Summary
Background
Drug overdose deaths in the USA have increased rapidly in the past 20 years, and understanding patterns and trends in mortality is essential to develop policy responses. This study aimed to determine whether cohort patterns in mortality due to drug overdose have changed in the past two decades and assess these patterns by race and sex.
Methods
The national records of accidental drug overdose death were extracted from Centers for Disease Control and Prevention, National Center for Health Statistics Mortality Data for 2000–2020. Age-period-cohort analysis was performed to examine independent effects of age, period and birth cohort on accidental drug overdose mortality.
Findings
The number of accidental drug overdose deaths increased by 622% between 2000 and 2020, and age-standardized mortality rates increased nearly four-fold in both men and women. Age-period-cohort decomposition found rapid increases in mortality since 2012 in men and women, with higher mortality risk in cohorts born after 1990. The fastest increase occurred in Black Americans since 2012, and Americans of all races born after 1975 had significantly higher mortality risk, with mortality risk increasing rapidly in more recent cohorts. The peak of mortality has shifted from the 40–59 age group to the 30–40 year age group in the past decade.
Interpretation
The burden of drug overdose mortality has shifted to younger Americans, and a new generation of Americans are at significantly higher and rapidly increasing risk of overdose death. Urgent action is needed to prevent an entire generation of young people being consigned to decades of preventable mortality.
Funding
None.
Keywords: Drug overdose, Age-period-cohort, Mortality, The USA
Research in context.
Evidence before this study
We conducted a comprehensive literature search in PubMed for English-language papers without any restrictions on publication date. We used terms "(drug overdose) AND (USA) AND (mortality) AND (age-period-cohort OR APC model)". We identified two studies that employed age-period-cohort analysis to estimate mortality trends in the US. One study focused on all-cause mortality among early and middle adulthood, while the other examined the impact of the baby boomer cohort on accidental poisoning mortality trends. However, neither of these studies systematically investigated drug overdose mortality trends by sex or race in the US population using the most recently available data, and new research is needed to build on their findings in light of the rapid growth of the opioid epidemic in the past five years.
Added value of this study
Data from the Centers for Disease Control and Prevention, National Center for Health Statistics Mortality Data on CDC WONDER was used to investigate the age, period, and cohort trends in drug overdose mortality in the USA from 2000 to 2020, disaggregating the analysis by sex and race. Our analysis showed rapidly growing mortality among both sexes and highlighted a shift in the peak of mortality rates from older to younger generations. We identified that drug overdose mortality rates in the past 10 years have risen fastest in younger Americans aged 20–40, in young men, and in Black Americans. We also provided the first age-period-cohort analysis of drug overdose mortality patterns in a highly marginalized population of American Indian and Alaska Native, using the most recently available national data.
Implications of all the available evidence
The US is experiencing an unprecedented crisis of drug-related mortality. Our study revealed that this crisis is at its most acute in vulnerable younger, non-White populations, and that there has been a generational shift in the burden of drug overdose in the past decade. Urgent actions such as significant policy reforms and an expansion of harm reduction policies will be crucial in preventing overdoses among young Americans.
Introduction
Since 2006, researchers have identified drug poisoning as a primary contributor to increasing premature mortality in the United States.1 In 2019, the age-adjusted rate of drug overdose deaths was 21.6 per 100,000 and the rate of drug overdose deaths was the highest ever for adults aged 35–44 at 40.5 deaths per 100,000.2 Between 2013 and 2019, the age-standardized rate of drug overdose deaths involving synthetic opioids increased from 1.0 to 11.4 per 100,000.2 More recently, concomitant exposure to fentanyl and stimulants has been associated with increasing numbers of overdose deaths in the United States.3,4 The age-adjusted rate of drug overdose deaths involving cocaine was 4.9 per 100,000 in 2019, which tripled from 1.4 in 2012. Between 2012 and 2019, the age-adjusted rate of drug overdose deaths involving psychostimulants such as methamphetamine, increased on average by 29% per year, resulting in a rate of 5.0 per 100,000.5 Although some studies have identified high levels of poisoning-related mortality in the 50–64 age group and debate has centered on the socio-economic factors that may be associated with increasing mortality in this age group,6 a recent report on generational effects on trends in drug-related mortality in the U.S. suggested that the early millennial cohort will see increasing overdose mortality rates, followed by a decrease in the late millennial cohort.7 Other research using age-period-cohort models has identified growing mortality in younger age groups, predicting very high peak mortality in people born after 1980,8 but did not disaggregate these findings by sex or race, and findings from earlier studies have been rendered obsolete by the rapid growth in overdose deaths. A recent study using national death registration data found rapidly increasing trends in drug overdose mortality among American Indian and Alaska Native (AIAN) Americans, driven by synthetic opioids, suggesting an urgent need to understand the age groups and birth cohorts affected by this epidemic in this highly marginalized population.9 Although the increase in drug overdose mortality has been reported since 1990,10 a comprehensive in-depth analysis of birth-cohort shifts in drug-related deaths has not been conducted, and there is little evidence about the difference in mortality patterns among races. With the rapid increase in mortality rate from drug poisoning in recent years, research needs to be updated to account for the last five years, to separate secular trends in mortality from cohort effects, and to conduct these analyses in detail by race and sex. This study aims to examine trends in drug overdose mortality in the U.S. from 2000 to 2020. We also identified cohort patterns in drug overdose mortality; isolated cohort, age and time effects; and compared these patterns by sex and race.
