Abstract
Lag screw positioning can be difficult to discern intraoperatively on lateral fluoroscopic imaging during intramedullary fixation of proximal femur fractures in some nailing systems due to the drill guide handle obstructing the view. We have described a method of obtaining non-obstructed lateral-oblique “peek” views that reliably assist in obtaining adequate tip-apex distance (TAD) measurements when using intramedullary fixation for these fractures. The purpose of this study was (1) to describe an intraoperative radiographic technique to obtain non-obscured views for appropriate center-center placement of the lag screw(s) within the femoral head during jig-aided cephalomedullary nailing of peritrochanteric hip fractures and (2) to present a case series detailing the radiographic results using this technique. This clinical series of sixty-five patients with intertrochanteric or subtrochanteric proximal femur fractures stabilized with a cephalomedullary nail had an average TAD of 15.1 ± 3.3mm (range: 9.4mm–26.2mm). This suggests that our technical trick of obtaining “peek” radiographs intraoperatively may aid in a precise lag-screw placement.
Keywords: Tip-apex distance, Cephalomedullary nail, Radiograph, Peek, Femur fracture, Intramedullary nail
1. Introduction
Fixation of peritrochanteric fractures is often accomplished with cephalomedullary nails.1 Fixation failure is most often due to cutting-out of the lag screw from the femoral head and varus collapse.3 Almost all instances of cut-out require revision surgery.5 The tip-apex distance (TAD), which indicates the position and depth of the screw in the femoral neck and head, has been consistently shown to be the strongest predictor of fixation failure, specifically a TAD greater than 25 mm.2,4,5 One potential obstacle to obtaining appropriate TAD involves the inability to properly visualize the location of the guide wire within the femoral head on the lateral view using intraoperative fluoroscopy secondary to obstruction from the insertion jig.
Herein, we present a technical trick to aid in the visualization of guide wire and lag screw(s) placement within the femoral head, when utilizing insertion guides that obscure the final screw placement in the femoral head [Fig. 1A and B]. To demonstrate the precision provided by this technique, we include a series of patients in whom this technical trick was used.
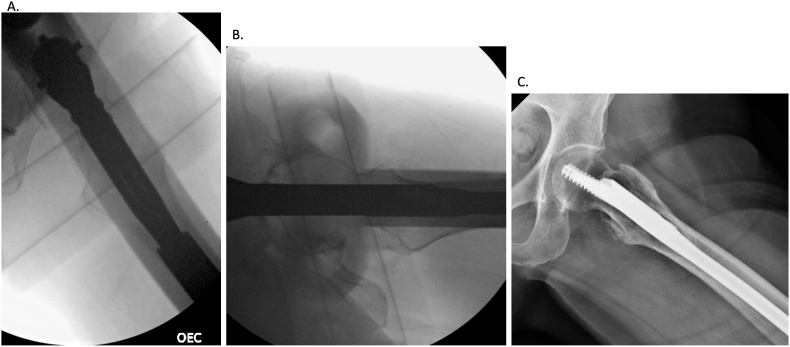
Fig. 1.
A, B, C: Intraoperative C-arm imaging showing a perfect lateral radiograph with the fracture reduced and jig partially (A) or fully (B) obscuring the femoral head. The femoral head, neck, shaft, nail and jig should ideally be aligned to estimate the position of the lag screw. If the alignment shows the position will be off-centered, then rotational adjustments can be made. (C) A perfect lateral radiograph, defined as the femoral head, neck and shaft aligned, while the fracture is reduced. This radiograph is necessary to obtain in order to measure an accurate tip-apex distance after lag screw placement.
2. Case report
We retrospectively identified all patients who received intramedullary fixation of an intertrochanteric or subtrochanteric fracture performed by a single fellowship-trained orthopaedic trauma surgeon, between September 2016 and February 2020. Inclusion criteria were all patients with a proximal femur fracture fixed with a TRIGEN™ INTERTAN™ or META-TAN™ Antegrade Nail (Smith & Nephew; Memphis, Tennessee), who had appropriate postoperative anteroposterior (AP) and lateral hip radiographs.
