Abstract
This prospective, randomized, controlled trial for parents of overweight and obese 3- to 7-year-olds was performed to assess the feasibility of a program promoting healthy eating and lifestyle by targeting parents as agents of change. The intervention was composed of 6-in-person group sessions and a customized website over 12 months. The control group received customary care. The primary outcome was feasibility of the intervention to promote healthy behavior change measured by attendance. The secondary outcome was effectiveness assessed by attaining reduced body mass index (BMI) scores, healthy behavior changes and increased parent self-efficacy. Seventy-three child-parent dyads were enrolled; 14 parents never attended any sessions. Participation in follow-up assessments did not meet the hypothesized level. Ultimate BMI scores did not differ between control and intervention groups. Parenting skills did not improve in the intervention group. This intervention to achieve healthy lifestyle changes in children via their parents as “change agents” was unsuccessful.
Keywords: children, obesity, parents, intervention, web-based
Introduction
Evidence indicates that obesity, the most common chronic disease in childhood, tracks into adolescence and adulthood and predisposes to the morbidities and premature mortality associated with hypertension, hyperlipidemia, type 2 diabetes, cardiovascular disease, and stroke.1–3 The US Preventive Services Task Force Recommendations (USPTF-2010) found evidence that multicomponent, moderate-to-high intensity behavioral interventions (>25 to 75 total hours) for obese children and adolescents ≥6 years can yield short-term improvements in weight status.4,5 However, resources for the practical replication of the few highly successful programs in the outpatient setting are extremely limited, making this an unlikely universal solution to an increasingly prevalent problem.6 Furthermore, families are unwilling or unable to devote the time necessary for participation in comprehensive programs.7,8
Pediatric providers are ideally situated to identify obese children since they are seen frequently for preventive care during their early years when treatment may be most likely to yield long-term change.9 Historically, family-based interventions have targeted the obese child and at least one or both parents. However, there are persuasive data indicating that the home environment is the most important contributor to shaping children’s eating and physical activity behaviors.10,11 Golan et al10 and Margarey et al12 convincingly demonstrate the effectiveness of an approach in which parents are the exclusive agents of change. This is especially true for the preschool and early school-aged child. Furthermore, studies suggest that children raised in authoritative homes eat healthier diets, are more physically active and have lower body mass index (BMI) levels compared with children raised with other parenting styles.13,14 Focusing an intervention on the parent who controls the home environment and can exercise positive parenting rather than the child and parent may be the best use of limited resources.15
The use of the internet as a resource for health information and as a modality to deliver health interventions has sky-rocketed in the past decade.16 A recent meta-analysis showed an improvement in outcomes for individuals using web-based interventions to achieve behavior change, including weight maintenance.17 CHESS (Comprehensive Health Enhancement System), an information and communication technology intervention developed at the University of Wisconsin in 1975, is a powerful and innovative communication tool that has been extensively studied.18–25
The objective of this study was to assess the feasibility of an innovative program designed to foster healthy eating and lifestyle in 3- to 7-year-old children by targeting their parents as agents of change.
Methods
This study, conducted in Madison, Wisconsin between November 2012 and April 2015, was a prospective, randomized, controlled trial for parents of overweight and obese 3- to 7-year-old children. Practitioners within each of 3 pediatric practices affiliated with the University of Wisconsin School of Medicine and Public Health requested a list of their patients between the ages of 30 and 83 months with a BMI ≥85th percentile who were seen for a health maintenance visit in the previous 6 months. A letter was sent to each family informing them about a study titled, “An Interactive Web-Based Intervention to Achieve Healthy Weight in Young Children.” The letter indicated that their child was eligible for this study because of their BMI; a color-coded BMI chart with their child’s BMI plotted was enclosed. The letter included a telephone number that parents were directed to call to express interest. The research nurse coordinator described the study and reviewed eligibility criteria. If parents were interested they were invited to come to the office for enrollment.
Inclusion Criteria
Families were eligible if office-based measurements verified that their 3- to 7-year-old child had a BMI ≥85th percentile, was seen for a health maintenance visit in the previous 6 months at one of the participating clinic sites and whose parents were English-speaking.
Exclusion Criteria
Children were excluded if they were known to have a developmental disorder (global cognitive impairment or motor delays) or other chronic underlying disease (eg, metabolic problem, muscle disorder, thyroid disorders, growth issues or asthma) that might be contributing to obesity. They were also excluded if they were taking a medication that would interfere with a healthy weight (eg, steroids, thyroid replacements, or antidepressants).
Informed consent was obtained for eligible children and families were randomized to an intervention or control group. The randomization code, which was concealed until the parent agreed to participate, was created by the statistician. All families/children were assessed similarly at baseline.
Data Collection
Information collected at baseline included current height (as measured by a stadiometer) and weight (as measured by a digital scale) of child and parent. Dietary intake of children, reported by a parent, was assessed using the National Cancer Institute’s automated, self-administered 24-hour recall (ASA24HR) system on 2 occasions.26 The parent completed 3 surveys: (1) Family Eating and Activity Habits Questionnaire (which measures the obesogenic factors in the environment (8 items), physical activity, including screen time (4 items), the relationship of eating to hunger (4 items) and the eating habits of the obese child and his/her parents (13 items)27,28; (2) Parental Authority Questionnaire (a revised 30-item questionnaire used to separate parenting styles into 3 prototypes: permissive, authoritarian and authoritative29; and (3) Parenting Sense of Competency Scale (a 17-item questionnaire assessing parenting self-efficacy).30
Data collection at 3, 6, and 9 months was undertaken only for families/children in the intervention group and included height, weight, BMI, BMI score, and child’s degree of overweight. The use of the CHESS website was automatically monitored and included data on which services within CHESS were used and the amount of time spent on each page.
