Abstract
Tension-type headache (TTH) and migraine are two common primary headaches distinguished by clinical characteristics according to the 3rd edition of the International Classification of Headache Disorders. Migraine is identified by specific features such as being more prevalent in females, being aggravated by physical activity, certain genetic factors, having photophobia, phonophobia, nausea, vomiting, or aura, and responding to specific drugs. Nonetheless, TTH and migraine share some common characteristics, such as onset occurring in the 20 s, and being triggered by psychological factors like stress, moderate pain severity, and mild nausea in chronic TTH. Both conditions involve the trigeminovascular system in their pathophysiology. However, distinguishing between TTH and migraine in clinical practice, research, and epidemiological studies can be challenging, as there is a lack of specific diagnostic tests and biomarkers. Moreover, both conditions may coexist, further complicating the diagnostic process. This review aims to explore the similarities and differences in the pathophysiology, epidemiology, burden and disability, comorbidities, and responses to pharmacological and non-pharmacological treatments of TTH and migraine. The review also discusses future research directions to address the diagnostic challenges and improve the understanding and management of these conditions.
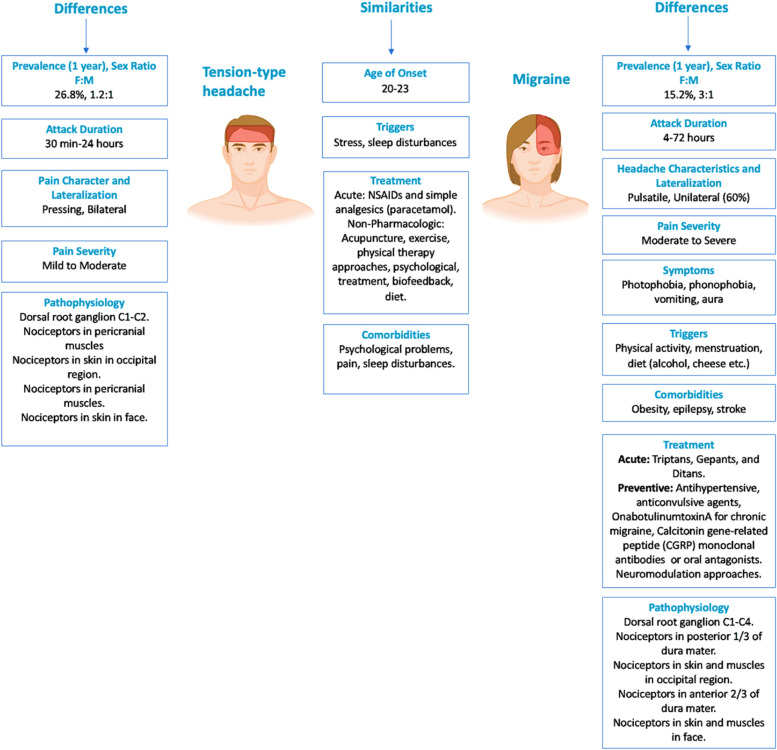
Graphical Abstract
Keywords: CGRP, Central sensitization, Headache, International Classification of Headache Disorders, Migraine, Pericranial tenderness, Tension-type headache, Triptan
Introduction
Headache disorders are prevalent neurological conditions and are estimated to affect around 50% of the general population (https://www.who.int/news-room/fact-sheets/detail/headache-disorders) [1]. Tension–type headache (TTH) and migraine are the two most prevalent primary headache disorders. While the International Classification of Headache Disorders (ICHD-3) [2] differentiates these headache conditions based on clinical characteristics, there is ongoing debate regarding the similarities and differences. The challenges associated with distinguishing TTH from migraine in clinical practice, clinical research, and epidemiological studies have been widely recognized [3, 4]. As there are currently no specific diagnostic tests and biomarkers available, the diagnosis of most primary headache disorders continues to rely solely on clinical assessment, making the diagnostic process complicated. This can result in clinicians mistakenly diagnosing a patient with migraine when they are actually experiencing TTH, and vice versa [3, 5, 6]. Moreover, the coexistence of TTH and migraine can add further complexity to the diagnosis. The Spectrum Study [6] found that 32% of patients who were initially diagnosed with TTH were later diagnosed with migraine or migrainous headache based on a neurologist’s evaluation of headache diaries and medical records kept for up to 6 months after the initial diagnosis. Of note, the current ICHD-3 diagnostic criteria for chronic migraine permit patients to have TTH-like headache [2]. This review aims to discuss the similarities and differences between TTH and migraine, with reference to current literature.
Epidemiology
According to epidemiological studies, tension-type headache (TTH) has a higher prevalence than migraine. The global 1-year prevalence for TTH is estimated to be 26.8%, while the global 1-year prevalence for migraine is 15.2% in the general population [7, 8]. It has been observed that there is no difference in the prevalence of TTH among individuals with migraine compared to individuals in the general population [8]. However, the frequency and severity of headache attacks may be higher in individuals with TTH coexistent with migraine when compared to the attacks experienced by individuals with TTH without migraine [8]. Migraine is more prevalent in females, with a female-to-male ratio of 3:1 [5]. In contrast, the prevalence in TTH is more equally distributed with a female-to-male ratio of 1.2:1, possibly indicating that hormonal factors play a bigger role in migraine than in TTH. The onset of migraine is reported by about 75% of individuals before the age of 35 years [9]. The onset of migraine may begin at any age, but it typically occurs during puberty and adolescence, and rarely after 50 years of age [10]. In comparison, the age of onset is overall lower in TTH than in migraine (< 30 years vs > 30 years) [11]. However, the prevalence of both migraine and TTH peaks between ages 35–39 years, followed by a decline [10].
One population study conducted on school-age children has reported that the 1-year prevalence of migraine was 7% [12]. In a recent review, the prevalence of both migraine (5%) and TTH (5.9%) in children (0–9 years) was reported comparably low, with no difference between boys (~ 5%) and girls (~ 6%) [7]. In adolescents (10–19 years), the prevalence increases, particularly in girls than in boys with migraine (15.3% vs 10.2%) (15.3% vs 10.2%). In contrast, the prevalence is similar between boys and girls with TTH (27.1% vs 25.5%). The review also showed that the prevalence of migraine declined (7.9%) in individuals above 65 years of age, while the prevalence of TTH further increased (32.2%) at age above 65 years (based on a single study in those above 64 years of age). These findings were in contrast to the Global Burden of Disease study, which found that the prevalence of TTH keeps declining with increasing age, including past 65 years of age, after peaking between ages 35–39 years [10].
In a 12-year longitudinal Danish population-based study, several risk factors were identified for migraine, including familial disposition, no vocational education, a high workload, and frequent TTH [13]. TTH was found to have different risk factors, including young age, female sex, poor self-rated health, not being able to relax after work, and sleeping a few hours per night. High migraine attack frequency and young age at onset (< 20 years) were found to be related to poor outcomes in migraine [14], defined as having > 14 migraine days/year either due to increased frequency or persisting high frequency of migraine. Poor outcomes in TTH were associated with baseline chronic TTH, coexisting migraine, being unmarried and sleeping problems are associated with poor outcomes in TTH [14]. In addition, poor outcome of pure TTH was associated with unilateral headache, nausea, and individual headache attack duration > 72 h, while migraine (with or without coexistent TTH) was associated with a baseline pulsating quality, severe pain intensity, photophobia, and phonophobia as well as longer duration of an individual headache attack [15].
Burden-impact-disability
Both migraine and TTH have a substantial impact on individuals and society. These primary headache disorders affect individuals at a younger age and potentially during the most productive period of their lives. According to the findings of the systematic review conducted by the Global Burden of Disease (GBD) in 2019, headache disorders are among the top ten for disability-adjusted life years (DALYs) for both females and males in the age range of 10–49 years [16]. The high number of people who suffer from migraines and TTH contributes to the burden associated with all headache disorders. In terms of years lived with a disability (YLD), migraine remains at the top of the list with 754/100,000 age-standardized YLD rates in 2019, while TTH is responsible for only 73.9/100,000 age-standardized YLDs. Both diseases have shown an increase of 7.7% and 4.1%, respectively, since 1990 [17].
In 2021, using data from population-based studies in nine different countries, it was found that there were positive correlations between migraine disability and lost paid work time was found with a statistical significance variation of < 0.05 to < 0.001 between some countries. Additionally, the association between migraine-attributed disability and lost household work time or total lost productivity (paid + household) was highly significant (p < 0.001) in almost all countries studied. The authors of the study emphasized the importance of appropriate treatment and suggested that it is reasonable to expect that migraine sufferers could recover more than twenty percent of their lost productivity [18]. A Europe-wide analysis has revealed that the average direct cost of episodic migraine (EM) was €746 per year, whereas the average direct cost of chronic migraine (CM) was €2,427 per year [19, 20]. In the United States, these costs are around three times higher [19, 21]. According to the Danish study, the number of work days lost due to TTH was 820 and the number of work days lost due to migraine was 270 per 1,000 individuals per year, indicating a greater burden of TTH [5, 22]. Studies indicate that migraine is associated with higher economic resource use and medical costs in outpatient, inpatient, and emergency admissions compared to TTH. In fact, this situation is exacerbated by the chronicity of the disease. In a 2002 study investigating the loss of productivity, it was reported as 5431 for migraine (3565 lost work days) and 2795 for TTH (1523 lost work days) in US dollars in the last 4 weeks before assessment [23]. In another study in 2020, it was stated that individuals experienced the loss of work days with a rate of 7.1% in migraine and 2.2% in TTH [24]. Therefore, there are opinions that migraine creates a greater burden compared to TTH, particularly in terms of lost work days and economic costs.
