Abstract
Background
Surgical-site infections (SSIs) are recognized as negatively affecting patient quality of life. No meta-analysis of SSI utility values is available in the literature to inform estimates of this burden and investment decisions in prevention.
Methods
A systematic search of PubMed, MEDLINE, CINAHL, and the National Health Service Economic Evaluation Database was performed in April 2022 in accordance with PROSPERO registration CRD 42021262633. Studies were included where quality-of-life data were gathered from adults undergoing surgery, and such data were presented for those with and without an SSI at similar time points. Two researchers undertook data extraction and quality appraisal independently, with a third as arbiter. Utility values were converted to EuroQol 5D (EQ-5D™) estimates. Meta-analyses were conducted using a random-effects model across all relevant studies, with subgroup analyses on type and timing of the SSI.
Results
In total, 15 studies with 2817 patients met the inclusion criteria. Six studies across seven time points were used in the meta-analysis. The pooled mean difference in EQ-5D™ utility in all studies combined was –0.08 (95 per cent c.i. −0.11 to −0.05; prediction interval −0.16 to −0.01; I2 = 40 per cent). The mean difference in EQ-5D™ utility associated with deep SSI was −0.10 (95 per cent c.i. −0.14 to −0.06; I2 = 0 per cent) and the mean difference in EQ-5D™ utility persisted over time.
Conclusion
The present study provides the first synthesized estimate of SSI burden over the short and long term. EQ-5D™ utility estimates for a range of SSIs are essential for infection prevention planning and future economic modelling.
Surgical-site infection (SSI) presents a considerable economic burden and greatly affects the quality of life of patients. This study is the first to synthesize health-related utility estimates of the associated decrement using a meta-analysis of published work. Estimates are provided for overall impact, SSI type, and time.
Introduction
Healthcare-associated infections (HAIs) are globally the most frequently reported adverse events. Surgical-site infection (SSI) is the most surveyed and frequent HAI in low- and middle-income countries, and the second most frequent HAI in Europe and the USA1. Once developed, SSIs present a significant burden in terms of disability and excess duration of hospital stay2, and contribute to the development of antimicrobial resistance through the increased use of antimicrobials3. Postoperative recovery is extended by SSI and increased use of healthcare resource is required. This impact on morbidity and mortality has a significant effect on patient quality of life4.
A recent systematic review5 highlighted the negative impact of SSI across six themes of patient functioning, namely physical, psychological, social, spiritual, economic, and the health care worker–patient relationship. Patients who develop SSI after surgery have a longer hospital stay by up to 24 days according to some estimates6, with an even greater impact in older people and those infected with resistant microbial strains. Deep SSIs have been reported to be associated with substantial levels of suffering and pain, which may become lifelong7. SSIs are also associated with poorer clinical pain and functional outcomes in a variety of surgical categories8,9. In an attempt to reduce the burden of such infections, SSI prevention is a mainstay of surgical patient care at both national4,10 and international1 levels.
Economic evaluations of interventions are used to inform investment decisions in healthcare within a constrained-resource context11. Cost–utility analysis, a specific form of cost-effectiveness analysis whereby effectiveness is measured through utility12, is ideally suited to explore the economic implications of SSI prevention strategies. Utility can be considered a health valuation on a scale anchored at 0 for dead and 1 for perfect health. This allows for a common outcome unit for interventions that affect both morbidity and mortality13, such as SSI. Utility values can subsequently be used to calculate quality-adjusted life years (QALYs), which are the standard health outcome measure sought by the National Institute for Health and Care Excellence for any interventions commissioned for the National Health Service (NHS) and other public sector bodies in the UK14. A recent systematic review15 identified a paucity of high-quality economic evaluations examining the benefits of SSI prevention. Synthesized utility values for SSI that could be used to generate such evidence are also lacking.
Therefore, a systematic review was undertaken to identify and summarize the utility decrement associated with SSI in adults undergoing surgery reported in the extant evidence base. This information can be used to both quantify the excess burden posed by SSI as well as for future cost–utility analyses evaluating the cost effectiveness of SSI prevention measures. The primary aim was to estimate the impact of any type of superficial, deep, and organ/space infections on the quality of life, as measured by utility score, of adults undergoing surgery.
