Abstract
Aim
This work aimed to evaluate the impact of automated dispensing cabinets on the dispensing error rate, the number of interruptions, and pillbox preparation times.
Methods
A prospective observational study was conducted across 16 wards in two departments (internal medicine and surgery) of a large teaching hospital. The study compared eight wards using automated dispensing cabinets (ADCs) and eight using a traditional ward stock (TWS) method. A disguised observation technique was used to compare occurrences of dispensing errors and interruptions and pillbox preparation times. The proportion of errors was calculated by dividing the number of doses with one or more errors by the total number of opportunities for error. Wards participating in the ‘More time for patients’ project—a Lean Management approach—were compared with those not participating. The potential severity of intercepted errors was assessed.
Results
Our observations recorded 2924 opportunities for error in the preparation of 570 pillboxes by 132 nurses. We measured a significantly lower overall error rate (1.0% vs 5.0%, p=0.0001), significantly fewer interruptions per hour (3.2 vs 5.7, p=0.008), and a significantly faster mean preparation time per drug (32 s vs 40 s, p=0.0017) among ADC wards than among TWS wards, respectively. We observed a significantly lower overall error rate (1.4% vs 4.4%, p=0.0268) and a non-significantly lower number of interruptions per hour (3.8 vs 5.1, p=0.0802) among wards participating in the ‘More time for patients’ project.
Conclusions
A high dispensing-error rate was observed among wards using TWS methods. Wards using ADCs connected to computerised physician order entry and installed in a dedicated room had fewer dispensing errors and interruptions and their nurses prepared pillboxes faster. Wards participating in a Lean Management project had lower error rates than wards not using this approach.
Keywords: automation, education department, hospital, facility design and construction, organization and administration, pharmacy service, hospital
Introduction
Improving the safety of the medication process is a constant objective; numerous technologies and other actions have been suggested to address the issue. Theoretically, this should be done using two complementary means: first, reducing the occurrence of errors; and second, identifying and intercepting errors that have already occurred before the drug is administered to the patient.
Dispensing medication is a complex process with the potential to lead to many medication errors. A review by Aldhwaihi et al 1 concluded that dispensing error rates detected using a prospective observation method were between 0.79% and 33.5% (median rate 3.35%). These dispensing error rates varied according to the countries where the studies were conducted, the dispensing systems and research methodologies used, and the classifications of dispensing error types. The review reported that the most common error types were dispensing the wrong medicine, the wrong drug strength, and the wrong dosage form.
Automated dispensing cabinets (ADCs) first appeared in hospitals in the late 1980s.2 These computerised drug storage devices are located on wards to position drugs as close to patients as possible. ADCs are designed to improve the efficiency of drug logistics, safety and the traceability of treatment preparation.3 4 The literature reveals many evaluations of the parameters surrounding the introduction of ADCs in healthcare facilities, such as deviations from the expected time of administration,5 6 medication omissions,7 staff workloads,8 cost-effectiveness,5 9 and the reduction of potentially preventable adverse events.10 11 Overall, these publications have confirmed how ADCs benefit and improve drug dispensing processes. In 2016, François et al 12 conducted a simulation study suggesting that fewer dispensing errors occurred when using ADCs and computerised physician order entry (CPOE) than when using traditional ward stock (TWS) methods (0.71% vs 4.13%, p<0.001), and that pillbox preparation times with ADCs were almost identical but slightly longer (33 s vs 31 s per drug). However, only a few small-scale studies of a single ward or a low number of wards have demonstrated the impact of ADCs on medication errors,7 13–18 and a large confirmatory study is currently missing.
The present study’s main objective was to compare dispensing error rates and types among wards using ADCs or TWS methods. Its secondary objectives were to compare the frequencies, types and management of the interruptions occurring during dispensing and the time taken to prepare pillboxes. We also sought to compare the medication errors and interruptions on wards participating in a Lean Management project aiming to re-engineer care processes with those on non-participating wards.
Methods
Setting
Geneva University Hospitals is a large, 1800 bed teaching hospital in Switzerland, spread over 10 hospital sites. The first ADCs (Pyxis MedStation, BD) were installed in 2014. In March 2017, a new hospital building was opened, and all 17 wards were equipped with ADCs. In 2018, the ADCs were connected to our in-house CPOE system, PRESCO. Consequently, all electronic prescriptions are immediately available in ADCs and the nurses just have to select the patient and the prescribed drugs on the screen to start dispensing. In the wards with TWS, nurses print prescriptions and use this paper tool to dispense drugs manually.