Comorbidities
Both migraine and TTH are associated with comorbidities, although there are differences in the relative frequency of some of the comorbidities between the two headache types. These differences may have clinical and therapeutic implications. Anxiety and depression are more prevalent in primary headache than in the non-headache population [25–27]. Additionally, anxiety and depression positively correlate with the frequency and intensity of headaches [28–30]. The relationship between psychiatric comorbidities and primary headaches comorbidity has been reported to be bidirectional [26, 31–33]. There is a higher prevalence of depression and anxiety in migraine (6.9% and 19.1%) than in TTH (4.5% and 12.1%) [27]. Depression in migraine is associated with an increased risk of chronification, which increases with depression severity [34]. The frequency of neck pain (NP) (90%) and low back pain (LBP) (80%) in TTH was shown to be high [35]. The headache frequency positively correlates with the frequency of NP in TTH [35, 36]. NP is 12 times more prevalent in migraine compared to non-headache controls and two times more prevalent in those with CM compared to EM [37]. The coexistence of TTH and migraine may influence the prevalence of NP in migraine, as pericranial tenderness in TTH may possibly increase the relative frequency of NP in migraine. One study showed relatively more frequent NP in patients with coexistent migraine and TTH than those with pure migraine [35]. The German Headache Consortium reported that low back pain (LBP) had a higher rate in CM and chronic TTH (CTTH) compared to those without headache, while LBP in EM and episodic TTH (ETTH) had a higher rate compared to those without headache. In fact, the rate in CM and CTTH was higher than the rate in EM and ETTH. An abnormal pain processing process may be associated with headaches and LBP [38]. One study showed a positive correlation between the number of days with TTH or migraine and the number of days with back pain in the past year [36]. Among comorbidities of primary headache disorders fibromyalgia is frequently encountered, with a prevalence of 26%, and occurring predominantly in the female and young population [39]. In patients with fibromyalgia, the lifetime prevalence of CTTH and migraine was estimated to be 48 and 56%, respectively [40]. This co-occurrence does not simply involve the sum of symptoms from both conditions but often results in an enhancement of symptoms from one condition (fibromyalgia) due to the triggering action of the other (migraine headache) [41]. The association between TTH and obesity is less studied. One study reported no association between adults with ETTH and obesity, and there is no difference in the frequency of headache when compared to individuals with normal weight [42, 43]. However, one study reported an increased risk of TTH in adolescents who were overweight or obese [44]. In contrast, there is a stronger association between migraine and obesity, supported by increased attack frequency and higher disability grades, suggesting body mass index (BMI)-dependent increased migraine severity [43, 45]. Higher BMI was associated with increased severity, frequency, and disability of migraine in children [46]. According to a population-based study, obesity is considered a risk factor for migraine chronification in overweight, obese, and morbidly obese groups, while for TTH, it is only a risk factor in the morbidly obese group [47]. Both sleep disturbance and stress are common migraine and TTH triggers [48–50]. The frequency of insomnia is higher in individuals with migraine compared to those without headache, and both migraine and non-migraine headache are more prevalent in individuals with insomnia compared to those without [51]. The prevalence of insomnia among individuals with TTH is higher than among those without headache [52]. Studies show the association between TTH and sleep issues, such as daytime sleepiness, insomnia, poor sleep quality, and shift work [5]. Insomnia is more prevalent in CTTH than ETTH [53] and sleep disorders may increase the risk of chronification in both TTH [53] and migraine [54]. Compared to TTH, migraine is more commonly associated with an increased risk of stroke (both ischemic and hemorrhagic) and myocardial infarction, especially in women and individuals with migraine with aura [55]. Studies also report the association between migraine and coronary procedures and cardiovascular mortality. TTH has not been associated with the risk of cerebrovascular or cardiovascular disease. Epilepsy is comorbid with migraine, likely in a bidirectional relationship, and may be due to shared genetic factors [56]. However, the relationship between epilepsy and TTH is less evident. According to cohort studies, 1–10% of epilepsy patients have pre-seizure headaches (30–60% of patients have a migraine-like headache, 20% of patients have TTH), and post-seizure headaches (50% of patients have a migraine-like headache) can be seen in 45% of epilepsy patients [56].
Disease phenotype
Migraine and TTH can have some overlap in their clinical features (Table 1). Diagnostic characteristics of TTH and migraine are presented in Tables 2 and 3. The ICHD-3, TTH is categorized into three subtypes: infrequent ETTH, frequent ETTH, and CTTH [57]. Migraine has been categorized as migraine with and without aura. Furthermore, similar to TTH, migraine can be classified as chronic. Chronic migraine is having at least 15 headache days a month, with at least 8 days of having migraine features headaches, for more than 3 months (Table 3) [2].
Table 1.
Clinical features of migraine and TTH
| Migraine | TTH | |
|---|---|---|
| Lateralization | Unilateral (60%) | Bilateral |
| Headache characteristics | Pulsatile | Pressing |
| Duration | 4–72 h | 30 min-24 h |
| Severity | Moderate to severe | Mild to moderate |
| Aggravated by normal physical activity | + | - |
| Nausea or Vomiting | Common | Mild nausea in CTTH |
| Photophobia, Phonophobia or Aura | Common | Typically not accompanied |
TTH Tension-type headache, CTTH Chronic tension-type headache
Table 2.
ICHD-3 diagnostic criteria for the tension-type headache
| Infrequent episodic tension-type headache with/without pericranial tenderness on manual palpation |
|
A. At least 10 episodes of headache occurring on < 1 day/month on average (< 12 days/year) and fulfilling criteria B-D B. Lasting from 30 min to 7 days C. At least two of the following four characteristics: 1. bilateral location 2. pressing or tightening (non-pulsating) quality 3. mild or moderate intensity 4. not aggravated by routine physical activity such as walking or climbing stairs D. Both of the following: 1. no nausea or vomiting 2. no more than one of photophobia or phonophobia E. Not better accounted for by another ICHD-3 diagnosis |
| Frequent episodic tension-type headache |
|
A. At least 10 episodes of headache occurring on 1–14 days/month on average for > 3 months (≥ 12 and < 180 days/year) and fulfilling criteria B-D B. Lasting from 30 min to 7 days C. At least two of the following four characteristics: 1. bilateral location 2. pressing or tightening (non-pulsating) quality 3. mild or moderate intensity 4. not aggravated by routine physical activity such as walking or climbing stairs D. Both of the following: 1. no nausea or vomiting 2. no more than one of photophobia or phonophobia E. Not better accounted for by another ICHD-3 diagnosis |
| Chronic tension-type headache |
|
A. Headache occurring on ≥ 15 days/month on average for > 3 months (≥ 180 days/year), fulfilling criteria B-D B. Lasting hours to days, or unremitting C. At least two of the following four characteristics: 1. bilateral location 2. pressing or tightening (non-pulsating) quality 3. mild or moderate intensity 4. not aggravated by routine physical activity such as walking or climbing stairs D. Both of the following: 1. no more than one of photophobia, phonophobia or mild nausea 2. neither moderate nor severe nausea nor vomiting E. Not better accounted for by another ICHD-3 diagnosis |
ICHD-3 International Classification Headache Disorders, 3 rd Edition
Table 3.
ICHD-3 diagnostic criteria for migraine
| Migraine without aura |
|
A. At least five attacks fulfilling criteria B-D B. Headache attacks lasting 4–72 h (when untreated or unsuccessfully treated) C. Headache has at least two of the following four characteristics: 1. Unilateral location 2. Pulsating quality 3. Moderate or severe pain intensity 4. Aggravation by or causing avoidance of routine physical activity (e.g. walking or climbing stairs) D. During headache at least one of the following: 1. Nausea and/or vomiting 2. Photophobia and phonophobia E. Not better accounted for by another ICHD-3 diagnosis |
| Migraine with aura |
|
A. At least two attacks fulfilling criteria B and C B. One or more of the following fully reversible aura symptoms: 1. Visual 2. Sensory 3. Speech and/or language 4. Motor 5. Brainstem 6. Retinal C. At least three of the following six characteristics: 1. At least one aura symptom spreads gradually over ≥ 5 min 2. Two or more aura symptoms occur in succession 3. Each individual aura symptom lasts 5–60 min 4. At least one aura symptom is unilateral 5. At least one aura symptom is positive 6. The aura is accompanied, or followed within 60 min, by headache D. Not better accounted for by another ICHD-3 diagnosis |
| Chronic migraine |
|
A. Headache (migraine-like or tension-type-like) on ≥ 15 days/month for > 3 months, and fulfilling criteria B and C B. Occurring in a patient who has had at least five attacks fulfilling criteria B-D for migraine without aura and/or criteria B and C for migraine with aura C. On ≥ 8 days/month for > 3 months, fulfilling any of the following: 1. Criteria C and D for migraine without aura 2. Criteria B and C for migraine with aura 3. Believed by the patient to be migraine at onset and relieved by a triptan or ergot derivative D. Not better accounted for by another ICHD-3 diagnosis |
ICHD-3 International Classification Headache Disorders, 3 rd edition
TTH is typically described as a bilateral, mild to moderate headache with a pressing or tightening quality that is not aggravated by routine physical activity [5, 58]. The headcahe is often can be described as a dull, aching pain that is felt in the forehead, temples, or back of the head, and can be described as a "hatband" or "vise-like" sensation [5, 57–59]. On the other hand, migraine usually presents as a unilateral, pulsating headache of moderate to severe intensity, although approximately 40% of patients with migraine may report bilateral headaches, and 26% report strictly unilateral headaches [60, 61]. Migraine and TTH can be triggered and aggravated by similar psychological factors such as stress, anxiety, and depressive symptoms [9, 60, 62]. Photophobia and phonophobia are more common in migraine than in TTH, with photophobia being present in over 80% of migraine patients, while nausea and vomiting are more common in migraine than in TTH, although mild nausea may be present in CTTH according to the ICHD-(3) [63, 64]. Nausea and vomiting are common symptoms in migraine but not in TTH. However, patients with CTTH may have mild nausea according to ICHD-3 [2].
Cranial autonomic symptoms are common in patients with migraine, occurring in 30–75% of cases, but are absent in patients with TTH [65–68]. Eye redness and tearing are the most commonly reported symptoms [68]. Patients with migraine commonly experience cutaneous allodynia, which can be cephalic and/or extracephalic [69, 70]. Ictal cutaneous allodynia is also frequently experienced by patients with migraine during the attack, with a relative frequency of 81.3% in episodic migraine, 92.5% in chronic migraine in clinic-based studies, and 63.2% in population studies [71, 72]. In addition, 79% of migraine patients have cutaneous allodynia when assessed with quantitative sensory testing [69]. Allodynia is more commonly reported in chronic migraine [71]. On the other hand, pericranial muscle tenderness is a common finding in TTH, particularly in CTTH [73, 74]. Both allodynia and pericranial tenderness are considered as clinical markers of central sensitization [75, 76].