Methods
This study is an age-period-cohort analysis of retrospective, cross-sectional nationally representative vital registration data from the United States of America.
Data source
Data on underlying cause of death was obtained from Centers for Disease Control and Prevention, National Center for Health Statistics Mortality Data on CDC WONDER (Website: https://wonder.cdc.gov/) for 2000–2020 by single-year ages, year, gender, and race for causes of accidental drug poisoning (X40-X44), as coded in the International Classification of Diseases, 10th Revision. Ages between 15 and 84 were selected for this study. None of the data used were provisional. Institutional Review Board approval was unnecessary for this study as all data were deidentified and publicly available.
Statistical analysis
Mortality rates by single year of age for men and women were smoothed using a first-order kernel density smoother with Gaussian kernel. Smoothing was necessary in order to ensure that original values of rates were not presented in the figures, following CDC guidelines for presentation of these data. Sex specific rates for each year were standardized per 100,000 population using the 2010 single year age- and sex-specific population of 2010 as standard.
We performed age-period-cohort (APC) analysis on unsmoothed data to examine independent effects of age, period and birth cohort on drug overdose mortality using the US NCI web-based statistical tool.11 APC analysis is a frequently employed statistical method for analyzing mortality data.12,13 In this analysis, age effects pertain to the influence of an individual's chronological age on drug overdose mortality. Period effects relate to the impact of external factors that affect the entire population at a specific point in time. These factors may include changes in the illicit drug market, medical technology, public health policies, or social and economic conditions. For instance, the presence of fentanyl in the drug supply has been increasing since 2013, potentially exacerbating the surge in drug overdose mortality during that corresponding period.4 Lastly, cohort effects refer to the influence of shared experiences and exposures that are exclusive to a specific generation or birth cohort. The APC web tool offers a user-friendly approach for conducting APC analysis. The web tool employs generalized linear models and weighted least squares methods to perform APC analysis, effectively identifying patterns in mortality rates by analyzing population-level count data that follows a Poisson distribution.
The APC model produced age-specific mortality rates, period-specific relative risks reflecting time trends in mortality common to all ages and cohorts, cohort relative risks that reflect the increased or reduced mortality specific to people born in specific time periods, and local drifts with net drift. The longitudinal age curve was fitted to three-year age groups over the 16–84-year age range (i.e., 16–18, 19–21, …..., and 82–84) in the reference cohort adjusted for period deviations. The period relative risks are presented as the ratio of mortality rates in each consecutive three-year calendar period from 2000 to 2020, with the 2009 to 2011 period as the reference group. The cohort relative risks were the ratio of the mortality rate in the 29 consecutive cohorts born from 1917 to 1919 (median, 1918) to 2001 to 2003 (median, 2002), with the birth cohort of 1959–1961 (median, 1960) as the reference group. We used these three year width time periods, age groups and cohorts to establish the most detailed possible cohort- and period-specific curves, while balancing the need for detail with the risk of over-fitting that would arise from single-year age groups. The net drift represents the overall annual percentage change in mortality and the local drifts indicates the annual percentage change within each age group. The Wald χ2 test was used to examine the significance of the estimable parameters and functions. A p value less than 0.05 was considered statistically significant.
Role of the funding source
The funders of this study had no role in study design, data collection, data analysis, data interpretation, and writing of the manuscript. All authors had full access to the data in the study and agreed to submit for publication.