At 12 months, data collection included height, weight, BMI, BMI score, child’s degree of overweight, and repeat surveys by their parents, including Family Eating and Activity Habits Questionnaire, Parental Authority Questionnaire and Parental Sense of Competency Scale.
The intervention was a family-based behavioral model in which healthy eating and activity was encouraged and authoritative parenting was supported. Eligible parents in the intervention group attended 6 face-to-face group meetings at weekly intervals and received group counseling from a primary care nurse. In addition to the in-person meeting, parents in the intervention group were given access to O-CHESS (Obesity-CHESS) for 1 year. After each meeting, O-CHESS was populated with materials from the session for parents to review and comment on. The intervention group had additional office visits at 3, 6, and 9 months.
Groups of 5 to 8 mothers of overweight and obese 3- to 7-year-olds met once weekly for 6 weeks at 5:30 to 6:30 pm with the “nurse champion” from the primary care office where their child received care. The meetings were held in the waiting room of one of the practices. Five topics for discussion were contained in a manual for nursing group leaders. Key messages were found on a checklist used by the group leader. Sessions were audiotaped and independently audited to confirm program fidelity. The format was a mix of short periods of didactic presentations and longer periods of interactive group discussion. Parenting skills were discussed at every session.
The sessions covered the general topics listed below:
Session 1: Principles of weight gain and loss, high-quality nutrition, and appropriate portion size (using food models and diagrams) were discussed. The O-CHESS website was introduced and passwords were distributed.
Session 2: Focused on “stimulus control” by eliminating high-calorie/low-nutrition foods from the household.
Session 3: Discussed reading labels, preparing healthy meals, and eating together at the table without screens and other distractions.
Session 4: Focused on increasing physical activity, decreasing sedentary activity, and decreasing screen time.
Session 5: Discussed parental responsibility, authoritative parenting, and parenting skills in general. Emphasized parental role in providing healthy meals, exerting stimulus control and modeling physical activity.
Session 6: Reviewed essential messages of parental responsibility, healthy eating (with focus on stimulus control and portion size), and modeling of increased physical activity and decreased sedentary activity.
The O-CHESS site was created and populated by the study coordinator with assistance from CHESS experts. It was password protected. It was a single location in which many types of information could be obtained and interaction with other parents and study coordinators was encouraged. The site contained information services (instant library with health topics related to nutrition and physical activity and answers to frequently asked questions, web links to other prescreened sources of information regarding nutrition and physical activity, local resources for current activities for children and families, personal stories that emphasized authoritative parenting, interactive discussion group, and Ask the Expert [questions were answered within 48 hours and usually sooner]). Topics included health risks of obesity, a section on shopping for food wisely, reading labels, cooking with children, healthy recipes, healthy and inexpensive meal planning, and merits of increasing physical activity and decreasing sedentary activities. Parents were trained to access and use the site by the nurse champion at the first session. Each parent accessed the site at the first visit and no less than one subsequent session as practice. The site was updated weekly. Discussion group entries were reviewed daily by the principal investigator. Parents were encouraged to share their triumphs and challenges so that all might benefit. This sympathetic, interactive, and supportive site was to become the backbone of the program, providing a convenient source for reinforcement of essential messaging provided in the face-to-face sessions.
The “control” group of children and parents received usual care. They were seen annually for well-child visits. There was no special counseling on diet and activity.
Two nurses/aides from each practice agreed to participate and be trained as “champions” in counseling. A 2-hour reading assignment included the USPTF-20104 and Expert Committee Guidelines on Obesity.31 A full day training session was conducted, which focused on (1) knowledge of obesity in children, (2) knowledge of successful interventions, including those that focus on dietary interventions and on increasing physical activity, and (3) review of content of 6 sessions specific to this program with an emphasis on successful parenting strategies in general and specifically for obese children. Three hours of training consisted of role play, with nurses taking turns at organizing a mock session with parents for each lesson.
The participating nurses, the research coordinator, Dr Wald, and Dr Ewing convened by teleconference weekly. During this conference, sessions of the previous week were discussed and there was preparation and discussion regarding the next session.
The primary aim of the study was to assess the feasibility of an intervention combining 6 face-to-face group counseling sessions with a 1-year longitudinal web-based component to help parents of overweight children promote healthy behavior change. We hypothesized that at least 70% of parents who enrolled in the program and were assigned to the intervention group would still be participating at the 3-, 6-, 9-, and 12-month follow-up in the office of the primary care provider. At least 2 reminder phone calls were made to each family for each visit.
A total of 26 families (1 parent and 1 child) from each of 3 practices (78 families) were to be enrolled in order to detect an anticipated mean difference of 8% in the BMI score change from the baseline to the 12-month visit with >80% power at the 2-sided .05 significance level, assuming an overall standard deviation of 11% and a loss to follow-up of up 10%. This difference in BMI was achieved in our previous studies.32,33 The number of parents attending each of the 6 counseling sessions in the intervention group was recorded as was the number who attended a primary care visit with their provider and nurse at 3, 6, 9, and 12 months.
The secondary outcome measures assessed the effectiveness of this intervention in achieving (1) a modest reduction of child BMI scores, (2) healthy behavior changes (related to improved nutrition and increased physical activity), and (3) an increase in self-efficacy as a parent as measured by the Parent Sense of Competency Scale.
