Abstract
Introduction
In Uganda, 2% of women die from maternal causes with a mortality rate of 336 maternal deaths per 100,000 live births. According to the World Health Organization Uganda is one of the top three contributors to maternal mortality in sub-Saharan Africa. Uganda has parallel weak ambulance systems, government, and non-government-owned, that transport obstetric emergencies to higher-level facilities. These two operations lack standards of medical care and inter-facility transfer (IFT) protocols to direct care. Limited studies exist which assess the state of Emergency Care Services in Uganda and none has been performed to assess the ambulance referral services utilized to address obstetric emergencies.
Objective
The present study was performed to describe the ambulance transfer processes of obstetric emergencies by analyzing cases arriving at Kawempe National Referral Hospital (KNRH) from outlying health facilities
Methods
The study was based at KNRH in Kampala, Uganda. It was a descriptive and analytic cross-sectional study. Trained research assistants enrolled participating patients who met the inclusion criteria consecutively on arrival by ambulance at the hospital. Utilizing a questionnaire, quantitative data was collected from the ambulance driver, the sending facility referral form, and the receiving hospital's ambulance log book for each case. The sample size was 215.
Results
The median age was 27 years and the majority of patients were referred because of hypertensive disorders (34.9%), obstructed labor (26.5%) and hemorrhage (20.9%). The median total response time for transfer of obstetric emergencies was 50 min, from ambulance activation until the mother was received at KNRH. Differences were identified between government and non-government-owned ambulances in regards to the method of activation, medical escort staffing, number of vital signs recorded, and ambulance onboard medical care. Ambulances parked at the facility took the shortest transfer time and EMT-supported ambulances had the greatest number of vital signs taken.
Conclusions
Recommendations are to develop an integrated ambulance system for both government and non-government ambulances with standards especially in regards to standardized scripted call-center calls analysis, dispatch activation time, response-to-patient time, and trained ambulance professional staffing and medical care whenever in patient transport mode.
Keywords: Obstetric emergencies, Ambulance, Transfer, Kawempe National Referral Hospita, Uganda
African Relevance
-
•
The first study in Uganda to document the maternal IFT process within the ambulance.
-
•
Results of the study reveal the lack of timely access to specialized care, hence inspiring comparison to the three-delay model which could serve as a standard that is relevant in reducing pregnancy-related mortality.
-
•
The results of this obstetrics emergency study can form the basis of policy development on ambulance emergency care services across the spectrum of disease and injury.
Introduction
Approximately 15% of all women of childbearing age develop complications in pregnancy, childbirth, and post-partum that can become life-threatening if they are not managed quickly and properly [1]. About 280,000 women, almost all in Low- and Middle-Income Countries (LMICs), die annually during pregnancy and childbirth yet most of these deaths could be prevented [1]. Obstetric emergencies, namely hemorrhage, hypertensive disorders, and sepsis, lead to at least half of maternal deaths globally, yet they are treatable [2].
In Sub-Saharan Africa, maternal mortality estimates are as high as 546 per 100,000 live births.
In Uganda, the maternal mortality rate is 336 maternal deaths per 100,000 live births and many women die from pregnancy and childbirth-related complications which can be reduced by better access to care [3].
Emergency care services are undergoing rapid development on the African continent with training programs for different health professional cadres and ambulance services being developed however challenges still exist like lack of governmental leadership, poor system and facility organization, resource limitations, staffing, and lack of community understanding of emergency medical services (EMS).
Ambulance services exist in one-third of African countries with injury and obstetric complaints most common in regards to their utilization, however, many low-income countries lack the basics of a functional system especially regarding IFT protocols, standards for ambulance care, and trained personnel to take care of emergencies [4]. Emergency care services are important to improving the quality of life in critically ill patients but this is dependent on timely interventions with the appropriate equipment and drugs, available to skilled credentialed medical professionals responding to alerts as early as possible [5].
