Abstract
Background/purpose
Additive manufacturing (AM), also known as 3D printing, has the potential to transform the industry. While there have been advancements in using AM for dental restorations, there is still a need for further research to develop functional biomedical and dental materials. It’s crucial to understand the current status of AM technology and research trends to advance dental research in this field. The aim of this study is to reveal the current status of international scientific publications in the field of dental research related to AM technologies.
Materials and methods
In this study, a systematic scoping review was conducted using appropriate keywords within the scope of international scientific publishing databases (PubMed and Web of Science). The review included related clinical and laboratory research, including both human and animal studies, case reports, review articles, and questionnaire studies. A total of 187 research studies were evaluated for quantitative synthesis in this review.
Results
The findings highlighted a rising trend in research numbers over the years (From 2012 to 2022). The most publications were produced in 2020 and 2021, with annual percentage increases of 25.7% and 26.2%, respectively. The majority of AM-related publications in dentistry research originate from Korea. The pioneer dental sub-fields with the ost publications in its category are prosthodontics and implantology, respectively.
Conclusion
The final review result clearly stated an expectation for the future that the research in dentistry would concentrate on AM technologies in order to increase the new product and process development in dental materials, tools, implants and new generation modelling strategy related to AM. The results of this work can be used as indicators of trends related to AM research in dentistry and/or as prospects for future publication expectations in this field.
Keywords: Additive manufacturing, 3D-printing, Dentistry, Dental research, Orthodontics, Prosthodontics, Implantology
1. Introduction
Design and production of a final form or a prototype for new concept/re-designed products thorough conventional methods might not be effective in the manner of design flexibility, manufacturability and production cost and it could be time-consuming most especially for complex forms. As an alternative solution, additive manufacturing (AM) has gained increasing attention from related users and decision-makers, consequently it has been actively utilised in many fields such as art, architecture, fashion design, machinery manufacturing, medical, aerospace, automotive, defence and food industries because of its advantages such as flexible design and manufacturing, shorter prototyping time, ease of manufacturing of complex formed products, lower design and manufacturing cost [1,2]. Companies now incorporate AM technologies into the overall manufacturing process. Research for Wohlers Report 2022 shows AM industry growth of 19.5% in 2021. This is up from 7.5% growth in 2020 [3]. Rapid prototyping, three-dimensional (3D) printing, and digital manufacturing are some of the nomenclatures that have been used to refer to this technique over time. The “ISO/ASTM 52900-21” standard defines its present name as ‘additive manufacturing’ [4]. AM technology is a potent manufacturing process that has been increasingly used in biomedical engineering since the late 1980s. The ability to fabricate improved complex and customized biomedical products enables this technology to rapidly diffuse all healthcare areas, including dentistry [5].
1.1. Fundamental principle of additive manufacturing
There are different AM technologies, with each having its own advantages, challenges, material types, and printing procedures, although the basis of them all is layer-by-layer production [6]. Today, available methods of production of the physical models through AM technologies can be categorised into seven groups according to the international standard of ISO/ASTM52900-21 (Additive manufacturing-general principles-fundamentals and vocabulary). These processes fall into the following categories: directed energy deposition (DED), material extrusion (MEX), material jetting (MJT), powder bed fusion (PBF), sheet lamination (SHL) and vat photopolymerization (VPP) [4]. Specific to the biomedical field, different materials with varying degrees of precision are available within these AM methods.
The first step of the typical process for three-dimensional (3D) printing of biomedical products is creating 3D models which is provided by obtaining the images from conventional computer-aided design (CAD) modelling of a patient through medical data capture methods such as magnetic resonance imaging (MRI), and computed tomography (CT). The second step is converting the data obtained from the patient into a 3D virtual model using CAD software. Then, the model is exported as a digital file, usually in the stereolithography (STL) file format. The STL file data is then sliced to create a series of two-dimensional (2D) layers, where each layer represents a cross-section of the 3D virtual model. Using the resulting 2D sliced data, the AM machine repositions materials, biomolecules, and even living cells layer-by-layer with extreme precision to produce 3D objects. These objects may require post-processing to remove support materials or improve structural properties in some cases [7]. The development of biocompatible and printable materials makes AM technologies increasingly useful in different clinical applications.
1.2. Historical progress of AM technologies
The patent of the first 3D printer for stereolithography, which used ultra violet (UV) light to produce 3D solid objects from photo-curable liquid polymer, was obtained by Hull in 1986 [8]. The selective laser sintering (SLS), which sinters solid powders layer-by-layer by using a laser beam, is also unveiled in 1986 by Deckard [9]. In the same period, Sachs et al. [10] proposed a novel powder bed-based method named 3D powder binding (3DPB). In 1989, Crump invented fused deposition modelling (FDM) which fabricates a 3D object by depositing layers of a heat-softened polymer onto a build platform [11]. Subsequently, a laminated object manufacturing technique was developed for making 3D objects, which uses a laser and adhesive system [12]. More recently, four-dimensional (4D) printing was announced by Tibbits in 2013 [13]. 4D printing appears based on the 3D printing facility and smart material and design [14]. In 4D printing, time is used as the fourth dimension, aside from/in addition to the conventional 3D space, allowing the production of smart objects, which can change their shape, function, or properties over time in response to available stimuli such as temperature, wind, water, and light [[15], [16], [17], [18], [19], [20]].
1.3. Research fields related to AM in dentistry
AM technologies have been utilised in many areas of dentistry for the last 20 years [1]. The main applications in dentistry vary from prototype models for anatomy teaching guidance to implants and personalized orthodontic brackets. When the use of AM technologies is reviewed in relation to the field of dentistry, it is seen that reconstruction (restoring the normal anatomy of the maxillofacial region) and orthognathic surgery (3D-printed surgical guiding templates to treat skeletal malocclusion) are the most significant current applications in Maxillofacial Surgery. Therefore, denture implantation (customized dental implants), auto-transplantation and allogenic tooth transplantation with a custom-made implant drill using AM systems have completely transformed approaches for Implantology [21]. Fixed partial dentures, removable partial or complete dentures, and facial prostheses are the prosthetic restorations commonly used with AM technology in Prosthodontics [21]. Additionally, CAD and computer-aided manufacturing (CAM) techniques have become increasingly popular in both dental laboratory and clinical dentistry over the past three decades. CAD-CAM technology offers several advantages to patients, including a decrease in the number of clinical visits, reduction in manufacturing costs, and time. Complete removable dental prostheses (CRDPs) manufactured using CAD-CAM technology are a prime example of this [22]. As knowledge on this subject continues to increase and materials and techniques continue to advance, it is anticipated that the importance of additive manufacturing, particularly in the production of prostheses, will also increase in the coming years [23] Furthermore, the study showed that methylmethacrylate concentrations were significantly lower in 3D-printed CRDPs than in milled CRDPs when using the resins mentioned in the study [24]. However, a recent study has shown that the shear bond strength of conventionally reprimed 3D-printed resins, which are used to fabricate CRDPs, is lower than that of the resins used in CAD-CAM milling and conventional heat polymerization techniques [25].
Resin models, which are not affected by humidity as traditional plaster models, personalized brackets, which are fitted better to the tooth surface with good aesthetic properties, and clear aligners are key application areas in Orthodontics [26,27]. In Endodontics, 3D-printed templates to access obliterated root canals, surgical guides for osteotomy, and apical resection procedures are examples of successful uses of AM Technologies [28,29]. To support tissue regeneration of gum and other supporting tissues of the teeth in patients with periodontitis, additive biomanufacturing can be used to produce different types of scaffolds which can mimic a type of periodontal tissue [30].
1.4. Process algorithm of AM applied in dentistry
The main workflow of AM technology follows these steps: Data collection, data processing, material selection, and the final fabrication procedure [21].
-
1.
Data collection: Currently, there are four common methods for data collection: software design, optical scanning, mechanical scanning, and radiological scanning. The most common methods for mechanical scanning are CT and MRI.
-
2.
Data processing: The scanned data (usually DICOM format) is imported into the software to rebuild a 3D model. The volumetric data are converted into 3D triangular mesh surfaces, after the segmentation process. The reconstructed data is saved as an STL file which can be identified and processed by AM machines.
-
3.
Material selection: Various types of metals, ceramics, polymers, and hydrogels are used in dentistry. Dental implants made from titanium material manufactured using SLM are effective, personalized, and have great mechanical qualities and dimensional correctness. Current dental materials utilised in AM are largely composed of bio-ceramics, notably Zirconia (ZrO2), Alumina (Al2O3), Leucite (KAlSi2O6), Lithium disilicate (Li2Si2O5) and Tricalcium phosphate [26,27].
-
4.
Printing procedure: The printing procedure used in all fields of dentistry commonly comprises the categories described in the ISO/ASTM52900-21.
1.5. Limitations of AM technologies in dentistry
Reduction of material waste, less production time, ease of manufacturing, customized production, and variability of materials are the advantages of AM technologies [31]. However, despite these advantages, there are some limitations to employing this technology in many fields of production including dentistry. For example, in patient-specific models to be fabricated, MRI technology cannot be used to collect the data for AM procedures in patients with metallic implants. Another limitation is that some materials are not compatible and cannot be processed by AM [31]. Fabrication and replacement of these materials may not be straightforward and/or economical to develop.
Some of studies reported aesthetic problems with the mandibular AM dentures shape. Most especially obtaining adequate quality of the product surface and post-processing needs can be underlined as the important points to be improved. Depending on the geometries being replicated, the manufacturing process, and the materials being used, the accuracy of the structures produced varies. Variations of each of the existing fabricating processes are being researched and show potential for producing nanoscale structures [32]. The bonding of printed denture teeth can be considered another limitation as it’s crucial to take the bond strength into consideration. It is reported that the bond strength of printed teeth to a printed denture base is lower than the bond strength obtained through conventional processing [23].