Methods
Inclusion and exclusion criteria
The PICOS (Population, Intervention, Comparison, Outcomes, and Study) framework16 was used to guide the inclusion criteria. The population comprised adults (as specified by the trialists) receiving any surgery in any setting. Interventions included any adult with any confirmed SSI using any prespecified diagnostic criteria. Comparators were adults undergoing surgery with no SSI. The main outcome measure was utility as measured by a standardized, validated quality-of-life questionnaire, such as EuroQol 5D (EQ-5D™; EuroQol Group, Rotterdam. The Netherlands) or Short Form 36 (SF-36, Ware, Kosinski and Keller, Boston. USA®17). Any study in which quality-of-life data were gathered prospectively or retrospectively from adults undergoing surgery, with such data presented for those with and without SSI at similar time points, was included. The main outcome effect measure was mean difference in EQ-5D™ utility. Study designs that were anticipated to fulfil this criterion were RCTs, controlled trials, case–control studies, matched control studies, or economic evaluation or modelling studies that completed primary data collection for utility values. Information was sought directly from authors if missing from published reports.
Studies were excluded if no set diagnostic criteria for SSI were used, secondary quality-of-life data from published sources (for example, economic modelling studies using published utility values that they did not themselves gather) were used, and studies on children. Studies for which the full text was not available (either published, unpublished or directly from the authors) were also excluded.
Search
The systematic review was registered with PROSPERO (registration number CRD 42021262633). The registration acted as the protocol for this review. Studies that met the PICOS criteria and published in English were included. The following databases were searched from inception to April 2022: PubMed, MEDLINE via EBSCO host, CINAHL via EBSCO host, and the NHS Economic Evaluation Database.
A prespecified search strategy was formulated and adapted for each database’s conventions; details of the main search strategy are available in the supplementary material. The NHS Economic Evaluation Database was searched using Medical Subject Headings only. Reference lists in relevant articles were screened to identify any further potential papers.
Study selection and data extraction
Two authors independently examined the titles and abstracts identified by the search strategy to remove any duplicate records and irrelevant reports. Full-text versions of potentially relevant studies identified by at least one author were retrieved and evaluated. The same two authors independently assessed each study to determine whether it met the eligibility criteria, and extracted data using a standardized data extraction form developed for this review. Any disagreements were resolved by discussion between the authors, with a further author acting as arbiter. The data extraction form included the following: general information (author(s), title, source, contact address, year of study, country of study, year of publication); trial characteristics (design, time horizon, quality-of-life instrument used); participants (baseline characteristics, type of surgery, inclusion and exclusion criteria, sample size, and number of patients allocated to each group or patient cohort details); interventions (SSI type; superficial, deep, organ/space); and outcomes (utility measure in both infected/non-infected groups).
All study outcomes were converted to a single index value of health state utility (EQ-5D™18) if not already presented as such in the studies. SF-12® and SF-36® summary measures are not preference-based and as such cannot be used to subsequently calculate QALYs17. Conversion to EQ-5D™ values is required, so SF-12® study-level data (mean and standard error) and SF-36® summary measures were converted to EQ-5D™ preference scores using UK tariff values19. SF-12® scores were converted using the two-variable model outlined by Lawrence and Fleishman20. SF-36® data were converted using Model EQ (1) from Ara and Brazier21. Synthesis was planned using a random-effects meta-analysis model, which assumes that the study effect sizes are different and that the collected studies represent a random sample from a larger population of studies. Heterogeneity was explored with forest plots and an χ² test. In addition, the I² statistic describing the percentage variation that may be attributed to between-study heterogeneity was calculated. The prediction interval, used to estimate the true effect size and plotting a distribution of true effects22, was also calculated. Finally, a funnel plot was generated23. Subgroup analysis and meta-regression was planned by infection type according to Centers for Disease Control and Prevention criteria (superficial, deep, organ/space), wound classification (clean, clean contaminated, contaminated, dirty or infected)24, National Nosocomial Infections Surveillance risk index criteria25, and time after surgery if possible. Analyses were undertaken using Stata® statistical software26 and the Prediction Intervals Program27.