A significant association exists between the timing of emergency obstetric care implementation and adverse maternal and fetal outcomes with complications of pregnancy including fetal and maternal deaths which be reduced by a functional ambulance system that enhances the impact of health service interventions through early recognition of severe conditions and immediate access to the right care [6]. This should be the responsibility of a well-organized call center, asking mandated, medically approved, standardized, scripted questions of callers, then delivering clear standardized scripted instructions to callers. A timely response is important when managing emergencies as chances of survival increase when care is given within the shortest period. And the first point-of-patient contact with medical professionals should be a professionally staffed call center, through which all maternal emergency requests should be mandatorily made, with the subsequent immediate dispatch of transport-capable response professionals to the patient. This can be achieved if access to specialized medical care is done promptly via ambulance transfers. In Uganda according to the National Emergency Medical Services Strategic Plan 2021–2025, ambulance transfers are both government and non-government owned and emphasis has been put at the National level to improve prehospital emergency care services.
In Uganda, the hospital-based medical care delivery system is organized into several levels: national referral hospitals, district hospitals, and health centers. Patients are referred to Kawempe National Referral Hospital (KNRH) to receive comprehensive care and specialized obstetric care.
These women qualifying for the present study arrive at KNRH by ambulance, however, no known data exists that documents medical care during this transfer process.
Limited studies addressing the state of emergency care services in Uganda exist, but none assess the obstetric emergencies at the earliest point, by documenting and analyzing the maternal IFT referral and ambulance transfer system.
The general objective of the study was to describe the transfer process of patients with obstetric emergencies arriving by ambulance to Kawempe National Referral Hospital. The ambulance IFT process for obstetric emergencies, with KNRH as the sole destination, is described through data collection, classification, and subsequent formation of tables. The accessible component data from the foregoing processes are analyzed in an attempt to form recommendations for the improvement of care.
Methods
Study design
A descriptive cross-sectional the study design was used. Data sources involved self-reports by the ambulance drivers, review of hospital-based intake ambulance logbooks, and sending facility referral forms (See Fig. 4) collected upon patient arrival at KNRH.
Fig. 4.
A sample referral form designed for patient referrals to KNRH.
Study setting
The study was conducted at KNRH in Kampala, Uganda.
Study population
The study population comprised all pregnant women of at least 18 years and with obstetric emergencies above 28 weeks’ gestation who arrived in an ambulance at KNRH from the greater Kampala metropolitan area during the study period and for whom written consent was obtained. All ambulance drivers transporting these obstetric emergency patients became sources of study data.
The inclusion criteria included all adult (18 years and older) pregnant women above 28 weeks with obstetric emergencies arriving by ambulance to KNRH from the Greater Kampala metropolitan area and their ambulance drivers during the study period who gave consent to participate in the study
The study excluded ambulance drivers who were transporting patients with obstetric emergencies arriving at KNRH from outside Greater Kampala metropolitan area. and pregnant women above 28 weeks with obstetric emergencies who arrived dead or died on arrival at KNRH, as determined by receiving doctor.
Study variables
The dependent study variable was the transfer process of the patient with the obstetric emergency while the independent study variables were those components related to the transfer process of the patient with an obstetric emergency transferred by ambulance to KNRH. These included ambulance response time, ambulance ownership, distance traveled to respond to patient and transport distance, certification of ambulance staff on board to medically escort the mother, maternal age, parity, gravidity, ethnicity, referring facility, and reasons for referral (See Table 2).
Table 2.
Characteristics of the ambulance transfer process of obstetric emergencies to KNRH.