In 2020, 63 further wards were equipped with ADCs, but TWS methods still existed on the wards located in an older building. In 2018, the ‘More time for patients’ project was rolled out across our hospital’s clinical units. This aimed to distribute activities better and introduce Lean Management methods to re-engineer ward organisation.
Study design and data collection
This prospective direct observational study was conducted on 16 wards and required 36 days of observations. The study included two observation and data collection periods (July–August 2019 and February–May 2020). A single pharmacist (MJ) observed both groups of eight wards (the ADC and TWC groups, each made up of four general internal medicine and four surgery wards), with observations occurring on weekdays during the hours of pillbox preparation so as to cover the different times of the day equitably. Each ward was observed on 2 non-consecutive days. The study used a disguised observation technique, and the observer stayed well away from the nurse to lessen the Hawthorne effect.19 Each observation collected the following information: whether the ward was participating in the ‘More time for patients’ project; the nurse’s employment status (hospital employee <3 months, hospital employee >3 months, substitute, student or agency nurse); the nurse’s experience in the department (<3 months, >3 months); the nurse’s experience with an ADC (<3 months, >3 months); and the nurse’s time on shift before the observation (<6 hours, >6 hours). The observation began when a nurse began preparing pillboxes. A pillbox is composed of four compartments corresponding to the time of day of each medication (morning, noon, evening, night). In the TWC groups, the pillboxes are made once a day for 24 hours, whereas in the ADC groups the pillboxes are made just before each administration time. That is to say, the nurse prepares the medication for the morning, noon, evening and night time. The nurse can only take medication from the ADC for the next 4 hours. The observer noted the time taken to prepare pillboxes and any interruptions. A picture of each pillbox was taken, and the content was compared with the prescription information in the patient’s treatment schedule in their electronic health record. The observer planned to intervene directly in cases involving a medication error with potentially harmful consequences.
Description of ADCs and TWS methods
ADCs are located in dedicated medication preparation rooms. Only one nurse at a time can retrieve medication from an ADC. First, they must identify themselves using biometric verification. The process of obtaining drugs consists of selecting the patient and then their prescribed drugs as displayed on the computer station screen thanks to an interface with the CPOE. Once the medication has been selected, the ADC opens a drawer containing it. Most drugs are stored in locked pockets (‘cubies’) containing a single drug in order to limit the risk of wrong-drug errors.
TWS methods are simply shelves on which medication is stored; nurses have free access to the medication stored in their office. Treatments are prepared directly from a computer display of the prescription or a printed list of the treatment to be dispensed. Several nurses can prepare pillboxes at the same time. On weekdays, a pharmacy technician replenishes both types of ward stocks daily.
Lean Management: the ‘More time for patients’ project
Since 2018, the ‘More time for patients’ project was progressively implemented in the medical services of our institution. This project aims at a better distribution of activities and is based on three objectives:
Simplify the processes
Include the patient in discussions about his or her care
Improve the communication between caregiver and patient.
On all wards participating in this project, with and without ADCs, an order of passage has been established for periods of high activity so that nurses do not have to queue at pharmacy cabinets to prepare pillboxes. Consequently only one nurse prepares the medications while the others are occupied with other activities. This avoids having several nurses preparing the pillboxes at the same time and contributes to greater concentration and efficiency. At the time of our study, this project was implemented in 6/8 wards of the ADC group and 5/8 wards of the TWS group.
Data analysis
Error was defined as a deviation between the medication in the pillbox and the patient’s prescription.1 The percentage of errors was determined using Allan and Barker’s method19: [(number of doses identified with one or more errors)/(total number of error opportunities) × 100]. The literature defines the total number of error opportunities as the total number of doses prepared plus the doses prescribed but omitted. The types of error were drug omission, wrong active ingredient, wrong dosage, wrong galenic form, wrong dosage, and mistimed drug administration. The definition of mistimed drug administration is the presence of the drug in the wrong time slot (eg, the drug is in the evening time slot instead of the noon time slot).