The other challenge is the standardization problem for AM-fabricated surgical models used in real clinical procedures. International standardization of AM models in terms of size, materials, machine types, and disease types also provides better communication among the operators in different hospitals and countries [7]. Additionally, FDA-approved synthetic polymers and metals are used for AM in these surgical applications. Nevertheless, immune rejection and/or inflammation can still be revealed after the surgery, which leads patients to need a second surgery [7]. Therefore, in the current literature, some studies should be considered with caution due to high standard deviations [33].
1.6. Raw materials utilised in AM processes in dental applications
Metals, ceramics, and polymers are the most commonly utilised materials in AM. Metals and ceramics are usually preferred in applications for implants, which should be inert. On the other hand, polymers are used in applications when the material is required to be degradable to provide tissue growth. Application of composite implants comprised of a mixture of materials may be necessary, when a single material alone fails to provide function. A wide range of materials (from metals to cells) can be produced by one of the AM processes [31]. To optimize the fabrication process, each procedure has its own specific dental applications and raw materials [6].
Recent studies have reported a growing interest in the use of additive manufacturing (AM) in dentistry. For instance, AM technology can provide highly accurate and aesthetic dental prostheses, and AM can be a valuable tool for the fabrication of dental implants with improved biomechanical properties. However, despite the increasing attention paid to AM in dentistry, there is limited comprehensive reviews that summarize the current state of research in this field. To address this gap, the present study conducts a systematic scoping review of the literature on AM in dental research between 2012 and 2022, focusing on the trends, gaps, and future prospects of AM applications in dentistry. This study aims to provide insights into the current state of research on AM in dentistry, as well as to identify potential directions for future research [1,21,[33], [34], [35], [36], [37], [38], [39], [40], [41], [42]].
2. Methodology
This systematic review of the literature was led by PRISMA-ScR guidelines (preferred reporting items for systematic reviews and meta-analyses) [43] and consisted of 187 selected studies. The research question was described according to PICO (P: Population/Patient/Problem; I: Intervention; C: Comparison; O: Outcome): Publications about additive manufacturing in dental research, conducted in different fields of dentistry: What is the current status, focus and distribution of international scientific publications by selected items (i.e. years, countries, institutions, research fields, research type etc.)?
2.1. Literature search strategy
An electronic search was limited to publications in the English language and performed in Web of Science (WOS) and PubMed databases using a combination of search terms applied with the Boolean Operators “AND” and “OR”, between the dates of 2012-03-01 and 2022-03-31. The keywords used in the electronic search were ‘additive manufacturing’, ‘rapid manufacturing’, ‘rapid prototyping’, ‘rapid tooling’, ‘3D-printing’, ‘dentistry’, and ‘dental’. The string search term created from the combination of relevant keywords was (TI = (additive manufacturing or rapid manufacturing or rapid prototyping or rapid tooling or 3D-printing)) AND TI = (dentistry or dental) and searched in title and abstract sections.
2.2. Inclusion and exclusion criteria
The studies matching with the following inclusion criteria were included in this systematic review: Additive manufacturing and 3D printing studies conducted in at least one field of dentistry such as maxillofacial surgery, implantology, restorative dentistry, prosthodontics, orthodontics, endodontics, and traumatology. The aim of this study was to identify the current state of additive manufacturing in dental research. To achieve this aim, studies that were written in languages other than English, studies that had no direct clinical relevance in dentistry, book chapters, letters, and opinion articles were excluded. Conversely, related clinical and laboratory research, including both human and animal studies, case reports, review articles, and questionnaire studies that were indexed in Web of Science (WOS) and PubMed databases, were included.
2.3. Evaluation of selected studies
After the careful assessment of both title and abstract sections during the review of related publications, the evaluation of full-texts was completed and the publications which did not match the inclusion criteria were excluded from this study. Disagreements concerning the inclusion and exclusion of a study were discussed by the authors until a decision was obtained by consensus. The data extraction form consisted of the following information identified for each study: Authors, year, country, name of the journal, name of the institution, department, the field of dentistry, type of article, and topic of study. For studies conducted in more than one centre, information belonging to the first author of the article was recorded in the data extraction form.
3. Results and discussion
3.1. Study selection
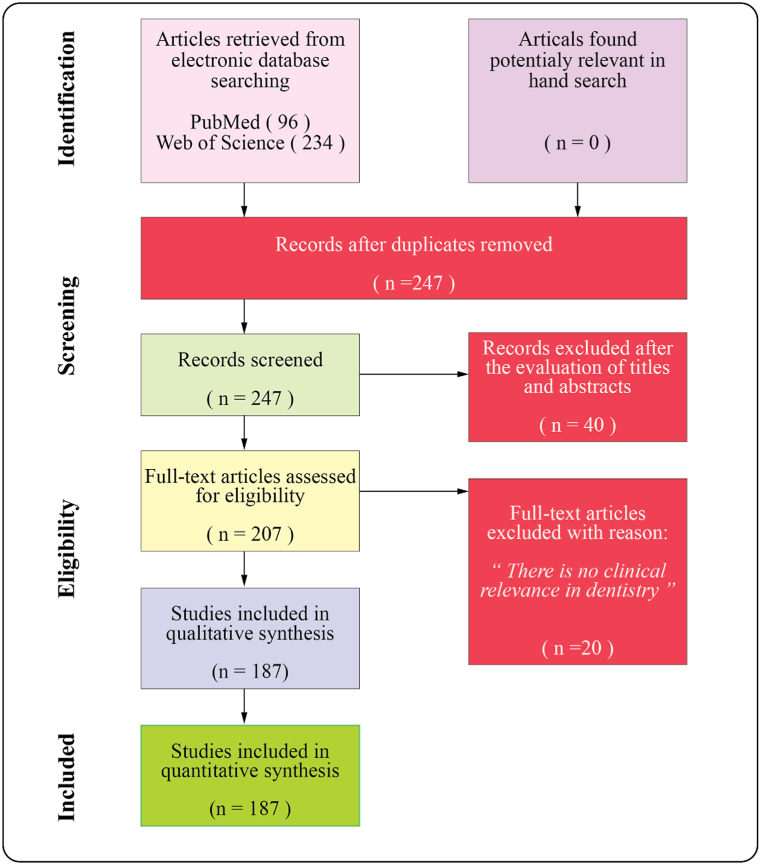
A total of 330 records were returned using the present electronic search strategy from the WoS and PubMed databases. After the removal of duplicates, 247 records remained for assessment of title and abstract. 207 eligible studies were involved in the full-text assessment and 187 studies were considered in-criteria (suitable) for this review work. The systematic flow chart of the study selection process is shown in detail in Fig. 1. The data of the included publications was listed in the supplementary document. This supplementary document provides publication records and the research content summary of the included studies in this review work [21,31,35,[44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109], [110], [111], [112], [113], [114], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124], [125], [126], [127], [128], [129], [130], [131], [132], [133], [134], [135], [136], [137], [138], [139], [140], [141], [142], [143], [144], [145], [146], [147], [148], [149], [150], [151], [152], [153], [154], [155], [156], [157], [158], [159], [160], [161], [162], [163], [164], [165], [166], [167], [168], [169], [170], [171], [172], [173], [174], [175], [176], [177], [178], [179], [180], [181], [182], [183], [184], [185], [186], [187], [188], [189], [190], [191], [192], [193], [194], [195], [196], [197], [198], [199], [200], [201], [202], [203], [204], [205], [206], [207], [208], [209], [210], [211], [212], [213], [214], [215], [216], [217], [218], [219], [220], [221], [222], [223], [224], [225], [226], [227]].
Fig. 1.
The systematic flow chart of the study selection process).
3.2. Scoping synthesis of the parameters
The quantitative results extracted from the review were represented through the graphs given in the following sections. Major publication numbers by items were priorate placed in the graphs. In the graphs, the column of “Others” indicates collection of the publications which have less than 2% of included publication number (187) in the review work.
3.2.1. Distribution of publications by year
According to the results of the examination of the distribution of the studies included in this review by publication years, it was indicated that three of these studies were published in 2013, three in 2014, five in 2015, five in 2016, 13 in 2017, 18 in 2018, 29 in 2019, 48 in 2020, 49 in 2021 and 14 in 2022 (Fig. 2a). The highest number of publications was in 2020 and 2021 with increasing percentages of 25.7% and 26.2%, respectively.
Fig. 2.
Distribution of publications (a) and the forecast (b) by years.
These results clearly indicate that there is an increasing trend up to 2021 in studies related to AM in dentistry in the previous years. This also indicates that research on AM technology in dentistry is gaining increased attention and advancements would be better adopted by the dental research field with a future perspective. It may be said that the technology and equipment is becoming both commercially viable and widely accepted in the dental industry as a consequence of the activity undertaken in the research arena.
It can also be seen in the graph that number of publications in 2020 (48) and 2021 (49) is close each other (Fig. 2a). When considering the volume of publications in previous years and their annual increase, there is an expectation that 2021 should look greater than it does. This may be as a consequence of a limitation on research outputs published due to the Covid-19 pandemic. Like in many research fields, research studies on AM in dentistry were possibly negatively affected during the pandemic. However, this would be better interpreted at the end of the year 2022 and so on.
Additionally, the number of publications in 2022 given in this review is less than the previous year of 2021, as this only covers the first three months of publications which are available in indexing databases. On the other hand, nominal expectation was calculated through a linear expectation forecast (exponential smoothing forecast) for the forthcoming years including 2025 which indicates that there will be an increase in the number of publications (approximately 53% in 2025) in AM related studies in dentistry (Fig. 2b).
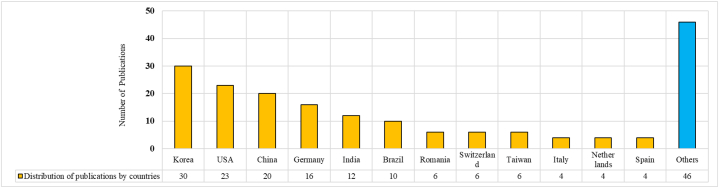
3.2.2. Distribution of publications by countries
The publications included in this study originated from 39 different countries. The graph was created for countries with at least four publications (greater than 2%) (Fig. 3). According to the results of the examination of the distribution of the studies included in this review by Countries: 30 publications were from Korea, 23 from the USA, 20 from China, 16 from Germany, 12 from India, 10 from Brazil, six from Romania, six from Switzerland, six from Taiwan, four from Italy, four from The Netherlands, and four from Spain. The greatest number of publications originated from Korea and USA (16% and 12.3%, respectively) (please see supplementary document for more details).