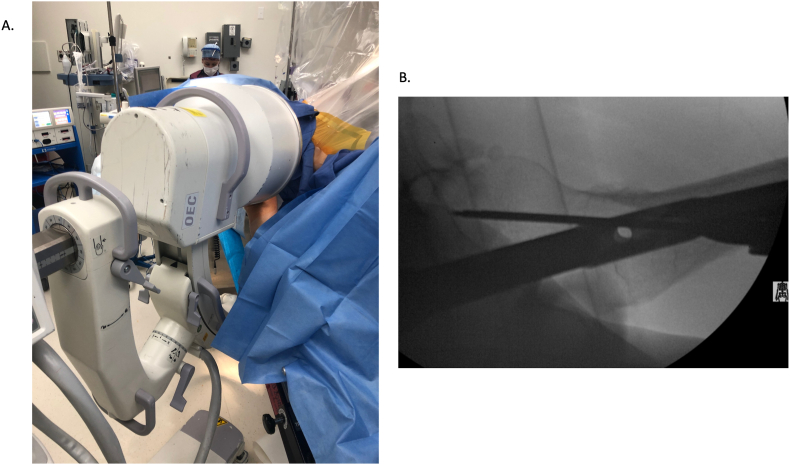
Antegrade cephalomedullary nailing was performed in the supine position, with the legs scissored on a fracture top table or in the lateral position on a radiolucent table for all patients included in this series. The technique will be described as it relates to the supine position. After reduction maneuvers are employed, standard trochanteric nailing was performed by obtaining a starting portal at or medial to the tip of the greater trochanter on the AP and in line with the femoral head, neck, and shaft on the perfect lateral radiograph (the head, neck, shaft, nail, and guide all in line) [Fig. 1C]. With a reduced fracture, the typical angulation required of the C-arm to obtain a perfect lateral X ray is between 70 and 80° off of the AP projection. The intersection of the guidewire and the subchondral bone of the femoral head on lateral radiographs will approximate the position of the cephalomedullary screw when the guidewire is appropriately positioned within the starting portal [Fig. 2A and B]. After obtaining the starting portal, the nail is seated on the AP projection. Then, the jig is aligned with the nail on the perfect lateral radiograph [Fig. 1 A,B], providing an estimate of the lag screw(s) trajectory within the femoral head and neck. The cephalomedullary guide wire can then be placed. The lateral-oblique “peek” radiograph views allow the surgeon to see around the nail and insertion guide for better visualization of the guide wire within the femoral neck head and are obtained by rotating the C-arm 10–15°off the perfect lateral in both directions. Angulation toward the AP view will provide visualization of the guide wire insertion with relation to the posterior femoral head and neck [Fig. 3A and B]. Angulation toward the horizontal from the perfect lateral view will provide visualization of the guide wire insertion in relation to the anterior femoral head and neck [Fig. 4A and B]. The visualization of the anterior “peek” is more difficult as the contralateral limb can start to obscure the image. It is ideal to have equal distances between the anterior and posterior femoral neck on the “peek” radiographs. Drilling and placement of the lag screw(s) is then performed in the usual fashion.
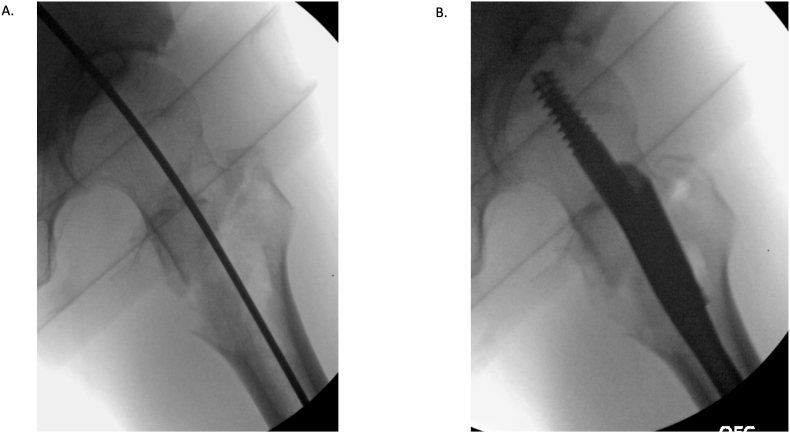
Fig. 2.
A. Intraoperative C-arm lateral radiograph showing the intersection of the guide wire and the subchondral bone of the femoral head. The guide wire position will approximate the location of the cephalomedullary screw when the guide wire is appropriately positioned in the starting portal. B. Intraoperative C-arm lateral radiograph showing appropriate cephalomedullary screw placement in the same position of the guidewire.
Fig. 3.
“Peek” radiograph technique. A. Intraoperative C-arm positioning - obtained by rotating the C-arm 10–15° off of the perfect lateral radiograph toward the AP view to visualize the posterior femoral neck. B. Visualization of the guidewire in relation to the posterior femoral neck.
Fig. 4.
“Peek” radiograph technique. A. Intraoperative C-arm positioning - obtained by rotating the C-arm 10–15° off of the perfect lateral radiograph toward the horizontal to visualize the anterior femoral neck. B. Visualization of the guidewire in relation to the anterior femoral neck.
In our case series, the distance from the tip of the lag screw to the apex of the femoral head was measured on immediate postoperative AP and lateral x-rays for each patient.6 A total of 65 patients were included in the study. The average TAD obtained using the “peek” technique was 15.1 ± 3.3mm (range: 9.4mm–26.2mm). The majority of these measurements were <20mm (92%). Only 1 (1.5%) patient had a TAD measuring >25mm (Table 1).