Quality assessment
Study quality assessment was completed independently by two authors using the STROBE checklist for case–control studies28, the Drummond checklist for economic evaluations29, and the Cochrane Risk of Bias (RoB 2) tool16 for RCTs. RCTs in which randomization of the intervention was not relevant to the SSI outcomes of primary interest of the present review were also assessed using the STROBE checklist. Study components were rated using the relevant ratings in each instrument. Utility valuation studies were rated against the components presented by Stalmeier et al.30. Any disagreement was resolved through discussion. Quality assessment was evaluated both within and across all included study types.
Results
Study selection and characteristics
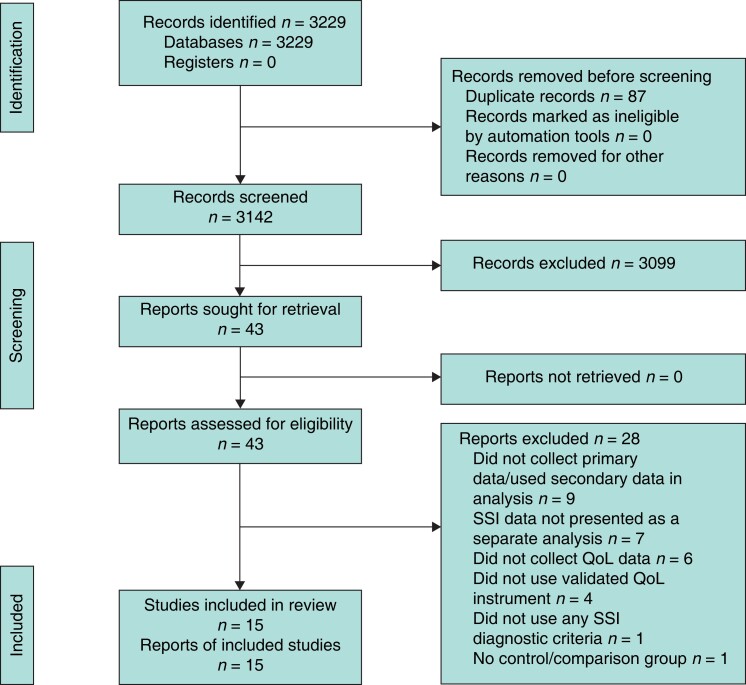
The search identified 3142 titles and abstracts after removal of duplicates. A total of 43 articles were initially identified as having potential and full texts of these were retrieved. Seven articles reported SSI utility data included with the main study comparison groups. The authors were contacted directly for information, but none was obtained. These articles were subsequently excluded. A further 21 were excluded for other reasons and 15 studies met the inclusion criteria (Fig. 1). Characteristics of all included studies are summarized in Table S1.
Fig. 1.
PRISMA flow diagram showing selection of articles for reviewSSI, surgical-site infection; QoL, quality of life.
Publication dates ranged from 2002 to 2021, with a peak in publication rates in the years 2018–2019. The majority of the studies were set in the USA31–36, then the UK37–39, and Australia40,41, with single studies from Brazil42, Spain43, Denmark44 or a combination of European countries8. Most studies examined SSI in orthopaedic surgery involving the spine8,31–33,35,42, total joint replacement37,40,41,43, trauma38 or a combination36. Single studies focused on obstetric44 or non-obstetric34 and vascular39 procedures. The studies predominantly focused on deep8,31–35,38,42 and organ/space40,41 SSI. Only one study43 looked at superficial infections and four36,37,39,44 included all infection types. All studies used a case–control design, with the exception of two RCTs38,39, an economic evaluation44, and a health state valuation using time trade-off interviews37. All studies used standardized validated quality-of-life questionnaires: EQ-5D™31,33,38,39,44, SF-36®8,32,35,36,41–43 or SF-12®34,40. Eight8,34–36,40–43 studies required utility conversions to EQ-5D™.