Premonitory or prodromal symptoms are characteristic of migraine and include yawning, change in mood, fatigue, and neck pain. These symptoms typically occur within 2–48 h of the onset of migraine headache [55, 77, 78]. No reports exist of premonitory symptoms in patients with TTH. Migraine headaches may also be associated with menstrual periods, with changes in female sex hormone levels affecting migraine headache frequency. Migraine attacks frequently occur during the perimenstrual period and are usually improved during pregnancy [79, 80].
Pathogenesis
Genetics
The pathophysiological mechanisms underlying migraine and TTH are complex, and while there are some similarities, there are also significant differences between these two primary headaches. Furthermore, the genetic mechanisms involved in these headaches differ as well. Genetic predisposition appears to be more evident in CTTH, with a threefold increase in the risk of inheritance in first-degree relatives of individuals with CTTH [81]. However, coexistent migraine and its possible influence on TTH genetic was not evaluated in this study [81]. Genetic factors may also be more evident in frequent ETTH, but not in infrequent ETTH [55].
Several genes have been linked to CTTH, including the serotonin transporter protein (5-HTT)-gene-linked polymorphic region (5-HTTLPR) genotype and the Val158Met COMT (encoding catechol-O-methyltransferase) polymorphism [82–84]. In migraine, genetic predisposition is stronger and accounts for 40%–60% of the cases [55]. The inheritance in migraine is mostly polygenic, with a few rare exceptions such as hemiplegic migraine (CACNA1A, ATP1A2, SCN1A) and cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) (NOTCH3) [55, 59]. One extensive genome-wide meta-analysis of migraine reported 123 migraine risk loci, with 86 newly explored [85]. Following the stratification, it was found that three risk variants appear to be specific for migraine with aura (HMOX2, CACNA1A, and MPPED2), two risk variants appear to be specific for migraines without aura (near SPINK2, and near FECH), and nine risk variants increase migraine susceptibility regardless of subtype. Genes that code for current therapeutic targets for migraines, such as calcitonin gene-related peptide (CGRP) (CALCA/CALCB) and serotonin 1F receptor, are among the new risk loci identified for the disease (HTR1F) [85]. The genetic factors are stronger in migraine with aura than in migraine without aura.
Nociceptive mechanisms
The trigeminovascular system is the anatomical and physiological substrate of TTH [5] and migraine [59] and refers to the interconnected network of nerves, blood vessels, and pain-sensitive structures in the head and neck region, including muscles (see Fig. 1). The afferent fibers of the first-order trigeminovascular neurons innervate the meninges and its blood vessels, while their cell bodies are located in the trigeminal ganglion. The ascending nociceptive input projects to second-order neurons in the brainstem, including the trigeminocervical complex, which further activates and sensitizes third-order neurons in the thalamus. From here, information is projected further to the somatosensory cortex and other cortical areas leading to the perception of pain [86].
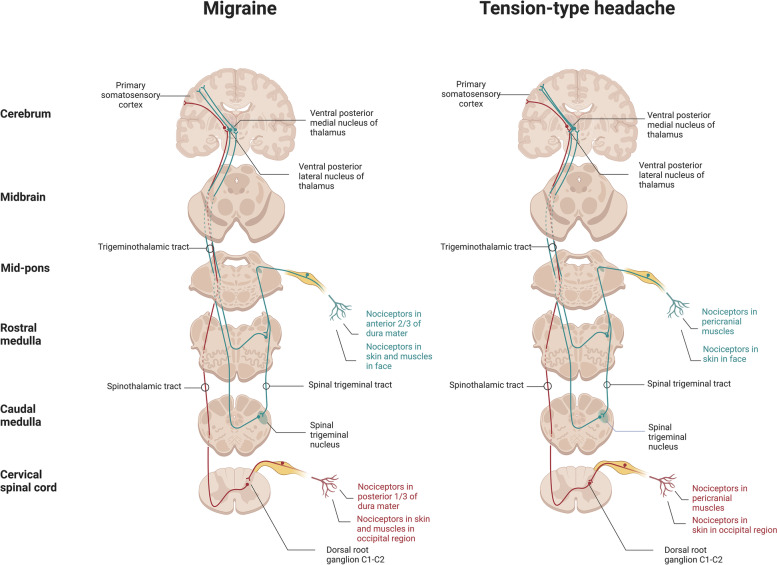
Fig. 1.
Pathophysiology of migraine and tension-type headache: nociceptive pathways
In migraine, activation and sensitization of the first-order trigeminovascular neurons, via input from the meninges and its vasculature, plays a prominent role in the onset of the nociceptive transmission, contributing to the perception of migraine pain [59, 87]. In TTH, muscular nociceptors may be involved in the initial pathophysiological events []. The input from myofascial structures via the trigeminal ganglion and the dorsal horns of the spinal cord at levels C1 to C4 contributes to headache onset in TTH. Cerebral vascular input is of minor importance in TTH compared to migraine [5, 88]. Tenderness of pericranial muscles and tendon insertions is more common in TTH than in migraine [5, 89], and is associated with increased headache frequency (more common in CTTH vs ETTH) [73, 90], intensity, and is exacerbated during the headache phase in TTH [91]. One population-based study showed that individuals with ETTH, who developed CTTH after 12 years also experienced concomitant lower pain thresholds, suggesting an association between sensitization and chronification or transformation from episodic to chronic (≥ 15 days with headache per month) headache [92]. However, pericranial tenderness is also prominent outside the headache phase in both ETTH and CTTH when compared to controls [93, 94]. In CTTH, there is a lower cutaneous and intramuscular pain detection thresholds and tolerance thresholds in both cephalic and extracephalic regions compared with controls [5].
Research suggests that the pain detection threshold is normal or low in the cephalic region of individuals with frequent ETTH, indicating that peripheral factors are more involved in this subtype of TTH [73, 95, 96]. Thus increasing headache frequency may likely lead to central sensitization, leading to the development of CTTH [76]. It is still debated whether the pericranial muscle tenderness contributes to the development of TTH attacks or is a consequence of the pain. Studies suggest that the widespread and unspecific nature of hypersensitivity in CTTH indicates that general pain sensitivity is affected at the central level [5]. In case of migraine, pericranial tenderness increases with attack frequency as well [97]. However, there is no difference in the mechanical pain threshold between individuals with chronic migraine during or outside the headache phase [98], or in the mechanical and thermal pain thresholds between episodic and chronic migraine [99]. These findings raise questions about whether central sensitization may explain the pericranial tenderness in migraine or if the tenderness is merely a secondary phenomenon of migraine attacks. In migraine, cephalic cutaneous allodynia is believed to be due to the sensitization of second-order neurons in the caudal trigeminal nucleus, while extracephalic cutaneous allodynia may be due to the sensitization of third-order thalamic neurons [55, 69].
Peripheral nociceptive fibers, originating from the C2 dorsal root ganglion, traverse the occipital muscles before innervating the posterior dura, suggesting a functional connection between intra- and extracranial structures [100]. This suggests that activation of the posterior dural nociceptors may stimulate the onset of headache and muscle tenderness instead of via the convergence of the dural and muscle nociceptors in the trigeminocervical complex [100]. Biopsies from the neck periosteum in individuals with chronic migraine and neck pain have shown increased expression of pro-inflammatory genes and decreased expression of anti-inflammatory genes [101], indicating the involvement of inflammation as a possible underlying cause of neck pain in migraine, in addition to pericranial tenderness. [91]. Studies in preclinical mouse models have shown that potential local inflammation in neck muscles leads to sensitization of muscle nociceptors with increased cytokine levels and subsequent activation of sensory afferents [102]. In individuals with frequent ETTH, increased pain sensitivity has been reported after intramuscular infusion of inflammatory substances, suggesting the onset of peripheral and central sensitization in TTH [5]. There are no consistent data on altered cytokine levels in TTH [5], while studies in migraine suggest the potential involvement of altered cytokine levels [103]. While both TTH and migraine involve pericranial muscles and myofascial factors, they differ in terms of the underlying pathways. In migraine, activation and sensitization of the first-order trigeminovascular neurons and vascular input likely play a greater role, whereas in TTH, peripheral muscular factors may be more involved, leading to central sensitization and the development of CTTH. Thus, central sensitization plays a role in both migraine and TTH. Furthermore, the central sensitization mechanism is involved in the pathophysiology of fibromyalgia [41]. This mechanism involves the impact of neuromediators on nociceptive stimulation within the central nervous system, leading to a decrease in pain threshold to various stimuli not only in localized painful areas but also in non-painful body parts [41]. Individuals with chronic headache may also exhibit heightened sensitivity to pain beyond the cephalic region [41, 69, 104]. Therefore, headache may play a role as a triggering factor for fibromyalgia in patients with migraine, TTH and fibromyalgia [41, 105, 106].
Neuropeptides
Experimental studies have shown that neuropeptides such as CGRP, pituitary adenylate-cyclase-activating polypeptide (PACAP)-38, and nitric oxide (NO)/GTN are involved in the pathophysiology of migraine [59, 85, 107]. Upon exposure to these neuropeptides, individuals with migraine develop migraine attacks, while healthy participants only report mild or no headache [59, 85]. The cAMP (mediated by CGRP and PACAP-38) and cGMP pathways (mediated by NO) and ATP-sensitive potassium (KATP) channels have been suggested to be involved in the pathophysiology of migraine [59, 85]. However, there is no change in peripheral or cranial blood or CSF levels of CGRP nor peripheral or cranial blood levels of vasoactive intestinal peptide (VIP), substance P, or neuropeptide Y in TTH, suggesting less or no prominent involvement of these peptides in the TTH pathophysiology [5, 108].
Nitric oxide
NO mechanisms appear to be involved in both migraine and TTH. GTN, a nitric oxide donor, induces migraine attacks in ~ 90% of individuals with migraine [85, 109, 110]. In one study with individuals with CTTH, after exposure to exposed to NO, the majority of individuals (~ 90%) developed TTH, while only two patients experienced an attack classified as migraine without aura [111]. These two patients described their usual TTH as both pressing and throbbing in quality, and moderate in intensity. Only a few healthy controls experienced a delayed headache after GTN, which was mainly mild in intensity, as opposed to the more pronounced headache in TTH [111]. The time to peak median headache intensity in TTH was 8 h after GTN infusion with a median pain score of 4 out of 10 [111]. In migraine, the time to peak headache intensity was earlier at 5.5 h post-infusion with a median pain score of 3 out of 10 [110]. Inhibition of nitric oxide synthase (NOS) effectively aborts migraine attacks [107, 112], and reduces the pain intensity of headache in CTTH compared to placebo [113]. NO may play a role in the development of central sensitization of nociceptive pathways, and it is likely that inhibition of NOS results in the reduction of central sensitization [113]. However, the role of NOS in chronic migraine patients has not been studied yet.
