Abstract
Objective:
Life stressors have been linked to cardiovascular risk; however, studies typically focus on stressors that directly impact the individual, i.e., personal stressors. Research suggests that women, particularly African-American women, may be more vulnerable to network stressors that involve family members and friends-- potentially due to norms around needing to be a “Superwoman.” Yet few studies have examined these phenomena.
Methods:
We examined associations between network, versus personal, stressors and elevated blood pressure (BP) in N=392 African-American women aged 30–46. Questionnaire-assessed negative life events were classified into upsetting network or personal stressors. BP was assessed in clinic and via 48-hour ambulatory monitoring. Linear and logistic regression models examined associations between type of stressors and 48-hour daytime and nighttime systolic BP (SBP) and diastolic BP (DBP), and sustained hypertension after adjusting for relevant covariates. Interactions with questionnaire-assessed superwoman schema (SWS) were tested in exploratory analyses
Results:
In age and sociodemographic-adjusted models, network stressors were significantly associated with daytime SBP (β (S.E.)= 2.01 (0.51), p=<0.0001)) and DBP (β (S.E.)= 1.59 (0.37), p=<0.0001), but personal stressors were not (p-values >.10). Associations persisted after adjustment for cardiovascular and psychosocial risk factors. Patterns were similar for nighttime BP and sustained hypertension. There were no interactions with SWS.
Conclusions:
Network, but not personal, stressors were associated with elevated rates of daytime SBP and DBP, as well as sustained hypertension in African-American women, irrespective of SWS endorsement. Future research is needed to determine whether stress-management interventions focused on network stressors might impact BP in this high-risk population.
Keywords: African-American, Blood pressure, Social Determinants of Health, stress, psychological, women
Abstracto:
Objetivo:
Los factores estresantes de la vida se han relacionado con el riesgo cardiovascular; sin embargo, los estudios generalmente se enfocan en los factores estresantes que impactan directamente al individuo, es decir, los factores estresantes personales. La investigación sugiere que las mujeres, en particular las mujeres afroamericanas, pueden ser más vulnerables a los factores estresantes de la red que involucran a familiares y amigos, posiblemente debido a las normas sobre la necesidad de ser una “supermujer”. Sin embargo, pocos estudios han examinado estos fenómenos.
Métodos:
Examinamos las asociaciones entre los factores estresantes de la red y personales, y la presión arterial (PA) elevada en N=392 mujeres afroamericanas de 30 a 46 años. Los eventos vitales negativos evaluados por el cues onario se clasificaron en perturbadores de la red o estresores personales. La PA se evaluó en la clínica y mediante monitorización ambulatoria de 48 horas. Los modelos de regresión lineal y logística examinaron las asociaciones entre el tipo de factores estresantes y la PA sistólica (PAS) y PA diastólica (PAD), diurna y nocturna de 48 horas, y la hipertensión sostenida después de ajustar las covariables relevantes. Las interacciones con el esquema de supermujer (SWS por sus siglas en inglés) evaluado por cuestionario se probaron en análisis exploratorios.
Resultados:
En modelos ajustados por edad y sociodemográficos, los estresores de la red se asociaron significativamente con la PAS diurna (b (Error Estándar) = 2,01 (0,51), p=<0,0001)) y la PAD durina (b (Error Estándar) = 1,59 (0,37), p=<0,0001), pero los estresores personales no (valores p > 0,10). Las asociaciones persistieron después del ajuste por factores de riesgo cardiovascular y psicosocial. Los patrones fueron similares para la PA nocturna y la hipertensión sostenida. No hubo interacciones con SWS.
Conclusiones:
Los factores estresantes de la red, pero no los personales, se asociaron con tasas elevadas de PAS y PAD diurnas, así como con hipertensión sostenida en mujeres afroamericanas, independientemente del respaldo de SWS. Se necesita investigación futura para determinar si las intervenciones de manejo del estrés centradas en los factores estresantes de la red podrían afectar la PA en esta población de alto riesgo.
Background
Rates of elevated blood pressure (BP) in African-Americans are among the highest in the world (Virani et al., 2021), and are a major contributor to the excess rates of heart disease, stroke, and kidney disease observed in this group (Carnethon et al., 2017). Among African-Americans, African-American women are disproportionately impacted, with steeper increases in blood pressure across the life course compared to African-American men (Ji et al., 2020). These differences in BP for African-American women versus men persist even after adjusting for traditional risk factors, such as smoking, body mass index (BMI), and diet (Ji et al., 2020). Thus, non-traditional factors might also play a role.
BP is known to be responsive to psychosocial stressors (Joseph et al., 2016; Spruill et al., 2016), and there is evidence that psychosocial stressors have a stronger impact on BP for women, compared to men (Landsbergis et al., 2013; Trudel et al., 2016). Yet most studies in this area have examined work-related stressors (Landsbergis et al., 2013; Trudel et al., 2016), despite the fact that for women (versus men), interpersonal stressors have been found to be more emotionally impactful than other forms of psychosocial stress (Davis et al., 1999; McLeod et al., 2016). Additionally, the majority of this research has focused on White women (Landsbergis et al., 2013; Trudel et al., 2016)—yet across studies, African-American women report more psychosocial stress than women from other racial/ethnic backgrounds (Burroughs Peña et al., 2019; Matthews et al., 2019). However, few studies have examined stressors that might be uniquely salient for women overall, and African-American women in particular.
One major form of psychosocial stress that has been found to be particularly relevant for women is network stress (Cohen et al., 2019; Helgeson, 2011; Turner & Avison, 1989). In their seminal work on gender differences in exposure to stressful life events, Kessler and McLeod (1984) defined network stressors as “life events that do not occur to the focal respondent, but to someone in his or her network who is considered important” (p. 620). Network stressors are a form of interpersonal stress as they involve relationships with others; however, in contrast to personal stressors, which primarily impact the individual, network stressors involve and/or impact an individual’s loved ones-- i.e. family members and/or friends. Several researchers have maintained that because women (from all racial/ethnic groups) are typically socialized to be more communal, and sensitive to occurances in their social networks than men (Helgeson, 2011), assessments of network stressors may be critically important in studies of psychosocial stress in women (Kessler & McLeod, 1984).
Network stressors may be an especially powerful source of psychosocial stress for African-American women (Woods-Giscombé et al., 2015). Stress theorists in the broader social sciences have argued that social context should be a key consideration in the conceptualization of stress exposure and stress processes for disadvantaged groups (Pearlin, 1989), and this may be particularly relevant for studies of network stressors among African-American women. Throughout history, African-American communities have been disproportionately targeted by both overt mistreatment as well as discriminatory policies (e.g. unequal policing, incarceration) (Alexander, 2020; Edwards et al., 2019) and practices (lower employment, wages) (Fryer et al., 2013) that diminish their life opportunities relative to individuals from other racial/ethnic groups. Because many of these practices have uniquely impacted African-American men (Alexander, 2020; Edwards et al., 2019), numerous scholars have argued that African-American women may have more family and community-level responsibilities than women from other racial/ethnic backgrounds (Haxton & Harknett, 2009; Sarkisian & Gerstel, 2004). For example, Settles and colleagues (2008) found that while both African-American and White women identified nurturing and caregiving as core components of their roles as women, African-American women also felt it important to “be the backbone” for the African-American community overall (p. 463). Thus, as members of a community exposed to disproportionately high rates of stress (Burroughs Peña et al., 2019), along with sociocultural norms around providing a high degree of caregiving and elevated support in the context of historical disadvantage (Settles et al., 2008; Woods-Giscombé et al., 2015), African-American women may be particularly vulnerable to network stressors.
To date, much of the extant literature on network stressors has focused on mental health outcomes. This research suggests that there is a “cost of caring” with respect to network stressors, whereby women may be more vulnerable to those negative life events that involve and/or impact close others, versus those that solely impact themselves. Studies have documented the deleterious impact of network, in comparison to non-network, stressors on depression and other mental health outcomes in White females (Kessler & McLeod, 1984; Shih et al., 2006; Turner & Avison, 1989), and linkages between network stressors and psychological distress have been observed among African-American women as well (Woods-Giscombé et al., 2015). Yet there has been limited work examining whether this “cost of caring” extends to physiological processes and/or objective clinical indicators of disease, although researchers have argued that accumulated exposure to network stressors might ultimately “take a physical toll” (p. 584) (Cichy et al., 2012).
