RJ, Bifulco E, et al. Menopause as a predictor of new-onset asthma: a longitudinal Northern European population study. J Allergy Clin Immunol. 2016;137:50–57.e6. doi: 10.1016/j.jaci.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 27.Yasobant S. Comprehensive public health action for our aging world: the quintessence of public health policy. J Int Med Res. 2018;46:555–556. doi: 10.1177/0300060517718452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.United Nations. World Population Prospects - population division [Internet] New York (NY): United Nations; 2022. [cited 2022 Dec 4]. Available from: https://population.un.org/wpp/ [Google Scholar]
- 29.Tuomisto LE, Ilmarinen P, Kankaanranta H. Prognosis of new-onset asthma diagnosed at adult age. Respir Med. 2015;109:944–954. doi: 10.1016/j.rmed.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 30.Rönmark E, Lindberg A, Watson L, Lundbäck B. Outcome and severity of adult onset asthma--report from the obstructive lung disease in northern Sweden studies (OLIN) Respir Med. 2007;101:2370–2377. doi: 10.1016/j.rmed.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 31.King MJ, Hanania NA. Asthma in the elderly: current knowledge and future directions. Curr Opin Pulm Med. 2010;16:55–59. doi: 10.1097/MCP.0b013e328333acb0. [DOI] [PubMed] [Google Scholar]
- 32.Iwanaga T, Sano H, Tohda Y. The current state and provisions for elderly patients with asthma. J Gen Fam Med. 2017;18:102–107. doi: 10.1002/jgf2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brehm JM, Acosta-Pérez E, Klei L, Roeder K, Barmada MM, Boutaoui N, et al. African ancestry and lung function in Puerto Rican children. J Allergy Clin Immunol. 2012;129:1484–1490.e6. doi: 10.1016/j.jaci.2012.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shen KI, Zhao J. Exploration of China children’s asthma action plan. Zhonghua Shiyong Erke Linchuang Zazhi. 2017;32:241–244. [Google Scholar]
- 35.Centers for Disease Control and Prevention (CDC) POLARIS. U.S. Department of Health and Human Services [Internet] Atlanta (GA): Centers for Disease Control and Prevention; 2019. [cited 2022 Jun 26]. Available from: https://www.cdc.gov/policy/polaris/index.html. [Google Scholar]
- 36.Pate CA, Zahran HS, Qin X, Johnson C, Hummelman E, Malilay J. Asthma Surveillance - United States, 2006-2018. MMWR Surveill Summ. 2021;70:1–32. doi: 10.15585/mmwr.ss7005a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stein MM, Thompson EE, Schoettler N, Helling BA, Magnaye KM, Stanhope C, et al. A decade of research on the 17q12-21 asthma locus: piecing together the puzzle. J Allergy Clin Immunol. 2018;142:749–764.e3. doi: 10.1016/j.jaci.2017.12.974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim KW, Ober C. Lessons learned from GWAS of asthma. Allergy Asthma Immunol Res. 2019;11:170–187. doi: 10.4168/aair.2019.11.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5:691–706. doi: 10.1016/S2213-2600(17)30293-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soto-Martínez ME, Soto-Quiros ME, Custovic A. Childhood asthma: low and middle-income countries perspective. Acta Med Acad. 2020;49:181–190. doi: 10.5644/ama2006-124.296. [DOI] [PubMed] [Google Scholar]
- 41.Cloutier MM, Dixon AE, Krishnan JA, Lemanske RF, Jr, Pace W, Schatz M. Managing asthma in adolescents and adults: 2020 asthma guideline update from the National Asthma Education and Prevention Program. JAMA. 2020;324:2301–2317. doi: 10.1001/jama.2020.21974. [DOI] [PubMed] [Google Scholar]
- 42.Li X, Cao X, Guo M, Xie M, Liu X. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: systematic analysis for the Global Burden of Disease Study 2017. BMJ. 2020;368:m234. doi: 10.1136/bmj.m234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teague WG. Up in smoke: accelerated loss of lung function in two clusters of smokers identified in a longitudinal cohort study of adult-onset asthma. J Allergy Clin Immunol Pract. 2017;5:979–980. doi: 10.1016/j.jaip.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 44.Guo Y, Moon JY, Laurie CC, North KE, Sanchez-Johnsen LA, Davis S, et al. Genetic predisposition to obesity is associated with asthma in US Hispanics/Latinos: results from the Hispanic Community Health Study/Study of Latinos. Allergy. 2018;73:1547–1550. doi: 10.1111/all.13450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Polinski KJ, Liu J, Boghossian NS, McLain AC. Maternal obesity, gestational weight gain, and asthma in offspring. Prev Chronic Dis. 2017;14:E109. doi: 10.5888/pcd14.170196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141:1169–1179. doi: 10.1016/j.jaci.2018.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389:1885–1906. doi: 10.1016/S0140-6736(17)30819-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet. 2021;397:2337–2360. doi: 10.1016/S0140-6736(21)01169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Global death burden of asthma in 204 countries or territories. (A) Absolute number of asthma deaths in 2019. (B) ASDR (per 100,000 persons) of asthma in 2019. (C) Estimated annual percentage change of asthma ASDRs between 1990 and 2019.
Global DALY burden of asthma in 204 countries or territories. (A) Absolute number of asthma DALYs in 2019. (B) Age-standardized DALY rate (per 100,000 persons) of asthma in 2019. (C) Estimated annual percentage change of asthma age-standardized DALY rate between 1990 and 2019.
Trends of the incidence, death, and DALY rates (per 100,000 persons) among different age groups between 1990 and 2019.
Proportion of deaths/DALYs attributable to 3 risk factors in 21 Global Burden of Disease regions in 1990 and 2019. Blue bars represent male individuals, and red bars represent female individuals; light bars represent 1990, and dark bars represent 2019.
Proportions of deaths/DALYs attributable to 3 risk factors in different age groups in 1990 and 2019. Blue bars represent male individuals, and red bars represent female individuals; light bars represent 1990, and dark bars represent 2019.
Correlation analyses of the proportions of 3 risk factors attributable to deaths/DALYs-SDI (2019). (A) Smoking attributable to deaths-SDI (2019) and (D) smoking attributable to DALYs-SDI (2019). (B) High body-mass index attributable to deaths-SDI (2019) and (E) high body-mass index attributable to DALYs-SDI (2019). (C) Occupational asthmagens attributable to deaths-SDI (2019) and (F) occupational asthmagens attributable to DALYs-SDI (2019). The size of the circle represents the quantity of asthmatic patients in a single country or territory.