Interruption was defined as ‘an identifiable external event, the occurrence of which is unpredictable and which interferes with cognitive attention in the context of a specific task’.20 Interruptions were systematically noted and analysed according to their frequencies, types (noise, answering the phone, a colleague talking, a colleague talking and making noise, complete interruption) and the nurse’s interruption management mode (multi-task, change task, momentary inattention or distraction, interruption of activity, non-optimal execution of activity).21
Statistical analysis
Based on the results of our previous simulation study,12 estimated error rates were 0.5% using the ADC connected to the CPOE and 4% using a TWS method. This suggested that we would require 300 observations from each group to ensure a statistically significant result with a 5% risk and 80% study power. We considered p<0.05 as significant. All comparisons between the different groups were made using the non-parametric Mann-Whitney test.
Results
Descriptive data
The present study involved 132 nurses, and 2924 opportunities for error were observed (1676 in the ADC group and 1248 in the TWS group). Descriptive data are provided in table 1. Mean (SD) preparation times were 32 (23) s/drug for the ADC group and 40 (29) s/drug for the TWS group (p=0.0017).
Table 1.
General characteristics of wards using automated dispensing cabinets and traditional ward stock methods
| ADC group | TWS group | |
| Opportunities for error | ||
| Total number of opportunities for error | n=1676 | n=1248 |
|
54% (n=906) | 44% (n=548) |
|
46% (n=770) | 56% (n=700) |
| Pill dispenser | ||
| Number of pillbox preparations observed | n=364 | n=206 |
| Mean number of opportunities for error/pillbox | n=4.6 | n=6.1 |
| Wards participating in the ‘More time for patients’ project | ||
| General internal medicine department | n=4 | n=3 |
| Surgery department | n=2 | n=2 |
| Wards not participating in the ‘More time for patients’ project | ||
| General internal medicine department | n=0 | n=1 |
| Surgery department | n=2 | n=2 |
| Nurses’ employment status | ||
| Number of nurses observed | n=77 | n=55 |
| Hospital employee for <3 months | 0% (n=0) | 2% (n=1) |
| Hospital employee for >3 months | 77% (n=59) | 73% (n=40) |
| Substitute nurse | 1% (n=1) | 7% (n=4) |
| Student nurse | 4% (n=3) | 5% (n=3) |
| Agency nurse | 18% (n=14) | 13% (n=7) |
| Experience on the ward | ||
| <3 months | 29% (n=22) | 20% (n=11) |
| >3 months | 71% (n=55) | 80% (n=44) |
| Experience with the ADC | ||
| <3 months | 16% (n=12) | |
| >3 months | 84% (n=65) | |
| Nurse’s hours worked at the time of observation | ||
| <6 hours | 99% (n=76) | 100% (n=55) |
| >6 hours | 1% (n=1) | 0% (n=0) |
| Distribution of hours of observation: | ||
| 8 am | n=30.9% | n=17.6% |
| 12 noon | n=17.9% | n=17.6% |
| 6 pm | n=20.8% | n=21.6% |
| 8 pm | n=18.3% | n=21.6% |
| 10 pm | n=12.2% | n=21.6% |
ADC, automated dispensing cabinet; TWS, traditional ward stock.
Impact of ADCs on medication errors
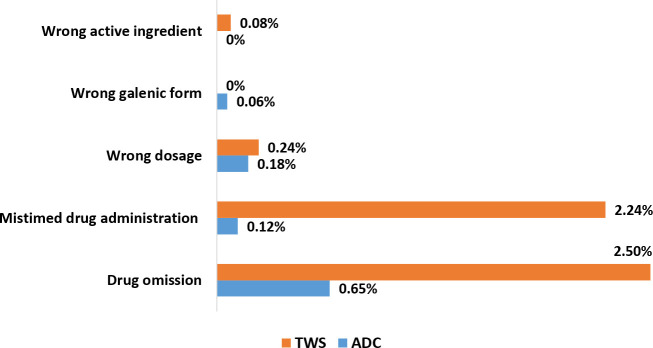
The observer detected 17 errors in the ADC group and 63 in the TWS group. The overall error rate was significantly lower in the ADC group than in the TWS group (1.0% vs 5.0%, p=0.0001) (figure 1). No differences were observed between general internal medicine and surgery wards.
Figure 1.
Types of errors and their percentages of total opportunities for errors using automated dispensing cabinets (ADC) or traditional ward stock (TWS) methods.
The most common error in both groups was drug omission. There were fewer omissions and errors in drug administration times in the ADC group than in the TWS group (0.7% vs 2.5%, and 0.1% vs 2.2%, respectively).