Results
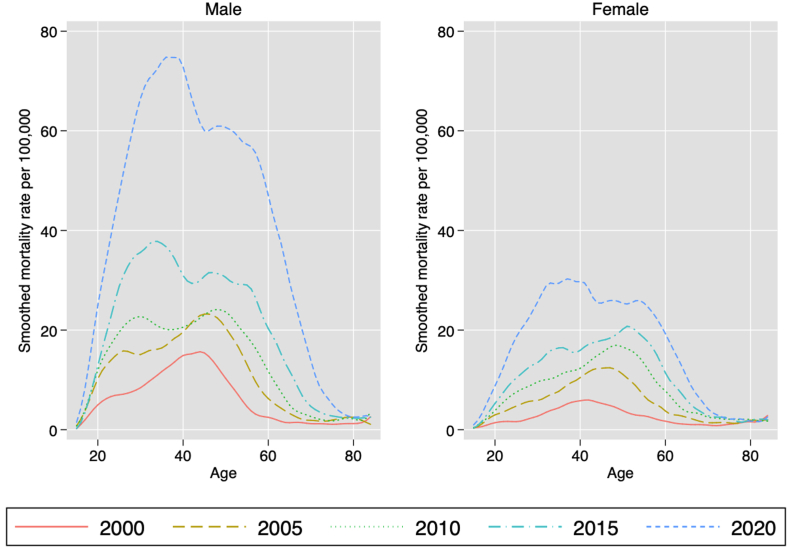
There were 83,293 drug overdose deaths between ages 15–84 in 2020, a 622% increase on the number of deaths in 2000.14 Fig. 1 shows the kernel-smoothed age-specific mortality rates for men and women (all races) for every five years from 2000 to 2020. This figure shows a clear shift in the peak of mortality upward along the age curve over time until 2015, after which the peak suddenly drops into a younger age cohort.
Fig. 1.
Smoothed mortality rates for drug overdose mortality in the most recent five census years, by sex. Figures were smoothed using a linear kernel density smoother with Gaussian kernel. Note mortality rates below 15 years and above 84 years of age were omitted.
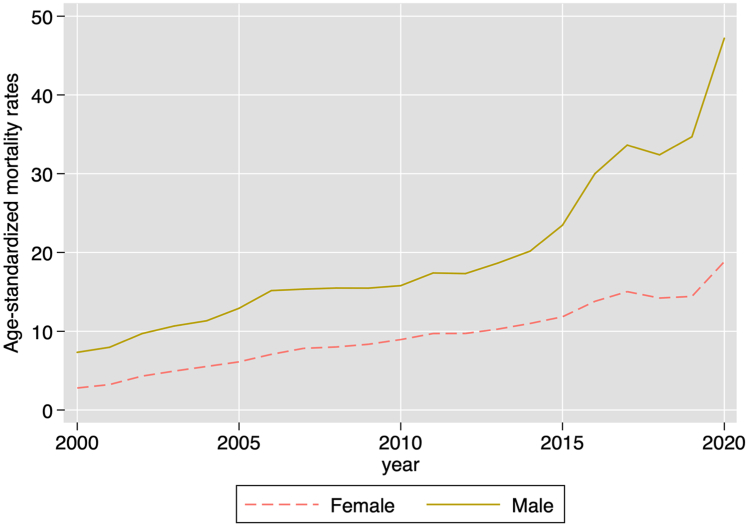
Fig. 2 shows the trend in age-standardized mortality rates for men and women from 2000 to 2020. There is a clear rapid increase in mortality rates in both sexes, but especially in men since 2010, and male mortality rates have consistently exceeded female mortality rates over the past 20 years.
Fig. 2.
Directly standardized mortality rates (DSR) for drug overdose by sex, from 2000 to 2020.