| Characteristic | Measure | |
|---|---|---|
| Median Total response time, minutes | 50 (35–67) | |
| Median transfer time, minutes | 40 (25–45) | |
| Median Activation time, minutes | 20 (0–25) | |
| Median distance, kilometres | 9 [7], [8], [9], [10], [11], [12], [13] | |
| Health facility, n (%) | Government Non-government |
191 (88.8) 24 (11.2) |
| Number of vital taken, n (%) | 0 1 2 3 4 |
162 (75.4) 28 (13.0) 11 (5.1) 12 (5.6) 2 (0.9) |
| Distance travelled by ambulance, n (%) | <7 km 7–13 km >13 km |
49 (22.8) 120 (55.8) 46 (21.4) |
| Total response time, n (%) | <35 min 35–67 min >67 min |
48 (22.3) 114 (53.0) 53 (24.7) |
| Referral form, n (%) | Present Absent |
95 (44.2) 120 (55.8) |
| Staff on board, n (%) | Present Absent |
111 (51.6) 104 (48.4) |
| Ambulance ownership, n (%) | Government Non-government |
158 (73.5) 57 (26.5) |
| Ambulance activation, n (%) | Phone call to the driver Call center At the facility |
133 (61.9) 15 (6.9) 67 (31.2) |
| Cadre of staff, n (%) | No staff Doctor Nurse EMT Unspecified |
104 (48.3) 2 (0.9) 95 (44.2) 13 (6.1) 1 (0.5) |
Sample size calculation
The sample size was calculated using Kish Leslie's (1965) formula.
Where N was the estimated sample size, Z1 − α/2 at a 5% level of significance was 1.96, p (50%) was the proportion that gives the maximum sample size and d was precision (the tolerable sampling error) of 0.05 at 5% level of significance. The estimated minimum sample size for objective 2 was 385. Therefore, the estimated sample size for this study was 385
Sample size adjustment
Using a study by Akii Bua [22] that showed there are 162 patients with obstetric emergencies were transported by ambulances to Kawempe National Referral Hospital per month.
The sample size was scaled down using:
S = N/(1 + N/Population size)
Where N was the sample size of 385 calculated
Population size in 3 months of the study was given by 162×3 = 486
The sample size was then estimated at 215 after scaling down.
Study procedure
Consecutive sampling was used to select obstetric emergencies that arrived at KNRH by ambulance, met the inclusion criteria, and consented to take part in the study.
Study participants were recruited on arrival at KNRH based on the inclusion criteria. The principal investigator and trained research assistants then obtained consent from the study participants. The study participants were mothers arriving by ambulance with an obstetric emergency, however, because of the critical status in which some arrived, the mother had to be resuscitated by the admitting clinician. In these cases, the attendant (an individual above 18 years looking after a given patient) then consented on behalf of the mother to get information about the transfer process in the ambulance. The second research assistant would then get consent from the ambulance driver and use the pretested questionnaire (Supplementary file 1). The ambulance driver provided information about the transfer process. The questionnaire was also completed by getting more information from the referral note and ambulance driver logbook.
Data quality assurance
Prospective quality assurance (Q/A) was performed by training research assistants and rehearsal of the tasks including objectives and procedure of the study, how to use the data collection tool, consent process, data storage, and role-play before beginning data collection. The questionnaire was pretested before beginning the study on 5% of the sample size using an external population. Questionnaires were checked for completeness and correctness. Weekly meetings were conducted to review the challenges, performance, and progress. Concurrent Q/A was conducted when data was entered into Epidata (version 4.2) software by two entrants and the Epidata form was designed with in-built checks (must enter). Data was also cleaned before being exported to Stata 14.0 for analysis. The data extraction process was done by two independent researchers who are emergency medical personnel with experience in dealing with obstetric emergencies. In case of any inconsistences, the original data collection form was sought for clarification.
Data analysis
As a retrospective quality assurance, quantitative data were analyzed using Stata (version 14) software. Descriptive characteristics were presented using frequencies and percentages or proportions in tables, graphs, and charts. Numerical data were summarized using means and standard deviations for normally distributed continuous data or medians and interquartile ranges for continuous but skewed variables.
Results
Study enrollment
From December 2021 to January 2022 three hundred and eighty (380) women with emergencies arrived at KNRH by ambulance. One hundred and sixty-five (165) were excluded due to different reasons. Two hundred and fifteen (215) women with obstetric emergencies met the inclusion criteria and consented to participate in the study as described below (see Fig. 1).
Fig. 1.
Study profile diagram.
