Abstract
Vanishing bile duct syndrome is a rare, acquired disease that has been described in different pathologic conditions‚ including adverse drug reactions, autoimmune diseases, graft vs host disease, and neoplasms. It is a condition characterized by progressive loss of intrahepatic bile ducts leading to ductopenia and cholestasis.
Here we report a 27-year-old female who presented with jaundice and cholestatic hepatitis and was finally diagnosed with vanishing Bile duct syndrome secondary to Hodgkin lymphoma.
Physicians need to consider a range of differential diagnoses, especially malignancies, in suspected cases of vanishing bile duct syndrome.
Keywords: Vanishing bile duct syndrome, Hodgkin's lymphoma, Cholestasis, Ductopenia
Introduction
Jaundice in patients with lymphoma has different causes‚ such as intra and extrahepatic bile duct obstruction‚ viral hepatitis‚ and hepatic infiltration by lymphoma cells [1]. Vanishing bile duct syndrome (VBDS) is a rare but serious consequence of Hodgkin's lymphoma and is clinically characterized by chronic cholestasis [2]. It's a ductopenic liver disease and was proven by liver biopsy and immunostaining for CK7 and CK 19 in specimens [3]. The prognosis depends on biliary epithelial regeneration. Recovery can occur over time, but irreversible bile duct injuries lead to biliary cirrhosis or hepatic failure [4]. VBDS has been described in different pathologic conditions‚ including adverse drug reactions, autoimmune diseases, graft vs host disease, and neoplasms. Usually‚ is diagnosed as a complication of primary pathology [5]. But in this article, we present a 27-year-old female with jaundice as a primary presentation of VBDS‚ which finally led to a diagnosis of Hodgkin's lymphoma stage 3B and a fatal outcome.
Case report
A 27-year-old woman was referred to our center complaining of jaundice and itching a month ago, along with generalized abdominal pain, nausea “non-bloody vomiting,” weakness, and weight loss of 5 kg. She was infected with COVID-19 about 6 months ago and was also treated with prednisolone 5 mg daily since 5 months ago due to subacute thyroiditis. The patient had been using ursodeoxycholic acid “famotidine montelukast hydroxyzine‚” and doxepin prescribed by a general practitioner for itching. She does not drink alcohol and does not smoke, and had no recent trips or family history of liver diseases. Laboratory tests showed an increase in liver enzymes, such as AST 96 U/L (NV < 35)‚ ALT 116 U/L (NV < 35)‚ ALP 1244 U/L (NV < 150)‚GGT 162 U/L (NV < 30)‚ total bilirubin 17.6 mg/dL (NV < 1.2)‚ direct bilirubin 10.6 (NV < 0.2). PT, PTT and INR were normal. The hemogram showed microcytic anemia with increased Ferritin and decreased TIBC (WBC = 4400 Hb = 7.9, MCV = 69.5, Plt = 371,000, Ferritin = 417 [NV = 10-124]‚ TIBC = 197 [250-450]). Thyroid function tests‚ viral hepatitis serologies‚ and other infectious disease panels‚ including HIV‚ CMV‚ and mononucleosis‚ were negative. Serum Ceruloplasmin‚ urine copper level‚ and serum protein electrophoresis were normal. ANA‚ Anti-dsDNA‚ ASMA‚ AMA‚ P-ANCA‚ C-ANCA and anti-LKM-1 were normal. An abdominal ultrasound and spiral CT scan showed multiple small lesions in the spleen and some porta hepatis‚ portocaval ‚and paraaortic lymphadenopathies with maximum SAD = 15 mm (Fig. 1). Due to the lesions seen in spleen and abdominal lymphadenopathies‚ which were suspicious for lymphomatous involvement‚ spiral neck and chest CT scans were performed and showed multiple cervical‚ mediastinal and right paratracheal lymphadenopathies (Fig. 2). The liver and biliary ducts were normal in ultrasound and MRCP.