Quality assessment
The single economic evaluation44 and health state valuation study37 completed most criteria on each respective quality assessment tool29,30. One RCT39 was assessed as having a low risk of bias, whereas the other38 had some concerns, mainly owing to elements in domain 2 (risk of bias due to deviations from the intended interventions) of the Cochrane RoB 2 tool45. The case–control studies were of reasonable quality. Generally, criteria relating to the title and abstract, introduction, and initial methods of the STROBE checklist28 were completed well. There was variability in checklist elements related to bias and statistical methods. Only two studies8,36 provided a flow diagram. One42 did not address limitations, and another36 did not provide details of funding. All other studies performed well on checklist criteria relating to discussion and other information. Overall, the quality of the included studies was fair, with case–control methodology being associated with lower levels of reporting quality than economic evaluation and health state valuation. Results of the quality assessments for all included studies can be found in the Table S2 (case control studies), Table S3 (RCTs), Table S4 (economic evaluation), and Table S5 (health state valuation).
Study-level utility impact of surgical-site infection
Single-study estimates of the utility decrement associated with SSI ranged from –0.203 in deep SSI following total joint replacement (34 cases of SSI) at more than 1 year after surgery41 to –0.03 in all SSIs requiring antibiotic treatment 30 days after caesarean section (39 cases of SSI) using standard wound dressing44. Table S6 outlines the study-level estimates of utility associated within the range of SSIs reported at various time points and SSI types.
Meta-analyses
The authors of studies that did not report the standard deviation, standard error or confidence interval of mean estimates for quality-of-life scores were contacted directly by e-mail for missing data. One supplied the information, one was no longer available, and no response was received from the others. Thus, data from six studies8,34,38,40,43,44 across seven time points (1 to more than 12 months) and a range of procedures (arthroplasty, spinal, lower limb trauma, caesarean section, and all non-obstetric in 1 study site) were available for meta-analysis. The mean difference in EQ-5D™ utility in all studies combined was –0.08 (95 per cent c.i. −0.11 to −0.05; I2 = 40 per cent) (Fig. 2).
Fig. 2.
Main meta-analysis outcome measure showing mean difference in EQ-5D™ utility estimates across six included studies
Mean differences are shown with 95% confidence intervals. A random-effects model was used for meta-analysis. a-dsignify different time points within the same study or for Hyldig the two dressing comparator groups (i.e both arms of the RCT).
Subgroup analyses
Data from two studies8,38 across five time points were available for meta-analysis of deep SSI only. The mean difference in EQ-5D™ utility associated with deep SSI was −0.10 (95 per cent c.i. −0.14 to −0.06; I2 = 0 per cent) (Fig. 3).
Fig. 3.
Forest plot for EQ-5D™ mean difference in deep surgical-site infection only
Mean differences are shown with 95% confidence intervals. *Values are mean(s.d.). EQ-5D™ utility estimates. A random-effects REML model was used for meta-analysis. a-dsignify different time points within the same study or for Hyldig the two dressing comparator groups (i.e both arms of the RCT).
To explore the impact of time since surgery, eligible studies were regrouped into three time-point categories of less than 4 months34,38,44, 6–9 months8,38, and 12 months or more8,38,40,43. The mean difference in EQ-5D™ utility was −0.09 (−0.14 to −0.04; I2 = 71 per cent) at less than 4 months, −0.11 (−0.17 to −0.04; I2 = 0.02 per cent) at 6–9 months, and −0.06 (−0.10 to −0.02; I2 = 0.02 per cent) at 12 months or more (Fig. 4). No data were available for the other planned subgroup analyses.
Fig. 4.
Forest plot for EQ-5D™ mean difference across all surgical-site infection types at different time points
Mean differences are shown with 95% confidence intervals. A random-effects REML model was used for meta-analysis. a-dsignify different time points within the same study or for Hyldig the two dressing comparator groups (i.e both arms of the RCT).
Heterogeneity
The estimate of mean difference in EQ-5D™ utility across all studies may represent moderate heterogeneity with an I2 value of 40 per cent16. An asymmetric funnel plot, as evidenced by scatter points outwith the pseudo 95 per cent confidence interval either side of the mean summary effect estimate46, may indicate this is due to publication bias (Fig. 5). Lower I2 values from subgroup analyses in which only one type of SSI was considered (for example I2 = 0 per cent for deep SSI) and higher ones when different types of surgery were considered (for example I2 = 71 per cent for all SSI types at less than 4 months since surgery) suggest a clinical source of the overall moderate heterogeneity found in the main meta-analysis outcome measure. For the main outcome measure, the true effect size in 95 per cent of all comparable populations fell in the interval −0.16 to −0.01 (Figure S6).