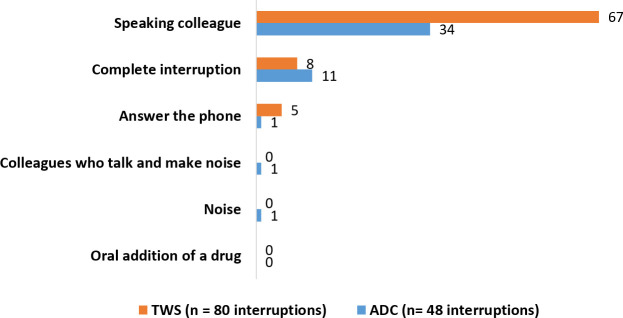
The vast majority (94%) of errors made using ADCs were by nurses with <3 months of experience with this technology, whereas those nurses represented only 15% of the observations (figure 2).
Figure 2.
Dispensing errors and experience with automated dispensing cabinets (ADC).
Impact of ADCs on interruption
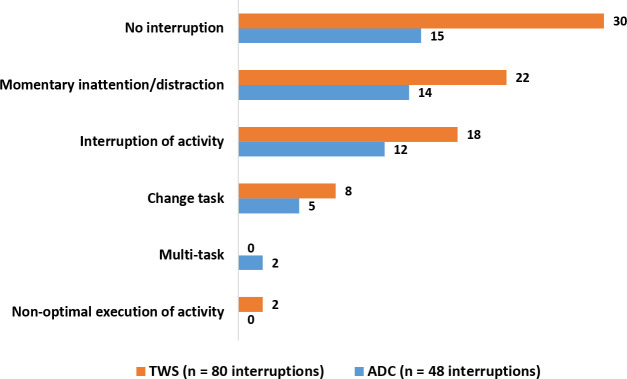
The observer noted 47 interruptions affecting the ADC group and 80 affecting the TWS group. The number of interruptions per hour was significantly lower for the ADC group than for the TWS group (3.2 vs 5.7, p=0.0008).
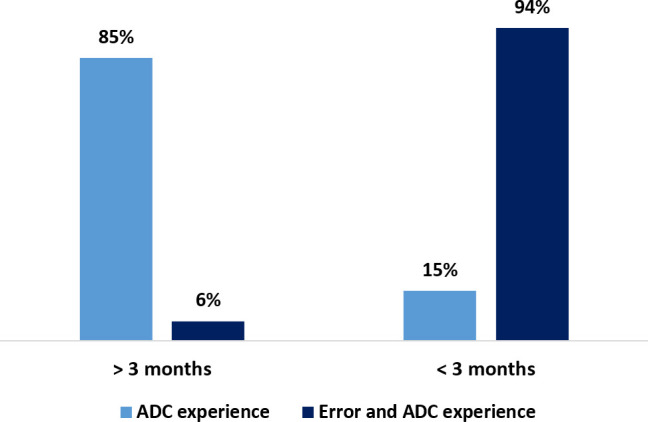
Interruptions noted as a ‘colleague speaking’ and ‘complete interruption’ were the most common types for both groups (figure 3). The most common interruption management modes used by both groups were ‘no interruption of activity’, ‘interruption of activity’ and ‘momentary inattention or distraction’. An analysis of the results showed that when errors did occur, none (out of 47) were related to interruptions in the ADC group, whereas four (out of 80) were linked to interruptions in the TWS group (figure 4).
Figure 3.
Number of each type of interruption affecting the automated dispensing cabinets (ADC) group and the traditional ward stock (TWS) method group.
Figure 4.
Numbers and types of interruption management modes used with automated dispensing cabinets (ADC) and traditional ward stock (TWS) methods.
The ‘More time for patients’ project
This Lean Management approach had already been implemented on six wards (out of eight) in the ADC group and five wards (out of eight) in the TWS group. We also found a statistically significant lower total percentage of errors in wards participating in the ‘More time for patients’ project than in those not participating (1.4% vs 4.4%, p=0.0268). A cumulative effect of ADC and Lean management was suggested (TWS+no Lean: 6.4% of errors; TWS+Lean: 3.7%; ADC+no Lean: 1.5%; ADC+Lean: 0.9%), even if the power of the study did not allow statistical differences to be reached.
In addition, the overall trend seemed to suggest fewer interruptions on wards implementing the ‘More time for patients’ project than on wards not doing so (3.8 vs 5.1 interruptions per hour, respectively). However, this result was not statistically significant (p=0.0802).
