Graphical Abstract
Graphical Abstract.
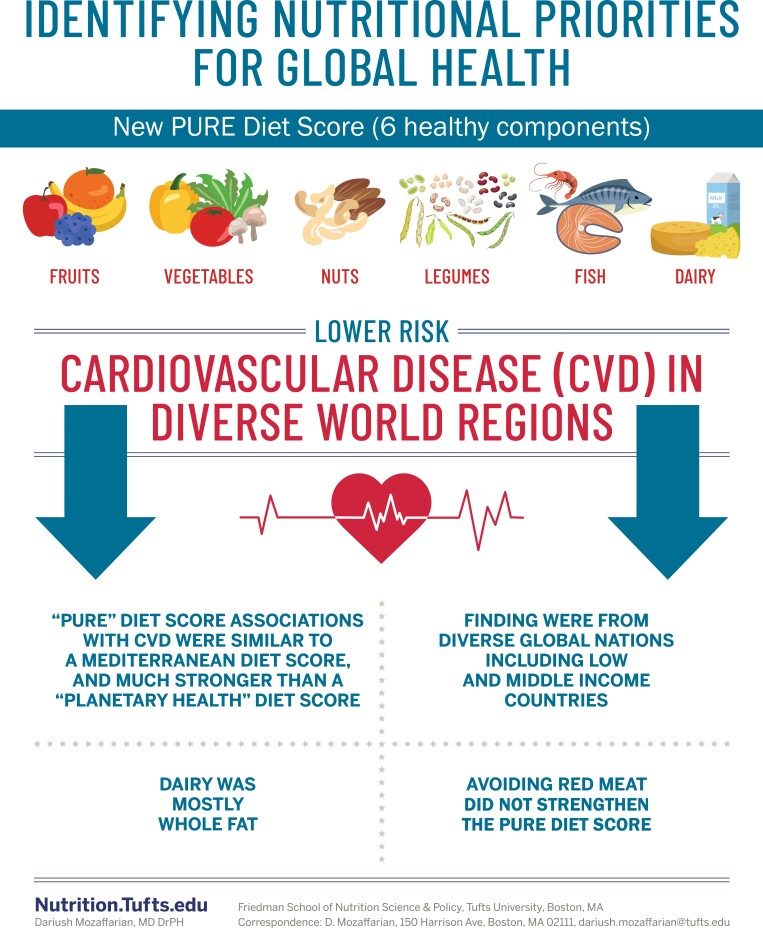
Summary of findings evaluating a new PURE diet score and cardiovascular disease and mortality including nearly 250,000 people across 80 countries.
This editorial refers to ‘Diet, cardiovascular disease, and mortality in 80 countries’, by A. Mente et al., https://doi.org/10.1093/eurheartj/ehad269.
Good nutrition is foundational for human health, and one of the top modifiable risk factors for death and disability across the world.1 Yet, few nations are on track to meet any of the multiple nutrition-related targets of the United Nations Sustainable Development Goals.1 Based on dietary intake data from the Global Dietary Database and established diet–disease relationships from epidemiological studies, the largest numbers of nutrition-related global deaths globally are attributable to insufficient intakes of protective foods including fruits, whole grains, vegetables, legumes, and nuts/seeds.1 Additional but smaller mortality burdens are attributable to insufficient fish and excess processed meats, unprocessed red meats, and sugary drinks. High dietary sodium also contributes to substantial mortality worldwide,2 while intakes of ultraprocessed foods—characterized by refined acellular nutrients, artificial additives, and depleted phytonutrients—also likely contribute3 although global intake levels and corresponding disease burdens for ultraprocessed foods have not been well characterized. Identifying sound policy, private sector, and civil society solutions to increase availability, convenience, affordability, and consumption of protective foods is a top public health priority.
In this issue of the European Heart Journal, Mente and colleagues add to this urgency by demonstrating robust, consistent associations between higher intakes of protective foods and lower risk of total mortality and cardiovascular disease (CVD) in diverse world regions.4 The investigators used previous observations of dietary habits and mortality derived from the Prospective Urban Rural Epidemiology (PURE) study, including ∼148 000 adults from 21 low, middle, and high income countries, to develop a diet score based on six components: intakes of fruits, vegetables, nuts, legumes, fish, and (mostly whole-fat) dairy. For each dietary component, one point was given for intake levels above the median, creating a final score ranging from 0 (worst) to 6 (best). The investigators assessed the risk of mortality and CVD associated with this PURE diet score, first in the PURE cohort and then in five other international studies totalling ∼97 000 adults. For comparison, several other dietary scores were calculated and evaluated, including the Healthy Eating Index (HEI), Mediterranean diet score, DASH diet score, and Planetary score.