Serotonin
In CTTH, the serotonin (5-HT) levels in platelets and plasma are normal or decreased, with a normal platelet 5-HT uptake compared with controls [114, 115]. In contrast, the serotonin levels are increased in ETTH with a decreased platelet 5-HT uptake in ETTH [116]. Platelet 5-HT decreases and 5-HIAA, a primary 5-HT metabolite, increases during migraine attacks as in CTTH [117]. This suggests the involvement of serotonergic mechanisms in both migraine and TTH. Descending inhibitory pathways involve the release of 5-HT [118]. One of the rich-5-HT nuclei, the nucleus raphe magnus (NRM), is the origin of the descending serotonergic pathways, which play a role in the pathophysiology of both CTTH and migraine [5].
Pharmacological treatment
The treatment of primary headaches, including migraine and TTH, involves both non-pharmacological and pharmacological interventions [5]. Pharmacological management for these headaches can be divided into acute and preventive treatment. In the case of migraine, a stepped-care approach is recommended using three lines of acute medications [119, 120]. The first line of medications includes NSAIDs (such as aspirin, ibuprofen, or diclofenac) and simple analgesics (such as paracetamol/acetaminophen) for those intolerant to NSAIDs [55, 59, 121]. For TTH, the pharmacologic approach to acute headache episodes remains disease non-specific. Simple NSAIDs and acetaminophen are generally safe, economical, and efficacious pharmacologic treatments for TTH as in the acute treatment of migraine [11]. The European Federation of Neurological Societies Task Force (EFNS-TF) recommends the use of multiple oral NSAIDs in the treatment of TTH [122]. Among NSAIDs, ibuprofen and ketoprofen have demonstrated the highest efficacy in the treatment of TTH [16]. Furthermore, caffeine combination therapies have demonstrated improved efficacy in TTH with minimal alteration to the previous safety profile [123].
According to the step-care approach, triptans are considered second-line medications for the acute treatment of migraine [124]. Randomized controlled trials (RCTs) have shown that triptans are effective in reducing the intensity and duration of migraine headaches and improving other migraine-related symptoms, such as nausea, vomiting, and sensitivity to light and sound [125]. In one study, sumatriptan was found to have an effect on chronic tension-type headache (CTTH) compared to placebo [126]. However, the small sample size, coexistence with migraine, or central sensitization effect may limit the power of the study. Limited evidence suggests that triptans are not effective for tension-type headaches (TTH) and are not recommended [58, 122, 127].
If triptans fail or are contraindicated, the third-line medications for acute treatment of migraine include newer drugs such as gepants and ditan (lasmiditan) [128]. However, at present time, these novel medications are not yet available in many countries and have not been studied in other primary headache disorders [120].
Preventive treatment
Traditional migraine preventive medications are non-specific and were initially intended for other indications. The most frequently used are antihypertensive, antidepressant, anticonvulsive agents, and calcium-channel blockers. Onabotulinumtoxin A is effective in chronic migraine but not in chronic TTH [122]. However, more recently, a new class of drugs has been specifically developed for migraine prevention: calcitonin gene-related peptide (CGRP) monoclonal antibodies (mAbs) targeting the CGRP or its receptor, as well as oral CGRP receptor antagonists [128].
In contrast, the preventative pharmacologic approach to TTH remains disease non-specific. Preventative pharmacologic treatments for TTH are recommended only for patients diagnosed with frequent ETTH and CTTH [5, 6]. Three medications are currently recommended by the EFNS-TF for the preventative treatment of CTTH: amitriptyline, mirtazapine, and venlafaxine. These medications have proven effects on the management of CTTH [5]. Of these, amitriptyline is supported by the highest level of evidence, but also a high frequency of adverse events [129]. Of note, amitriptyline and venlafaxine have been shown to be effective in preventing migraine in clinical trials [127, 128]. These drugs are commonly used as first-line treatments for chronic migraine prevention, with amitriptyline being supported by the highest level of evidence [127, 128]. Alternative medications such as tetracyclic and atypical antidepressants are supported by a lower level of evidence for TTH prevention and are primarily reserved for patients that have reported severe adverse events or poor initial efficacy to the aforementioned therapies [5, 122]. Amitriptyline and venlafaxine have also been proven to be effective in the prevention of migraine.
Non-pharmacological treatment
The non-pharmacological interventions can have varying degrees of impact on headache symptoms, disability, and the quality of life in both TTH and migraine (Table 4). Acupuncture has been found to provide improvements in acute medication for TTH and headache intensity and frequency for migraine [130–133]. Studies on exercise interventions are more limited for TTH, but aerobic, strengthening, and stretching exercises have shown potential benefits in reducing headache duration, pain intensity, frequency, disability, quality of life, and psychological variables for both TTH and migraine [130, 134–136]. Trigger point therapy and manual therapy can also be effective in reducing headache symptoms, with trigger point therapy reducing intensity and manual therapy reducing the duration and frequency of headaches in TTH and migraine [137–139]. Physical therapy interventions such as transcutaneous electrical nerve stimulation (TENS), massage, and cold application, as well as neuromodulation applications, may also be beneficial for both TTH and migraine [140–143]. Psychological treatments [144–148] and biofeedback [149–151] can help to regulate pain pathways and improve the quality of life for both types of headaches, while diet modifications may be useful in identifying trigger foods and reducing headache severity [152–154]. It is not known whether one treatment is superior to others in either TTH or migraine, and there is a lack of evidence about the optimal duration, frequency, and number of sessions for non-pharmacological approaches [134]. Patient preferences for drug side effects or non-pharmacological approaches may be an important consideration [155]. While active physical therapy approaches have not shown negative effects, more comprehensive and long-term relaxation therapy may be required for psychological treatments [137, 156]. Further randomized controlled studies are needed for neuromodulation applications in both types of headaches [143].
Table 4.
Similarities and differences in treatment responses between TTH and migraine for non-pharmacological approaches
| TTH | Migraine | |
|---|---|---|
| Acupuncture | Medication use ↓ |
Headache intensity ↓ (Epis., Chr.) Headache days ↓ (Epis., Chr.) |
| Aerobic Exercise |
Headache duration ↓ Disability ↓ Quality of Life ↑ Psychological well-being ↑ |
Headache intensity ↓ (8–12 weeks) Headache frequency ↓ Headache duration ↓ (8–12 weeks) Medication use v (12 weeks) Disability ↓ Quality of Life ↑ Psychological well-being ↑ |
| Strengthening Exercise |
Headache intensity ↓ (3 weeks-3 months) |
Headache frequency ↓ |
| Cranio-cervical Exercises |
Headache duration ↓ (6 weeks) Medication use ↓ (6 weeks) |
Disability ↓ Neck Muscle performance ↑ |
| Stretching Exercise |
Headache frequency ↓ (6 weeks) |
Headache frequency ↓ |
| Trigger Point Therapy | Headache intensity ↓ | Not clear |
| Manuel Therapy |
Monthly headache days ↓ Headache duration ↓ |
Quality of Life ↑ |
| Spinal Manipulative Treatment |
Headache intensity ↓ (6 weeks) (Chr.) Headache frequency ↓ (6 weeks) (Chr.) Medication use ↓ (6 weeks) (Chr.) Functional well-being ↑ (Chr.) |
Headache intensity ↓ Migraine days ↓ |
| Mixed Physical Therapy |
Headache intensity ↓ (TENS, Massage, Coldpack) Muscle sensitivity ↓ (TENS, Massage, Coldpack) Headache intensity ↓ (Physical therapy + Craniocervical exercises) Headache frequency ↓ (Physical therapy + Craniocervical exercises) |
Headache frequency ↓ (Diaphragm training + Cervical mobilization + Massage + Myofascial release + Trigger Point + Passive stretch + Medications) |
| Headache duration ↓ (Physical therapy + Craniocervical exercises) | ||
| Neuromodulation Treatment |
Headache intensity ↓ Quality of Life ↑ |
Monthly headache days ↓ Headache duration ↓ Medication use ↓ |
| Psychological Treatment |
Headache frequency ↓ Disability ↓ |
Headache intensity ↓ Headache duration ↓ Disability ↓ Quality of Life ↑ |
| Biofeedback | Headache frequency ↓ | Headache frequency ↓ |
| Diet | Low-fat diet | Low-fat diet |
TENS Transcuteneous electric nerve stimulation
Lessons learned and future directions
The studies suggest that TTH and migraine are distinct primary headache disorders, despite some similarities in their clinical presentation. One major challenge in diagnosing these headaches is the lack of available biomarkers, and diagnosis is largely based on criteria and self-reporting by patients While a headache diary can be helpful, it is not optimal, and future research should explore potential biomarkers, including imaging biomarkers. Clinical distinctions between TTH and migraine include the lack of accompanying autonomic symptomatology in TTH, as well as accompanying symptoms of photophobia, phonophobia, and nausea, and worsening of headache upon routine physical activity more specific to migraine than TTH [5, 83]. TTH episodes may continue for up to 7 days, while individual migraine episodes do not last longer than 3 days, although the mechanisms involved in the termination of both types of headaches remain unknown [5]. Despite these clinical differences, TTH is often misdiagnosed as migraine, and both types of headaches are commonly underdiagnosed [3, 5, 157]. The prevalence and characteristics of TTH in individuals with coexistent migraine are similar to the general population, but TTH attacks are more severe in intensity [8]. The concurrence of migraine and TTH may occur by chance, but further investigation is needed to determine if there is a causal mechanistic relationship between the two disorders [5].