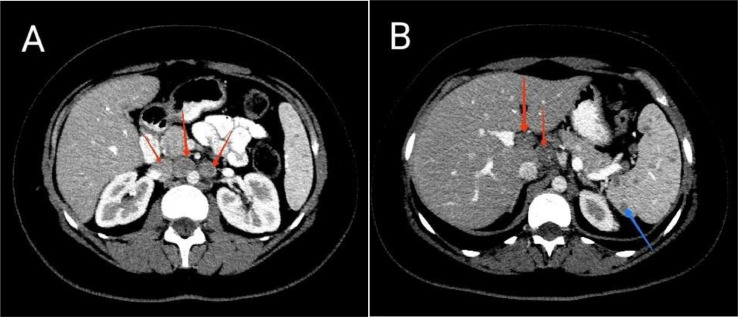
Fig. 1.
Axial section Abdominal CT scan with IV contrast. (A) Paraaortic and aortocaval lymphadenopathy (red arrows). (B) Porta hepatis lymphadenopathy (red arrows) and multiple hypodense splenic lesions (blue arrow).
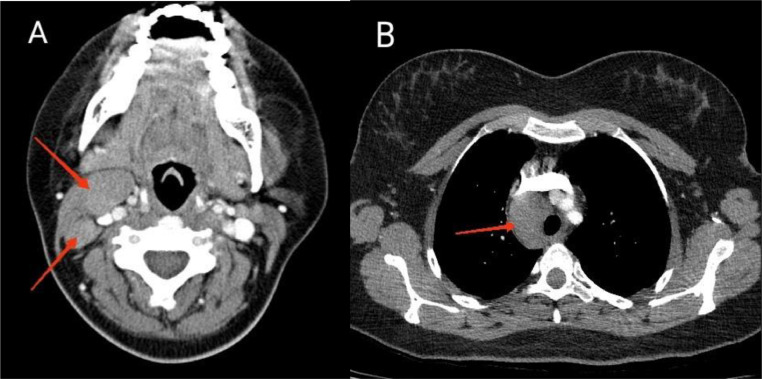
Fig. 2.
Axial section Neck and Chest CT scan with IV contrast showing (A) Neck and (B) mediastinal lymphadenopathy (red arrows).
Core needle biopsy of cervical lymphadenopathy was performed, and histological analysis revealed multiple stripes of lymphoid tissue with occasional scattered large, atypical cells in the background of small mature lymphocytes admixed with scattered occasional eosinophils which were positive for CD30 and CD15 on immunohistochemistry stains. Overall morphological and IHC findings were suggestive of classic Hodgkin lymphoma. Also‚ due to intrahepatic cholestasis and the normality of other additional laboratory tests‚ percutaneous liver biopsy was done. It showed liver tissue with bile duct paucity and mild inflammation‚ confirmed with immunostaining for CK7 and CK19. No interface hepatitis‚ confluent necrosis‚ fibrosis‚ and steatosis were identified. Liver histology findings were compatible with vanishing bile duct syndrome secondary to Hodgkin lymphoma as a paraneoplastic manifestation (Fig. 3). The bone marrow biopsy was negative for lymphoma involvement.