To address these gaps in the literature, we examined associations between network stressors, personal stressors, and elevated BP assessed via 48-hour ambulatory BP (ABP) monitoring in a cohort of pre-menopausal African-American women. In contrast to clinic BP, ABP is believed to assess the “true” BP over the course of a given day and night (Schwartz et al., 2016; Whelton et al., 2018). Further, research suggests that ABP is a stronger predictor of outcomes than resting/clinic BP (Matsumoto et al., 2021), especially among women (Boggia et al., 2011). In keeping with the “cost of caring” framework, we hypothesized that network stressors would be more strongly associated with elevated BP among African-American women than personal stressors, even after adjusting for sociodemographics, risk factors, and depressive symptoms. Finally, because Woods-Giscombé and colleagues (2015) have posited that network stressors may be particularly problematic for African-American women because of sociocultural norms around being the aforementioned backbone of the community-- i.e., “superwomen,” who take care of everyone else-- in exploratory analyses we also examined whether our hypothesized network stress and BP associations were moderated by superwoman schema endorsement (Woods-Giscombe et al., 2019), and more specifically the felt obligation to take care of others.
Methods
Participants were from the Mechanisms Underlying Stress and Emotions (MUSE) in African-American Women’s Health Study (McKinnon et al., 2022; Spikes et al., 2022). Women were identified via consumer residential lists and voter registration records from a range of census tracts in the greater Atlanta, GA metropolitan area. An introductory brochure was sent via mail, followed by a telephone call for pre-screening. Eligibility criteria were: self-identification as a Black/African-American woman; aged 30–45 (at screening); premenopausal; not pregnant or lactating; having a uterus and ≥1 ovary. Ineligibility criteria were: history of clinical cardiovascular disease (CVD) (e.g., myocardial infarction, angina, intermittent claudication, cerebrovascular disease or coronary revascularization); chronic illness known to influence atherosclerotic disease (e.g., HIV, kidney disease); current treatment for psychiatric disorders; and current illicit drug use or alcohol abuse. Women who worked overnight shifts were also ineligible, due to the influence of shift work on circadian rhythms. The final cohort consisted of N=422 women. However, N=8 did not have ABP data, three due to arm circumferences larger than the largest available cuff size (XL), three due to equipment failures, and two refusals, resulting in N=414. Of these, N=17 were missing at least one item on the life events scale and N=5 were missing covariate data, for a final N=392. Two additional participants did not have nighttime ABP values and were excluded from those analyses.
Procedures.
Between 2016–2019, participants completed an in-person visit, where study staff collected height, weight, resting blood pressure, and additional clinical data. Following this, demographic and psychosocial characteristics were assessed via face-to-face interview and women were fit with the ABP monitor. All procedures were approved by the Emory University Institutional Review Board (IRB), and all participants provided written, informed consent.
Ambulatory Blood Pressure Outcomes
Prior to fitting, the ABP monitor (OnTrak model 90227, SpaceLabs; Issaquah, WA) was programmed to record systolic BP (SBP) and diastolic BP (DBP) every 30-minutes during the day (8am to 10pm) and every hour during the night, over a 48-hour period. We chose fixed time windows a priori in order to avoid recall bias in self-reported sleep times. This is particularly relevant for the current cohort, given research documenting greater night-to-night variability in sleep times for African-American men and women relative to other racial/ethnic groups (Huang & Redline, 2019; Knutson et al., 2007), which could increase the likelihood of inaccurate self-report. Participants were trained on proper application/removal techniques and instructed to remove the device only to shower/bathe. Upon completion, monitors were retrieved by study staff. Continuous outcomes were average 48-hour SBP and DBP, separated into daytime and nighttime values based on the timing of assessments. Daytime and nighttime BP were examined as separate outcomes because studies have found that nighttime BP is often predictive of clinical events independent of daytime BP (Hansen et al., 2011). Further, although prior studies have examined BP non-dipping (frequently defined as the percent difference between daytime and nighttime values) as a relevant outcome (Rodriguez et al., 2013), recent studies have found that measures of daytime and nighttime BP values have higher levels of reproducibility than measures of BP non-dipping (Abdalla et al., 2015; Muntner et al., 2019). Our clinically relevant outcome was sustained hypertension, defined as clinically elevated BP in both clinic and daily life, utilizing 2017 blood pressure thresholds of 130/80 mm/Hg (Whelton et al., 2018). This is in contrast to clinic BP alone, which includes some proportion of individuals who only display elevated clinic, but not daily, BP (i.e., “White coat” hypertension) (Muntner et al., 2019).
Personal and Network Stressors.
Network and personal stressors were assessed using a 22-item version of the Psychiatric Epidemiology Research Interview Life Events Scale (Dohrenwend et al., 1978), modified for midlife women to assess eight domains: school, work, romantic relationships, children, family, criminal and legal matters, finances, and health (Troxel et al., 2003). Fifteen events were classified as personal stressors (e.g., “Quit, fired, or laid off from a job?” “Major accident, assault, disaster, robbery or other violent event happened to yourself?” “Major money problems?” “Unwanted pregnancy?” “Stillbirth or miscarriage?” “A close relative (husband/partner, child or parent) died” “Were separated or divorced or a long-term relationship ended?” “Partner had an affair?” “You had an affair?” among others) and seven were classified as network stressors. In keeping with theoretical work on network stressors (Helgeson, 2011) particularly among African-American women (Woods-Giscombé et al., 2015), the 7-item network stress subscale included events that happened solely to others (e.g., “Major accident, assault, disaster, robbery or other violent event happened to a family member?” “Family member had legal problems or a problem with police?” “Serious physical illness, injury or drug/alcohol problem in family member, partner or close friend?” “Husband/partner became unemployed?”) as well as events that involved relationships with close others, specifically children and/or friends (e.g., “A child moved out of the house or left the area?” “Had a serious problem with child or family member (other than husband/partner) or with a close friend?,” “Took on responsibility for the care of another child, grandchild, parent, other family member or friend?”). For each event, participants rated whether it occurred during the past year and how upsetting it was from “not at all upsetting” to “very upsetting and still upsetting.” Events rated “very” to “very and still” upsetting were summed to create the upsetting personal and network stressors scales, respectively. This was done to be consistent with prior studies using this scale (Matthews et al., 2019; Troxel et al., 2003), and to create comparability between network and personal stressors. This avoids the possibility of comparing personal stressors that were experienced as very upsetting to network stressors that were perceived as non-upsetting, and vice versa. Both types of stressors were modeled continuously to preserve power, but were categorized into 0, 1, 2, or ≥ 3 for descriptive purposes, utilizing the distribution of the data. Finally, because some of the items in the network stress subscale involve others but have been conceptualized as personal stressors in other studies (e.g., caregiving) we ran sensitivity analyses to: 1) remove the caregiving item from the network stress subscale and include it in the personal stressors subscale and 2) restrict the network stressors subscale to those four events that only happened to others, and move the remaining three items to the personal stress subscale.
Superwoman Schema.
The Giscombé Superwoman Schema (SWS) scale was administered to assess endorsement of the felt need to be a “superwoman” (Woods-Giscombé et al. 2019). This 35-item scale includes five multi-item subscales: 1) obligation to present an image of strength ( “I try to present an image of strength”), 2) obligation to suppress emotions (“My tears are a sign of weakness”), 3) resistance to being vulnerable ( “I resist help to prove that I can make it on my own”), 4) intense motivation to succeed ( “I accomplish my goals with limited resources”), and 5) obligation to help others (“I put everyone else’s needs before my own,” “I take on too many responsibilities in my family,” “there is no time for me because I am always taking care of others”). Response categories ranged from 0 “not true for me” to 3 (“true for me all the time”). Items for the overall and each subscale were summed, with higher scores indicating greater endorsement. We examined the full SWS, but due to its relevance to the current analysis, focused on the obligation to help others subscale. The full SWS and the obligation to help others subscale had very good to excellent internal reliability (Cronbach’s alphas = .94 and .88, respectively) in the current cohort.