Epidemiological studies are needed to better distinguish these headaches and control for common covariate variables, such as medication overuse, age, sex, and psychiatric comorbidities. Both TTH and migraine are common primary headache disorders with a substantial disease burden, with migraine ranking at the top in terms of years lived with disability [5, 17, 157]. While current research shows a similar prevalence of migraine and TTH in children, with no difference between boys and girls, more data are needed in these age groups. From age 20–64, there is a difference in sex distribution, as migraine becomes more prevalent in females as opposed to the more equal distribution of TTH in the same age group. These data altogether further support the notion of stronger hormonal influences on migraine compared to TTH. Further investigation into this aspect of headache is needed. While both are associated with genetic factors, specific genes responsible for TTH's heritable nature remain unknown, in contrast to multiple risk loci associated with migraine [5, 85]. While muscular factors appear to play a more important role in TTH than in migraine, additional studies are needed to further explore the involvement of muscles in TTH. Recent research has demonstrated the role of neuropeptides, including CGRP, in the pathophysiology of migraine. Additionally, novel targets of interest include pituitary adenylate cyclase-activating polypeptide 38 (PACAP-38), adrenomedullin, and multiple transient receptor potential (TRP) channels. It should be recognized that significantly less is known regarding the cellular and molecular explanation of TTH. Although pharmacological provocation studies have provided valuable information leading to the discovery of the aforementioned targets of migraine pathophysiology, these results have not been thoroughly investigated in TTH. Interestingly, nitric oxide (NO) mechanisms might be involved in both migraine and TTH, which needs further investigation. Allodynia, a marker of central sensitization, has been observed in both CTTH and migraine, highlighting a potential commonality between the two conditions (164, 165). While the trigeminovascular system is implicated in both TTH and migraine, the activation and processing of nociceptive input seem to differ between the two conditions. Further research is needed to elucidate the mechanisms underlying nociceptive input in both TTH and migraine. Both neck pain and pericranial tenderness are highly prevalent in both migraine and tension-type headache (TTH), challenging the notion that the onset of TTH pain is primarily through the trigeminocervical complex compared to migraine. While vascular input in TTH appears to be of lesser significance than in migraine, further data are required to confirm this observation. In contrast, the increased risk of stroke and myocardial infarction in migraine patients supports the involvement of vascular factors in migraine rather than TTH.
Several treatments have been shown to be effective for migraine but not TTH, including onabotulinumtoxinA, antihypertensive preventatives, and triptan. NSAIDs are commonly used to treat both TTH and migraine patients; however, no additional medications have demonstrated efficacy in TTH [5]. Several novel molecular entities are undergoing clinical trials for efficacy in migraine, with a particular interest in prophylaxis. The entities of interest include CGRP and PACAP-38 targeting drugs, and drugs that target specific TRP channels.
The role of non-responsive patients remains debatable and poses the question of the benefits in further subdividing clinical cohorts by the underlying molecular mechanisms of their individual migraine attacks. Unfortunately, due to the lack of current therapeutic targets, this approach is not yet feasible for TTH patients.
Acknowledgements
The authors wish to thank Prof. Dr. Messoud Ashina from the Danish Headache Center, Department of Neurology, Rigshospitalet Glostrup, University of Copenhagen, Denmark for valuable comments and opinions on this article.
Authors’ contributions
All authors on behalf of the European Headache Federation contributed equally to the drafting and critical revisions of the manuscript. Dilara Onan took the lead in drafting the manuscript. Sait Ashina and Paolo Martelletti supervised the entire process and designed the concept of the review. All authors read and gave final approval and accepted responsibility for the manuscript. Introduction (D.O., W.D.W), Epidemiology (S.Y., O.G), Burden-Impact-Disability (F.F, S.A, M.M.Z. U.M.), Comorbidities (S.Y., O.G., A.A., Y.R.), Disease Phenotype (A.J., F.F.), Pathogenesis (S.Y., S.A., Y.R.), Pharmacological Treatment (D.O., A.A., A.J.,), Non-Pharmacological Treatment (D.O), Lessons Learned and Future Directions (W.D.W., S.Y). D.O prepared graphical abstract and Table 4. S. A. prepared Fig. 1. A.J, F.F prepared Tables 1, 2 and 3.
Funding
The publication fee for the present article was granted by a full waiver.
Availability of data and materials
There is no data available in the article, but the corresponding author can be contacted if more information is requested.
Declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
Dilara Onan, Samaira Younis, William David Wellsgatnik, Fatemeh Farham, Saulius Andruškevičius, Ana Abashidze, Asel Jusupova, Yuriy Romanenko, Oxana Grosu, Meerimgul Zamirbekovna Moldokulova, Ulkar Mursalova and Saida Saidkhodjaeva declare no conflict of interest.
Sait Ashina received honoraria for consulting from Allergan/AbbVie, Amgen, Biohaven Pharmaceuticals, Eli Lilly and Company, Impel NeuroPharma, Linpharma, Lundbeck, Novartis, Satsuma, Supernus, Teva, Theranica, Percept. Sait Ashina is an associate editor for Neurology Reviews, Frontiers in Neurology, and BMC Neurology, serves on the advisory board for the Journal of Headache and Pain, and is a member of the Education Committee of the International Headache Society. Paolo Martelletti is the Editor in Chief of The Journal of Headache and Pain and Editor-in-Chief of SN Comprehensive Clinical Medicine.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Paolo Martelletti and Sait Ashina contributed equally.
References
- 1.Stovner L, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210. doi: 10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 2.Headache Classification Committee of the International Headache Society (IHS) The ınternational classification of headache disorders. Cephalalgia. 2018;38(1):1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 3.Kaniecki RG. Migraine and tension-type headache: an assessment of challenges in diagnosis. Neurology. 2002;58(9 Suppl 6):S15–20. doi: 10.1212/WNL.58.9_suppl_6.S15. [DOI] [PubMed] [Google Scholar]
- 4.Turner DP, et al. Are migraine and tension-type headache diagnostic types or points on a severity continuum? An exploration of the latent taxometric structure of headache. Pain. 2015;156(7):1200–1207. doi: 10.1097/j.pain.0000000000000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashina S, et al. Tension-type headache. Nat Rev Dis Primers. 2021;7(1):24. doi: 10.1038/s41572-021-00257-2. [DOI] [PubMed] [Google Scholar]
- 6.Lipton RB, et al. Diagnostic lessons from the spectrum study. Neurology. 2002;58(9 Suppl 6):S27–31. doi: 10.1212/WNL.58.9_suppl_6.S27. [DOI] [PubMed] [Google Scholar]
- 7.IHME (2020) GBD Results Tool. Available from: http://ghdx.healthdata.org/gbd-results-tool. Accessed 30 Jan 2023
- 8.Rasmussen BK, et al. Interrelations between migraine and tension-type headache in the general population. Arch Neurol. 1992;49(9):914–918. doi: 10.1001/archneur.1992.00530330036012. [DOI] [PubMed] [Google Scholar]
- 9.Ashina M, et al. Migraine: epidemiology and systems of care. Lancet. 2021;397(10283):1485–1495. doi: 10.1016/S0140-6736(20)32160-7. [DOI] [PubMed] [Google Scholar]
- 10.Lancet Neurol Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954–976. doi: 10.1016/S1474-4422(18)30322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rasmussen BK. Migraine and tension-type headache in a general population: precipitating factors, female hormones, sleep pattern and relation to lifestyle. Pain. 1993;53(1):65–72. doi: 10.1016/0304-3959(93)90057-V. [DOI] [PubMed] [Google Scholar]
- 12.Wöber C, et al. Undifferentiated headache: broadening the approach to headache in children and adolescents, with supporting evidence from a nationwide school-based cross-sectional survey in Turkey. J Headache Pain. 2018;19(1):18. doi: 10.1186/s10194-018-0847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lyngberg AC, et al. Incidence of primary headache: a Danish epidemiologic follow-up study. Am J Epidemiol. 2005;161(11):1066–1073. doi: 10.1093/aje/kwi139. [DOI] [PubMed] [Google Scholar]
- 14.Lyngberg AC, et al. Prognosis of migraine and tension-type headache: a population-based follow-up study. Neurology. 2005;65(4):580–585. doi: 10.1212/01.wnl.0000172918.74999.8a. [DOI] [PubMed] [Google Scholar]
- 15.Ashina S, Lyngberg A, Jensen R. Headache characteristics and chronification of migraine and tension-type headache: A population-based study. Cephalalgia. 2010;30(8):943–952. doi: 10.1177/0333102409357958. [DOI] [PubMed] [Google Scholar]
- 16.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raggi A, et al. Incidence, prevalence and disability associated with neurological disorders in Italy between 1990 and 2019: an analysis based on the Global Burden of Disease Study 2019. J Neurol. 2022;269(4):2080–2098. doi: 10.1007/s00415-021-10774-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas H, et al. The relationship between headache-attributed disability and lost productivity: 2 Empirical evidence from population-based studies in nine disparate countries. J Headache Pain. 2021;22(1):153. doi: 10.1186/s10194-021-01362-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burch RC, Buse DC, Lipton RB. Migraine: epidemiology, burden, and comorbidity. Neurol Clin. 2019;37(4):631–649. doi: 10.1016/j.ncl.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 20.D'Amico D, et al. Multimorbidity in patients with chronic migraine and medication overuse headache. Acta Neurol Scand. 2018;138(6):515–522. doi: 10.1111/ane.13014. [DOI] [PubMed] [Google Scholar]