Fig. 3.
Distribution of publications by countries.
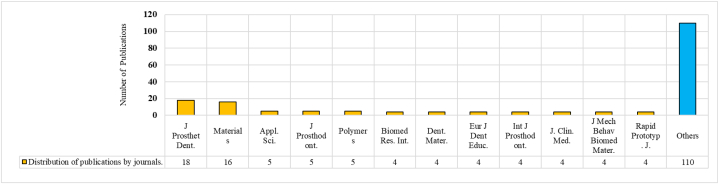
3.2.3. Distribution of publications by journals
The publications included in this study were published in 89 different journals reviewed on WoS and Pubmed databases. The graph created for journals with at least four publications (greater than 2%) is shown in Fig. 4. According to the results of the examination of the distribution of the studies included in this review by Journals: there were 18 studies published in J Prosthet Dent., 16 studies published in Materials, five studies each published in Polymers, Appl. Sci. and J Prosthodont., four studies each published in J. Mech. Behav. Biomed Mater., Biomed Res. Int, Dent. Mater., Eur J Dent Educ., Int J Prosthodont., J. Clin. Med., and Rapid Prototyp. J. The greatest number of publications was published in J Prosthet Dent. and Materials (9.6% and 8.6%, respectively) (please see supplementary document for more details). In short, the journals included in this review can be grouped under engineering, material science and dental research fields.
Fig. 4.
Distribution of publications by journals.
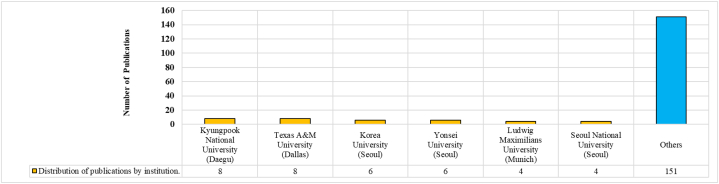
3.2.4. Distribution of publications by institutions
The research that led to the publications included in this study were conducted at 137 different institutions, three of them were private clinics, two of them were research centres and the others were universities or university hospitals. The graph was plotted for institutions with at least four publications (greater than 2%) as shown in Fig. 5. According to the results of the examination of the distribution of the studies included in this review by institutions: Ludwig Maximilians University (Munich-Germany), and Seoul National University (Seoul-Korea) have four publications; Korea University (Seoul-Korea) and Yonsei University (Seoul-Korea) have six publications; Kyungpook National University (Daegu-Korea), and Texas A&M University (Dallas-USA) have eight publications. The highest number of publications originated in Kyungpook National University (Daegu-Korea), and Texas A&M University (Dallas-USA) with percentage of 4.3% (8 publications for each).
Fig. 5.
Distribution of publications by institution.
3.2.5. Distribution of publications by field of dentistry
The studies were categorised into 10 different groups and the distribution of the number of studies according to the fields of dentistry is as follows: one for paediatric dentistry, two for traumatology, three for endodontics and periodontology, 10 for orthodontics, 11 for restorative dentistry, 14 for maxillofacial surgery, 27 for general dentistry, 30 for implantology and 86 for prosthodontics (Fig. 6). The review studies evaluating the dental applications of additive manufacturing were accepted as general dentistry; studies including implant treatments were accepted as implantology, and the remaining surgical treatments were accepted as maxillofacial surgery. The highest number of publications were from prosthodontics and implantology with percentages of 46% and 16%, respectively.
Fig. 6.
Distribution of publications by field of dentistry.
3.2.6. Distribution of publications by type of publications
The studies were categorised into six different groups and the distribution of the number of studies according to the type of publication is as follows: three of them were Animal Study, four were Technical Notes, five were Questionnaires, 10 were Case Report/Series, 42 were Reviews and 127 were Original Research (Fig. 7), equating to 65.8% overall. These statistics revealed that research studies on AM in dentistry is the major focus, however, Reviews are a considerable number. This may indicate that the researchers wish to follow the advancements in AM technology and its trends as they see its future potential in dental applications.
Fig. 7.
Distribution of publications by type of publication.
3.2.7. Future Outlook
Although AM technologies have been widely utilised in many areas, studies are still conducted to shorten the time required for the production process and to provide improved software in order to obtain more accurate outcomes. For this purpose, research continues to develop new materials that can be processed in a shorter time and do not require further processing with AM technologies [6]. Obtaining an improved final product’s surface quality is another important perspective. 3D printed scaffolds to guide the growth of the tissue made from biological materials that are used in tissue engineering for bone grafting, regeneration, or repair of soft and hard tissues are another focal area of AM technologies [31]. It is thought that this field of application will expand further in the future [6]. On the other hand, some of the previous reviews highlighted the limited number of in-vivo studies on the subject of AM technologies, indicating the need for additional studies with sufficient follow-up time [228,229].
The final findings of this review made it apparent that the expectation for the future was that research in dentistry would focus on AM technology development in particular, in order to accelerate the increase in the number of novel dental materials, tools, implants, and next generation modelling strategies.
The detailed methodology employed in this scoping review, including the well-defined inclusion and exclusion criteria, the wide range of time limitation, and the current relevance, are some of its strengths. Moreover, the adherence to the PRISMA guidelines adds to the methodological reliability of this review [230]. However, this scoping review also had some limitations. It is worth noting that the use of AM technology is still not widespread, as it is mostly limited to research centres and universities due to the high cost of the required hardware. Additionally, only articles with clinical relevance were included in this review, which implies that studies conducted in the field of tissue engineering and stem cells, which have not yet entered clinical routine use, were excluded.
4. Conclusion
The systematic scoping review conducted in this paper revealed the current status and the future expectation of scientific publications indexed in the selected databases (WoS and PubMed). The approach of this study is to provide insight to research trends related to the use of AM technology in dentistry and build a foundation for future research, from which new research opportunities could be envisaged. The review results indicated an increasing trend in research in this field over the years. Within the scoped publication number of 187 considered in this study, the most publications were produced in 2020 and 2021, with annual percentage increases of 25.7% and 26.2%, respectively. 49 publications were realised in 2021 and expectation for coming up years is higher. Korea has the highest number of publications related to AM employed in dental research. Prosthodontics and implantology are the sub-fields in dentistry which has the highest number of publications in its category.
With the aid of CAD/CAM technology and 3D imaging, additive manufacturing is at the forefront of, and has a significant impact on, all areas including dentistry. However, there are some difficulties, such as prohibitively expensive materials, lengthy post-processing, and a laborious manual process to fulfil. Although contemporary additive manufacturing machines can produce models in a short amount of time, obtaining digital data and its processing can take more time; as a result, additive manufacturing does not look like it is currently the most appropriate for deployment in emergency situations.
Beside the limitations of this technology, the review of the publications included in this study highlighted in short that future development of digital dentistry would be accelerated through the utilisation of AM technology. AM appears to offer the ability to address a number of issues in dentistry, including customization requirements, denture alignment and retention, and the need to enhance current dental implants. Finally, it can be said that, although the high investment costs and technical limitations of this technology for dental applications create difficulties its adoption in this field, additive manufacturing and technological applications will be increasingly specialised and advanced through future research and development in order to overcome the utilisation limitations of AM applications in dentistry.
Based on this review work, three important future research recommendations can be summarised;
-
1.
Research on new materials: Future research could focus on developing cost-effective, durable, and biocompatible materials for AM technology in dentistry. This includes the exploration of hybrid, nanomaterials, and composite materials with improved properties.
-
2.
Efficient post-processing: Future research could develop new post-processing techniques to improve efficiency and reduce labour and time costs. This includes automated systems and new post-processing materials.
-
3.
New applications: Future research could explore new applications of AM technology in dentistry such as endodontics, orthodontics, and oral surgery. This includes the development of new printing techniques, customization of implants, and the use of AM in emergency situations.
Author contribution statement
H. Kursat CELIK: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Simay KOC: Performed the experiments; Analysed and interpreted the data; Wrote the paper.
Alper KUSTARCI; Allan E.W. RENNIE: Conceived and designed the experiments; Analysed and interpreted the data.
