Abstract
This study is the first systematic review to investigate the relationship between food insecurity (FI) and disordered eating behaviors exclusively in children and adolescents. Database searches were conducted in PUBMED, Embase, PsycINFO, ProQuest, and Gale OneFile: Informe Académico using English and Spanish search terms. Studies were included if they were published before August 2022, included youth aged 18 years and below, included either parent- or child-report of food security status, included either parent- or child-report of child disordered eating behaviors, and examined the relationship between food security status and child disordered eating behaviors. Following independent title/abstract and full-text screening, 20 studies were included in the review. There were 13 cross-sectional studies, five longitudinal studies, and two qualitative studies, from the United States (19 studies), and Bangladesh (1 study). Sample sizes ranged from 33 to 6,077. Findings generally indicated a relationship between FI and behaviors such as binge eating, loss-of-control eating, eating in the absence of hunger, unhealthy weight control behaviors, and picky eating in children and adolescents, though this association varied depending on the type of disordered eating behavior assessed and FI severity. Results highlight the importance of screening for disordered eating behaviors among youth with FI towards eating disorder prevention and intervention. However, given the limited number of primary research articles examining this relationship in youth, further hypothesis-driven research is needed. In addition, more global representation and additional longitudinal studies are needed to further examine the generalizability and temporality of FI and disordered eating in children and adolescents.
Keywords: Food insecurity, children, adolescents, disordered eating, eating disorders, social determinants of health
1. Food Insecurity and Disordered Eating Behaviors in Children and Adolescents: A Systematic Review
Food insecurity (FI) is “a household-level economic and social condition of limited or uncertain access to adequate food” (United States (US) Department of Agriculture, 2022) and is associated with both physical and mental health consequences. Research with adults has found a positive association between FI and obesity, type II diabetes, hypertension, depression, anxiety, and other deleterious mental health outcomes (Abdurahman et al., 2019; Arenas et al., 2019; Jones, 2017; Weaver & Fasel, 2018). In children and adolescents, FI has been linked to lower educational achievement, cognitive deficits, impaired growth and development, depression, suicidal ideation, and other poor mental health indices (Burke et al., 2016; Jones, 2017; McIntyre et al., 2013; Shankar et al., 2017). In 2021, 12.5% of US households with children experienced FI (Coleman-Jensen et al., 2021). Of those households, about half reported FI that affected both the adults and children, which is usually a more severe form of FI, as parents generally attempt to shield their children from the effects of FI when possible (Coleman-Jensen et al., 2021).
Hazzard and colleagues (2020) published a review on the emerging research between FI and eating disorders (EDs), finding positive associations between FI and disordered eating; however, most studies available at the time were conducted with adults. Considering ED risk factors and behaviors tend to emerge in early/late adolescence (Rohde et al., 2015), the harmful mental and physical health effects associated with EDs (Hudson et al., 2007; Mitchell & Crow, 2006; Smith et al., 2019), and the association between FI and disordered eating in adults (Hazzard et al., 2020), a systematic review examining the relationship between FI and disordered eating in children and adolescents is needed. The purpose of this study was to gather, review, and summarize the available information on the relationship between FI and disordered eating in children and adolescents in English and Spanish language literature. We hypothesized there would be a positive association between FI and disordered eating in children and adolescents.
2. Method
2.1. Search Strategy
The authors followed PRISMA guidelines throughout the systematic review process, and the study was preregistered at https://osf.io/84nr6/. Empirical articles published before August 2022 were searched for using PUBMED, Embase, PsycINFO, ProQuest, and Gale OneFile: Informe Académico online databases. The latter database was used for searching Spanish-language articles using Spanish search terms. The first authors (TB and AVC) are both native Spanish speakers and used Spanish translations of disordered eating-related terms for the Spanish-language article search. All search terms are in Table 1 and were searched in the title, abstract, full text, and keywords of the articles. To identify grey literature (e.g., unpublished theses, dissertations, and conference abstracts), the first authors (TB and AVC) conducted searches on ProQuest utilizing the same search terms used for the empirical article search. Additionally, TB contacted corresponding authors of the included empirical articles, asking for unpublished works on the topic of FI and disordered eating in youth ≤18 for a systematic review. TB posted a similar request on Twitter and via a listserv of ED clinicians and researchers to solicit unpublished data for inclusion in this review.
Table 1.
Search terms used across online databases*
| Search Terms English |
Search Terms Spanish |
|---|---|
|
| |
| food insecurity OR food security OR food insufficiency OR food neglect | inseguridad alimentaria OR inseguridad alimenticia OR seguridad alimentaria OR seguridad alimenticia OR descuido alimenticio OR inseguridad nutricional |
| AND | AND |
| anorexia nervosa OR bulimia nervosa OR avoidant/restrictive food intake disorder OR binge-eating disorder OR dietary restraint OR restrictive eating OR disordered eating OR food restriction OR loss of control eating OR food addiction OR eating pathology OR eating disorder | anorexia nervosa OR bulimia nervosa OR trastorno por evitación OR trastorno por restricción de la ingesta de alimentos OR trastorno por atracón OR restricción dietética OR alimentación restrictiva OR restricción de alimentos OR pérdida de control alimenticio OR adicción a la comida OR desorden alimentario OR desorden alimenticio |
Note
Databases searched using both English and Spanish search terms included: PUBMED, Embase, PsycINFO, and ProQuest. Database searched using only Spanish search terms was Gale OneFile: Informe Académico.
2.2. Inclusion and Exclusion Criteria
For inclusion in the review, studies must have: (1) been published in English or Spanish prior to August 2022, (2) included youth aged 18 years and below, (3) included either parent- or child-report of food security status, (4) included either parent- or child-report of child disordered eating symptoms, and (5) examined the relationship between food security status and child disordered eating symptoms. Case studies, systematic and non-systematic reviews, commentaries and letters to the editor, exact duplicates, registered reports, grant proposals, and research in non-human subjects were excluded.
2.3. Screening, Selection, and Data Extraction
Article titles and abstracts obtained through database searches were imported to Covidence, an online systematic review management tool. Duplicates were removed via Covidence, and all other duplicates that were not detected by Covidence were manually removed. The first authors (AVC and TB) independently screened article titles and abstracts on Covidence. When their decisions whether to move a study on to full text review were in conflict, the remaining authors (blind to the initial reviewers’ ratings) made the final decision. Full text files were then downloaded and imported to Covidence. A double-blinded full text review by two independent reviewers and, if needed, a third independent and blinded reviewer, was conducted to assess final study inclusion.
3. Results
The initial database searches yielded 2363 articles. One unpublished manuscript was obtained via a Twitter announcement (Urban et al., n.d.). Of these 2363 articles, 454 were duplicates. The remaining 1910 underwent title/abstract screening, and 61 articles were identified for full-text review. Forty-one articles were excluded from the review, resulting in a final sample size of 20. Notably, no Spanish-language studies met inclusion criteria. The PRISMA flow diagram is shown in Figure 1.
Figure 1.