Fig. 5.
Funnel plot of all included studies
Discussion
The primary aim of the review was to estimate the impact of an SSI on quality of life, as measured by utility score, for adults undergoing surgery of any type for all SSIs.
In the meta-analysis of six studies across all time points since surgery, the mean difference in EQ-5D™ utility across all SSI types was −0.08 (95 per cent c.i. −0.11 to −0.05; I2 = 40 per cent) (Fig. 2). For deep SSI, the utility decrement associated with these infections dropped to −0.10 (−0.14 to −0.06; I2 = 0 per cent). The greatest utility decrement was associated with the interval 6–9 months after surgery (−0.11, −0.17 to −0.04; I2 = 0.02 per cent) and this reduced with time (−0.06, −0.10 to −0.02; I2 = 0.02 per cent, at 12 months or more).
The 0.08 utility decrement in the primary outcome meta-analysis may appear relatively minimal. There are, however, certain contextual and methodological considerations to acknowledge. Analysing beyond the EQ-5D™ overall mean score provides insight into which aspects of health are contributing to the reported changes47. Thus, a 0.08 drop in overall EQ-5D™ utility may represent changes in up to two health state dimensions of the valuation instrument48. In practical terms, this could mean that SSIs have influenced health to the extent that moderate, severe or even extreme problems are now present in mobility, self-care, usual activities, pain/discomfort or anxiety/depression. Indeed, given the prediction interval from the analysis, some patients may experience decrements of up to 0.16, compounding this effect. The distribution of true effects indicates that 95 per cent of patients in all comparable populations would consistently experience a decrement in utility due to SSI, highlighting the importance of this clinical issue. The utility value decrement must also be viewed in the context of the high global prevalence of SSI1, resulting in significant cumulative effects on health at the population level. The finding that this decrement is present even at 12 months or more after surgery further highlights the importance of prevention efforts and investment in this area.
To the authors’ knowledge, this is the first systematic review to combine utility valuations of SSI in a meta-analysis. Previous work49 that aimed to summarize the evidence base on SSI utility values identified 28 studies, but no meta-analysis was completed. Additionally, only nine of these studies used patient-level data for health state valuations. The remaining 19 used values mainly sourced from the literature and were of poor methodological quality. The range of utility decrement reported49 is comparable at the lower end of estimates (0.04 versus 0.03 in this study) but not at high the higher end (0.48 versus 0.203 in this study). Interestingly, the authors concluded that the SSI utility decrement is suggested to be near 0.1, in alignment with the findings from the meta-analysis presented here, with an overall mean difference in EQ-5D™ utility of 0.08 in all studies combined.
The scope for heterogeneity across studies examining SSI is wide because of the diverse nature of the infection, evidenced by multilevel diagnostic criteria, surgical classifications24, and specialties. The lack of previous meta-analyses in this field has been justified on this basis50. The included studies for this review predominantly examined deep SSI in orthopaedic surgery and so meta-analysis was deemed appropriate. Studies were not excluded based on surgery and infection type, in line with the primary aim of the review. The moderate levels of heterogeneity found in the main meta-analysis outcome measure support this decision.
Overall, the methodological quality of the studies in this review was good. Several studies did not, however, report the standard deviation, standard error or confidence interval for mean estimates of quality-of-life scores, and only one author responded to the request for such information. Thus, the scope for meta-analysis was limited by the reporting in the original studies. This highlights the need for consistency in reporting of future work in this field, such as the use of reporting tools or checklists for peer review. A further limitation of this review is the lack of data relating to superficial and organ/space SSI and surgical classifications. Although the orthopaedic focus of most included studies facilitated meta-analysis, the utility decrements reported are heavily weighted towards this surgical specialty and may not be appropriate for use in other surgical settings.
Global guidelines1 on the prevention of SSI from the WHO specifically call for robust SSI economic and burden studies to address clinical need. The present study contributes to this call. As with European SSI surveillance, where specific surgical categories are used as indicator metrics for overall SSI burden51, the present findings may offer insight into a wider scope of surgical specialty than those of the studies in the meta-analyses (orthopaedic and obstetrics). Given the paucity of synthesized estimates of SSI impact on health-related quality of life, the review is presented as a reference point from which clinicians may begin to infer utility decrements within wider specialty groupings based on associated clinical risk of other surgical categories. A synthesized estimate offers methodological advantage and increased precision over those derived from single studies52. As such, the present review provides a higher rank of evidence53 for this purpose than previously published work.