Baseline characteristics
Of the 215 patients who were enrolled in the study, the median age was 27 (24–31) years with 40.9% of the participants being between the ages of 25–29 (Table 1). The number of obstetric emergencies representing the median age was 116 (55.9%). The median gestational age was 35 (33–36) weeks with 55.8% being ≥35 weeks pregnant. The number of obstetrics emergencies representing the median gestation age was 117 (54.4%).
Table 1.
Baseline characteristics of patients enrolled in the study.
| Characteristic | Measure | |
|---|---|---|
| Median age, years | 27 (24–31) | |
| Median gestation age, weeks | 35 (33–36) | |
| District of residence, n (%) | Kampala Wakiso Mukono Butamabala Mpigi Gomba |
128 (59.5) 69 (32.0) 11 (5.12) 3 (1.4) 3 (1.4) 1 (0.5) |
| Parity, n (%) | Nulliparous Para 2–4 Para ≥5 |
25 (11.6) 187 (87.0) 3 (1.4) |
| Gravida, n (%) | Primigravida Gravida 2–4 Gravida ≥5 |
25 (11.6) 180 (83.7) 10 (4.7) |
| Ethnicity, n (%) | Baganda Nilotes Eastern Bantu Western Bantu Others |
64 (29.8) 30 (13.9) 32 (14.9) 74 (34.4) 15 (7.0) |
| Gestational age, n (%) | 20–27 28–34 ≥35 |
1 (0.5) 94 (43.7) 116 (55.8) |
| Age, n (%) | ≤19 20–24 25–29 30–34 ≥35 |
6 (2.8) 58 (27.0) 88 (40.9) 15 (7.0) 48 (22.3) |
Prevalence of different obstetric emergencies that arrive by ambulance at KNRH
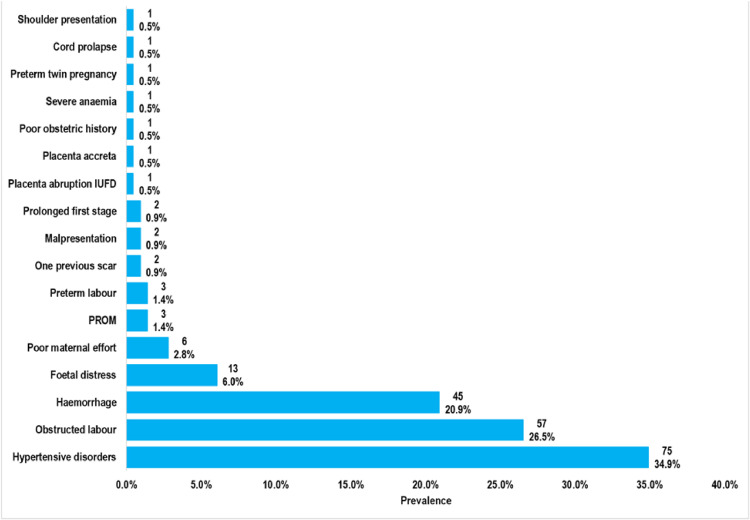
The prevalence of different obstetric emergencies that arrive by ambulance to KNRH was as follows. The biggest reasons for referral were hypertensive disorders (34.9%), followed by obstructed labor (26.5%), and thirdly, hemorrhage (20.9%) as shown in Fig. 2.
Fig. 2.
Prevalence of different obstetric emergencies that arrived by ambulance at KNRH.
Transfer process of obstetric emergencies that arrive by ambulance to KNRH
The median total patient transport time taken for the transfer of patients with obstetric emergencies was 50 min, with mm moo the referrals being in the range of 35–67 mInutes (53%) even though the median distance travelled was 9 km with most ambulances travelling 7–13 km, (55.8%) from the referring facility to KNRH (See Table 2).
Activation time refers to the period from receipt of a call to the arrival of the Ambulance at the referring facility.
Transfer time refers to the time from the arrival of the ambulance to the referring facility where the patient is loaded to the time the ambulance arrives at KNRH.
Total response time refers to the sum of the activation and transfer time.
Description of ambulance and activation process
The study showed that the majority of government facilities activated the ambulances by a phone call to the driver (68.6%) compared to the non-government facilities which hadmm moof the ambulances parked at the facility (91.7%).