Covariates
Covariates were chosen based on prior research (Cundiff et al., 2015; Gavrilova & Zawadzki, 2021; Gilbert-Ouimet et al., 2017; Rodriguez et al., 2013; Turner & Avison, 1989). Age and Partners (married/living with partner versus not), were self-reported. Education was self-reported in years and as highest degree status and categorized into: high school or less, some college or occupational training, and college or higher. Family Income was self-reported into pre-defined ranges and collapsed into: <$35,000, $35,000-$49,999, $50,000-$74,999, ≥ $75,000/year, with a 5th category created to capture volunteered responses of “Refused/Don’t know.” Family Size was reported as number of individuals in the household. Body Mass Index (BMI) was calculated as weight/height (kg/m2) and modeled continuously. Current Smoking and Anti-hypertensive use were self-reported as yes/no. Depressive Symptoms were assessed with the 21-item Beck Depression Inventory (BDI) (Beck et al., 1961) and modeled continuously. Because of the cross-sectional nature of the study and the resulting difficulty in determining temporality (particularly for depressive symptoms, as there is considerable evidence that depressed individuals might appraise life events more negatively), we treated all covariates as confounders, rather than mediators.
Primary Statistical analyses
Descriptive statistics were utilized to detail characteristics of the cohort. Following this, linear regression analyses were conducted to assess associations between network/personal stressors modeled continuously and continuous ABP outcomes. Model 1 was age-adjusted. Model 2 added additional sociodemographics including marital/live-in partner status, education, family income and family size (as a further adjustment for family income). Model 3 added BMI and smoking as standard hypertension risk factors, and Model 4 added anti-hypertensive medication, as in prior ABP analyses (Gilbert-Ouimet et al., 2017; Spruill et al., 2016). Model 5 adjusted for depressive symptoms. Separate models were run for network and personal stressors, followed by a Model 6 with both stressors, to examine the independence of network stressors from personal stressors. This sequence of models (Models 1–6) was repeated with sustained hypertension as the outcome, utilizing logistic regression analyses. We also ran sensitivity analyses examining overall (i.e., not only upsetting) exposures to network and personal stressors and our outcomes. Effect sizes were slightly smaller, but findings were similar in both sets of analyses; thus, we retained our focus on upsetting stressors. Additional sensitivity analyses 1) excluding the caregiving item from the network stressors subscale and 2) limiting the network stress subscale to those four items that only impacted others were also conducted. These additional analyses resulted in almost identical interpretations as our initial categorizations (see Supplemental Table A for the most conservative, 4-item coding); consequently, we retained our original coding.
Exploratory Analyses
Following our primary models, we ran a series of exploratory analyses to examine whether overall SWS endorsement, or endorsement of an obligation to help others specifically, moderated the hypothesized associations between type of stressor and ABP outcomes. Utilizing the same sequence of initial analyses (Models 1–6), we added a main effect of SWS to each model, followed by the network stress X SWS interaction. Following this, we ran a second set of sequential Models 1–6 adding the main effect of obligation to help others, and a network stress X obligation to help others interaction term. All analyses were conducted in SAS V 9.4. with a 2-sided Type-I error rate of .05.
Results
Participant Characteristics.
Participant characteristics are presented in Table 1. Women were between 30–46 years of age. Approximately 38% were married/living with a partner. The cohort was socioeconomically diverse, with annual household incomes ranging from <$35,000 to > $75,000, and 48.2% reporting ≥ a college degree. On average, BMIs were in the obese range, and 9.9% of participants were current smokers. Average daytime BPs were in the normal range, with mean nighttime SBP and DBPs in the normal (Ravenell et al., 2017) to elevated range (Muntner et al., 2019), based on recent definitions (Whelton et al., 2018). Approximately 30.87% women had sustained hypertension, and 16.3% of participants reported anti-hypertensive use.
Table 1.
Demographic, Psychosocial and Risk Factor Characteristics
| Participant Characteristic | Range | |
|---|---|---|
| Age (years) | 37.83 (4.29) | 30 – 46 |
| Marital/Partnered Status | 148 (37.8%) | |
| Education | ||
| HS or Less | 121 (30.9%) | |
| Some College | 82 (20.9%) | |
| College or Higher | 189 (48.2%) | |
| Income | ||
| <35k | 90 (23.0%) | |
| 35k-50k | 83 (21.2%) | |
| 50k-75k | 90 (23.0%) | |
| >75k | 121 (30.9%) | |
| Upsetting Network Stressors | 1.01 (1.18) | 0–5 |
| 0 | 178 (45.4%) | |
| 1 | 103 (26.3%) | |
| 2 | 60 (15.3%) | |
| 3 or more | 51 (13.0%) | |
| Upsetting Personal Stressors | 2.27 (SD=1.78) | 1–9 |
| 0 | 72 (18.4%) | |
| 1 | 75 (19.1%) | |
| 2 | 86 (21.9%) | |
| 3 or more | 159 (40.6%) | |
| SWS-overall | 66.72 (17.62) | 16–100 |
| SWS-obligation to help others | 15.26 (6.12) | 0–27 |
| Body Mass Index (kg/m2) | 32.56 (8.02) | 17.16–57.43 |
| Current Smoking | 39 (9.9%) | |
| Daytime Systolic Blood Pressure | 121.35 (12.24) | 94.26–157.31 |
| Daytime Diastolic Blood Pressure | 77.54 (8.82) | 50.58–105.38 |
| Nighttime Systolic Blood Pressure | 111.23 (11.72) | 84.12–151.00 |
| Nighttime Diastolic Blood Pressure | 68.50 (8.58) | 49.90–105.36 |
| Anti-Hypertensive Use | 64 (16.3%) | |
| Depressive Symptoms (BDI score) | 5.82 (6.66) | 0 – 39 |
Note: Values are mean ± SD or percentage.
SWS=Superwoman Schema
On average, women reported 1.01 (SD=1.18) upsetting network stressor(s) in the previous 12 months. Forty-five percent of women reported no upsetting network stressors over this period, 26.3% reported one, 15.3% reported two, and 13.0% reported ≥ three. Reports of upsetting personal stressors were more common, with women reporting on average, 2.27 (SD=1.78) upsetting personal stressors in the prior year. Only 18.4% of women reported no upsetting personal stressors during the previous 12 months, whereas 19.1% reported one, 21.9% reported two, and 40.6% reported ≥ three. With respect to SWS, mean overall scores were in the “moderate” range at 66.72 (SD=17.62) and average scores on the SWS obligation to help others subscale were consistent with prior research (Woods-Giscombe et al., 2019).
Associations among Network Stressors, ABP Outcomes, and Other Variables of Interest
Bivariate correlations (Spearman for continuous, Pearson for categorical) among type of stressor, SWS variables, covariates and ABP outcomes are presented in Supplemental Table B.
Type of Stressor and Continuous ABP outcomes
In age-adjusted linear regression models (Table 2; Model 1), upsetting network stressors were positively associated with daytime SBP (β(S.E.) = 2.13 (0.51), p<.0001), indicating that for every additional upsetting network stressor, there was an increase of 2.13 mm/Hg in SBP. The association between upsetting personal stressors and daytime SBP was not significant (β(S.E.) = .62 (0.35), p=.07), and the estimate was smaller than that for network stressors. This association is shown in Figure 1 with predicted means from age-adjusted analyses, using descriptive categories of 0, 1, 2, ≥3 upsetting stressors for illustrative purposes only. Predicted daytime SBP means for 0 network and 0 personal upsetting stressors were similar at 118.99 (SD=1.17) mmHg and 118.44 (SD=1.28) mmHg for upsetting network and personal stressors, respectively. However, for 1, 2, and ≥3 upsetting network stressors, predicted daytime SBP means were 122.10 (SD=1.13), 122.49 (SD=1.11), and 126.80 (SD=1.11) mmHg; while predicted means for 1, 2, and ≥3 upsetting personal stressors were 120.23 (SD=1.21), 123.06 (SD=1.50), and 122.7 (SD=1.39) mmHg, respectively (Figure 1). Thus, there was an approximate predicted mean difference of 7.81 mmHg in daytime SBP for women reporting 0 versus ≥3 upsetting network stressors. For upsetting personal stressors, this difference was 4.26 mmHg.