- 21.Bloudek LM, et al. Cost of healthcare for patients with migraine in five European countries: results from the International Burden of Migraine Study (IBMS) J Headache Pain. 2012;13(5):361–378. doi: 10.1007/s10194-012-0460-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rasmussen BK, Jensen R, Olesen J. Impact of headache on sickness absence and utilisation of medical services: a Danish population study. J Epidemiol Community Health. 1992;46(4):443–446. doi: 10.1136/jech.46.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pop PH, et al. Epidemiological aspects of headache in a workplace setting and the impact on the economic loss. Eur J Neurol. 2002;9(2):171–174. doi: 10.1046/j.1468-1331.2002.00355.x. [DOI] [PubMed] [Google Scholar]
- 24.Simić S, et al. Impact of ındividual headache types on the work and work efficiency of headache sufferers. Int J Environ Res Public Health. 2020;17(18):6918. doi: 10.3390/ijerph17186918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ashina S, et al. Neuroticism, depression and pain perception in migraine and tension-type headache. Acta Neurol Scand. 2017;136(5):470–476. doi: 10.1111/ane.12751. [DOI] [PubMed] [Google Scholar]
- 26.Song TJ, et al. Anxiety and depression in tension-type headache: a population-based study. PLoS ONE. 2016;11(10):e0165316. doi: 10.1371/journal.pone.0165316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lampl C, et al. Headache, depression and anxiety: associations in the Eurolight project. J Headache Pain. 2016;17:59. doi: 10.1186/s10194-016-0649-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Minen MT, et al. Migraine and its psychiatric comorbidities. J Neurol Neurosurg Psychiatry. 2016;87(7):741–749. doi: 10.1136/jnnp-2015-312233. [DOI] [PubMed] [Google Scholar]
- 29.Buse DC, et al. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. 2013;260(8):1960–1969. doi: 10.1007/s00415-012-6725-x. [DOI] [PubMed] [Google Scholar]
- 30.Mitsikostas DD, Thomas AM. Comorbidity of headache and depressive disorders. Cephalalgia. 1999;19(4):211–217. doi: 10.1046/j.1468-2982.1999.019004211.x. [DOI] [PubMed] [Google Scholar]
- 31.Seng EK, Seng CD. Understanding migraine and psychiatric comorbidity. Curr Opin Neurol. 2016;29(3):309–313. doi: 10.1097/WCO.0000000000000309. [DOI] [PubMed] [Google Scholar]
- 32.Breslau N, et al. Comorbidity of migraine and depression: investigating potential etiology and prognosis. Neurology. 2003;60(8):1308–1312. doi: 10.1212/01.WNL.0000058907.41080.54. [DOI] [PubMed] [Google Scholar]
- 33.Buse DC, et al. Comorbid and co-occurring conditions in migraine and associated risk of increasing headache pain intensity and headache frequency: results of the migraine in America symptoms and treatment (MAST) study. J Headache Pain. 2020;21(1):23. doi: 10.1186/s10194-020-1084-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ashina S, et al. Depression and risk of transformation of episodic to chronic migraine. J Headache Pain. 2012;13(8):615–624. doi: 10.1007/s10194-012-0479-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ashina S, et al. Prevalence of neck pain in migraine and tension-type headache: a population study. Cephalalgia. 2015;35(3):211–219. doi: 10.1177/0333102414535110. [DOI] [PubMed] [Google Scholar]
- 36.Ashina S, et al. Increased pain sensitivity in migraine and tension-type headache coexistent with low back pain: A cross-sectional population study. Eur J Pain. 2018;22(5):904–914. doi: 10.1002/ejp.1176. [DOI] [PubMed] [Google Scholar]
- 37.Al-Khazali HM, et al. Prevalence of neck pain in migraine: A systematic review and meta-analysis. Cephalalgia. 2022;42(7):663–673. doi: 10.1177/03331024211068073. [DOI] [PubMed] [Google Scholar]
- 38.Yoon MS, et al. Chronic migraine and chronic tension-type headache are associated with concomitant low back pain: results of the German headache consortium study. Pain. 2013;154(3):484–492. doi: 10.1016/j.pain.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 39.Caponnetto V, et al. Comorbidities of primary headache disorders: a literature review with meta-analysis. J Headache Pain. 2021;22(1):71. doi: 10.1186/s10194-021-01281-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kleykamp BA, et al. The prevalence of psychiatric and chronic pain comorbidities in fibromyalgia: an ACTTION systematic review. Semin Arthritis Rheum. 2021;51(1):166–174. doi: 10.1016/j.semarthrit.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 41.Giamberardino MA, et al. Impact of migraine on fibromyalgia symptoms. J Headache Pain. 2015;17:28. doi: 10.1186/s10194-016-0619-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chai NC, et al. Obesity and headache: part I–a systematic review of the epidemiology of obesity and headache. Headache. 2014;54(2):219–234. doi: 10.1111/head.12296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bigal ME, et al. Body mass index and episodic headaches: a population-based study. Arch Intern Med. 2007;167(18):1964–1970. doi: 10.1001/archinte.167.18.1964. [DOI] [PubMed] [Google Scholar]
- 44.Robberstad L, et al. An unfavorable lifestyle and recurrent headaches among adolescents: the HUNT study. Neurology. 2010;75(8):712–717. doi: 10.1212/WNL.0b013e3181eee244. [DOI] [PubMed] [Google Scholar]
- 45.Bigal ME, Liberman JN, Lipton RB. Obesity and migraine: a population study. Neurology. 2006;66(4):545–550. doi: 10.1212/01.wnl.0000197218.05284.82. [DOI] [PubMed] [Google Scholar]
- 46.Hershey AD, et al. Obesity in the pediatric headache population: a multicenter study. Headache. 2009;49(2):170–177. doi: 10.1111/j.1526-4610.2008.01232.x. [DOI] [PubMed] [Google Scholar]
- 47.Bigal ME, Lipton RB. Obesity is a risk factor for transformed migraine but not chronic tension-type headache. Neurology. 2006;67(2):252–257. doi: 10.1212/01.wnl.0000225052.35019.f9. [DOI] [PubMed] [Google Scholar]
- 48.Russell MB, et al. Migraine without aura and migraine with aura are distinct clinical entities: a study of four hundred and eighty-four male and female migraineurs from the general population. Cephalalgia. 1996;16(4):239–245. doi: 10.1046/j.1468-2982.1996.1604239.x. [DOI] [PubMed] [Google Scholar]
- 49.Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27(5):394–402. doi: 10.1111/j.1468-2982.2007.01303.x. [DOI] [PubMed] [Google Scholar]
- 50.Wang J, et al. Triggers of migraine and tension-type headache in China: a clinic-based survey. Eur J Neurol. 2013;20(4):689–696. doi: 10.1111/ene.12039. [DOI] [PubMed] [Google Scholar]
- 51.Kim J, et al. Impact of migraine on the clinical presentation of insomnia: a population-based study. J Headache Pain. 2018;19(1):86. doi: 10.1186/s10194-018-0916-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim J, et al. Insomnia in tension-type headache: a population-based study. J Headache Pain. 2017;18(1):95. doi: 10.1186/s10194-017-0805-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cho SJ, Song TJ, Chu MK. Sleep and tension-type headache. Curr Neurol Neurosci Rep. 2019;19(7):44. doi: 10.1007/s11910-019-0953-8. [DOI] [PubMed] [Google Scholar]
- 54.Odegård SS, et al. The long-term effect of insomnia on primary headaches: a prospective population-based cohort study (HUNT-2 and HUNT-3) Headache. 2011;51(4):570–580. doi: 10.1111/j.1526-4610.2011.01859.x. [DOI] [PubMed] [Google Scholar]
- 55.Ferrari MD, et al. Migraine Nat Rev Dis Primers. 2022;8(1):2. doi: 10.1038/s41572-021-00328-4. [DOI] [PubMed] [Google Scholar]
- 56.Bauer PR, et al. Headache in people with epilepsy. Nat Rev Neurol. 2021;17(9):529–544. doi: 10.1038/s41582-021-00516-6. [DOI] [PubMed] [Google Scholar]
- 57.Jensen RH. Tension-type headache - the normal and most prevalent headache. Headache. 2018;58(2):339–345. doi: 10.1111/head.13067. [DOI] [PubMed] [Google Scholar]
- 58.Bentivegna E, et al. Recent advancements in tension-type headache: a narrative review. Expert Rev Neurother. 2021;21(7):793–803. doi: 10.1080/14737175.2021.1943363. [DOI] [PubMed] [Google Scholar]
- 59.Ashina M. Migraine. N Engl J Med. 2020;383(19):1866–1876. doi: 10.1056/NEJMra1915327. [DOI] [PubMed] [Google Scholar]
- 60.Rasmussen BK, Olesen J. Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia. 1992;12(4):221–8. doi: 10.1046/j.1468-2982.1992.1204221.x. [DOI] [PubMed] [Google Scholar]
- 61.Da Silva AN, Tepper SJ, Evans RW. Side-locked and side shifting primary headaches. Headache. 2012;52(7):1178–1183. doi: 10.1111/j.1526-4610.2012.02196.x. [DOI] [PubMed] [Google Scholar]
- 62.Andress-Rothrock D, King W, Rothrock J. An analysis of migraine triggers in a clinic-based population. Headache. 2010;50(8):1366–1370. doi: 10.1111/j.1526-4610.2010.01753.x. [DOI] [PubMed] [Google Scholar]
- 63.Choi JY, et al. Usefulness of a photophobia questionnaire in patients with migraine. Cephalalgia. 2009;29(9):953–959. doi: 10.1111/j.1468-2982.2008.01822.x. [DOI] [PubMed] [Google Scholar]
- 64.Russell MB, et al. Tension-type headache in adolescents and adults: a population based study of 33,764 twins. Eur J Epidemiol. 2006;21(2):153–160. doi: 10.1007/s10654-005-6031-3. [DOI] [PubMed] [Google Scholar]
- 65.Barbanti P, et al. Unilateral cranial autonomic symptoms in migraine. Cephalalgia. 2002;22(4):256–259. doi: 10.1046/j.1468-2982.2002.00358.x. [DOI] [PubMed] [Google Scholar]
- 66.Obermann M, et al. Prevalence of trigeminal autonomic symptoms in migraine: a population-based study. Cephalalgia. 2007;27(6):504–509. doi: 10.1111/j.1468-2982.2007.01316.x. [DOI] [PubMed] [Google Scholar]
- 67.Gupta R, Bhatia MS. A report of cranial autonomic symptoms in migraineurs. Cephalalgia. 2007;27(1):22–28. doi: 10.1111/j.1468-2982.2006.01237.x. [DOI] [PubMed] [Google Scholar]