Statistical Analysis
All outcome measures were summarized in terms of means standard deviations or frequencies and percentages. The intent-to-treat (ITT) population was used as the primary analysis population while the per-protocol (PP) population was used as a secondary analysis population. The comparisons of baseline characteristics between groups were conducted using a 2-sample t test or chi-square/Fisher’s exact test. Changes from baseline in BMI, BMI score, BMI percentiles, and parenting outcomes were evaluated using a paired t test. Normal probability plots and histograms were examined to validate the normal distribution assumption. For outcomes that did not follow a normal distribution, changes from baseline were evaluated using a nonparametric Wilcoxon signed rank test. The comparisons of changes in BMI, BMI scores, BMI percentiles, and parenting outcomes between groups were conducted using a 2-sample t test or nonparametric Wilcoxon rank sum test. All values are 2-sided and was used to define statistical significance. Statistical analysis was conducted using SAS software (SAS Institute Inc, Cary, NC), version 9.4.
Results
Enrollment
Enrollment began in November 2012, but the first group sessions were delayed until April 2013 due to sluggish recruitment. Because of slow accrual, the decision was made to extend the study and conduct a second intervention and control group in the subsequent spring (April 2014). The results of both intervention groups were combined. Figure 1 shows the combined flowchart for recruitment, retention, and analysis of patients. A total of 73 children (each with a single parent) were enrolled: 38 children were randomized to the intervention group and 35 to the control group. Fourteen parents randomized to the intervention group never attended a single session (ie, PP analysis involves 24 children in the intervention group). Dropouts were families in which the parent indicated that they did not wish to participate any longer. Patients deemed as “lost to follow-up” stopped attending sessions and did not respond to phone calls and letters.
Figure 1.
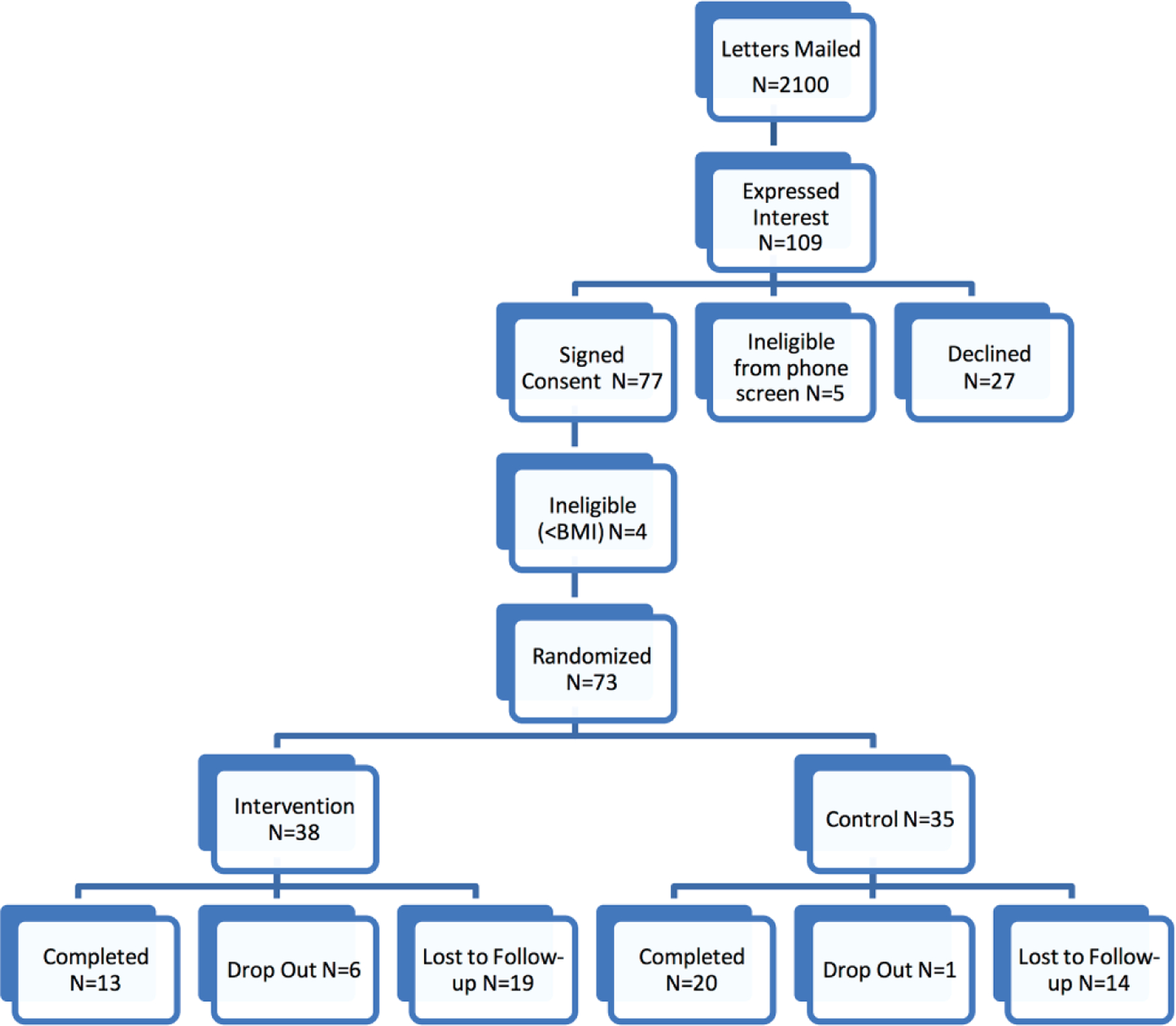
Combined flowchart for recruitment, retention, and analysis of patients. Dropouts are families that discontinue participation after notification. Lost to follow-up is the designation for subjects who discontinue attendance with refusal to respond to calls or letters.