Nuri CAGLAYAN: Analysed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Acknowledgement
This research was partly supported financially by The Scientific Research Projects Coordination Unit of Akdeniz University (Antalya-Turkey). The authors declare that there is no conflict of interest to disclose and they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e17462.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Rouf S., et al. Additive manufacturing technologies: industrial and medical applications, Sustain. Oper. Comput. 2022;3:258–274. [Google Scholar]
- 2.Jemghili R., Ait Taleb A., Khalifa M. Emerald Group Holdings Ltd; 2021. A Bibliometric Indicators Analysis of Additive Manufacturing Research Trends from 2010 to 2020; pp. 1432–1454. [DOI] [Google Scholar]
- 3.Wohlers-Report . 2022. Wohlers Report 2022.https://wohlersassociates.com/resource/wohlers-report-2022-finds-strong-industry-wide-growth/ Available from. [Google Scholar]
- 4.ISO/ASTM-52900:2021(E) 2022. ISO/ASTM52900-21 (Additive Manufacturing - General Principles - Fundamentals and Vocabulary) (ISO/ASTM 52900:2021(E), I.A. 52900). (USA) [Google Scholar]
- 5.Liaw C.-Y., Guvendiren M. Current and emerging applications of 3D printing in medicine. Biofabrication. 2017;9(2) doi: 10.1088/1758-5090/aa7279. [DOI] [PubMed] [Google Scholar]
- 6.Alammar A., et al. Additive manufacturing technologies: current status and future perspectives. J. Prosthodont. 2022;31(S1):4–12. doi: 10.1111/jopr.13477. [DOI] [PubMed] [Google Scholar]
- 7.Lai J., Wang C., Wang M. 3D printing in biomedical engineering: processes, materials, and applications. Appl. Phys. Rev. 2021;8(2) [Google Scholar]
- 8.Hull C.W. 1986. Apparatus for Production of Three-Dimensional Objects by Stereolithography. (Google Patents) [Google Scholar]
- 9.Deckard C.R. 1989. Method and Apparatus for Producing Parts by Selective Sintering. Google Patents. [Google Scholar]
- 10.Sachs E.M., et al. 1993. Three-dimensional Printing Techniques. (Google Patents) [Google Scholar]
- 11.Crump S.S. 1992. Apparatus and Method for Creating Three-Dimensional Objects. (Google Patents) [Google Scholar]
- 12.Feygin M., et al. 1998. Laminated Object Manufacturing System. US Patent, (5730817) [Google Scholar]
- 13.Tibbits S. 2013. The Emergence of “4D Printing”. (TED Conference). [Google Scholar]
- 14.Choi J., et al. 4D printing technology: a review. 3D Print. Addit. Manuf. 2015;2(4):159–167. [Google Scholar]
- 15.Jacobsen M. 2016. Clearing the way for pivotal 21st-century innovation; pp. 163–179. (Giftedness and Talent in the 21st Century). [DOI] [Google Scholar]
- 16.Khoo Z.X., et al. 3D printing of smart materials: a review on recent progresses in 4D printing. Virtual Phys. Prototyp. 2015;10(3):103–122. [Google Scholar]
- 17.Pei E. Assembly Automation; 2014. 4D Printing: Dawn of an Emerging Technology Cycle. [Google Scholar]
- 18.Ge Q., Qi H.J., Dunn M.L. Active materials by four-dimension printing. Appl. Phys. Lett. 2013;103(13):131901. [Google Scholar]
- 19.Tibbits S., et al. 2014. 4D printing and universal transformation; pp. 539–548. (ACADIA 2014 - Design Agency: Proceedings of the 34th Annual Conference of the Association for Computer Aided Design in Architecture). [DOI] [Google Scholar]
- 20.Tibbits S. 4D printing: multi‐material shape change. Architect. Des. 2014;84(1):116–121. [Google Scholar]
- 21.Huang G., et al. Main applications and recent research progresses of additive manufacturing in dentistry. BioMed Res. Int. 2021:2022. doi: 10.1155/2022/5530188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ellakany P., et al. Influence of CAD/CAM milling and 3D-printing fabrication methods on the mechanical properties of 3-unit interim fixed dental prosthesis after thermo-mechanical aging process. Polymers (Basel) 2022;14(19) doi: 10.3390/polym14194103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goodacre B.J., Goodacre C.J. Additive manufacturing for complete denture fabrication: a narrative review. J. Prosthodont. 2022;31(S1):47–51. doi: 10.1111/jopr.13426. [DOI] [PubMed] [Google Scholar]
- 24.Srinivasan M., et al. Analysis of the residual monomer content in milled and 3D-printed removable CAD-CAM complete dentures: an in vitro study. J. Dent. 2022;120 doi: 10.1016/j.jdent.2022.104094. [DOI] [PubMed] [Google Scholar]
- 25.Mert D., et al. CAD-CAM complete denture resins: effect of relining on the shear bond strength. J. Dent. 2023;131 doi: 10.1016/j.jdent.2023.104438. [DOI] [PubMed] [Google Scholar]
- 26.Kim S.-Y., et al. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am. J. Orthod. Dentofacial Orthop. 2018;153(1):144–153. doi: 10.1016/j.ajodo.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 27.Yang L., et al. A novel customized ceramic bracket for esthetic orthodontics: in vitro study. Prog. Orthod. 2019;20(1):1–10. doi: 10.1186/s40510-019-0292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tavares W.L.F., et al. Guided endodontic access of calcified anterior teeth. J. Endod. 2018;44(7):1195–1199. doi: 10.1016/j.joen.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 29.Hawkins T., et al. Targeted endodontic microsurgery and endodontic microsurgery: a surgical simulation comparison. Int. Endod. J. 2020;53(5):715–722. doi: 10.1111/iej.13243. [DOI] [PubMed] [Google Scholar]
- 30.Carter S.-S.D., et al. Additive biomanufacturing: an advanced approach for periodontal tissue regeneration. Ann. Biomed. Eng. 2017;45(1):12–22. doi: 10.1007/s10439-016-1687-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhargav A., et al. Applications of additive manufacturing in dentistry: a review. J. Biomed. Mater. Res. B Appl. Biomater. 2018;106(5):2058–2064. doi: 10.1002/jbm.b.33961. [DOI] [PubMed] [Google Scholar]
- 32.Barazanchi A., et al. Additive technology: update on current materials and applications in dentistry. J. Prosthodont. 2017;26(2):156–163. doi: 10.1111/jopr.12510. [DOI] [PubMed] [Google Scholar]
- 33.Methani M.M., et al. Additive manufacturing in dentistry: current technologies, clinical applications, and limitations. Curr. Oral Health Rep. 2020;7(4):327–334. [Google Scholar]
- 34.Richter M., et al. Additive manufacturing technologies: current status and future perspectives. Materials. 2021;13(1):4–12. doi: 10.1007/s40496-020-00288-w. [DOI] [PubMed] [Google Scholar]
- 35.Revilla‐León M., Özcan M. Additive manufacturing technologies used for processing polymers: current status and potential application in prosthetic dentistry. J. Prosthodont. 2019;28(2):146–158. doi: 10.1111/jopr.12801. [DOI] [PubMed] [Google Scholar]
- 36.Javaid M., Haleem A. Current status and applications of additive manufacturing in dentistry: a literature-based review. J. Oral Biol. Craniofacial Res. 2019;9(3):179–185. doi: 10.1016/J.JOBCR.2019.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jawahar A., Maragathavalli G. Applications of 3D printing in dentistry – a review. J. Pharmaceut. Sci. Res. 2019;11(5):1670–1675. [Google Scholar]
- 38.Alharbi N., Wismeijer D., Osman R.B. Additive manufacturing techniques in prosthodontics: where do we currently stand? A critical review. Int. J. Prosthodont. (IJP) 2017;30(5):474–484. doi: 10.11607/ijp.5079. [DOI] [PubMed] [Google Scholar]
- 39.Khanlar L.N., et al. Additive manufacturing of zirconia ceramic and its application in clinical dentistry: a review. Dent. J. 2021;9(9):104. doi: 10.3390/dj9090104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jockusch J., Özcan M. Additive manufacturing of dental polymers: an overview on processes, materials and applications. Dent. Mater. J. 2020:2019–2123. doi: 10.4012/dmj.2019-123. [DOI] [PubMed] [Google Scholar]
- 41.Alammar A., et al. Additive manufacturing technologies: current status and future perspectives. J. Prosthodont. 2022;31:4–12. doi: 10.1111/JOPR.13477. [DOI] [PubMed] [Google Scholar]
- 42.Revilla-León M., Özcan M. Additive manufacturing technologies used for 3D metal printing in dentistry. Curr. Oral Health Rep. 2017;4(3):201–208. doi: 10.1007/s40496-017-0152-0. [DOI] [Google Scholar]
- 43.Page M.J., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst. Rev. 2021;10(1):1–11. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aati S., et al. Development of 3D printed resin reinforced with modified ZrO2 nanoparticles for long-term provisional dental restorations. Dent. Mater. 2021;37(6):e360–e374. doi: 10.1016/j.dental.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 45.Alharbi N., Osman R., Wismeijer D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016;115(6):760–767. doi: 10.11607/ijp.4835. [DOI] [PubMed] [Google Scholar]
- 46.Alharbi N., Osman R.B., Wismeijer D. Factors influencing the dimensional accuracy of 3D-printed full-coverage dental restorations using stereolithography technology. Int. J. Prosthod. 2016;29(5):503–510. doi: 10.11607/ijp.4835. [DOI] [PubMed] [Google Scholar]
- 47.Alifui-Segbaya F., et al. Characterization of the double bond conversion of acrylic resins for 3D printing of dental prostheses. Compendium. 2019;40(10) [PubMed] [Google Scholar]
- 48.Anadioti E., et al. 3D printed complete removable dental prostheses: a narrative review. BMC Oral Health. 2020;20(1):1–9. doi: 10.1186/s12903-020-01328-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Atria P.J., et al. 3D‐printed resins for provisional dental restorations: comparison of mechanical and biological properties. J. Esthetic Restor. Dent.34. 2022;5:804–815. doi: 10.1111/jerd.12888. [DOI] [PubMed] [Google Scholar]
- 50.Atzeni E., Salmi A. Evaluation of additive manufacturing (AM) techniques for the production of metal–ceramic dental restorations. J. Manuf. Process. 2015;20:40–45. [Google Scholar]