Ambulance transfer time and distance traveled
The study showed that most ambulances took a total response time of fewer than 35 min. The majority of these were ambulances parked at the sending/referral facility (61.2%). Majority of the ambulances recording the shortest transfer times were ambulances from non-government facilities (75%).
Distance travelled
Majority of government ambulances (60.2%) traveled between 7 and 13 km to reach KNRH while the majority of non-government ambulances (45.8%) traveled more than 13 km.
Ambulance medical care
The majority of government ambulances (63.3%) did not have medical staff on board compared to
93% of the non-government which had staff on board.
The study revealed that 27.9% of government ambulances had nurses as medical escorts compared to non-government ambulances which had 89.4% with a nurse as a medical escort.
The Majority of ambulances (92.3%) that had Emergency Medical Technician (EMT) staff on board had three different types of vital signs taken compared to the ones which had nurses on board that had a majority (60%) without any vital signs taken (see Fig. 3).
Fig. 3.
Number of vitals taken by different cadres.
Discussion
This study set out with the aim of describing the transfer process of patients with obstetric emergencies arriving by ambulance to Kawempe National Referral Hospital.
Our study showed that the majority of obstetric emergencies were transferred to KNRH by government-owned compared to the non-government-owned ambulances. Surprisingly, there was no uniform approach or standards followed by both types of ambulances despite recent advancements in the provision of emergency care including the launch of the EMS policy. This finding corroborates the findings of Ningwa and colleagues in 2018 [5] which showed that Uganda had a poor referral coordination at both national and sub-national levels.
Our study showed that pregnant women with parity between two and four were most likely to get an obstetric emergency from lower-level facilities requiring specialized intervention. This finding does not match the findings of a study done at Mulago hospital by Kaye et al. looking at maternal mortality and associated near-misses among emergency intrapartum obstetric referrals in Mulago hospital showed that the majority of patients referred were primigravid patients [7]. However, this finding is similar to that of a study done in Nigeria looking at obstetric emergencies in rural hospitals by Ntoimo and friends showed that the majority were multiparous (parity 2–4) [8]. Another study done in India that looked at the obstetric emergencies at a rural hospital done by Catherin and colleagues showed that the mean maternal age was 30±2 years with the parity ranging from zero to four with mean of one [9].
Our study found that the majority of patients were referred because of hypertensive disorders (34.9%), obstructed labor (26.5%), and hemorrhage (20.9%). This is in line with a similar study done at Mulago hospital by Kaye et al. [7], which had similar reasons for referral. A systematic review done by Musarandega and colleagues showed that the leading cause of maternal mortality in sub-Saharan Africa was hemorrhage, followed by hypertensive disorders [10]. This finding is in agreement with another study conducted in Ethiopia by Menbeu and friends looking at the epidemiology of patients utilizing ambulances in Addis Ababa, which reported that obstetric emergencies were transferred between facilities using ambulances, with prolonged labor being the most common reason for referral [11]. Uganda is ranked among the top countries which contribute to the maternal and newborn mortality rate in the world [12]. Obstetric complications such as sepsis, hemorrhage, hypertensive disorders, and obstructed labor are the major causes of maternal mortality. Particularly central to this problem is the current health worker gap, especially among midwives at community-level health centers, to deliver a range of life-saving interventions [13]. This could explain why this study showed that low-level facilities referred patients mainly for hemorrhage, obstructed labor, and hypertensive disorders There is a notable gap in the management of these conditions at lower-level facilities.
It is encouraging to compare challenges in the transfer process for obstetric emergencies by an ambulance arriving at KNRH from lower-level facilities which our study identified with finds of other prior studies conducted in Ghana on emergency obstetric cases in primary health facilities [14] and in Ethiopia [15]. The major challenges identified in this study included long transfer times, lack of appropriate medical escort with poor monitoring during transit, and different standards in ambulance activation criteria. Timely access to specialized care for women with obstetric complications is recognized as being essential to reducing maternal mortality [16]. Ensuring that an effective referral system is in place to help achieve timely access to specialized care fits within the framework of the minimal initial services package for reproductive health [17].