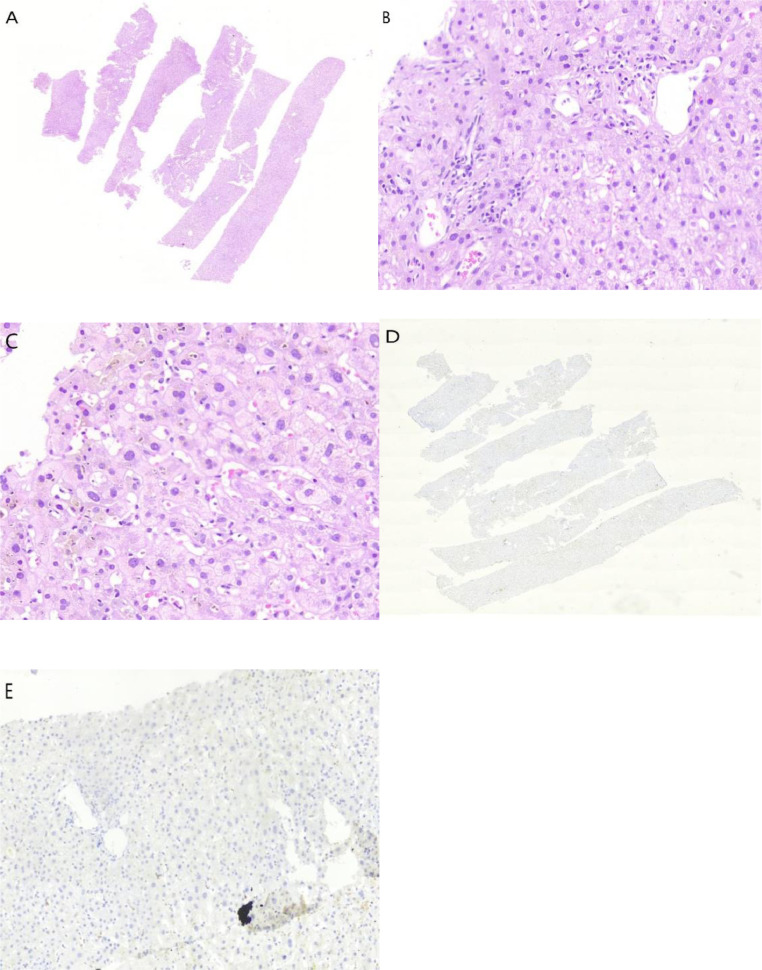
Fig. 3.
Liver biopsy. (A) Liver tissue with relatively preserved architecture and no significant necroinflammation (H&E‚ × 4). (B) No interlobular bile duct was noted in most portal tracts (H&E). (C) scatter bile plugs are seen in the liver parenchyma. (D) immunostaining for CK 19 confirms the absence of interlobular bile duct in most portal tracts (IHC ‚ × 4). (E) immunostaining for CK 19 confirms the absence of interlobular bile duct and ductular proliferation (IHC).
In follow up patient underwent chemotherapy. Liver enzymes and bilirubin didn't decrease‚ and finally, she died of liver failure after about 2 months.
Discussion
The association of Hodgkin's lymphoma with VBDS causes poor prognosis‚ and patients with VBDS generally don't survive even when hepatic failure doesn't occur. Although the prognosis depends on the underlying disease because intrahepatic bile ducts don't have high regeneration capacity‚ injured biliary ducts lead to irreversible damage and hepatic failure [6]. In Bakhit et al. case report article and literature review‚ a total of 51 Hodgkin's related VBDS cases from 1962 to 2014 were studied. Most patients died (60%). The most common causes of death were hepatic failure and sepsis‚ respectively‚ like our patient [4]. In the Wong et al. [1] article‚ 13 out of 23 patients (53%) died ‚mostly because of hepatic failure and sepsis. Also‚ in Ballonof et al. literature review‚ 65% (24/37) of patients died‚ mostly from liver failure [7]. The basis of treatment is treating the underlying disease. There are different treatment options‚ such as chemotherapy alone‚ chemotherapy and radiotherapy with or without steroids [1]. Some patients die because of liver failure despite lymphoma remission. So liver transplantation should be considered in addition to medical therapy. Aleem et al. reported a 33-year-old male patient diagnosed with Hodgkin's lymphoma-related vanishing bile duct syndrome and finally died due to hepatic encephalopathy despite lymphoma remission [8]. Therefore, some authors believe patients should be prepared for liver transplantation followed by chemotherapy regardless of remission. Although the role of liver transplantation due to limited data is unclear‚ and it remains controversial [4,7,9]. In summary‚ long-term follow-up is needed to monitor for the recurrence of lymphoma‚ liver function and biopsy after treatment to evaluate the clinical course and biliary duct regeneration capacity. Like most cases‚ our patient presented with symptoms of jaundice‚ pruritus‚ and weight loss. The important point is multiple splenic hypoechoic lesions in ultrasound as the first modality‚ which is one of the manifestations of splenic lymphoma involvement. On the other hand, liver imaging modalities‚ including liver ultrasound‚ computed tomography‚ and MRCP‚ were normal.