Discussion
Wards with ADCs showed significantly lower error rates, significantly less frequent interruptions and significantly shorter pillbox preparation times. Our study also showed the positive effects of the ‘More time for patients’ project, a Lean Management approach, on error rates and interruptions; however, our study’s power did not enable us to show a statistically significant result for interruptions (p=0.0802).
Our direct observation methodology has been described in the majority of similar publications.7 13–18 The major advantages are that they include unselected nurses followed under usual conditions and collect data corresponding to real life. The inconveniences are that the presence of the observer might influence the behaviour and that information is collected over a short period and only provide a picture of the situation at the time of observation.
Our study succeeded in assessing the impact of ADCs on 16 wards, whereas other studies had only been conducted on one or two wards.7 13–18 The overall error rate on our wards with ADCs connected to the CPOE was 80% lower than those using TWS methods, which was mostly in accordance with the literature and our previous simulation study.12 Indeed, the literature shows a great deal of variability in error rates, ranging from 0.33%14 to 22%.16 This could be explained by the presence or absence of a CPOE interface, the method of expressing the overall error rate (the percentage of detailed opportunities for error; the percentage of total opportunities for error; errors per patient per day), the types of wards studied (general internal medicine, surgery, intensive care, emergency, geriatrics, paediatrics), and the data collection methods (direct observation, retrospective analysis of records). To be able to compare our results with those of other studies, we expressed error rates according to the method developed by Allan and Barker.12 Errors resulting from dose omissions and mistimed drug administration were shown to be markedly lower when using ADCs. Drug omission errors were the most common type of error in both groups, which might be explained by stock-out situations and the complexity of reading printed treatment schedules. Errors in the timing of drug administration were lower because a patient’s medication in an ADC can only be withdrawn following a single treatment schedule. The relationship revealed between nurses’ lack of experience with ADCs and the occurrence of errors has given us a warning, and we will reinforce initial training on ADCs with new nurses. Our results pointed to very low error rates with ADCs once nurses are sufficiently experienced with them.
However, it is well known that dispensing errors can sometimes have a negative impact on patients. The very much lower rates of dispensing errors on wards operating ADCs will necessarily reduce the risks to patients.
The significantly lower numbers of interruptions in the ADC group than in the TWS group have a dual explanation. First, ADCs are all located in closed rooms dedicated to medication storage and preparation, whereas TWS methods take place in rooms adjacent to nursing offices, and only one nurse at a time can remove medication from the ADC. As interruptions are a root cause of errors, they should be prevented22 by improving room ergonomics and work organisation, identifying and neutralising sources of interruptions, clearly identifying employees who should not be interrupted, and having strategies in place for safely recommencing interrupted tasks. Many studies have investigated the prevention of interruptions.23–26 Most interventions to reduce interruptions eventually fail because they are cumbersome to implement (headphones/tabards) and are inflexible to the realities of clinical practice (zero tolerance) because some interruptions are legitimate and unavoidable. These studies conclude that finally the reorganisation of work and prioritisation are the determining factors to reduce interruptions. The ADCs, because of their location in a room dedicated to the preparation of medicines and their mode of operation (faster and easier to locate medicines), facilitate the reduction of interruptions.
In our simulation study,12 pillbox preparation times were almost identical in the ADC and TWS groups, whereas in the present study, they were significantly lower in the ADC group (p=0.0017). This was an interesting result as ADCs are intuitively considered to slow down the dispensing process. However, once nurses become familiar with using an ADC, they can complete dispensing tasks very rapidly. Room ergonomics, fewer interruptions, the prescription interface, blister packs being already out of their boxes, and storage in individual pockets containing the right medication are all contributing factors to a high-speed process.
To enhance ward organisation further, the wards participating in the ‘More time for patients’ project have implemented a Lean Management approach. Among many issues, this has optimised the organisation of drug dispensing. An order of passage has been set up for nurses who must prepare pillboxes, and thus they no longer waste time queuing for access to the cabinet. This is a very important organisational issue, as queuing is a frequently mentioned drawback of ADCs. The ability to prepare treatments in a quiet environment, without feeling the pressure of colleagues waiting for their turn, is probably a contributing factor to a safer dispensing process. Indeed, the improvements in medication errors may not be solely related to the ADCs and our results suggest a cumulative effect with the Lean Management approach.
