Abstract
Background
Nighttime sleep disruptions negatively impact the experience of hospitalized patients.
Objective
To determine the impact of adopting a sleep-promoting nighttime clinical workflow for hospitalized patients on nocturnal disruptions and sleep.
Design
Survey-based pre- and post-intervention cross-sectional study using convenience samples.
Participants
Hospitalized veterans on a 23-bed general medical ward at a tertiary Veterans Administration Hospital.
Interventions
Baseline sleep surveys (N=149) identified two major sources of interruptions: blood pressure checks at 4 am for telemetry patients and subcutaneous (SQ) heparin injections between 4:30 and 6 am for venous thromboembolism prophylaxis. Clinical workflow was restructured to eliminate these disruptions: moving 4 am blood pressure checks to 6 am and providing daily SQ enoxaparin at 9 am as an alternative to Q 8-h SQ heparin, which had prompted an injection between 4:30 and 6 am. The impact of these changes was assessed in a second round of surveys (N=99).
Main Measures
Frequency and sources for nighttime sleep disruptions; percentage of patients reporting longer time to fall asleep, more interruptions, and worse sleep quality (vs. home) before and after restructuring nighttime clinical workflow.
Key Results
After restructuring nighttime clinical workflow, medication administration as a source of nighttime disruption decreased from 40% (59/149) to 4% (4/99) (p<0.001). Blood pressure checks as a source of disruption decreased from 56% (84/149) to 42% (42/99) (p=0.033). Fewer patients reported taking longer to fall asleep in the hospital vs. home (39% pre-intervention vs. 25% post-intervention, p=0.021). Similarly, fewer patients experienced waking up more frequently in the hospital vs. home (46% pre-intervention vs. 32% post-intervention, p=0.036). Fewer patients reported sleeping worse in the hospital (44% pre-intervention vs. 39% post-intervention), though this trend was not statistically significant (p=0.54).
Conclusions
Nighttime disruptions in hospitalized patients frequently interfere with sleep. Restructuring of the clinical workflow significantly reduced disruptions and improved sleep.
KEY WORDS: disruptions, noise, quality improvement, sleep, hospital
INTRODUCTION
Poor sleep is a common experience for hospitalized patients. Fragmented, non-restorative sleep engenders patient dissatisfaction with care.1,2 Furthermore, poor sleep has a direct adverse clinical impact, promoting delirium and interfering with blood pressure control.3,4 Noise and light pollution, as well as nighttime clinical activities, have been cited as reasons for poor sleep.5 One of the most frequent complaints at our teaching hospital’s weekly patient experience rounds was difficulty in getting rest at night due to noise and interruptions. In the Survey of Healthcare Experiences of Patients (SHEP), which is the Veterans Affairs (VA) version of Hospital Consumer Assessment of Healthcare Providers (HCAHPS), the question consistently posting the lowest score was as follows: “During this hospitalization, how often was the area around your room quiet at night?” In each month from May 2016 to June 2017, our score on this question at the VA Connecticut ranked below the 50th percentile, while every other question performed better.
A variety of interventions to promote sleep have been reported, mostly targeting reducing noise, light, and nighttime clinical activities in critically ill ICU patients, with variable success.6,7 More recently, increasing attention has been devoted to patients in non-ICU settings, but little has been reported about the impact of modifying nighttime disruptions on patients’ perception of sleep.1,8
In this study, we sought to identify prominent sources of nocturnal disruptions and noise by surveying hospitalized patients and examining nighttime clinical workflow. We then restructured the nighttime workflow, modifying standard clinical activities to take place outside of normal sleeping hours (11 pm–6 am), without compromising patient safety. The impact of this change on patients’ sleep was assessed by surveying hospitalized patients post-intervention, specifically determining sleep latency, frequency of nocturnal disruptions, and overall sleep quality.