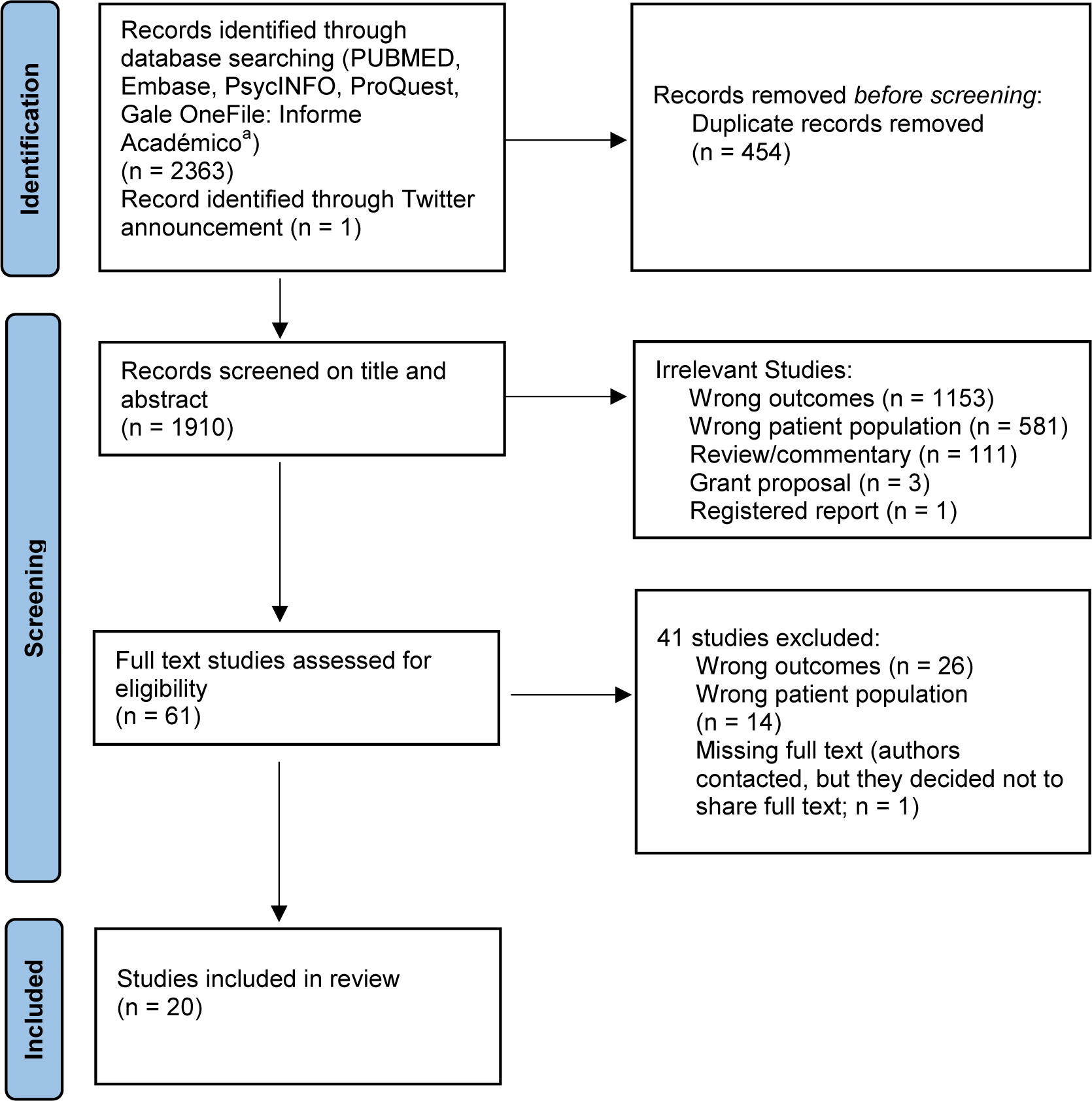
PRISMA flow diagram
Note:
a Thirty-eight records were identified using Spanish-language search terms. Eight were duplicates. The remaining 30 were screened using titles/abstracts; however, none met inclusion criteria (wrong outcomes (20), wrong population (4), review/commentary (6)). These studies are included in the PRISMA diagram above.
Most studies employed a cross-sectional design (n=13), followed by longitudinal (n=5) and qualitative (n=2) designs. Sample sizes ranged from 33 to 6,077 (see Table 2). Ages ranged from 5–23, though studies that solely focused on individuals aged 19 years or older were excluded. In other words, studies including 19–23-year-olds (yo) were included only if they reported results relevant to youth ≤18yo and the baseline mean age was ≤18. Studies were based in the US (n=19), and Bangladesh (n=1). Cis-gender male and female youth were well-represented; however, only three studies included gender non-binary and transgender youth. Studies varied significantly in terms of the racial/ethnic backgrounds of study participants. Five of the 20 studies (Hazzard et al., 2022; Hooper et al., 2022; Hooper et al., 2020; West et al., 2019; Wickel, 2014) were conducted using data from Project EAT (Eating and Activity in Teens), EAT 2010, and Project F-EAT (including family/home factors), which surveyed adolescents and their parents/guardians across multiple time points in Minnesota, US.
Table 2.
Studies included in the systematic review
| Study and Country | Study type | Sample size | Mean age (yrs.) | Age range (yrs.) | Gender | Race and/or Ethnicity |
|---|---|---|---|---|---|---|
| Barry et al., 2022, US | C | 194 children | 8.9 | 8–10 | F: 53.6% M: 46.4% |
Reported only for female primary caregivers Caregiver of Color: 40.7% (Black/African American: 67.1%, Asian: 2.5%, Hispanic: 3.8%, Middle Eastern/North African: 1.3%, Multiracial/Multiethnic: 13.9%, Other: 11.4%) White: 69.3% |
| Berge et al., 2020, US | C | 150 families | 6.4 | 5–7 | F: 52.7% M: 47.3% |
Black/African American: 16.7% White: 16.7% Hmong: 16.7% Hispanic: 16.7% Native American: 16.7% Somali: 16.7% |
| Blum et al., 2019, Bangladesh | Q | 33 girls; teachers (2), community leaders (1), community health workers (4), fathers (4), mothers (4), and boys (4) |
Reported only for adolescent girls School going: 15.8 Non-school-going: 16.1 Married: 17.5 |
15–19 | F: 71.2% M: 15.4% |
Not reported |
| Harshman et al., 2022, US | L | 407 children | 9.6 | 6–12 | F: 45% M: 55% |
Hispanic: 92.9% |
| Hazzard et al., 2022, US | L | 1813 youth | EAT-I: 14.9 EAT-II: 19.5 |
EAT-I: 11–18 EAT-II: 16–23 |
F: 57.1% M: 42.9% |
Black/African American: 17.8 % White: 50.7% Asian: 17.9% Hispanic: 5.7% Multiracial/Multiethnic or Other: 7.9% |
| Hooper et al., 2022, US | L | 1340 youth | Baseline: 14.5 Follow-Up: 22.0 |
Not reported | F: 53.0% M: 46.3% T/NB: 0.7% |
Black/African American: 28.6% White: 20.3% Asian: 19.3% Hispanic: 16.9% Multiracial/Multiethnic or Other: 14.9% |
| Hooper et al., 2020, US | C | 2285 parent and adolescent dyads | 14.5 | 10–22 | F: 54.2% M: 45.8% |
Black/African American: 28.0% White: 21.0% Asian: 19.5% Native American: 3.2% Hispanic: 17.2% Multiracial/Multiethnic or Other: 11.3% |
| Kim et al., 2021, US | C | 58 adolescents | 15.2 | 11.1–18.9 | F: 62.1% M: 37.9% |
Black/African American: 50% White: 15% Native American: 1.7% Hispanic: 34.5% Multiracial/Multiethnic: 6.9% Other: 19% |
| Kral et al., 2017, US | C | 50 families | Not provided for total sample Food Insecure: 9.8 Food Secure: 9.5 |
8–10 | Not provided for total sample Food Insecure: F: 61.5% M: 38.5% Food Secure: F: 48.6% M: 51.4% |
Not provided for total sample Food Insecure: Black/African American: 84.6% White: 0% Multiracial/Multiethnic: 15.4% Food Secure: Black/African American: 62.2% White: 29.7% Multiracial/Multiethnic: 8.1% |
| Linsenmeyer et al., 2021, US | C | 164 participants | 17.0 | 12–23 | TF: 17.1% TM: 78.0% NB: 4.9% |
Not reported |
| Masler et al., 2021, US | C | 6077 participants | Not reported | 8–15 | F: 49.1% M: 50.9% |
Black/African American: 14.2% White: 57.7% Hispanic: 20.0% Other: 8.1% |
| McCurdy et al., 2022, US | C | 66 families | 3.6 | 2–5 | F: 44.6% M: 55.4% |
Hispanic: 86.6% |
| McGowan et al., 2022, US | C | 183 children | 9.0 | 8–10 | F: 54.6% M: 45.4% |
Reported only for primary female caregivers Black/African American: 26.2% White: 60.7% Asian: 1.1% Middle Eastern/North African: 0.5% Hispanic: 1.6% Multiracial/Multiethnic: 4.9% Other: 4.9% |
| Ruzicka, 2020, US | C | 73 adolescents | 13.6 | 12–17 | F: 47.9% M: 52.1% |
Black/African American: 34.2% White: 56.2% Multiracial/Multiethnic or Other: 9.6% |
| Stadterman et al., 2021, US | C | 34 youth | 12.8 | 8–18 | F: 59% M: 41% |
Black/African American: 48.6% White: 2.9% Asian: 2.9% Hispanic: 22.9% Multiracial/Multiethnic: 17.1% Other: 5.8% |
| Tester et al., 2016, US | Q | 37 children represented by 47 focus group participants: caregivers (42), siblings (2), patients (3) | 11.5 | 2–18 | F: 46%, M: 54% | Not reported |
| Urban et al., n.d., US | L | 729 youth | 16.0 | 6–24 | F: 82% M: 11% T/NB: 6% Other: 1% |
Black/African American: 1.2% White: 64% Asian: 7.6% Hispanic: 5.5% Multiracial/Multiethnic: 15.4% Other: 6.4% |
| West et al., 2021, US | C | 60 children | 13.9 | 12–18 | F: 53.3% M: 46.7% |
Black/African American: 9.0% White: 73.1% Asian: 1.7% Multiracial/Multiethnic: 6.0% Hispanic: 1.7% Other or Don’t Know: 20.0% |
| West et al., 2019, US | L | 2179 adolescents | EAT-I: 14.9, EAT-II: Not reported | EAT-I: 11–18 EAT-II: 16–23 |
F: 52.8%, M: 47.2% | High SES: Black/African American: 6.3% White: 80.7% Asian: 9.6% Hispanic: 1.9% Other: 1.3% Low SES: Black/African American: 13.2% White: 49.8% Asian: 27.3% Hispanic: 5.7% Other: 4.0% |
| Wickel, 2014, US | C | 883 adolescents | Not reported | Not reported | F: 53.7% M: 46.3% |