- 68.Togha M, et al. Cranial autonomic symptoms in episodic and chronic migraine: a cross sectional study in Iran. BMC Neurol. 2021;21(1):493. doi: 10.1186/s12883-021-02513-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burstein R, et al. An association between migraine and cutaneous allodynia. Ann Neurol. 2000;47(5):614–624. doi: 10.1002/1531-8249(200005)47:5<614::AID-ANA9>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 70.Burstein R, Cutrer MF, Yarnitsky D. The development of cutaneous allodynia during a migraine attack clinical evidence for the sequential recruitment of spinal and supraspinal nociceptive neurons in migraine. Brain. 2000;123(Pt 8):1703–1709. doi: 10.1093/brain/123.8.1703. [DOI] [PubMed] [Google Scholar]
- 71.Benatto MT, et al. Cutaneous allodynia is more frequent in chronic migraine, and its presence and severity seems to be more associated with the duration of the disease. Arq Neuropsiquiatr. 2017;75(3):153–159. doi: 10.1590/0004-282x20170015. [DOI] [PubMed] [Google Scholar]
- 72.Lipton RB, et al. Cutaneous allodynia in the migraine population. Ann Neurol. 2008;63(2):148–158. doi: 10.1002/ana.21211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jensen R, et al. Muscle tenderness and pressure pain thresholds in headache. A population study. Pain. 1993;52(2):193–199. doi: 10.1016/0304-3959(93)90131-8. [DOI] [PubMed] [Google Scholar]
- 74.Aaseth K, et al. Pericranial tenderness in chronic tension-type headache: the Akershus population-based study of chronic headache. J Headache Pain. 2014;15(1):58. doi: 10.1186/1129-2377-15-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Louter MA, et al. Cutaneous allodynia as a predictor of migraine chronification. Brain. 2013;136(Pt 11):3489–3496. doi: 10.1093/brain/awt251. [DOI] [PubMed] [Google Scholar]
- 76.Bendtsen L. Central sensitization in tension-type headache–possible pathophysiological mechanisms. Cephalalgia. 2000;20(5):486–508. doi: 10.1046/j.1468-2982.2000.00070.x. [DOI] [PubMed] [Google Scholar]
- 77.Blau JN. Migraine prodromes separated from the aura: complete migraine. Br Med J. 1980;281(6241):658–660. doi: 10.1136/bmj.281.6241.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Giffin NJ, et al. Premonitory symptoms in migraine: an electronic diary study. Neurology. 2003;60(6):935–940. doi: 10.1212/01.WNL.0000052998.58526.A9. [DOI] [PubMed] [Google Scholar]
- 79.Ferrari MD, et al. Migraine pathophysiology: lessons from mouse models and human genetics. Lancet Neurol. 2015;14(1):65–80. doi: 10.1016/S1474-4422(14)70220-0. [DOI] [PubMed] [Google Scholar]
- 80.van Oosterhout WPJ, et al. Female sex hormones in men with migraine. Neurology. 2018;91(4):e374–e381. doi: 10.1212/WNL.0000000000005855. [DOI] [PubMed] [Google Scholar]
- 81.Ostergaard S, et al. Comparison of first degree relatives and spouses of people with chronic tension headache. BMJ. 1997;314(7087):1092–1093. doi: 10.1136/bmj.314.7087.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Park JW, et al. Serotonin transporter polymorphism and harm avoidance personality in chronic tension-type headache. Headache. 2004;44(10):1005–1009. doi: 10.1111/j.1526-4610.2004.04194.x. [DOI] [PubMed] [Google Scholar]
- 83.Fernández-de-las-Peñas C, et al. Genetic contribution of catechol-O-methyltransferase polymorphism (Val158Met) in children with chronic tension-type headache. Pediatr Res. 2011;70(4):395–399. doi: 10.1203/PDR.0b013e318229448a. [DOI] [PubMed] [Google Scholar]
- 84.Fernández-de-Las-Peñas C, et al. Catechol-O-Methyltransferase (COMT) rs4680 Val158Met Polymorphism is associated with widespread pressure pain sensitivity and depression in women with chronic, but not episodic tension-type headache. Clin J Pain. 2019;35(4):345–352. doi: 10.1097/AJP.0000000000000684. [DOI] [PubMed] [Google Scholar]
- 85.Hautakangas H, et al. Genome-wide analysis of 102,084 migraine cases identifies 123 risk loci and subtype-specific risk alleles. Nat Genet. 2022;54(2):152–160. doi: 10.1038/s41588-021-00990-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Edvinsson JCA, et al. The fifth cranial nerve in headaches. J Headache Pain. 2020;21(1):65. doi: 10.1186/s10194-020-01134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Olesen J, et al. Origin of pain in migraine: evidence for peripheral sensitisation. Lancet Neurol. 2009;8(7):679–690. doi: 10.1016/S1474-4422(09)70090-0. [DOI] [PubMed] [Google Scholar]
- 88.Olesen J. Clinical and pathophysiological observations in migraine and tension-type headache explained by integration of vascular, supraspinal and myofascial inputs. Pain. 1991;46(2):125–132. doi: 10.1016/0304-3959(91)90066-7. [DOI] [PubMed] [Google Scholar]
- 89.Jensen R. Peripheral and central mechanisms in tension-type headache: an update. Cephalalgia. 2003;23(Suppl 1):49–52. doi: 10.1046/j.1468-2982.2003.00574.x. [DOI] [PubMed] [Google Scholar]
- 90.Langemark M, Olesen J. Pericranial tenderness in tension headache. A blind, controlled study. Cephalalgia. 1987;7(4):249–55. doi: 10.1046/j.1468-2982.1987.0704249.x. [DOI] [PubMed] [Google Scholar]
- 91.Ulrich V, Gervil M, Olesen J. The relative influence of environment and genes in episodic tension-type headache. Neurology. 2004;62(11):2065–2069. doi: 10.1212/01.WNL.0000129498.50793.8A. [DOI] [PubMed] [Google Scholar]
- 92.Buchgreitz L, et al. Increased pain sensitivity is not a risk factor but a consequence of frequent headache: a population-based follow-up study. Pain. 2008;137(3):623–630. doi: 10.1016/j.pain.2007.10.023. [DOI] [PubMed] [Google Scholar]
- 93.Ashina M, et al. Muscle hardness in patients with chronic tension-type headache: relation to actual headache state. Pain. 1999;79(2–3):201–205. doi: 10.1016/S0304-3959(98)00167-5. [DOI] [PubMed] [Google Scholar]
- 94.Bendtsen L, et al. Muscles and their role in episodic tension-type headache: implications for treatment. Eur J Pain. 2016;20(2):166–175. doi: 10.1002/ejp.748. [DOI] [PubMed] [Google Scholar]
- 95.Buchgreitz L, et al. Frequency of headache is related to sensitization: a population study. Pain. 2006;123(1–2):19–27. doi: 10.1016/j.pain.2006.01.040. [DOI] [PubMed] [Google Scholar]
- 96.Fernández-de-Las-Peñas C, et al. Evidence of localized and widespread pressure pain hypersensitivity in patients with tension-type headache: a systematic review and meta-analysis. Cephalalgia. 2021;41(2):256–273. doi: 10.1177/0333102420958384. [DOI] [PubMed] [Google Scholar]
- 97.Hvedstrup J, et al. Ictal neck pain investigated in the interictal state - a search for the origin of pain. Cephalalgia. 2020;40(6):614–624. doi: 10.1177/0333102419896369. [DOI] [PubMed] [Google Scholar]
- 98.Iljazi A, et al. Hypersensitivity to calcitonin gene-related peptide in chronic migraine. Cephalalgia. 2021;41(6):701–710. doi: 10.1177/0333102420981666. [DOI] [PubMed] [Google Scholar]
- 99.Schwedt TJ, et al. Episodic and chronic migraineurs are hypersensitive to thermal stimuli between migraine attacks. Cephalalgia. 2011;31(1):6–12. doi: 10.1177/0333102410365108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Noseda R, et al. Non-trigeminal nociceptive innervation of the posterior dura: implications to occipital headache. J Neurosci. 2019;39(10):1867–1880. doi: 10.1523/JNEUROSCI.2153-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Perry CJ, et al. Upregulation of inflammatory gene transcripts in periosteum of chronic migraineurs: Implications for extracranial origin of headache. Ann Neurol. 2016;79(6):1000–1013. doi: 10.1002/ana.24665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sutton BC, Opp MR. Acute increases in intramuscular inflammatory cytokines are necessary for the development of mechanical hypersensitivity in a mouse model of musculoskeletal sensitization. Brain Behav Immun. 2015;44:213–220. doi: 10.1016/j.bbi.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 103.Thuraiaiyah J, et al. The role of cytokines in migraine: A systematic review. Cephalalgia. 2022;42(14):1565–1588. doi: 10.1177/03331024221118924. [DOI] [PubMed] [Google Scholar]
- 104.Ashina S, et al. Generalized hyperalgesia in patients with chronic tension-type headache. Cephalalgia. 2006;26(8):940–948. doi: 10.1111/j.1468-2982.2006.01150.x. [DOI] [PubMed] [Google Scholar]
- 105.Cho SJ, et al. Fibromyalgia among patients with chronic migraine and chronic tension-type headache: a multicenter prospective cross-sectional study. Headache. 2017;57(10):1583–1592. doi: 10.1111/head.13191. [DOI] [PubMed] [Google Scholar]
- 106.Arnall CRI, et al. Headache and fibromyalgia. DOLOR. 2011;26(1):7–12. [Google Scholar]
- 107.Ashina M, et al. Human models of migraine - short-term pain for long-term gain. Nat Rev Neurol. 2017;13(12):713–724. doi: 10.1038/nrneurol.2017.137. [DOI] [PubMed] [Google Scholar]
- 108.Ashina M. Calcitonin gene-related peptide in tension-type headache. ScientificWorldJournal. 2002;2:1527–1531. doi: 10.1100/tsw.2002.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Christiansen I, et al. Glyceryl trinitrate induces attacks of migraine without aura in sufferers of migraine with aura. Cephalalgia. 1999;19(7):660–7. doi: 10.1046/j.1468-2982.1999.019007660.x. [DOI] [PubMed] [Google Scholar]
- 110.Thomsen LL, et al. A nitric oxide donor (nitroglycerin) triggers genuine migraine attacks. Eur J Neurol. 1994;1(1):73–80. doi: 10.1111/j.1468-1331.1994.tb00053.x. [DOI] [PubMed] [Google Scholar]
- 111.Ashina M, et al. Nitric oxide-induced headache in patients with chronic tension-type headache. Brain. 2000;123(Pt 9):1830–1837. doi: 10.1093/brain/123.9.1830. [DOI] [PubMed] [Google Scholar]
- 112.Lassen LH, et al. Nitric oxide synthase inhibition in migraine. Lancet. 1997;349(9049):401–402. doi: 10.1016/S0140-6736(97)80021-9. [DOI] [PubMed] [Google Scholar]
- 113.Ashina M, et al. Effect of inhibition of nitric oxide synthase on chronic tension-type headache: a randomised crossover trial. Lancet. 1999;353(9149):287–289. doi: 10.1016/S0140-6736(98)01079-4. [DOI] [PubMed] [Google Scholar]
- 114.Bendtsen L, et al. Serotonin metabolism in chronic tension-type headache. Cephalalgia. 1997;17(8):843–848. doi: 10.1046/j.1468-2982.1997.1708843.x. [DOI] [PubMed] [Google Scholar]
- 115.Bendtsen L, Mellerup ET. The platelet serotonin transporter in primary headaches. Eur J Neurol. 1998;5(3):277–282. doi: 10.1046/j.1468-1331.1998.530277.x. [DOI] [PubMed] [Google Scholar]