Baseline Characteristics
Baseline characteristics of the groups are shown in Table 1. The mean age at enrollment was 5.4 () years in the control group and 5.5 () years in the intervention group (). There was no significant difference in gender, maternal age, maternal education, or type of insurance between the groups either in the ITT analysis or PP analysis. The mother was named as the primary shopper and cook for household meals in most families. The average screen time for all participants (parent and child) was about 10 hours per week. There was no difference in weight, BMI, or BMI scores for children at enrollment.
Table 1.
Baseline Characteristics.
| Characteristic | Control (N = 35) |
Intervention (N = 38) |
Total (N = 73) |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Child’s age at enrollment, y | ||||||
| ≤6 | 25 | 71 | 20 | 53 | 45 | 62 |
| >6 | 10 | 29 | 18 | 47 | 28 | 38 |
| Mean (SD) | 5.4 (1.2) | 5.5 (1.5) | 5.5 (1.4) | |||
| Gender | ||||||
| Female | 21 | 60 | 18 | 47 | 39 | 53 |
| Child’s geographic ancestry | ||||||
| Native American | 1 | 3 | 0 | 0 | 1 | 1 |
| Asian | 2 | 6 | 1 | 3 | 3 | 4 |
| Black/African American | 2 | 6 | 7 | 18 | 9 | 12 |
| White/Caucasian | 27 | 77 | 27 | 71 | 54 | 74 |
| Multiracial | 2 | 6 | 3 | 8 | 5 | 7 |
| Missing | 1 | 3 | 0 | 0 | 1 | 1 |
| Ethnicity | ||||||
| Hispanic | 7 | 20 | 7 | 18 | 14 | 19 |
| Non-Hispanic | 28 | 80 | 30 | 79 | 58 | 79 |
| Missing | 0 | 0 | 1 | 3 | 1 | 1 |
| Mother’s age, y | ||||||
| ≤40 | 26 | 74 | 30 | 79 | 56 | 77 |
| >40 | 9 | 26 | 8 | 21 | 17 | 23 |
| Mean (SD) | 38.1 (11.8) | 39.0 (11.4) | 38.5 (11.5) | |||
| Mother’s education | ||||||
| High school | 1 | 3 | 6 | 16 | 7 | 10 |
| Vocation/Technical school | 3 | 9 | 2 | 5 | 5 | 7 |
| Some college | 6 | 17 | 8 | 21 | 14 | 19 |
| College degree | 16 | 46 | 14 | 37 | 30 | 41 |
| Graduate/profession school | 8 | 23 | 7 | 18 | 15 | 21 |
| Missing | 1 | 3 | 1 | 3 | 2 | 3 |
| Marital status | ||||||
| Single | 9 | 26 | 9 | 24 | 18 | 25 |
| Married | 21 | 60 | 25 | 66 | 46 | 63 |
| Divorced | 4 | 11 | 3 | 8 | 7 | 10 |
| Separated | 1 | 3 | 0 | 0 | 1 | 1 |
| Missing | 0 | 0 | 1 | 3 | 1 | 1 |
| Insurance | ||||||
| Private | 22 | 63 | 25 | 66 | 47 | 64 |
| Public | 12 | 34 | 12 | 32 | 24 | 33 |
| None | 1 | 3 | 0 | 0 | 1 | 1 |
| Missing | 0 | 0 | 1 | 3 | 1 | 1 |
| Household income, $ | ||||||
| 0–25 000 | 9 | 26 | 9 | 24 | 18 | 25 |
| 25,000–50,000 | 7 | 20 | 5 | 13 | 12 | 16 |
| 50 000–75 000 | 4 | 11 | 7 | 18 | 11 | 15 |
| 75 000–100 000 | 6 | 17 | 5 | 13 | 11 | 15 |
| >100 000 | 6 | 17 | 10 | 26 | 16 | 22 |
| Missing | 3 | 9 | 2 | 6 | 5 | 7 |
| Majority of shopping/cooking | ||||||
| Mother | 28 | 80 | 28 | 74 | 56 | 77 |
| Father | 2 | 6 | 7 | 18 | 9 | 12 |
| Grandparents | 1 | 3 | 1 | 3 | 2 | 3 |
| Both mother and father | 3 | 9 | 1 | 3 | 4 | 5 |
| Missing | 1 | 3 | 1 | 3 | 2 | 3 |
| Child screen time (h/wk) Mean (SD) | 9.5 (6.9) | 10.4 (8.3) | 10.0 (7.6) | |||
| Parent screen time (h/wk) Mean (SD) | 9.7 (6.9) | 11.3 (9.0) | 10.5 (8.0) | |||
| Weight, kg, mean (SD) | 26.3 (6.8) | 26.9 (9.2) | 26.6 (8.1) | |||
| Body mass index, kg/m2, mean (SD) | 19.5 (3.3) | 19.9 (3.3) | 19.7 (3.3) | |||
| Body mass index z score, mean (SD) | 1.77 (0.61) | 1.85 (0.60) | 1.79 (0.57) | |||
| Parental sense of competency, mean (SD) | 47.2 (10.8) | 40.5 (7.6) | 43.9 (9.4) | |||
| Permissive style score, mean (SD) | 37.6 (5.4) | 36.3 (3.1) | 37.0 (4.4) | |||
| Authoritarian style score, mean (SD) | 29.9 (4.7) | 30.1 (4.9) | 30.0 (4.8) | |||
| Authoritative style score, mean (SD) | 19.3 (3.3) | 20.3 (4.0) | 19.8 (3.7) | |||
Each parent completed a Parental Authority Questionnaire (used to categorize parenting styles into 3 prototypes: permissive, authoritarian, and authoritative) and a Parenting Sense of Competency Scale. The mean and median score for permissive style, authoritative style, and authoritarian style were nearly identical in the intervention and control group. However, scores for parents in the control group indicated a significantly greater sense of competency than those in the intervention group ().