The findings of this study confirm the significant burden that SSIs present to the surgical patient population both in the short and long term. The authors sought to quantify the known clinical burden of these infections and demonstrate the long-term (12 months after surgery and beyond) impact on patient quality of life. EQ-5D™ utility estimates for a range of SSIs for use in future economic modelling are also provided. Recommendations for future work in this area include improvement in the quality and consistency of reporting quality-of-life outcomes and data collection across the full scope of the SSI clinical pathway and timeline.
Supplementary Material
Contributor Information
Agi M McFarland, Faculty of Health Sciences and Sport, University of Stirling, Stirling, UK.
Sarkis Manoukian, Faculty of Health Sciences and Sport, University of Stirling, Stirling, UK; Glasgow Caledonian University Yunus Centre for Social Business, Glasgow.
Helen Mason, Faculty of Health Sciences and Sport, University of Stirling, Stirling, UK; Glasgow Caledonian University Yunus Centre for Social Business, Glasgow.
Jacqui S Reilly, Faculty of Health Sciences and Sport, University of Stirling, Stirling, UK; Health and Safeguarding Health through Infection Prevention (SHIP) Research Group, Glasgow.
Funding
Funding for this work was received from Glasgow Caledonian University and Health Protection Scotland via the Evaluation of the Cost of Nosocomial Infection Study.
Author contributions
Agi McFarland (Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Writing—original draft, Writing—review & editing), Sarkis Manoukian (Conceptualization, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Writing—review & editing), Helen Mason (Investigation, Resources, Supervision, Validation, Writing—review & editing), and Jacqui Reilly (Funding acquisition, Methodology, Resources, Supervision, Validation, Writing—review & editing).
Disclosure
The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS online.
Data availability
Data generated for this review are available directly from the corresponding author.
References
- 1. WHO . Global Guidelines for the Prevention of Surgical Site Infection. Geneva, Switzerland: WHO, 2018 [PubMed] [Google Scholar]
- 2. Manoukian S, Stewart S, Dancer S, Graves N, Mason H, McFarland Aet al. Estimating excess length of stay due to healthcare-associated infections: a systematic review and meta-analysis of statistical methodology. J Hosp Infect 2018;100:222–235 [DOI] [PubMed] [Google Scholar]
- 3. WHO . Report on the Burden of Endemic Health Care-associated Infection Worldwide. Geneva, Switzerland: WHO, 2011
- 4. National Institute for Health and Care Excellence . Surgical Site Infections: Prevention and Treatment. NICE Guideline [NG125].https://www.nice.org.uk/guidance/ng125 (accessed 22 April 2022) [PubMed]
- 5. Avsar P, Patton D, Ousey K, Blackburn J, O’Connor T, Moore Z. The impact of surgical site infection on health-related quality of life: a systematic review. Wound Manag Prev 2021;67:10–19 [PubMed] [Google Scholar]
- 6. Jenks PJ, Laurent M, McQuarry S, Watkins R. Clinical and economic burden of surgical site infection (SSI) and predicted financial consequences of elimination of SSI from an English hospital. J Hosp Infect 2014;86:24–33 [DOI] [PubMed] [Google Scholar]
- 7. Andersson AE, Bergh I, Karlsson J, Nilsson K. Patients’ experiences of acquiring a deep surgical site infection: an interview study. Am J Infect Control 2010;38:711–717 [DOI] [PubMed] [Google Scholar]
- 8. Haddad S, Núñez-Pereira S, Pigrau C, Rodríguez-Pardo D, Vila-Casademunt A, Alanay Aet al. The impact of deep surgical site infection on surgical outcomes after posterior adult spinal deformity surgery: a matched control study. Eur Spine J 2018;27:2518–2528 [DOI] [PubMed] [Google Scholar]
- 9. Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Di Cesare PE. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am 2007;89:33–38 [DOI] [PubMed] [Google Scholar]