Black/African American: 13.9% White: 27.86% Asian: 27.63% Hispanic: 21.5% Other: 8.6% |
Note: ND/UP. = No date/unpublished; C = Cross-sectional, L = Longitudinal, Q = Qualitative; F = Female, M = Male, TF = Transgender Female, TM = Transgender Male, NB = Nonbinary, T/NB = Transgender/Non-Binary
3.1. Assessment of Food Insecurity and Disordered Eating
FI was most frequently measured using a version of the US Department of Agriculture’s Household Food Security Survey Module (Carlson et al., 1999; n=15). Other studies (Harshman et al., 2022; Linsenmeyer et al., 2021) utilized the Hunger Vital Sign screening tool (Hager et al., 2010), an adapted version of the Child Food Security Assessment (Fram et al., 2013; McGowan et al., 2022), a one-item measure of FI developed by the study team (Urban et al., n.d.), and open-ended questions (Blum et al., 2019) to assess FI. Regarding disordered eating outcomes, six studies focused on multiple aspects of eating pathology, including unhealthy weight control behaviors (e.g., fasting, skipping meals, taking diet pills), dietary restraint, binge eating, picky eating1 behaviors, and/or general eating pathology (Barry et al., 2022; Hazzard et al., 2022; Hooper et al., 2022; Hooper et al., 2020; Kim et al., 2021; Linsenmeyer et al., 2021; McGowan et al., 2022; Urban et al., n.d.; West et al., 2019; Wickel, 2014). Other studies focused on binge eating and loss-of-control eating (Ruzicka, 2020; West et al., 2021), eating in the absence of hunger (Harshman et al., 2022; Kral et al., 2017), eating in response to negative emotions or boredom (Kral et al., 2017; McCurdy et al., 2022; Ruzicka, 2020), unhealthy weight control behaviors (Masler et al., 2021), dietary restraint (Stadterman et al., 2021), picky eating (Berge et al., 2020), food hiding behaviors (Harshman et al., 2022), disordered eating in pediatric weight management (Harshman et al., 2022; Tester et al., 2016), and gender-related restrictive eating during food shortages (Blum et al., 2019).
3.2. Synthesis of Study Results
3.2.1. Cross-Sectional Studies
Linsenmeyer et al., 2021, examined the relationship between FI and disordered eating in 164 transgender and gender nonbinary youth (12–23yo, Mage=17.0, SD=2.3). In this sample, 21.2% screened positive for FI, 8.7% had a previous ED diagnosis, and a significant, positive correlation between binge eating and FI was found. In addition, those with a previous ED diagnosis scored higher on the hunger questionnaire, suggesting a potentially compounding effect with FI (Linsenmeyer et al., 2021).
FI was not associated with endorsement of binge eating or dietary restraint among 58 adolescents (11.1–18.9yo, Mage=15.2, SD=2.1) recruited from clinical and community samples (Kim et al., 2021). However, for adolescents who endorsed at least one binge-eating episode, those who experienced FI reported a greater number of binge-eating episodes compared to those who did not experience FI. Such findings indicate that FI may have a particular association with binge-eating severity, and this relationship was particularly salient for adolescents identifying with Hispanic ethnicity (n=20; Kim et al., 2021). Another study examining the relationship between FI and dietary restraint in a sample of 34 youth did not find statistically significant relationships between FI status and dietary restraint (Mage=12.8, SD=2.6; Stadterman et al., 2021). However, when examining effect sizes, a moderate effect size was found for dietary restraint, such that food insecure youth endorsed greater dietary restraint (Stadterman et al., 2021). Additional studies exploring the relationship between FI and dietary restraint with larger sample sizes are needed. Related to binge-eating behaviors, in a sample of 60 adolescents (12–17yo, Mage=13.9, SD=1.8), more severe FI was positively associated with loss-of-control eating when adjusting for sociodemographic factors (West et al., 2021). Further, FI significantly moderated the relationship between household income-to-needs ratio and number of loss-of-control eating episodes, such that higher FI and lower income-to-needs ratio were related to a greater number of loss-of-control eating episodes (West et al., 2021).
Nevertheless, in unadjusted models using EAT 2010 and F-EAT data (N=2,285, 10–22yo, Mage=14.5, SD=2.0), FI was not related to binge eating, self-induced vomiting, or using diet pills or food substitutes (Hooper et al., 2020). However, FI was associated with higher endorsement of unhealthy weight control behaviors (UWCBs), including fasting, eating little food, skipping meals, and using laxatives or diuretics for weight-control purposes. In models adjusting for sociodemographic factors, however, only the associations between FI and fasting and laxative use remained significant. Additionally, a study using a subsample from EAT 2010 and F-EAT data (N=883, Mage=not reported, SD=not reported) examined whether concordance or discordance between adolescent and parent-report of FI were differentially associated with binge eating or UWCBs in middle and high school-aged adolescents (Wickel, 2014). In an adjusted model predicting UWCBs, discordant conditions (in particular, the following conditions: (1) adolescents who endorsed food security while one parent endorsed FI and the other parent endorsed food security and (2) adolescents who endorsed FI while both parents endorsed food security) was associated with lower odds (0.36 and 0.34, respectively) of UWBCs compared to the concordant condition where both adolescents and parents reported food security (Wickel, 2014). Further, in an adjusted model predicting binge eating, the discordant condition in which adolescents endorsed FI while both parents endorsed food security was associated with 3.38 greater odds of binge eating compared to the concordant condition where both adolescents and parents reported food security (Wickel, 2014).