- 51.Bae E.-J., et al. A comparative study of additive and subtractive manufacturing for dental restorations. J. Prosthet. Dent. 2017;118(2):187–193. doi: 10.1016/j.prosdent.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 52.Bae S., et al. Reliability of metal 3D printing with respect to the marginal fit of fixed dental prostheses: a systematic review and meta-analysis. Materials. 2020;13(21):4781. doi: 10.3390/ma13214781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Balamurugan P., Selvakumar N. Development of patient specific dental implant using 3D printing. J. Ambient Intell. Hum. Comput. 2021;12(3):3549–3558. [Google Scholar]
- 54.Barbin T., et al. 3D metal printing in dentistry: an in vitro biomechanical comparative study of two additive manufacturing technologies for full-arch implant-supported prostheses. J. Mech. Behav. Biomed. Mater. 2020;108 doi: 10.1016/j.jmbbm.2020.103821. [DOI] [PubMed] [Google Scholar]
- 55.Barone S., et al. Interactive design of dental implant placements through CAD-CAM technologies: from 3D imaging to additive manufacturing. Int. J. Interact. Des. Manuf. (IJIDeM) 2016;10(2):105–117. [Google Scholar]
- 56.Baumgartner S., et al. Stereolithography-based additive manufacturing of lithium disilicate glass ceramic for dental applications. Mater. Sci. Eng. C. 2020;116 doi: 10.1016/j.msec.2020.111180. [DOI] [PubMed] [Google Scholar]
- 57.Bose S., et al. Calcium phosphate coated 3D printed porous titanium with nanoscale surface modification for orthopedic and dental applications. Mater. Des. 2018;151:102–112. doi: 10.1016/j.matdes.2018.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Branco A., et al. Suitability of 3D printed pieces of nanocrystalline zirconia for dental applications. Dent. Mater. 2020;36(3):442–455. doi: 10.1016/j.dental.2020.01.006. [DOI] [PubMed] [Google Scholar]
- 59.Brouwer de Koning S., et al. Utilization of a 3D printed dental splint for registration during electromagnetically navigated mandibular surgery. Int. J. Comput. Assist. Radiol. Surg. 2020;15(12):1997–2003. doi: 10.1007/s11548-020-02271-3. [DOI] [PubMed] [Google Scholar]
- 60.Cahuana-Bartra P., et al. The use of 3D additive manufacturing technology in autogenous dental transplantation. 3D Print. Med. 2020;6(1):1–10. doi: 10.1186/s41205-020-00070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Çakmak G., et al. Effect of printing layer thickness on the trueness and margin quality of 3D-printed interim dental crowns. Appl. Sci. 2021;11(19):9246. [Google Scholar]
- 62.Canciglieri M.B., et al. An approach for dental prosthesis design and manufacturing through rapid manufacturing technologies. Int. J. Comput. Integrated Manuf. 2019;32(9):832–847. [Google Scholar]
- 63.Chakraborty A., et al. Finite element and experimental analysis to select patient’s bone condition specific porous dental implant, fabricated using additive manufacturing. Comput. Biol. Med. 2020;124 doi: 10.1016/j.compbiomed.2020.103839. [DOI] [PubMed] [Google Scholar]
- 64.Chan K.S., et al. Fatigue life of titanium alloys fabricated by additive layer manufacturing techniques for dental implants. Metall. Mater. Trans. 2013;44(2):1010–1022. [Google Scholar]
- 65.Chaudhari P.K., et al. 3D printing for fostering better dental education. Evid. Base Dent. 2021;22(4):154–155. doi: 10.1038/s41432-021-0217-8. [DOI] [PubMed] [Google Scholar]
- 66.Chen R.-S., et al. Challenge tooth regeneration in adult dogs with dental pulp stem cells on 3D-printed hydroxyapatite/polylactic acid scaffolds. Cells. 2021;10(12):3277. doi: 10.3390/cells10123277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen S.-G., et al. TiO2 and PEEK reinforced 3D printing PMMA composite resin for dental denture base applications. Nanomaterials. 2019;9(7):1049. doi: 10.3390/nano9071049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cho J.-H., et al. Creating protective appliances for preventing dental injury during endotracheal intubation using intraoral scanning and 3D printing: a technical note. J. Dent. Anesthes. Pain Med. 2017;17(1):55–59. doi: 10.17245/jdapm.2017.17.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cunico M.W.M. Investigation of ceramic dental prostheses based on ZrSiO4-glass composites fabricated by indirect additive manufacturing. Int. J. Bioprint. 2021;7(1) doi: 10.18063/ijb.v7i1.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Czajkowska M., et al. Comparison of dental stone models and their 3D printed acrylic replicas for the accuracy and mechanical properties. Materials. 2020;13(18):4066. doi: 10.3390/ma13184066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.David O.T., et al. Polylactic acid 3D printed drill guide for dental implants using CBCT. Rev. Chim.-Bucharest. 2017;68:341–342. [Google Scholar]
- 72.Dawood A., et al. 3D printing in dentistry. Br. Dent. J. 2015;219(11):521–529. doi: 10.1038/sj.bdj.2015.914. [DOI] [PubMed] [Google Scholar]
- 73.Dehurtevent M., et al. Stereolithography: a new method for processing dental ceramics by additive computer-aided manufacturing. Dent. Mater. 2017;33(5):477–485. doi: 10.1016/j.dental.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 74.Demiralp E., DoĞRu G., Yilmaz H. Additive manufacturing (3D PRINTING) methods and applications in dentistry. Clin. Exp. Health Sci. 2021;11(1):182–190. [Google Scholar]
- 75.Derban P., et al. Influence of the printing angle and load direction on flexure strength in 3D printed materials for provisional dental restorations. Materials. 2021;14(12):3376. doi: 10.3390/ma14123376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dhokar A.A., et al. Knowledge and practices of 3d printing in dental practitioners of Maharashtra: a cross-sectional study. J. Indian Acad. Oral Med. Radiol. 2020;32(2):127. [Google Scholar]
- 77.Dikova T.D., et al. Adhesion strength of ceramic coatings to dental Ni–Cr alloy fabricated by casting with 3D printed patterns. Russ. Metall. (Metally) 2019;2019(4):385–391. [Google Scholar]
- 78.Dobroś K., Hajto‐Bryk J., Zarzecka J. Application of 3D‐printed teeth models in teaching dentistry students: a scoping review. Eur. J. Dent. Educ. 2022;27(1):126–134. doi: 10.1111/eje.12784. [DOI] [PubMed] [Google Scholar]
- 79.Dong T., et al. Accuracy of different tooth surfaces on 3D printed dental models: orthodontic perspective. BMC Oral Health. 2020;20(1):1–8. doi: 10.1186/s12903-020-01338-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dos Santos L.C.P., Malheiros F.C., Guarato A.Z. Surface parameters of as-built additive manufactured metal for intraosseous dental implants. J. Prosthet. Dent. 2020;124(2):217–222. doi: 10.1016/j.prosdent.2019.09.010. [DOI] [PubMed] [Google Scholar]
- 81.Dostálová T., et al. Intraoral scanner and stereographic 3D print in dentistry—quality and accuracy of model—new laser application in clinical practice. Laser Phys. 2018;28(12) [Google Scholar]
- 82.Du L., et al. E-quality control in dental metal additive manufacturing inspection using 3D scanning and 3D measurement. Front. Bioeng. Biotechnol. 2020:1038. doi: 10.3389/fbioe.2020.01038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Edelmann A., Riedel L., Hellmann R. Realization of a dental framework by 3D printing in material cobalt-chromium with superior precision and fitting accuracy. Materials. 2020;13(23):5390. doi: 10.3390/ma13235390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.El Chaar E., et al. Treatment of atrophic ridges with titanium mesh: a retrospective study using 100% mineralized allograft and comparing dental stone versus 3D-printed models. Int. J. Periodontics Restor. Dent. 2019;39(4) doi: 10.11607/prd.3733. [DOI] [PubMed] [Google Scholar]
- 85.Etajuri E.A., et al. Deviation of dental implants placed using a novel 3D-printed surgical guide: an in vitro study. Dent. Med. Probl. 2020;57(4):359–362. doi: 10.17219/dmp/123976. [DOI] [PubMed] [Google Scholar]
- 86.Fernandez P.K., et al. Rapid additive manufacturing of an obturator prosthesis with the use of an intraoral scanner: a dental technique. J. Prosthet. Dent. 2022;127(1):189–193. doi: 10.1016/j.prosdent.2020.07.033. [DOI] [PubMed] [Google Scholar]
- 87.Galante R., Figueiredo-Pina C.G., Serro A.P. Additive manufacturing of ceramics for dental applications: a review. Dent. Mater. 2019;35(6):825–846. doi: 10.1016/j.dental.2019.02.026. [DOI] [PubMed] [Google Scholar]
- 88.Ganbold B., et al. Human stem cell responses and surface characteristics of 3D printing Co-Cr dental material. Materials. 2019;12(20):3419. doi: 10.3390/ma12203419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gonzalez A.M., et al. Fiber‐reinforced composite fixed dental prosthesis using an additive manufactured silicone index. J. Esthetic Restor. Dent. 2020;32(7):626–633. doi: 10.1111/jerd.12628. [DOI] [PubMed] [Google Scholar]
- 90.Goodacre B.J., et al. A 3D-printed guide for lateral approach sinus grafting: a dental technique. J. Prosthet. Dent. 2018;119(6):897–901. doi: 10.1016/j.prosdent.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 91.Haleem A., Javaid M. Polyether ether ketone (PEEK) and its manufacturing of customised 3D printed dentistry parts using additive manufacturing. Clin. Epidemiol. Global Health. 2019;7(4):654–660. [Google Scholar]
- 92.Han X., et al. An in vitro study of osteoblast response on fused-filament fabrication 3D printed PEEK for dental and cranio-maxillofacial implants. J. Clin. Med. 2019;8(6):771. doi: 10.3390/jcm8060771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Han X., et al. Carbon fiber reinforced PEEK composites based on 3D-printing technology for orthopedic and dental applications. J. Clin. Med. 2019;8(2):240. doi: 10.3390/jcm8020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hanisch M., et al. 3D-printed surgical training model based on real patient situations for dental education. Int. J. Environ. Res. Publ. Health. 2020;17(8):2901. doi: 10.3390/ijerph17082901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hata K., et al. Development of dental poly (methyl methacrylate)-based resin for stereolithography additive manufacturing. Polymers. 2021;13(24):4435. doi: 10.3390/polym13244435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hazeveld A., Slater J.J.H., Ren Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofacial Orthop. 2014;145(1):108–115. doi: 10.1016/j.ajodo.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 97.Hegedus T., et al. User experience and sustainability of 3D printing in dentistry. Int. J. Environ. Res. Publ. Health. 2022;19(4):1921. doi: 10.3390/ijerph19041921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Henderson J.Y., et al. Failure load of milled, 3D-printed, and conventional chairside-dispensed interim 3-unit fixed dental prostheses. J. Prosthet. Dent. 2022;127(2):275.e1–275.e7. doi: 10.1016/j.prosdent.2021.11.005. [DOI] [PubMed] [Google Scholar]