METHODS
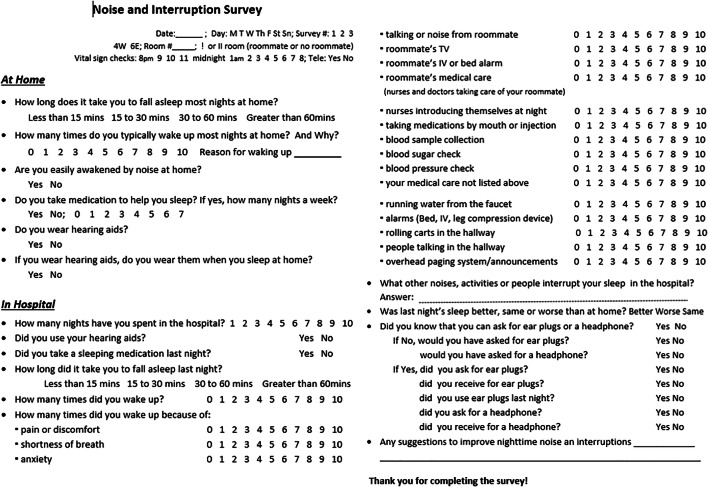
We designed a 16-question sleep survey to assess (1) the sources and magnitudes of nocturnal disruptions in the hospital and (2) their impact on sleep in the hospital compared to sleep at home (Fig. 1). Existing sleep questionnaires for hospitalized patients such as Potential Hospital Sleep Disruptions and Noises Questionnaire (PHSDNQ) are useful in identifying the sources of nocturnal disruptions and measuring their disruptiveness on sleep.2 However, the existing questionnaires do not ask respondents to directly compare sleep in the hospital vs. home. Because insomnia is prevalent in the general population, and even more so among veterans and military personnel with rates of insomnia 2–3 times higher than those in the general US adult population, we reasoned that the impact of nocturnal disruptions on sleep in the hospital could be more accurately assessed by asking respondents to compare sleep qualities in the hospital vs. at home.5,9 Thus, our survey included questions about patients’ usual sleep patterns at home in order to provide a reference point for comparison. Our surveys queried sleep latency, number of and reasons for awakenings, and overall quality of sleep during the previous night in the hospital compared to home.
Figure 1.
Sleep surveys administered to assess quality of sleep on a medical ward.
A total of 149 pre-intervention surveys were prospectively administered to hospitalized patients (57 telemetry, 91 non-telemetry) in a 23-bed general medical and surgical ward at a tertiary medical center between February and March 2018. Patients were screened each morning by nurses for their ability to complete the surveys. Those with dementia or delirium, or those who were off the floor for testing, were not surveyed. Surveyed patients who were hospitalized for more than one night were allowed to be surveyed again since the survey questions focused only on the prior night’s sleep. Because the goal was to maximize the number of unique patients surveyed, each patient was surveyed only up to 3 times. Informed by the results of the baseline surveys, we designed and implemented interventions in April 2019 to reduce nighttime disruptions. Nighttime workflow was restructured by moving the 4 am blood pressure (BP) check for telemetry patients to 6 am and adding a daily enoxaparin injection at 9 am for venous thromboembolism (VTE) prophylaxis as an alternative to q 8-h subcutaneous (SQ) heparin injections (scheduled for 6 am, 2 pm, 10 pm). New order sets were created in our electronic medical records (CPRS) to reflect these changes.
The housestaff were informed about the new order sets and were encouraged to consider the impact of nighttime orders on sleep and to place orders outside sleep hours when clinically safe. The nursing staff were also educated about the rationale for restructuring the clinical workflow and were encouraged to avoid giving medications before the scheduled times in the morning.
In order to assess the impact of these changes, a second round of 99 surveys (45 telemetry, 54 non-telemetry) was completed post-intervention in the same ward during July–August 2019. The 2-proportion Z-test was used to compare pre- and post-intervention groups, specifically comparing sleep latency, frequency of nocturnal disruptions, and overall sleep quality.