Similarly, in a cohort of 194 preadolescent children (8–10yo, Mage=8.9, SD=0.8), investigators examined whether children endorsed differential levels of disordered eating symptoms in relation to child versus parent report of FI (Barry et al., 2022). Adjusted models indicated that child-reported FI was associated with higher overall disordered eating symptoms and higher preoccupation with food and weight (but not UWCBs like dieting or vomiting), whereas caregiver-reported FI was not associated with any disordered eating symptoms (Barry et al., 2022). However, the relationship between caregiver-reported FI and dieting behavior was moderated by gender. The association was null for boys, but for girls, those from food insecure households endorsed less dieting behavior compared to girls from food secure households (Barry et al., 2022). When child-reported FI was included in adjusted models as a continuous variable, analyses stratified by gender identified that boys who endorsed higher levels of FI endorsed greater dieting behavior, whereas this association was not significant in girls (Barry et al., 2022). Differences in child and parent reports of FI appear to be related to disordered eating outcomes in children, such that child but not parent recognition of FI status is associated with greater overall ED symptoms, and gender may modify this relationship for UWCBs like dieting.
Another large study examining the association between FI and UWCBs and weight loss attempts among 6077 children (8–15yo, Mage and SD not reported) found that, in unadjusted models, children with low and very low food security were more likely to engage in UWCBs compared to children who were food secure (Masler et al., 2021). However, in multivariate analyses controlling for sociodemographic factors, those with low food security were no longer more likely to engage in UWCBs compared to food secure youth. The results were maintained for those with very low food security, and those with marginal food security emerged as more likely to engage in UWCBs compared to food secure children. In unadjusted analyses, children with low food security and very low food security attempted to lose weight more frequently than children who were food secure. However, in multivariate analyses, the significant difference only remained for children with very low food security, and among those, weight status moderated the relationship, such that it was significant among children with average weight but not among children with overweight/obesity. Taken together, some of the significant findings between FI and UWCBs from larger studies tend to lose (or sometimes gain) significance when relevant sociodemographic covariates are considered, and those with very low food security have more consistent associations.
In a younger sample, children who reported experiencing FI expressed significantly higher levels of disordered eating behaviors when compared to children from food-secure households (N=183, 8–10yo, Mage=9.0, SD=0.8; McGowan et al., 2022) as measured by total scores on the Children’s Eating Attitudes Test (Maloney et al., 1988). In a similarly aged sample of 50 8–10yo children, those from food insecure households (n=13, Mage=9.8, SD=0.8) reportedly engaged in greater eating past satiation and in the absence of hunger than their peers from food secure households (n=37, Mage=9.5, SD=0.8; Kral et al., 2017). However, this association became non-significant when adjusting for household income and maternal race. In the same study, FI was unrelated to eating in response to negative affect or boredom (Kral et al., 2017). Research conducted in adolescents (N=73, 12–17yo, Mage=13.6, SD=1.4) similarly showed that FI was not significantly associated with emotional eating (Ruzicka, 2020). Further, FI was not significantly correlated with loss-of-control eating in the same study (Ruzicka, 2020). It is unclear whether, when examining correlations between FI and disordered eating symptoms (i.e., emotional eating and loss-of-control eating), the study authors examined FI continuously rather than using rank-order correlations depending on FI severity categorizations (i.e., families with food security, families with FI without hunger, families with FI with hunger, and families with FI with severe hunger), which may account for potential differences in findings.
In even younger samples of children, those from food insecure households had significantly higher levels of food responsiveness (i.e., the desire to eat palatable food when exposed to it) and enjoyment of food compared to children from food secure households (N=66 families, Mage=3.6, SD=0.9; McCurdy et al., 2022). However, FI was not related to overeating in response to emotions (McCurdy et al., 2022). Cross-sectional data from ecological momentary assessment surveys examined the relationship between FI and picky eating (assessed by food refusal) among children in relation to their caregivers’ mood (N=150; 5–7yo, Mage=6.4, SD=0.8; Berge et al., 2020). Children in food secure, but not food insecure, households were more likely to display picky eating behaviors on days in which parents reported depressed mood or stress. Children in food insecure households did not alter picky eating behaviors in response to parent mood/stress, but still refused food more than food secure children (Berge et al., 2020).
3.2.2. Longitudinal Studies
Children (N=407; 6–12yo, Mage=9.58, SD=1.83) enrolled in a weight management treatment trial were assessed for overeating behaviors (defined by the authors as sneaking, hiding, or hoarding food, and eating in the absence of hunger) at baseline and 12 months (Harshman et al., 2022). Across conditions, children decreased overeating behaviors over time. However, children from food insecure households were approximately two times as likely to engage in eating in the absence of hunger at follow-up compared to children from food secure households. However, FI was not associated with food-hiding behaviors.
Results from youth with FI in a 20-week family-based treatment (FBT) program for EDs (predominantly anorexia nervosa, with 13% meeting criteria for avoidant restrictive food intake disorder; N=72; 6–24yo, Mage =16.0, SD=2.77) showed that youth with FI had higher average global ED symptoms compared to youth without FI at baseline (Urban et al., n.d.). Further, when comparing treatment progress over the 20-week program, youth with FI experienced non-linear trajectories in symptom improvement (i.e., symptoms decreasing until eight weeks, increasing at 12 weeks, and decreasing through 20 weeks), whereas youth without FI experienced linear decreases in ED symptoms across the treatment program (Urban et al., n.d.). Though the statistical significance of these findings were not reported, the results represent preliminary evidence that FI status may be associated with variability in treatment response for youth with diagnosed EDs (Urban et al., n.d.).
Two population-based studies focused on Project EAT-I and II, where participants were surveyed in 1998–1999 and 2003–2004 (Hazzard et al., 2022; West et al., 2019)2. West et al. (2019) stratified the sample by low and high socioeconomic status (SES; primarily based on parent education ≥college (high) or not (low)), examining whether risk factors for disordered eating differed between groups (N=2,179; age range not reported, Mage=14.9, SD=1.6). Among participants in the low SES group, FI (9.3% of participants) significantly predicted higher risk of binge eating across time. However, risk of binge eating could not be calculated for the high SES group due to the lower prevalence of FI (3.4% of participants; West et al., 2019). Hazzard and colleagues (2022) focused on understanding both cross-sectional and longitudinal relationships between severe FI (i.e., any economically-driven past-year hunger) and disordered eating in 1,813 youth (EAT-I: 11–18yo, Mage=14.9, SD=1.6; EAT-II: 16–23yo, Mage=19.5, SD=1.6). Severe FI was associated with UWCBs (i.e., fasting, skipping meals, eating very little food, using food substitutes, and smoking more cigarettes), extreme weight control behaviors (i.e., self-induced vomiting, diet pill use, laxative use, and diuretic use), chronic dieting, overeating, and binge eating cross-sectionally at both time points. Among the disordered eating behaviors analyzed, the associations between severe FI and extreme weight control behaviors and severe FI and binge eating were the strongest. Severe FI at baseline was associated with a 41% increase in binge eating five years later but was not significantly associated with other assessed behaviors. Importantly, the relationship between severe FI and UWCBs was significant only until participants were 20yo, suggesting this association may be particularly relevant for children and adolescents (Hazzard et al., 2022).
As a follow-up to cross-sectional analysis using EAT 2010 and F-EAT data (Hooper et al., 2020), Hooper et al. (2022) conducted a longitudinal analysis examining the prospective relationship between FI status at baseline and UWCBs and binge eating after eight years. In unadjusted models, baseline FI was associated with elevated use of UWCBs and binge eating after eight years. However, when race/ethnicity and parental education were adjusted for, neither of these relationships remained significant. These results are contrary to previous cross-sectional findings that FI was associated with UWCBs (i.e., fasting and laxative use; Hooper et al., 2020) and longitudinal findings suggesting significant relationships between FI, binge eating, and UWCBs utilizing other EAT samples (Hazzard et al., 2022; West et al., 2019).