- 116.D'Andrea G, et al. Metabolism and menstrual cycle rhythmicity of serotonin in primary headaches. Headache. 1995;35(4):216–221. doi: 10.1111/j.1526-4610.1995.hed3504216.x. [DOI] [PubMed] [Google Scholar]
- 117.Silberstein SD. Serotonin (5-HT) and migraine. Headache. 1994;34(7):408–417. doi: 10.1111/j.1526-4610.1994.hed3407408.x. [DOI] [PubMed] [Google Scholar]
- 118.Millan MJ. Descending control of pain. Prog Neurobiol. 2002;66(6):355–474. doi: 10.1016/S0301-0082(02)00009-6. [DOI] [PubMed] [Google Scholar]
- 119.Mayans L, Walling A. Acute Migraine Headache: Treatment Strategies. Am Fam Physician. 2018;97(4):243–251. [PubMed] [Google Scholar]
- 120.Eigenbrodt AK, et al. Diagnosis and management of migraine in ten steps. Nat Rev Neurol. 2021;17(8):501–514. doi: 10.1038/s41582-021-00509-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Stephens G, Derry S, Moore RA. Paracetamol (acetaminophen) for acute treatment of episodic tension-type headache in adults. Cochrane Database Syst Rev. 2016;2016(6):Cd011889. doi: 10.1002/14651858.CD011889.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bendtsen L, et al. EFNS guideline on the treatment of tension-type headache - report of an EFNS task force. Eur J Neurol. 2010;17(11):1318–1325. doi: 10.1111/j.1468-1331.2010.03070.x. [DOI] [PubMed] [Google Scholar]
- 123.Diener HC, Gold M, Hagen M. Use of a fixed combination of acetylsalicylic acid, acetaminophen and caffeine compared with acetaminophen alone in episodic tension-type headache: meta-analysis of four randomized, double-blind, placebo-controlled, crossover studies. J Headache Pain. 2014;15(1):76. doi: 10.1186/1129-2377-15-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Goadsby PJ, et al. Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev. 2017;97(2):553–622. doi: 10.1152/physrev.00034.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ferrari MD, et al. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: detailed results and methods of a meta-analysis of 53 trials. Cephalalgia. 2002;22(8):633–658. doi: 10.1046/j.1468-2982.2002.00404.x. [DOI] [PubMed] [Google Scholar]
- 126.Brennum J, Kjeldsen M, Olesen J. The 5-HT1-like agonist sumatriptan has a significant effect in chronic tension-type headache. Cephalalgia. 1992;12(6):375–379. doi: 10.1111/j.1468-2982.1992.00375.x. [DOI] [PubMed] [Google Scholar]
- 127.Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the american headache society evidence assessment of migraine pharmacotherapies. Headache. 2015;55(1):3–20. doi: 10.1111/head.12499. [DOI] [PubMed] [Google Scholar]
- 128.Ailani J, Burch RC, Robbins MS. The American headache society consensus statement: update on integrating new migraine treatments into clinical practice. Headache. 2021;61(7):1021–1039. doi: 10.1111/head.14153. [DOI] [PubMed] [Google Scholar]
- 129.Banzi R, et al. Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) for the prevention of tension-type headache in adults. Cochrane Database Syst Rev. 2015;2015(5):Cd011681. doi: 10.1002/14651858.CD011681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pi C et al (2022) Effects on neuromodulation, acupuncture, and aerobic exercises on migraine and tension-type headache outcomes: a systematic review and meta-analysis. Medicine (Baltimore) 101(45):e30530 [DOI] [PMC free article] [PubMed]
- 131.Zheng H, et al. Topiramate, acupuncture, and BoNT-A for chronic migraine: a network meta-analysis. Acta Neurol Scand. 2021;143(5):558–568. doi: 10.1111/ane.13391. [DOI] [PubMed] [Google Scholar]
- 132.Linde K, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. 2016;2016(6):Cd001218. doi: 10.1002/14651858.CD001218.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Schytz HW, et al. Reference programme: diagnosis and treatment of headache disorders and facial pain Danish headache society 3rd edition, 2020. J Headache Pain. 2021;22(1):22. doi: 10.1186/s10194-021-01228-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Varangot-Reille C, et al. Effects of different therapeutic exercise modalities on migraine or tension-type headache: a systematic review and meta-analysis with a replicability analysis. J Pain. 2022;23(7):1099–1122. doi: 10.1016/j.jpain.2021.12.003. [DOI] [PubMed] [Google Scholar]
- 135.Woldeamanuel YW, Oliveira ABD. What is the efficacy of aerobic exercise versus strength training in the treatment of migraine? A systematic review and network meta-analysis of clinical trials. J Headache Pain. 2022;23(1):134. doi: 10.1186/s10194-022-01503-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Benatto MT, et al. Neck-specific strengthening exercise compared with placebo sham ultrasound in patients with migraine: a randomized controlled trial. BMC Neurol. 2022;22(1):126. doi: 10.1186/s12883-022-02650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Luedtke K, et al. Efficacy of interventions used by physiotherapists for patients with headache and migraine-systematic review and meta-analysis. Cephalalgia. 2016;36(5):474–492. doi: 10.1177/0333102415597889. [DOI] [PubMed] [Google Scholar]
- 138.Bove G, Nilsson N. Spinal manipulation in the treatment of episodic tension-type headache: a randomized controlled trial. JAMA. 1998;280(18):1576–1579. doi: 10.1001/jama.280.18.1576. [DOI] [PubMed] [Google Scholar]
- 139.Olesiejuk M, Marusiak J, Chalimoniuk M. Myofascial Trigger Points therapy decreases myotonometric tone and stiffness of trapezius muscle, benefits headaches and muscle pain in migraine. NeuroRehabilitation. 2023;52(2):299–310. doi: 10.3233/NRE-220237. [DOI] [PubMed] [Google Scholar]
- 140.Carlsson J, Fahlcrantz A, Augustinsson LE. Muscle tenderness in tension headache treated with acupuncture or physiotherapy. Cephalalgia. 1990;10(3):131–141. doi: 10.1046/j.1468-2982.1990.1003131.x. [DOI] [PubMed] [Google Scholar]
- 141.van Ettekoven H, Lucas C. Efficacy of physiotherapy including a craniocervical training programme for tension-type headache; a randomized clinical trial. Cephalalgia. 2006;26(8):983–991. doi: 10.1111/j.1468-2982.2006.01163.x. [DOI] [PubMed] [Google Scholar]
- 142.Bevilaqua-Grossi D, et al. Additional effects of a physical therapy protocol on headache frequency, pressure pain threshold, and improvement perception in patients with migraine and associated neck pain: a randomized controlled trial. Arch Phys Med Rehabil. 2016;97(6):866–874. doi: 10.1016/j.apmr.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 143.Martelletti P, et al. Neuromodulation of chronic headaches: position statement from the European Headache Federation. J Headache Pain. 2013;14(1):86. doi: 10.1186/1129-2377-14-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tajerian M, Clark JD. Nonpharmacological interventions in targeting pain-related brain plasticity. Neural Plast. 2017;2017:2038573. doi: 10.1155/2017/2038573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sharon H, et al. Mindfulness meditation modulates pain through endogenous opioids. Am J Med. 2016;129(7):755–758. doi: 10.1016/j.amjmed.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 146.Grazzi L, Bussone G. Italian experience of electromyographic-biofeedback treatment of episodic common migraine: preliminary results. Headache. 1993;33(8):439–441. doi: 10.1111/j.1526-4610.1993.hed3308439.x. [DOI] [PubMed] [Google Scholar]
- 147.Lee HJ, et al. Efficacy of psychological treatment for headache disorder: a systematic review and meta-analysis. J Headache Pain. 2019;20(1):17. doi: 10.1186/s10194-019-0965-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lehrer P, Eddie D. Dynamic processes in regulation and some implications for biofeedback and biobehavioral interventions. Appl Psychophysiol Biofeedback. 2013;38(2):143–155. doi: 10.1007/s10484-013-9217-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ingvaldsen SH, et al. A biofeedback app for migraine: development and usability study. JMIR Form Res. 2021;5(7):e23229. doi: 10.2196/23229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nestoriuc Y, Martin A. Efficacy of biofeedback for migraine: a meta-analysis. Pain. 2007;128(1–2):111–127. doi: 10.1016/j.pain.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 151.Nestoriuc Y, Rief W, Martin A. Meta-analysis of biofeedback for tension-type headache: efficacy, specificity, and treatment moderators. J Consult Clin Psychol. 2008;76(3):379–396. doi: 10.1037/0022-006X.76.3.379. [DOI] [PubMed] [Google Scholar]
- 152.Haghdoost F, Togha M. Migraine management: Non-pharmacological points for patients and health care professionals. Open Med (Wars) 2022;17(1):1869–1882. doi: 10.1515/med-2022-0598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Tai MS, Yap JF, Goh CB. Dietary trigger factors of migraine and tension-type headache in a South East Asian country. J Pain Res. 2018;11:1255–1261. doi: 10.2147/JPR.S158151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Domínguez-Balmaseda D, et al. Associations between fatty acid ıntake and tension-type headache: a cross-sectional study. J Clin Med. 2022;11(23):7139. doi: 10.3390/jcm11237139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Beier D, et al. Manual joint mobilisation techniques, supervised physical activity, psychological treatment, acupuncture and patient education in migraine treatment A systematic review and meta-analysis. Cephalalgia. 2022;42(1):63–72. doi: 10.1177/03331024211034489. [DOI] [PubMed] [Google Scholar]
- 156.D'Souza PJ, et al. Relaxation training and written emotional disclosure for tension or migraine headaches: a randomized, controlled trial. Ann Behav Med. 2008;36(1):21–32. doi: 10.1007/s12160-008-9046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Steiner TJ, et al. Migraine remains second among the world's causes of disability, and first among young women: findings from GBD2019. J Headache Pain. 2020;21(1):137. doi: 10.1186/s10194-020-01208-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
There is no data available in the article, but the corresponding author can be contacted if more information is requested.