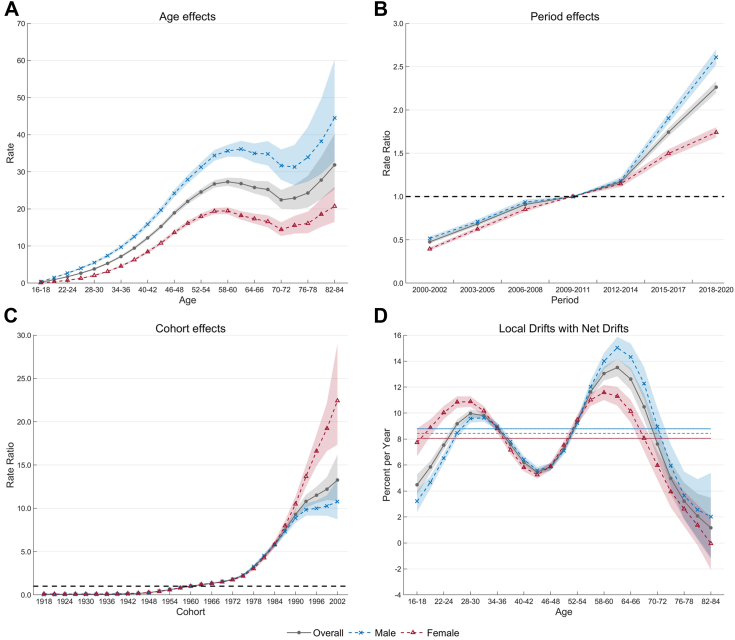
Age-period-cohort effects by sex
Fig. 3 shows the estimates of age, period, and cohort effects on drug overdose mortality by sex, with detailed values reported in Table S1. The mortality rates increased continuously before age 60, then decreased between age 61–72, and increased again after age 73. Male mortality rates were higher than female rates across all age groups. The period effects increased continuously, with higher relative risk among men since 2012. Mortality risk remained stable in the pre-1945 cohorts, then started to increase with a J-shaped pattern afterward. The slope of the cohort effect sharply increased in the cohorts born after 1975. The latest 2002 cohort had the highest risk (RR = 13.27, [95% CI, 10.88 to 16.20]). After stratification, the cohort effect in both sexes followed the overall pattern, while the risk was higher for women in the post-1990 cohorts. Wald tests indicated statistically significant cohort and period effects for the whole population and by sex (Table S1).
Fig. 3.
Accidental drug overdose mortality by sex in the United States, 2000 to 2020, by age-period-cohort analysis. A Longitudinal age curve of drug overdose mortality rates (per 100,000 people) in the reference cohort (1960) adjusted for period effects and corresponding 95% confidence intervals. B Period rate ratios (RRs) for drug overdose mortality relative to the 2009–2011 period and corresponding 95% confidence intervals. C Cohort rate ratios (RRs) for drug overdose mortality (reference group: 1960 birth cohort) and corresponding 95% confidence intervals. D Local drift value for drug overdose mortality rates: age group-specific annual percent change (%) in drug overdose mortality rates and corresponding 95% confidence intervals.
Fig. 3D shows the local drifts with net drifts by sex. The overall annual percentage change of mortality rates across the study period was 8.44% (95% CI, 8.20 to 8.67). The local drift showed a bimodal distribution with increasing age. The annual increase was slightly higher in 61–63 years (13.51% [95% CI, 12.83 to 14.20]) than in 28–30 years (9.98% [95% CI, 9.68 to 10.28]). Local drift values for all age groups in both sexes were above zero, indicating both sexes experienced increasing trends in drug overdose mortality. The net drifts and local drifts for both sexes were statistically significant in Wald χ2 test (p < 0.001).
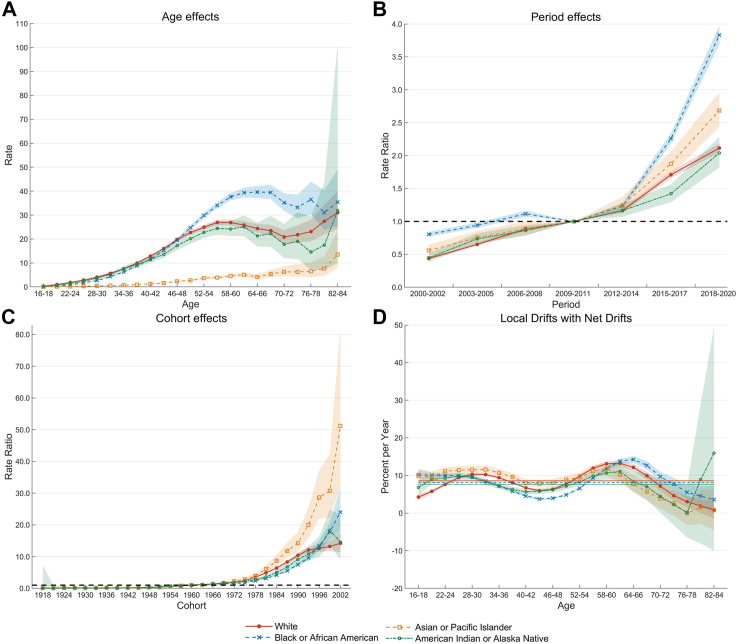
Age-period-cohort effects by race
Fig. 4 shows the estimated age-period-cohort effects stratified by race, with detailed values reported in Table S2. For White people, the mortality rates increased continuously before age 57, then decreased between age 58–72, and increased again since age 73. For Black people, the mortality rates increased continuously before age 66, then showed decreased trends, while among AIAN mortality rates had similar increasing trend until 63 years, after which uncertainty in estimates made peaks difficult to describe. The period effects for all races showed continuous upward trends. Black Americans had a more pronounced increasing trend and higher relative risk of period effects than other races since 2012. Cohort effects for each race remained stable in the pre-1945 cohorts, then started to increase with a J-shaped pattern afterward. Cohort-specific risk increased fastest in Asian and Pacific Islander Americans born after 1975, increasing from 2.87 (95% CI, 2.43 to 3.40) in the 1975 cohort to 51.17 (95% CI, 31.79 to 82.38) in the 2002 cohort. Cohort effects among the Black Americans and AIAN exceeded the ones among the White Americans since recent birth cohorts after 1996, albeit with wide uncertainty. The 2002 birth cohort of the Black Americans had an approximately 24.03 times higher mortality rate (95% CI: 18.14 to 31.82) than the 1960 cohort. Period and cohort effects for each race were statistically significant (Table S2).