Conclusion
In conclusion‚ this case highlights that VBDS can precede the diagnosis of Hodgkin's lymphoma‚ and it's important to investigate this syndrome and underlying malignancies in patients with cholestatic hepatitis and normal liver imaging modalities.
Patient consent
We obtained written informed consent from the patient when she was alive to prepare this case report.
Footnotes
Acknowledgments: This study was not funded.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Wong k.-M., Chang Ch.-S., Wu Ch.-Ch, Yin Hs.-L. Hodgkin's lymphoma-related vanishing bile duct syndrome: a case report and literature review. The Kaohsiung Journal of Medical Sciences. 2013;29(11):636–641. doi: 10.1016/j.kjms.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin W.-C., Hsieh T.-S., Chu C.-Y. Case report: Development of vanishing bile duct syndrome in Stevens-Johnson syndrome complicated by hemophagocytic lymphohistiocytosis. Frontiers in Medicine. 2022;9:3201. doi: 10.3389/fmed.2022.975754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jia Y., Liu L., Deng B., Huang Y., Zhao J., Bai G. Atypical primary biliary cholangitis results in vanishing bile duct syndrome with cutaneous xanthomas: a case report. Diagnostic Pathology. 2022;17(1):57. doi: 10.1186/s13000-022-01228-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bakhit M., McCarty Th.-R Park S., Njei B., Cho M., Karagozian R. Vanishing bile duct syndrome in Hodgkin's lymphoma: A case report and literature review. World Journal of Gastroenterology. 2017;23(2):366. doi: 10.3748/wjg.v23.i2.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anugwom C., Goetz G., Hassan M. Vanishing bile duct syndrome preceding the diagnosis of Hodgkin lymphoma. ACG Case Reports Journal. 2020;7(2) doi: 10.14309/crj.0000000000000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kun P.-A., McLin Valerie A., Rushton Jennifer R., Kearney Debra L., Hasting Caroline A., Margolin Judith F. Vanishing bile duct syndrome and Hodgkin disease: a case series and review of the literature. Journal of pediatric hematology/oncology. 2008;30(12):976–980. doi: 10.1097/MPH.0b013e31818b37c4. [DOI] [PubMed] [Google Scholar]
- 7.Ballonoff A., Kavanagh B., Nash R., Drabkin H., Trotter J., Costa L., et al. Hodgkin lymphoma-related vanishing bile duct syndrome and idiopathic cholestasis: statistical analysis of all published cases and literature review. Acta Oncologica. 2008;47(5):962–970. doi: 10.1080/02841860701644078. [DOI] [PubMed] [Google Scholar]
- 8.Aleem A., Al‑Katari M., Alsaleh Kh., AlSwat Kh., Al‑Sheikh A. Vanishing bile duct syndrome in a hodgkin's lymphoma patient with fatal outcome despite lymphoma remission. Saudi Journal of Gastroenterology: Official Journal of the Saudi Gastroenterology Association. 2013;19(6):286. doi: 10.4103/1319-3767.121037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rossini M.-S., Lorand-Metze I., Oliveira G.-B., De Souza C.-A. Vanishing bile duct syndrome in Hodgkin's disease: case report. Sao Paulo Medical Journal. 2000;118:154–157. doi: 10.1590/S1516-31802000000500008. [DOI] [PMC free article] [PubMed] [Google Scholar]