Table 2.
Network Stressors, Personal Stressors, and Daytime ABP in Early Middle-Aged African-American Women, N=392
| Network Stressors | Personal Stressors | |||||||
|---|---|---|---|---|---|---|---|---|
| Daytime SBP | Daytime DBP | Daytime SBP | Daytime DBP | |||||
| β (S.E.) | p-value | β (S.E.) | p-value | β (S.E.) | p-value | β (S.E.) | p-value | |
| Model 1 | 2.13 (0.51) | <0.0001 | 1.59 (0.37) | <0.0001 | 0.62 (0.35) | 0.08 | 0.39 (0.25) | 0.12 |
| Model 2 | 2.01 (0.51) | <0.0001 | 1.53 (0.37) | <0.0001 | 0.42 (0.35) | 0.23 | 0.29 (0.25) | 0.25 |
| Model 3 | 1.97 (0.51) | <0.0001 | 1.49 (0.37) | <0.0001 | 0.39 (0.35) | 0.27 | 0.26 (0.26) | 0.31 |
| Model 4 | 1.97 (0.49) | <0.0001 | 1.49 (0.36) | <0.0001 | 0.35 (0.33) | 0.29 | 0.23 (0.25) | 0.35 |
| Model 5 | 1.85 (0.50) | <0.0001 | 1.47 (0.37) | <0.0001 | 0.17 (0.35) | 0.63 | 0.15 (0.26) | 0.56 |
| Model 6 | 2.02 (0.54) | 0.0002 | 1.59 (0.39) | <0.0001 | -- | -- | -- | -- |
Model 1: Age-adjusted
Model 2: Adjusted for age, marital status, education, family income and family size
Model 3: Model 2 + BMI, smoking
Model 4: Model 3 + anti-hypertensive medication
Model 5: Model 4 + depressive symptoms.
Model 6: Model 5 adjusting for personal stressors
Figure 1.
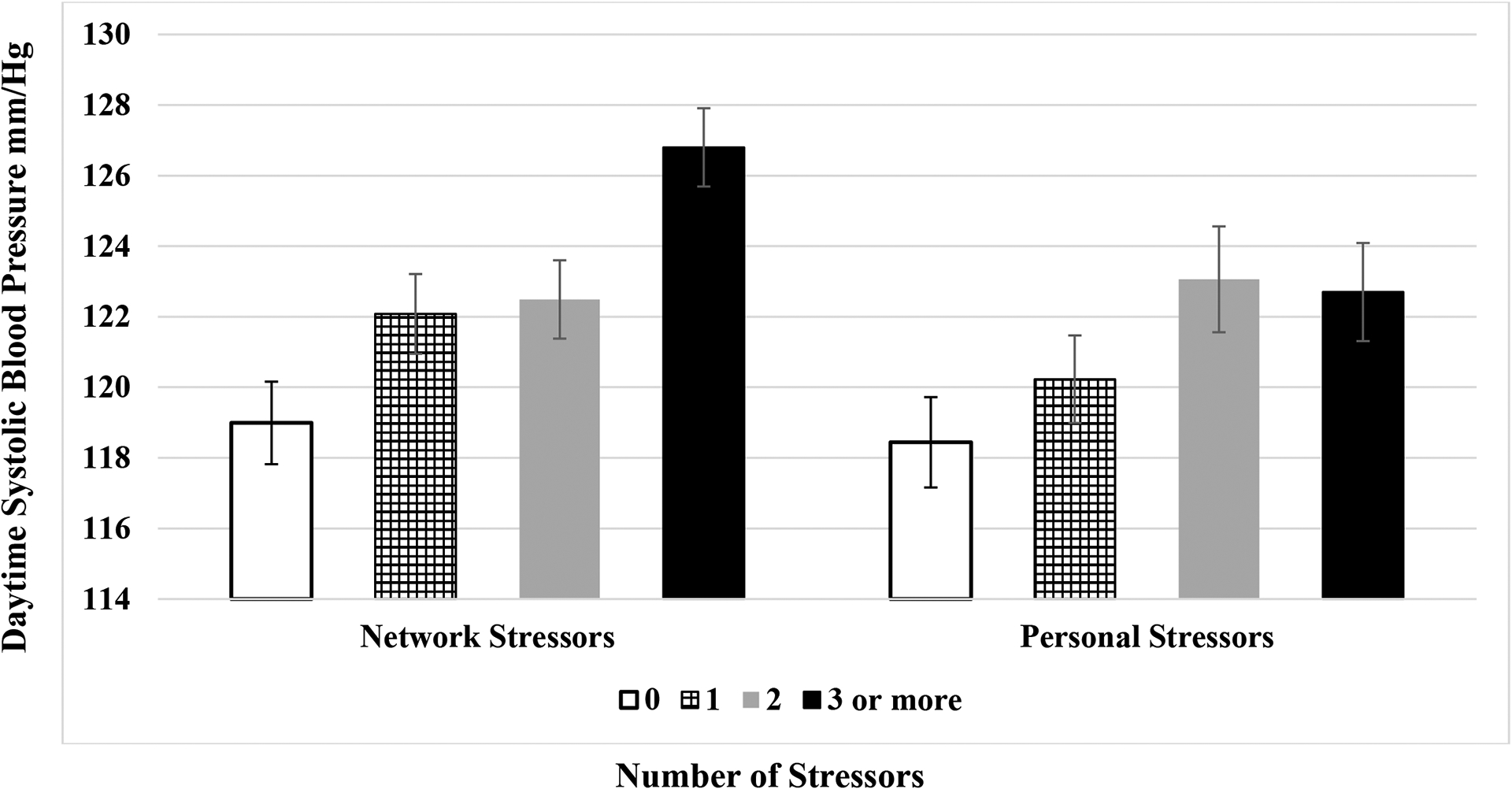
Network Stressors, Personal Stressors, and Daytime Systolic Blood Pressure in Early Middle-Aged African-American Women, N=392
Note: Predicted means from age-adjusted analyses using categories of upsetting stressors for illustrative purposes.
The association between network stressors and daytime SBP persisted after adjustment for marital/live-in partner status, education, family income and family size, BMI, smoking, anti-hypertensive use and depressive symptoms (Models 2–5). Findings were similar for daytime DBP (Table 2). For personal stressors, associations with daytime SBP were no longer marginally significant after adjustment for additional sociodemographics in Model 2 and other covariates in Models 3–5. This patterning of results was similar for daytime DBP (Table 2). Finally, in a fully adjusted Model 6 with both network and personal stressors, the association between network stressors and both daytime SBP and DBP remained significant (Table 2).
Results for nighttime SBP and DBP are shown in Table 3. In an age-adjusted Model 1 there were significant, positive associations between upsetting network stressors and nighttime SBP and DBP, such that a greater number of upsetting network stressors were associated with higher levels of BP. Associations persisted after adjusting for additional sociodemographics, BMI, smoking, anti-hypertensive use and depressive symptoms (Table 3; Models 2–5). There were no significant associations between personal stressors and nighttime SBP or DBP (Table 3). Findings between network stressors and nighttime SBP and DBP also remained significant in a final Model 6, fully-adjusted for all covariates as well as upsetting personal stressors (Table 3).