Fig. 4.
Accidental drug overdose mortality by race in the United States, 2000 to 2020, by age-period-cohort analysis. A Longitudinal age curve of drug overdose mortality rates (per 100,000 people) in the reference cohort (1960) adjusted for period effects and corresponding 95% confidence intervals. B Period rate ratios (RRs) for drug overdose mortality relative to the 2009–2011 period and corresponding 95% confidence intervals. C Cohort rate ratios (RRs) for drug overdose mortality (reference group: 1960 birth cohort) and corresponding 95% confidence intervals. D Local drift value for drug overdose mortality rates: age group-specific annual percent change (%) in drug overdose mortality rates and corresponding 95% confidence intervals.
Fig. 4D shows the local drifts with net drifts stratified by race. The overall annual percentage change in mortality rates for each race across the study were above zero but largest in White people (8.60% [95% CI, 8.33 to 8.86]), followed by Asian and Pacific Islanders (8.52% [95%CI, 7.78 to 9.26]), Black Americans (8.09% [95% CI, 7.82 to 8.36]) and AIAN (7.61% [95% CI, 6.49 to 8.75]). The local drift showed a bimodal distribution with increasing age for each race. with the largest peaks among Black Americans (10.22% [95% CI, 9.01 to 11.45] among 16–18 year olds versus 14.25% [95% CI, 13.38 to 15.13] among 64–66 year olds). Local drift values for all age groups in both races were above zero. The net drifts and local drifts for both races were statistically significant in the Wald χ2 test (p < 0.001).
Discussion
In this study, we presented the age-profile of drug overdose deaths in the USA from 2000 to 2020 and applied an age-period-cohort model using national vital registration data. Our analysis shows rapidly growing mortality among men and women, and highlights a shift in the peak of mortality rates from older to younger generations. The rapid increase in drug overdose deaths was especially notable in men and in Black Americans in recent years. Previous research using age-period-cohort models has not disaggregated the analysis by sex or race, was published before the recent rapid increase in accidental drug overdose deaths, or erroneously identified a generational effect among 45–64-year-old White Americans due to a lack of proper age standardization.6 Our research builds on recent work that has identified age-, sex- and race-based differences in mortality to decompose recent rises in drug overdose mortality into contributions due to cohorts, age groups and a time trend, and updating older research results in light of the rapid growth in opioid overdoses.15,16 We found that mortality rates in the past 10 years have risen fastest in younger Americans aged 20–40, in young men, and in Black Americans, in a complete change from research published just a decade earlier before the rapid growth of drug overdose deaths in younger age groups.16 The rapid shift of the mortality peak from the 50–59 age group to the 20–40 age group also shows that the distribution of deaths has shifted from the bimodal age distribution identified in earlier research to a sharpening peak in younger age groups,15 perhaps consistent with the rapid growth of fentanyl as a primary cause of opioid overdose death in the past five years, and affecting more recent birth cohorts in particular. Both sexes born after 1975 had a rapid increase in mortality risk, especially for women born after the 1990s. Asian and Pacific Islander experienced the fastest increase in mortality rates among those born during 1975 and 2002. Although confidence intervals were wide, we found very rates of overdose death in AIAN, consistent with recent research finding rapid increases in this marginalized community,17 and also among recent cohorts of Black Americans. Recent APC analyses of overall mortality rates predicted a maximum mortality rate in people born in 1990 of more than 80 per 100,000,8 but this research did not disaggregate by sex or race, and our findings suggest that the maximum mortality rate among men and Black Americans may significantly exceed these predictions. In the past decade, accidental drug overdose mortality rates have rapidly increased, accompanied by a shift towards greater racial and ethnic diversity in the underlying demographic patterns, and robust analyses without detailed sex and race disaggregation have become outdated within a decade. More research is urgently needed on patterns of overdose mortality among AIAN and other excluded populations, such as Hispanic and Latino Americans.