RESULTS
Baseline sleep characteristics of hospitalized patients in the pre-intervention and post-intervention cohorts are summarized in Table 1. The two cohorts had similarly poor sleep qualities at baseline. Long sleep latency was common, with 32% reporting sleep latency of greater than 30 min. Nocturnal awakenings were frequent with nearly 70% reporting waking up two or more times a night, mostly to urinate. More than half of patients described themselves as being easily woken by noise. More than a third were taking a sleep medication at home.
Table 1.
Baseline Sleep Quality at Home
| Pre-intervention cohort (N=149) | Post-intervention cohort (N=99) | ||||
|---|---|---|---|---|---|
| Percent responding (# respondents/total) |
Proportion responding (# respondents) |
Percent responding (# respondents/total) |
Proportion responding (# respondents) |
||
| Time to fall asleep | <15 min | 100% (148/149) | 32% (48) | 100% (99/99) | 41% (41) |
| 15–30 min | 35% (52) | 26% (26) | |||
| 30–60 min | 20% (30) | 22% (22) | |||
| >60 min | 12% (18) | 10% (10) | |||
| # of times typically woken | 0 | 99% (147/149) | 9% (13) | 99% (98/99) | 4% (4) |
| 1 | 19% (28) | 29% (28) | |||
| 2 | 31% (46) | 29% (28) | |||
| 3 | 24% (35) | 24% (24) | |||
| 4 | 10% (15) | 4% (4) | |||
| 5 | 4% (6) | 4% (4) | |||
| 6 | 3% (4) | 1% (1) | |||
| ≥7 | 0% (0) | 5% (5) | |||
| Easily woken by noise | Yes | 99% (147/149) | 43% (63) | 99% (98/99) | 43% (42) |
| No | 57% (84) | 57% (56) | |||
| Do you take medications to help you sleep? | Yes | 99% (147/149) | 38% (56) | 100% (99/99) | 35% (35) |
| No | 62% (91) | 65% (64) | |||
| If you take sleep medication, how many nights a week do you take it? | 1 | 98% (55/56)a | 16% (9) | 100% (35/35)c | 9% (3) |
| 2 | 9% (5) | 6% (2) | |||
| 3 | 5% (3) | 6% (2) | |||
| 4 | 2% (1) | 0% (0) | |||
| 5 | 0% (0) | 3% (1) | |||
| 6 | 0% (0) | 0% (0) | |||
| 7 | 67% (37) | 77% (27) | |||
| Do you wear hearing aids? | Yes | 100% (149/149) | 17% (25) | 100% (99/99) | 27% (27) |
| No | 83% (124) | 73% (72) | |||
| If yes, do you wear them while sleeping? | Yes | 100% (25/25)b | 16% (4) | 100% (27/27)d | 0% (0) |
| No | 84% (21) | 100% (27) | |||
aOf 56 respondents who answered yes to taking a sleep medication, 55 responded to the follow-up question about the frequency of medication.
bN = 25 patients that responded “Yes” to wearing hearing aids
cN = 35 patients that responded “Yes” to taking sleep medications
dN = 27 patients that responded “Yes” to wearing hearing aids
A total of 149 pre-intervention surveys were completed with 107 patients surveyed once, 32 patients surveyed twice, and 10 patients surveyed three times. As shown in Table 2, the most frequent causes of nocturnal disruptions were blood pressure (BP) checks (56% of surveys (84/149)) and medication administration (40% (59/149)), both in the category of medical care. Other frequent causes of nocturnal interruptions were as follows: noise from hallway (39% (58/149)); blood collection (35% (52/149)); pain (34% (51/149)); and nurses introducing themselves at shift changes at midnight (30% (45/149)). As summarized in Table 3, compared to sleep at home, the patients in the pre-intervention cohort experienced longer sleep latency (39% of those surveyed), more frequent disruptions (46% surveyed), and overall decline in sleep quality (44%) in the hospital. Telemetry patients were much more likely to experience nighttime disruptions than non-telemetry patients: 51% of telemetry vs. 32% non-telemetry patients reported longer sleep latency, 62% of telemetry vs. 36% of non-telemetry patients reported more disruptions, and 51% of telemetry vs. 39% non-telemetry patients reported worse sleep.