The Government of Uganda, through the department of EMS, has established regional call centers where a government ambulance can be dispatched to respond to an emergency. However, this study has shown that the government facilities preferred to activate the government ambulances by directly calling the driver's phone instead of the call center. Also, none of the non-government facilities activated any ambulance through the call center. Similar findings were found in a study done in Kenya which showed that health facilities preferred to call the driver's mobile phone to activate ambulances compared to the existing call center system [18].
The study showed that the median total response time taken for the transfer of patients with obstetric emergencies was 50 min, with most of the referrals being in the range of 35 to 67 min. The response time for ambulances is an important quality of ambulance care for time-sensitive emergency conditions. Despite our study not measuring the average time taken for an ambulance to reach a scene from dispatch, a similar study done in Ethiopia by, Menbeu et al. [11] showed that ambulances generally spend more than nine minutes to reach a scene. However, research has shown that in trauma patients the mortality risk for patients with an ambulance response time of more than five minutes is three times higher than those of less than five minutes [19]. The estimated effect of a one-minute reduction in response time shows improved odds of survival by 24% [20].
Our study also showed that ambulances parked at the facility took the shortest transfer time, followed by those that are activated through the call center. Worldwide, there is no consensus on what the minimum transfer time should be for patients in an ambulance. Even though the WHO Emergency care framework includes transport and transfer of patients, it does not state how long this transportation should take. There is limited available data as well as guidelines on transfer time. A common benchmark response time in high-income settings has been recommended to be less than eight minutes in trauma patients [21]. This can be related to our study because of the lack of sufficient evidence on specific ambulance responses for the different patient groups.
Our study also showed that there were different cadres of staff on board for both types of ambulances. Also, the number of vital signs taken differed depending on which cadre of staff was on board the ambulance. It is important to note that EMT-supported ambulances which are directly supervised by the Ministry of Health, had the greatest number of vital signs taken. Could this be because the EMT staff are on ambulances with equipment or because they are better trained in prehospital care and therefore appreciate the importance of taking vital signs of patients even when in the ambulance? Transporting patients during emergency transfers in ambulances helps to ensure continuity of care as emergency medical technicians can monitor and provide necessary first aid to help stabilize patients’ conditions before they arrive at the referred facilities.
Strength and limitations of the study
Strengths
-
•
The first study in Uganda to document the transfer process within the ambulance.
-
•
Large sample size
-
•
The study design allowed the collection of multiple variables.
-
•
Information from multiple centres referring to KNRH.
Limitations
There was inadequate data from the referring facility in the referral note. Data on specific interventions done from the referral facility, delay in deciding to transfer the patient, the quality of care, and the level of skill of the referring clinicians were not collected. This data could potentially affect the patient's emergent condition. Additionally, the study only focused on the receiver end of the referral system and to have a comprehensive view of the challenges of the entire system it will be prudent to involve referring facilities.
This study was carried out at a single facility in Uganda. Therefore, there is need to look at other specialised facilities around the country to get more comprehensive data. There was a potential for information bias due to recall and self-reported review of the ambulance transfer process, limited data from the mother such as antenatal history, and obstetric history.
Information from self-reports was verified with observation and visual confirmation by research assistants to reduce information bias.
Conclusion
This study offers an introduction to ambulance transfers which is a critical component of EMS systems in Uganda There is limited research in the area of emergency medical services but this study raises important clinical, operational, and public health questions based on how this transportation occurs. The questions raised about this process from this study create an opportunity to benchmark developing systems that will improve ambulance services for all emergencies. The transfer process of patients with obstetric emergencies does not have standards and lacks protocols. The ambulance call center was not utilized by non-government facilities. There was generally poor monitoring and documentation of vital signs for patients transported by ambulance. EMT-supported ambulances, which are directly supervised by the Ministry of Health, had better monitoring and documentation of vital signs for patients. Therefore, this study creates an opportunity to benchmark developing systems that will improve ambulance services for all emergencies.