Table 1.
Bivariate analysis: Characteristics of the study population.
| Parameter | Incidence (%) |
|---|---|
| Total | 65 |
| Age (yr) | 73.3 ± 15.4 |
| Sex | |
| Female | 48 (74) |
| Male | 17 (26) |
| BMI | 23.6 ± 6.2 |
| OTA/AO Fracture Classification | |
| 31A1.2 | 3 (4.6) |
| 31A1.3 | 3 (4.6) |
| 31A2.2 | 20 (30.8) |
| 31A2.3 | 14 (21.5) |
| 31A3.3 | 7 (10.8) |
| 31B3 | 3 (4.6) |
| 32A1.a | 5 (7.7) |
| 32A2.b | 1 (1.5) |
| 32B2.a | 1 (1.5) |
| No fracture | 8 (12.3) |
| Fixation Device | |
| CMN nail with compression screw | 65 (100) |
| TRIGEN™ INTERTAN™ | 56 (86) |
| TRIGEN™ META-TAN™ | 9 (14) |
| TAD | 15.1 ± 3.3 |
| <15mm | 37 (56.9) |
| 15–20mm | 23 (35.4) |
| 21–25mm | 4 (6.2) |
| >25mm | 1 (1.5) |
TAD: tip-apex-distance; CMN: cephalomedullary nail; mm: millimeters; BMI: body mass index; OTA: Orthopaedic Trauma Association.
3. Discussion
Confirmation of appropriate 3-dimensional positioning of the guide wire and lag screw within the femoral head can be difficult to ascertain intraoperatively due to obstruction by the jig on the lateral radiograph. We have described a technical trick that allows for a non-obstructed view of guide wire placement within the femoral neck and femoral head. By rotating the C-arm 10–15° in both directions away from the lateral view, the orientation of the tip of the guide wire and its relation to the apex of the femoral head can be discerned.
A TAD of >25mm is a predictor of lag screw-cut out when using intramedullary nails.3, 4, 5,7 Geller et al. found an average TAD of 20±9mm with a cut-out rate of 8.5% in a population undergoing nailing. When stratified by the presence of postoperative cut-out, they identified a significantly greater TAD in the cut-out group.2 This is in comparison to our series, which demonstrated an average TAD of 15.1 ± 3.3mm, and only 1 patient (1.5%) with a TAD >25mm. This suggests that our technical trick of obtaining “peek” radiographs intraoperatively may aid in a precise lag-screw placement. A separate study reported screw cut-out in 3.6% and identified TAD as the variable most significantly associated with screw cut-out. Interestingly, they reported higher measurements on the lateral component of the TAD compared to the AP component, suggesting increased difficulty in obtaining appropriate screw placement on the lateral view.4
Lag screw positioning within the femoral head for intramedullary fixation of proximal femur fractures can be difficult to discern intraoperatively on lateral imaging due to view obstruction from jig in some implant systems. We have described a method of obtaining non-obstructed lateral-oblique “peek” views that reliably assist in obtaining adequate TAD measurements when using intramedullary fixation for these fractures.
Disclosure
No external funding was received for this article. This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
CRediT authorship contribution statement
Anna K. Michalowski: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. Richard N. Puzzitiello: Conceptualization, Investigation, Formal analysis, Writing – review & editing. Scott P. Ryan: Conceptualization, Supervision, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Niu E., Yang A., Harris A.H.S., et al. Which fixation device is preferred for surgical treatment of intertrochanteric hip fractures in the United States? A survey of orthopaedic surgeons. Clin Orthop Relat Res. 2015;473(11):3647–3655. doi: 10.1007/s11999-015-4469-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geller J.A., Saifi C., Morrison T.A., et al. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int Orthop. 2010;34(5):719–722. doi: 10.1007/s00264-009-0837-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fujii T., Nakayama S., Hara M., et al. Tip-apex distance is most important of six predictors of screw cutout after internal fixation of intertrochanteric fractures in women. JB JS Open Access. 2017;2(4) doi: 10.2106/JBJS.OA.16.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lobo-Escolar A., Joven E., Iglesias D., et al. Predictive factors for cutting-out in femoral intramedullary nailing. Injury. 2010;41(12):1312–1316. doi: 10.1016/j.injury.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 5.John B., Sharma A., Mahajan A., et al. Tip-apex distance and other predictors of outcome in cephalomedullary nailing of unstable trochanteric fractures. J Clin Orthop Trauma. 2019;10:S88–S94. doi: 10.1016/j.jcot.2019.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baumgaertner M.R., Curtin S.L., Lindskog D.M., et al. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77(7):1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Strauss E., Frank J., Lee J., et al. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006;37(10):984–989. doi: 10.1016/j.injury.2006.06.008. [DOI] [PubMed] [Google Scholar]