- 10. Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RRet al. Centers for Disease Control and Prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 2017;152:784–791 [DOI] [PubMed] [Google Scholar]
- 11. Folland S, Goodman AC, Stano M. The Economics of Health and Health Care (6th edn). London, England: Pearson Education, 2009 [Google Scholar]
- 12. McFarland A. Economic evaluation of interventions in health care. Nurs Stand 2014;29:49–58 [DOI] [PubMed] [Google Scholar]
- 13. Drummond MF, Sculpher MJ, Torrance GW, O’Brien B, Stoddart G. Methods for the Economic Evaluation of Health Care Programmes. Oxford, England: Oxford University Press, 2015 [Google Scholar]
- 14. National Institute for Health and Care Excellence . Developing NICE Guidelines: the Manual.https://www.nice.org.uk/process/pmg20/chapter/introduction (accessed 22 April 2022) [PubMed]
- 15. McFarland A, Reilly J, Manoukian S, Mason H. The economic benefits of surgical site infection prevention in adults: a systematic review. J Hosp Infect 2020;106:76–101 [DOI] [PubMed] [Google Scholar]
- 16. Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page Met al. Cochrane Handbook for Systematic Reviews of Interventions. https://training.cochrane.org/handbook/current (accessed 6 May 2022)
- 17. Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: aA User’s Manual. Boston: Health Assessment Lab, New England Medical Centre, 1994 [Google Scholar]
- 18. EuroQol Group . Euroqol—a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199–206 [DOI] [PubMed] [Google Scholar]
- 19. Dolan P, Gudex C, Kind P, Williams A. A Social Tariff For EuroQol: Results From a UK General Population Survey. Discussion Paper 138. York, England: Centre for Health Economics University of York,1995
- 20. Lawrence WF, Fleishman JA. Predicting EuroQoL EQ-5D preference scores from the SF-12 health survey in a nationally representative sample. Med Decis Making 2004;24:160–169 [DOI] [PubMed] [Google Scholar]
- 21. Ara R, Brazier J. Deriving an algorithm to convert the eight mean SF-36 dimension scores into a mean EQ-5D preference-based score from published studies (where patient level data are not available). Value Health 2008;11:1131–1143 [DOI] [PubMed] [Google Scholar]
- 22. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 2010;1:97–111 [DOI] [PubMed] [Google Scholar]
- 23. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Centers for Disease Control and Prevention. National Healthcare Safety Network (NHSN) Patient Safety Component Manual. https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf (accessed 22 April 2022)
- 25. Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TGet al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med 1991;91:152S–157S [DOI] [PubMed] [Google Scholar]
- 26. Timberlake. Stata. 2022; 17 [Google Scholar]
- 27. Comprehensive Meta Analysis . Prediction Intervals Program. 2013; 3 [Google Scholar]
- 28. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–349 [DOI] [PubMed] [Google Scholar]
- 29. Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ economic evaluation working party. BMJ 1996;313:275–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stalmeier PF, Goldstein MK, Holmes AM, Lenert L, Miyamoto J, Stiggelbout AMet al. What should be reported in a methods section on utility assessment? Med Decis Making 2001;21:200–207 [DOI] [PubMed] [Google Scholar]
- 31. Kuhns BD, Lubelski D, Alvin MD, Taub JS, McGirt MJ, Benzel ECet al. Cost and quality of life outcome analysis of postoperative infections after subaxial dorsal cervical fusions. J Neurosurg Spine 2015;22:381–386 [DOI] [PubMed] [Google Scholar]
- 32. Mok JM, Guillaume TJ, Talu U, Berven SH, Deviren V, Kroeber Met al. Clinical outcome of deep wound infection after instrumented posterior spinal fusion: a matched cohort analysis. Spine (Phila Pa 1976) 2009;34:578–583 [DOI] [PubMed] [Google Scholar]
- 33. Pennington Z, Sundar SJ, Lubelski D, Alvin MD, Benzel EC, Mroz TE. Cost and quality of life outcome analysis of postoperative infections after posterior lumbar decompression and fusion. J Clin Neurosci 2019;68:105–110 [DOI] [PubMed] [Google Scholar]