- 99.Hesse H., Özcan M. A review on current additive manufacturing technologies and materials used for fabrication of metal-ceramic fixed dental prosthesis. J. Adhes. Sci. Technol. 2021;35(23):2529–2546. [Google Scholar]
- 100.Hodásová Ľ., et al. 3D-Printed polymer-infiltrated ceramic network with biocompatible adhesive to potentiate dental implant applications. Materials. 2021;14(19):5513. doi: 10.3390/ma14195513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Höhne C., Schmitter M. 3D printed teeth for the preclinical education of dental students. J. Dent. Educ. 2019;83(9):1100–1106. doi: 10.21815/JDE.019.103. [DOI] [PubMed] [Google Scholar]
- 102.Höhne C., Schwarzbauer R., Schmitter M. 3D printed teeth with enamel and dentin layer for educating dental students in crown preparation. J. Dent. Educ. 2019;83(12):1457–1463. doi: 10.21815/JDE.019.146. [DOI] [PubMed] [Google Scholar]
- 103.Hong M.-H., Min B.K., Kwon T.-Y. Fabricating high-quality 3D-printed alloys for dental applications. Appl. Sci. 2017;7(7):710. [Google Scholar]
- 104.Hwangbo N.-K., et al. Effects of the washing time and washing solution on the biocompatibility and mechanical properties of 3D printed dental resin materials. Polymers. 2021;13(24):4410. doi: 10.3390/polym13244410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jang Y., et al. Accuracy of 3-unit fixed dental prostheses fabricated on 3D-printed casts. J. Prosthet. Dent. 2020;123(1):135–142. doi: 10.1016/j.prosdent.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 106.Javaid M., Haleem A., Kumar L. Current status and applications of 3D scanning in dentistry. Clin. Epidemiol. Global Health. 2019;7(2):228–233. [Google Scholar]
- 107.Jeong Y.-G., Lee W.-S., Lee K.-B. Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method. J. Adv. Prosthodont. 2018;10(3):245–251. doi: 10.4047/jap.2018.10.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jin S.J., et al. Accuracy of dental replica models using photopolymer materials in additive manufacturing: in vitro three‐dimensional evaluation. J. Prosthodont. 2019;28(2):e557–e562. doi: 10.1111/jopr.12928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jin S.-J., et al. Accuracy (trueness and precision) of dental models fabricated using additive manufacturing methods. Int. J. Comput. Dent. 2018;21(2):107–113. [PubMed] [Google Scholar]
- 110.Jindal P., et al. Effects of post-curing conditions on mechanical properties of 3D printed clear dental aligners. Rapid Prototyp. J. 2020;26(8):1337–1344. [Google Scholar]
- 111.Jindal P., et al. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofacial Orthop. 2019;156(5):694–701. doi: 10.1016/j.ajodo.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 112.Jindal P., et al. Mechanical behaviour of 3D printed vs thermoformed clear dental aligner materials under non-linear compressive loading using FEM. J. Mech. Behav. Biomed. Mater. 2020;112 doi: 10.1016/j.jmbbm.2020.104045. [DOI] [PubMed] [Google Scholar]
- 113.Jockusch J., Özcan M. Additive manufacturing of dental polymers: an overview on processes, materials and applications. Dent. Mater. J. 2020:2019–2123. doi: 10.4012/dmj.2019-123. [DOI] [PubMed] [Google Scholar]
- 114.Joda T., Matthisson L., Zitzmann N.U. Impact of aging on the accuracy of 3D-printed dental models: an in vitro investigation. J. Clin. Med. 2020;9(5):1436. doi: 10.3390/jcm9051436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kalman L. 3D printing of a novel dental implant abutment. J. Dent. Res. Dent. Clin. Dent. Prospects. 2018;12(4):299. doi: 10.15171/joddd.2018.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kamali A.H., et al. A discrete event simulation method for performance analysis of an additive manufacturing in the dental clinic. Int. J. Adv. Des. Manuf. Technol. 2022;118(9):2949–2979. doi: 10.1007/s00170-021-08135-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kamio T., et al. Utilizing a low-cost desktop 3D printer to develop a “one-stop 3D printing lab” for oral and maxillofacial surgery and dentistry fields. 3D Print. Med. 2018;4(1):1–7. doi: 10.1186/s41205-018-0028-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kessler A., Hickel R., Reymus M. 3D printing in dentistry—state of the art. Operat. Dent. 2020;45(1):30–40. doi: 10.2341/18-229-L. [DOI] [PubMed] [Google Scholar]
- 119.Khanlar L.N., et al. Additive manufacturing of zirconia ceramic and its application in clinical dentistry: a review. Dent. J. 2021;9(9):104. doi: 10.3390/dj9090104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kim J.-H., et al. Accuracy and precision of polyurethane dental arch models fabricated using a three-dimensional subtractive rapid prototyping method with an intraoral scanning technique. Kor. J. Orthodont. 2014;44(2):69–76. doi: 10.4041/kjod.2014.44.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kim J.-H., et al. Mechanophysical and biological properties of a 3D-printed titanium alloy for dental applications. Dent. Mater. 2020;36(7):945–958. doi: 10.1016/j.dental.2020.04.027. [DOI] [PubMed] [Google Scholar]
- 122.Konieczny B., et al. Challenges of Co–Cr alloy additive manufacturing methods in dentistry—the current state of knowledge (systematic review) Materials. 2020;13(16):3524. doi: 10.3390/ma13163524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kunrath M.F., et al. Influence of saliva interaction on surface properties manufactured for rapid osseointegration in dental implants. Biofouling. 2021;37(7):757–766. doi: 10.1080/08927014.2021.1964487. [DOI] [PubMed] [Google Scholar]
- 124.Kwon J.-S., et al. Durable oral biofilm resistance of 3d-printed dental base polymers containing zwitterionic materials. Int. J. Mol. Sci. 2021;22(1):417. doi: 10.3390/ijms22010417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lee D., et al. A hybrid dental model concept utilizing fused deposition modeling and digital light processing 3D printing. Int. J. Prosthodont. (IJP) 2020;33:229–231. doi: 10.11607/ijp.6534. [DOI] [PubMed] [Google Scholar]
- 126.Lee D.-H., et al. The effect of 4, 4'-bis (N, N-diethylamino) benzophenone on the degree of conversion in liquid photopolymer for dental 3D printing. J. Adv. Prosthodont. 2015;7(5):386–391. doi: 10.4047/jap.2015.7.5.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lee H.-C., et al. Numerical method for the design of healing chamber in additive-manufactured dental implants. BioMed Res. Int. 2017;2017 doi: 10.1155/2017/1970680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lee J., et al. Assessment of the inner surface roughness of 3D printed dental crowns via optical coherence tomography using a roughness quantification algorithm. IEEE Access. 2020;8:133854–133864. [Google Scholar]
- 129.Li C.-H., Wu C.-H., Lin C.-L. Design of a patient-specific mandible reconstruction implant with dental prosthesis for metal 3D printing using integrated weighted topology optimization and finite element analysis. J. Mech. Behav. Biomed. Mater. 2020;105 doi: 10.1016/j.jmbbm.2020.103700. [DOI] [PubMed] [Google Scholar]
- 130.Li H., et al. Dental ceramic prostheses by stereolithography-based additive manufacturing: potentials and challenges. Adv. Appl. Ceram. 2019;118(1–2):30–36. [Google Scholar]
- 131.Li L., et al. Comparison of 3D-printed dental implants with threaded implants for osseointegration: an experimental pilot study. Materials. 2020;13(21):4815. doi: 10.3390/ma13214815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Li X., et al. Additive manufacturing of dental root-analogue implant with desired properties. Mater. Technol. 2021;36(14):894–906. [Google Scholar]
- 133.Lian Q., et al. Additive manufacturing of ZrO2 ceramic dental bridges by stereolithography, Rapid Prototyp. J. 2018;24(1):114–119. [Google Scholar]
- 134.Lin L., et al. 3D printing and digital processing techniques in dentistry: a review of literature. Adv. Eng. Mater. 2019;21(6) [Google Scholar]
- 135.Liu Y., et al. Preliminary investigation on the geometric accuracy of 3D printed dental implant using a monkey maxilla incisor model. Int. J. Bioprint. 2022;8(1) doi: 10.18063/ijb.v8i1.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Londono J., et al. Digital design and 3D printing of an implant-supported prosthetic stent for protecting complete arch soft tissue grafts around dental implants: a dental technique. J. Prosthet. Dent. 2018;120(6):801–804. doi: 10.1016/j.prosdent.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 137.Lugassy D., et al. 3D-Printed teeth with multicolored layers as a tool for evaluating cavity preparation by dental students. Appl. Sci. 2021;11(14):6406. [Google Scholar]
- 138.Mai H.-N., et al. Antibacterial drug-release polydimethylsiloxane coating for 3d-printing dental polymer: surface alterations and antimicrobial effects. Pharmaceuticals. 2020;13(10):304. doi: 10.3390/ph13100304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Malyala S.K., Kumar R., Alwala A.M. A 3D-printed osseointegrated combined jaw and dental implant prosthesis–A case study. Rapid Prototyp. J. 2017 [Google Scholar]
- 140.Maricic S., et al. Additive manufacturing technology in dental education, Rapid Prototyp. J. 2021;27(9):1700–1708. [Google Scholar]
- 141.Marty M., et al. Comparison of student’s perceptions between 3D printed models versus series models in paediatric dentistry hands‐on session. Eur. J. Dent. Educ. 2019;23(1):68–72. doi: 10.1111/eje.12404. [DOI] [PubMed] [Google Scholar]