Attendance at Intervention Sessions
Every session was led by a trained office nurse and each session was monitored and recorded by the research coordinator. Attendance at the face-to-face sessions was variable. Families were defined as “completers” if they attended at least 4 of the 6 sessions. Thirteen of 38 (34%) were completers in the ITT analysis and 13 of 24 (54%) in the PP analysis.
Attendance/Feasibility
The primary outcome measure for this feasibility study was attendance at the 3-, 6-, 9-, and 12-month visit with the primary care provider. Although 38 children were enrolled in the intervention group, 16 (42%), 17 (45%), 15 (39%), and 11 (29%) attended follow-up visits at 3, 6, 9, and 12 months, respectively. Participation did not meet the hypothesized level of 70% at any visit. PP analysis showed rates of attendance at 66%, 71%, 63%, and 46%, respectively, for the 4 time points.
Use of O-CHESS Website
There was automatic tracking of when participants logged on to O-CHESS. All 24 intervention participants logged on to the O-CHESS site during the face-to-face sessions. Twenty-one of the 24 logged on at least 1 additional time during the first 6 weeks (Table 2). Only 7 of 24 (29%) logged on after the face-to-face sessions.
Table 2.
Use of O-CHESS Site.
| Total log ons | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Log on during face-to-face | 4 | 3 | 2 | 1 | 2 | 1 | 0 | 0 | 1 | 0 |
| Log on after face-to-face | 0 | 3 | 0 | 0 | 2 | 0 | 0 | 1 | 0 | 1 |
Abbreviation: O-CHESS, Obesity–Comprehensive Health Enhancement System.
Changes in BMI, Screen Time, and Diet at 12 Months
Among children with 12-month visits (19 control, 11 intervention), BMI scores decreased from baseline to 12 months in both the control and intervention arms, with a mean decrease in control arm of −0.36 () versus −0.28 () in the intervention arm. However, mean reductions were not significantly different between the control and intervention groups () (Table 3). When a PP analysis was performed, there was a significant decrease in both BMI score (−0.26 0.42, ) and BMI % (−4.67% 8.39%, ) from baseline to month 3 in the intervention group. However, no significant differences in changes from baseline to month 12 were observed between the 2 groups.
Table 3.
Change in Body Mass Index (BMI), BMI z Score, and BMI % From Baseline to 12-Month Visit.
| Control (N = 19) |
Intervention (N = 11) |
||||
|---|---|---|---|---|---|
| Outcome | Mean (SD) | P a | Mean (SD) | P b | P c |
| BMI | 0.1 (2.26) | .8026 | 0.3 (1.65) | .6037 | .8688 |
| BMI z score | −0.36 (0.75) | .0593 | −0.28 (0.49) | .0890 | .7492 |
| BMI % | −4.1 (9.0) | .0680 | −6.4 (8.8) | .0376 | .5193 |
P value for evaluating changes from baseline to 12-month visit within control group.
P value for evaluating changes from baseline to 12-month visit within intervention group.
P value for comparing changes between control and intervention groups.
As shown in Table 4, the percent of children who reduced their screen time by ≥15% did not differ significantly between the intervention and control groups (27% vs 31%, ). Parenting skills did not improve from baseline to 12 months among parents in the intervention group. In addition, changes in parenting skills were not significantly different between the control and intervention groups (Table 4).
Table 4.
Changes in Parenting Outcomes From Baseline to 12-Month Visit.
| Outcome | Control (N = 19) | Intervention (N = 11) | P a | |
|---|---|---|---|---|
| Child screen time (h/wk), Mean (SD) | 0.5 (5.8) | 0.6 (4.2) | .9804 | |
| Child reduced screen time by 15%, n (%) | 4 (31) | 3 (27) | 1.0000 | |
| Parental sense of competency, mean (SD) | −0.9 (8.4) | −1.6 (3.0) | .8262 | |
| Authoritative style score, mean (SD) | 0.6 (3.4) | −1.1 (3.1) | .2552 | |
P value for comparing changes between control and intervention groups.
Insufficient dietary information was obtained at baseline and follow-up to assess changes.
Discussion
Obesity in children and adolescents imposes a huge burden on their physical health and emotional well-being. Despite successfully enrolling families to begin participating in a novel program based on melding previously successful family-based interventions designed to promote healthy weight and lifestyle, we could not engage them in the longitudinal component sufficiently to demonstrate feasibility of a program combining face-to-face sessions with a web-based component.