In multivariable-adjusted analyses in the PURE cohort, each quintile (about one point) higher PURE diet score was associated with lower risk of total mortality (hazard ratio = 0.91; 95% confidence interval = 0.89–0.93], major CVD (0.94; 0.92–0.97), and their composite (0.93; 0.92–0.95). Similar associations were seen in the other international studies. Findings were consistent in adults with or without CVD and with or without diabetes at baseline. When the PURE score was evaluated with vs. without each of the food components, all six appeared generally contributory to the observed protection associations. When other dietary scores were compared with the PURE score, HEI had a generally similar association with mortality and CVD; Mediterranean, a slightly weaker association; DASH, a notably weaker association; and Planetary, no significant association. Formal assessments of prediction using area under the receiver operating characteristic curve (AUC) were consistent with these observed risk differences (the PURE score had the highest AUC, but this prediction is likely to be overestimated given that the scoring components were identified in the same cohort as the prediction). In subgroup analyses, the PURE score’s associations with death or CVD appeared stronger in lower income nations, and in South Asia and China. Consistent with this, the PURE score’s associations also appeared non-linear, with stronger associations when scores were lower (<4). In contrast, the HEI score’s associations with death or CVD appeared more linear across the whole range of HEI scores.
What are the implications of these new findings? First, these results in multiple international studies confirm prior observations from mostly Western nations5 that low intakes of fruits, vegetables, nuts, legumes, and fish are major risk factors for poor health. This suggests that common human biology, not merely confounding, explains these observed diet–disease relationships, strengthening causal inference on the power of nutrition. Second, these findings provide further support that dairy foods, including whole-fat dairy, can be part of a healthy diet. (Dairy in this study included milk, yoghurt, cheese, or mixed dishes with these foods; butter and whipped cream were not included.) As the authors discuss, prior literature suggests benefits of dairy consumption on lean body mass and protective associations for diabetes, hypertension, and metabolic syndrome, often most notable for yoghurt and cheese rather than milk, and with no consistent differences in these associations for reduced-fat vs. whole-fat dairy products.6 Biomarker studies of dairy fat intake, which avoid many of the pitfalls of self-reported diet, are supportive of these findings. One such study, including de novo individual-level analysis of 64 000 adults from 16 cohort studies in 12 nations, identified significant protective associations of blood biomarker levels of dairy fat consumption with incidence of diabetes.7 The new results in PURE, in combination with prior reports, call for a re-evaluation of unrelenting guidelines to avoid whole-fat dairy products.
A third implication relates to unprocessed red meats, the inclusion of which in the PURE score had little material effect. Furthermore, the Planetary score, which emphasizes reductions in red meat and other animal products, had no significant associations with death or CVD in PURE—and was associated with higher risk in South Asia and China. The Planetary score, developed with the aim of addressing both health and sustainability, has been associated with lower incidence of disease outcomes in some but not all Western cohorts.8–10 This suggests imperfect overlap in nutritional priorities for human disease vs. planetary sustainability. In addition, relationships of the Planetary score have not always been reported with vs. without red meat as a component, raising uncertainty as to the specific contribution of red meat to the observations. Earlier meta-analyses of published cohorts suggest modest associations of red meat intake with CVD, although generally based on few (n = 3–6) cohorts, raising concern for publication bias. Pooled results from a larger number of cohorts (n = 11) show positive associations of red meat intake with incident diabetes, consistent with mechanistic harms of excess dietary iron and associations of higher body iron stores with type 2 diabetes.11 The net health effects of unprocessed red meats remain uncertain—a high priority area for further investigation. Based on current data, the authors’ findings and conclusions appear sound, providing evidence that unprocessed red meats are not a priority target for health to either avoid (as strongly emphasized by the EAT-Lancet report) or to include (as strongly emphasized by ‘paleo’ and ‘keto’ diets).’
In sum, this new report from the PURE study provides valuable confirmatory evidence from diverse nations on the importance of health-protecting foods such as fruits, whole grains, vegetables, legumes, nuts/seeds, and dairy. These results are highly consistent with most dietary guidelines around the world (except for current guidelines often emphasizing low-fat, rather than any fat, dairy). Notably, the findings do not support the authors’ conclusion that ‘the key to a healthy diet is probably one that includes diverse natural foods in moderation’, or ‘the ideal diet for each population is likely one of variety and moderation’. Rather, the findings support targeting specific foods, including higher levels of fruits and vegetables (in the top quintile of the PURE score, 5 servings/day), dairy (2 servings/day), and nuts (1.2 servings/day), and at least moderate levels of legumes (0.5 servings/day) and fish (0.3 servings/day). The present findings provide no support for major health benefits of inclusion or ‘variety and moderation’ of other ‘natural foods’ such as red meat, poultry, or butter.