Recommendations
-
1.
There is a need for the Ministry of Health to develop an integrated functional system for all ambulances with standards to streamline the referral process, especially regarding activation, response time, staffing, and medical care while in transit.
-
2.
The Uganda clinical guidelines should be updated by ministry of health to cater for an ambulance obstetric referral protocol to ensure adequate medical care while in the ambulance.
-
3.
There should be follow up studies to identify the outcomes in patients with obstetric emergencies that arrive by ambulance to tertiary hospitals. This will help in assessing the impact of ambulance transfer on perinatal morbidity and mortality. Studies should be done to determine the reasons for long response time and the outcomes of different response times on the mother and the baby.
Ethical considerations
Ethical Approval was sought from School of Medicine Research and Ethics Committee (SOMREC) of Makerere University. Permission to do the study was sought from the Makerere University Department of Anesthesia Critical care and Emergency medicine. Consent was obtained from caregivers of the mother, and the ambulance staff. Administrative permission was sought from Kawempe National Referral Hospital research ethics committees. All data was given unique codes and kept in a safe place that was only accessible to the research team. The study protected the privacy of the patients by using unique identifiers in the documentation and ensuring that the information collected was only accessible to the research team.
Consent for publication
Not applicable.
Dissemination of results
Results from this study will be shared with the Department of Anesthesia Critical Care and Emergency Medicine, and staff members at the Department of Emergency Medical Services, Ministry of Health of Uganda. The results will also be included in the department's annual report to the senior top management at the Ministry of Health of Uganda. Results from this research study will also be shared with staff members at the data collection site through an informal presentation.
Authors’ contribution
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: ODA contributed 60%; PKA 15%; AK 15%; JK 10%; KJ and MSN contribute 5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Data availability statement
Minimal dataset is available within the paper. Additional data is available upon reasonable requests from the corresponding author.
Declaration of Competing Interests
The authors declared no conflicts of interest.
Acknowledgments
Acknowledgments
We would like to thank the administration of Kawempe National Referral hospital, our study participants, and research assistants for making this study a success. We also would like to acknowledge the scientific, review committee at the Department of Anesthesia, Critical Care and Emergency Medicine, Makerere University, College of Health Sciences for critiquing and refining the initial research idea and making it more feasible and clinically relevant.
Funding
This work was not funded.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.afjem.2023.06.003.
Appendix. Supplementary materials
References
- 1.UNFPA. Urgent response: providing emergency obstetric and newborn care. Updated with technical feedback. 2012.
- 2.Getiye Y., Fantahun M. Factors associated with perinatal mortality among public health deliveries in Addis Ababa, Ethiopia, an unmatched case control study. BMC Pregnancy Childbirth. 2017;17(1):1–7. doi: 10.1186/s12884-017-1420-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babughirana G., Gerards S., Mokori A., Nangosha E., Kremers S., Gubbels J. Maternal and newborn healthcare practices: assessment of the uptake of lifesaving services in Hoima District, Uganda. BMC Pregnancy Childbirth [Internet] 2020;20(1):686. doi: 10.1186/s12884-020-03385-x. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WORLD BANK . 2017. Disease Control Priorities: Improving Health and Reducing Poverty. [PubMed] [Google Scholar]