Table 3:
Network Stressors, Personal Stressors, and Nighttime ABP in Early Middle-Aged African-American Women, N=390
| Network Stressors | Personal Stressors | |||||||
|---|---|---|---|---|---|---|---|---|
| Nighttime SBP | Nighttime DBP | Nighttime SBP | Nighttime DBP | |||||
| β (S.E.) | p-value | β (S.E.) | p-value | β (S.E.) | p-value | β (S.E.) | p-value | |
| Model 1 | 1.59 (0.50) | 0.002 | 1.21 (0.36) | 0.001 | 0.43 (0.33) | 0.20 | 0.39 (0.24) | 0.11 |
| Model 2 | 1.49 (0.50) | 0.003 | 1.13 (0.36) | 0.002 | 0.26 (0.34) | 0.44 | 0.28 (0.25) | 0.27 |
| Model 3 | 1.44 (0.48) | 0.003 | 1.08 (0.36) | 0.003 | 0.23 (0.33) | 0.49 | 0.24 (0.25) | 0.33 |
| Model 4 | 1.45 (0.46) | 0.002 | 1.09 (0.35) | 0.002 | 0.20 (0.32) | 0.53 | 0.22 (0.24) | 0.35 |
| Model 5 | 1.37 (0.48) | 0.005 | 1.05 (0.36) | 0.004 | 0.06 (0.33) | 0.85 | 0.15 (0.25) | 0.56 |
| Model 6 | 1.52 (0.51) | 0.003 | 1.11 (0.39) | 0.0041 | -- | -- | -- | -- |
Model 1: Age-adjusted
Model 2: Adjusted for age, marital status, education, family income and family size
Model 3: Model 2 + BMI, smoking
Model 4: Model 3 + anti-hypertensive medication
Model 5: Model 4 + depressive symptoms.
Model 6: Model 5 adjusting for personal stressors
Type of Stressor and Sustained Hypertension
As shown in Table 4 in age-adjusted models, upsetting network (OR=1.37; 95% CI=1.15–1.64), but not personal, stressors were associated with increased odds of sustained hypertension. These associations persisted in fully-adjusted models (Table 4). Additionally, the association between upsetting network stressors and sustained hypertension remained significant in a separate Model 6, after adding an adjustment for personal stressors (Table 4).
Table 4:
Network Stressors, Personal Stressors, and Sustained Hypertension in Early Middle-Aged African-American Women, N=392
| Network Stressors | Personal Stressors | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Model 1 | 1.37 | 1.15–1.64 | 1.09 | 0.97–1.23 |
| Model 2 | 1.37 | 1.14–1.64 | 1.07 | 0.95–1.21 |
| Model 3 | 1.37 | 1.14–1.65 | 1.07 | 0.94–1.21 |
| Model 4 | 1.40 | 1.15–1.69 | 1.06 | 0.94–1.21 |
| Model 5 | 1.39 | 1.14–1.69 | 1.04 | 0.91–1.20 |
| Model 6 | 1.42 | 1.15–1.76 | -- | -- |
Model 1: Age-adjusted
Model 2: Adjusted for age, marital status, education, family income and family size
Model 3: Model 2 + BMI, smoking
Model 4: Model 3 + anti-hypertensive medication
Model 5: Model 4 + depressive symptoms.
Model 6: Model 5 adjusting for personal stressors
The Potential Moderating Role of overall SWS and Obligation to Help Others
In an age-adjusted exploratory linear regression analyses, with terms for network stressors, overall SWS, and the network stressors by overall SWS interaction, there was no significant interaction for daytime SBP (p=.48), daytime DBP (p=.06), nighttime SBP (p=.62) or nighttime DBP (p=.17). Findings remained non-significant after adjusting for additional covariates in models 2–6 (all p-values >.15). Similarly, in age-adjusted linear regression analyses with terms for network stressors, the obligation to help others subscale, and the network stressors by obligation to help others subscale interaction, the interaction was non-significant for daytime SBP (p=.20), nighttime SBP (p=.21) and nighttime DBP (p=.10); but was significant for daytime DBP (p=.02). Findings for daytime SBP, nighttime SBP and nighttime DBP remained non-significant in all subsequent models (Models 2–6) and findings for daytime DBP were non-significant after adjusting for anti-hypertensive use. Results for sustained hypertension were comparable to those for daytime DBP. There were no significant interactions between personal stressors and overall SWS, or personal stressors and the SWS obligation to help others subscale on daytime SBP or DBP, or nighttime SBP or DBP, or sustained hypertension in any model (all p-values >.49)
Discussion
To our knowledge, this study is the first to examine the association between network, versus personal, stressors and an objective, physiological indicator of health. In our cohort of early middle-aged African-American women from a range of SES backgrounds, we found that upsetting network stressors were less common, yet more impactful with respect to ABP outcomes than personal stressors. More specifically, after adjusting for sociodemographics, we observed significant associations between upsetting network, but not personal, stressors and 48-hour daytime and nighttime SBP and DBP, as well as sustained hypertension. Results persisted after additional controls for smoking, BMI, anti-hypertensive use, and depressive symptoms.
Our observed findings are somewhat consistent with prior studies of psychosocial stress and BP in African-American adults, which documented significant stress and BP associations in African-American women specifically, underscoring the importance of additional research in this at-risk group. For example, in a cross-sectional analysis of N=3,980 African-American adults from the Jackson Heart Study, both global perceived stress and negative life events were associated with hypertension in African-American women, but not African-American men (Gebreab et al., 2012). Similarly, in a longitudinal analysis of N=1,829 participants from the same cohort without hypertension at baseline, high perceived stress over time was associated with incident hypertension among African-American women, but not African-American men (Spruill et al., 2019). However, in contrast to the current study, these prior studies used resting, rather than ABP, which likely overestimated the prevalence of hypertension, and may have resulted in less accurate estimates of the overall stress and BP association. Additionally, because both studies focused on stress exposure more broadly, they did not distinguish between personal, versus network, stressors as a possible explanation for the notable vulnerability to psychosocial stress observed in African-American women compared to African-American men. Consequently, the current research advances the literature in this area both methodologically and conceptually.
Our differential findings for network, versus personal, stressors are in keeping with Kessler and McLeod’s (1984) original “cost of caring” hypothesis which posits that women may be more vulnerable to negative events that impact close others, versus those that impact themselves. Our associations are also quite strong. For example, a reduction of 5 mm/Hg or more in SBP is associated with a 10% reduction in later life cardiovascular events (Blood Pressure Lowering Treatment Trialists, 2021). Differences in predicted values of daytime SBP from descriptive analyses comparing the highest versus lowest categories of network stress were actually larger than this, with an approximate mean difference of 7.81 mm/Hg between those reporting no upsetting network stressors in the prior 12 months compared to those reporting 3 or more. Although reports of upsetting network stressors were not particularly elevated in our cohort (similar to findings from Giscombé et al (2015), approximately 45% of women reported none), these findings have profound implications for those African-American women who are exposed to a high number of upsetting network stressors.
The current analysis examined stressors that occurred in the 12-month period preceding the assessment of ABP, with an exclusive focus on African-American women. This is important because many of the network events examined such as unemployment, chronic illnesses, problems with the police/legal system, and even caregiving (if resulting from potential foster care placement of a child, or debilitating health conditions in a network member) are disproportionately experienced by African-American men and women, relative to men and women from other racial/ethnic backgrounds (Lee et al., 2015; Looney & Turner, 2018; Roberts, 2022). Moreover, in many instances these stressors have been shaped by both historical and contemporary discriminatory policies and practices (Alexander, 2020; Edwards et al., 2019). Hence they may co-occur and/or accumulate over a 12-month period. Consequently, given the social context of African-American women’s lives, the “cost of caring” in a given year may be especially pronounced. Prior studies have examined individual network stressors as contributors to poor health in African-American women (e.g. partner legal problems/incarceration and health) (Lee et al., 2014), but to date there has been limited research on whether the accumulation of multiple types of network stressors are associated with physical health outcomes in this group. Thus, the current findings fill an important gap in the literature, by documenting linkages between a greater number of network stressors and higher levels of BP in a disproportionately impacted group of women.
Interestingly, while there was a graded association observed between the number of personal stressors and daytime SBP in our cohort, associations between personal stressors and ABP outcomes were not significant. This is a particularly noteworthy finding, because although we expected stronger associations for network, versus personal stressors, the relatively weak and nonsignificant effect sizes for personal stressors were somewhat surprising. In keeping with theoretical work on network stressors among African-American women, we explored the possibility that network stressors might be more impactful than personal stressors because of the added pressure that African-American women may face due to community norms around needing to be the backbone, or “Superwoman,” who takes care of everyone else. However, findings from exploratory analyses examining SWS endorsement (particularly the obligation to take care of others subscale), as a moderator of the association between type of stressor and BP outcomes yielded largely null results. There was also no primary association between SWS endorsement and elevated BP in our cohort, which suggests that other factors may be driving our observed associations.