Although there has been a large increase in poisoning deaths from stimulants such as cocaine and methamphetamine since 2012,18 the great majority of poisoning-related deaths remain due to synthetic opioids, with a rapid increase in deaths due to synthetic opioids other than methadone occurring since 2013 and a growing share of total overdose deaths due to opioids.2 This rapid increase in deaths due to synthetic opioids has occurred on the same approximate time scale as the sudden rapid shift in the peak mortality rate from 40 to 64-year-olds to 20–40-year-olds, and the rapid increase in period effects identified in our APC analysis. However, mortality rates within the synthetic opioid category are not reported in detail, and it is unclear how much of the growth in mortality in this category since 2013 is due to fentanyl rather than more traditional synthetic opioids such as tramadol. For example, between 2012 and 2015 rates of tramadol prescribing increased by 22.8%,19 with large regional variations, and although tramadol has been found to be less strongly associated with substance use disorder,20 better disaggregation of statistics on deaths due to these synthetic opioids is essential to properly formulate a response to this growing epidemic. Effective measures to prevent opioid overdose death are essential to stop the rapid increase in opioid overdose mortality, but they may also need to be adapted to deal with this new wave of synthetic opioids.
The large number of drug-related deaths in the U.S. is a complex social and political issue. To address the rapidly increasing mortality rates, a multi-faceted public health approach is urgently needed. National guidelines for opioid prescription must be reviewed routinely and modified. In 2016 the CDC published a guideline to address the overprescribing of opioid drugs.21 Since then, the U.S. has seen a decrease in opioid dispensing rate per 100 persons from 70.6 in 2015 to 43.3 in 2020.22 In 2022, CDC released another Clinical Practice Guideline for prescribing opioids for adult outpatients with pain.23 However, these guidelines have some limitations as they do not situate prescription opioids within the context of opioid overdose epidemic. Although rates of opioid prescription have declined since 2012 the guideline does not note that the overdose deaths have increased. In addition, these guidelines do not clearly identify the risk of concurrent alcohol use for overdose deaths.24 Moreover, the guidelines do not address those who are uninsured or in a low-income household who are at higher risk of opioid deaths but for whom opioid pain relief may be the only option for managing chronic pain.25 Challenges in implementing the guidelines correctly, and barriers to financing alternatives to opioid-based pain relief, have also been identified.25 Although the newly-released 2022 guidelines make reference to the opioid crisis, they still lack reference to the management of multi-drug use and concomitant alcohol use, give little guidance on balancing patient needs for pain relief with federal rules on prescription limits, and incorporate recommendations for alternative pain-relief strategies that despite identifying that these are supported only by low quality evidence. Further refinement of these guidelines is essential in light of the rapid growth of opioid overdose deaths in the USA.23
In addition, treatments and resources should be provided to people who use drugs, in particular expansion of opioid agonist and antagonist treatments, such as methadone or buprenorphine, which need to be made widely available and routinely covered by insurance. Prescribing guidelines and state-level public health policies must be grounded in evidence, with the priority of saving lives. In particular, the US needs to take urgent action to make its national and state-level policies consistent with the CDC's evidence-based strategies for preventing opioid overdose.26 These include Naloxone distribution to people who inject drugs and to the family members of people using opiates to manage chronic pain, wide spread medication-assisted treatment, syringe services programs and other strategies that are known to be effective in the US context. Above and beyond these interventions, the rapidly rising scale of this epidemic of drug overdose deaths suggests that it will be better managed using strategies beyond those recommended by the CDC, which have been shown to be effective overseas. These include the establishment of a widespread network of medically supervised injecting centers and a greater focus on harm reduction policies, which have been shown to effectively complement prohibition strategies in preventing mortality.27,28 However, recent comprehensive assessment of coverage of evidence-based strategies for managing opioid addiction and preventing overdose has rated the USA as having low coverage of opioid agonist treatments and needle/syringe services.29 Lastly, a better coordinated effort among quality policing, first responders, emergency departments, public health departments, and poison control centers is needed to prevent excessive overdose deaths. Such widespread policy changes will necessarily require legal reform, changes in law enforcement policy and procedures, and much closer coordination between law enforcement and health authorities, building on a basis of harm reduction rather than prohibition and punishment.