- 34. Perencevich EN, Sands KE, Cosgrove SE, Guadagnoli E, Meara E, Platt R. Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis 2003;9:196–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Petilon JM, Glassman SD, Dimar JR, Carreon LY. Clinical outcomes after lumbar fusion complicated by deep wound infection: a case–control study. Spine (Phila Pa 1976) 2012;37:1370–1374 [DOI] [PubMed] [Google Scholar]
- 36. Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol 2002;23:183–189 [DOI] [PubMed] [Google Scholar]
- 37. Matza LS, Kim KJ, Yu H, Belden KA, Chen AF, Kurd Met al. Health state utilities associated with post-surgical Staphylococcus aureus infections. Eur J Health Econ 2019;20:819–827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Parker B, Petrou S, Masters JPM, Achana F, Costa ML. Economic outcomes associated with deep surgical site infection in patients with an open fracture of the lower limb. Bone Joint J 2018;100-B:1506–1510 [DOI] [PubMed] [Google Scholar]
- 39. Totty JP, Moss JWE, Barker E, Mealing SJ, Posnett JW, Chetter ICet al. The impact of surgical site infection on hospitalisation, treatment costs, and health-related quality of life after vascular surgery. Int Wound J 2021;18:261–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Aboltins C, Dowsey MM, Peel T, Lim WK, Parikh S, Stanley Pet al. Early prosthetic hip joint infection treated with debridement, prosthesis retention and biofilm-active antibiotics: functional outcomes, quality of life and complications. Intern Med J 2013;43:810–815 [DOI] [PubMed] [Google Scholar]
- 41. Cahill JL, Shadbolt B, Scarvell JM, Smith PN. Quality of life after infection in total joint replacement. J Orthop Surg (Hong Kong) 2008;16:58–65 [DOI] [PubMed] [Google Scholar]
- 42. Falavigna A, Righesso O, Traynelis VC. Teles AR, da Silva PG. Effect of deep wound infection following lumbar arthrodesis for degenerative disc disease on long-term outcome: a prospective study: clinical article. J Neurosurg Spine 2011;15:399–403 [DOI] [PubMed] [Google Scholar]
- 43. Guirro P, Hinarejos P, Puig-Verdie L, Sánchez-Soler J, Leal-Blanquet J, Torres-Claramunt Ret al. Superficial wound infection does not cause inferior clinical outcome after TKA. Knee Surg Sports Traumatol Arthrosc 2016;24:3088–3095 [DOI] [PubMed] [Google Scholar]
- 44. Hyldig N, Joergensen JS, Wu C, Bille C, Vinter CA, Sorensen JAet al. Cost-effectiveness of incisional negative pressure wound therapy compared with standard care after caesarean section in obese women: a trial-based economic evaluation. BJOG 2018;126:619–627 [DOI] [PubMed] [Google Scholar]
- 45. Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing Risk of Bias in a Randomized Trial.https://training.cochrane.org/handbook/current/chapter-08 (accessed 22 April 2022)
- 46. Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 2001;54:1046–1055 [DOI] [PubMed] [Google Scholar]
- 47. Devlin NJ, Parkin D, Browne J. Patient-reported outcome measures in the NHS: new methods for analysing and reporting EQ-5D data. Health Econ 2010;19:886–905 [DOI] [PubMed] [Google Scholar]
- 48. Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095–1108 [DOI] [PubMed] [Google Scholar]
- 49. Gheorghe A, Moran G, Duffy H, Roberts T, Pinkney T, Calvert M. Health utility values associated with surgical site infection: a systematic review. Value Health 2015;18:1126–1137 [DOI] [PubMed] [Google Scholar]
- 50. Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect 2017;96:1–15 [DOI] [PubMed] [Google Scholar]
- 51. European Centre for Disease Prevention and Control . Facts About Surgical Site Infections.www.ecdc.europa.eu/en/surgical-site-infections/facts (accessed 21 December 2022)
- 52. Haidich AB. Meta-analysis in medical research. Hippokratia 2010;14:29–37 [PMC free article] [PubMed] [Google Scholar]
- 53. Sackett DL. Evidence-based Medicine: How to Practice and Teach EBM (2nd edn). Edinburgh, Scotland:: Churchill Livingstone, 2000 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data generated for this review are available directly from the corresponding author.