- 142.Mayer J., et al. Temporary 3D printed fixed dental prosthesis materials: impact of post printing cleaning methods on degree of conversion as well as surface and mechanical properties. Int. J. Prosthodont. (IJP) 2021;34:784–795. doi: 10.11607/ijp.7048. [DOI] [PubMed] [Google Scholar]
- 143.Mehboob H., et al. Bioinspired porous dental implants using the concept of 3D printing to investigate the effect of implant type and porosity on patient’s bone condition. Mech. Adv. Mater. Struct. 2021:1–15. [Google Scholar]
- 144.Moon W., et al. Dimensional accuracy evaluation of temporary dental restorations with different 3d printing systems. Materials. 2021;14(6):1487. doi: 10.3390/ma14061487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Moraru E., et al. Comparative study and mechanical analysis of some additive manufactured dental models. Acta Tech. Napocensis-Series: Appl. Math., Mech., Eng. 2021;64(3) [Google Scholar]
- 146.Mortadi N.A.A., et al. 2022. Cytotoxicity of 3D Printed Materials for Potential Dental Applications: an in Vitro Study. [Google Scholar]
- 147.Moshman A.T. 3D printing technologies and protocols to enhance the dental workflow. Compendium. 2021;42(5) [PubMed] [Google Scholar]
- 148.Nagrath M., et al. Functionalized prosthetic interfaces using 3D printing: generating infection-neutralizing prosthesis in dentistry. Mater. Today Commun. 2018;15:114–119. [Google Scholar]
- 149.Nam N.-E., et al. Effects of artificial tooth brushing and hydrothermal aging on the mechanical properties and color stability of dental 3D printed and CAD/CAM materials. Materials. 2021;14(20):6207. doi: 10.3390/ma14206207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nayar S., Bhuminathan S., Bhat W.M. Rapid prototyping and stereolithography in dentistry. J. Pharm. BioAllied Sci. 2015;7(Suppl 1):S216. doi: 10.4103/0975-7406.155913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Nesic D., et al. 3D printing approach in dentistry: the future for personalized oral soft tissue regeneration. J. Clin. Med. 2020;9(7):2238. doi: 10.3390/jcm9072238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Oberoi G., et al. 3D Printing—encompassing the facets of dentistry. Front. Bioeng. Biotechnol. 2018:172. doi: 10.3389/fbioe.2018.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Øilo M., et al. Mechanical properties of cobalt-chromium 3-unit fixed dental prostheses fabricated by casting, milling, and additive manufacturing. J. Prosthet. Dent. 2018;120(1):156.e1–156.e7. doi: 10.1016/j.prosdent.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 154.Oliveira T.T., Reis A.C. Fabrication of dental implants by the additive manufacturing method: a systematic review. J. Prosthet. Dent. 2019;122(3):270–274. doi: 10.1016/j.prosdent.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 155.Önöral Ö., Abugofa A. Advancements in 3D printing technology: applications and options for prosthetic dentistry. Cyprus J. Med. Sci. 2020;5(2):176–182. [Google Scholar]
- 156.Orel L., et al. Evaluation of the shaping ability of three thermally treated nickel–titanium endodontic instruments on standardized 3D-printed dental replicas using cone-beam computed tomography. Medicina. 2021;57(9):901. doi: 10.3390/medicina57090901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Osman R.B., Alharbi N., Wismeijer D. Build angle: does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology? Int. J. Prosthod. 2017;30(2) doi: 10.11607/ijp.5117. [DOI] [PubMed] [Google Scholar]
- 158.Ouldyerou A., et al. Finite element analyses of porous dental implant designs based on 3D printing concept to evaluate biomechanical behaviors of healthy and osteoporotic bones. Mech. Adv. Mater. Struct. 2022:1–13. [Google Scholar]
- 159.Özcan M., et al. Additive manufacturing technologies for fabrication of biomaterials for surgical procedures in dentistry: a narrative review. J. Prosthodont. 2022;31(S1):105–135. doi: 10.1111/jopr.13484. [DOI] [PubMed] [Google Scholar]
- 160.Pantea M., et al. Comparative study on two methods used in obtaining 3D printed dental models. Mater. Plast. 2019;56(4):812. [Google Scholar]
- 161.Park C., et al. Combining 3D-printed metal and resin for digitally fabricated dentures: a dental technique. J. Prosthet. Dent. 2020;123(3):389–392. doi: 10.1016/j.prosdent.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 162.Park J.-H., et al. Cytocompatibility of 3D printed dental materials for temporary restorations on fibroblasts. BMC Oral Health. 2020;20(1):1–9. doi: 10.1186/s12903-020-01150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Park J.-H., et al. 3D-printed titanium implant with pre-mounted dental implants for mandible reconstruction: a case report. Maxillofac. Plast. Reconstruct. Surg. 2020;42(1):1–4. doi: 10.1186/s40902-020-00272-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Park J.-M., et al. Dimensional accuracy and surface characteristics of 3D-printed dental casts. J. Prosthet. Dent. 2021;126(3):427–437. doi: 10.1016/j.prosdent.2020.07.008. [DOI] [PubMed] [Google Scholar]
- 165.Park S.-M., et al. Flexural strength of 3D-printing resin materials for provisional fixed dental prostheses. Materials. 2020;13(18):3970. doi: 10.3390/ma13183970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Peters O., et al. Evaluation of dental students' skills acquisition in endodontics using a 3D printed tooth model. Euro. Endodont. J. 2021;6(3):290–294. doi: 10.14744/eej.2021.07088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Pillai S., et al. Dental 3D-printing: transferring art from the laboratories to the clinics. Polymers. 2021;13(1):157. doi: 10.3390/polym13010157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Pompa G., et al. Comparison of conventional methods and laser-assisted rapid prototyping for manufacturing fixed dental prostheses: an in vitro study. BioMed Res. Int. 2015;2015 doi: 10.1155/2015/318097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Presotto A.G.C., et al. Feasibility of 3D printed Co–Cr alloy for dental prostheses applications. J. Alloys Compd. 2021;862 [Google Scholar]
- 170.Puškar T., et al. In vitro cytotoxicity assessment of the 3D printed polymer based epoxy resin intended for use in dentistry. Vojnosanit. Pregl. 2019;76(5) [Google Scholar]
- 171.Qin W., et al. Design, 3D printing, and evaluation of full-contact dental models for denture tests. Int. J. Comput. Dent. 2022;25(2):141–150. doi: 10.3290/j.ijcd.b2588203. [DOI] [PubMed] [Google Scholar]
- 172.Qu F., Du X., Liu W.-C. 3D-printed custom trays with a Gothic arch for centric relation recording and definitive impression making for complete dentures: a dental technique. J. Prosthet. Dent. 2019;121(1):32–36. doi: 10.1016/j.prosdent.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 173.Reddy R.R., et al. Additive manufacturing of a human mandible and Finite element analysis of dental implant for prosthodontic applications. Mater. Today: Proc. 2021;45:3028–3035. [Google Scholar]
- 174.Řehounek L., Jíra A. Experimental and numerical analyses of a 3D-printed titanium trabecular dental implant. Acta Polytech. 2017;57(3):218–228. [Google Scholar]
- 175.Revilla León M., et al. 3D metal printing-additive manufacturing technologies for frameworks of implant-borne fixed dental prosthesis. Eur. J. Prosthodont. Restor. Dent. 2017;25(3):143–147. doi: 10.1922/EJPRD_RevillaLeon05. [DOI] [PubMed] [Google Scholar]
- 176.Revilla-León M., et al. Workflow of a fiber-reinforced composite fixed dental prosthesis by using a 4-piece additive manufactured silicone index: a dental technique. J. Prosthet. Dent. 2021;125(4):569–575. doi: 10.1016/j.prosdent.2020.02.030. [DOI] [PubMed] [Google Scholar]
- 177.Revilla-León M., et al. Adhesion of veneering porcelain to cobalt-chromium dental alloys processed with casting, milling, and additive manufacturing methods: a systematic review and meta-analysis. J Prosthet. Dent. 2021;128(4):575–588. doi: 10.1016/j.prosdent.2021.01.001. [DOI] [PubMed] [Google Scholar]
- 178.Revilla‐León M., et al. Position accuracy of implant analogs on 3D printed polymer versus conventional dental stone casts measured using a coordinate measuring machine. J. Prosthodont. 2018;27(6):560–567. doi: 10.1111/jopr.12708. [DOI] [PubMed] [Google Scholar]
- 179.Revilla-León M., et al. Additive manufacturing technologies for processing zirconia in dental applications. Int. J. Comput. Dent. 2020;23(1):27–37. [PubMed] [Google Scholar]
- 180.Revilla-León M., et al. Digital workflow for an esthetic rehabilitation using a facial and intraoral scanner and an additive manufactured silicone index: a dental technique. J. Prosthet. Dent. 2020;123(4):564–570. doi: 10.1016/j.prosdent.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 181.Revilla-León M., Sadeghpour M., Özcan M. An update on applications of 3D printing technologies used for processing polymers used in implant dentistry. Odontology. 2020;108(3):331–338. doi: 10.1007/s10266-019-00441-7. [DOI] [PubMed] [Google Scholar]
- 182.Revilla‐León M., Sadeghpour M., Özcan M. A review of the applications of additive manufacturing technologies used to fabricate metals in implant dentistry. J. Prosthodont. 2020;29(7):579–593. doi: 10.1111/jopr.13212. [DOI] [PubMed] [Google Scholar]
- 183.Revilla-León M., et al. A report on a diagnostic digital workflow for esthetic dental rehabilitation using additive manufacturing technologies. Int. J. Esthet. Dent. 2018;13(2):184–196. [PubMed] [Google Scholar]
- 184.Revilla-León M., et al. Color dimensions of additive manufactured interim restorative dental material. J. Prosthet. Dent. 2020;123(5):754–760. doi: 10.1016/j.prosdent.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 185.Reymus M., et al. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: the impact of resin material, build direction, post-curing, and artificial aging—an in vitro study. Clin. Oral Invest. 2020;24(2):701–710. doi: 10.1007/s00784-019-02952-7. [DOI] [PubMed] [Google Scholar]