Our previous family-based behavioral interventions (in school-age children) conducted in a primary care setting using a train-the-trainer method have been moderately successful.32,33 Targeting school-aged children was based on evidence that in a research setting this approach was successful32–34 and most published interventions have focused on the school-age child. However, there are strong data that both eating habits and patterns of physical activity are molded in early childhood and track into adulthood, suggesting that starting at an earlier age might be preferable.35–37 There have been several studies published in the past 8 years specifically focusing on reduction of obesity in the preschool age group.38–43 Most of these have been comprehensive, family-centered interventions which have demonstrated modest improvements in BMI that have been sustained over 12 months. Although family-based interventions (aimed at both children and their parents) are most common, some investigators have popularized an approach in which parents are the exclusive agents of change, thereby conserving the human resource required to intervene.12,15,27,44 Two recent systematic reviews suggest that parent-only interventions in the treatment of childhood obesity may be comparable to interventions that target parent and child with potential for cost saving.45,46 Furthermore, there is evidence that authoritative parenting may foster positive lifestyle changes.13,14
A review undertaken by the USPTF to determine the effectiveness of various behavioral interventions for obese children and adolescents 6 years and older showed that more intense interventions (at least 25 hours) are most successful at helping children achieve a healthier weight.4 However, loss to follow-up is a major issue and relapse is still common, suggesting that programs with long duration or continual reinforcement are desirable. This knowledge led to the inclusion of a longitudinal web-based component into our program. Access to a website such as CHESS seemed very attractive. It appeared to offer the creation of a social network of peers (in essence a built-in support group, available at any and all times) that could provide a longitudinal component that might be the essential ingredient to promote the sustained effort needed to change behavior and maintain the change.47 Frequent use of the CHESS platform has been the rule in most studies. Nearly half of its use occurs between 9:00 PM and 7:00 AM, underscoring the importance of availability of the intervention when convenient for the user.24
CHESS is built on the foundation of self-determination theory, which holds that three basic psychological needs must be satisfied to foster well-being: autonomy, competency, and relatedness.48,49 This theory is based on a rich tradition of research in behavior change,50 social learning,51 persuasive communication,52 motivational interviewing53 and behavioral intent.54 CHESS encourages these psychological qualities by focusing on the user’s role in deciding his or her goals (autonomy), acquiring the information and skills needed to accomplish those goals (competency, confidence, self-efficacy) and using clinical and social supports available in the system (relatedness).55 CHESS facilitates communication and bonding between participants, reinforces information transmission and, most important, promotes long term adherence (which is necessary in chronic disease) and becomes a therapeutic tool that also fosters authoritative behaviors.
After enrollment, 14 parents in the intervention group failed to attend any sessions. Furthermore, engagement of families in the use of the web-based resource was modest during the period in which face-to-face sessions were being conducted and was poor after the in-person component of the program was completed. Despite introducing several different strategies at each encounter (eg, posing a question that could be answered by accessing the O-CHESS site or attempting to initiate a dialogue), there was infrequent use of the website. Because parents did not enthusiastically engage with the website during the face-to-face sessions, the web-based modality did not become useful as a bridge after the more intense component was complete. Accordingly, the significant decrease in BMI score achieved in the first 3 months in the intervention group was not sustained at 6 or 12 months.
The CHESS intervention has been successfully employed in numerous studies for patients and families with chronic and life-threatening diseases (including breast or other cancers) and addiction.19,23–25,56 Because internet-delivered group interventions are continuously available from any location that has internet access, they offer theoretical advantages over face-to-face support groups.57 Our inability to engage families may reflect the fact that a diagnosis of obesity in their young child (despite its considerable potential morbidity) does not elicit the same parental anxiety as diagnoses of cancer and addiction and therefore the need for a support group. This is consistent with the well-known phenomenon in which parents frequently do not even recognize that their preschool child is obese.58–60 Alternatively, failure of parents to engage may reflect their own general emotional well-being and perception of strong social support.61 In addition, the initiation of involvement in this instance came from the medical establishment rather than the family’s concern. Although families consented, indicating some “readiness for change,” motivation may have been insufficient for a sustained effort.
Loss to follow-up (a high dropout rate) is a product of numerous factors and is very common in obesity treatment programs.62 Young families have many competing activities to attend during evening and weekend hours. Attendance is also influenced by degree of engagement and compliance/adherence to the program. When attendees are not really “ready for change,” they may be unable or unwilling to comply with the espoused principles and practices and may decide to forego attending out of embarrassment for failure to meet anticipated goals.
Although this study had several unique and innovative components, there were substantial limitations. Accrual was slower than expected and necessitated prolongation of enrollment and a second intervention and control group. Although food diaries would have allowed a comparison of food consumption between groups, the participants found this exercise tedious and time-consuming and did not comply. A substantial number of participants assigned to the intervention group never attended any sessions, thereby limiting our sample size (and the strength of any conclusions) and, unfortunately, we were not successful in engaging most subjects in the use of O-CHESS. The conduct of focus groups or exit interviews might have yielded insight into the failure to engage participants more fully.