Drug overdose deaths are preventable, and the experience of other countries has shown that the seemingly inexorable upward trends in mortality can be reversed. Australia experienced a similar surge in opioid overdose deaths in the mid-1990s, and was able to begin reversing them by 1998 through a combination of expanded methadone treatment, needle/syringe programs, policing reform and a greater commitment to harm reduction,28 which culminated in 2001 with the establishment of Australia's first Medically Supervised Injecting Center.30 Given that overdose mortality in the USA now is significantly higher than that experienced in Australia when its national and state governments put their response on an emergency footing, an even more urgent shift in tactics is recommended for the USA.
This study also has some limitations. First, information on covariates that could explain cohort and period effects was lacking. Second, although previous studies identified substantial geographical variations in opioid-related deaths, data suppression prevented us exploring APC patterns by states and by drug types. Future studies are warranted when detailed unsuppressed data available. Third, this study focused on the mortality rates of accidental drug overdose, which may be underestimated due to underreporting and misclassification of vital statistics. Especially, mutual misclassification exists between deaths due to drug overdose and suicide deaths, as it is challenging to accurately distinguish between overdose deaths in individuals with suicidal intent and suicide deaths in individuals with opioid use disorder. To the extent that the misclassification is systematic and consistent across the calendar years, it does not threaten the robustness of our conclusions, because we focus on temporal trends and cohort patterns over time and not the true level of drug overdose mortality in any specific year.
Our study shows that the US is experiencing an unprecedented crisis of drug-related mortality, that this crisis is at its most acute in vulnerable younger, non-White populations, and that there has been a generational shift in the burden of opioid overdose in the past decade. Significant policy reforms, further prescribing restrictions, and a huge expansion of harm reduction policies will be necessary to contain this epidemic, and a wholesale reform of public health, law enforcement and social policy will be needed to see real gains in overdose prevention. National and state policy makers need to move to an emergency footing and implement coordinated, radical but achievable policy changes if they are to have any hope of reversing the explosive growth in drug mortality in the past decade. If these changes are not made, US policy-makers will consign an entire generation of young people to decades of tragically preventable mortality.
Contributors
SG, JKMS and SI conceived the study. SG and JL provided overall guidance. SI, JX, BD, XW, PN and YW conducted data analysis. SI, JX, BD, JL, JKMS and SG prepared the first draft and finalised the manuscript. PN, JS, JL, and SG critically reviewed results and provided valuable inputs on revision. All authors contributed to the critical review and editing of the manuscript. All authors had full access to the data in the study and accepted the responsibility for submitting this study for publication.
Data sharing statement
All data used in this study can be freely accessed on CDC WONDER (https://wonder.cdc.gov/).
Declaration of interests
We declare no competing interests.
Acknowledgements
None.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2023.102079.
Appendix A. Supplementary data
APC_Analysis_Asian
References
- 1.Shiels M.S., Berrington de González A., Best A.F., et al. Premature mortality from all causes and drug poisonings in the USA according to socioeconomic status and rurality: an analysis of death certificate data by county from 2000-15. Lancet Public Health. 2019;4(2):e97–e106. doi: 10.1016/S2468-2667(18)30208-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hedegaard H., Miniño A.M., Warner M. Drug overdose deaths in the United States, 1999-2019. NCHS Data Brief. 2020;(394):1–8. [PubMed] [Google Scholar]
- 3.Scholl L., Seth P., Kariisa M., Wilson N., Baldwin G. Drug and opioid-involved overdose deaths - United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419–1427. doi: 10.15585/mmwr.mm675152e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Fentanyl. 2022 https://www.cdc.gov/opioids/basics/fentanyl.html [Google Scholar]
- 5.Jones C.M., Bekheet F., Park J.N., Alexander G.C. The evolving overdose epidemic: synthetic opioids and rising stimulant-related harms. Epidemiol Rev. 2020;42(1):154–166. doi: 10.1093/epirev/mxaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Case A., Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Venter G. Generational cohort effects on trends in the drug overdose mortality epidemic in the United States. 2017. SSRN: https://ssrn.com/abstract=2992349