- 186.Reymus M., et al. 3D‐printed model for hands‐on training in dental traumatology. Int. Endod. J. 2018;51(11):1313–1319. doi: 10.1111/iej.12947. [DOI] [PubMed] [Google Scholar]
- 187.Richter M., et al. 3D printed versus commercial models in undergraduate conservative dentistry training. Euro. J. Dent. Educ. 2021 doi: 10.1111/eje.12742. [DOI] [PubMed] [Google Scholar]
- 188.Romero L., et al. New design for rapid prototyping of digital master casts for multiple dental implant restorations. PLoS One. 2015;10(12) doi: 10.1371/journal.pone.0145253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Sa L., et al. 3D printing dental composite resins with sustaining antibacterial ability. J. Mater. Sci. 2019;54(4):3309–3318. [Google Scholar]
- 190.Sabbah A., Romanos G., Delgado-Ruiz R. Impact of layer thickness and storage time on the properties of 3d-printed dental dies. Materials. 2021;14(3):509. doi: 10.3390/ma14030509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Santos E.O., et al. Surface characteristics and microbiological analysis of a vat-photopolymerization additive-manufacturing dental resin. Materials. 2022;15(2):425. doi: 10.3390/ma15020425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Schönhoff L.M., et al. 3D printing of dental restorations: mechanical properties of thermoplastic polymer materials. J. Mech. Behav. Biomed. Mater. 2021;119 doi: 10.1016/j.jmbbm.2021.104544. [DOI] [PubMed] [Google Scholar]
- 193.Schweiger J., et al. Histo-anatomic 3D printing of dental structures. Br. Dent. J. 2016;221(9):555–560. doi: 10.1038/sj.bdj.2016.815. [DOI] [PubMed] [Google Scholar]
- 194.Schweiger J., Edelhoff D., Güth J.-F. 3D printing in digital prosthetic dentistry: an overview of recent developments in additive manufacturing. J. Clin. Med. 2021;10(9):2010. doi: 10.3390/jcm10092010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Scribante A., et al. Properties of CAD/CAM 3D printing dental materials and their clinical applications in orthodontics: where are we now? Appl. Sci. 2022;12(2):551. [Google Scholar]
- 196.Sheeba T.B., et al. Analysis of silica based prosthetic human teeth using 3D printing machine for dental assistance. Mater. Today: Proc. 2021;45:2440–2443. [Google Scholar]
- 197.Shin S.-H., et al. Evaluation of the 3D printing accuracy of a dental model according to its internal structure and cross-arch plate design: an in vitro study. Materials. 2020;13(23):5433. doi: 10.3390/ma13235433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Sidhom M., et al. Effect of different CAD/CAM milling and 3D printing digital fabrication techniques on the accuracy of PMMA working models and vertical marginal fit of PMMA provisional dental prosthesis: an in vitro study. Polymers. 2022;14(7):1285. doi: 10.3390/polym14071285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Soares P.V., et al. Rapid prototyping and 3D‐virtual models for operative dentistry education in Brazil. J. Dent. Educ. 2013;77(3):358–363. [PubMed] [Google Scholar]
- 200.Son K., Lee J.-H., Lee K.-B. Multidisciplinary Digital Publishing Institute; 2021. Comparison of Intaglio Surface Trueness of Interim Dental Crowns Fabricated with SLA 3D Printing, DLP 3D Printing, and Milling Technologies. (Healthcare). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Son K., Lee K.-B. A novel method for precise guided hole fabrication of dental implant surgical guide fabricated with 3d printing technology. Appl. Sci. 2020;11(1):49. [Google Scholar]
- 202.Srinivasan M., et al. CAD-CAM complete removable dental prostheses: a double-blind, randomized, crossover clinical trial evaluating milled and 3D-printed dentures. J. Dent. 2021;115 doi: 10.1016/j.jdent.2021.103842. [DOI] [PubMed] [Google Scholar]
- 203.Su C.-Y., et al. Additive manufacturing of dental prosthesis using pristine and recycled zirconia solvent-based slurry stereolithography. Ceram. Int. 2020;46(18):28701–28709. [Google Scholar]
- 204.Tamimi F., et al. Osseointegration of dental implants in 3D-printed synthetic onlay grafts customized according to bone metabolic activity in recipient site. Biomaterials. 2014;35(21):5436–5445. doi: 10.1016/j.biomaterials.2014.03.050. [DOI] [PubMed] [Google Scholar]
- 205.Tancu A., et al. 3D printed dental models. Mater. Plast. 2019;56:51–54. [Google Scholar]
- 206.Tatar N., Tuzlalı M., Bahçe E. Investigation of the lattice production of removable dental prostheses with CoCr alloy using additive manufacturing. J. Mater. Eng. Perform. 2021;30(9):6722–6731. [Google Scholar]
- 207.Tedesco J., et al. Osseointegration of a 3D printed stemmed titanium dental implant: a pilot study. Int. J. Dent. 2017;2017 doi: 10.1155/2017/5920714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Tian Y., et al. A review of 3D printing in dentistry: technologies, affecting factors, and applications. Scanning. 2021;2021 doi: 10.1155/2021/9950131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Tichy A., et al. Release of bisphenol A from milled and 3D-printed dental polycarbonate materials. Materials. 2021;14(19):5868. doi: 10.3390/ma14195868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Told R., et al. Manufacturing a first upper molar dental forceps using continuous fiber reinforcement (CFR) additive manufacturing technology with carbon-reinforced polyamide. Polymers. 2021;13(16):2647. doi: 10.3390/polym13162647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Towers A., et al. Combining virtual reality and 3D‐printed models to simulate patient‐specific dental operative procedures—a study exploring student perceptions. Eur. J. Dent. Educ. 2022;26(2):393–403. doi: 10.1111/eje.12715. [DOI] [PubMed] [Google Scholar]
- 212.Tunchel S., et al. 3D printing/additive manufacturing single titanium dental implants: a prospective multicenter study with 3 years of follow-up. Int. J. Dent. 2016;2016 doi: 10.1155/2016/8590971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Turkyilmaz I., Wilkins G.N. 3D printing in dentistry–Exploring the new horizons. J. Dent. Sci. 2021;16(3):1037. doi: 10.1016/j.jds.2021.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Waldecker M., et al. Fully digital fabrication of an occlusal device using an intraoral scanner and 3D printing: a dental technique. J. Prosthet. Dent. 2019;121(4):576–580. doi: 10.1016/j.prosdent.2018.09.021. [DOI] [PubMed] [Google Scholar]
- 215.Wang H., Lim J.Y. Metal-ceramic bond strength of a cobalt chromium alloy for dental prosthetic restorations with a porous structure using metal 3D printing. Comput. Biol. Med. 2019;112 doi: 10.1016/j.compbiomed.2019.103364. [DOI] [PubMed] [Google Scholar]
- 216.Wang Y.-C., Chen T., Lin Y.-C. Multidisciplinary Digital Publishing Institute; 2019. A Collaborative and Ubiquitous System for Fabricating Dental Parts Using 3D Printing Technologies. (Healthcare). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Wang Y.-T., et al. Developing customized dental miniscrew surgical template from thermoplastic polymer material using image superimposition, CAD system, and 3D printing. BioMed Res. Int. 2017;2017 doi: 10.1155/2017/1906197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Yang F., et al. Laser beam melting 3D printing of Ti6Al4V based porous structured dental implants: fabrication, biocompatibility analysis and photoelastic study. Sci. Rep. 2017;7(1):1–12. doi: 10.1038/srep45360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Yang Y., et al. Fabrication and evaluation of dental fillers using customized molds via 3D printing technology. Int. J. Pharm. 2019;562:66–75. doi: 10.1016/j.ijpharm.2019.03.024. [DOI] [PubMed] [Google Scholar]
- 220.Yang Z., et al. 3D printing of diamond tools for dental ceramics processing. Adv. Eng. Mater. 2018;20(3) [Google Scholar]
- 221.Ye N., et al. Precision of 3D-printed splints with different dental model offsets. Am. J. Orthod. Dentofacial Orthop. 2019;155(5):733–738. doi: 10.1016/j.ajodo.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 222.Yoo S.-Y., et al. Dimensional accuracy of dental models for three-unit prostheses fabricated by various 3D printing technologies. Materials. 2021;14(6):1550. doi: 10.3390/ma14061550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Zafar S., Renner M.P., Zachar J.J. Dental trauma simulation training using a novel 3D printed tooth model. Dent. Traumatol. 2020;36(6):641–647. doi: 10.1111/edt.12585. [DOI] [PubMed] [Google Scholar]
- 224.Zhang C., et al. 3D-printed pre-tapped-hole scaffolds facilitate one-step surgery of predictable alveolar bone augmentation and simultaneous dental implantation. Compos. B Eng. 2022;229 [Google Scholar]
- 225.Zhang X., et al. Mechanical properties and osteoblast proliferation of complex porous dental implants filled with magnesium alloy based on 3D printing. J. Biomater. Appl. 2021;35(10):1275–1283. doi: 10.1177/0885328220957902. [DOI] [PubMed] [Google Scholar]
- 226.Zhao M., et al. 3D-printed strong hybrid materials with low shrinkage for dental restoration. Compos. Sci. Technol. 2021;213 [Google Scholar]
- 227.Zhao M., et al. 3D‐Printed strong dental crown with multi‐scale ordered architecture, high‐precision, and bioactivity. Adv. Sci. 2022;9(5) doi: 10.1002/advs.202104001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Monzón M.D., Paz R., Bordón P. In: 12 - Present and Future of Standardization of Additive Manufacturing in the Medical Field, second ed. Kalaskar D.M., editor. Woodhead Publishing; 2023. pp. 361–378. (3D Printing in Medicine). [DOI] [Google Scholar]
- 229.Srinivasan M., et al. CAD-CAM removable complete dentures: a systematic review and meta-analysis of trueness of fit, biocompatibility, mechanical properties, surface characteristics, color stability, time-cost analysis, clinical and patient-reported outcomes. J. Dent. 2021;113 doi: 10.1016/j.jdent.2021.103777. [DOI] [PubMed] [Google Scholar]
- 230.Moher D., et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supplementary material/referenced in article.