Table 2.
Sources of Nocturnal Disruptions After at Least One Night in the Hospital
| Pre-intervention cohort (N=149) | Post-intervention cohort (N=99) | p-value | |
|---|---|---|---|
| Medical care | |||
| Blood pressure checks | 56% | 42% | 0.03 |
| Medication administrations | 40% | 4% | <0.001 |
| Blood draws | 35% | 18% | 0.004 |
| RN introduction at 12 am shift change | 30% | 0% | <0.001 |
| Blood glucose finger sticks | 20% | 4% | <0.001 |
| Roommate | |||
| Noise (talking/TV) | 13% | 4% | 0.026 |
| Medical care | 12% | 11% | NS |
| Environmental | |||
| Talking in hallway | 23% | 16% | NS |
| Carts in hallway | 16% | 4% | 0.006 |
| IV alarms | 10% | 2% | 0.03 |
| Overhead alarm | 5% | 0% | 0.048 |
| Patients’ symptoms | |||
| Pain | 34% | 24% | NS |
| Anxiety | 16% | 6% | 0.02 |
| Shortness of breath | 10% | 4% | NS |
Values refer to the percentage of pre-intervention surveys (N=149) and post-intervention surveys (N = 99) reporting that particular nocturnal disruption
Table 3.
Impact of Rescheduling Vital Sign Monitoringa and Venous Thromboembolism Prophylaxis Injectionsb on Patients’ Perception of Sleep in the Hospital vs. at Home
| Pre-intervention cohort (N = 149) Proportion responding (# respondents/total) |
Post-intervention cohort (N = 99) Proportion responding (# respondents/total) |
p-value | ||
|---|---|---|---|---|
| Longer sleep latency | All | 39% (56/143) | 25% (24/97) | 0.02 |
| Telemetry | 51% (28/55) | 22% (10/45) | 0.003 | |
| Non-telemetry | 32% (28/87) | 27% (14/52) | NS | |
| More nocturnal disruptions | All | 46% (67/147) | 32% (31/97) | 0.034 |
| Telemetry | 62% (34/55) | 27% (12/44) | <0.001 | |
| Non-telemetry | 36% (33/91) | 36% (19/53) | NS | |
| Worse sleep | All | 44% (58/131) | 39% (39/99) | NS |
| Telemetry | 51% (26/51) | 40% (18/45) | NS | |
| Non-telemetry | 39% (31/79) | 39% (21/54) | NS | |
aBlood pressure measurement was rescheduled to occur 2 h later at 6 am, instead of 4 am. bVenous thromboembolism prophylaxis was simplified to a single enoxaparin injection at 9 am vs. TID injections of heparin at 6 am, 2 pm, and 10 pm.