Investigations such as the one by Mente and colleagues remind us of the continuing and devastating rise in diet-related chronic diseases globally, and of the power of protective foods to help address these burdens. Advances in nutrition science and national dietary guidelines are converging on minimally processed, fibre- and phytonutrient-rich plant foods, together with fish and fermented dairy products (yoghurt, cheese, etc.), as top priorities for health. Unfortunately, as the authors also warn us, ‘despite these changes, public purchasing choices, industry formulations, and policy actions have not yet been updated with this newer evidence. For example, the public and industry remain heavily focused on low-fat foods and… policy actions (e.g. front-of-package nutrition labels in the UK, Chile’s black box warning labels, and recently proposed warning labels in Canada) remain mainly focused on reducing certain nutrients…’.
As the authors appropriately conclude, ‘while the findings from PURE are largely consistent with the nutrition science and modern dietary recommendations to focus on protective foods, the public’s understanding of healthy eating and relevant global policies has not yet caught up to this science’. It is time for national nutrition guidelines, private sector innovations, government tax policy and agricultural incentives, food procurement policies, labelling and other regulatory priorities, and food-based healthcare interventions to catch up to the science. Millions of lives depend on it.
Acknowledgements
The author is grateful to Ink&Pixel Agency for assistance with the Graphical Abstract.
Data availability
No data were generated or analysed for or in support of this paper.
Funding
This work was supported by the National Institutes of Health (R01 HL115189).
References
- 1. Global Nutrition Report . 2021 Global Nutrition Report: the state of global nutrition. 2021. https://globalnutritionreport.org/reports/2021-global-nutrition-report/. (17 June 2021).
- 2. Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med 2014;371:624–634. 10.1056/NEJMoa1304127 [DOI] [PubMed] [Google Scholar]
- 3. Juul F, Deierlein AL, Vaidean G, Quatromoni PA, Parekh N. Ultra-processed foods and cardiometabolic health outcomes: from evidence to practice. Curr Atheroscler Rep 2022;24:849–860. 10.1007/s11883-022-01061-3 [DOI] [PubMed] [Google Scholar]
- 4. Mente A, Dehghan M, Rangarajan S, O'Donnell M, Hu W, Dagenais G, et al. Diet, cardiovascular disease, and mortality in 80 countries. Eur Heart J 2023;44:2560–2579. 10.1093/eurheartj/ehad269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Miller V, Micha R, Choi E, Karageorgou D, Webb P, Mozaffarian D. Evaluation of the quality of evidence of the association of foods and nutrients with cardiovascular disease and diabetes: a systematic review. JAMA Netw Open 2022;5:e2146705. 10.1001/jamanetworkopen.2021.46705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Feng Y, Zhao Y, Liu J, Huang Z, Yang X, Qin P, et al. Consumption of dairy products and the risk of overweight or obesity, hypertension, and type 2 diabetes mellitus: a dose–response meta-analysis and systematic review of cohort studies. Adv Nutr 2022;13:2165–2179. 10.1093/advances/nmac096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Imamura F, Fretts A, Marklund M, Ardisson Korat AV, Yang WS, Lankinen M, et al. Fatty acid biomarkers of dairy fat consumption and incidence of type 2 diabetes: a pooled analysis of prospective cohort studies. PLoS Med 2018;15:e1002670. 10.1371/journal.pmed.1002670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang S, Dukuzimana J, Stubbendorff A, Ericson U, Borné Y, Sonestedt E. Adherence to the EAT-Lancet diet and risk of coronary events in the Malmo Diet and Cancer cohort study. Am J Clin Nutr 2023;117:903–909. 10.1016/j.ajcnut.2023.02.018 [DOI] [PubMed] [Google Scholar]
- 9. Berthy F, Brunin J, Allès B, Fezeu LK, Touvier M, Hercberg S, et al. Association between adherence to the EAT-Lancet diet and risk of cancer and cardiovascular outcomes in the prospective NutriNet-sante cohort. Am J Clin Nutr 2022;116:980–991. 10.1093/ajcn/nqac208 [DOI] [PubMed] [Google Scholar]
- 10. Stubbendorff A, Sonestedt E, Ramne S, Drake I, Hallström E, Ericson U. Development of an EAT-Lancet index and its relation to mortality in a Swedish population. Am J Clin Nutr 2022;115:705–716. 10.1093/ajcn/nqab369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Miao R, Fang X, Zhang Y, Wei J, Zhang Y, Tian J. Iron metabolism and ferroptosis in type 2 diabetes mellitus and complications: mechanisms and therapeutic opportunities. Cell Death Dis 2023;14:186. 10.1038/s41419-023-05708-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data were generated or analysed for or in support of this paper.