This study has some limitations. First, the disguised observation method can still influence nurses’ behaviour, even if the literature tends to confirm that this impact is limited.13 Second, several definitions of overall error rate and other methodologies exist in the literature, making comparisons with these studies difficult. We decided on the most frequently used definition, and our method enabled the prospective direct measurement of errors, which probably better reflects reality than a retrospective chart analysis. Finally, drug administration itself was not directly observed; consequently, occurrences of administration error could not be formally confirmed and nor could their real consequences for patients.
Conclusion
A high dispensing-error rate was observed on wards using TWS methods. The use of ADCs connected to CPOE and installed in a dedicated room was effective in providing a significantly lower overall error rate, significantly fewer interruptions and significantly faster pillbox preparation. Using a Lean Management approach also contributed to wards having significantly lower overall error rates.
The automation of stock management has great advantages in terms of patient safety, efficiency and drug traceability. However, to be optimal, ADCs must be installed in rooms dedicated to drug management, preferably with an interface linked to the institution’s CPOE. Furthermore, it is essential that nurses learn about how dispensing is organised and that they are adequately trained.
What this paper adds.
What is already known on this subject?
Dispensing medication is a complex process with the potential to lead to many medication errors.
Automated dispensing cabinets (ADC) improve drug dispensing processes.
This study compares dispensing error rates and types among wards using ADC or traditional ward stock (TWS) methods.
What does this study add?
A high dispensing-error rate was observed on wards using TWS methods.
The use of ADC is effective in providing a significantly lower dispensing-error rate.
Footnotes
Twitter: @bonnabry
Contributors: Conception and design: MJ, PB. Provision of study materials or patients: MJ, OF. Collection and assembly of data: MJ. Data analysis and interpretation: all authors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. All data relevant to the study are included in the article.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study does not fall within the scope of the Swiss law on research on human beings (LRH) and has obtained a request for no objection from the Cantonal Commission for Ethics in Human Research (CCER). We submitted our project to the institutional Evaluation Council for Studies not under the jurisdiction of the Commission for Research Ethics (CEENCER) and received the authorisation to carry out this study. Ethics committee approval for the study was obtained in July 2019 (protocol number 2019–03).
References
- 1. Aldhwaihi K, Schifano F, Pezzolesi C, et al. A systematic review of the nature of dispensing errors in hospital pharmacies. Integr Pharm Res Pract 2016;5:1–10. 10.2147/IPRP.S95733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. ISMP . ISMP list of high-alert medications in acute care settings [online], 2018. Available: https://www.ismp.org/sites/default/files/attachments/2018-08/highAlert2018-Acute-Final.pdf
- 3. Schneider PJ, Pedersen CA, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: dispensing and administration-2017. Am J Health Syst Pharm 2018;75:1203–26. 10.2146/ajhp180151 [DOI] [PubMed] [Google Scholar]
- 4. Billstein-Leber M, Carrillo CJD, Cassano AT, et al. ASHP guidelines on preventing medication errors in hospitals. Am J Health Syst Pharm 2018;75:1493–517. 10.2146/ajhp170811 [DOI] [PubMed] [Google Scholar]
- 5. Shirley KL. Effect of an automated dispensing system on medication administration time. Am J Health Syst Pharm 1999;56:1542–5. 10.1093/ajhp/56.15.1542 [DOI] [PubMed] [Google Scholar]
- 6. Cottney A. Improving the safety and efficiency of nurse medication rounds through the introduction of an automated dispensing cabinet. BMJ Qual Improv Rep 2014;3:u204237.w1843. 10.1136/bmjquality.u204237.w1843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barker KN, Pearson RE, Hepler CD, et al. Effect of an automated bedside dispensing machine on medication errors. Am J Hosp Pharm 1984;41:1352–8. 10.1093/ajhp/41.7.1352 [DOI] [PubMed] [Google Scholar]