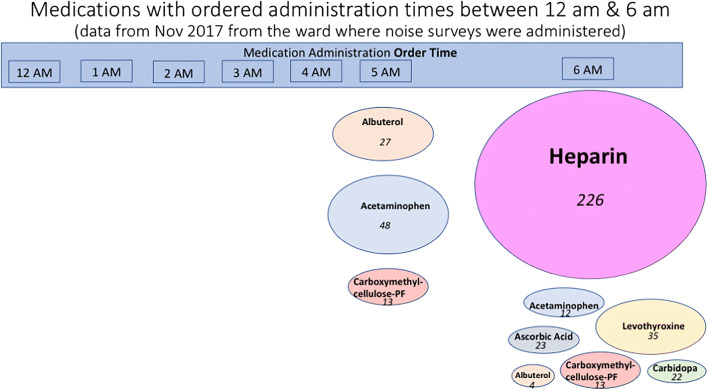
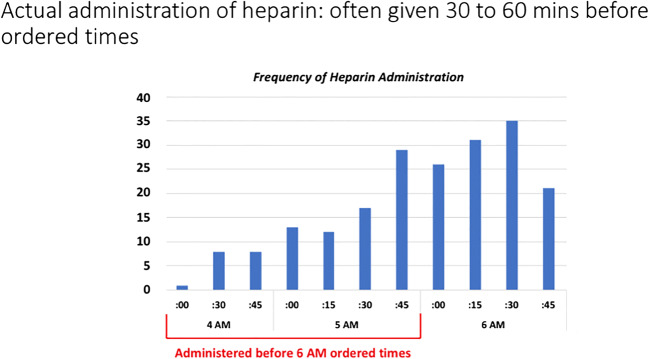
We investigated why BP checks and medication administrations were causing such frequent sleep disruptions. Vital signs were being checked three times a day (12 am, 8 am, and 4 pm) for non-telemetry patients and six times a day for telemetry patients (12 am, 4 am, 8 am, 12 pm, 4 pm, and 8 pm). The 4 am vital sign check was waking up telemetry patients every night while the 12 am vital sign check was contributing to longer sleep latency and more frequent nocturnal awakenings for both telemetry and non-telemetry patients. We reviewed medications that were ordered between 12 am and 6 am in the month of November 2017 on the same ward where sleep surveys were later administered. We found that SQ heparin injections for VTE prophylaxis were the medications most commonly ordered between 12 am and 6 am (Fig. 2). When actual administration times for heparin were reviewed, we found that heparin injections were often administered 30–90 min before the ordered time of 6 AM, resulting in injections as early as 4 am (Fig. 3). Per nursing and pharmacy policy, a medication could be given up to 90 min before or after the ordered time. Administration times for a TID dosing schedule were 6 am, 2 pm, and 10 pm, therefore allowing TID medications to be administered before 6 am.
Figure 2.
Medications and their administration times between 12 am and 6 am prior to intervention.
Figure 3.
Actual administration times for heparin subcutaneous injections scheduled for 6 am.
The pre-intervention surveys clearly identified an opportunity for improvement in sleep quality for hospitalized patients. We designed an intervention to address the two leading causes of sleep disruptions in our hospital: vital sign checks at 4 am and heparin injections before 6 am. The goal of our intervention was to reduce the disruptions of sleep from planned routine clinical activities between midnight and 6 am in order to preserve the natural circadian rhythm. Nursing, pharmacy, and hospitalist services all collaborated in the design and implementation of the intervention, which consisted of two components: (1) moving blood pressure checks for telemetry patients from 4 am to 6 am and (2) making daily enoxaparin injections available as an alternative to TID heparin injections for VTE prophylaxis. The timing of TID orders was changed from 6 am, 2 pm, and 10 pm to 7 am, 2 pm, and 9 pm in our electronic medical records to avoid giving medications before 6 am. After the intervention, the proportion of patients receiving daily enoxaparin for VTE prophylaxis significantly increased from 16% (11 patients receiving enoxaparin vs. 58 patients receiving heparin in Nov 2017) to 48% (48 patients receiving enoxaparin vs. 52 patients receiving heparin in July and Aug 2019, p < 0.001).
After implementation of the restructured nighttime clinical workflow, 99 post-intervention surveys were completed with 65 patients surveyed once, 24 patients surveyed twice, and 10 patients surveyed three times. Post-intervention surveys showed considerable improvement in the patients’ perception of nighttime disruptions and sleep. Medication administration became an infrequent source of nighttime disruption (4% (4/99) in post-surveys vs. 40% (59/149) in pre-surveys; p < 0.001) (Table 2). BP checks were also reported less frequently as a source of nocturnal disruption (42% (42/99) post-surveys vs. 56% (84/149) pre-surveys; p = 0.04). As shown in Table 3, 25% of post-intervention patients (vs. 39% of pre-intervention patients) reported taking longer to fall asleep in the hospital than at home. 32% of post-intervention (vs. 46% of pre-intervention patients) reported more frequent awakenings in the hospital. 39% of post-intervention patients (vs. 44% of pre-intervention patients) reported sleeping worse in the hospital.