Thus, although our findings shed light on a relatively understudied correlate of elevated BP in African-American women, the psychological and physiological mechanisms underlying these associations require further exploration. While it is plausible that network stressors are associated with physical health outcomes simply due to stress “spillover” or contagion (Bolger et al., 1989; Everett et al., 2010)-- i.e. because they create a cascade of additional stressors in the individual (e.g. legal problems for a partner or child leading to financial problems for the participant), the lack of an observed association between personal stressors and ABP outcomes suggests that this may not be the case in our cohort. Additionally, while network stressors have been linked to mental health outcomes in women, our findings were also independent of depressive symptoms. Consequently, other factors likely play a role.
We are unable to attribute our findings for network, compared to personal, stressors solely to the interpersonal nature of the events in the network stress subscale, because the personal stressors subscale also included interpersonal events. However, it is possible that because the network stressors subscale only included events that involved others, those events were experienced as more unpredictable, or uncontrollable, than the events on the personal stressors subscale. Both laboratory and community-based studies have found that stressors experienced as uncontrollable or unpredictable are more strongly associated with elevated BP and increases in markers of autonomic arousal (precurses to elevated BP) than stressors that are predictable or controllable in nature (Breier et al., 1987; Kiecolt-Glaser et al., 2020; Peters et al., 1998; Steptoe et al., 1999). Hence, future research examining the role of uncontrollability or unpredictability in the relationship between network stressors and BP is warranted.
Other psychosocial factors may also be relevant. Our findings were independent of negative affect in the form of depressive symptoms; however research suggests that positive affect may be important to consider. In a daily diary study of a predominantly female cohort of African-American and White middle-aged adults, Cichy et al (2012) found that on days where individuals experienced high levels of network stressors, both African-Americans and Whites had elevated rates of negative affect—however, only African-Americans had lower rates of positive affect (Cichy et al., 2012). The finding that positive affect was uniquely salient for African-Americans compared to Whites suggests that for African-American women, network stressors could potentially impact health via reductions in positive affect, or psychological well-being, rather than increases in negative affect or psychological distress alone.
Lower levels of psychological well-being (e.g. positive affect, optimism, purpose in life) have been associated with risk factors for elevated BP including smoking, BMI, diet and inflammation (Kubzansky et al., 2018). We were able to control for smoking and BMI, but these other factors, along with measures of autonomic arousal, are all potential mechanisms that should be examined in future studies. Understanding linkages among network stress, reduced psychological well-being and CVD risk in African-American women may be particularly important given prior research suggesting that the association between aspects of psychological well-being (e.g. high optimism and low pessimism) and incident CVD may be more pronounced for African-American, compared to White women (Tindle et al., 2009). The potential importance of low psychological well-being also has significant implications for intervention, as most psychological interventions emphasize the reduction of negative affect/emotional states. However, interventions that focus on increasing psychological well-being might also be useful for African-American women’s CV health. Additional research in this area is warranted.
This study has limitations that should be noted. First, our findings are cross-sectional; thus we are unable to fully determine the temporal associations among network stressors, health behaviors, depressive symptoms and elevated BP. Moreover, we focused on women from a single race/ethnicity, and while prior theoretical and empirical research suggests that African-American women likely have the most exposure to network stressors compared to women (and men) from other racial/ethnic backgrounds (Burroughs Peña et al., 2019; Matthews et al., 2019), it is unclear whether our findings would generalize to individuals from other racial/ethnic groups. Our cohort was also fairly well-educated, and while it is possible that the prevalence of network and/or personal stressors would be higher in a lower-SES cohort of African-American women, the levels of stress reported in our cohort are comparable to those observed in other studies of African-American women (Woods-Giscombé et al., 2015), including those with a higher proportion of women from lower-SES backgrounds (Matthews et al., 2019; Troxel et al., 2003). Also, qualitative studies of African-American women have found that both high and low-SES African-American women report having low SES African-Americans in their immediate (e.g. parents, siblings) as well as extended family and social networks (Everett et al., 2010; Heflin & Pattillo, 2006; Pattillo, 2013). Because these low SES network members often experience high levels of stress, higher SES may not be especially protective against network stressors for African-American women (Walton & Boone, 2019). Similarly, research suggests that higher education is not protective against poor cardiovascular health for African-American women (Assari et al., 2018; Lewis et al., 2005) due to the “diminishing returns” of higher SES in this group. Nonetheless, it is possible that our findings would differ with a larger proportion of lower SES women. Additionally, our cohort was recruited from a single city in the Southeastern United States, and while rates of CVD among African-Americans are highest in this region (Zheng et al., 2021), findings from this area may not generalize to other geographic regions. Finally, we used fixed times for the assessment of daytime and nighttime ABP readings, and while research suggests that this results in limited bias in estimating ABP-assessed nighttime BP relative to self-report or actigraphy-assessed sleep times (Booth et al., 2016), objective sleep times remain the gold standard.
Our study also has several strengths. To begin with, we focused on an at-risk group, at a critical life stage. Elevated BP is a significant contributor to excess rates of CVD, and recent studies have found that CVD events occur in women (irrespective of race/ethnicity) at lower thresholds of BP than in men-- and this association is especially pronounced under age 52 (Ji et al., 2021). Among women, rates of elevated BP are highest in African-American women, compared to women of all other racial/ethnic backgrounds (Virani et al., 2021), yet between 2007–2010 and 2015–2018 rates of hypertension awareness, treatment, and control declined the most for African-American women, compared to other race-gender groups (Virani et al., 2021), further underscoring the importance of understanding unique contributors to elevated BP in this group. Other strengths of the study include the inclusion of women from a relatively wide range of SES backgrounds, and our highly rigorous assessment of BP.
In sum, our findings indicate that network stressors may be an important contributor to elevated daytime BP in African-American women, independent of personal stressors, depressive symptoms, and several CVD risk factors. Future studies are needed to identify the psychological, behavioral, and physiological mechanisms underlying our observed associations, and to determine whether network stressors are associated with increases in BP over time. Additional research is also needed to examine upstream, structural factors (i.e., unequal policing, discriminatory labor practices, community violence) that might give rise to both network stressors and elevated BP in African-American women. Nonetheless, given the high prevalence of stressors observed among African-American populations compared to other racial/ethnic groups, tailored stress-management interventions specifically focused on managing the “cost of caring”-- i.e. the burden associated with negative life events that involve important others—might ultimately prove beneficial for the health of African-American women.
Supplementary Material
Public Significance:
Compared to women from other racial/ethnic groups, African-American women have the highest rates of elevated blood pressure and hypertension, and psychosocial stressors are believed to play a role. The current findings suggest that stressors that involve family members and close friends (i.e., network stressors) may actually have a greater impact on elevated blood pressure for African-American women than stressors that impact them as individuals. Given the high rates of stress in African-American communities overall, this “cost of caring” may have profound implications for the health of African-American women.
Acknowledgements
The MUSE study was funded by grants R01 HL130471 and R01 HL158141. TT Lewis received additional funding from K24 HL163696. R Parker, II McKinnon and T Spikes were funded by T32 HL130025.