In summary, our attempt to provide a combination intervention (in which a web-based interactive component complemented and then followed a face-to-face component) to achieve healthy life-style changes in young children via their parents as “agents of change” was unsuccessful. While each of these interventions has been successful on their own, blending the two, as attempted in this study, did not engage families.63 Future focus groups with parents of overweight young children may increase our understanding of the causes of failure of this program and help provide modifications to enhance success.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by a grant from the National Institute of Child Health and Human Development (R21HD068783), awarded to Ellen R. Wald.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Janssen I, Katzmarzyk PT, Srinivasan SR, et al. Utility of childhood BMI in the prediction of adulthood disease: comparison of national and international references. Obes Res 2005;13:1106–1115. [DOI] [PubMed] [Google Scholar]
- 2.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. Risk factors and adult body mass index among overweight children: the Bogalusa Heart Study. Pediatrics 2009;123:750–757. [DOI] [PubMed] [Google Scholar]
- 3.Type 2 diabetes in children and adolescents. American Diabetes Association. Pediatrics 2000;105(3 Pt 1):671–680. [DOI] [PubMed] [Google Scholar]
- 4.Barton M Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics 2010;125:361–367. [DOI] [PubMed] [Google Scholar]
- 5.US Preventive Services Task Force, Grossman DC, Bibbins-Domingo K, et al. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA 2017;317:2417–2426. [DOI] [PubMed] [Google Scholar]
- 6.Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA 2007;297:2697–2704. [DOI] [PubMed] [Google Scholar]
- 7.Golley RK, Magarey AM, Baur LA, Steinbeck KS, Daniels LA. Twelve-month effectiveness of a parent-led, family-focused weight-management program for prepubertal children: a randomized, controlled trial. Pediatrics 2007;119:517–525. [DOI] [PubMed] [Google Scholar]
- 8.Cote MP, Byczkowski T, Kotagal U, Kirk S, Zeller M, Daniels S. Service quality and attrition: an examination of a pediatric obesity program. Int J Qual Health Care 2004;16:165–173. [DOI] [PubMed] [Google Scholar]
- 9.Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr 2007;19:354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treatment of childhood obesity. Am J Clin Nutr 1998;67:1130–1135. [DOI] [PubMed] [Google Scholar]
- 11.Golan M Parents as agents of change in childhood obesity—from research to practice. Int J Pediatr Obes 2006;1:66–76. [DOI] [PubMed] [Google Scholar]
- 12.Magarey AM, Perry RA, Baur LA, et al. A parent-led family-focused treatment program for overweight children aged 5 to 9 years: the PEACH RCT. Pediatrics 2011;127:214–222. [DOI] [PubMed] [Google Scholar]
- 13.Sleddens EF, Gerards SM, Thijs C, de Vries NK, Kremers SP. General parenting, childhood overweight and obesity-inducing behaviors: a review. Int J Pediatr Obes 2011;6:e12–e27. [DOI] [PubMed] [Google Scholar]
- 14.Rhee KE, Lumeng JC, Appugliese DP, Kaciroti N, Bradley RH. Parenting styles and overweight status in first grade. Pediatrics 2006;117:2047–2054. [DOI] [PubMed] [Google Scholar]
- 15.Golan M, Kaufman V, Shahar DR. Childhood obesity treatment: targeting parents exclusively v. parents and children. Br J Nutr 2006;95:1008–1015. [DOI] [PubMed] [Google Scholar]
- 16.Devine T, Broderick J, Harris LM, Wu H, Hilfiker SW. Making quality health websites a national public health priority: toward quality standards. J Med Internet Res 2016;18:e211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of web-based vs. non-web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res 2004;6:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gustafson DH, Hawkins R, Pingree S, et al. Effect of computer support on younger women with breast cancer. J Gen Intern Med 2001;16:435–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaw BR, McTavish F, Hawkins R, Gustafson DH, Pingree S. Experiences of women with breast cancer: exchanging social support over the CHESS computer network. J Health Commun 2000;5:135–159. [DOI] [PubMed] [Google Scholar]
- 20.McTavish FM, Pingree S, Hawkins R, Gustafson D. Cultural differences in use of an electronic discussion group. J Health Psychol 2003;8:105–117. [DOI] [PubMed] [Google Scholar]
- 21.Meis TM, Gaie M, Pingree S, et al. Development of a tailored, internet-based smoking cessation intervention for adolescents. J Comput Mediated Commun 2002;7(3):1–7. [Google Scholar]
- 22.Gustafson DH, McTavish FM, Boberg E, et al. Empowering patients using computer based health support systems. Qual Health Care 1999;8:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Japuntich SJ, Zehner ME, Smith SS, et al. Smoking cessation via the internet: a randomized clinical trial of an internet intervention as adjuvant treatment in a smoking cessation intervention. Nicotine Tob Res 2006;8(suppl 1):S59–S67. [DOI] [PubMed] [Google Scholar]
- 24.Gustafson DH, McTavish FM, Stengle W, et al. Use and impact of eHealth system by low-income women with breast cancer. J Health Commun 2005;10(suppl 1):195–218. [DOI] [PubMed] [Google Scholar]
- 25.Gustafson DH, McTavish FM, Stengle W, et al. Reducing the digital divide for low-income women with breast cancer: a feasibility study of a population-based intervention. J Health Commun 2005;10(suppl 1):173–193. [DOI] [PubMed] [Google Scholar]
- 26.Subar AF, Thompson FE, Potischman N, et al. Formative research of a quick list for an automated self-administered 24-hour dietary recall. J Am Diet Assoc 2007;107:1002–1007. [DOI] [PubMed] [Google Scholar]
- 27.Golan M, Weizman A. Reliability and validity of the Family Eating and Activity Habits Questionnaire. Eur J Clin Nutr 1998;52:771–777. [DOI] [PubMed] [Google Scholar]
- 28.Golan M Fifteen years of the Family Eating and Activity Habits Questionnaire (FEAHQ): an update and review. Pediatr Obes 2014;9:92–101. [DOI] [PubMed] [Google Scholar]
- 29.Reitman D RP, Hupp SDA, Altobello C. Development and validation of the Parental Authority Questionnaire–Revised. J Psychopath Behav Assess 2002;24:119–127. [Google Scholar]
- 30.Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. J Clin Child Psychol 1989;18:167–175. [Google Scholar]