3.2.3. Qualitative Studies
Tester and colleagues (2016) utilized focus group interviews with caregivers of children (2–18yo, Mage=11.8, SD not reported) recruited from a pediatric weight management clinic. Caregivers were divided into food secure and food insecure focus groups to understand challenges in weight management for children with obesity by food security status. Within both groups, caregivers reported children often engaging in overeating behaviors. However, most participants who experienced FI said their children also engaged in binge eating, which was not mentioned in the food secure groups. Additionally, caregivers with FI mentioned children’s secretive eating and night-time eating were common (Tester et al., 2016). Thus, disordered eating behaviors, like secretive, night-time, and binge eating, emerged as particularly salient issues among food insecure children in a weight management setting.
Blum and colleagues (2019) conducted focus groups and individual interviews in Bangladesh with teenage girls (5–19yo, Mage school-attending=15.8, Mage non-school-attending=16.1, Mage married, non-school-attending=17.5, SDs not reported); key informant interviews with community leaders, teachers, and community health workers; and group discussions with parents and adolescent boys (15–19yo). The authors aimed to determine factors affecting eating behaviors of girls from low-income families, particularly in the context of cultural and gender norms. In Bangladeshi culture, during times of lower food availability, girls are generally expected to eat less food than boys and may be required to sacrifice meals so that boys can have enough to eat (Blum et al., 2019). Girls identified feeling positively about sacrificing their meals to boys/men within their family; however, as a result of eating less, Bangladeshi girls were susceptible to malnourishment as they received inadequate food compared to their male counterparts. Those who were at increased risk for restricting food intake were newly married adolescent girls, as they wanted to meet the family’s expectations during financial hardship. Other factors, such as long breaks between meals for school-going girls, also played a role in reduced dietary intake in Bangladeshi girls. The authors reported scant information from boys, but noted that boys reported being angry when they perceived food was insufficient from parents (Blum et al., 2019).
4. Discussion
The goal of this systematic review was to gather, synthesize, and evaluate research on the association between FI and disordered eating in children and adolescents. Across studies, FI is generally related to greater endorsement of disordered eating behaviors, consistent with the adult literature (e.g., Hazzard et al., 2020). However, the associations are nuanced, at times differing by disordered eating outcome and FI severity, among other factors.
4.1. Binge-Eating Type Behaviors
Studies examining binge eating and loss-of-control eating generally found that children within food insecure households were more likely to engage in these disordered eating behaviors (Kim et al., 2021; Kral et al., 2017; Linsenmeyer et al., 2021; West et al., 2021), though there were some nuanced and mixed results. For example, for binge eating and FI, some found no significant relationship (Hooper et al., 2022; Hooper et al., 2020), a significant relationship (Hazzard et al., 2022; Linsenmeyer et al., 2021; West et al., 2021), and a significant relationship only for those who endorsed at least one binge-eating episode (Kim et al., 2021). Though studies sometimes differed in terms of the population and sample size, two from similar cohorts (i.e., Project EAT-related) still evidenced mixed results, possibly due to how FI was operationalized. Two studies (Hooper et al., 2022; Hooper et al., 2020) utilized a lower-severity cut-off from a 6-item measure, whereas Hazzard and colleagues (2022) utilized one item to assess severe FI. Further, it is well-documented that loss-of-control eating is more prevalent than full-threshold binge eating in youth (Tanofsky-Kraff et al., 2020) and assessing binge eating in youth is difficult (Goldschmidt et al., 2008). This may explain why the relationship between FI and binge eating is less clear than the relationship between FI and loss-of-control eating in youth. Altogether, cross-sectional studies were more likely to find a positive association between binge eating and FI, though FI severity and endorsement of any binge eating may be important factors to consider. Importantly, longitudinal studies indicated FI was predictive of binge eating over time, with one notable exception (Hooper et al., 2022). This seeming paradox – that FI predicts binge eating – may be explained by the feast-or-famine cycle (Dinour et al., 2007), which proposes that binge eating occurs in response to restriction secondary to periods of food scarcity. Still, though the adult literature has started parsing out dietary restriction for any reasons (e.g., due to food scarcity) versus shape/weight reasons (e.g., Becker et al., 2019), such distinctions are just starting to be investigated in youth (e.g., Stadterman et al., 2022). More research on the mechanisms by which FI confers risk for binge-eating type behaviors is needed. Additionally, determining if there is added risk for certain sub-populations (e.g., those with greater severity of FI, those who endorse at least one binge-eating episode, racial/ethnic and sexual minorities, etc.) in other samples is warranted.
4.2. Unhealthy Weight-Control Behaviors and Dietary Restraint
Data on UWCBs as a group were consistently and positively associated with FI cross-sectionally (Hazzard et al., 2022; Hooper et al., 2022; Hooper et al., 2020; Masler et al., 2021; Stadterman et al., 2021). Importantly, however, some of the associations with UWCBs diminished when sociodemographic factors like parent education, race/ethnicity, age, and sex were accounted for (Hooper et al., 2022; Hooper et al., 2020). It would be helpful to better understand if such sociodemographic factors independently or interactively moderate the FI/UWCB association. One study identified that the relationship between caregiver- and child-reported FI and specific UWCBs (i.e., dieting behavior) may differ by gender (Barry et al., 2022).. Research suggests that UWCBs differ by gender, with girls more likely to endorse such behaviors (Stephen et al., 2014). However, Barry and colleagues (2022) found that boys expressed more dieting in relation to higher child-reported FI. The authors provide a plausible explanation that parents from food insecure households are more likely to engage in controlling food parenting practices (e.g., restricting food; Barry et al., 2022), which is related to dieting behavior for boys, but not for girls (Bauer et al., 2015; Loth et al., 2014). Additional research is still needed to examine this. Yet, severe FI did not predict UWCBs over time (Hazzard et al., 2022). As those with severe FI seem to be more at risk for disordered eating compared to their counterparts, it is unlikely that those with less severe FI would show this prospective association. Still, as only one study investigated FI and UWCBs longitudinally, and data from this research is currently two decades old, additional research in other samples and more recent cohorts is warranted.
4.3. Food Refusal and Food Responsiveness
Only one study examined the relationship between FI and food refusal (“picky eating”). Food refusal was greater for youth with food security when parents were stressed or depressed, but overall, food refusal was greater for youth with FI regardless of parent mood (Berge et al., 2020). This might seem paradoxical, as one might expect youth with FI to be more willing to eat food considering its scarcity. However, there may be less variety in food insecure households and less ability to purchase preferred items, potentially leading to more food refusal if children are disinterested in the options available. This might also be why parents report that children in food insecure households are more likely to desire eating palatable foods when exposed to it compared to children from food secure households (McCurdy et al., 2022). More research is needed to determine if these hypotheses are correct, but it would fit with the explanation that parents with FI perceive their children to be pickier eaters (Berge et al., 2020). Still, only one item was used to assess food refusal (Berge et al., 2020). Therefore, more nuanced and validated measures are needed to elucidate the nature of the relationship, as well as research in older children and adolescents.
4.4. Eating in Response to Negative Affect and in the Absence of Hunger
Consistently, eating in response to negative affect, emotions, or boredom was not associated with FI (Kral et al., 2017; McCurdy et al., 2022; Ruzicka, 2020). It is possible that children within food insecure households have alternative, non-food related methods of coping with negative emotions typically associated with FI (e.g., sadness, frustration, worry, anger). Indeed, children experiencing FI report using distraction (e.g., listening to music) or imagination (e.g., imagining eating a desired food) as coping mechanisms for FI-related distress (Leung et al., 2020). Given that food may not be readily accessible during moments of negative affect, emotions, or boredom for youth with FI, they may be more apt to using these alternative methods of coping to alleviate psychological distress.