References
- Abdalla M, Goldsmith J, Muntner P, Diaz KM, Reynolds K, Schwartz JE, & Shimbo D (2015). Is Isolated Nocturnal Hypertension a Reproducible Phenotype? Am J Hypertens, 29(1), 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander M (2020). The New Jim Crow: Mass Incarceration in the Age of Colorblindness. The New Press. [Google Scholar]
- Assari S, Thomas A, Caldwell CH, & Mincy RB (2018). Blacks’ Diminished Health Return of Family Structure and Socioeconomic Status; 15 Years of Follow-up of a National Urban Sample of Youth. Journal of Urban Health, 95(1), 21–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, & Erbaugh J (1961). An Inventory for Measuring Depression. Arch Gen Psychiatry, 4, 561–571. [DOI] [PubMed] [Google Scholar]
- Blood Pressure Lowering Treatment Trialists, C. (2021). Pharmacological Blood Pressure Lowering for Primary and Secondary Prevention of Cardiovascular Disease across Different Levels of Blood Pressure: An Individual Participant-Level Data Meta-Analysis. Lancet, 397(10285), 1625–1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boggia J, Thijs L, Hansen TW, Li Y, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Olszanecka A, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Maestre G, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’brien E, & Staessen JA (2011). Ambulatory Blood Pressure Monitoring in 9357 Subjects from 11 Populations Highlights Missed Opportunities for Cardiovascular Prevention in Women. Hypertension, 57(3), 397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolger N, Delongis A, Kessler RC, & Wethington E (1989). The Contagion of Stress across Multiple Roles. Journal of Marriage and the Family, 175–183. [Google Scholar]
- Booth JN 3rd, Muntner P, Abdalla M, Diaz KM, Viera AJ, Reynolds K, Schwartz JE, & Shimbo D (2016). Differences in Night-Time and Daytime Ambulatory Blood Pressure When Diurnal Periods Are Defined by Self-Report, Fixed-Times, and Actigraphy: Improving the Detection of Hypertension Study. J Hypertens, 34(2), 235–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breier A, Albus M, Pickar D, Zahn TP, Wolkowitz OM, & Paul SM (1987). Controllable and Uncontrollable Stress in Humans: Alterations in Mood and Neuroendocrine and Psychophysiological Function. The American journal of psychiatry. [DOI] [PubMed] [Google Scholar]
- Burroughs Peña MS, Mbassa RS, Slopen NB, Williams DR, Buring JE, & Albert MA (2019). Cumulative Psychosocial Stress and Ideal Cardiovascular Health in Older Women: Data by Race/Ethnicity. Circulation, 139(17), 2012–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnethon MR, Pu J, Howard G, Albert MA, Anderson C. a. M., Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA, Willis M, & Yancy CW (2017). Cardiovascular Health in African Americans: A Scientific Statement from the American Heart Association. Circulation, 136. [DOI] [PubMed] [Google Scholar]
- Cichy KE, Stawski RS, & Almeida DM (2012). Racial Differences in Exposure and Reactivity to Daily Family Stressors. J Marriage Fam, 74(3), 572–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Murphy ML, & Prather AA (2019). Ten Surprising Facts About Stressful Life Events and Disease Risk. Annual review of psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cundiff JM, Uchino BN, Smith TW, & Birmingham W (2015). Socioeconomic Status and Health: Education and Income Are Independent and Joint Predictors of Ambulatory Blood Pressure. J Behav Med, 38(1), 9–16. [DOI] [PubMed] [Google Scholar]
- Davis MC, Matthews KA, & Twamley EW (1999). Is Life More Difficult on Mars or Venus? A Meta-Analytic Review of Sex Differences in Major and Minor Life Events. Ann Behav Med, 21(1), 83–97. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BS, Krasnoff L, Askenasy AR, & Dohrenwend BP (1978). Exemplification of a Method for Scaling Life Events: The Peri Life Events Scale. J Health Soc Behav, 19(2), 205–229. [PubMed] [Google Scholar]
- Edwards F, Lee H, & Esposito M (2019). Risk of Being Killed by Police Use of Force in the United States by Age, Race–Ethnicity, and Sex. Proceedings of the National Academy of Sciences, 116(34), 16793–16798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett JE, Camille Hall J, & Hamilton-Mason J (2010). Everyday Conflict and Daily Stressors: Coping Responses of Black Women. Affilia, 25(1), 30–42. [Google Scholar]
- Fryer RG, Pager D, & Spenkuch JL (2013). Racial Disparities in Job Finding and Offered Wages. The Journal of Law and Economics, 56(3), 633–689. [Google Scholar]
- Gavrilova L, & Zawadzki MJ (2021). Testing the Associations between State and Trait Anxiety, Anger, Sadness, and Ambulatory Blood Pressure and Whether Race Impacts These Relationships. Annals of Behavioral Medicine. [DOI] [PubMed] [Google Scholar]
- Gebreab SY, Diez-Roux AV, Hickson DA, Boykin S, Sims M, Sarpong DF, Taylor HA, & Wyatt SB (2012). The Contribution of Stress to the Social Patterning of Clinical and Subclinical Cvd Risk Factors in African Americans: The Jackson Heart Study. Social science & medicine, 75(9), 1697–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert-Ouimet M, Brisson C, Milot A, & Vézina M (2017). Double Exposure to Adverse Psychosocial Work Factors and High Family Responsibilities as Related to Ambulatory Blood Pressure at Work: A 5-Year Prospective Study in Women with White-Collar Jobs. Psychosom Med, 79(5), 593–602. [DOI] [PubMed] [Google Scholar]
- Hansen TW, Li Y, Boggia J, Thijs L, Richart T, & Staessen JA (2011). Predictive Role of the Nighttime Blood Pressure. Hypertension, 57(1), 3–10. [DOI] [PubMed] [Google Scholar]
- Haxton CL, & Harknett K (2009). Racial and Gender Differences in Kin Support: A MixedMethods Study of African American and Hispanic Couples. Journal of family Issues, 30(8), 1019–1040. [Google Scholar]
- Heflin CM, & Pattillo M (2006). Poverty in the Family: Race, Siblings, and Socioeconomic Heterogeneity. Social Science Research, 35(4), 804–822. [Google Scholar]
- Helgeson VS (2011). Gender, Stress, and Coping. In The Oxford Handbook of Stress, Health, and Coping. (pp. 63–85). Oxford University Press. [Google Scholar]
- Huang T, & Redline S (2019). Cross-Sectional and Prospective Associations of Actigraphy-Assessed Sleep Regularity with Metabolic Abnormalities: The Multi-Ethnic Study of Atherosclerosis. Diabetes Care, 42(8), 1422–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji H, Kim A, Ebinger JE, Niiranen TJ, Claggett BL, Bairey Merz CN, & Cheng S (2020). Sex Differences in Blood Pressure Trajectories over the Life Course. JAMA Cardiology, 5(3), 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji H, Niiranen TJ, Rader F, Henglin M, Kim A, Ebinger JE, Claggett B, Merz CNB, & Cheng S (2021). Sex Differences in Blood Pressure Associations with Cardiovascular Outcomes. Circulation, 143(7), 761–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph NT, Muldoon MF, Manuck SB, Matthews KA, Macdonald LA, Grosch J, & Kamarck TW (2016). The Role of Occupational Status in the Association between Job Strain and Ambulatory Blood Pressure During Working and Nonworking Days. Psychosom Med, 78(8), 940–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, & Mcleod JD (1984). Sex Differences in Vulnerability to Undesirable Life Events. American Sociological Review, 620–631. [Google Scholar]
- Kiecolt-Glaser JK, Renna ME, Shrout MR, & Madison AA (2020). Stress Reactivity: What Pushes Us Higher, Faster, and Longer—and Why It Matters. Current Directions in Psychological Science, 29(5), 492–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL, Rathouz PJ, Yan LL, Liu K, & Lauderdale DS (2007). Intra-Individual Daily and Yearly Variability in Actigraphically Recorded Sleep Measures: The Cardia Study. Sleep, 30(6), 793–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubzansky LD, Huffman JC, Boehm JK, Hernandez R, Kim ES, Koga HK, Feig EH, Lloyd-Jones DM, Seligman MEP, & Labarthe DR (2018). Positive Psychological Well-Being and Cardiovascular Disease: Jacc Health Promotion Series. J Am Coll Cardiol, 72(12), 1382–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landsbergis PA, Dobson M, Koutsouras G, & Schnall P (2013). Job Strain and Ambulatory Blood Pressure: A Meta-Analysis and Systematic Review. Am J Public Health, 103(3), e61–e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Mccormick T, Hicken MT, & Wildeman C (2015). Racial Inequalities in Connectedness to Imprisoned Individuals in the United States. Du Bois Review, 12(2), 269. [Google Scholar]