- 31.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120(suppl 4):S164–S192. [DOI] [PubMed] [Google Scholar]
- 32.Wald ER, Ewing L, Cluss P, Goldstrohm S, Cipriani L, Colborn K. Establishing a family-based intervention for overweight children in pediatric practice. Ann Fam Med 2005;3(suppl 2):S45–S47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ewing LJ, Cluss P, Goldstrohm S, et al. Translating an evidence-based intervention for pediatric overweight to a primary care setting. Clin Pediatr (Phila) 2009;48:397–403. [DOI] [PubMed] [Google Scholar]
- 34.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA 1990;264:2519–2523. [PubMed] [Google Scholar]
- 35.Russell CG, Worsley A. A population-based study of preschoolers’ food neophobia and its associations with food preferences. J Nutr Educ Behav 2008;40:11–19. [DOI] [PubMed] [Google Scholar]
- 36.Lau PW, Lee A, Ransdell L. Parenting style and cultural influences on overweight children’s attraction to physical activity. Obesity (Silver Spring, Md) 2007;15:2293–2302. [DOI] [PubMed] [Google Scholar]
- 37.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics 1998;101(3 pt 2):539–549. [PubMed] [Google Scholar]
- 38.Stark LJ, Clifford LM, Towner EK, et al. A pilot randomized controlled trial of a behavioral family-based intervention with and without home visits to decrease obesity in preschoolers. J Pediatr Psychol 2014;39:1001–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bocca G, Corpeleijn E, Stolk RP, Sauer PJ. Results of a multidisciplinary treatment program in 3-year-old to 5-year-old overweight or obese children: a randomized controlled clinical trial. Arch Pediatr Adolesc Med 2012;166:1109–1115. [DOI] [PubMed] [Google Scholar]
- 40.Kelishadi R, Zemel MB, Hashemipour M, Hosseini M, Mohammadifard N, Poursafa P. Can a dairy-rich diet be effective in long-term weight control of young children? J Am Coll Nutr 2009;28:601–610. [DOI] [PubMed] [Google Scholar]
- 41.Quattrin T, Roemmich JN, Paluch R, Yu J, Epstein LH, Ecker MA. Efficacy of family-based weight control program for preschool children in primary care. Pediatrics 2012;130:660–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Colquitt JL, Loveman E, O’Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database Syst Rev 2016;3:CD012105. doi: 10.1002/14651858.CD14012105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lanigan J, Collins S, Birbara T, Kokoreli M, Singhal A. The TrimTots programme for prevention and treatment of obesity in preschool children: evidence from two randomised controlled trials. Lancet 2013;382:S58. [Google Scholar]
- 44.Ball GD, Ambler KA, Keaschuk RA, et al. Parents as agents of change (PAC) in pediatric weight management: the protocol for the PAC randomized clinical trial. BMC Pediatr 2012;12:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ewald H, Kirby J, Rees K, Robertson W. Parent-only interventions in the treatment of childhood obesity: a systematic review of randomized controlled trials. J Public Health 2014;36:476–489. [DOI] [PubMed] [Google Scholar]
- 46.Jull A, Chen R. Parent-only vs. parent-child (family-focused) approaches for weight loss in obese and overweight children: a systematic review and meta-analysis. Obes Rev 2013;14:761–768. [DOI] [PubMed] [Google Scholar]
- 47.Gruver RS, Bishop-Gilyard CT, Lieberman A, et al. A social media peer group intervention for mothers to prevent obesity and promote healthy growth from infancy: development and pilot trial. JMIR Res Protoc 2016;5:e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68–78. [DOI] [PubMed] [Google Scholar]
- 49.Ryan RM, Deci EL. From ego depletion to vitality: theory and findings concerning the facilitation of energy available to the self. Soc Person Psychol Compass 2008;2:702–717. [Google Scholar]
- 50.Bandura A Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191–215. [DOI] [PubMed] [Google Scholar]
- 51.Rhodes F, Fishbein M, Reis J. Using behavioral theory in computer-based health promotion and appraisal. Health Educ Behav 1997;24:20–34. [DOI] [PubMed] [Google Scholar]
- 52.Hovland CL, Janis IL, Kelley HH. Communication and Persuasion New Haven, CT: Yale University Press; 1964. [Google Scholar]
- 53.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior New York, NY: Guilford Press; 1991. [Google Scholar]
- 54.Ajzen I, Fishbein M. Attitude-behavior relations: a theoretical analysis and review of empirical research. Psychol Bull 1977;84:888–918. [Google Scholar]
- 55.Williams GC, Gagne M, Ryan RM, Deci EL. Facilitating autonomous motivation for smoking cessation. Health Psychol 2002;21:40–50. [PubMed] [Google Scholar]
- 56.Gustafson DH, Johnson PR, Molfenter TD, Patton T, Shaw BR, Owens BH. Development and test of a model to predict adherence to a medical regimen. J Pharm Technol 2001;17:198–208. [Google Scholar]
- 57.Taylor C, Luce K. Computer- and internet-based psychotherapy interventions http://wwwpsychologicalscienceorg/journals/cd/12_1/Taylorcfm. Accessed September 9, 2017.
- 58.Wald ER, Ewing LJ, Cluss P, et al. Parental perception of children’s weight in a paediatric primary care setting. Child Care Health Dev 2007;33:738–743. [DOI] [PubMed] [Google Scholar]
- 59.Czajka K, Kolodziej M. Parental perception of body weight in preschool children and an analysis of the connection between selected parent-related factors and the assessment of their children’s weight. Dev Period Med 2015;19(3 pt 2):375–382. [PubMed] [Google Scholar]
- 60.Katz DL. Oblivobesity: looking over the overweight that parents keep overlooking. Child Obes 2015;11: 225–226. [DOI] [PubMed] [Google Scholar]
- 61.Kim SC, Shah DV, Namkoong K, McTavish FM, Gustafson DH. Predictors of online health information seeking among women with breast cancer: the role of social support perception and emotional well-being. J Comput Mediated Commun 2013;18:98–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miller BM, Brennan L. Measuring and reporting attrition from obesity treatment programs: a call to action! Obes Res Clin Pract 2015;9:187–202. [DOI] [PubMed] [Google Scholar]
- 63.Wentzel J, van der Vaart R, Bohlmeijer ET, van Gemert-Pijnen JE. Mixing online and face-to-face therapy: how to benefit from blended care in mental health care. JMIR Ment Health 2016;3:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]