Eating in the absence of hunger was positively associated with FI in the two studies that assessed it. Participants from one study were in a weight management trial and primarily from low income backgrounds (Harshman et al., 2022). Participants from the other study were community-based, from a wider income range, and of varied weight statuses (Kral et al., 2017). Notably, within the latter study, the association between FI and eating in the absence of hunger became non-significant when household income and maternal race were accounted for. Therefore, it is unclear if participant characteristics, study type, and/or sociodemographic factors may be driving the association or lack thereof. Further research that comprehensively evaluates these factors is needed. One question this also raises is how does the scarcity from FI interact with nutrition related goals of weight management interventions? Based on scarcity principles (e.g., Mullainathan & Shafir, 2013), regardless of whether one needs an item or not, if it is perceived to be in short supply/unavailable, individuals tend to acquire the item when it is available. This may be one reason why eating in the absence of hunger exists in food insecure populations and may be particularly salient for food insecure individuals in weight management programs who may experience nutrition recommendation components differently than peers who have not experienced FI. This is an important area for future research, particularly given the differential reporting of secretive, night-time, and binge eating among food insecure (vs. food secure) children in a weight management setting (Tester et al., 2016). FI status is important to consider for youth and families in weight management programs, and attention is needed to ensure that interventions are sensitive to the unique needs of individuals with a history of FI, such as how periods of food scarcity and availability may conflict with nutrition recommendations received in weight management programs.
4.5. Additional Factors to Consider in the Association Between FI and Disordered Eating
4.5.1. Socioeconomic Status
For some studies, SES (and its related proxies such as parental education and income) parsed some of the variance between FI and disordered eating behaviors. One may wonder if FI and SES assess the same underlying construct. Though FI is more common is lower SES households (Loopstra et al., 2019), FI exists in higher SES households for a variety of reasons (Karvay et al., 2022). Therefore, FI and SES are strongly related, but distinct, constructs. As such, FI may confer unique risk for disordered eating behaviors above and beyond the contribution of SES (Hazzard et al., 2020). Though one study attempted to examine the associations between FI and binge eating by SES (West et al., 2019), the food insecure sample size was insufficient for the higher SES group. In future studies, researchers may consider combining datasets to obtain the requisite number of participants with FI in higher SES groups.
4.5.2. Development
Only one study examined the relationship between FI and disordered eating behaviors by age, finding the association between FI and UWCBs significant for adolescents but not adult-aged participants (Hazzard et al., 2022). As the authors suggested, this could be because adolescents may have less control over food purchasing choices than young adults. Additionally, parents from food insecure households are more likely to engage in restrictive and pressured food parenting practices (Bauer et al., 2015), which are associated with increased levels of disordered eating behaviors among youth (Loth et al., 2014). Though younger children are often shielded from the effects of FI by their parents (Coleman-Jensen et al., 2021), no studies analyzed the relationship between FI and disordered eating behaviors longitudinally between childhood and adolescence. Examining if/how the relationship between FI and disordered eating behaviors changes throughout childhood and adolescence would shed light on proper timing of ED prevention and intervention targets. Studies are needed to close this knowledge gap.
4.5.3. ED Treatment Outcomes
Preliminary evidence shows that FI status is associated with ED treatment outcomes in youth, with food insecure youth experiencing variable levels of symptom improvement relative to food secure youth over a 20-week FBT program (Urban et al., n.d.). The non-linear trajectory of symptom improvement in food insecure youth indicates that they may have greater difficulty obtaining similar benefits from an empirically supported treatment like FBT relative to food secure peers. Possibly, families with FI may have greater difficulty assisting their children with meeting nutrition-related goals that are associated with FBT treatment for EDs due to economic barriers and variability in food access. However, results from this study should be interpreted with caution, as only 2.3% of participants in this study endorsed FI, and the authors did not report inferential statistics. The small proportion of participants who endorsed FI in this treatment study is illustrative of the underrepresentation of youth with FI in ED treatment programs. As this is an emerging area of study, further understanding of barriers to accessing ED treatment in food insecure youth and how FI affects ED treatment outcomes in youth is vital.
4.5.4. Parent-Child Agreement of Food Security Status
Two studies examined whether parent-child agreement of food security status was differentially related to disordered eating (i.e., general eating pathology, UWCBs, and binge eating) in children and adolescents (Barry et al., 2022; Wickel, 2014). Wickel (2014) found that some – but not all – discordant conditions (e.g., conditions in which adolescents and parent(s) did not agree on whether their household was food secure) were differentially associated with lower endorsement of UWCBs and higher endorsement of binge eating compared to the concordant condition where adolescents and both parents agreed that their household was food secure (Wickel, 2014). It is possible that a third variable (e.g., parental warmth or closeness; Berge et al., 2014) may be predictive of both discordancy among adolescents and parents and adolescent disordered eating symptoms. Additionally, when adolescents and parents agree about their FI status, this may signal more severe FI, which could explain why adolescents in the concordant condition expressed greater UWCBs compared to those in the discordant condition. Further, adolescent endorsement of disordered eating behaviors was dichotomized, which limits the ability to determine how parent-child agreement of food security status is related to severity of UWCBs or binge eating.
Barry and colleagues (2022) did not measure concordance between parent and child-reported FI status but found that child-reported rather than caregiver-reported FI was associated with greater disordered eating symptoms in children. It is possible that child-reported FI may be a better indicator of child disordered eating symptoms rather than caregiver-reported FI. Extant literature exploring concordance between adolescent and parent reports of FI indicate that youth and their parents have discordant perceptions of FI status (Frank & Sato, 2022). Reasons for this discordance and why disagreement in FI status may be related to disordered eating in children and adolescence are important questions to explore in further analyses.
4.5.5. Geography and Socially Constructed Factors
Despite FI being a worldwide phenomenon, and searches for the current review conducted in both English and Spanish, only one included study was conducted outside of the US. The Bangladeshi study (Blum et al., 2019) provided a great example of cultural and gender-based influences on the association between FI and dietary restraint. How cultural norms may affect the relationship between FI and disordered eating behaviors in other cultural groups and countries is still unknown and is a fruitful area for review. In addition, given structural factors that lead several marginalized populations (e.g., racial/ethnic minorities, sexual and gender minorities) to experience more FI than their peers, additional studies examining these socially constructed factors in the context of FI and disordered eating behaviors are necessary to identify individuals who may be at heightened vulnerability to EDs in response to FI.
4.6. Strengths and Limitations
This study fills a needed gap in the literature by synthesizing the burgeoning literature on FI and disordered eating behaviors in children and adolescents. The two first authors conducted literature searches in both English and Spanish across English- and Spanish-language research platforms, increasing the possibility of obtaining studies conducted in cross-cultural contexts. Further, this review included both quantitative and qualitative study designs. The rigorous methodology of this study, which only included articles that measured disordered eating behaviors rather than studies focused on general eating or parental feeding behaviors (e.g., parental monitoring of child food intake), made the information gathered more valid when applied to psychiatric diagnoses based on the DSM-5. Nonetheless, this limited the number of studies included and highlights the need for more studies measuring outcomes related to FI and EDs in youth. Further, given the focus on cognitive and behavioral indicators of disordered eating, this review excluded biological markers typically associated with disordered eating (e.g., bone mineral density, serum liver enzyme levels; Montagnese et al., 2007; Schvey et al., 2009) as potential outcomes of interest, and this is an area for future research.
5. Conclusion
This is the first systematic review examining the relationship between FI and disordered eating behaviors in youth. Findings show that FI is associated with a variety of disordered eating behaviors in children and adolescents. Most studies were from the US and cross-sectional in design. More global representation is needed, and more longitudinal studies would provide important information about how the relationship between FI and disordered eating changes over time. Additionally, whether associations between FI and disordered eating varies by FI severity remains understudied. Thus, research capturing how FI severity - ideally, using continuous measures of FI rather than one-item or dichotomous measures of FI - is related to disordered eating is necessary in future research. Future work should examine sociodemographic and cultural variables to provide greater context to our understanding of FI and disordered eating behaviors. As all the included studies except one were from the past six years, this is fortunately a fast-growing research area. Still, most of the included studies were secondary data analyses, and hypothesis-driven, primary analyses are needed.
Funding Statement:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflicts of interest: The authors have no conflicts to declare.