- Lee H, Wildeman C, Wang EA, Matusko N, & Jackson JS (2014). A Heavy Burden: The Cardiovascular Health Consequences of Having a Family Member Incarcerated. Am J Public Health, 104(3), 421–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Sternfeld B, Karavolos K, Wesley D, & Powell LH (2005). Race, Education, and Weight Change in a Biracial Sample of Women at Midlife. Arch Intern Med, 165(5), 545–551. [DOI] [PubMed] [Google Scholar]
- Looney A, & Turner N (2018). Work and Opportunity before and after Incarceration. Washington, DC: Brookings Institution. Accessed October, 5, 2018. [Google Scholar]
- Matsumoto K, Jin Z, Homma S, Elkind MSV, Schwartz JE, Rundek T, Mannina C, Ito K, Sacco RL, & Tullio MRD (2021). Office, Central, and Ambulatory Blood Pressure for Predicting First Stroke in Older Adults: A Community-Based Cohort Study. Hypertension, 78(3), 851–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Hall MH, Lee L, Kravitz HM, Chang Y, Appelhans BM, Swanson LM, Neal-Perry GS, & Joffe H (2019). Racial/Ethnic Disparities in Women’s Sleep Duration, Continuity, and Quality, and Their Statistical Mediators: Study of Women’s Health across the Nation. Sleep, 42(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mckinnon II, Johnson DA, Murden RJ, Erving CL, Parker R, Van Dyke ME, Vaccarino V, Booker B, Moore RH, & Lewis TT (2022). Extreme RacismRelated Events and Poor Sleep in African-American Women. Social science & medicine, 115269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcleod GF, Horwood LJ, Fergusson DM, & Boden JM (2016). Life-Stress and Reactivity by Gender in a Longitudinal Birth Cohort at 30 and 35 years. Soc Psychiatry Psychiatr Epidemiol, 51(10), 1385–1394. [DOI] [PubMed] [Google Scholar]
- Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, Myers MG, Ogedegbe G, Schwartz JE, Townsend RR, Urbina EM, Viera AJ, White WB, & Wright JT Jr. (2019). Measurement of Blood Pressure in Humans: A Scientific Statement from the American Heart Association. Hypertension, 73(5), e35–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattillo M (2013). Black Picket Fences: Privilege & Peril among the Black Middle Class. University of Chicago Press. [Google Scholar]
- Pearlin LI (1989). The Sociological Study of Stress. J Health Soc Behav, 241–256. [PubMed] [Google Scholar]
- Peters ML, Godaert GLR, Ballieux RE, Van Vliet M, Willemsen JJ, Sweep FCGJ, & Heijnen CJ (1998). Cardiovascular and Endocrine Responses to Experimental Stress: Effects of Mental Effort and Controllability. Psychoneuroendocrinology, 23(1), 1–17. [DOI] [PubMed] [Google Scholar]
- Ravenell J, Shimbo D, Booth JN, Sarpong DF, Agyemang C, Moody DLB, Abdalla M, Spruill TM, Shallcross AJ, Bress AP, Muntner P, & Ogedegbe G (2017). Thresholds for Ambulatory Blood Pressure among African Americans in the Jackson Heart Study. Circulation, 135(25), 2470–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts D (2022). Torn Apart: How the Child Welfare System Destroys Black Families--and How Abolition Can Build a Safer World. Basic Books. [Google Scholar]
- Rodriguez CJ, Jin Z, Schwartz JE, Turner-Lloveras D, Sacco RL, Di Tullio MR, & Homma S (2013). Socioeconomic Status, Psychosocial Factors, Race and Nocturnal Blood Pressure Dipping in a Hispanic Cohort. Am J Hypertens, 26(5), 673–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkisian N, & Gerstel N (2004). Kin Support among Blacks and Whites: Race and Family Organization. American Sociological Review, 69(6), 812–837. [Google Scholar]
- Schwartz JE, Burg MM, Shimbo D, Broderick JE, Stone AA, Ishikawa J, Sloan R, Yurgel T, Grossman S, & Pickering TG (2016). Clinic Blood Pressure Underestimates Ambulatory Blood Pressure in an Untreated Employer-Based Us Population. Circulation, 134(23), 1794–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settles IH, Pratt-Hyatt JS, & Buchanan NT (2008). Through the Lens of Race: Black and White Women’s Perceptions of Womanhood. Psychol Women Q, 32(4), 454–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih JH, Eberhart NK, Hammen CL, & Brennan PA (2006). Differential Exposure and Reactivity to Interpersonal Stress Predict Sex Differences in Adolescent Depression. Journal of Clinical Child & Adolescent Psychology, 35(1), 103–115. [DOI] [PubMed] [Google Scholar]
- Spikes T, Murden R, Mckinnon Ii, Bromfield S, Van Dyke ME, Moore RH, Rahbari-Oskoui FF, Quyummi A, Vaccarino V, & Lewis TT (2022). Association of Net Worth and Ambulatory Blood Pressure in Early Middle-Aged African American Women. JAMA Netw Open, 5(2), e220331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruill TM, Butler MJ, Thomas SJ, Tajeu GS, Kalinowski J, Castañeda SF, Langford AT, Abdalla M, Blackshear C, Allison M, Ogedegbe G, Sims M, & Shimbo D (2019). Association between High Perceived Stress over Time and Incident Hypertension in Black Adults: Findings from the Jackson Heart Study. J Am Heart Assoc, 8(21), e012139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruill TM, Shallcross AJ, Ogedegbe G, Chaplin WF, Butler M, Palfrey A, Shimbo D, Muntner P, Sims M, Sarpong DF, Agyemang C, & Ravenell J (2016). Psychosocial Correlates of Nocturnal Blood Pressure Dipping in African Americans: The Jackson Heart Study. Am J Hypertens, 29(8), 904–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Cropley M, & Joekes K (1999). Job Strain, Blood Pressure and Response to Uncontrollable Stress. J Hypertens, 17(2), 193–200. [DOI] [PubMed] [Google Scholar]
- Tindle HA, Chang Y-F, Kuller LH, Manson JE, Robinson JG, Rosal MC, Siegle GJ, & Matthews KA (2009). Optimism, Cynical Hostility, and Incident Coronary Heart Disease and Mortality in the Women’s Health Initiative. Circulation, 120(8), 656–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, & Sutton-Tyrrell K (2003). Chronic Stress Burden, Discrimination, and Subclinical Carotid Artery Disease in African American and Caucasian Women. Health Psychol, 22(3), 300–309. [DOI] [PubMed] [Google Scholar]
- Trudel X, Brisson C, Milot A, Masse B, & Vézina M (2016). Adverse Psychosocial Work Factors, Blood Pressure and Hypertension Incidence: Repeated Exposure in a 5-Year Prospective Cohort Study. J Epidemiol Community Health, 70(4), 402–408. [DOI] [PubMed] [Google Scholar]
- Turner RJ, & Avison WR (1989). Gender and Depression: Assessing Exposure and Vulnerability to Life Events in a Chronically Strained Population. Journal of nervous and Mental Disease, 177(8), 443–455. [DOI] [PubMed] [Google Scholar]
- Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, Vanwagner LB, Wang N-Y, & Tsao CW (2021). Heart Disease and Stroke Statistics 2021 Update: A Report from the American Heart Association. Circulation, 0(0), CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- Walton QL, & Boone C (2019). Voices Unheard: An Intersectional Approach to Understanding Depression among Middle-Class Black Women. Women & Therapy, 42(3–4), 301–319. [Google Scholar]
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, Depalma SM, Gidding S, Jamerson KA, Jones DW, Maclaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr., Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr., Williamson JD, & Wright JT Jr. (2018). 2017 Acc/Aha/Aapa/Abc/Acpm/Ags/Apha/Ash/Aspc/Nma/Pcna Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension, 71(6), e13–e115. [DOI] [PubMed] [Google Scholar]
- Woods-Giscombe CL, Allen AM, Black AR, Steed TC, Li Y, & Lackey C (2019). The Giscombe Superwoman Schema Questionnaire: Psychometric Properties and Associations with Mental Health and Health Behaviors in African American Women. Issues Ment Health Nurs, 40(8), 672–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods-Giscombé CL, Lobel M, Zimmer C, Wiley Cené C, & Corbie-Smith G (2015). Whose Stress Is Making Me Sick? Network-Stress and Emotional Distress in African-American Women. Issues Ment Health Nurs, 36(9), 710–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y, Wen X, Bian J, Zhao J, Lipkind HS, & Hu H (2021). Racial, Ethnic, and Geographic Disparities in Cardiovascular Health among Women of Childbearing Age in the United States. J Am Heart Assoc, 0(0), e020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