The beneficial impact of the restructured nighttime clinical workflow on patients’ perceptions of nighttime disruptions and sleep was more pronounced in telemetry patients (Table 3). For example, 22% of post-intervention telemetry patients (vs. 51% of pre-intervention telemetry patients; p = 0.003) reported taking longer to fall asleep in the hospital than at home. For non-tele patients, there was no significant difference pre- and post-intervention in terms of longer sleep latency in the hospital compared to home. 27% of post-intervention (vs. 62% of pre-intervention; p < 0.001) telemetry patients reported more frequent awakenings in the hospital. In contrast, the percentage of non-telemetry patients reporting more frequent awakenings in the hospital remained unchanged (36% pre-intervention vs. 36% post-intervention). 40% of post-intervention telemetry patients (vs. 51% pre-intervention patients) reported sleeping worse in the hospital, although the difference did not reach statistical significance.
DISCUSSION
We found that standard clinical activities such as vital sign checks and medication administrations were routinely taking place during normal sleeping hours (11 pm–6 am) and interrupting sleep, especially among telemetry patients. Telemetry patients had twice the frequency of BP checks as non-tele patients, including checks at 12 am, 4 am, and 8 am, not allowing for continuous sleep. Many providers were not aware of this practice of collecting vital signs every 4 h, which has been an ongoing practice since 1893 with little evidence to support it, and some have advocated for using the Modified Early Warning Score to identify low-risk patients to forgo overnight vital sign monitoring.10,11
Upon analysis of medication administrations ordered between 12 am and 6 am in November 2017 on the ward that was later surveyed, we found that prophylactic heparin was the most frequently administered medication (Fig. 2). Heparin injections were often given 30–60 min before ordered times, resulting in injections as early as 4 am (Fig. 3). By replacing subcutaneous heparin injections with once-daily enoxaparin injections at 9 am, patients reporting disruptions due to medication administration decreased 10-fold. No adverse events were noted. Prior meta-analysis comparing low molecular weight heparin to unfractionated heparin showed no significant differences in deep venous thrombosis, pulmonary embolism, death, or major bleeding.12 Cost did not increase, as our cost of three injections of heparin at $2.04 per day ($0.69 per dose) was nearly the same as the cost of a single dose of enoxaparin at $2.07.
Overall, restructuring modifiable clinical activities to occur outside normal sleeping hours significantly reduced patients’ perceptions of sleep latency and nocturnal disruptions. This improvement was most pronounced in telemetry patients, who also experienced improvement in overall sleep quality.
There were several limitations to the study. First, a convenience sample from an observational study was used and the sample size was constrained, as survey administration was limited to general ward patients (not ICU or stepdown) deemed capable of completing them, who were on the floor at the time of surveying and willing to participate. Sleep was assessed via subjective patient responses to our custom-designed survey rather than a well-validated tool such as the Pittsburgh Sleep Quality Index or objective measures such as actigraphy which has been used in some other studies.1,2 Surveys were administered to different groups of patients pre- and post-intervention, separated in time. Additionally, surveying patients more than once can introduce confounding factors: a prior study showed that improvements in sleep resulting from an intervention became more pronounced with subsequent nights in the hospital.1 Strengths of this pilot study are its simple design and intervention requiring no added cost. The interventions improved sleep quality and duration, and they can easily be adapted and modified at other institutions. Many providers do not inquire about a patient’s sleep and are not even aware of all the nocturnal disruptions that are occurring and detrimental to the health of their patients.13 This quality improvement project calls attention to this commonly neglected issue and demonstrates that meaningful improvement can be achieved.
CONCLUSIONS
Nighttime interruptions in hospitalized patients frequently interfere with sleep. Restructuring standard nocturnal workflow significantly reduced interruptions and improved sleep. Consequently, hospitals should identify and assess nocturnal disruptions caused by modifiable standard clinical activities and consider moving vital sign monitoring and medication administration outside of normal sleeping hours to minimize nocturnal disruptions.