Though the literature on picky eating is mixed regarding whether picky eating is classified as a disordered eating behavior (save for severe picky eating associated with a diagnosis of avoidant restrictive food intake disorder), with some authors concluding that picky eating is not associated with disordered eating (Jacobi et al., 2008) and others indicating that picky eating is associated with greater reported disordered eating symptoms (He et al., 2020) picky eating was included as an outcome of interest in this review. Youth from socially disadvantaged backgrounds (i.e., youth of low income and of racial/ethnic minority backgrounds), who are more likely to experience FI, engage in picky eating beyond the developmentally normative preschool ages (Cardona Cano et al., 2015). Thus, picky eating was considered a relevant outcome.
EAT-I and II were included in this review as they had individuals ≤18yo; EAT-III data were excluded. EAT-II included individuals 19–23yo, so caution is warranted when interpreting these results.
References
- Abdurahman AA, Chaka EE, Nedjat S, Dorosty AR, & Majdzadeh R (2019). The association of household food insecurity with the risk of type 2 diabetes mellitus in adults: a systematic review and meta-analysis. European Journal of Nutrition, 58(4), 1341–1350. 10.1007/s00394-018-1705-2 [DOI] [PubMed] [Google Scholar]
- Agriculture U. D. o. (2022, October 17, 2022). Definitions of Food Security. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/definitions-of-food-security/
- Arenas DJ, Thomas A, Wang J, & DeLisser HM (2019). A systematic review and meta-analysis of depression, anxiety, and sleep disorders in US adults with food insecurity. Journal of General Internal Medicine, 34(12), 2874–2882. 10.1007/s11606-019-05202-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry MR, Sonneville KR, McGowan AR, Needham BL, Kobayashi LC, & Leung CW (2022). Caregiver-reported household food insecurity and child-reported food insecurity in relation to eating disorder risk factors and symptoms among preadolescent children. International Journal of Eating Disorders, 55(10), 1331–1341. 10.1002/eat.23784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer KW, MacLehose R, Loth KA, Fisher JO, Larson NI, & Neumark-Sztainer D (2015). Eating- and weight-related parenting of adolescents in the context of food insecurity. J Acad Nutr Diet, 115(9), 1408–1416. 10.1016/j.jand.2015.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker CB, Middlemass KM, Gomez F, & Martinez-Abrego A (2019). Eating disorder pathology among individuals living with food insecurity: A replication study. Clinical Psychological Science, 7(5), 1144–1158. 10.1177/2167702619851811 [DOI] [Google Scholar]
- Berge JM, Fertig AR, Trofholz A, Neumark-Sztainer D, Rogers E, & Loth K (2020). Associations between parental stress, parent feeding practices, and child eating behaviors within the context of food insecurity. Preventive Medicine Reports, 19. 10.1016/j.pmedr.2020.101146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Wall M, Larson N, Eisenberg ME, Loth KA, & Neumark-Sztainer D (2014). The unique and additive associations of family functioning and parenting practices with disordered eating behaviors in diverse adolescents. Journal of Behavioral Medicine, 37(2), 205–217. 10.1007/s10865-012-9478-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum LS, Khan R, Sultana M, Soltana N, Siddiqua Y, Khondker R, Sultana S, & Tumilowicz A (2019). Using a gender lens to understand eating behaviours of adolescent females living in low-income households in Bangladesh. Maternal and Child Nutrition, 15. 10.1111/mcn.12841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke MP, Martini LH, Çayır E, Hartline-Grafton HL, & Meade RL (2016). Severity of household food insecurity is positively associated with mental disorders among children and adolescents in the United States. The Journal of Nutrition, 146(10), 2019–2026. 10.3945/jn.116.232298 [DOI] [PubMed] [Google Scholar]
- Cardona Cano S, Tiemeier H, Van Hoeken D, Tharner A, Jaddoe VWV, Hofman A, Verhulst FC, & Hoek HW (2015). Trajectories of picky eating during childhood: A general population study. International Journal of Eating Disorders, 48(6), 570–579. 10.1002/eat.22384 [DOI] [PubMed] [Google Scholar]
- Carlson SJ, Andrews MS, & Bickel GW (1999). Measuring food insecurity and hunger in the United States: development of a national benchmark measure and prevalence estimates. The Journal of Nutrition, 129(2S Suppl), 510s–516s. 10.1093/jn/129.2.510S [DOI] [PubMed] [Google Scholar]
- Coleman-Jensen A, Rabbitt MP, Gregory CA, & Singh A (2021). Household food security in the United States in 2021. U. D. o. Agriculture. [Google Scholar]
- Dinour LM, Bergen D, & Yeh M-C (2007). The food insecurity & obesity paradox: A review of the literature and the role food stamps may play. Journal of the American Dietetic Association, 107(11), 1952–1961. 10.1016/j.jada.2007.08.006 [DOI] [PubMed] [Google Scholar]
- Fram MS, Frongillo EA, Draper CL, & Fishbein EM (2013). Development and validation of a child report assessment of child food insecurity and comparison to parent report assessment. Journal of Hunger & Environmental Nutrition, 8(2), 128–145. 10.1080/19320248.2013.790775 [DOI] [Google Scholar]
- Frank ML, & Sato AF (2022). A multi-informant assessment of food security in adolescents: Discordance in self-report and parent-proxy report. Journal of Hunger and Environmental Nutrition. 10.1080/19320248.2022.2117002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky-Kraff M, & Wilfley DE (2008). Disordered eating attitudes and behaviors in overweight youth. Obesity, 16(2), 257–264. 10.1038/oby.2007.48 [DOI] [PubMed] [Google Scholar]
- Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, Cook JT, de Cuba SAE, Casey PH, Chilton M, Cutts DB, Meyers AF, & Frank DA (2010). Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics, 126(1), e26–e32. 10.1542/peds.2009-3146 [DOI] [PubMed] [Google Scholar]
- Harshman SG, Castro I, Perkins M, Luo M, Mueller KB, Cena H, Portale S, Raspini B, Taveras E, & Fiechtner L (2022). Pediatric weight management interventions improve prevalence of overeating behaviors. International Journal of Obesity, 46, 630–636. 10.1038/s41366-021-00989-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazzard VM, Hooper L, Larson N, Loth KA, Wall MM, & Neumark-Sztainer D (2022). Associations between severe food insecurity and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Preventive Medicine, 154. 10.1016/j.ypmed.2021.106895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazzard VM, Loth KA, Hooper L, & Becker CB (2020). Food insecurity and eating disorders: A review of emerging evidence. Current Psychiatry Reports, 22(12), 74. 10.1007/s11920-020-01200-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Zickgraf HF, Essayli JH, & Fan X (2020). Classifying and characterizing Chinese young adults reporting picky eating: A latent profile analysis. International Journal of Eating Disorders, 53(6), 883–893. 10.1002/eat.23231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper L, Mason SM, Telke S, Larson N, & Neumark-Sztainer D (2022). Experiencing household food insecurity during adolescence predicts disordered eating and elevated body mass index 8 years later. Journal of Adolescent Health, 70(5), 788–795. 10.1016/j.jadohealth.2021.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper L, Telke S, Larson NI, Mason SM, & Neumark-Sztainer D (2020). Household food insecurity: Associations with disordered eating behaviours and overweight in a population-based sample of adolescents. Public Health Nutrition, 23, 3126–3135. 10.1017/S1368980020000464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey replication. Biological Psychiatry, 61(3), 348–358. 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Schmitz G, & Agras WS (2008). Is picky eating an eating disorder? International Journal of Eating Disorders, 41(7), 626–634. 10.1002/eat.20545 [DOI] [PubMed] [Google Scholar]
- Jones AD (2017). Food insecurity and mental health status: A global analysis of 149 countries. American Journal of Preventive Medicine, 53, 264–273. 10.1016/j.amepre.2017.04.008 [DOI] [PubMed] [Google Scholar]