- 8. Guerrero RM, Nickman NA, Jorgenson JA. Work activities before and after implementation of an automated dispensing system. Am J Health Syst Pharm 1996;53:548–54. 10.1093/ajhp/53.5.548 [DOI] [PubMed] [Google Scholar]
- 9. McCarthy BC, Ferker M. Implementation and optimization of automated dispensing cabinet technology. Am J Health Syst Pharm 2016;73:1531–6. 10.2146/ajhp150531 [DOI] [PubMed] [Google Scholar]
- 10. Bates DW, Boyle DL, Vander Vliet MB, et al. Relationship between medication errors and adverse drug events. J Gen Intern Med 1995;10:199–205. 10.1007/BF02600255 [DOI] [PubMed] [Google Scholar]
- 11. Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. implications for prevention. ADE Prevention Study Group. JAMA 1995;274:29–34. [PubMed] [Google Scholar]
- 12. Francois O, Meddeb L, Guegueniat-Dupessey C. Influence d’une armoire pharmacie automatisée et des interruptions de tâches sur le taux d’erreur de dispensation des médicaments, étude de simulation. Pharm Hosp Clin 2017;52:e37–8. [Google Scholar]
- 13. Borel JM, Rascati KL. Effect of an automated, nursing unit-based drug-dispensing device on medication errors. Am J Health Syst Pharm 1995;52:1875–9. 10.1093/ajhp/52.17.1875 [DOI] [PubMed] [Google Scholar]
- 14. Holdsworth MT, Fichtl RE, Raisch DW, et al. Impact of computerized prescriber order entry on the incidence of adverse drug events in pediatric inpatients. Pediatrics 2007;120:1058–66. 10.1542/peds.2006-3160 [DOI] [PubMed] [Google Scholar]
- 15. Chapuis C, Roustit M, Bal G, et al. Automated drug dispensing system reduces medication errors in an intensive care setting. Crit Care Med 2010;38:2275–81. 10.1097/CCM.0b013e3181f8569b [DOI] [PubMed] [Google Scholar]
- 16. Rodriguez-Gonzalez CG, Herranz-Alonso A, Martin-Barbero ML, et al. Prevalence of medication administration errors in two medical units with automated prescription and dispensing. J Am Med Inform Assoc 2012;19:72–8. 10.1136/amiajnl-2011-000332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fanning L, Jones N, Manias E. Impact of automated dispensing cabinets on medication selection and preparation error rates in an emergency department: a prospective and direct observational before-and-after study. J Eval Clin Pract 2016;22:156–63. 10.1111/jep.12445 [DOI] [PubMed] [Google Scholar]
- 18. Risør BW, Lisby M, Sørensen J. Complex automated medication systems reduce medication administration errors in a Danish acute medical unit. Int J Qual Health Care 2018;30:457–65. 10.1093/intqhc/mzy042 [DOI] [PubMed] [Google Scholar]
- 19. Allan EL, Barker KN. Fundamentals of medication error research. Am J Hosp Pharm 1990;47:555–71. 10.1093/ajhp/47.3.555 [DOI] [PubMed] [Google Scholar]
- 20. Speier C, Valacich JS, Vessey I. The influence of task interruption on individual decision making: an information overload perspective. Decis Sci 1999;30:337–60. 10.1111/j.1540-5915.1999.tb01613.x [DOI] [Google Scholar]
- 21. Savoldelli GL, Thieblemont J, Clergue F, et al. Incidence and impact of distracting events during induction of general anaesthesia for urgent surgical cases. Eur J Anaesthesiol 2010;27:683–9. 10.1097/EJA.0b013e328333de09 [DOI] [PubMed] [Google Scholar]
- 22. Haute Autorité de Santé . L’interruption de tâche lors de l’administration des médicaments « Comment pouvons-nous créer un système où les bonnes interruptions sont autorisées et les mauvaises bloquées [online], 2016. Available: https://www.has-sante.fr/upload/docs/application/pdf/2016-03/guide_it_140316vf.pdf
- 23. Palese A, Sartor A, Costaperaria G, et al. Interruptions during nurses’ drug rounds in surgical wards: observational study. J Nurs Manag 2009;17:185–92. 10.1111/j.1365-2934.2007.00835.x [DOI] [PubMed] [Google Scholar]
- 24. Westbrook JI, Li L, Hooper TD, et al. Effectiveness of a ‘Do not interrupt’ bundled intervention to reduce interruptions during medication administration: a cluster randomised controlled feasibility study. BMJ Qual Saf 2017;26:734–42. 10.1136/bmjqs-2016-006123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mortaro A, Pascu D, Pancheri S, et al. Reducing interruptions during medication preparation and administration. Int J Health Care Qual Assur 2019;32:941–57. 10.1108/IJHCQA-12-2017-0238 [DOI] [PubMed] [Google Scholar]
- 26. Kreckler S, Catchpole K, Bottomley M, et al. Interruptions during drug rounds: an observational study. Br J Nurs 2008;17:1326–30. 10.12968/bjon.2008.17.21.31732 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. All data relevant to the study are included in the article.