- 5.Ningwa A., Muni K., Oporia F., Kalanzi J., Zziwa E.B., Biribawa C., et al. The state of emergency medical services and acute health facility care in Uganda: findings from a National Cross-Sectional Survey. BMC Health Serv Res. 2020;20(1):1–10. doi: 10.1186/s12913-020-05508-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Humphreys G. Improving emergency care in Uganda. World Health Organ Bull World Health Organ. 2019;97(5):314–315. doi: 10.2471/BLT.19.020519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaye D., Mirembe F., Aziga F., Namulema B. Maternal mortality and associated near-misses among emergency intrapartum obstetric referrals in Mulago Hospital, Kampala, Uganda. East Afr Med J. 2003;80(3):144–149. doi: 10.4314/eamj.v80i3.8684. [DOI] [PubMed] [Google Scholar]
- 8.Ntoimo L.F., Okonofua F.E., Ogu R.N., Galadanci H.S., Gana M., Okike O.N., et al. Prevalence and risk factors for maternal mortality in referral hospitals in Nigeria: a multicenter study. Int J Womens Health. 2018;10:69. doi: 10.2147/IJWH.S151784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Catherin N., Anushila S., Goud B.R. Obstetric emergencies presenting to a rural community maternity hospital, Southern Karnataka, India. Int J Curr Res Aca Rev. 2014;2(9):264–269. [Google Scholar]
- 10.Musarandega R., Nyakura M., Machekano R., Pattinson R., Munjanja S.P. Causes of maternal mortality in sub-Saharan Africa: a systematic review of studies published from 2015 to 2020. J Glob Health. 2021:11. doi: 10.7189/jogh.11.04048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sultan M., Abebe Y., Tsadik A.W., Jennings C.A., Mould-Millman NK. Epidemiology of ambulance utilized patients in Addis Ababa, Ethiopia. BMC Health Serv Res [Internet] 2018;18(1):997. doi: 10.1186/s12913-018-3820-4. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO . WHO; Geneva, Switzerland: 2021. World Health Statistics 2021: monitoring health for the SDGs, sustainable development goals. [Internet] Available from. [Google Scholar]
- 13.WHO . WHO; Geneva, Switzerland: 2011. Maternal and child health: Uganda. [Internet] Available from. [Google Scholar]
- 14.Afari H., Hirschhorn L.R., Michaelis A., Barker P., Sodzi-Tettey S. Quality improvement in emergency obstetric referrals: qualitative study of provider perspectives in Assin North district, Ghana. BMJ Open [Internet] 2014;4(5) doi: 10.1136/bmjopen-2014-005052. https://bmjopen.bmj.com/content/4/5/e005052 [cited 2022 Oct 2]Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Austin A., Gulema H., Belizan M., Colaci D.S., Kendall T., Tebeka M., et al. Barriers to providing quality emergency obstetric care in Addis Ababa, Ethiopia: healthcare providers’ perspectives on training, referrals and supervision, a mixed methods study. BMC Pregnancy Childbirth [Internet]. 2015;15(1):74. doi: 10.1186/s12884-015-0493-4. [cited 2022 Oct 2]Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paxton A., Maine D., Freedman L., Fry D., Lobis S. The evidence for emergency obstetric care. Int J Gynecol Obstet. 2005;88(2):181–193. doi: 10.1016/j.ijgo.2004.11.026. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization . 2010. Inter-agency field manual on reproductive health in humanitarian settings. [PubMed] [Google Scholar]
- 18.Kalisa R., Muriithi M.K., Bijlmakers L., van den Akker T., van Roosmalen J. 2020. Cost-effectiveness of emergency obstetric care in rural Kenya: comparing ambulance transfer and self-referral. [Google Scholar]
- 19.Blackwell T.H., Kaufman J.S. Response time effectiveness: comparison of response time and survival in an urban emergency medical services system. Acad Emerg Med. 2002;9(4):288–295. doi: 10.1111/j.1553-2712.2002.tb01321.x. [DOI] [PubMed] [Google Scholar]
- 20.O'Keeffe C., Nicholl J., Turner J., Goodacre S. Role of ambulance response times in the survival of patients with out-of-hospital cardiac arrest. Emerg Med J. 2011;28(8):703–706. doi: 10.1136/emj.2009.086363. [DOI] [PubMed] [Google Scholar]
- 21.Pons P.T., Markovchick V.J. Eight minutes or less: does the ambulance response time guideline impact trauma patient outcome? J Emerg Med. 2002;23(1):43–48. doi: 10.1016/s0736-4679(02)00460-2. [DOI] [PubMed] [Google Scholar]
- 22.Akii Bua D. Rapid Assessment of the current functionality of the Call & Dispatch Centre and referral system in Kampala. KCCA. 2020 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Minimal dataset is available within the paper. Additional data is available upon reasonable requests from the corresponding author.