- Karvay YG, Guarecuco JS, Feuerstahler L, & Burke NL (2022). Development and validation of the food availability and related eating behaviors questionnaire: A stage 1 registered report. International Journal of Eating Disorders, 55(10), 1404–1410. 10.1002/eat.23797 [DOI] [PubMed] [Google Scholar]
- Kim BH, Ranzenhofer L, Stadterman J, Karvay YG, & Burke NL (2021). Food insecurity and eating pathology in adolescents. International Journal of Environmental Research and Public Health, 18. 10.3390/ijerph18179155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral TVE, Chittams J, & Moore RH (2017). Relationship between food insecurity, child weight status, and parent-reported child eating and snacking behaviors. Journal for Specialists in Pediatric Nursing, 22. 10.1111/jspn.12177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung CW, Stewart AL, Portela-Parra ET, Adler NE, Laraia BA, & Epel ES (2020). Understanding the psychological distress of food insecurity: A qualitative study of children’s experiences and related coping strategies. Journal of the Academy of Nutrition and Dietetics, 120(3), 395–403. 10.1016/j.jand.2019.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linsenmeyer WR, Katz IM, Reed JL, Giedinghagen AM, Lewis CB, & Garwood SK (2021). Disordered eating, food insecurity, and weight status among transgender and gender nonbinary youth and young adults: A cross-sectional study using a nutrition screening protocol. LGBT Health, 8, 359–366. 10.1089/lgbt.2020.0308 [DOI] [PubMed] [Google Scholar]
- Loopstra R, Reeves A, & Tarasuk V (2019). The rise of hunger among low-income households: an analysis of the risks of food insecurity between 2004 and 2016 in a population-based study of UK adults. Journal of Epidemiology and Community Health, 73(7), 668–673. 10.1136/jech-2018-211194 [DOI] [PubMed] [Google Scholar]
- Loth KA, MacLehose RF, Fulkerson JA, Crow S, & Neumark-Sztainer D (2014). Are food restriction and pressure-to-eat parenting practices associated with adolescent disordered eating behaviors? International Journal of Eating Disorders, 47(3), 310–314. 10.1002/eat.22189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney MJ, McGuire JB, & Daniels SR (1988). Reliability testing of a children’s version of the Eating Attitude Test. Journal of the American Academy of Child and Adolescent Psychiatry, 27(5), 541–543. 10.1097/00004583-198809000-00004 [DOI] [PubMed] [Google Scholar]
- Masler IV, Palakshappa D, Skinner AC, Skelton JA, & Brown CL (2021). Food insecurity is associated with increased weight loss attempts in children and adolescents. Pediatric Obesity, 16. 10.1111/ijpo.12691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurdy K, Gans KM, Risica PM, Fox K, & Tovar A (2022). Food insecurity, food parenting practices, and child eating behaviors among low-income Hispanic families of young children. Appetite, 169. 10.1016/j.appet.2021.105857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan A, Barry MR, Sonneville KR, & Leung CW (2022). Greater social adversity associated with more disordered eating attitudes and behaviors among children from Southeast Michigan. The International journal of eating disorders. 10.1002/eat.23775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre L, Williams JVA, Lavorato DH, & Patten S (2013). Depression and suicide ideation in late adolescence and early adulthood are an outcome of child hunger. Journal of Affective Disorders, 150(1), 123–129. 10.1016/j.jad.2012.11.029 [DOI] [PubMed] [Google Scholar]
- Mitchell JE, & Crow S (2006). Medical complications of anorexia nervosa and bulimia nervosa. Current Opinion in Psychiatry, 19(4), 438–443. 10.1097/01.yco.0000228768.79097.3e [DOI] [PubMed] [Google Scholar]
- Montagnese C, Scalfi L, Signorini A, De Filippo E, Pasanisi F, & Contaldo F (2007). Cholinesterase and other serum liver enzymes in underweight outpatients with eating disorders. International Journal of Eating Disorders, 40(8), 746–750. 10.1002/eat.20432 [DOI] [PubMed] [Google Scholar]
- Mullainathan S, & Shafir E (2013). Scarcity: Why having too little means so much. Macmillan. [Google Scholar]
- Rohde P, Stice E, & Marti CN (2015). Development and predictive effects of eating disorder risk factors during adolescence: Implications for prevention efforts. International Journal of Eating Disorders, 48(2), 187–198. 10.1002/eat.22270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruzicka EB (2020). Parent and adolescent perception of child feeding practices and adolescent weight and obesogenic eating in families from a low-income household (Publication Number 28121630) [Ph.D., Kent State University]. ProQuest Dissertations & Theses Global. United States — Ohio. [Google Scholar]
- Schvey NA, Tanofsky-Kraff M, Yanoff LB, Checchi JM, Shomaker LB, Brady S, Savastano DM, Ranzenhofer LM, Yanovski SZ, Reynolds JC, & Yanovski JA (2009). Disordered-eating attitudes in relation to bone mineral density and markers of bone turnover in overweight adolescents. Journal of Adolescent Health, 45(1), 33–39. 10.1016/j.jadohealth.2008.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar P, Chung R, & Frank DA (2017). Association of food insecurity with children’s behavioral, emotional, and academic outcomes: A systematic review. Journal of Developmental & Behavioral Pediatrics, 38(2), 135–150. 10.1097/DBP.0000000000000383 [DOI] [PubMed] [Google Scholar]
- Smith AR, Velkoff EA, Ribeiro JD, & Franklin J (2019). Are eating disorders and related symptoms risk factors for suicidal thoughts and behaviors? A meta-analysis. Suicide and Life-Threatening Behavior, 49(1), 221–239. 10.1111/sltb.12427 [DOI] [PubMed] [Google Scholar]
- Stadterman J, Karvay YG, & Burke NL (2021). Preliminary comparison of eating pathology and weight status in youth with and without food insecurity [Poster session]. Annual Meeting of The Obesity Society at ObesityWeek, Virtual. [Google Scholar]
- Stadterman J, Karvay YG, Feuerstahler L, & Burke NL (2022). Comparison of ad libitum snack consumption and acquisition between adolescents living with food security and food insecurity: A stage 1 registered report. International Journal of Eating Disorders, 55(3), 406–414. 10.1002/eat.23693 [DOI] [PubMed] [Google Scholar]
- Stephen EM, Rose JS, Kenney L, Rosselli-Navarra F, & Weissman RS (2014). Prevalence and correlates of unhealthy weight control behaviors: Findings from the national longitudinal study of adolescent health. Journal of Eating Disorders, 2(1), 16. 10.1186/2050-2974-2-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Schvey NA, & Grilo CM (2020). A developmental framework of binge-eating disorder based on pediatric loss of control eating. American Psychologist, 75, 189–203. 10.1037/amp0000592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tester JM, Lang TC, & Laraia BA (2016). Disordered eating behaviours and food insecurity: A qualitative study about children with obesity in low-income households. Obesity Research and Clinical Practice, 10, 544–552. 10.1016/j.orcp.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urban B, Jones N, Freestone D, Steinberg D, & Baker JH (n.d.). Food insecurity among youth seeking eating disorder treatment. Equip Heallth, Inc. [DOI] [PubMed] [Google Scholar]
- Weaver LJ, & Fasel CB (2018). A systematic review of the literature on the relationships between chronic diseases and food insecurity. Food and Nutrition Sciences, 9(5), 22, Article 84666. 10.4236/fns.2018.95040 [DOI] [Google Scholar]
- West CE, Darling KE, Ruzicka EB, & Sato AF (2021). Household income and loss of control eating in adolescence: Examining the role of food insecurity. Appetite, 165. 10.1016/j.appet.2021.105291 [DOI] [PubMed] [Google Scholar]
- West CE, Goldschmidt AB, Mason SM, & Neumark-Sztainer D (2019). Differences in risk factors for binge eating by socioeconomic status in a community-based sample of adolescents: Findings from Project EAT. International Journal of Eating Disorders, 52, 659–668. 10.1002/eat.23079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickel K (2014). Utilizing family systems theory to understand adolescent disordered eating behaviors: Exploring the implications of triadic family discord (Publication Number 3628043) [Ph.D., University of Minnesota]. ProQuest Dissertations & Theses Global. United States — Minnesota. [Google Scholar]