Declarations
The project was deemed a quality improvement initiative by the Research Office which waived further review by our institutional review board.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior Presentations
Oral presentation at SGIM New England Regional Conference at Harvard Medical School, 11/2019.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gathecha E, Rios R, Buenaver LF, Landis R, Howell E, Wright S. Pilot study aiming to support sleep quality and duration during hospitalizations. J Hosp Med. 2016;11(7):467-72. 10.1002/jhm.2578. [DOI] [PubMed]
- 2.Grossman MN, Anderson SL, Worku A, Marsack W, Desai N, Tuvilleja A, et al. Awakenings? Patient and hospital staff perceptions of nighttime disruptions and their effect on patient sleep. J Clin Sleep Med. 2017;13(2):301-6. 10.5664/jcsm.6468. [DOI] [PMC free article] [PubMed]
- 3.Arora VM, Chang KL, Fazal AZ, Staisiunas PG, Meltzer DO, Zee PC, et al. Objective sleep duration and quality in hospitalized older adults: associations with blood pressure and mood. J Am Geriatr Soc. 2011;59(11):2185-6. 10.1111/j.1532-5415.2011.03644.x. [DOI] [PMC free article] [PubMed]
- 4.Figueroa-Ramos MI, Arroyo-Novoa CM, Lee KA, Padilla G, Puntillo KA. Sleep and delirium in ICU patients: a review of mechanisms and manifestations. Intensive Care Med. 2009;35(5):781-95. 10.1007/s00134-009-1397-4. [DOI] [PubMed]
- 5.Arora VM, Stewart N. Sleep in hospitalized older adults. Sleep Med Clin. 2018; 13(1):127-135. [DOI] [PMC free article] [PubMed]
- 6.Hu R, Jiang X, Chen J, Zeng Z, Chen XY, Li Y, Huining X, Evans DJW. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane Database Syst Rev. 2015; (10) Art. No.: CD008808. [DOI] [PMC free article] [PubMed]
- 7.Dubose JR, Khatereh H. Improving inpatient environments to support patient sleep. Int J Qual Health Care. 2016;28(5), 540-553. [DOI] [PubMed]
- 8.Arora VM, Machado N, Anderson SL, et al. Effectiveness of SIESTA on objective and subjective metrics of nighttime hospital sleep disruptors. J Hosp Med. 2019;14:138–41. 10.12788/jhm.309110.12788/jhm.3091. [DOI] [PubMed]
- 9.Hughes JM, Ulmer CS, Gierisch JM, Hastins SN, Howard MO. Insomnia in United States Military Veterans: an integrated theoretical model. Clin Psychol Rev. 2018; 59: 118-127 10.1016/j.cpr.2017.11.005. [DOI] [PMC free article] [PubMed]
- 10.Yoder JC, Yuen TC, Churpek MM, Arora VM, Edelson DP. A prospective study of nighttime vital sign monitoring frequency and risk of clinical deterioration. JAMA Intern Med. 2013;173(16):1554-5. 10.1001/jamainternmed.2013.7791. [DOI] [PMC free article] [PubMed]
- 11.Orlov NM, Arora VM. Things we do for no reason: routine overnight vital sign checks. J Hosp Med. 2020; 15(5): 272-274. [DOI] [PMC free article] [PubMed]
- 12.Phung OJ, Kahn SR, Cook DJ, Murad MH. Dosing frequency of unfractionated heparin thromboprophylaxis: a meta-analysis. Chest. 2011;140(2):374-81. 10.1378/chest.10-3084. [DOI] [PubMed]
- 13.Meissner HH, Riemer A, Santiago SM, Stein M, Goldman MD, Williams AJ. Failure of physician documentation of sleep complaints in hospitalized patients. West J Med. 1998;169(3):146-9. [PMC free article] [PubMed]