- 8.Jalal H., Buchanich J.M., Sinclair D.R., Roberts M.S., Burke D.S. Age and generational patterns of overdose death risk from opioids and other drugs. Nat Med. 2020;26(5):699–704. doi: 10.1038/s41591-020-0855-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qeadan F., Madden E.F., Mensah N.A., et al. Epidemiological trends in opioid-only and opioid/polysubstance-related death rates among American Indian/Alaska Native populations from 1999 to 2019: a retrospective longitudinal ecological study. BMJ Open. 2022;12(5) doi: 10.1136/bmjopen-2021-053686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paulozzi L.J., Budnitz D.S., Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg P.S., Check D.P., Anderson W.F. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2014;23(11):2296–2302. doi: 10.1158/1055-9965.EPI-14-0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cao J., Eshak E.S., Liu K., Gero K., Liu Z., Yu C. Age-Period-cohort analysis of stroke mortality attributable to high sodium intake in China and Japan. Stroke. 2019;50(7):1648–1654. doi: 10.1161/STROKEAHA.118.024617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Su Z., Zou Z., Hay S.I., et al. Global, regional, and national time trends in mortality for congenital heart disease, 1990-2019: an age-period-cohort analysis for the Global Burden of Disease 2019 study. eClinicalMedicine. 2022;43 doi: 10.1016/j.eclinm.2021.101249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention Underlying cause of death, 1999-2020 request. 2021. https://wonder.cdc.gov/ucd-icd10.html
- 15.Jalal H., Buchanich J.M., Roberts M.S., Balmert L.C., Zhang K., Burke D.S. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;(6408):361. doi: 10.1126/science.aau1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miech R., Koester S., Dorsey-Holliman B. Increasing US mortality due to accidental poisoning: the role of the baby boom cohort. Addiction. 2011;106(4):806–815. doi: 10.1111/j.1360-0443.2010.03332.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman J., Hansen H., Gone J.P. Deaths of despair and Indigenous data genocide. Lancet. 2023;401(10379):874–876. doi: 10.1016/S0140-6736(22)02404-7. [DOI] [PubMed] [Google Scholar]
- 18.Abuse NioD . 2022. Drug overdose death rates.https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates [Google Scholar]
- 19.Bigal L.M., Bibeau K., Dunbar S. Tramadol prescription over a 4-year period in the USA. Curr Pain Headache Rep. 2019;23(10):76. doi: 10.1007/s11916-019-0777-x. [DOI] [PubMed] [Google Scholar]
- 20.Silverman S., Rice J.B., White A.G., et al. Clinical and economic burden of prescribing tramadol and other opioids for patients with osteoarthritis in a commercially insured population in the United States. Pain. 2022;163(1):75–82. doi: 10.1097/j.pain.0000000000002300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dowell D., Haegerich T.M., Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention U.S. Opioid dispensing rate maps. 2021. https://www.cdc.gov/drugoverdose/rxrate-maps/index.html
- 23.Dowell D., Ragan K.R., Jones C.M., Baldwin G.T., Chou R. CDC clinical Practice guideline for prescribing opioids for pain - United States, 2022. MMWR Recomm Rep. 2022;71(3):1–95. doi: 10.15585/mmwr.rr7103a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Darke S., Zador D. Fatal heroin 'overdose': a review. Addiction. 1996;91(12):1765–1772. doi: 10.1046/j.1360-0443.1996.911217652.x. [DOI] [PubMed] [Google Scholar]
- 25.Altekruse S.F., Cosgrove C.M., Altekruse W.C., Jenkins R.A., Blanco C. Socioeconomic risk factors for fatal opioid overdoses in the United States: findings from the mortality disparities in American communities study (MDAC) PLoS One. 2020;15(1) doi: 10.1371/journal.pone.0227966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention Evidence-based strategies for preventing opioid overdose: what's working in the United States. 2018. https://www.cdc.gov/drugoverdose/pdf/pubs/2018-evidence-based-strategies.pdf
- 27.van Beek I., Kimber J., Dakin A., Gilmour S. The Sydney medically supervised injecting centre: reducing harm associated with heroin overdose. Crit Publ Health. 2004;14(4):391–406. [Google Scholar]
- 28.Degenhardt L., Day C., Gilmour S., Hall W. The "lessons" of the Australian "heroin shortage". Subst Abuse Treat Prev Policy. 2006;1:11. doi: 10.1186/1747-597X-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Colledge-Frisby S., Ottaviano S., Webb P., et al. Global coverage of interventions to prevent and manage drug-related harms among people who inject drugs: a systematic review. Lancet Global Health. 2023;11(5):e673–e683. doi: 10.1016/S2214-109X(23)00058-X. [DOI] [PubMed] [Google Scholar]
- 30.Willis K. Australian Institute of Criminology; Canberra: 2002. Evaluation of the impact of drug summit initiatives in two NSW regions.https://www.aic.gov.au/publications/archive/archive-116 Available at: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
APC_Analysis_Asian